A Case of Acute Promyelocytic Leukemia Disclosures None


- Slides: 19
A Case of Acute Promyelocytic Leukemia
Disclosures None
Presentation 62 f presented to Canadian hospital with constitutional symptoms and diagnosed with acute promyelocytic leukemia and referred for urgent management to regional oncology center
Worsening clinical status After starting ATRA and TLS prophylaxis the patient started to develop worsening respiratory distress and AKI The patient was transferred to the ICU when patient was requiring >60%FM for management of worsening hypoxic respiratory failure. At that time patient was pancytopenic with PMN <0. 1, Plt 43, Hg 83, INR 1. 5
Continued deterioration Patient was already being treated with piptazo, vancomycin and fluconazole empirically with no positive cultures at that point in time With recommendation from ID service was stepped up to Meropenem/Vanco/Caspofungin
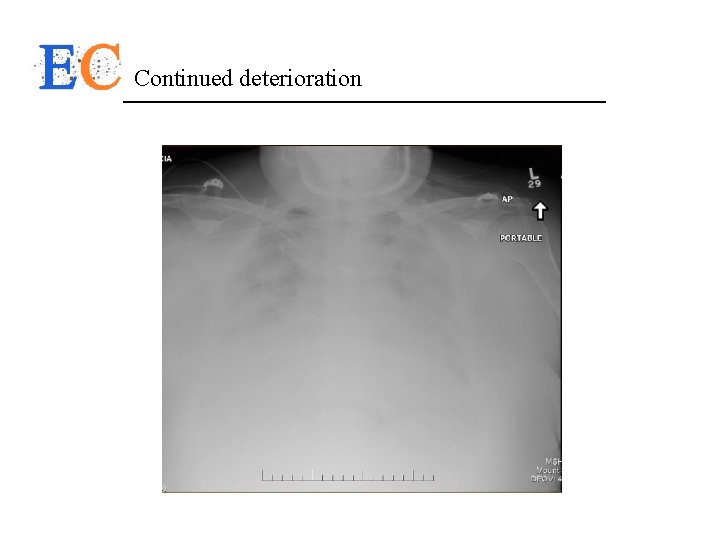
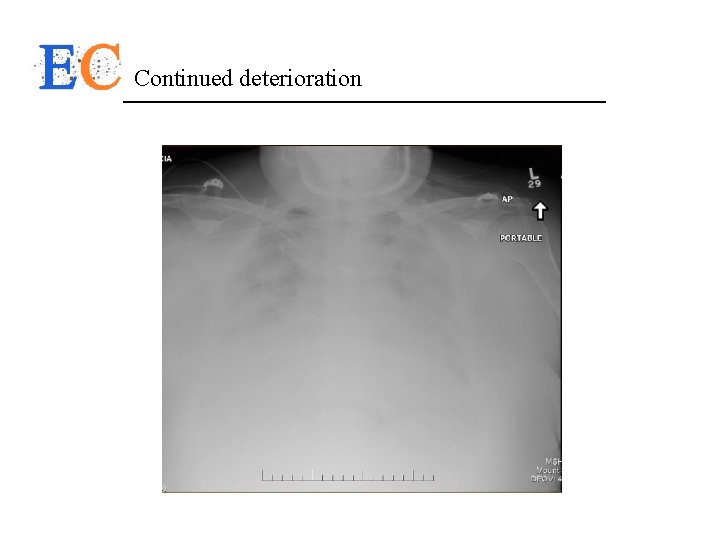
Continued deterioration
Continued deterioration With ongoing respiratory failure despite attempts with non-invassive ventilation patient was intubated for hypoxia At time of intubation patient was alert and communicative with no clear deficits. BAL was done after intubation that demonstrated culture negative washings, no active pulmonary hemorrhage
Continued deterioration Despite ongoing urine output, the likelihood of pulmonary edema contributing to respiratory failure and relative ineffective diuresis on lasix patient was started on CRRT for Uf requirements. Patient continued to deteriorate to severe ARDS requiring paralysis and proning. Throughout their stay the patient was requiring ongoing intermittent transfusions of platelets and hemoglobin. Her platelets ranged from 10 -42 and hemoglobin from 62 -86. INR remained stable 1. 4 -1. 8 with normal fibrinogen

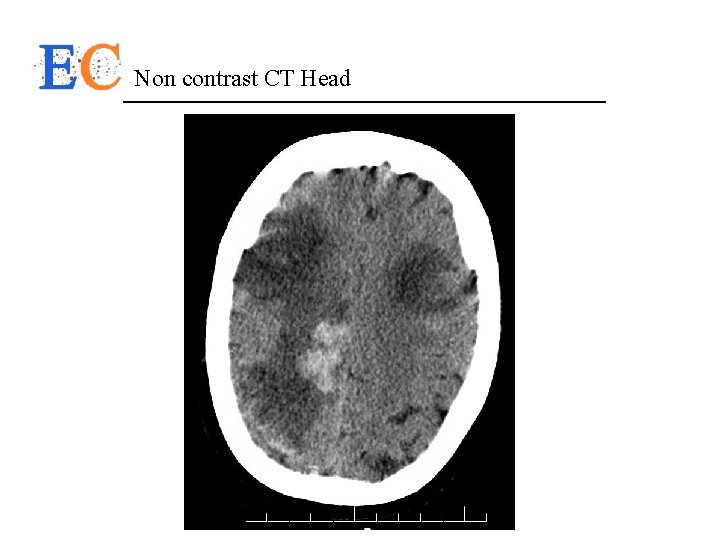
Finally improvement… With lung protective ventilation, proning/paralysis, consistently negative fluid balance and broad spectrum antibiotics the patient slowly improved over the next week to minimal ventilation requirements. At this point sedation was weaned off in the hopes of moving towards extubation After 72 h off sedation patient had still not awoke. As a result had CT head to screen for structural causes.
