a realistic approach to emergency anticipatory care planning
















- Slides: 55

- a realistic approach to emergency anticipatory care planning Dr Juliet Spiller Consultant in Palliative Medicine Marie Curie Hospice Edinburgh Juliet. spiller@mariecurie. org. uk @JASpiller

q What is Re. SPECT? q Where Re. SPECT come from and why? q Forth Valley experience q Supporting realistic patient choice – explaining prognostic uncertainty, risk benefit balance,

What is ? www. respectprocess. org. uk

What is ? Re. SPECT is a process, it is not a form
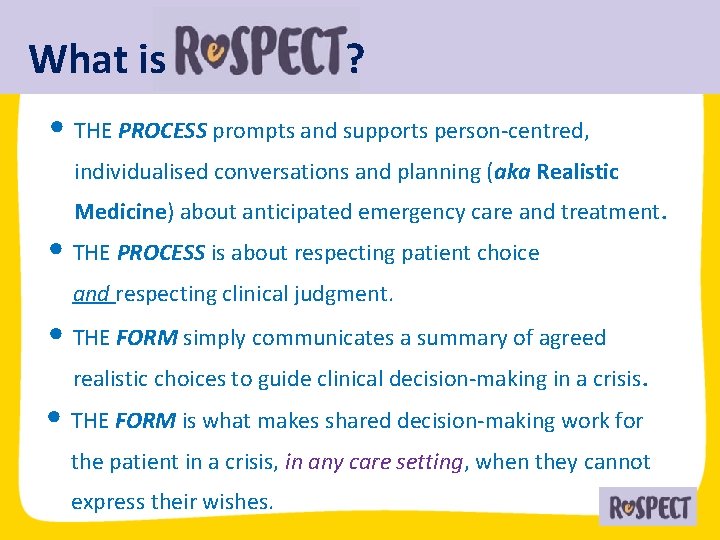
What is ? • THE PROCESS prompts and supports person-centred, individualised conversations and planning (aka Realistic Medicine) about anticipated emergency care and treatment. • THE PROCESS is about respecting patient choice and respecting clinical judgment. • THE FORM simply communicates a summary of agreed realistic choices to guide clinical decision-making in a crisis. • THE FORM is what makes shared decision-making work for the patient in a crisis, in any care setting, when they cannot express their wishes.
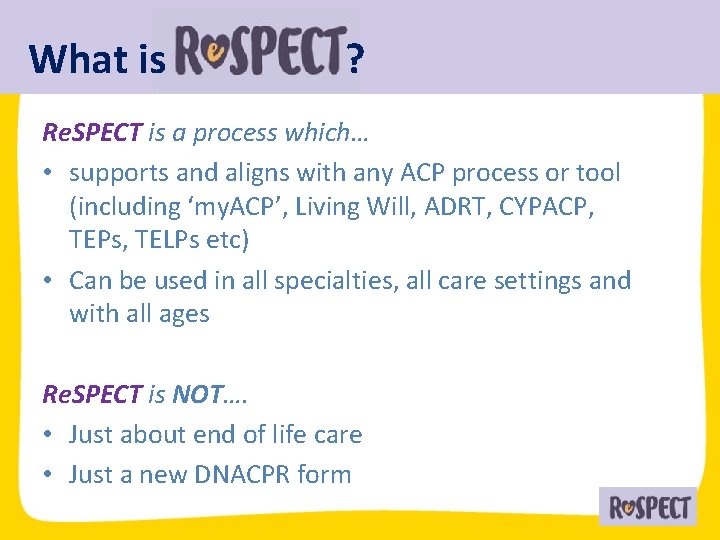
What is ? Re. SPECT is a process which… • supports and aligns with any ACP process or tool (including ‘my. ACP’, Living Will, ADRT, CYPACP, TEPs, TELPs etc) • Can be used in all specialties, all care settings and with all ages Re. SPECT is NOT…. • Just about end of life care • Just a new DNACPR form
- Where did it come from? NCEPOD (2012)– Time to Intervene? • Lack of appropriate advance decision-making • CPR attempted in 52 patients with DNACPR decisions and 7 on end-of-life care pathways CIPOLD (2013) • 42% premature deaths (n=238) • “inappropriate or poorly documented DNACPR orders” contributed to premature unexpected death

- Where did it come from? Court of Appeal – Tracey 2014 “. . . presumption in favour of patient involvement. . . preserving Human Right to information” Winspear v Sunderland NHS FT Where a patient lacks capacity: Involve someone who knows them as long as it is ‘practicable and appropriate’
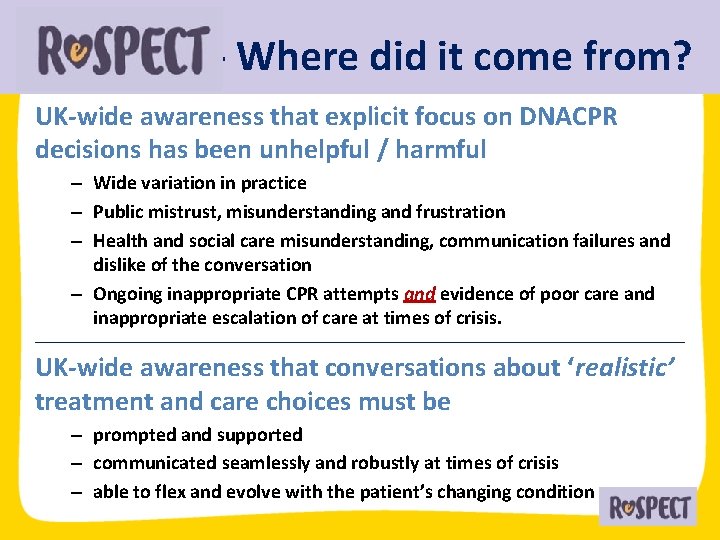
- Where did it come from? UK-wide awareness that explicit focus on DNACPR decisions has been unhelpful / harmful – Wide variation in practice – Public mistrust, misunderstanding and frustration – Health and social care misunderstanding, communication failures and dislike of the conversation – Ongoing inappropriate CPR attempts and evidence of poor care and inappropriate escalation of care at times of crisis. ___________________________________________________________ UK-wide awareness that conversations about ‘realistic’ treatment and care choices must be – prompted and supported – communicated seamlessly and robustly at times of crisis – able to flex and evolve with the patient’s changing condition
- Where did it come from? • 2015 Working group set up by RC(UK), BMA, GMC, RCN • Representatives from 37 patient and clinical organisations • Sponsored by Resuscitation Council UK • Additional funding from RCN, Macmillan and Scottish Government for specific workstreams • Public and stakeholder consultation • Early usability Pilots (acute, care home, hospice, paeds) • Early adopter evaluation (Acute) funded by NIHR • Design input from Helix

is not (just) a form its a process “We didn’t redesign a form. We redesigned a relationship” Ivor Williams – Helix centre Designing the form to support the process ‘Designing in’ the conversation(s) • Clarifies outcomes patients wish for and those they fear • Clarifies realistic treatment options • Summarises person-centred and realistic patient wishes for emergency care and treatment

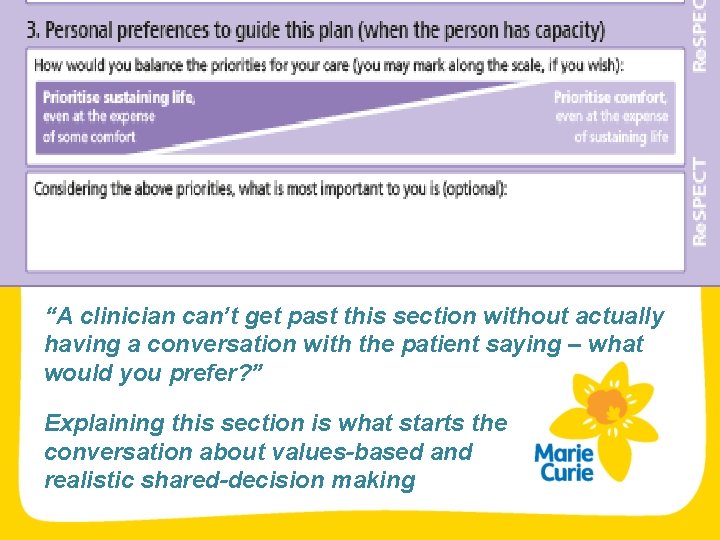
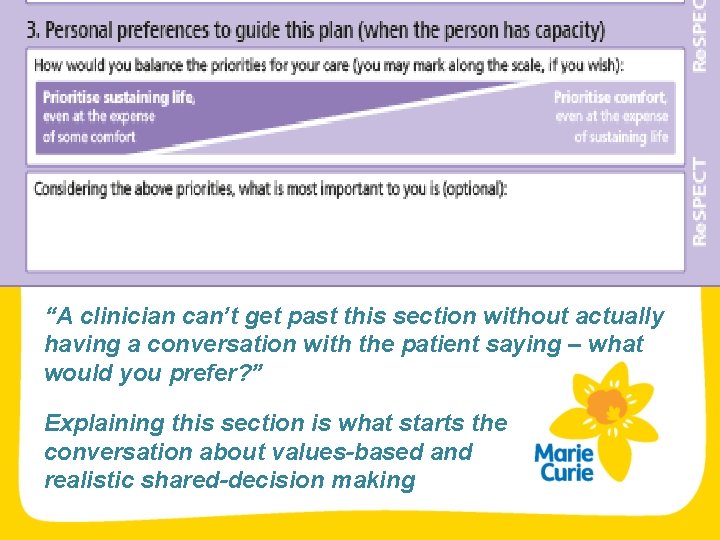
“A clinician can’t get past this section without actually having a conversation with the patient saying – what would you prefer? ” Explaining this section is what starts the conversation about values-based and realistic shared-decision making

