Anticipatory Care Planning Making it Happen Lets Think
- Slides: 17
Anticipatory Care Planning Making it Happen Let’s Think Ahead Janette Barrie National Clinical Lead (Nursing) ACP
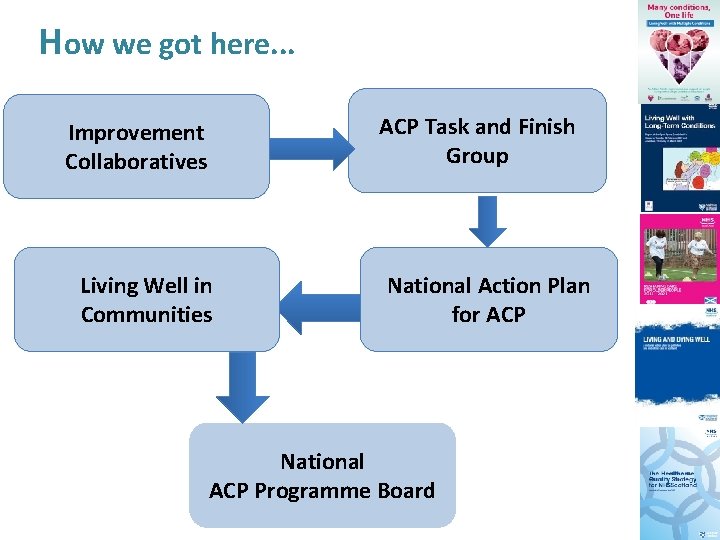
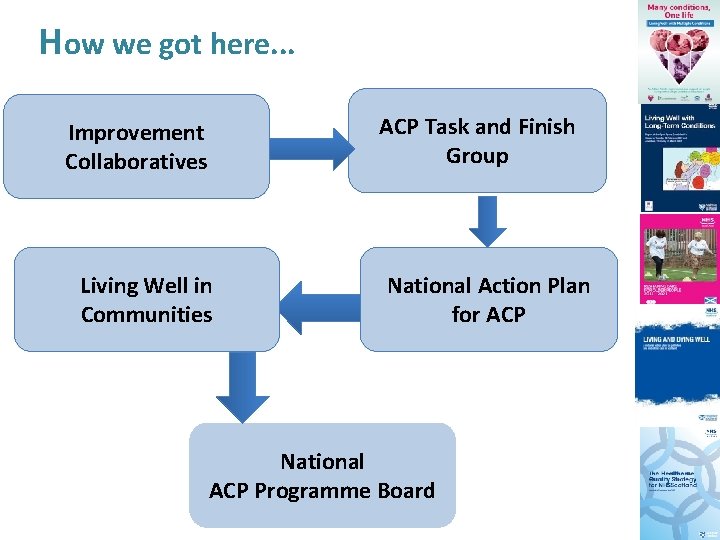
How we got here. . . ACP Task and Finish Group Improvement Collaboratives Living Well in Communities National Action Plan for ACP National ACP Programme Board
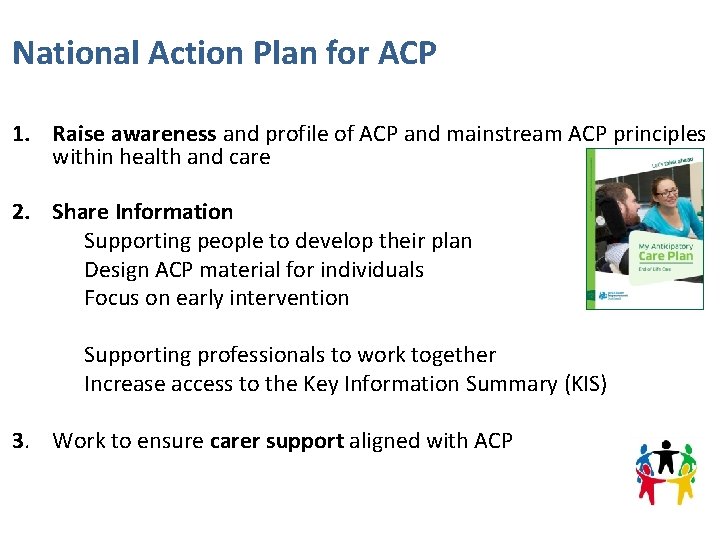
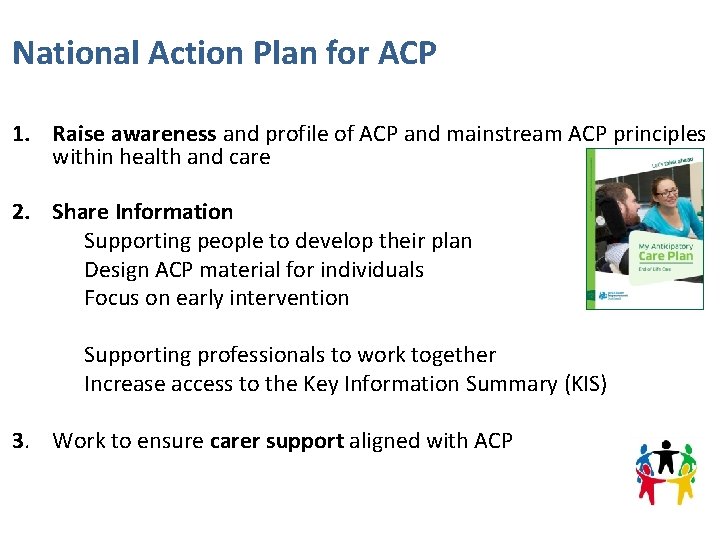
National Action Plan for ACP 1. Raise awareness and profile of ACP and mainstream ACP principles within health and care 2. Share