2018 IHCP 1 st Quarter Workshop MDwise Updates


- Slides: 32
2018 IHCP 1 st Quarter Workshop MDwise Updates Spring 2018 HHW-HIPP 0541(2/18) Exclusively serving Indiana families since 1994.
Agenda • Meet you Provider Relations Team • Quality Review • ER Utilization • Tips for Claims Adjudication • Contact Information • Resources • Questions -2 -
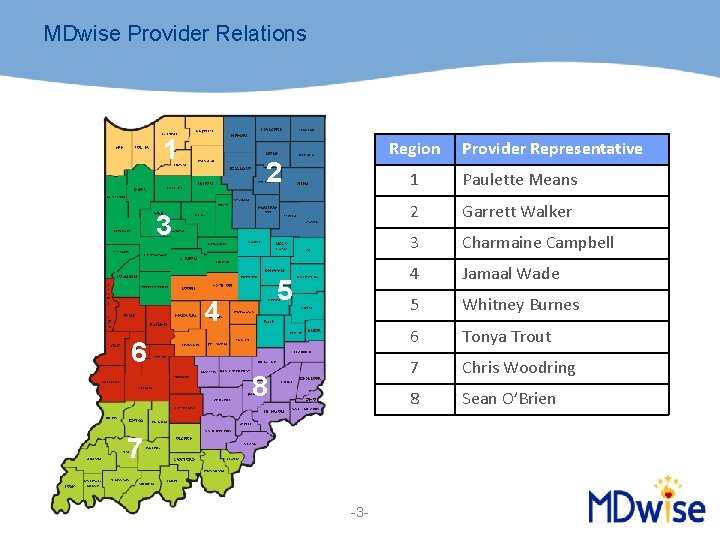
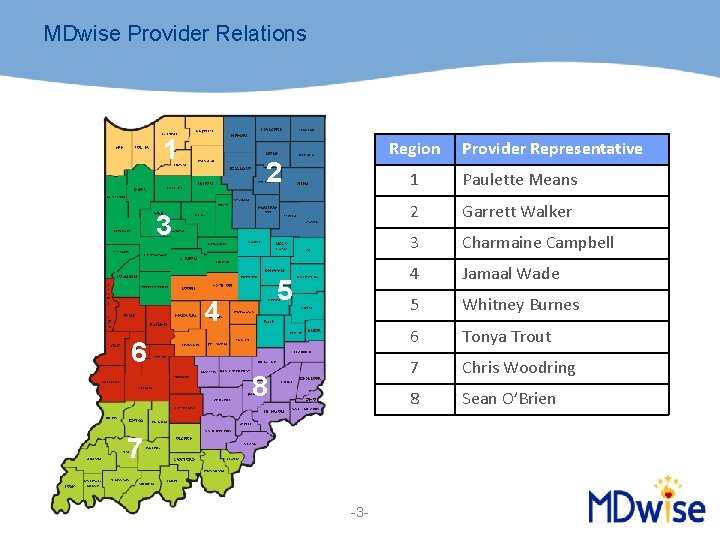
MDwise Provider Relations 1 Region 2 3 5 4 6 8 7 -3 - Provider Representative 1 Paulette Means 2 Garrett Walker 3 Charmaine Campbell 4 Jamaal Wade 5 Whitney Burnes 6 Tonya Trout 7 Chris Woodring 8 Sean O’Brien
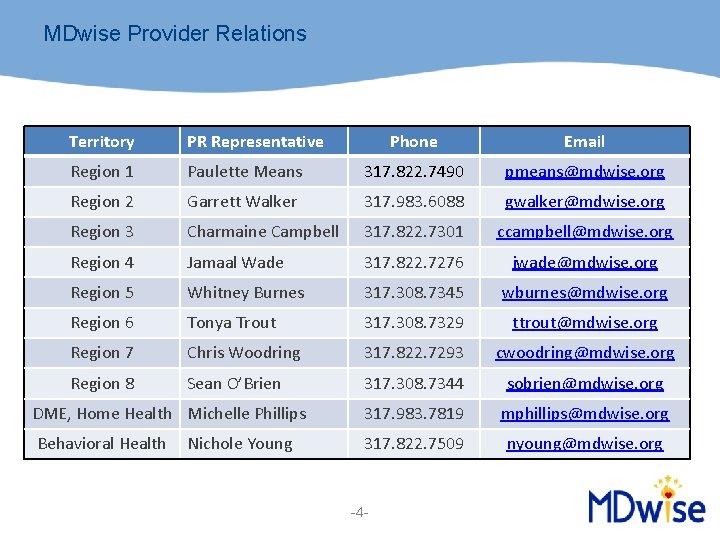
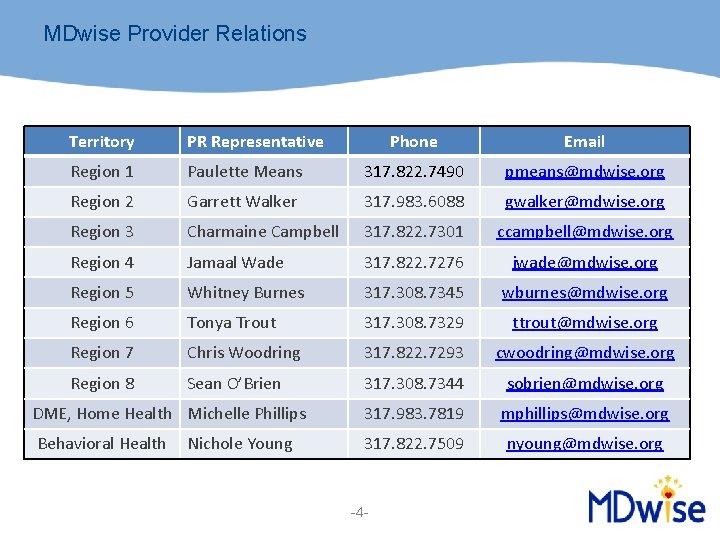
MDwise Provider Relations Territory PR Representative Phone Email Region 1 Paulette Means 317. 822. 7490 pmeans@mdwise. org Region 2 Garrett Walker 317. 983. 6088 gwalker@mdwise. org Region 3 Charmaine Campbell 317. 822. 7301 ccampbell@mdwise. org Region 4 Jamaal Wade 317. 822. 7276 jwade@mdwise. org Region 5 Whitney Burnes 317. 308. 7345 wburnes@mdwise. org Region 6 Tonya Trout 317. 308. 7329 ttrout@mdwise. org Region 7 Chris Woodring 317. 822. 7293 cwoodring@mdwise. org Region 8 Sean O’Brien 317. 308. 7344 sobrien@mdwise. org DME, Home Health Michelle Phillips 317. 983. 7819 mphillips@mdwise. org Behavioral Health 317. 822. 7509 nyoung@mdwise. org Nichole Young -4 -