Adoption in the UK. • Launched for use in Feb 2017 • 6 early adopter sites (Warwickshire/Coventry was first) • Currently 7 CCGs, 14 Acute/Foundation Trusts, 1 Community Health Service/ 1 Health Board (Forth Valley) • Planned for 2019, 31 Acute Trusts & CCGs, and NHS Borders
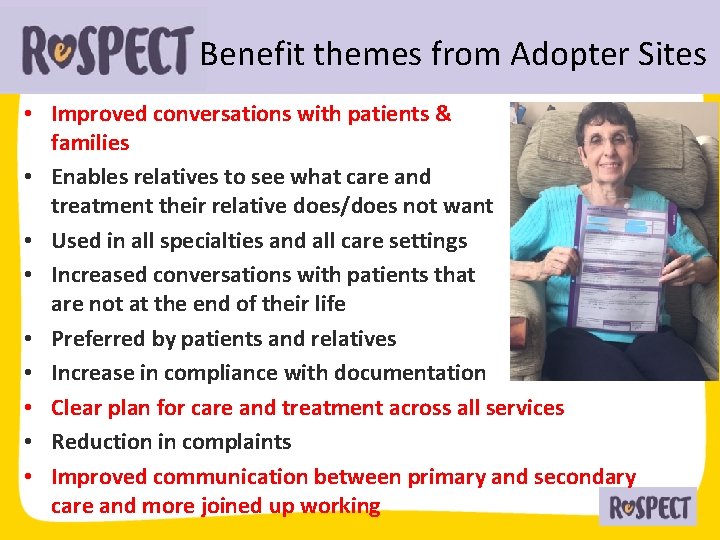
Benefit themes from Adopter Sites • Improved conversations with patients & families • Enables relatives to see what care and treatment their relative does/does not want • Used in all specialties and all care settings • Increased conversations with patients that are not at the end of their life • Preferred by patients and relatives • Increase in compliance with documentation • Clear plan for care and treatment across all services • Reduction in complaints • Improved communication between primary and secondary care and more joined up working

Forth Valley experience • Pilot started in September 2017 • Small test of change in 4 areas (older adult ward, mental health ward, day hospice, primary care) Pilot preparation • Re. SPECT Steering Group with Executive Sponsor • Wider education • Quality Improvement Support- Measurement Framework • Utilise existing electronic systems • Establish email address for correspondence • Use alongside DNACPR documentation where appropriate • Remove pre-existing HACP

