EMS Seminar 1 Introduction Training Medical Oversight Joseph








- Slides: 49

EMS Seminar #1 – Introduction, Training, Medical Oversight Joseph Ip BSc (Hon), MSc, MD, FRCPC Attending Emergency Physician, Royal Columbian Hospital, Vancouver, BC Local Medical Consultant, Standard of Care Committee, Region 2 W, British Columbia Ambulance Services
PART I - Introduction l History of BCAS l Health Emergency Act l Organization of BCAS l Regionalization of BCAS l Review of 2001 call volumes
History of BCAS l Prior to 1974, multiple providers – Private companies – Municipal – Volunteer l 1974, Foulkes Royal Commission Report: – recommended “… that the fractionated ambulance services provided by private companies, volunteer agencies and municipal fire departments be amalgamated under one jurisdiction”. – BCAS took over private and volunteer operators while 40 municipal fire department were permitted to continue providing pre-hospital emergency medical services under agreements with BCAS
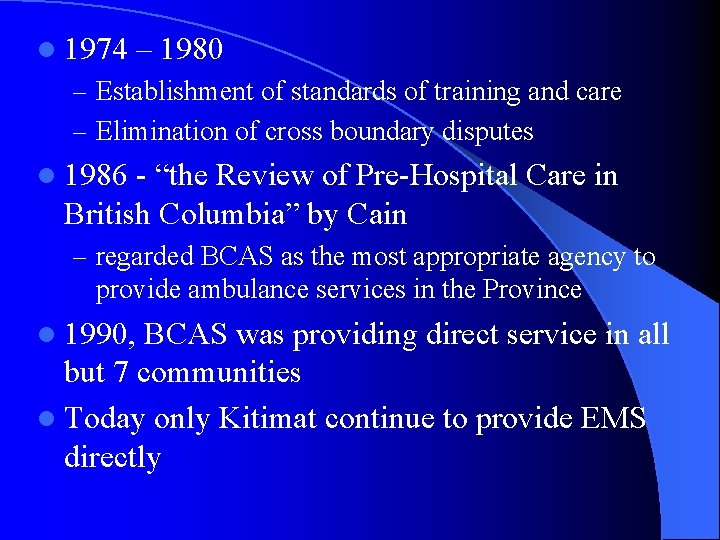
l 1974 – 1980 – Establishment of standards of training and care – Elimination of cross boundary disputes l 1986 - “the Review of Pre-Hospital Care in British Columbia” by Cain – regarded BCAS as the most appropriate agency to provide ambulance services in the Province l 1990, BCAS was providing direct service in all but 7 communities l Today only Kitimat continue to provide EMS directly
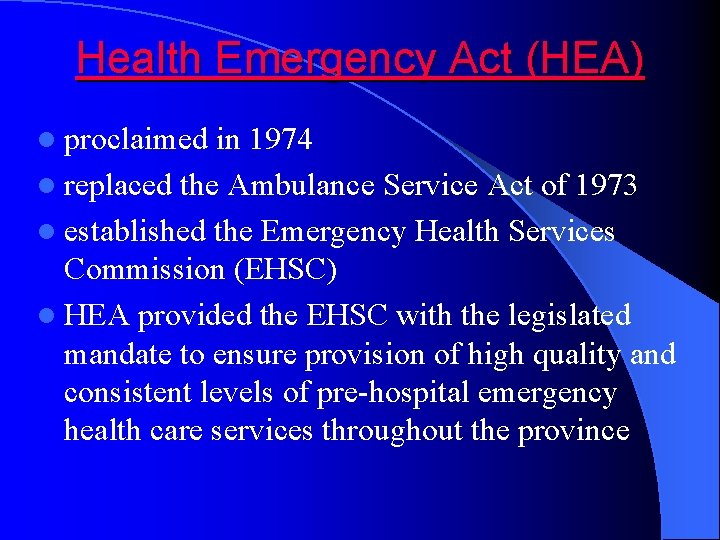
Health Emergency Act (HEA) l proclaimed in 1974 l replaced the Ambulance Service Act of 1973 l established the Emergency Health Services Commission (EHSC) l HEA provided the EHSC with the legislated mandate to ensure provision of high quality and consistent levels of pre-hospital emergency health care services throughout the province
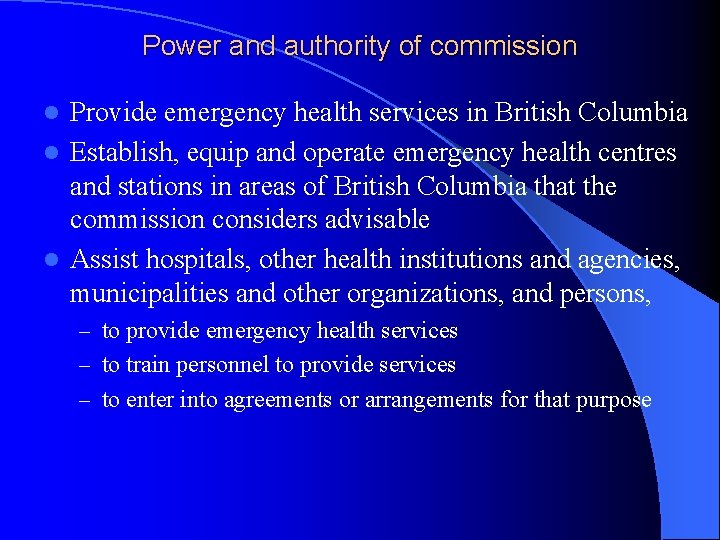
Power and authority of commission Provide emergency health services in British Columbia l Establish, equip and operate emergency health centres and stations in areas of British Columbia that the commission considers advisable l Assist hospitals, other health institutions and agencies, municipalities and other organizations, and persons, l – to provide emergency health services – to train personnel to provide services – to enter into agreements or arrangements for that purpose
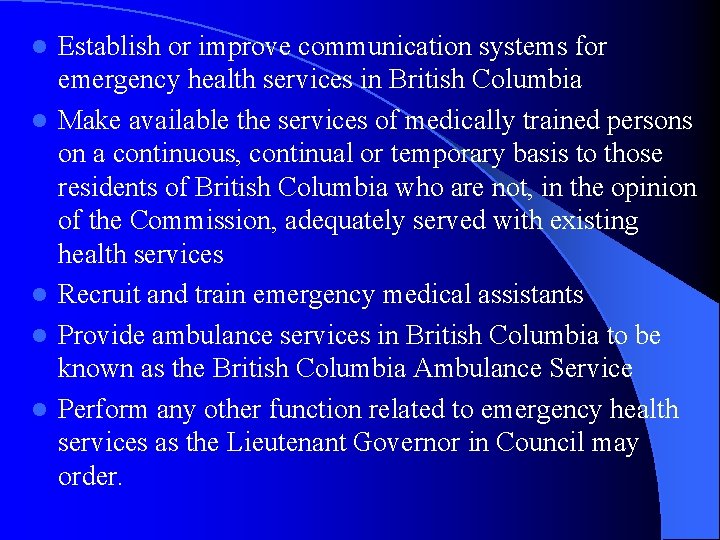
l l l Establish or improve communication systems for emergency health services in British Columbia Make available the services of medically trained persons on a continuous, continual or temporary basis to those residents of British Columbia who are not, in the opinion of the Commission, adequately served with existing health services Recruit and train emergency medical assistants Provide ambulance services in British Columbia to be known as the British Columbia Ambulance Service Perform any other function related to emergency health services as the Lieutenant Governor in Council may order.
Practise of medicine by emergency medical assistant l Nothing in this Act authorizes a person to practise medicine without being registered under the Medical Practitioners Act; but if the unavailability of a medical practitioner is likely to result in a person's death or deterioration of health, an available emergency medical assistant may perform emergency procedures that he or she has been trained for and considers necessary to preserve the person's life or health until the services of a medical practitioner are available.
Licence required l A person must not assume or use the title "emergency medical assistant" or otherwise represent himself or herself to be an emergency medical assistant unless the person is the holder of a valid and subsisting licence under this Act.
Emergency Medical Assistants Licensing Board (1) The Emergency Medical Assistants Licensing Board is continued. l (2) The board is composed of 3 members, one of whom must be an emergency medical assistant selected in the prescribed manner and another of whom must be a medical practitioner, appointed by the Lieutenant Governor in Council. l (3) The Lieutenant Governor in Council may l – (a) establish the remuneration and other terms and conditions of appointments under subsection (2), and – (b) designate a member of the board as its chair.
