A Coordinated Approach Towards a Provincial Stroke Competency


















- Slides: 42
A Coordinated Approach Towards a Provincial Stroke Competency Framework October 27 th 2014 Michelle Donald Rebecca Fleck On Behalf of the OREG Stroke Competency Task Team
Outline Background: §What is a Competency? Rationale: §Canadian Best Practice Recommendations for Stroke Care §Stroke Distinction – Accreditation Canada Theoretical Underpinnings: Context: §Local Initiatives: Central South & Toronto Provincial Initiative: §Ontario Regional Educators Group(OREG)
What is a Competency? “The capability to apply or use a set of related knowledge, skills, and abilities required to successfully perform "critical work functions" or tasks in a defined work setting. Competencies often serve as the basis for skill standards that specify the level of knowledge, skills, and abilities required for success in the workplace as well as potential measurement criteria for assessing competency attainment. ” Bloom, Benjamin S. and David R. Krathwohl. (1956). Taxonomy of educational objectives: The classification of educational goals, by a committee of college and university examiners. Handbook 1: Cognitive domain. New York, Longmans.

1 1. Benner, P. (1982). From novice to expert. American Journal of Nursing, 82(3), 402 -407

Rationale

The Canadian Best Practice Recommendations for Stroke Care: “The core interprofessional team on the stroke unit should consist of healthcare professionals with stroke expertise from medicine, nursing, occupational therapy, physiotherapy, speech-language pathology, social work, and clinical nutrition” [Evidence Level A] Casaubon LK, Suddes M, on behalf of the Acute Stroke Care Writing Group. (2013). Chapter 4: Acute Inpatient Stroke Care. In Lindsay MP, Gubitz G, Bayley M, and Phillips S (Editors) on behalf of the Canadian Stroke Best Practices and Standards Advisory Committee. Canadian Best Practice Recommendations for Stroke Care: Ottawa, Ontario Canada: Heart and Stroke Foundation of Canada, and the Canadian Stroke Network.

Evidence ØThere is Level A Evidence that Stroke Unit care reduces the likelihood of death and disability by as much as 30% for men and women of any age with mild, moderate, or severe stroke. ØOne of the key components of Stroke Unit Care is that the core interprofessional team should consist of healthcare professionals with stroke expertise. Casaubon et al. (2013)
Accreditation Canada Stroke Distinction Standards 2. 1 The team has expertise in stroke care and uses an interprofessional approach to deliver inpatient rehabilitation services to clients and families 2. 4 The team orients new staff and services providers about unique aspects of acute/rehabilitation stroke services. 2. 5 The team receives ongoing professional development and training to deliver current evidence based hyper-acute and acute stroke/stroke rehabilitation services. 2. 6 The team uses information from staff performance evaluations to improve acute/rehabilitation stroke services and to identify support, training or development needs for the team. 2. 7 The team has adopted and implemented the Canadian Best Practice Recommendations for stroke care for the assessment and management of stroke clients. Accreditation Canada. (2013). www. accreditation. ca
Reflection §Are you using stroke competencies for your own professional development or for your staff? §Do you feel confident in suggesting resources to accomplish stroke competencies? §Are you able to measure whether or not a competency has been achieved? §Do you work towards shared competencies as a team?