Quality What is Quality? • Quality is comprised of HEDIS measures and NCQA guidelines – HEDIS – Healthcare Effectiveness Data and Information Set – National Committee for Quality Assurance (NCQA) uses these performance measures for commercial insurance, Medicare, and Medicaid – HEDIS is the most used set of performance measures in the Managed Care industry, developed and maintained by NCQA – Administrative data is calculated by a claim or an encounter submitted to the health plan – Annual State mandated quality improvement initiative required of all Health plans -5 -
Quality MDwise Quality Improvement (QI) program • Designed to lead to improvements in the delivery of health care and services, inclusive of both physical and behavioral health, to its members, as well as in all health plan functional areas • MDwise conducts an annual CAHPS (Consumer Assessment of Healthcare Providers and Systems) survey to determine member satisfaction with the plan and network providers • MDwise is focused on providing services to members that are culturally and linguistically appropriate • MDwise quality improvement initiatives strive to achieve significant improvement over time in identified clinical care and non-clinical care/service areas -6 -
Quality Did you know: • MDwise has dedicated teams who educate on HEDIS, NCQA, and OMPP standards through office visits – MDwise Quality and Network Improvement Teams • These teams are here to maximize the opportunity for MDwise, Inc. to recoup as much of the State withhold on quality as possible in the targeted Pay for Outcomes (P 4 O) measures -7 -