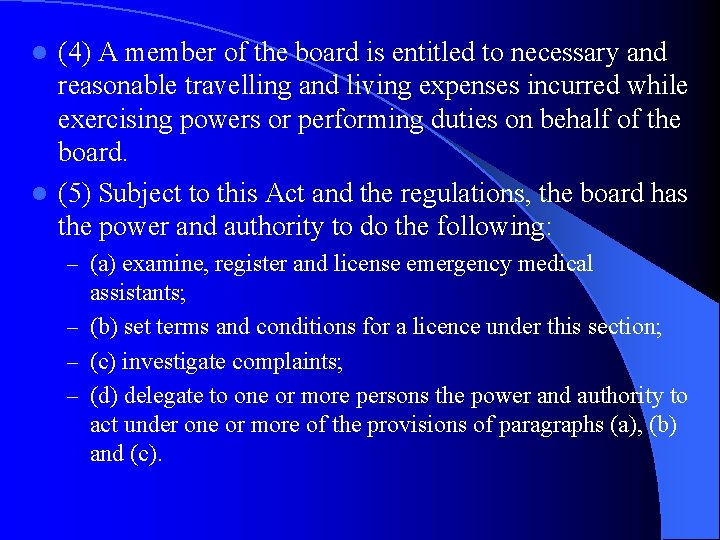
(4) A member of the board is entitled to necessary and reasonable travelling and living expenses incurred while exercising powers or performing duties on behalf of the board. l (5) Subject to this Act and the regulations, the board has the power and authority to do the following: l – (a) examine, register and license emergency medical assistants; – (b) set terms and conditions for a licence under this section; – (c) investigate complaints; – (d) delegate to one or more persons the power and authority to act under one or more of the provisions of paragraphs (a), (b) and (c).

HEA – EMA regulation
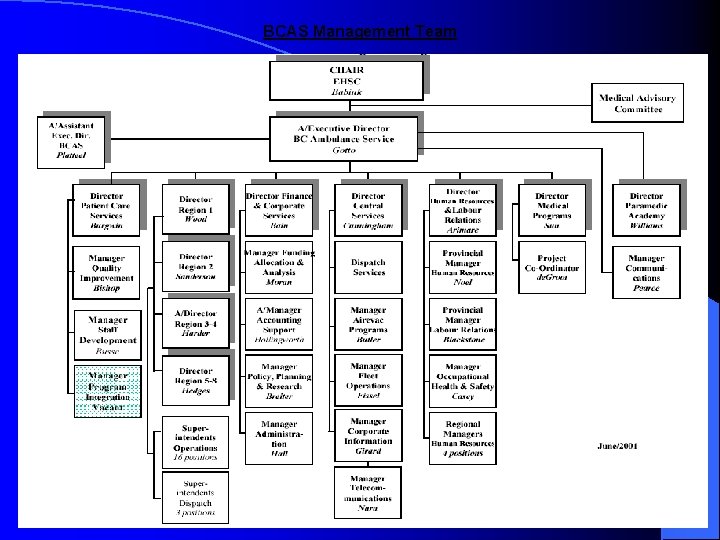
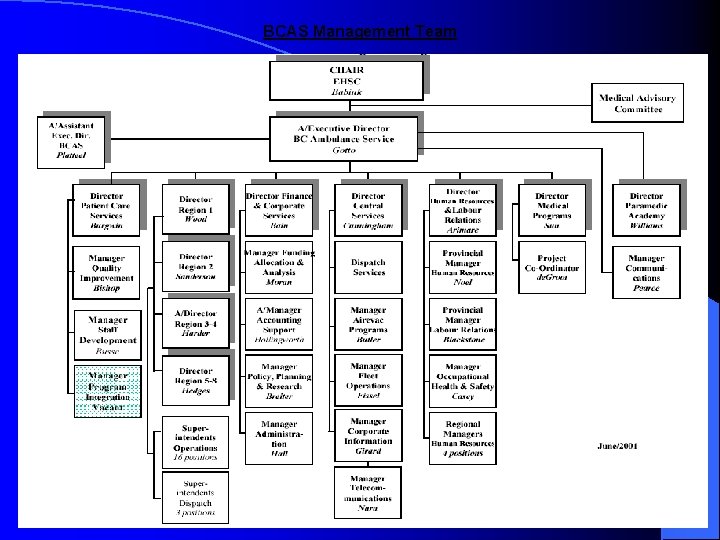
BCAS Management Team
BCAS functions l Pre-hospital emergency care - 911 calls l Inter-facility transports l Stand-by at public events (450 standby locations in 2000 -2001; 50% film industry) l Disaster Readiness
Regionalization of BCAS l 198 ambulance stations in 163 communities across the province l ground ambulances dispatch centres are located in Victoria, Vancouver and Kamloops l air ambulance services dispatch centre in Victoria

Employee composition: l 3300 paramedics – 2100 part time – 1200 full time l Average of paramedic is 48 yo l By 2005, 161 full time staff will be eligible for retirement – 37/161 are ALS attendants
Air Ambulance Program l l l budget is $22. 5 million Approximately $16 million for aircraft charters, fuel and associated costs. remainder for wages and benefits, training, equipment and contracts with physician advisors. 60 flight paramedics positions based in Victoria, Vancouver, Kelowna and Prince George. 4 Management positions
2000 -2001 Ground Ambulance Statistics
Call Volume breakdown by stations
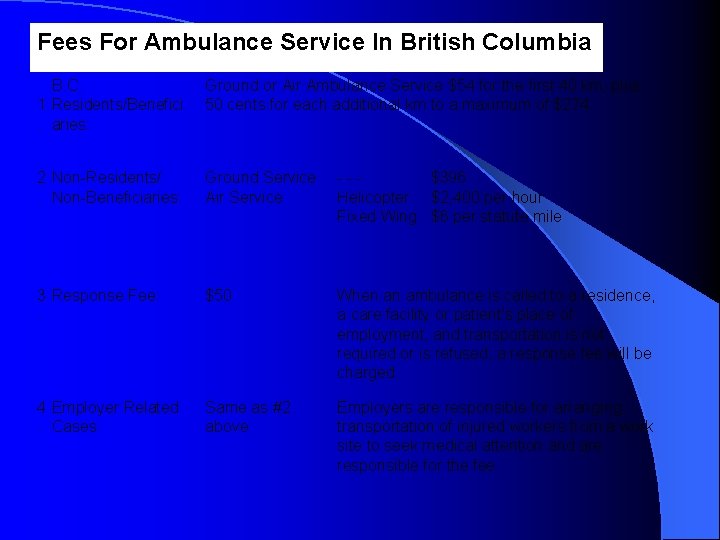
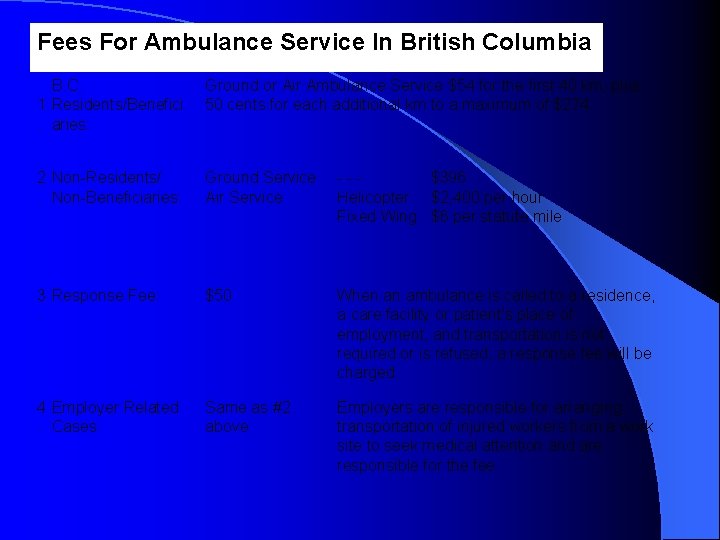
Fees For Ambulance Service In British Columbia (Effective April 1, 1998 - Subject to Change) B. C. 1 Residents/Benefici. aries: Ground or Air Ambulance Service $54 for the first 40 km, plus 50 cents for each additional km to a maximum of $274. 2 Non-Residents/. Non-Beneficiaries: Ground Service Air Service - - $396 Helicopter $2, 400 per hour Fixed Wing $6 per statute mile 3 Response Fee: . $50 When an ambulance is called to a residence, a care facility or patient's place of employment, and transportation is not required or is refused, a response fee will be charged. 4 Employer Related . Cases: Same as #2 above Employers are responsible for arranging transportation of injured workers from a work site to seek medical attention and are responsible for the fee.