Overall Aims of Re. SPECT Pilot • To test the Re. SPECT process Emergency Care Planning • Up to Date • Useful • Easily accessible Earlier conversations • Person Centred Care • Shared decision making
Forth Valley experience • • • Main Pilot Ward Identification at MDT or ward round Sticker as prompt Conversation (initially consultants only) Complete form, scan and email to fv-uhb. respect@nhs. net Communicated in IDL and GP to update Ki. S
Forth Valley experience • • • Naturally the process widened beyond initial pilot area Education - App - Drop in Sessions/Hospital/Departmental Meetings - Staff Intranet/Email Re. SPECT nurse (1 day per week) Challenges • staff turnover, • process evolving • keeping up to date • fast moving snowball effect • resistance to change • refine electronic process • overlap with KIS
Measurement Framework Emphasis on Qualitative Feedback • Patient/Relatives • Carers Forum • Staff Form Analysis • Qualitative/Quantitative Outcomes • KIS updated within 1 month discharge • Time at home • Place of death
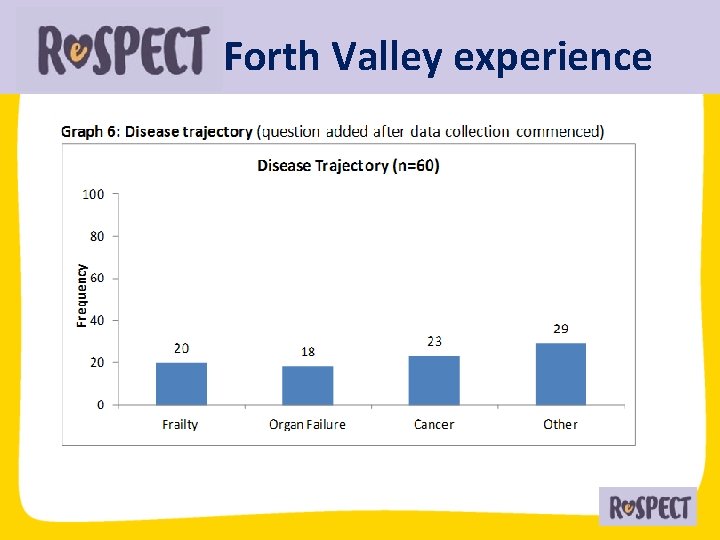
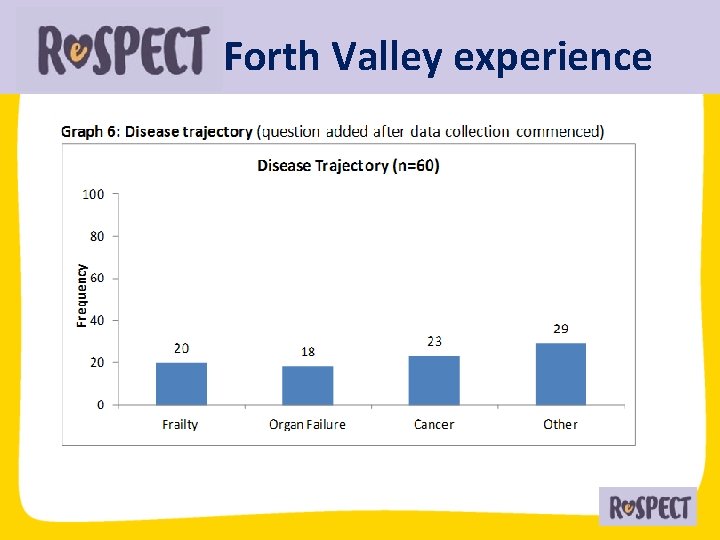
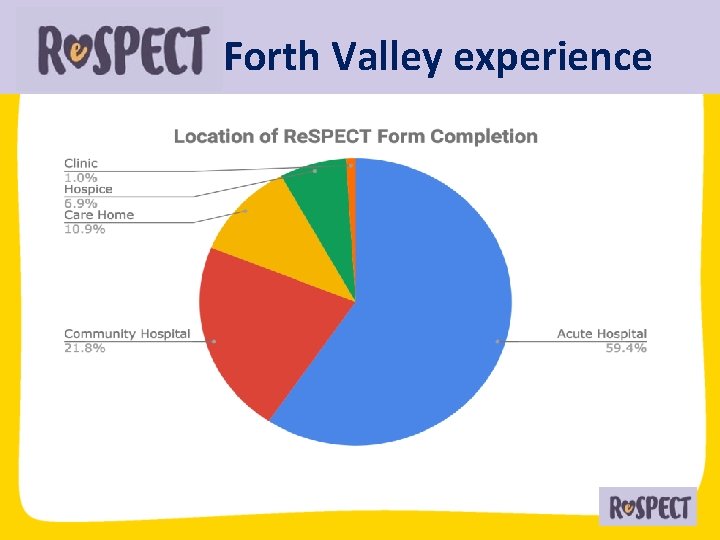
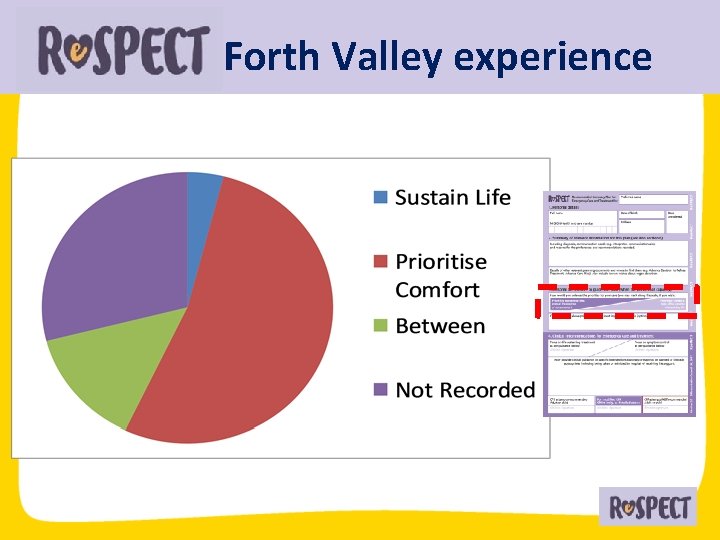
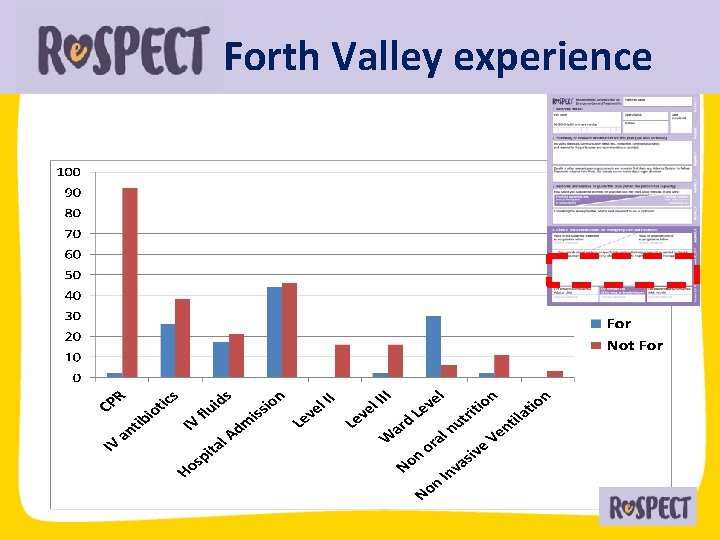
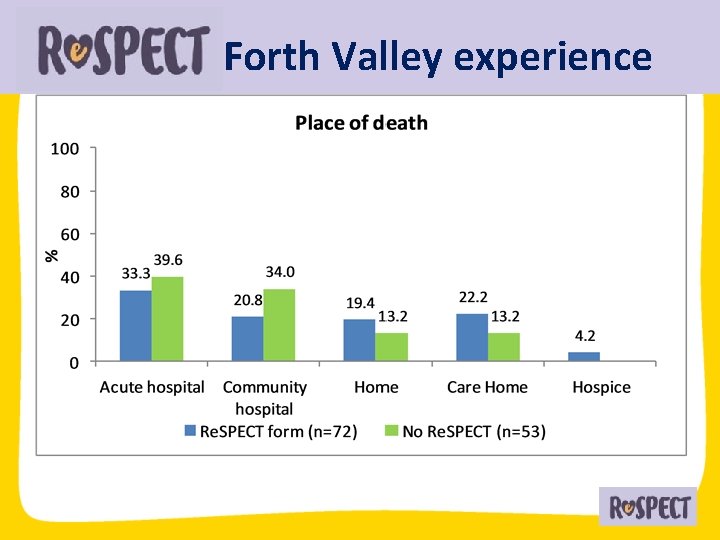
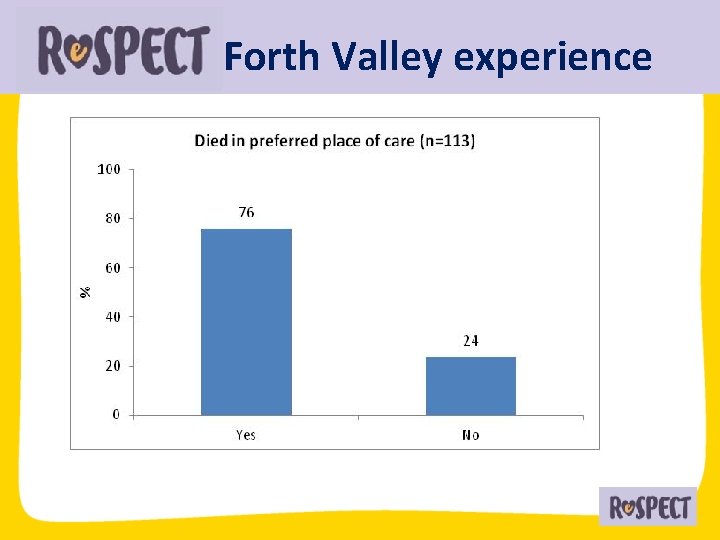
Forth Valley experience