Information Supporting people to develop their plan Design ACP material for individuals Focus on early intervention Supporting professionals to work together Increase access to the Key Information Summary (KIS) 3. Work to ensure carer support aligned with ACP
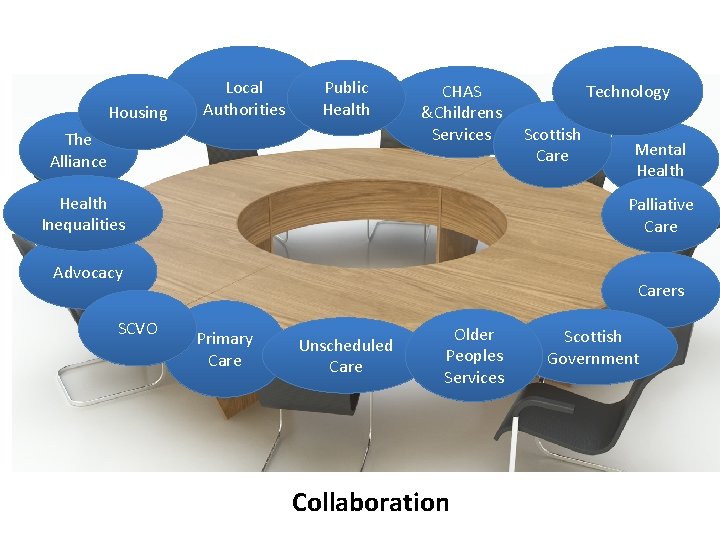
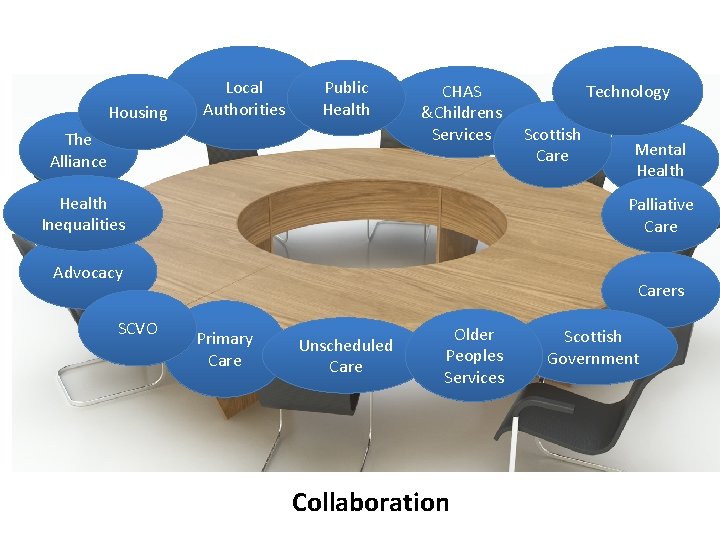
Housing Local Authorities Public Health The Alliance CHAS &Childrens Services Health Inequalities Scottish Care Mental Health Palliative Care Advocacy SCVO Technology Carers Primary Care Unscheduled Care Older Peoples Services Collaboration Scottish Government
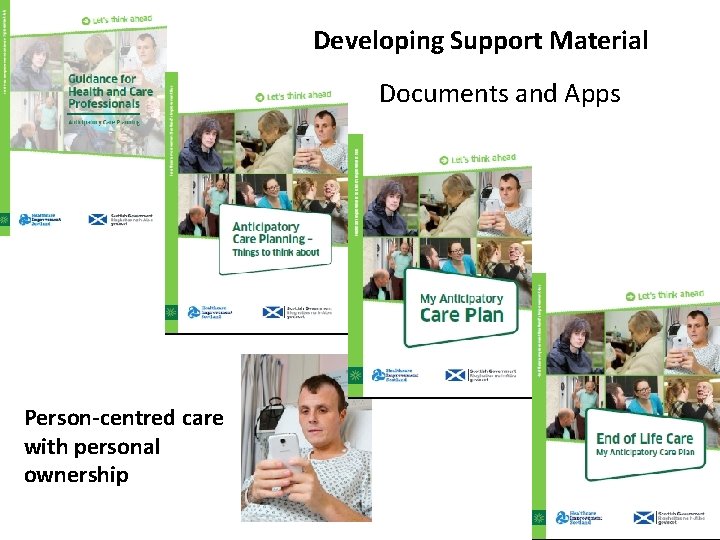