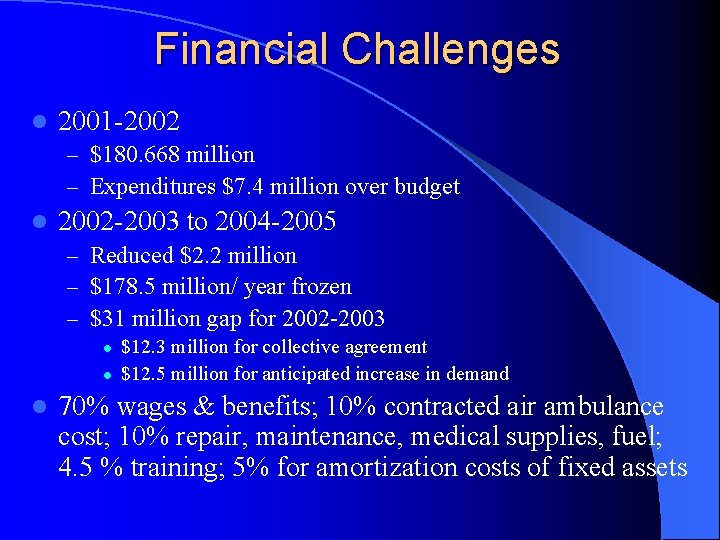
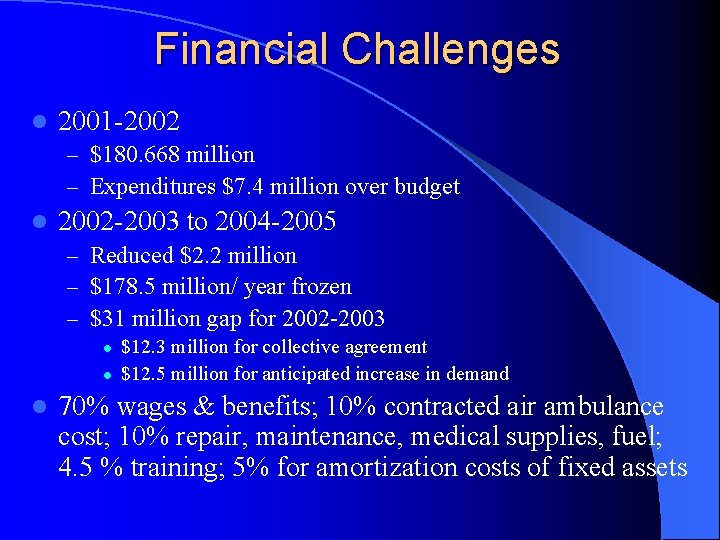
Financial Challenges l 2001 -2002 – $180. 668 million – Expenditures $7. 4 million over budget l 2002 -2003 to 2004 -2005 – Reduced $2. 2 million – $178. 5 million/ year frozen – $31 million gap for 2002 -2003 l l l $12. 3 million for collective agreement $12. 5 million for anticipated increase in demand 70% wages & benefits; 10% contracted air ambulance cost; 10% repair, maintenance, medical supplies, fuel; 4. 5 % training; 5% for amortization costs of fixed assets
PART II - Training l P 1 training curriculum & protocols l EMA III/ ALS training curriculum & protocols l CME program
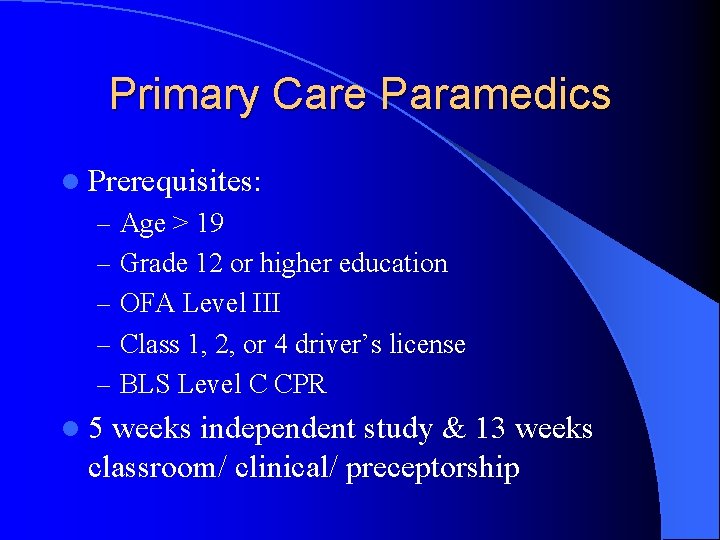
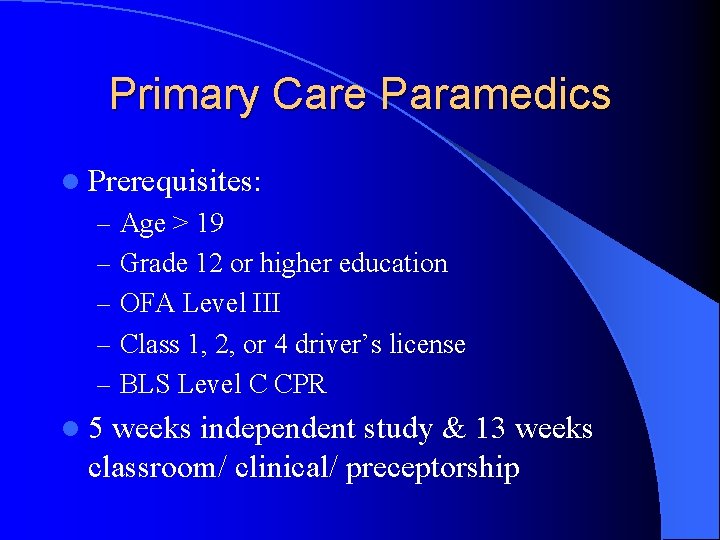
Primary Care Paramedics l Prerequisites: – Age > 19 – Grade 12 or higher education – OFA Level III – Class 1, 2, or 4 driver’s license – BLS Level C CPR l 5 weeks independent study & 13 weeks classroom/ clinical/ preceptorship
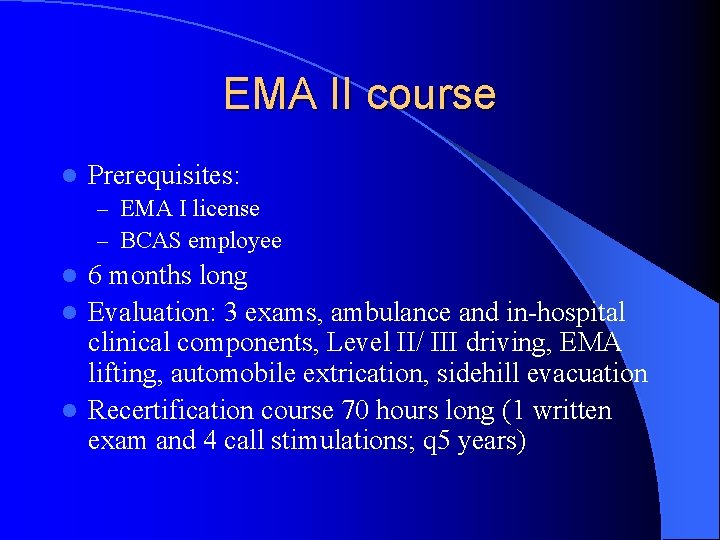
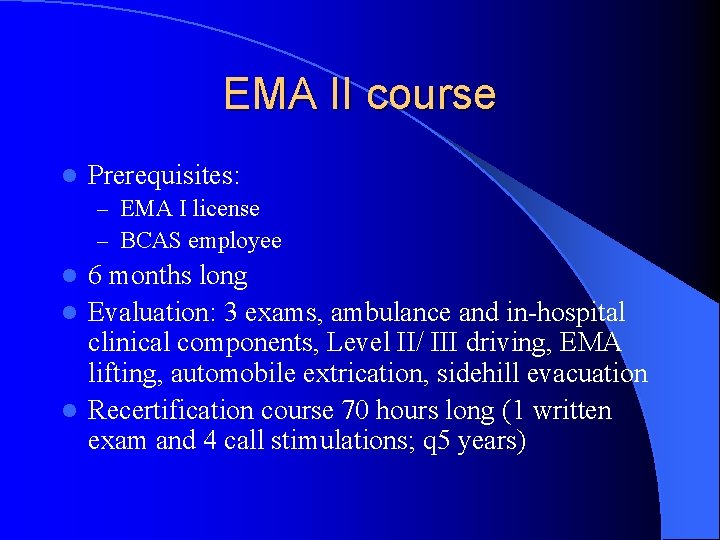
EMA II course l Prerequisites: – EMA I license – BCAS employee 6 months long l Evaluation: 3 exams, ambulance and in-hospital clinical components, Level II/ III driving, EMA lifting, automobile extrication, sidehill evacuation l Recertification course 70 hours long (1 written exam and 4 call stimulations; q 5 years) l
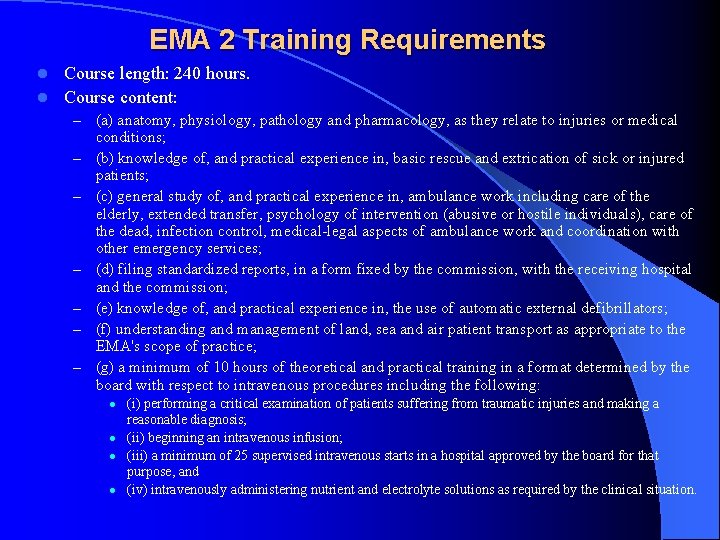
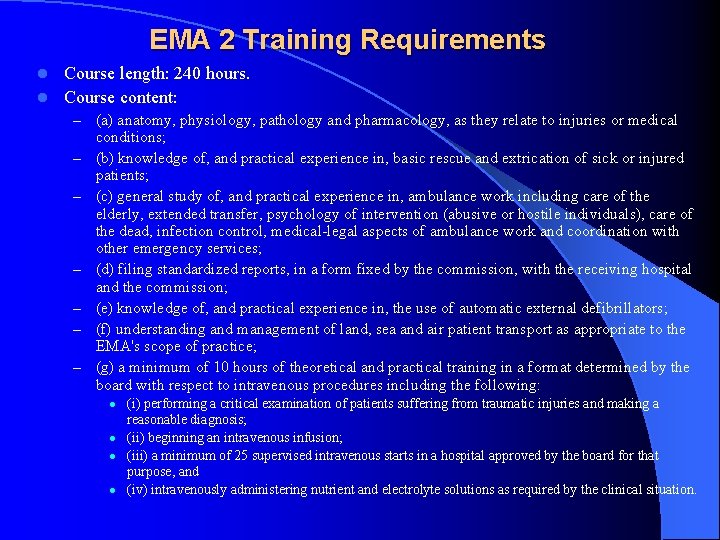
EMA 2 Training Requirements Course length: 240 hours. l Course content: l – – – – (a) anatomy, physiology, pathology and pharmacology, as they relate to injuries or medical conditions; (b) knowledge of, and practical experience in, basic rescue and extrication of sick or injured patients; (c) general study of, and practical experience in, ambulance work including care of the elderly, extended transfer, psychology of intervention (abusive or hostile individuals), care of the dead, infection control, medical-legal aspects of ambulance work and coordination with other emergency services; (d) filing standardized reports, in a form fixed by the commission, with the receiving hospital and the commission; (e) knowledge of, and practical experience in, the use of automatic external defibrillators; (f) understanding and management of land, sea and air patient transport as appropriate to the EMA's scope of practice; (g) a minimum of 10 hours of theoretical and practical training in a format determined by the board with respect to intravenous procedures including the following: l l (i) performing a critical examination of patients suffering from traumatic injuries and making a reasonable diagnosis; (ii) beginning an intravenous infusion; (iii) a minimum of 25 supervised intravenous starts in a hospital approved by the board for that purpose, and (iv) intravenously administering nutrient and electrolyte solutions as required by the clinical situation.