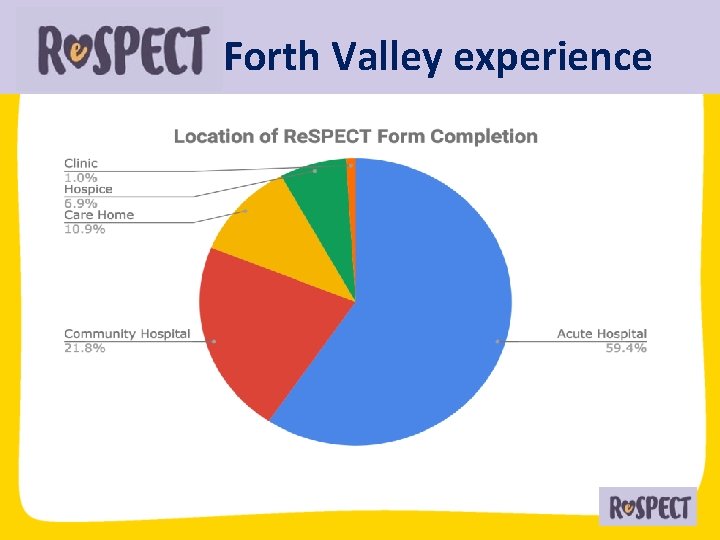
Forth Valley experience
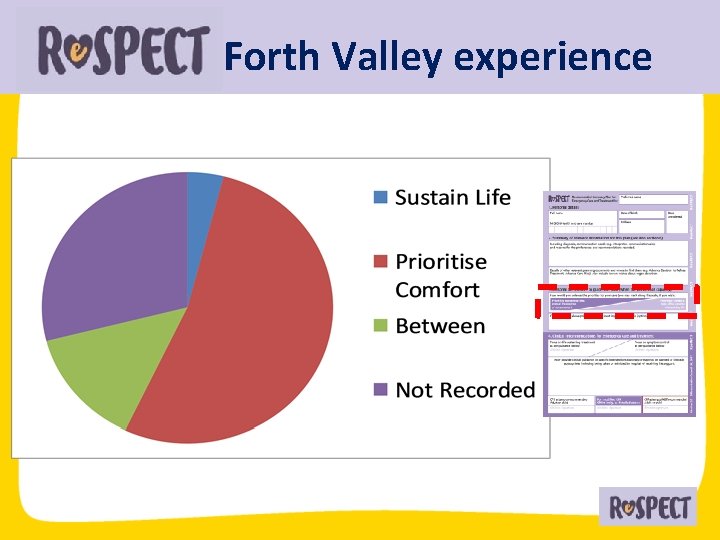
Forth Valley experience
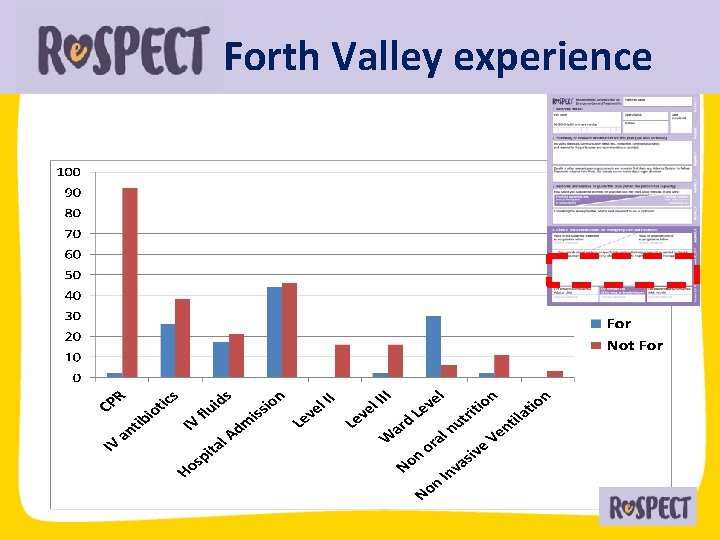
Forth Valley experience
Forth Valley experience • 100% involved in discussions • Improved communication in IDL needed • Ki. S not always updated (70% at 1 month)
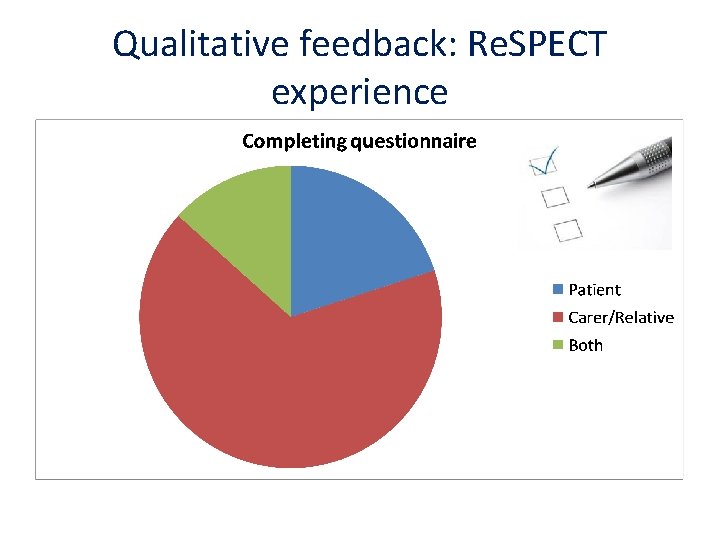
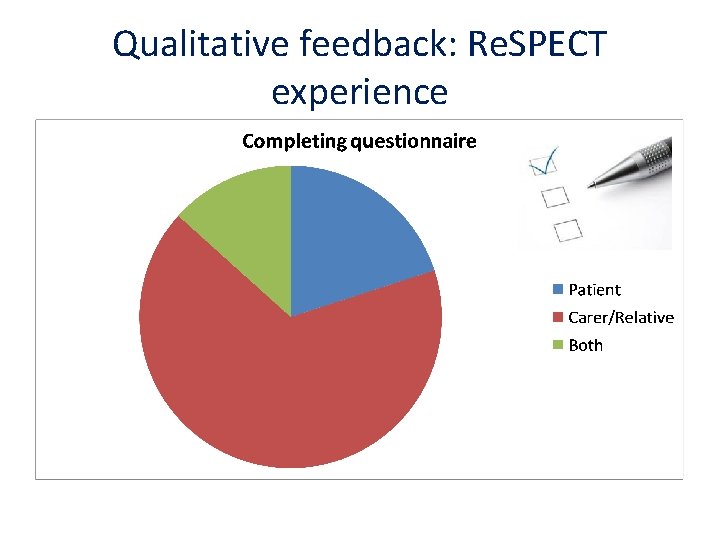
Qualitative feedback: Re. SPECT experience
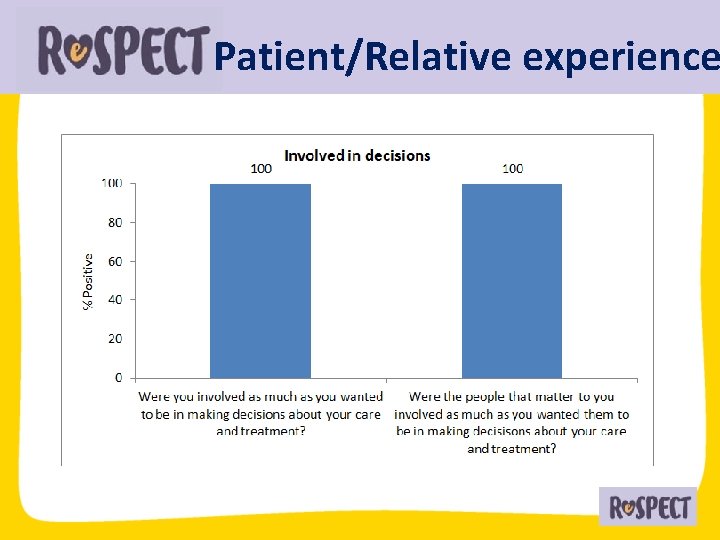
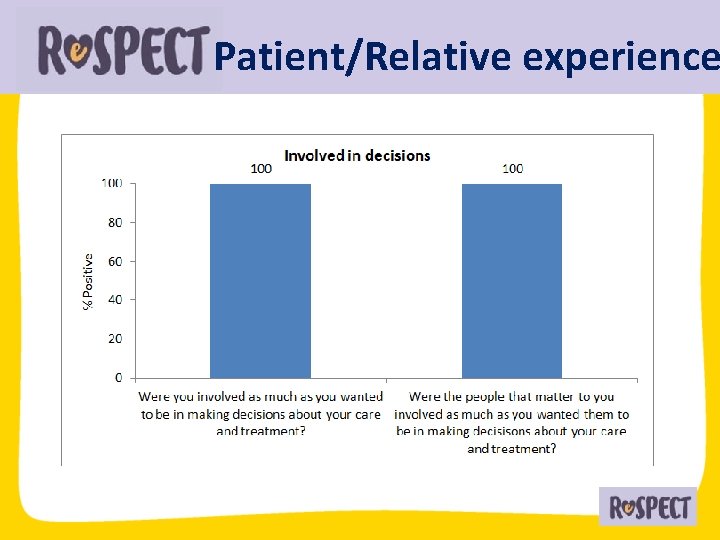
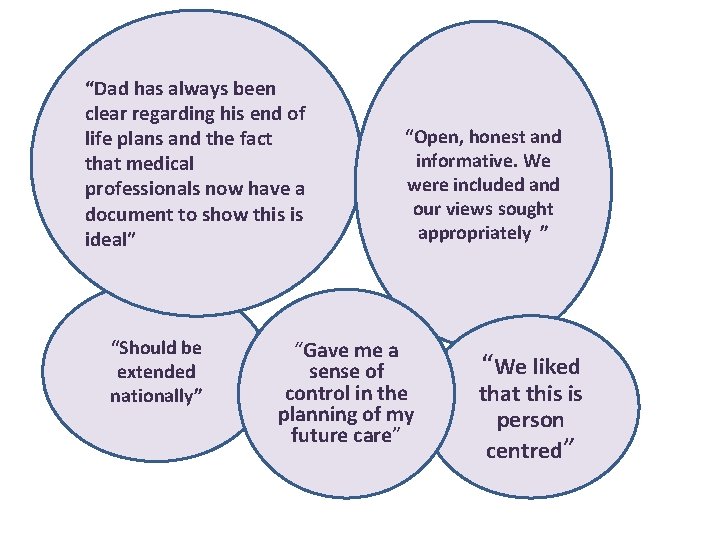
Patient/Relative experience
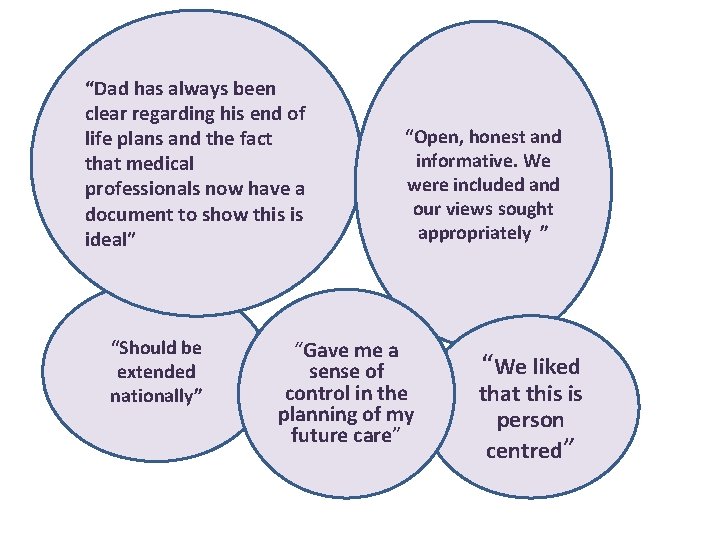
“Dad has always been clear regarding his end of life plans and the fact that medical professionals now have a document to show this is ideal” “Should be extended nationally” “Open, honest and informative. We were included and our views sought appropriately ” “Gave me a sense of control in the planning of my future care” “We liked that this is person centred”
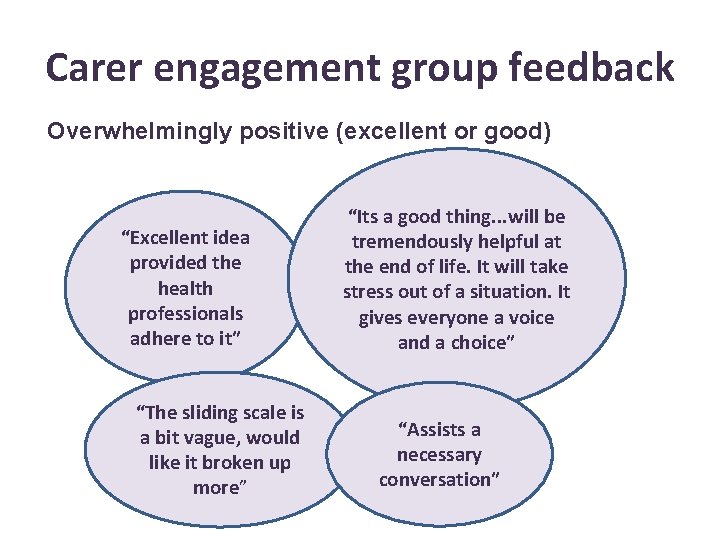
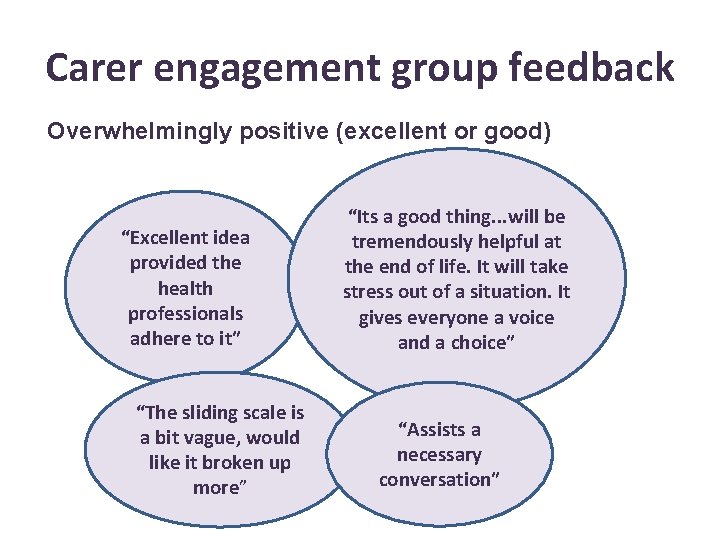
Carer engagement group feedback Overwhelmingly positive (excellent or good) “Excellent idea provided the health professionals adhere to it” “The sliding scale is a bit vague, would like it broken up more” “Its a good thing. . . will be tremendously helpful at the end of life. It will take stress out of a situation. It gives everyone a voice and a choice” “Assists a necessary conversation”