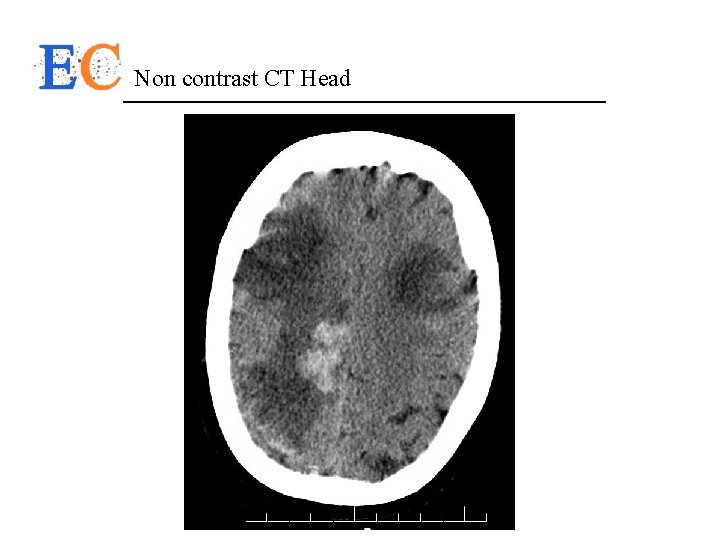
Non contrast CT Head
Outcome After discussion with the patients SDM: Severe disability and unclear recovery clinically would not have been in fitting with the patients previously expressed wishes. As a result, there was withdrawal of life sustaining therapies with palliation.

Outcomes in APML Since the introduction of all-trans retinoic acid (ATRA) in the treatment and optimization of the ATRA-based regimens, the clinical remission (CR) rate was raised up to 90% to 95% and 5 -year disease free survival (DFS) to 74%. The use of arsenic trioxide (ATO) since early 1990 s further improved the clinical outcome of refractory or relapsed as well as newly diagnosed APML Acute promyelocytic leukemia: from highly fatal to highly curable Zhen-Yi Wang and Zhu Chen Blood 2008 111: 2505 -2515 doi: http: //dx. doi. org/10. 1182/blood-2007 -07 -102798
What to target? 5. 1. 2. Other supportive measures. Apart from the aforementioned specific measures, general supportive care aspects in APL, the use of antibiotics, hematopoietic growth factors, prevention of tumor lysis syndrome, and transfusion policy, including red cell, granulocyte, and platelet transfusions (once the coagulopathy is under control), do not differ from those applied in patients with other subtypes of AML. Management of acute promyelocytic leukemia: recommendations from an expert panel on behalf of the European Leukemia. Net Miguel A. Sanz, David Grimwade, Martin S. Tallman, Bob Lowenberg, Pierre Fenaux, Elihu H. Estey, Tomoki Naoe, Eva Lengfelder, Thomas Büchner, Hartmut. Döhner, Alan K. Burnett and Francesco Lo-Coco Blood 2009 113: 1875 -1891; doi: http: //dx. doi. org/10. 1182/blood-2008 -04150250
What to target? “The US Intergroup and the Programa de Estudio y Tratamiento de las Hemopatías Malignas (PETHEMA) group have reported around 5% of patients considered not eligible for induction therapy due to very poor clinical condition (Eastern Cooperative Oncology Group [ECOG] performance status 3), mostly due to lethal or life-threatening hemorrhages before starting therapy. ”
What to target? “Such replacement therapy should continue during induction therapy until disappearance of all clinical and laboratory signs of coagulopathy” SEFTEL, M. D. et al. A Canadian consensus on the management of newly diagnosed and relapsed acute promyelocytic leukemia in adults. Current Oncology, [S. l. ], v. 21, n. 5, p. 234 -250, aug. 2014. ISSN 17187729. Available at: <http: //www. current-oncology. com/index. php/oncology/article/view/2183/1621>. Date accessed: 13 dec. 2016. doi: http: //dx. doi. org/10. 3747/co. 2183. Management of acute promyelocytic leukemia: recommendations from an expert panel on behalf of the European Leukemia. Net Miguel A. Sanz, David Grimwade, Martin S. Tallman, Bob Lowenberg, Pierre Fenaux, Elihu H. Estey, Tomoki Naoe, Eva Lengfelder, Thomas Büchner, Hartmut. Döhner, Alan K. Burnett and Francesco Lo-Coco Blood 2009 113: 1875 -1891; doi: http: //dx. doi. org/10. 1182/blood-2008 -04 -150250