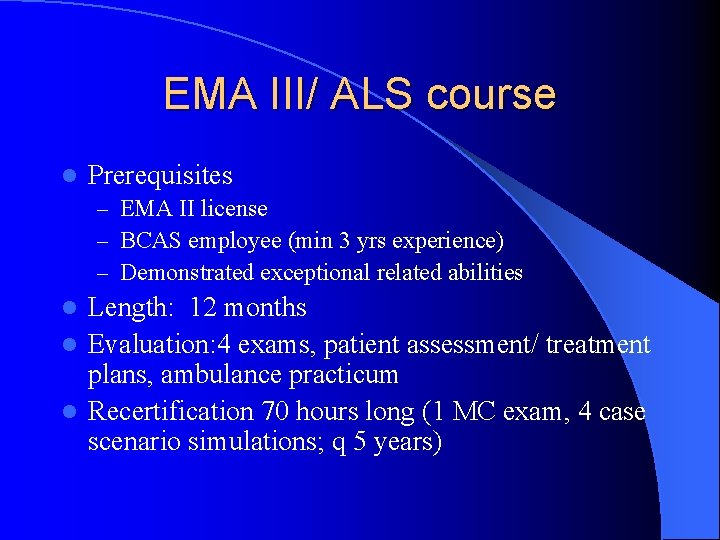
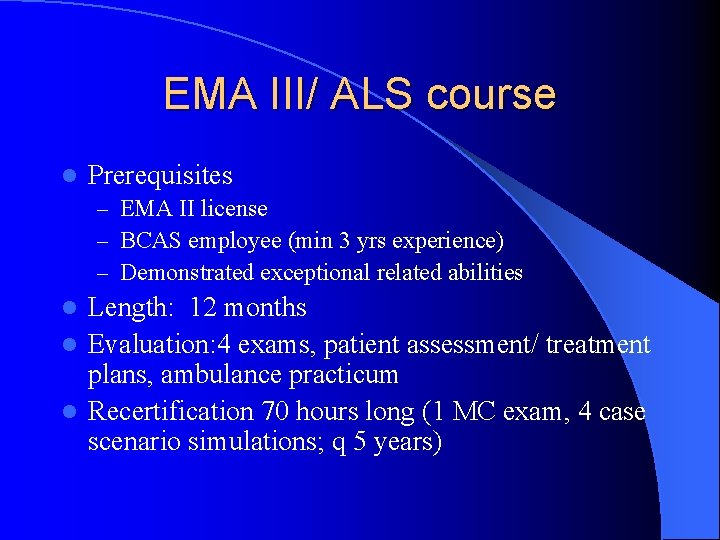
EMA III/ ALS course l Prerequisites – EMA II license – BCAS employee (min 3 yrs experience) – Demonstrated exceptional related abilities Length: 12 months l Evaluation: 4 exams, patient assessment/ treatment plans, ambulance practicum l Recertification 70 hours long (1 MC exam, 4 case scenario simulations; q 5 years) l
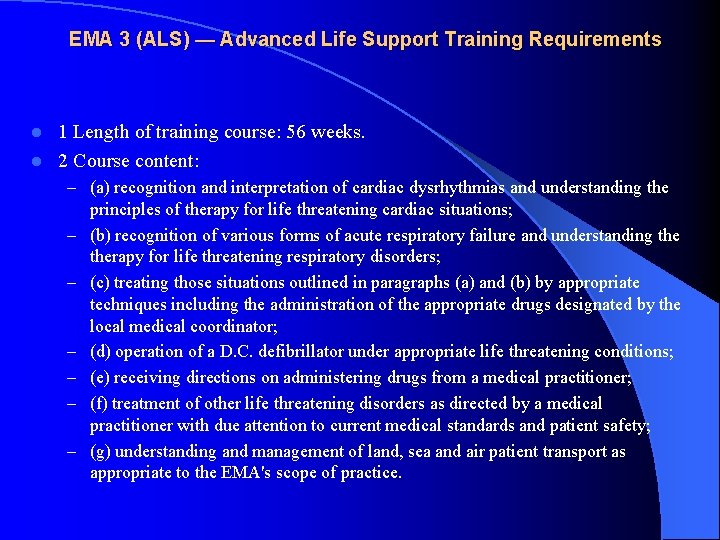
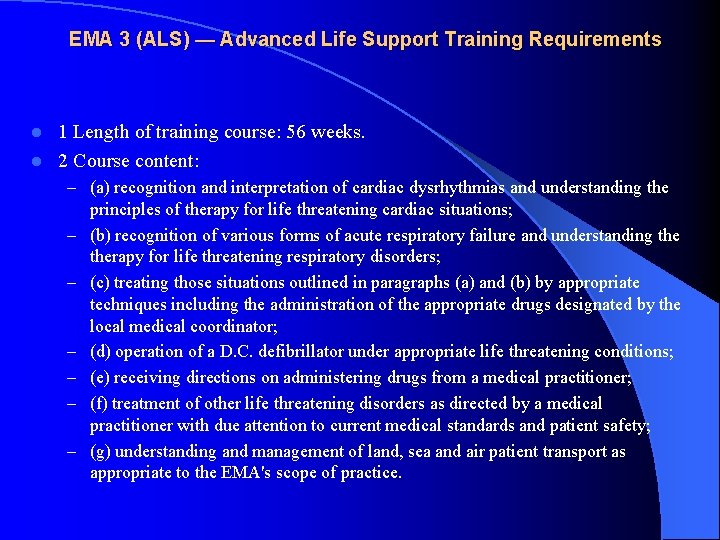
EMA 3 (ALS) — Advanced Life Support Training Requirements 1 Length of training course: 56 weeks. l 2 Course content: l – (a) recognition and interpretation of cardiac dysrhythmias and understanding the – – – principles of therapy for life threatening cardiac situations; (b) recognition of various forms of acute respiratory failure and understanding therapy for life threatening respiratory disorders; (c) treating those situations outlined in paragraphs (a) and (b) by appropriate techniques including the administration of the appropriate drugs designated by the local medical coordinator; (d) operation of a D. C. defibrillator under appropriate life threatening conditions; (e) receiving directions on administering drugs from a medical practitioner; (f) treatment of other life threatening disorders as directed by a medical practitioner with due attention to current medical standards and patient safety; (g) understanding and management of land, sea and air patient transport as appropriate to the EMA's scope of practice.