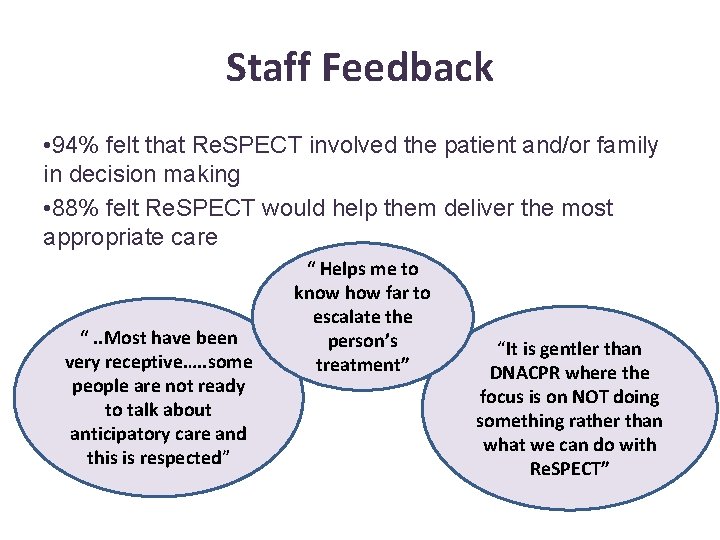
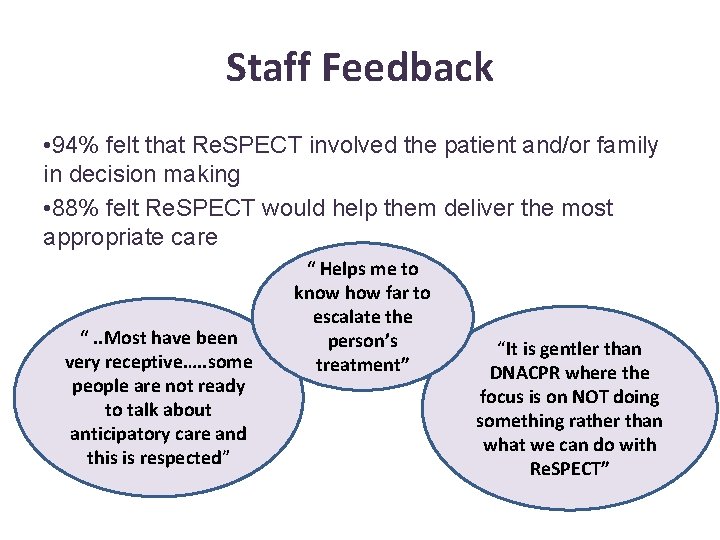
Staff Feedback • 94% felt that Re. SPECT involved the patient and/or family in decision making • 88% felt Re. SPECT would help them deliver the most appropriate care “. . Most have been very receptive…. . some people are not ready to talk about anticipatory care and this is respected” “ Helps me to know how far to escalate the person’s treatment” “It is gentler than DNACPR where the focus is on NOT doing something rather than what we can do with Re. SPECT”
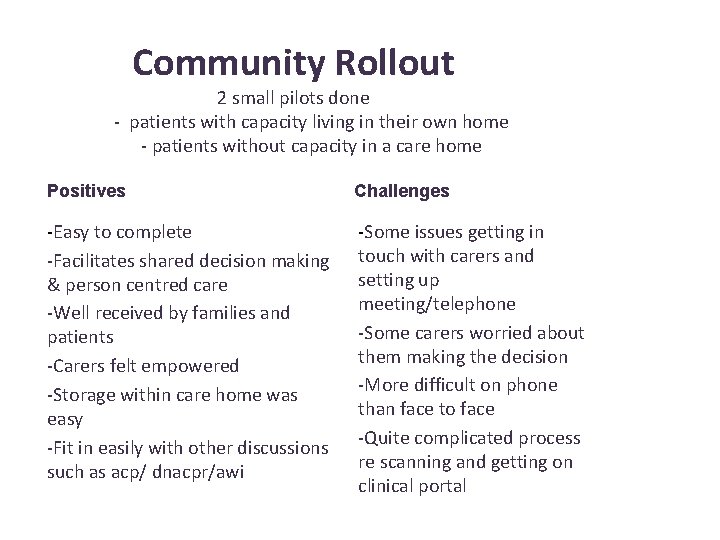
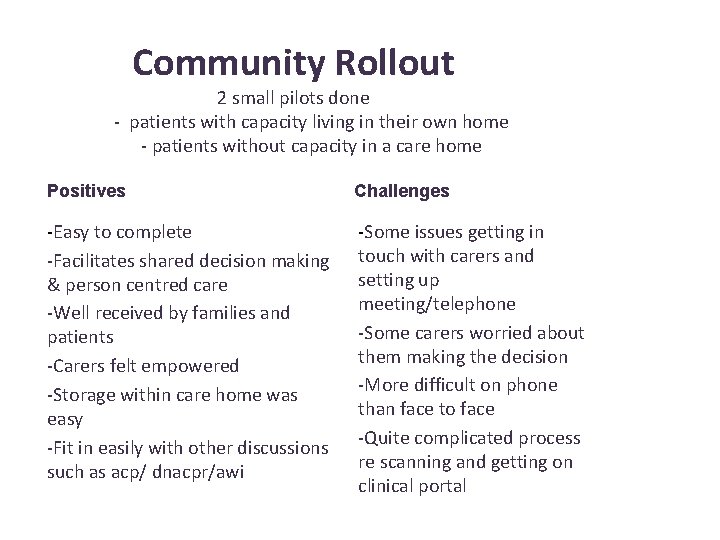
Community Rollout 2 small pilots done - patients with capacity living in their own home - patients without capacity in a care home Positives Challenges -Easy to complete -Facilitates shared decision making & person centred care -Well received by families and patients -Carers felt empowered -Storage within care home was easy -Fit in easily with other discussions such as acp/ dnacpr/awi -Some issues getting in touch with carers and setting up meeting/telephone -Some carers worried about them making the decision -More difficult on phone than face to face -Quite complicated process re scanning and getting on clinical portal