Quality How We Promote Quality Care: • Provider and staff education • Network Improvement Program (NIP) Team • Billing and process audits • Member education and incentives • Provider Incentives • Care Management services for members -8 -
Quality Opportunities for Quality Improvement • Maximize every member interaction to provide preventive and well-care • Proactive Outreach: Staff who does scheduling can identify members that need services to schedule in a timely fashion • Ensure proper billing for services rendered • Be sure that the documentation is complete • Implement alerts to reflect the non–compliant members in the quality measures if EMRs (electronic medical records) are used -9 -
Quality What is P 4 O? • A reward through FSSA for providers who meet the standards of high quality preventive care What determines if I am eligible for P 4 O? • FSSA established benchmarks that are set on an annual basis • Standards defined in health plan contract • Measures are typically nationally recognized HEDIS measures developed by NCQA for use in health plan accreditation • Performance of network providers is tracked based on submitted claims -10 -
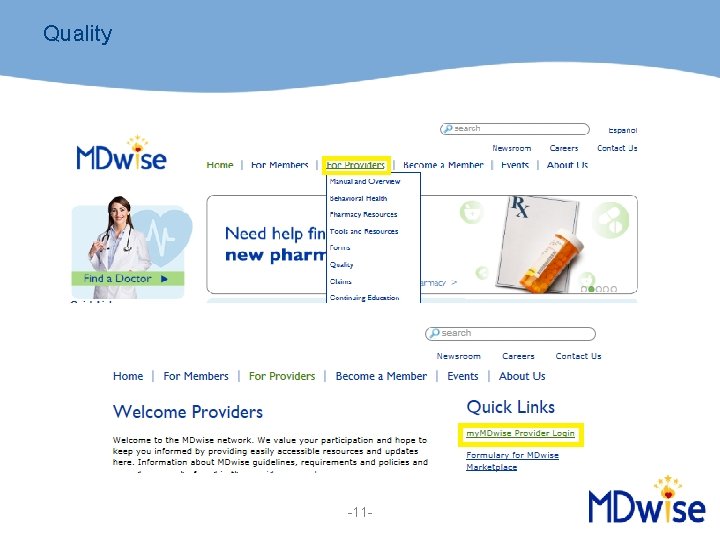
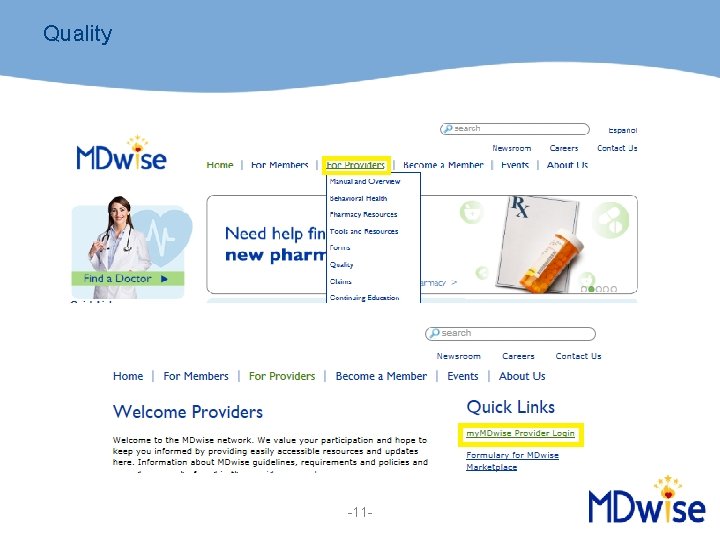
Quality -11 -
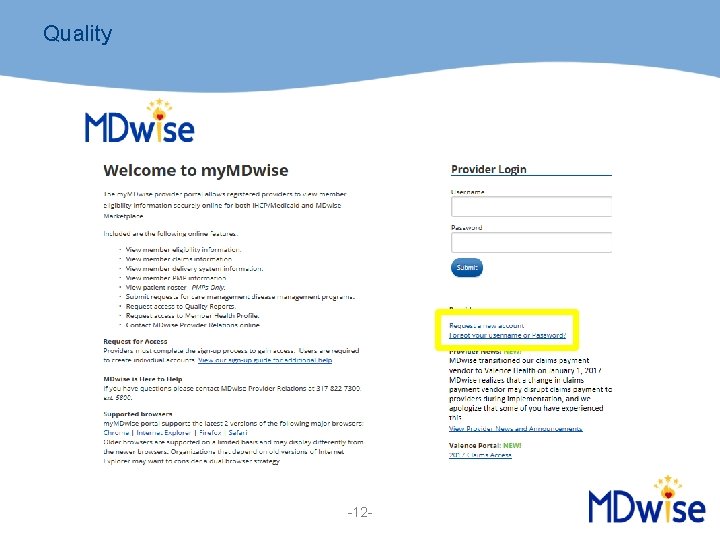
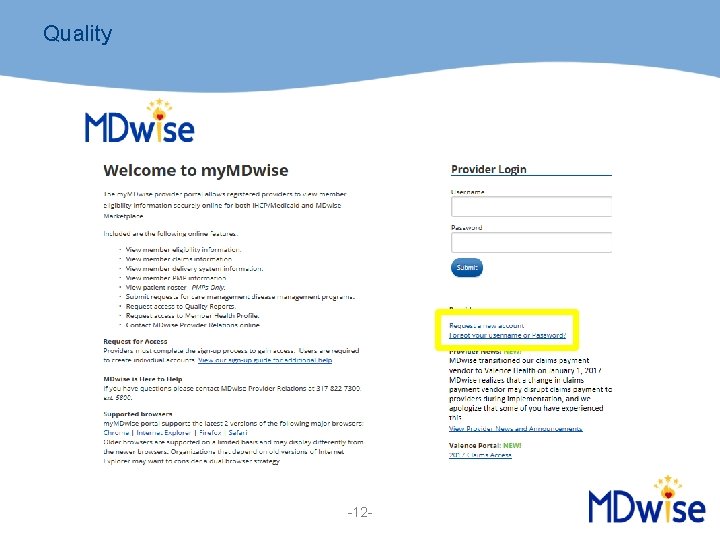
Quality -12 -