ITT course l Prerequisites: – EMA II license – BCAS employee l Length: 18 months l Evaluation: BCLS CPR, PALS, NRP, 4 exams, ambulance internship l License valid for 5 years
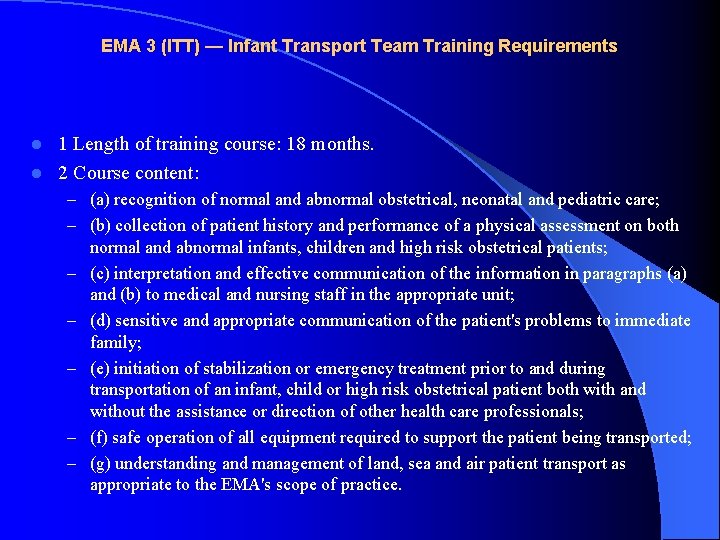
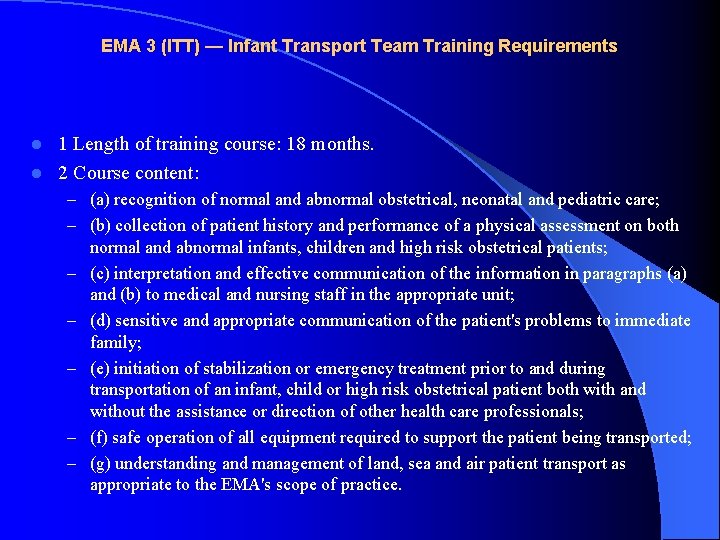
EMA 3 (ITT) — Infant Transport Team Training Requirements 1 Length of training course: 18 months. l 2 Course content: l – (a) recognition of normal and abnormal obstetrical, neonatal and pediatric care; – (b) collection of patient history and performance of a physical assessment on both – – – normal and abnormal infants, children and high risk obstetrical patients; (c) interpretation and effective communication of the information in paragraphs (a) and (b) to medical and nursing staff in the appropriate unit; (d) sensitive and appropriate communication of the patient's problems to immediate family; (e) initiation of stabilization or emergency treatment prior to and during transportation of an infant, child or high risk obstetrical patient both with and without the assistance or direction of other health care professionals; (f) safe operation of all equipment required to support the patient being transported; (g) understanding and management of land, sea and air patient transport as appropriate to the EMA's scope of practice.
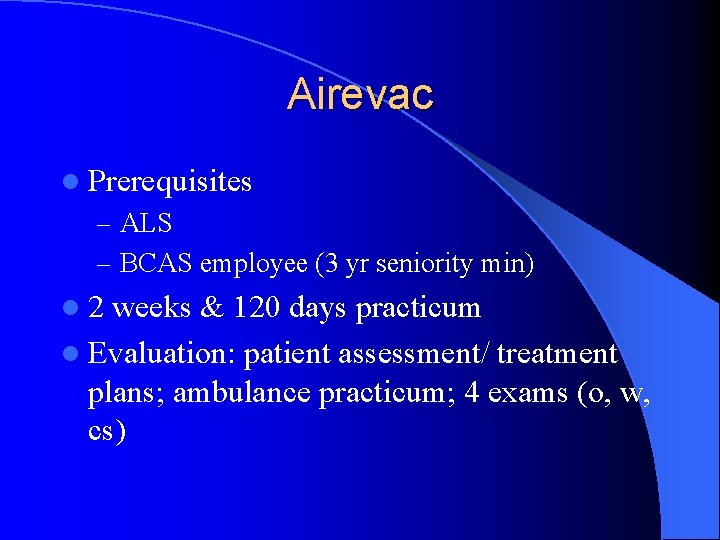
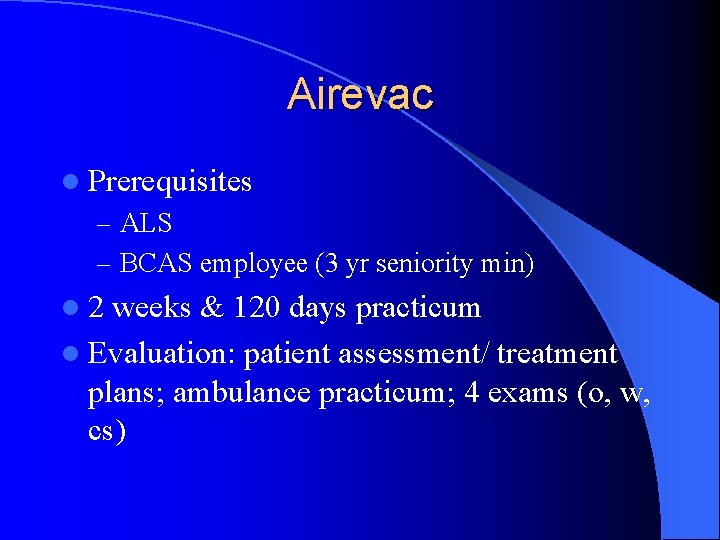
Airevac l Prerequisites – ALS – BCAS employee (3 yr seniority min) l 2 weeks & 120 days practicum l Evaluation: patient assessment/ treatment plans; ambulance practicum; 4 exams (o, w, cs)
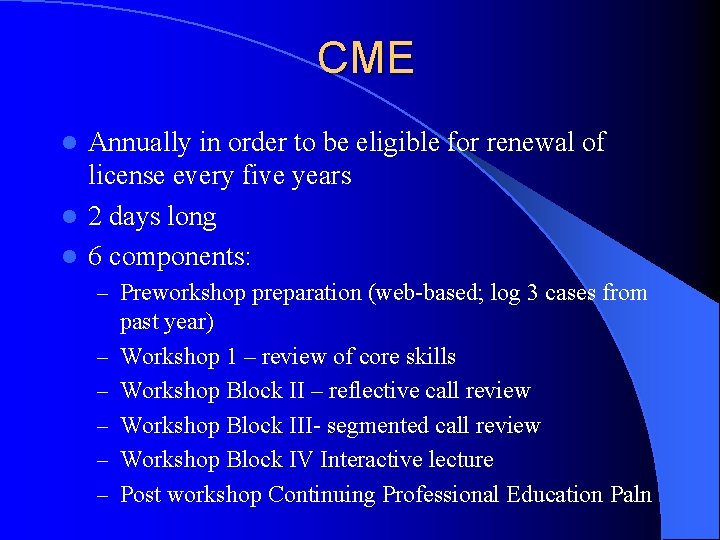
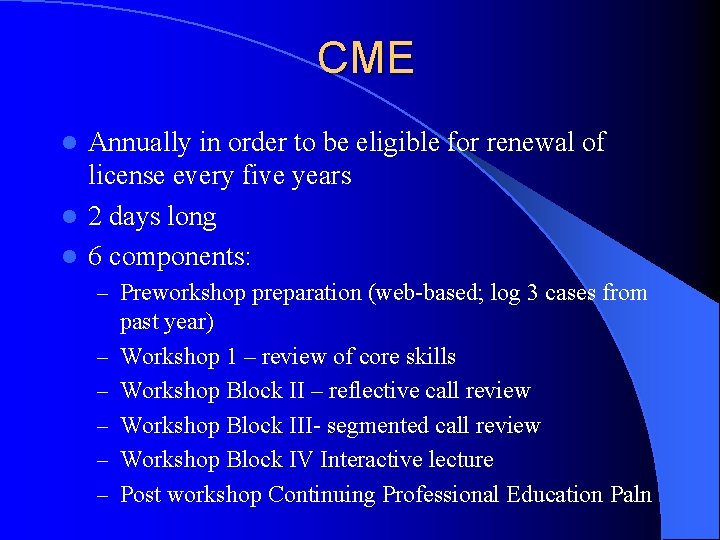
CME Annually in order to be eligible for renewal of license every five years l 2 days long l 6 components: l – Preworkshop preparation (web-based; log 3 cases from – – – past year) Workshop 1 – review of core skills Workshop Block II – reflective call review Workshop Block III- segmented call review Workshop Block IV Interactive lecture Post workshop Continuing Professional Education Paln
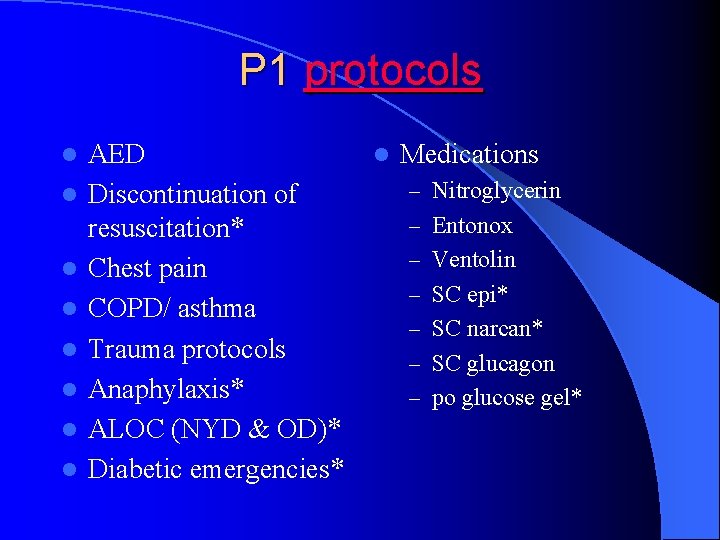
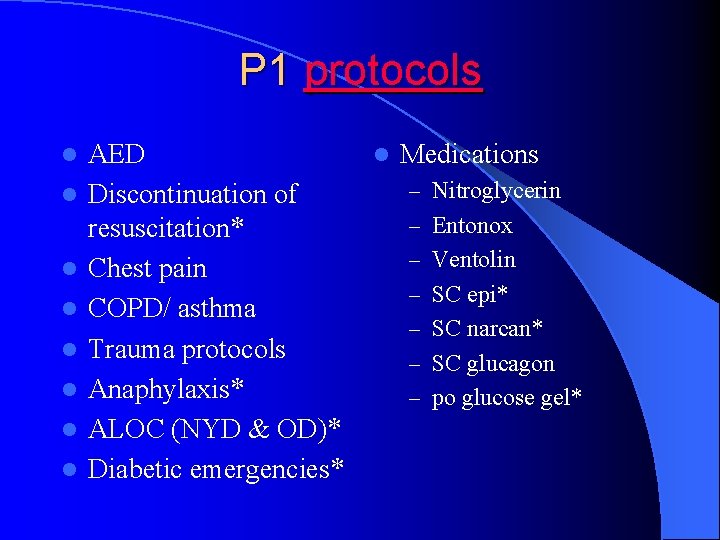
P 1 protocols l l l l AED Discontinuation of resuscitation* Chest pain COPD/ asthma Trauma protocols Anaphylaxis* ALOC (NYD & OD)* Diabetic emergencies* l Medications – Nitroglycerin – Entonox – Ventolin – SC epi* – SC narcan* – SC glucagon – po glucose gel*
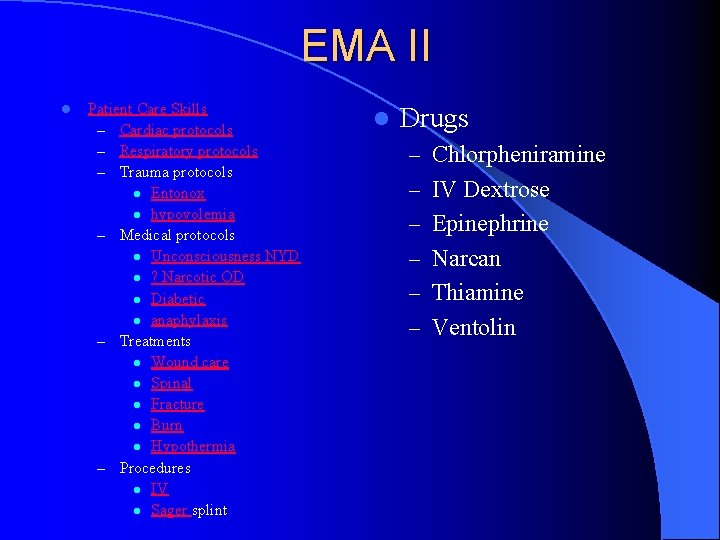
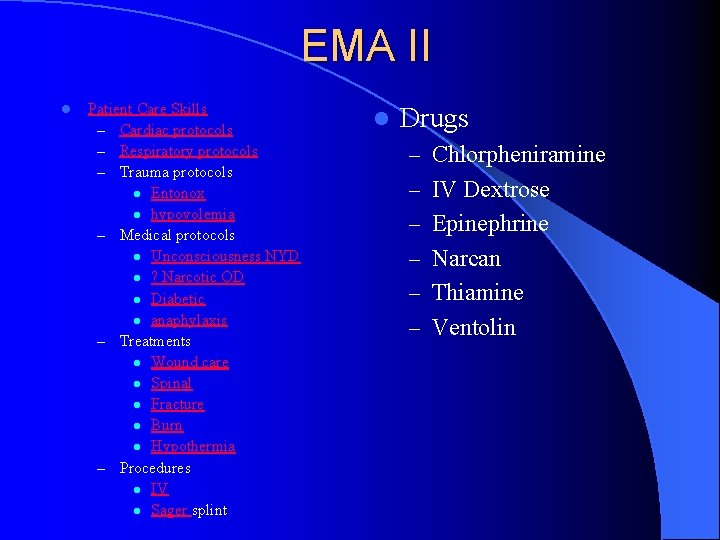