Developing Support Material Documents and Apps Person-centred care with personal ownership
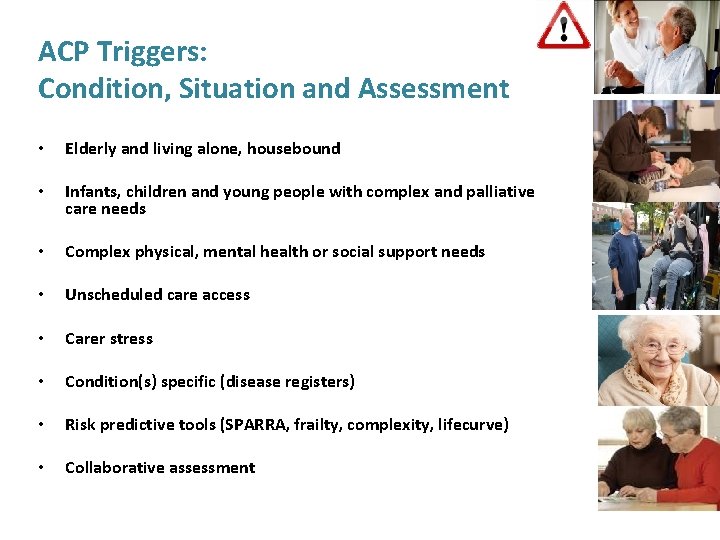
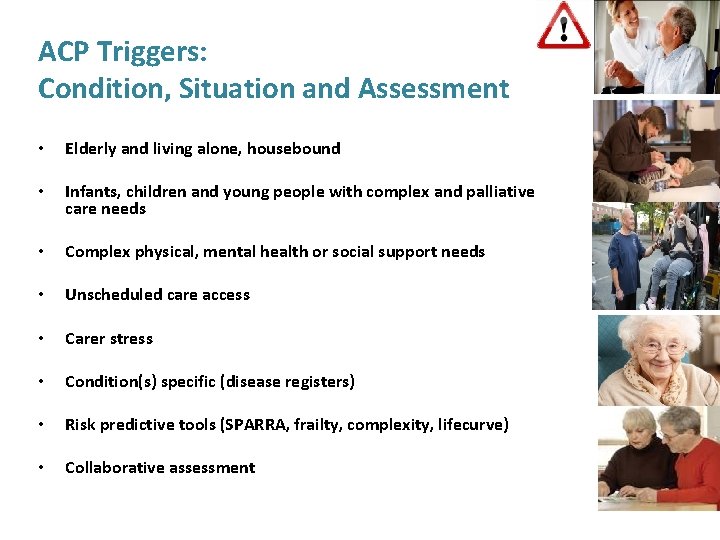
ACP Triggers: Condition, Situation and Assessment • Elderly and living alone, housebound • Infants, children and young people with complex and palliative care needs • Complex physical, mental health or social support needs • Unscheduled care access • Carer stress • Condition(s) specific (disease registers) • Risk predictive tools (SPARRA, frailty, complexity, lifecurve) • Collaborative assessment
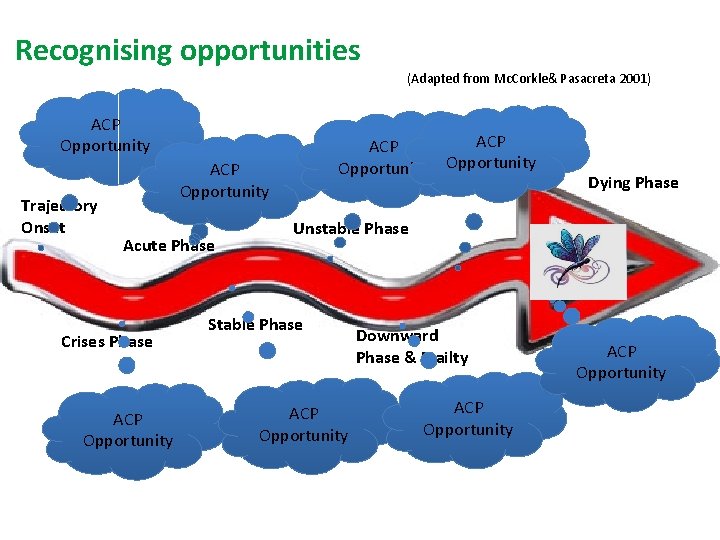