Early Outcome Data

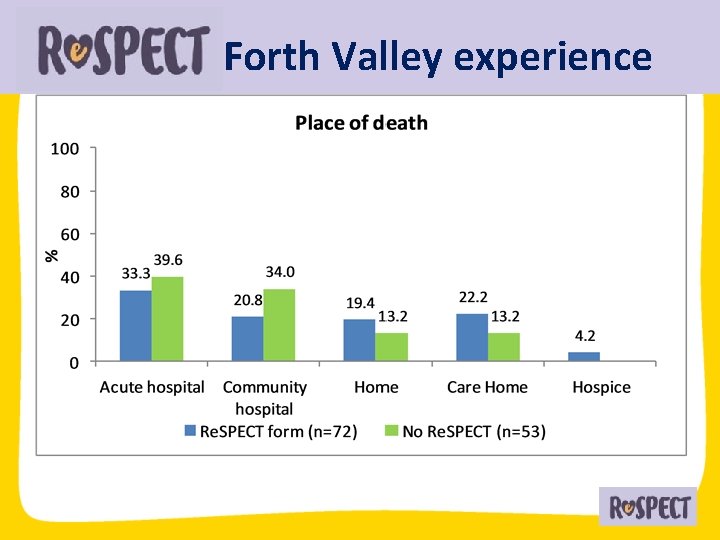
Forth Valley experience
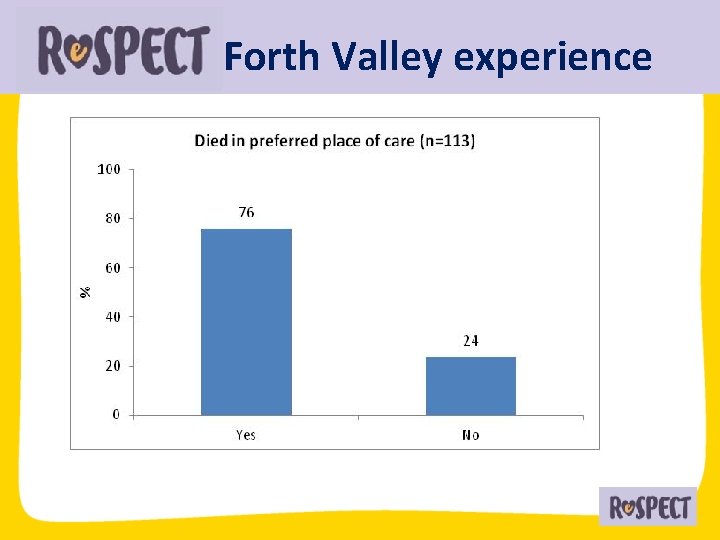
Forth Valley experience

Forth Valley experience • Patient Preference • Person Centred • Provides a standardised approach cf. KIS • Summary • Stays with patient • More clinicians can create plans • • • Positive Feedback Facilitates involvement of the person and those close to them Accessible to more people to view Collaboration Outcomes Maintaining the integrity of the Process is key in project management!

Currently. . üCurrently being rolled out across hospital, primary care, hospice üIntranet page üEducation and engagement events üIntegrated in WSW and Nursing Home L. E. S üIntegrated into existing electronic systems üShare good practice in other areas üSupporting good communication WE NEED YOU!!
Next Steps • • • Re. SPECT as a stand alone document Improve electronic systems Adapt to ‘paper light’ system Increase project management Promotional video