EMA II l Patient Care Skills – Cardiac protocols – Respiratory protocols – Trauma protocols l Entonox l hypovolemia – Medical protocols l Unconsciousness NYD l ? Narcotic OD l Diabetic l anaphylaxis – Treatments l Wound care l Spinal l Fracture l Burn l Hypothermia – Procedures l IV l Sager splint l Drugs – Chlorpheniramine – IV Dextrose – Epinephrine – Narcan – Thiamine – Ventolin
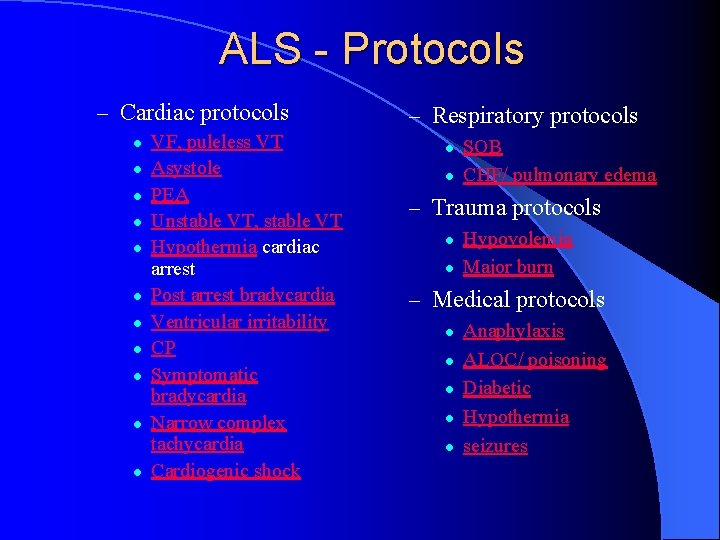
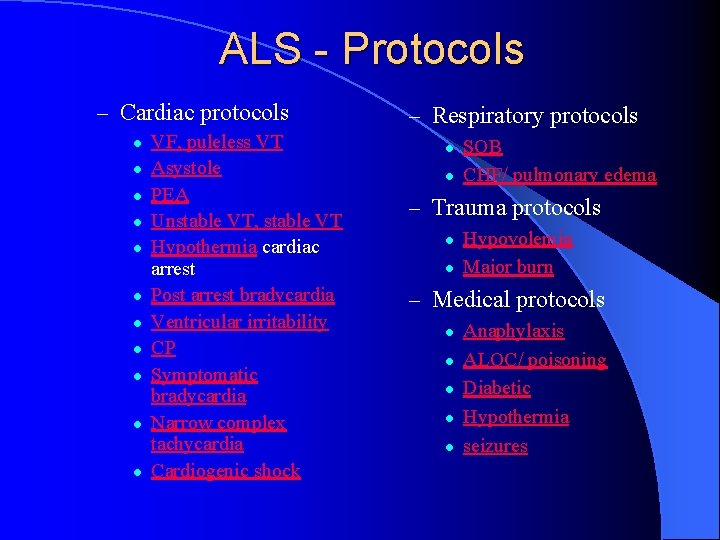
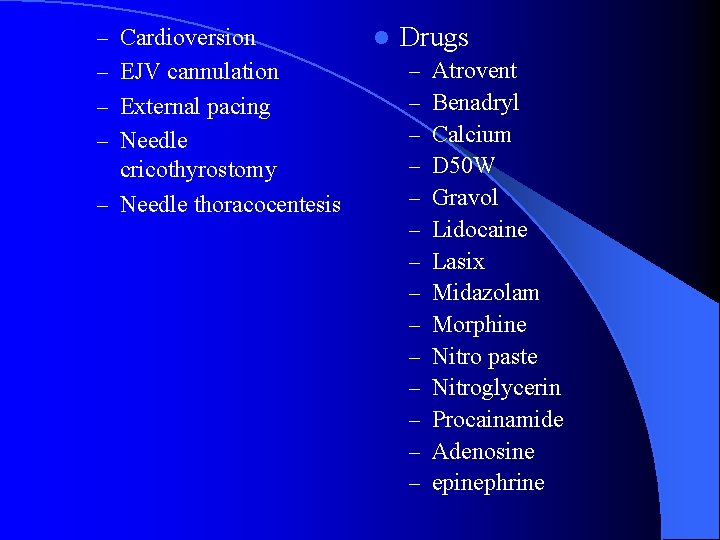
ALS - Protocols – Cardiac protocols l l l VF, puleless VT Asystole PEA Unstable VT, stable VT Hypothermia cardiac arrest Post arrest bradycardia Ventricular irritability CP Symptomatic bradycardia Narrow complex tachycardia Cardiogenic shock – Respiratory protocols l l SOB CHF/ pulmonary edema – Trauma protocols l l Hypovolemia Major burn – Medical protocols l l l Anaphylaxis ALOC/ poisoning Diabetic Hypothermia seizures
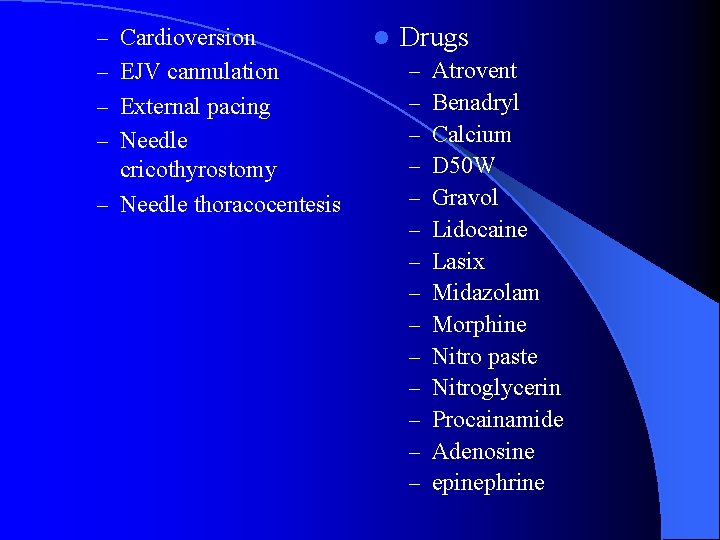
– Cardioversion – EJV cannulation – External pacing – Needle cricothyrostomy – Needle thoracocentesis l Drugs – – – – Atrovent Benadryl Calcium D 50 W Gravol Lidocaine Lasix Midazolam Morphine Nitro paste Nitroglycerin Procainamide Adenosine epinephrine

PART III – Medical Oversight
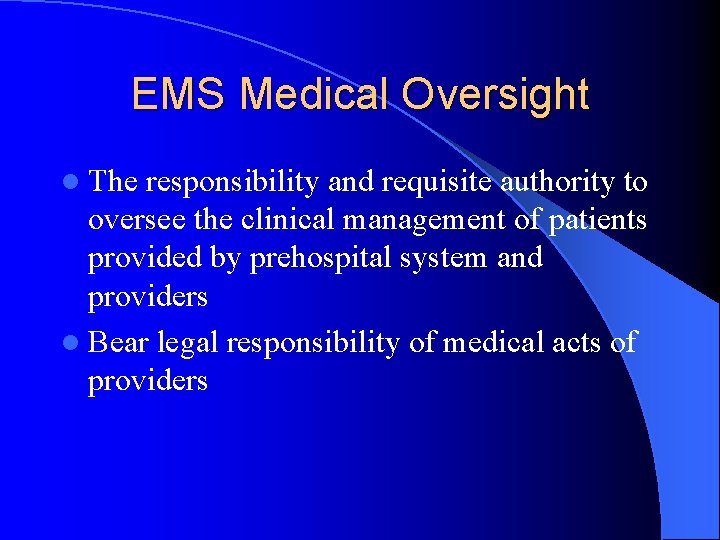
EMS Medical Oversight l The responsibility and requisite authority to oversee the clinical management of patients provided by prehospital system and providers l Bear legal responsibility of medical acts of providers

Desirable qualification l Board certified in EM l Active clinical practice in EM l EMS fellowship
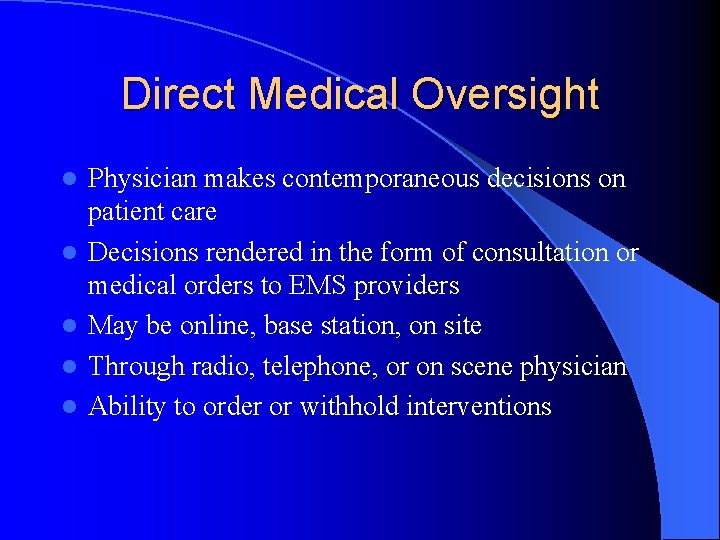
Direct Medical Oversight l l l Physician makes contemporaneous decisions on patient care Decisions rendered in the form of consultation or medical orders to EMS providers May be online, base station, on site Through radio, telephone, or on scene physician Ability to order or withhold interventions

Examples of Direct Medical Oversight – – – – – Medical orders Refusal of medical aid Transportation destinations Medevac authorizations Hospital diversion requests Triage out of system Pronouncement of death Quality assurance mechanism management Patient discharge with community follow up
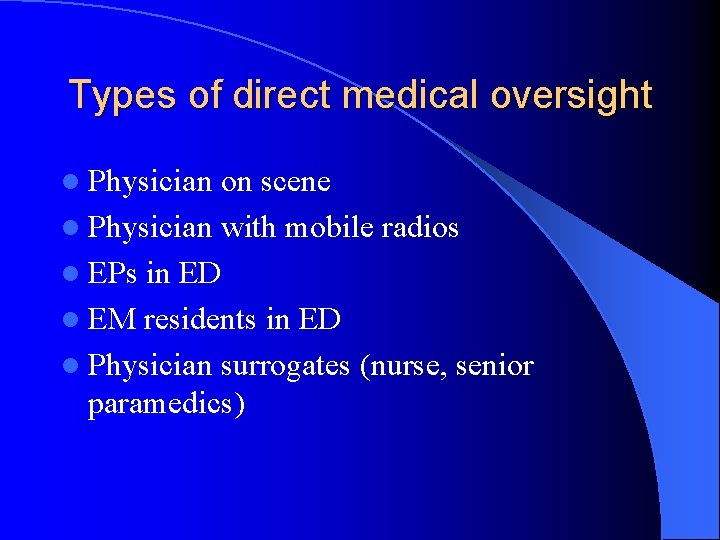
Types of direct medical oversight l Physician on scene l Physician with mobile radios l EPs in ED l EM residents in ED l Physician surrogates (nurse, senior paramedics)
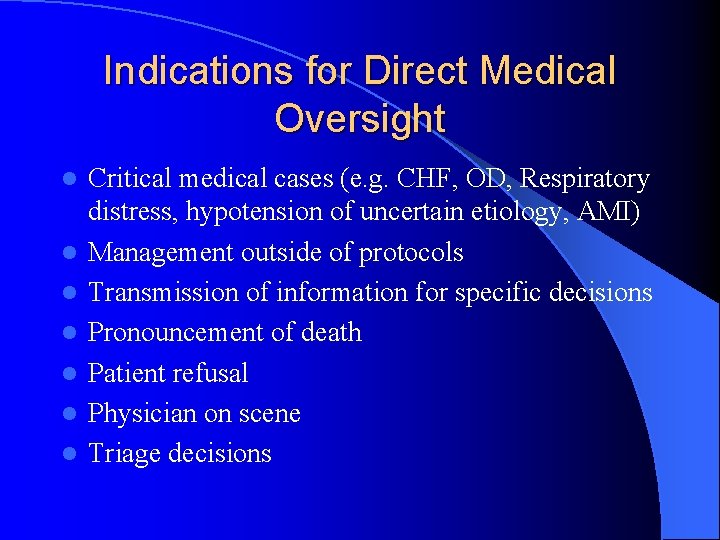
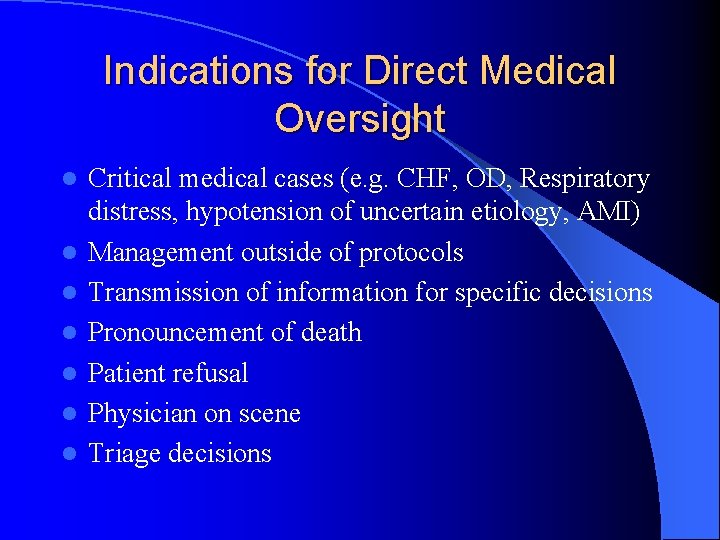
Indications for Direct Medical Oversight l l l l Critical medical cases (e. g. CHF, OD, Respiratory distress, hypotension of uncertain etiology, AMI) Management outside of protocols Transmission of information for specific decisions Pronouncement of death Patient refusal Physician on scene Triage decisions