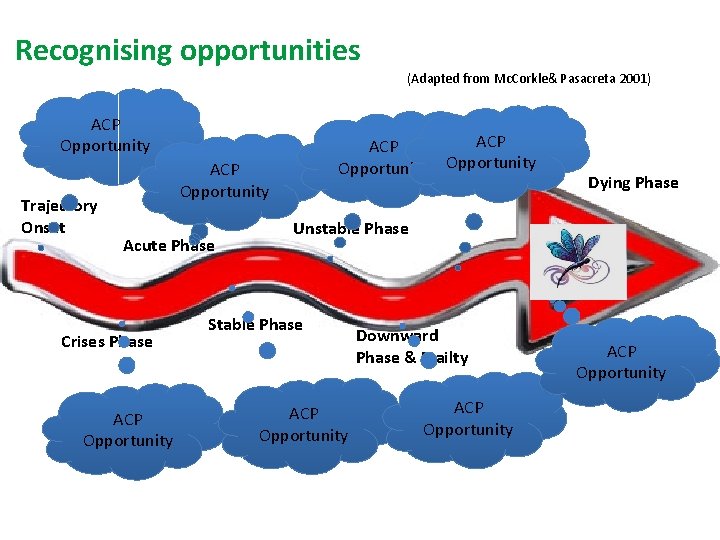
Recognising opportunities (Adapted from Mc. Corkle& Pasacreta 2001) ACP Opportunity Trajectory Onset ACP Opportunity Acute Phase Crises Phase ACP Opportunity Dying Phase Unstable Phase Stable Phase ACP Opportunity Downward Phase & Frailty ACP Opportunity
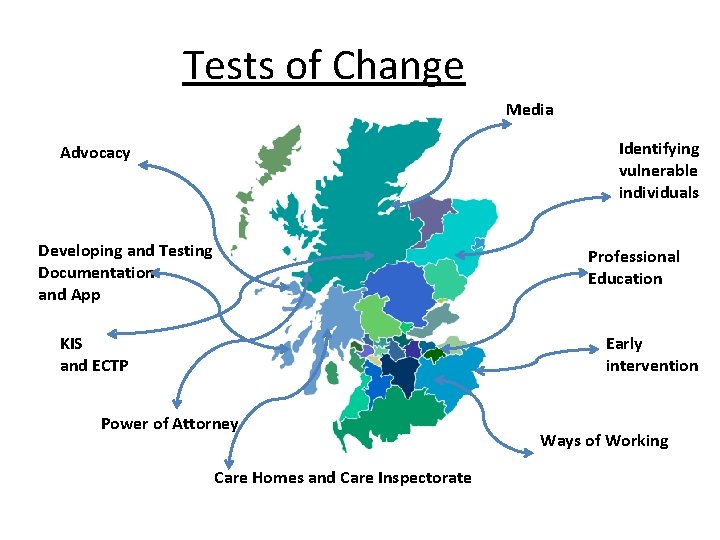
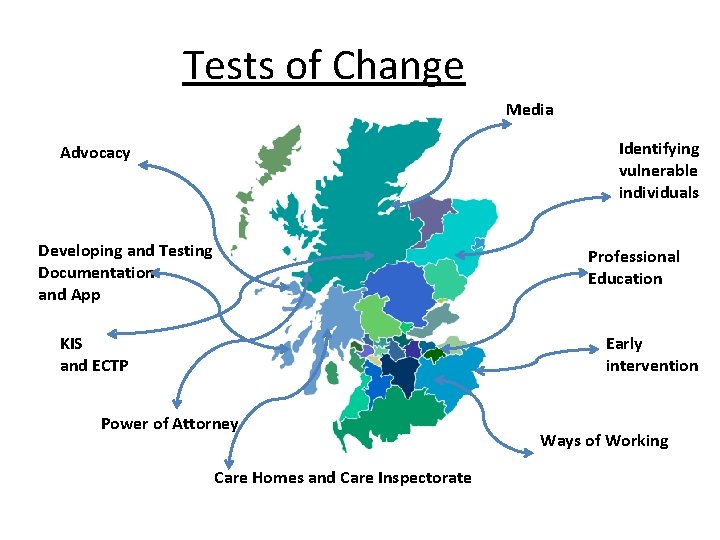
Tests of Change Media Identifying vulnerable individuals Advocacy Developing and Testing Documentation and App Professional Education KIS and ECTP Early intervention Power of Attorney Care Homes and Care Inspectorate Ways of Working
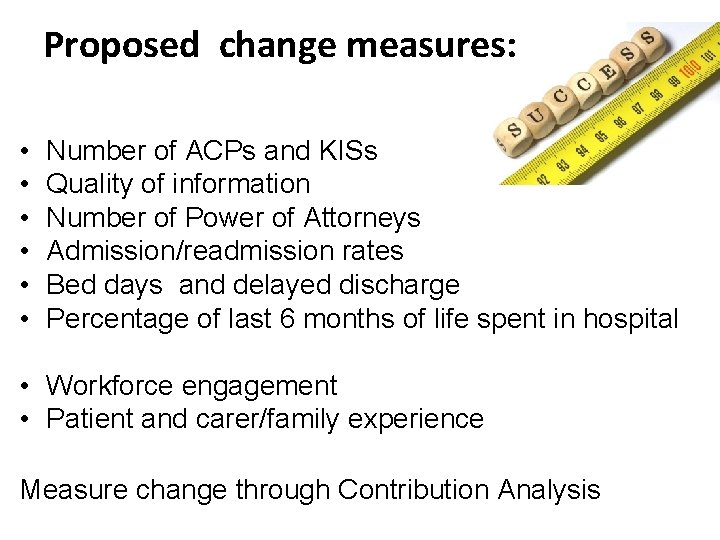