Opportunities §Consensus §Measurement §Interprofessional §Implementation

Theoretical Underpinnings
Competency Based Education §Has its roots in teacher training beginning in the 1960’s §Assessment of mastery of specific elements of professional practice §Organized around a knowledge base for that specific profession §Movement for health care professionals began in the 1970’s §PERFORMANCE OUTCOMES AS THE PRIORITY! Banbridge, L. & Orchard, C et al. (2012). Canadian Interprofessional Health Collaborative. Commission on Accreditation for Respiratory Care. (2012).
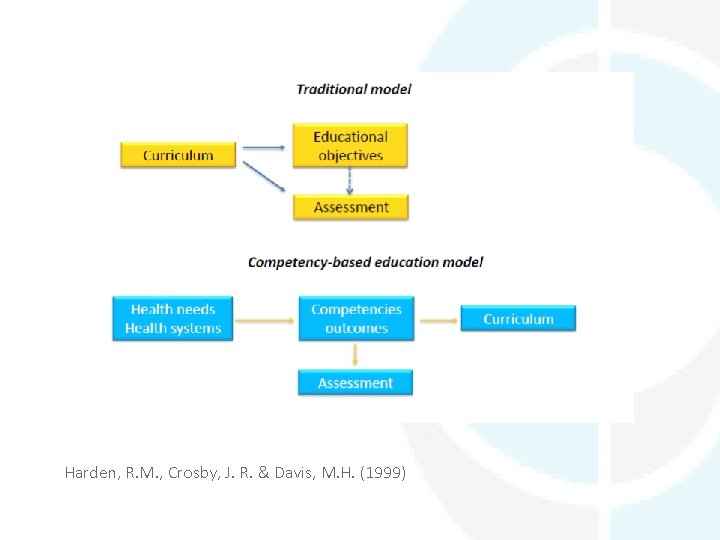
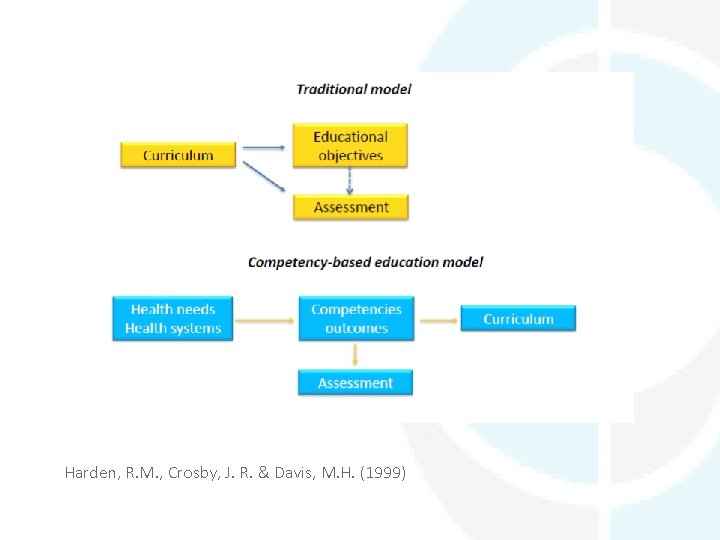
Harden, R. M. , Crosby, J. R. & Davis, M. H. (1999)
Interprofessional Education §Developing mutual understanding of, and respect for, the contributions of various disciplines. §Socializing health professionals to work together, share problem-solving and decision making, for the benefit of patients. §Learning together to promote collaboration. Health Canada. (www. hc-sc. gc. ca/hcs-sss/hhr-rhs/strateg/interprof)
Provincial Initiative: Ontario Regional Educators Group (OREG) Knowledge Translation : §Making users aware of knowledge and facilitating their use of it to improve health and health care systems §Closing the gap between what we know and what we do (moving knowledge to action) §Transforming evidence into practice (Graham et al. , 2006)

Knowledge to Action Process Monitor Knowledge Usee Evaluation Outcomes ge Knowledge Inquiry Syntheses Products/ Tools or Ta il Adapt Knowledge to Local Context ing Kn Assess Barriers to Knowledge Use Knowledge Creation ow led Select, Tailor, Implement Interventions Identify Problem/ Identify, Review Select Knowledge (Graham et. al (2006) Sustain Knowledge Use
Benefits to Moving Towards a Competency Approach §Relevance to individual practice §Improved accountability §Promotes self-directed learning §Acts as a guide for assessment and self-assessment §Encourages continuity of education (Harden at al. , 2014)
Context

Heart & Stroke Foundation/ Central South Regional Stroke Network/ Hamilton Health Sciences § In 2007, The Heart and Stroke Foundation of Ontario, the Central South Regional Stroke Network and Hamilton Health Sciences developed and piloted § Goal to develop and test a resource that outlines learning objectives shared by the regulated health disciplines as well as discipline-specific learning objectives, across 16 learning areas related to stroke care www. heartandstroke. ca/profed

16 Learning Areas for Stroke Care 1. Principles of Stroke Care 2. Anatomy and Physiology of Stroke 3. Cardiovascular Respiratory Effects 4. Psychosocial Effects 5. Communication 6. Independence in Mobility and Prevention of Complications 7. Routine Activities of Daily Living 8. Instrumental Activities of Daily Living
16 Learning Areas for Stroke Care 9. Cognitive, Perceptual and Behavioural Changes Post Stroke 10. Nutrition 11. Dysphagia 12. Skin Care 13. Sexuality 14. Continence Management 15. Primary/Secondary Stroke Prevention 16. Transition Management

Objectives §Give healthcare professionals working with stroke survivors a framework for learning. §Establish guidelines for knowledge and skill development related to stroke care for all eight regulated health professionals. §Form the foundation for learning plans for ongoing individual professional development.