Follow Our Progress @lynseyfielden 1
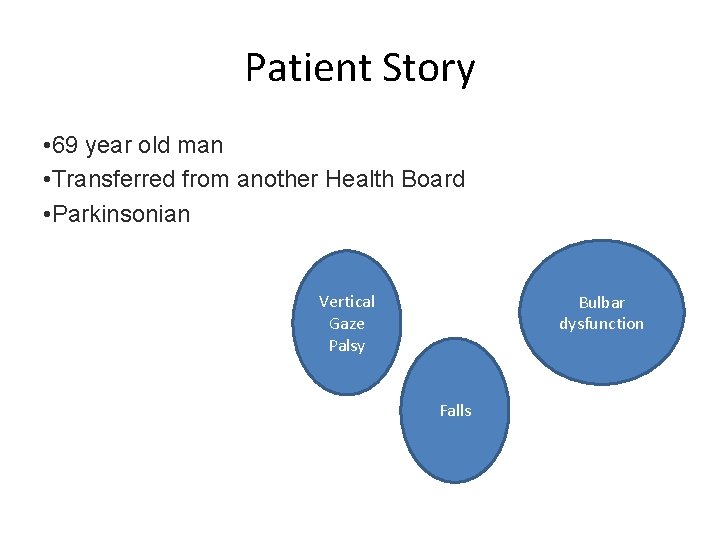
Patient Story • 69 year old man • Transferred from another Health Board • Parkinsonian Vertical Gaze Palsy Bulbar dysfunction Falls
Progressive Supranuclear palsy • Neurodegenerative disorder ‘Parkinson’s Plus’ • Tauopathy • Marked Bulbar Dysfunction • Falls • Vertical gaze palsy • Doesn’t respond well to usual treatment • Cognition usually intact
Hospital admission • The first encounter is as an acute admission • Awaiting OP clinic • Aspiration pneumonia • Bulbar dysfunction • Communication challenging
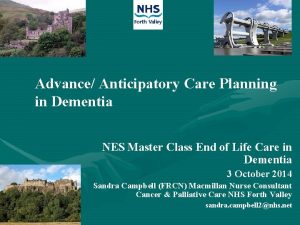
How do we embark on ACP? • Appropriate for ACP? • Timing? • Who do we need to involve
Prepare • Clarify the persons capacity (remember it is decision-specific) • What is important to them? What would matter in an emergency? “What outcomes would you value/ What outcomes would you fear? ” • Who is important to them? • What other clinical information is required? • Consider from a clinicians perspective what would be important to discuss • What tools are you going to use to support this? • Are there any religious or cultural beliefs to consider?
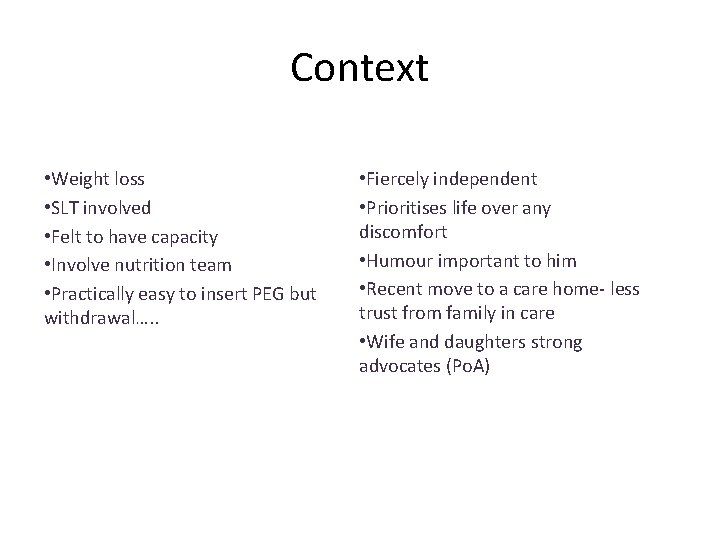
Context • Weight loss • SLT involved • Felt to have capacity • Involve nutrition team • Practically easy to insert PEG but withdrawal…. . • Fiercely independent • Prioritises life over any discomfort • Humour important to him • Recent move to a care home- less trust from family in care • Wife and daughters strong advocates (Po. A)
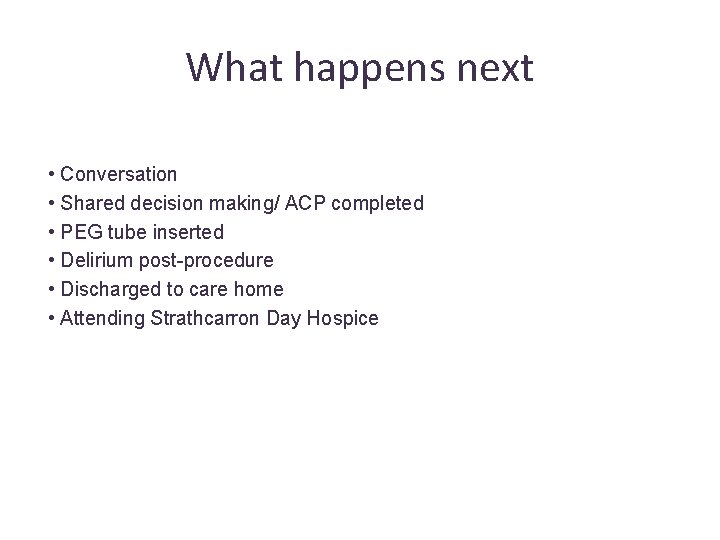
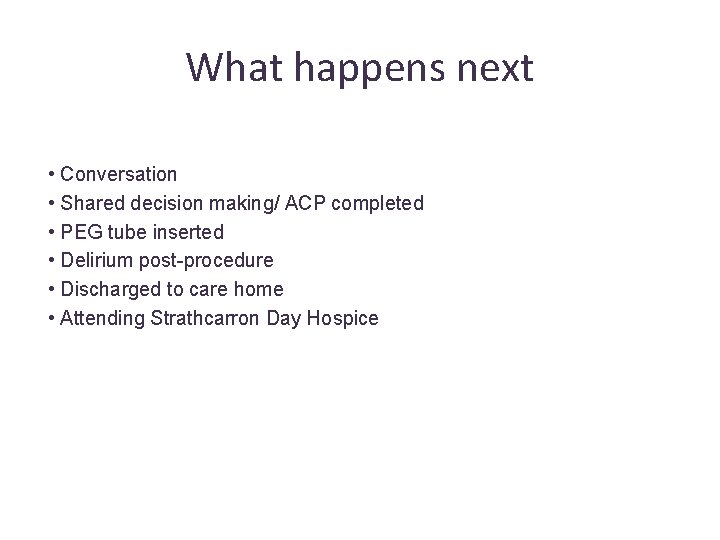
What happens next • Conversation • Shared decision making/ ACP completed • PEG tube inserted • Delirium post-procedure • Discharged to care home • Attending Strathcarron Day Hospice
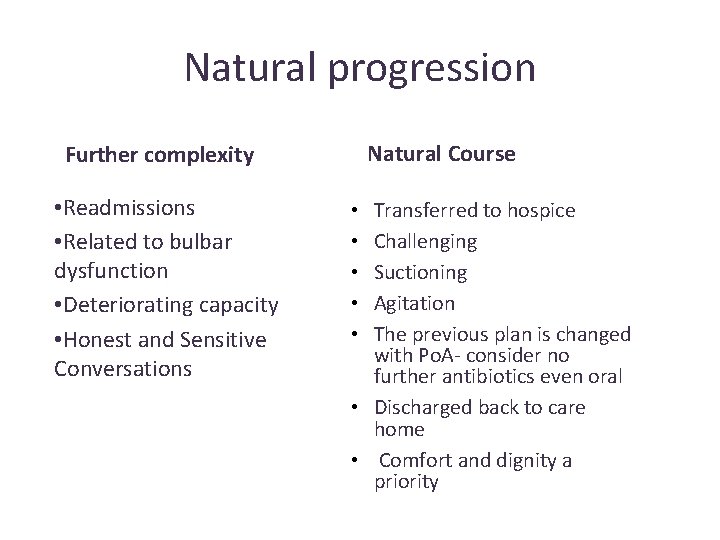
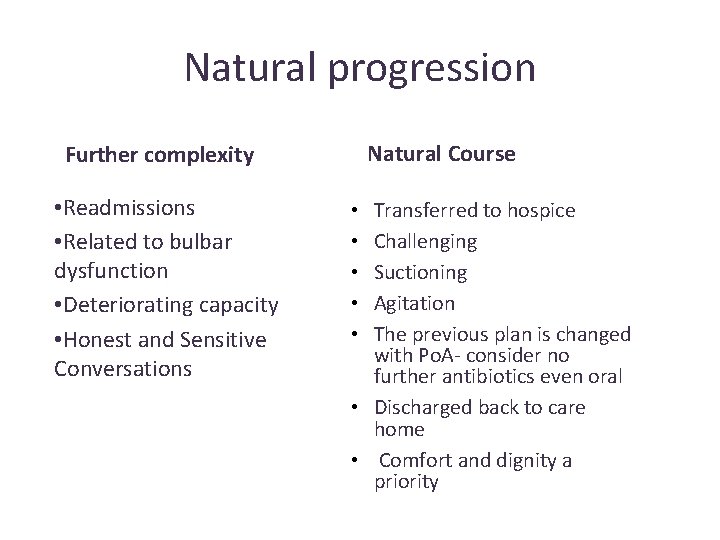
Natural progression Natural Course Further complexity • Readmissions • Related to bulbar dysfunction • Deteriorating capacity • Honest and Sensitive Conversations Transferred to hospice Challenging Suctioning Agitation The previous plan is changed with Po. A- consider no further antibiotics even oral • Discharged back to care home • Comfort and dignity a priority • • •
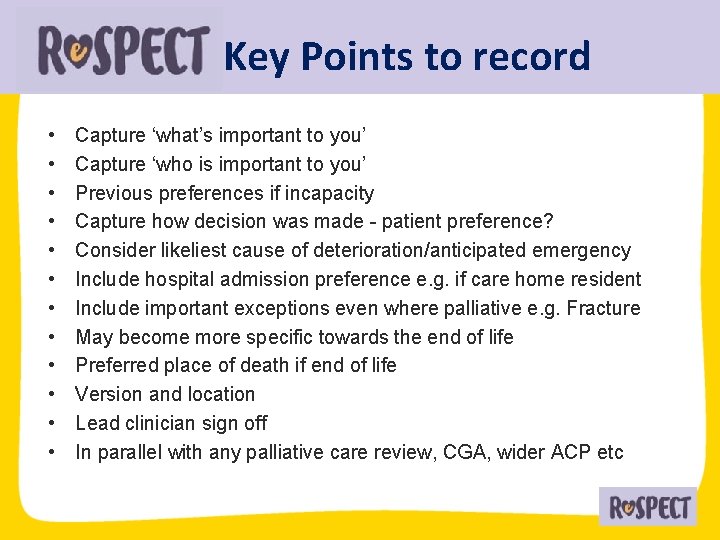
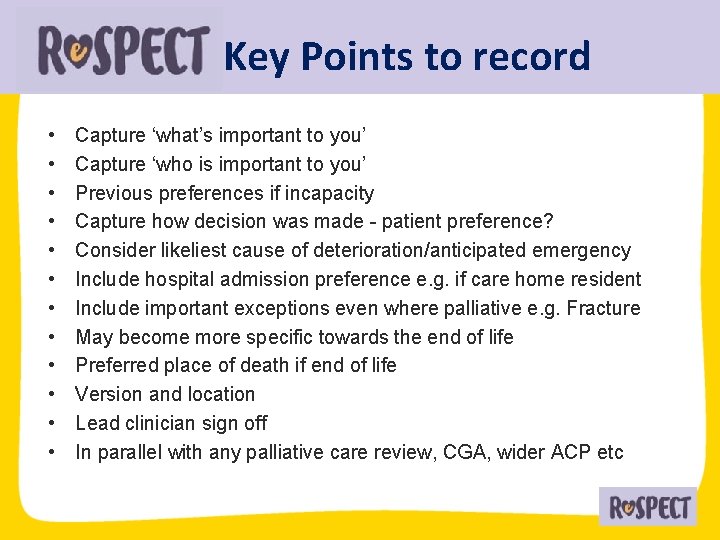
Key Points to record • • • Capture ‘what’s important to you’ Capture ‘who is important to you’ Previous preferences if incapacity Capture how decision was made - patient preference? Consider likeliest cause of deterioration/anticipated emergency Include hospital admission preference e. g. if care home resident Include important exceptions even where palliative e. g. Fracture May become more specific towards the end of life Preferred place of death if end of life Version and location Lead clinician sign off In parallel with any palliative care review, CGA, wider ACP etc
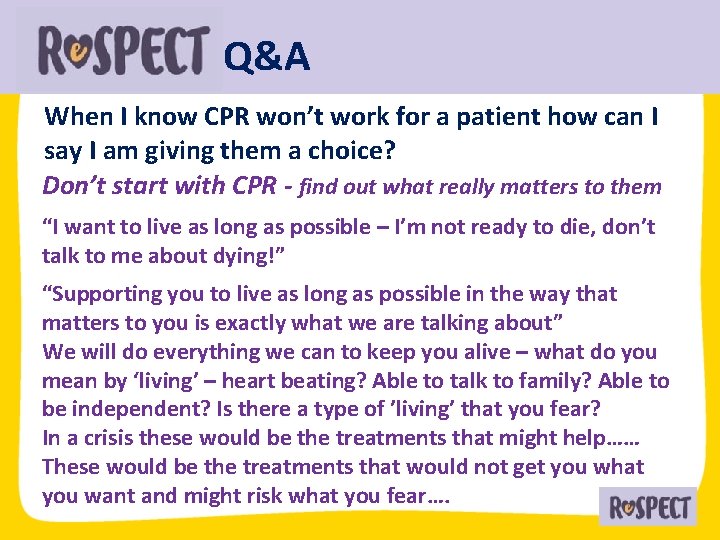
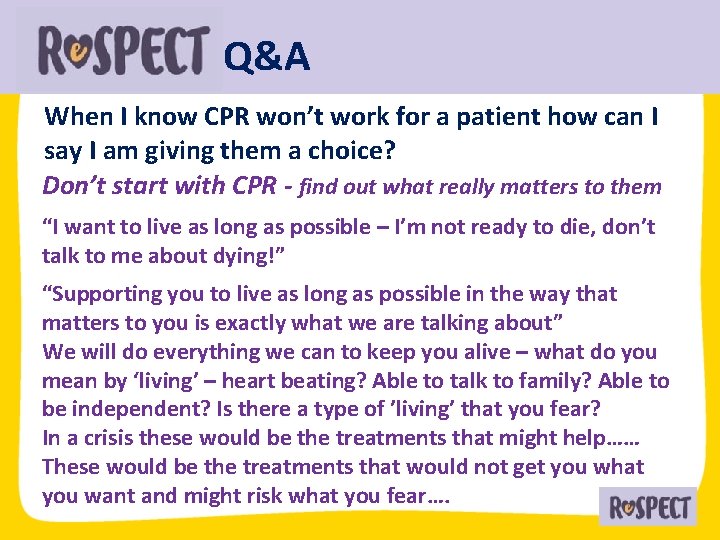
Q&A When I know CPR won’t work for a patient how can I say I am giving them a choice? Don’t start with CPR - find out what really matters to them “I want to live as long as possible – I’m not ready to die, don’t talk to me about dying!” “Supporting you to live as long as possible in the way that matters to you is exactly what we are talking about” We will do everything we can to keep you alive – what do you mean by ‘living’ – heart beating? Able to talk to family? Able to be independent? Is there a type of ’living’ that you fear? In a crisis these would be the treatments that might help…… These would be the treatments that would not get you what you want and might risk what you fear….
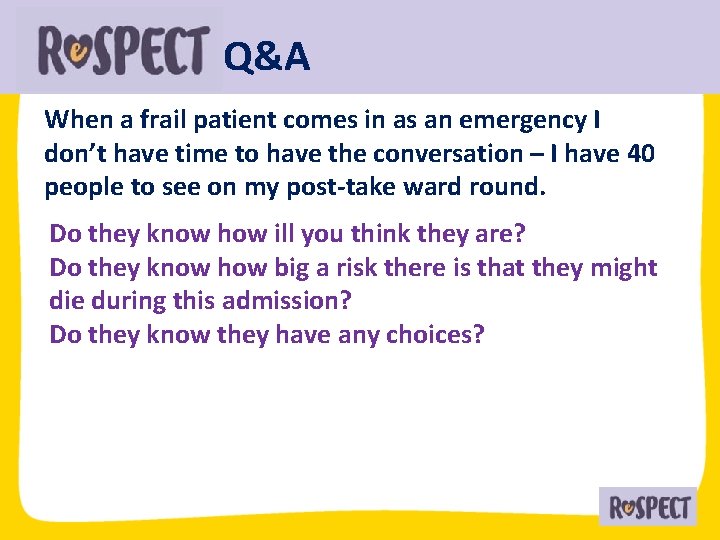
Q&A When a frail patient comes in as an emergency I don’t have time to have the conversation – I have 40 people to see on my post-take ward round. Do they know how ill you think they are? Do they know how big a risk there is that they might die during this admission? Do they know they have any choices?
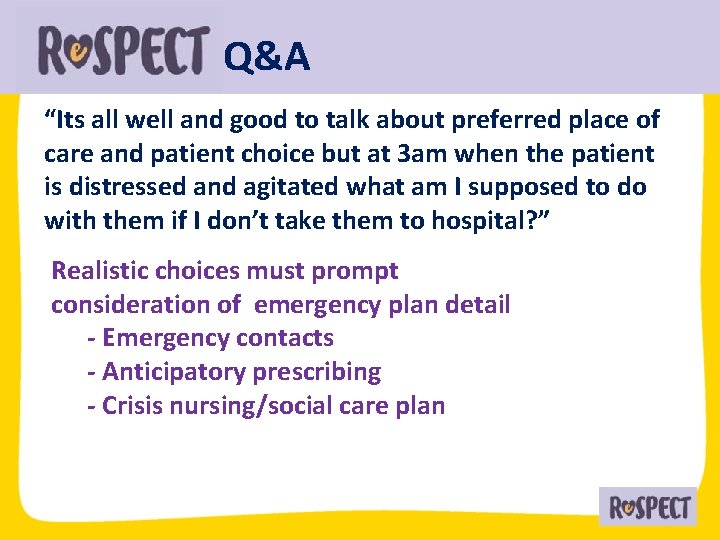
Q&A “Its all well and good to talk about preferred place of care and patient choice but at 3 am when the patient is distressed and agitated what am I supposed to do with them if I don’t take them to hospital? ” Realistic choices must prompt consideration of emergency plan detail - Emergency contacts - Anticipatory prescribing - Crisis nursing/social care plan
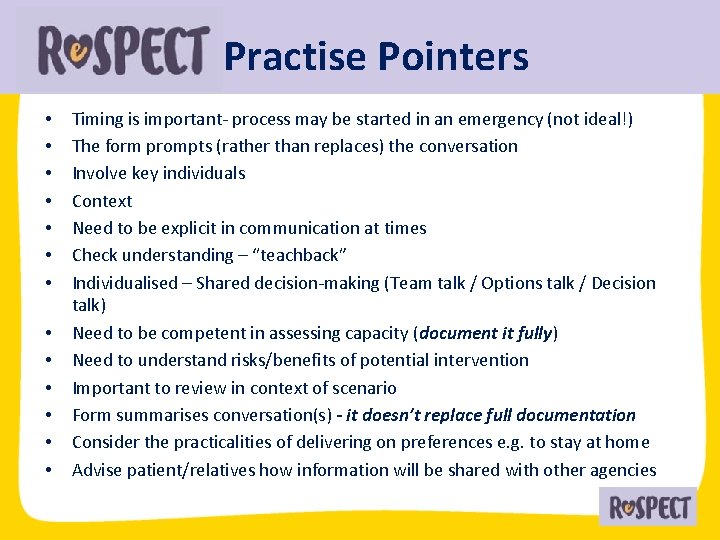
Practise Pointers • • • • Timing is important- process may be started in an emergency (not ideal!) The form prompts (rather than replaces) the conversation Involve key individuals Context Need to be explicit in communication at times Check understanding – “teachback” Individualised – Shared decision-making (Team talk / Options talk / Decision talk) Need to be competent in assessing capacity (document it fully) Need to understand risks/benefits of potential intervention Important to review in context of scenario Form summarises conversation(s) - it doesn’t replace full documentation Consider the practicalities of delivering on preferences e. g. to stay at home Advise patient/relatives how information will be shared with other agencies
Key Points • Re. SPECT and ACP are complementary processes • Re. SPECT is not just about end of life care • Re. SPECT links realistic emergency care options /choices with what is of value to the patient • Significant Health Literacy and communication skills & culture challenges need to be addressed • KIS can be optimised to communicate Re. SPECT information but system-wide open. EHR integration is essential to make planning work for the patient in the crisis