Proposed change measures: • • • Number of ACPs and KISs Quality of information Number of Power of Attorneys Admission/readmission rates Bed days and delayed discharge Percentage of last 6 months of life spent in hospital • Workforce engagement • Patient and carer/family experience Measure change through Contribution Analysis
Jack’s Story https: //www. youtube. com/watch? v=Cckvfdiw. Z 3 Q
Anticipatory Care Planning for babies, children and young people Fiona Reid (Diana Children’s Nurse (North) CHAS)
§ § § Lothian ACP for BCYP Antenatal ACP Holistic assessments - GIRFEC Statistics and audit (Lothian, MSN, Highland) Databases Case scenario demonstrating usage
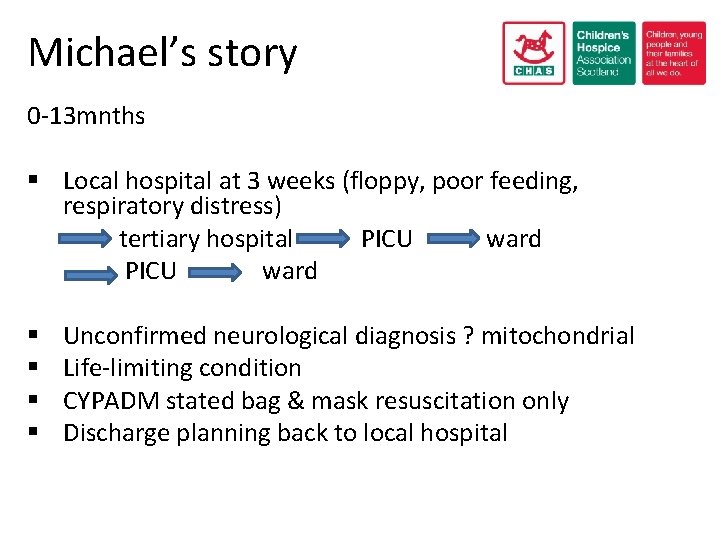
Michael’s story 0 -13 mnths § Local hospital at 3 weeks (floppy, poor feeding, respiratory distress) tertiary hospital PICU ward § § Unconfirmed neurological diagnosis ? mitochondrial Life-limiting condition CYPADM stated bag & mask resuscitation only Discharge planning back to local hospital
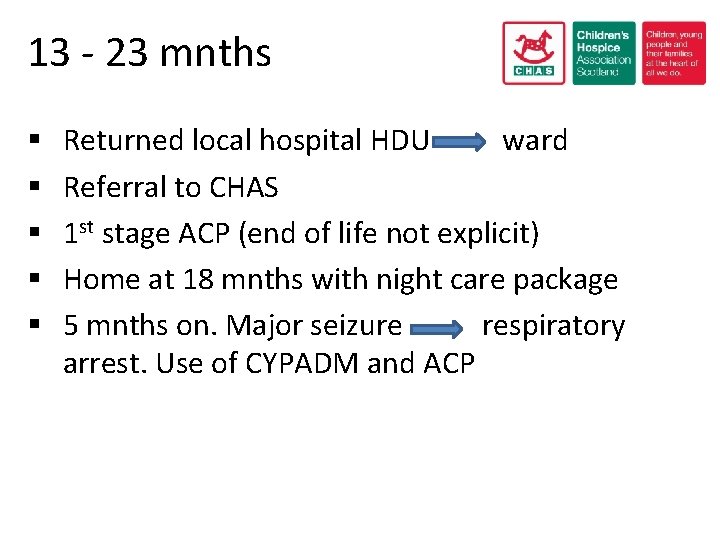
13 - 23 mnths § § § Returned local hospital HDU ward Referral to CHAS 1 st stage ACP (end of life not explicit) Home at 18 mnths with night care package 5 mnths on. Major seizure respiratory arrest. Use of CYPADM and ACP