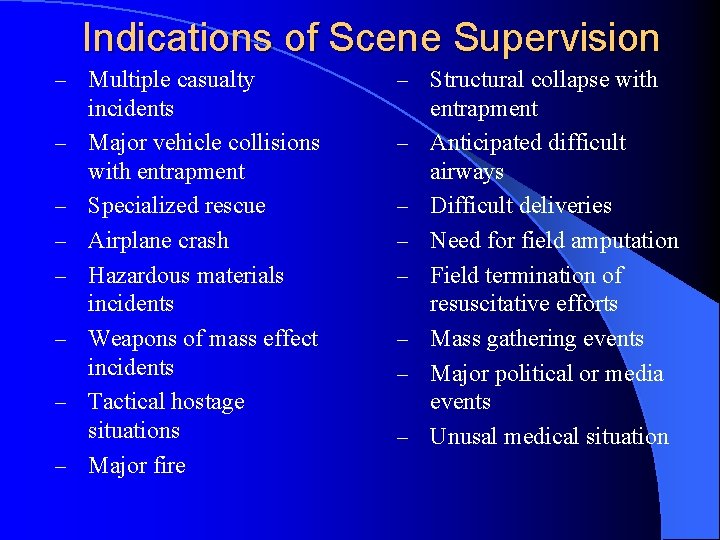
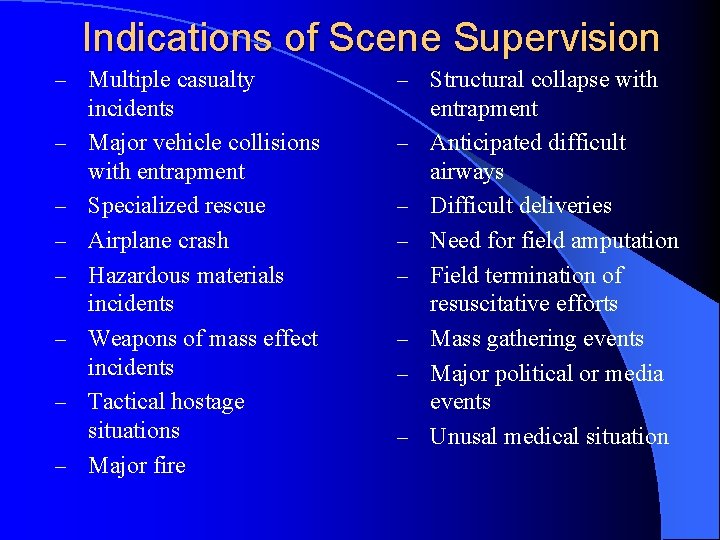
Indications of Scene Supervision – Multiple casualty – – – – incidents Major vehicle collisions with entrapment Specialized rescue Airplane crash Hazardous materials incidents Weapons of mass effect incidents Tactical hostage situations Major fire – Structural collapse with – – – – entrapment Anticipated difficult airways Difficult deliveries Need for field amputation Field termination of resuscitative efforts Mass gathering events Major political or media events Unusal medical situation

Indirect Medical Oversight l Medical oversight activities that are performed prospective, concurrent, retrospective, to prehospital care of the patient l Protocols, policy, QA/QI, education, operations, communications, system design, disaster management, public health
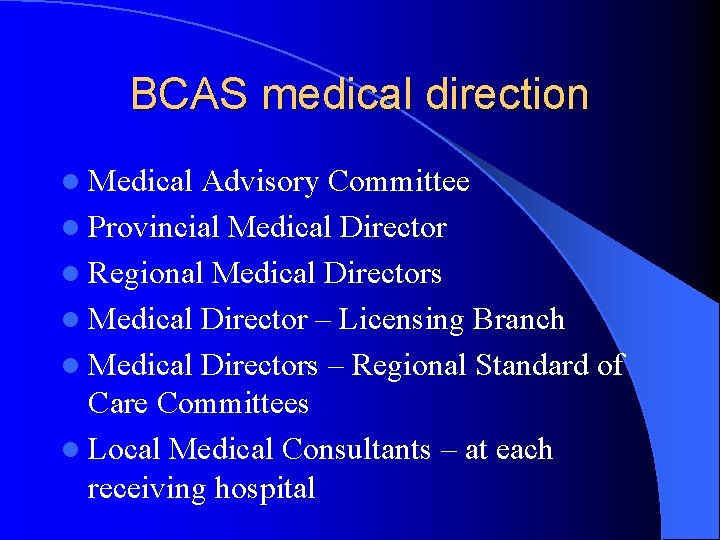
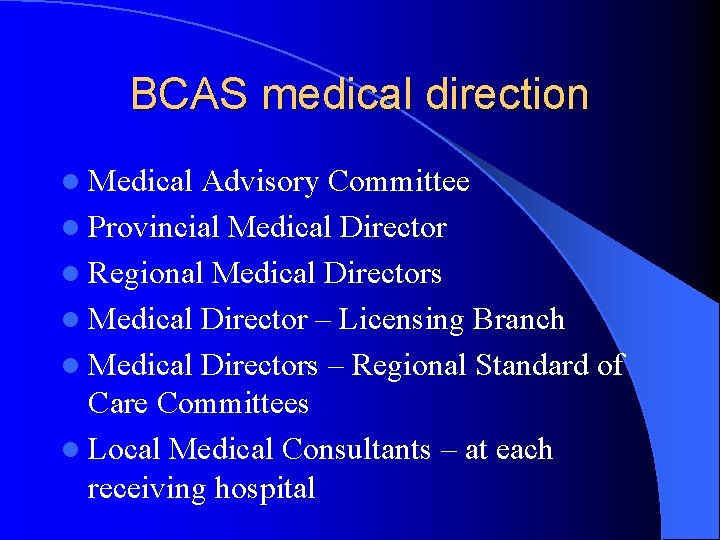
BCAS medical direction l Medical Advisory Committee l Provincial Medical Director l Regional Medical Directors l Medical Director – Licensing Branch l Medical Directors – Regional Standard of Care Committees l Local Medical Consultants – at each receiving hospital
Principles in protocol development l Medically appropriate l Can be implemented in the field l Cost effective
Factors to consider when developing medical protocols l Need l Evidence based medicine l Financial and administrative impact l Educational requirement l Performance measure indicator l Agreement among all stakeholders
Practice management issues in protocol development l Definition of patient vs non-patient l Definition of a minor l Transport vs non transport criteria l Refusal of care process and requirement l Termination of field resuscitation l Assessment of patient competency l On scene physician authority l Transport destination determination l Hospital diversion issues l Credentiating and decreditiating requirements for providers l Patient record documentation requirements l Mass casualty management
Patient Care issues in protocol development l Communication issues l Clinical practice in the field l Criteria for determination of death l Criteria for performing clinical procedures and interventions
 Provincial medical oversight
Provincial medical oversight Introduction to ems
Introduction to ems Role of audit oversight board in malaysia
Role of audit oversight board in malaysia Functional capabilities board
Functional capabilities board Aob sanction
Aob sanction Brig. gen