Objectives, cont… §Support self-directed learning. §Support interprofessional education and collaborative practice through shared learning opportunities. §Support knowledge translation and the integration of best available evidence into practice.
A Local Initiative at Hamilton Health Sciences Central South Regional Stroke Network
HHS Initiative In preparation for Stroke Distinction in 2012, we realized that the HHS integrated stroke model staff orientation and ongoing stroke competency process was not meeting the Canadian Best Practice Recommendations for Stroke Care or Accreditation Canada – Stroke Distinction Standards related to stroke unit care - staff education and stroke expertise.
HHS Stroke Orientation and Staff Competency Process ØHHS conducted a LEAN process to standardize, develop, support, monitor and evaluate the level of stroke expertise of the interprofessional staff working within the HHS Integrated Stroke Model ØIdentified the need to address both Stroke Competencies and Expertise - based on the Interdisciplinary Learning Objectives for Stroke Care (ILO’s)


A Local Initiative in Toronto

GTA Nursing Leadership Committee §Mission: to promote best practice, knowledge translation, education and research across the continuum of stroke care using collaboration and partnership §Membership: nurse leaders from the Toronto Stroke Networks, their partner sites, and neighbouring networks, including community stakeholders and stroke rehabilitation centers. Regional Stroke Network representatives on ad hoc basis §Committee represents 17 organizations
GTA Nursing Leadership Committee §Identified stroke nursing competencies as a potential committee project §Reviewed existing resources – identified a need for consistency across disciplines and a need to work towards shared competencies §Committee is currently developing the nursing competencies for our provincial framework
Provincial Initiative: Ontario Regional Educators Group (OREG)

Provincial Initiative: Ontario Regional Educators Group (OREG) Statement of Purpose §A forum for the Ontario Stroke System’s Regional Education Coordinators to establish educational priorities and for the development, implementation and evaluation of provincial/regional professional education plans. §This forum also promotes opportunities to maximize efficiencies in the development, implementation and evaluation of professional education resources.
Knowledge Brokers OREG has identified itself to be a provincial knowledge broker: §Contributing to the achievement of cross continuum stroke best practices §Building capacity to improve stroke outcomes
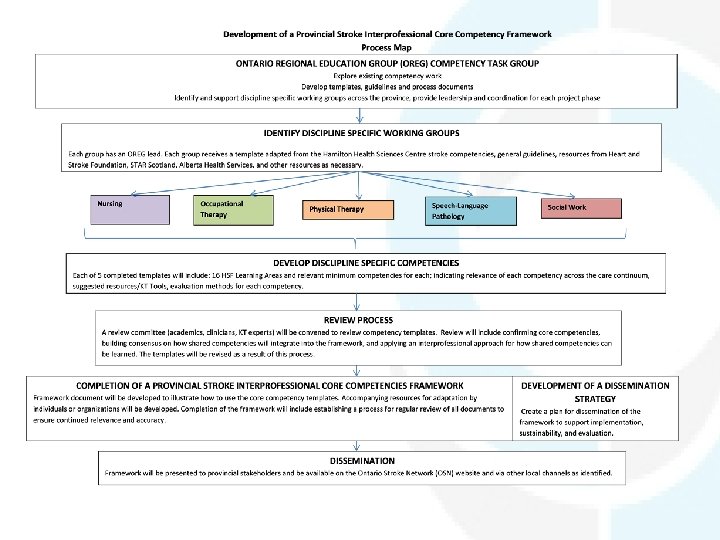
OREG Core Competency Task Group was convened to: §Build upon the work of HSF, Central South & Toronto §Maximize collaboration and input across the province §Confirm relevance of core competencies across the care continuum §Identify resources for achievement of competencies §Develop a more robust evaluation component to the competencies