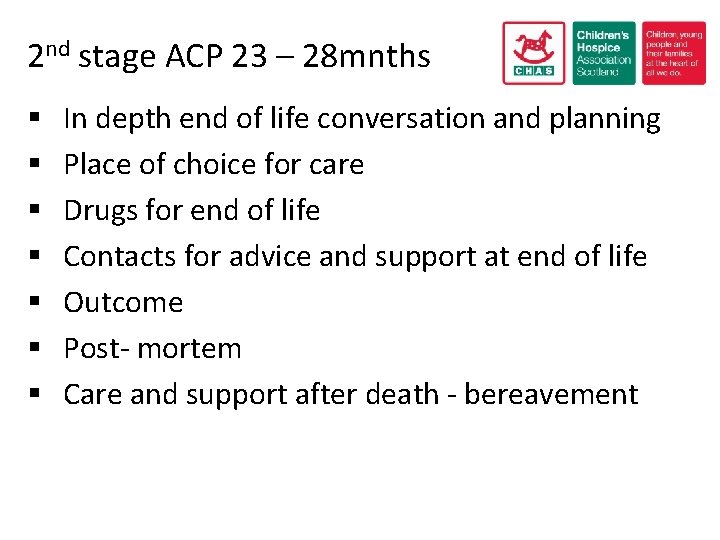
2 nd stage ACP 23 – 28 mnths § § § § In depth end of life conversation and planning Place of choice for care Drugs for end of life Contacts for advice and support at end of life Outcome Post- mortem Care and support after death - bereavement
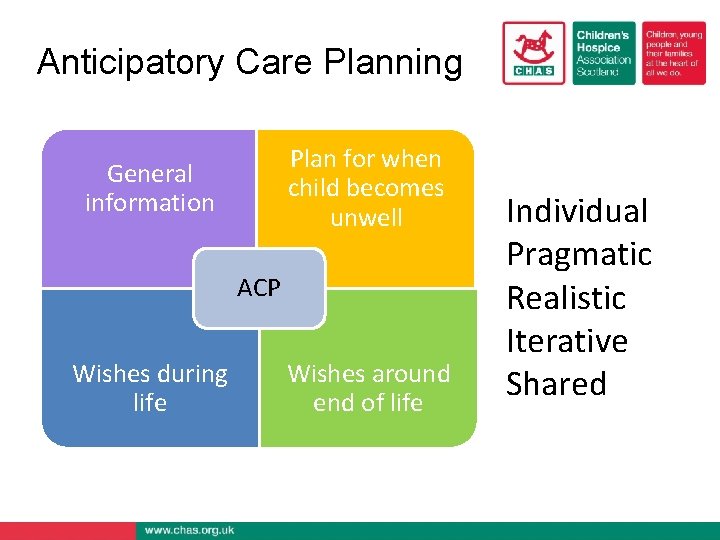
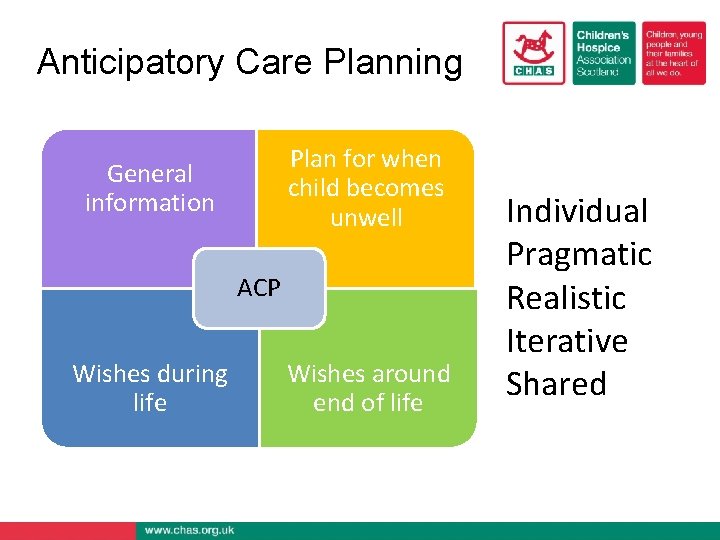
Anticipatory Care Planning Plan for when child becomes unwell General information ACP Wishes during life Wishes around end of life Individual Pragmatic Realistic Iterative Shared
Janette Barrie Janette. barrie 1@nhs. net Fiona Reid fionareid@chas. org. uk fiona. reid 7@nhs. net