Brig. gen Board of directors risk oversight responsibilities
Board of directors risk oversight responsibilities Management oversight and risk tree
Management oversight and risk tree Public procurement oversight advisory board
Public procurement oversight advisory board Ohrp is an oversight body
Ohrp is an oversight body Delivery oversight
Delivery oversight Ohrp is an oversight body
Ohrp is an oversight body Administrative oversight definition
Administrative oversight definition Risk based oversight
Risk based oversight Regulatory oversight definition
Regulatory oversight definition Low income oversight board
Low income oversight board The idea that judges ought to freely strike down
The idea that judges ought to freely strike down Felmores doctors
Felmores doctors Computer training seminar memo
Computer training seminar memo National training seminar
National training seminar Chicago management training seminar
Chicago management training seminar Introduction to seminar presentation
Introduction to seminar presentation Left driving countries
Left driving countries Introduction to seminar
Introduction to seminar Debate introduction examples
Debate introduction examples California medical license application
California medical license application Greater baltimore medical center medical records
Greater baltimore medical center medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records Nipt test kuwait
Nipt test kuwait Dfps medical consent training
Dfps medical consent training Dot regulated medical waste
Dot regulated medical waste Joint special operations medical training center
Joint special operations medical training center Introduction to medical informatics
Introduction to medical informatics Medical terminology chapter 1 answer key
Medical terminology chapter 1 answer key Pathological waste disposal
Pathological waste disposal The word root athr means ________
The word root athr means ________ Introduction to emergency medical care
Introduction to emergency medical care Introduction to medical virology
Introduction to medical virology Medical shorthand symbols
Medical shorthand symbols Introduction to medical terminology chapter 1
Introduction to medical terminology chapter 1 Basic medical ethics
Basic medical ethics Chapter 1 introduction to medical terminology
Chapter 1 introduction to medical terminology Hydroclave treatment
Hydroclave treatment Screw feed technology of waste management
Screw feed technology of waste management Tdh ems
Tdh ems Medical
Medical Introduction to emergency medical care
Introduction to emergency medical care Wi ems elicensing
Wi ems elicensing