Environmental Scan Heart and Stroke Interprofessional Learning Objectives for Stroke Care Hamilton Health Sciences Centre Orientation and Stroke Competencies Process Alberta Stroke Competency Framework Stroke Training and Awareness Resources (STAR) Comprehensive learning areas Basic and expert competencies Identified shared learning areas Working template Comprehensive framework available on-line On-line program with interactive resources linked to relevant competencies Care Continuum Current Process to differentiation learn from
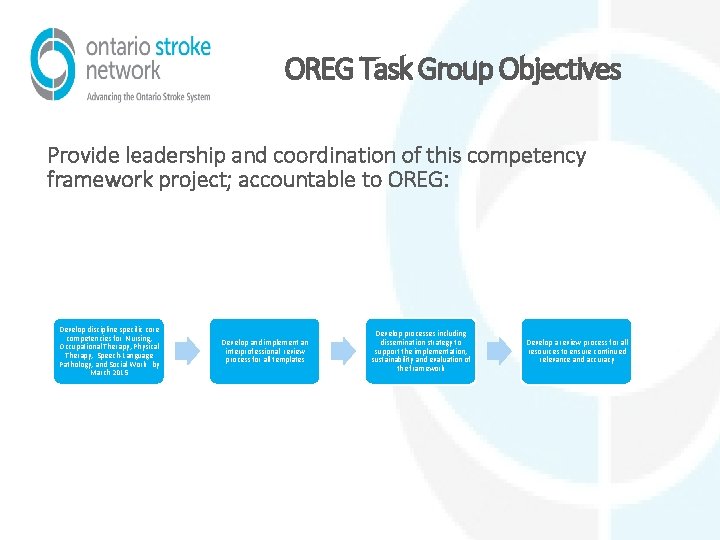
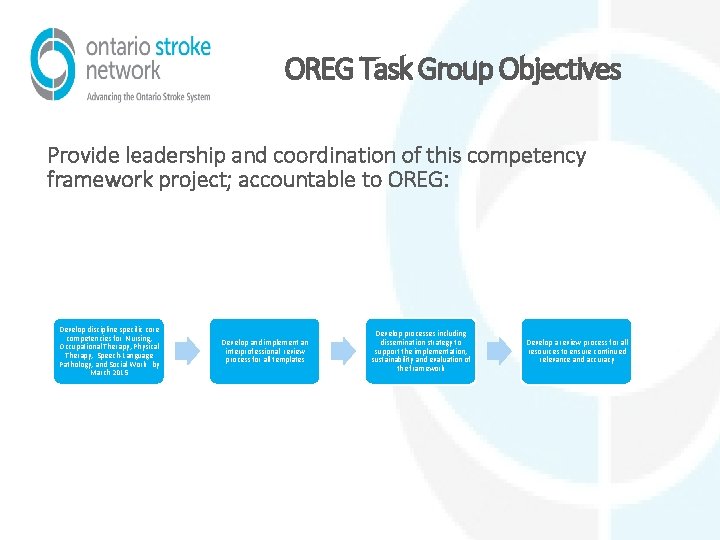
OREG Task Group Objectives Provide leadership and coordination of this competency framework project; accountable to OREG: Develop discipline specific core competencies for Nursing, Occupational Therapy, Physical Therapy, Speech-Language Pathology, and Social Work by March 2015 Develop and implement an interprofessional review process for all templates Develop processes including dissemination strategy to support the implementation, sustainability and evaluation of the framework Develop a review process for all resources to ensure continued relevance and accuracy