Patients at Higher Risk for life threatening bleed • Active bleeding • hypofibrinogenemia (<100 mg/d. L) • increased levels of fibrin degradation products or D-dimers combined with prolonged prothrombin time or activated partial thromboplastin time • increased WBC counts or peripheral blast counts • abnormal levels of creatinine • poor performance status SEFTEL, M. D. et al. A Canadian consensus on the management of newly diagnosed and relapsed acute promyelocytic leukemia in adults. Current Oncology, [S. l. ], v. 21, n. 5, p. 234 -250, aug. 2014. ISSN 1718 -7729. Available at: <http: //www. current-oncology. com/index. php/oncology/article/view/2183/1621>. Date accessed: 13 dec. 2016. doi: http: //dx. doi. org/10. 3747/co. 2183.
Guideline Goals • the recommendations call for aggressive and ongoing transfusions with fresh frozen plasma, cryoprecipitate, and platelet concentrates • maintain fibrinogen levels above 1. 5 g/L • platelet levels at 30– 50× 109/L Minimum work up: • platelet count, prothrombin time, activated partial thromboplastin time, and fibrinogen level at diagnosis and q 6 h thereafter as daily may be inadequate SEFTEL, M. D. et al. A Canadian consensus on the management of newly diagnosed and relapsed acute promyelocytic leukemia in adults. Current Oncology, [S. l. ], v. 21, n. 5, p. 234 -250, aug. 2014. ISSN 1718 -7729. Available at: <http: //www. current-oncology. com/index. php/oncology/article/view/2183/1621>. Date accessed: 13 dec. 2016. doi: http: //dx. doi. org/10. 3747/co. 2183.
Guideline Goals • The use of anticoagulant or antifibrinolytic therapy such as heparin or tranexamic acid to reduce the risk of bleeding is not recommended • Invasive procedures such as lumbar puncture and central venous catheterization are to be avoided before and during the early stages of remission induction because of the high risk of bleeding in APML SEFTEL, M. D. et al. A Canadian consensus on the management of newly diagnosed and relapsed acute promyelocytic leukemia in adults. Current Oncology, [S. l. ], v. 21, n. 5, p. 234 -250, aug. 2014. ISSN 1718 -7729. Available at: <http: //www. current-oncology. com/index. php/oncology/article/view/2183/1621>. Date accessed: 13 dec. 2016. doi: http: //dx. doi. org/10. 3747/co. 2183.
Our Guideline Goals Question to the group: - Should we be trending fibrinogen levels q 6 h? - Should we have a strict 30– 50× 109/L platelet transfusion threshold? - What should the anti-coagulant approach be if that threshold is used?
 Acute promyelocytic leukemia
Acute promyelocytic leukemia Differentiation syndrome
Differentiation syndrome Acute mylogenous leukemia
Acute mylogenous leukemia Voluntary disclosures meaning
Voluntary disclosures meaning No disclosure slide
No disclosure slide Website disclosures under companies act 2013
Website disclosures under companies act 2013 No disclosures slide
No disclosures slide When becomes weakness
When becomes weakness Best case worst case average case
Best case worst case average case Pas staining principle
Pas staining principle Zhang wang leukemia
Zhang wang leukemia Chronic myeloid leukemia
Chronic myeloid leukemia Conclusion differentiation
Conclusion differentiation Leukemia
Leukemia Nk leukemia
Nk leukemia Leukemia death rate
Leukemia death rate What is the difference between lymphoma and leukemia
What is the difference between lymphoma and leukemia Asparagine
Asparagine Hairy cell leukemia
Hairy cell leukemia Leukemia statics
Leukemia statics