For more information; Re. SPECT clinical lead; catherine. baldock@resus. org. uk Website; www. respectprocess. org. uk Scottish Re. SPECT collaborative; Jamie. begbie@gov. uk
 Sue marsden
Sue marsden Anticipatory care definition
Anticipatory care definition Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary Why is socialization a lifelong process
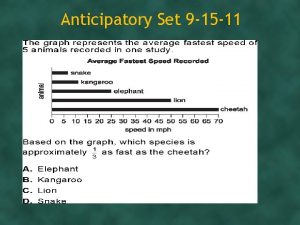
Why is socialization a lifelong process Define anticipatory set
Define anticipatory set Example of anticipatory socialization
Example of anticipatory socialization Example of anticipatory socialization
Example of anticipatory socialization What is meant by resocialization
What is meant by resocialization Anticipatory set
Anticipatory set Anticipatory guidance for adults
Anticipatory guidance for adults Desocialization definition
Desocialization definition Anticipatory guidance for autism
Anticipatory guidance for autism Anticipatory set examples
Anticipatory set examples Anticipatory governance definition
Anticipatory governance definition Leaflet anticipatory guidance
Leaflet anticipatory guidance What is anticipatory bail
What is anticipatory bail Define anticipatory set
Define anticipatory set Who emergency care system framework
Who emergency care system framework Prehospital emergency care 10th edition
Prehospital emergency care 10th edition Pre-hospital communication
Pre-hospital communication Pa wc bureau
Pa wc bureau Emergency care enfield
Emergency care enfield Emergency care 13th edition chapter 1
Emergency care 13th edition chapter 1 Chapter 7 emergency care and disaster preparation
Chapter 7 emergency care and disaster preparation Chapter 54 basic emergency care
Chapter 54 basic emergency care Outdoor emergency care 6th edition
Outdoor emergency care 6th edition Care for a victim of an immunologic emergency
Care for a victim of an immunologic emergency Nhs 7 pillars
Nhs 7 pillars Chapter 8 emergency care first aid and disasters
Chapter 8 emergency care first aid and disasters Emergency care and disaster preparation chapter 7
Emergency care and disaster preparation chapter 7 Prehospital emergency care 11th edition chapter 1
Prehospital emergency care 11th edition chapter 1 Prehospital emergency care 11th edition study guide
Prehospital emergency care 11th edition study guide Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Golden rules of emergency care
Golden rules of emergency care Introduction to emergency medical care
Introduction to emergency medical care Emergency care harrow
Emergency care harrow Interagency integrated triage tool
Interagency integrated triage tool Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Tdh ems
Tdh ems Medical
Medical The goal of modern emergency care includes
The goal of modern emergency care includes Emergency care limmer
Emergency care limmer Introduction to emergency medical care
Introduction to emergency medical care Jigsaw classroom psychology definition
Jigsaw classroom psychology definition Realistic fiction definition
Realistic fiction definition Realistic fiction defintion
Realistic fiction defintion The hello goodbye window summary
The hello goodbye window summary Realistic conflict theory
Realistic conflict theory Realistic conflict theory
Realistic conflict theory Realistic conflict theory
Realistic conflict theory Characteristics of mystery flash fiction
Characteristics of mystery flash fiction Mystery
Mystery Semi abstract mannequin
Semi abstract mannequin Realistic drama characteristics
Realistic drama characteristics Magical realism genre
Magical realism genre Fictional character examples
Fictional character examples