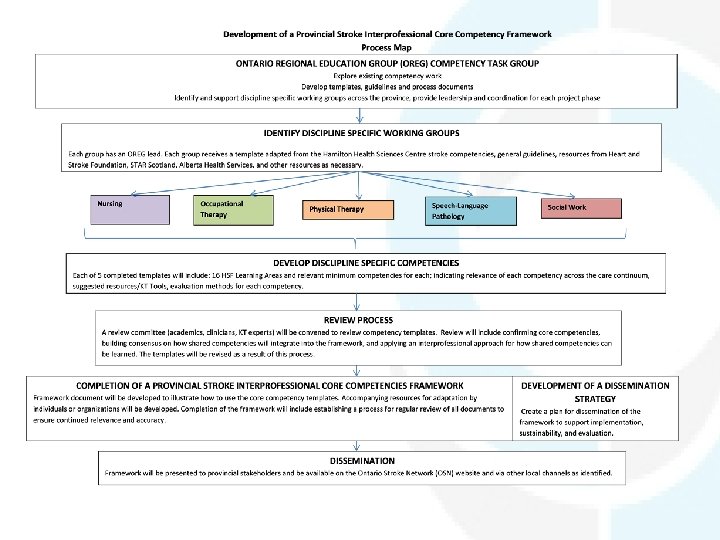
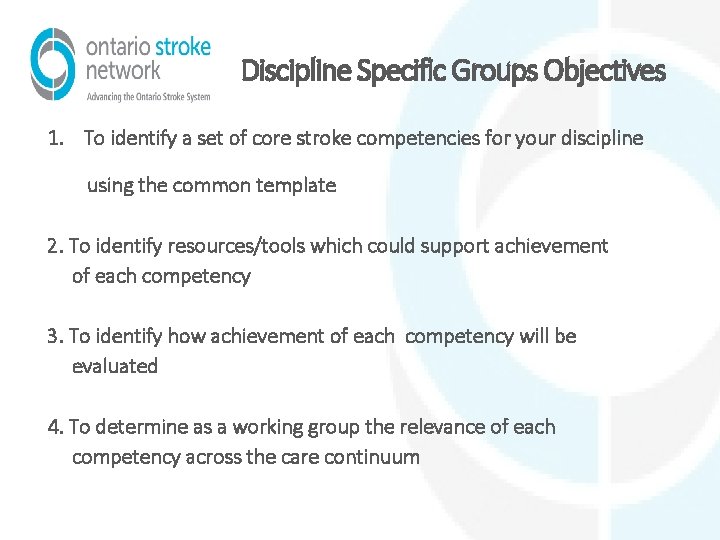
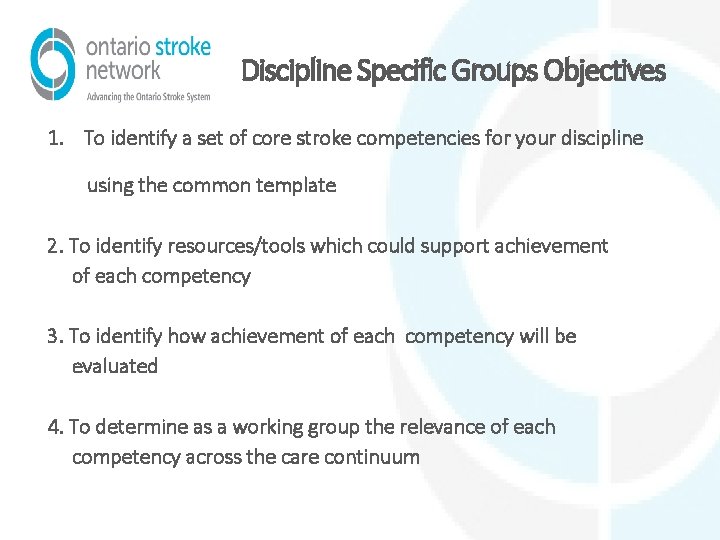
Discipline Specific Groups Objectives 1. To identify a set of core stroke competencies for your discipline using the common template 2. To identify resources/tools which could support achievement of each competency 3. To identify how achievement of each competency will be evaluated 4. To determine as a working group the relevance of each competency across the care continuum

LEARNING AREA *SELF-RATING Care Continuum Relevance Suggested Evaluation Completion Resources/Knowledge Date Translation Tools (How will Start 6 Date months achievement be 12 months (completion) measured) INDEPENDENCE IN MOBILITY AND PREVENTION OF COMPLICATIONS OF IMMOBILITY I demonstrate awareness of proper handling of patients with hemiplegia to prevent complications and optimize mobility and function Acute/Hyperacute In-Patient Out-Patient Secondary Prevention Clinic Community

Next Steps §Completion of discipline specific templates §Review process to confirm core competencies and apply and IPE approach to shared competencies §Dissemination of the framework with supporting materials
Questions ?