Quality Online Quality Reports • Quality reports, members in need of services, and provider panels available online and updated monthly -13 -
ER Utilization An emergency medical condition is defined in IC 12 -15 -12 -0. 3 as a medical condition manifesting itself by acute symptoms, including severe pain, could reasonably expect the absence of immediate medical attention to result in: • Serious jeopardy to the health of: – the individual – in the case of a pregnant woman, the woman or her unborn child • Serious impairment to bodily functions • Serious dysfunction of any bodily organ or part -14 -
ER Utilization Instead of the emergency room, encourage members to utilize: • • Assigned PMP Urgent Care Walk-In Clinics After Hours Offices • Find A Doctor – http: //www. mdwise. org/find-a-doctor – Select the Hoosier Healthwise or HIP – Search by provider type -15 -
ER Utilization Reminder: • If a member has an urgent health need or is unsure if it is an emergency, they are always encouraged to call: – Assigned PMP – MDwise NURSEon-call – 24 -hour nurse hotline • If you feel a member may be inappropriately using the emergency room for primary care services, please inform MDwise by calling 1 -800 -356 -1204 or contact your Provider Relations Representative -16 -
ER Utilization Care Management/Disease Management • MDwise identifies care management as an integral part of medical management — Care management involves the development and implementation of a coordinated, member-focused plan of care that meets the member’s needs and promotes optimal outcomes — Care management objectives include: • Developing and facilitating interventions that coordinate care across the continuum of health care services • Decreasing fragmentation or duplication of services • Promoting access or utilization of appropriate resources -17 -
ER Utilization The Right Choices (RCP) program was created to safeguard against unnecessary or inappropriate use of Medicaid services by identifying members who use Indiana Health Coverage Programs (IHCP) services more extensively than their peers MDwise considers multiple factors in enrolling a member into this program. They include, but are not limited to: • • • ER utilization Pharmacy utilization Member compliance Outcomes of member interventions Referrals from providers -18 -
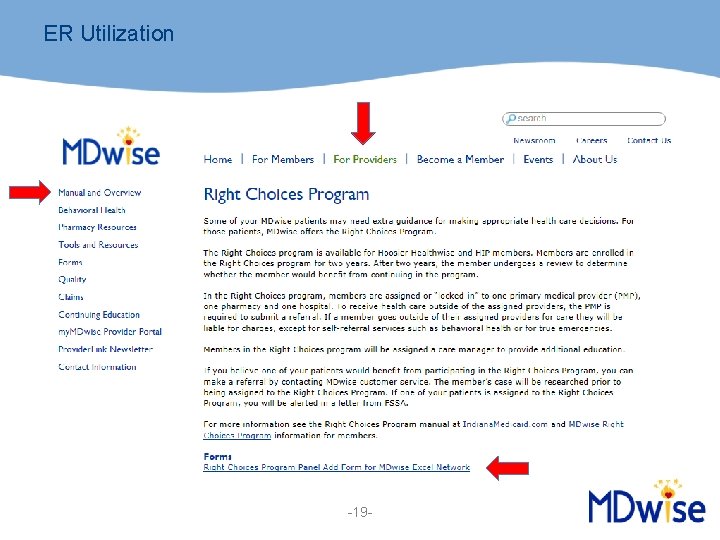
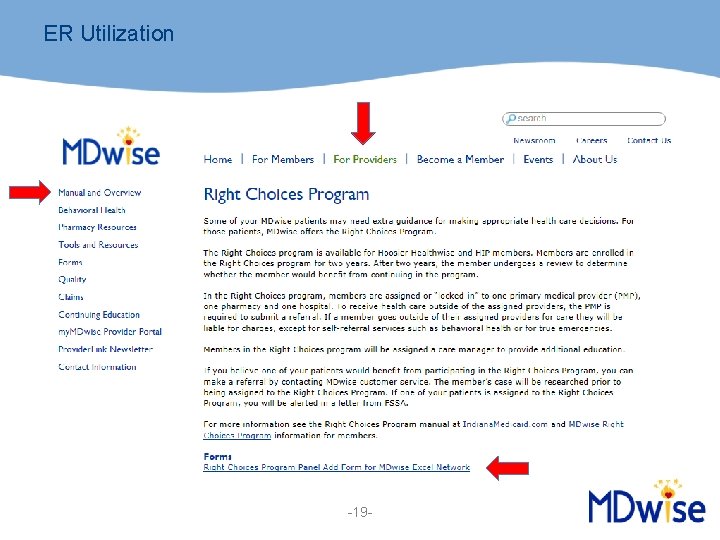
ER Utilization -19 -
ER Utilization • ER services do not require a PA but may require prudent layperson (PLP) review • Certain ER codes are paid according to the ER auto-pay list found at MDwise. org • To automatically initiate PLP review and receive possible additional payment, claims should be submitted with medical records -20 -
Claims Tips Provider Requirements • Provider must: – Be registered and be actively eligible with the Indiana Health Coverage Program (IHCP) – Be enrolled with the appropriate MDwise delivery system – Obtain a prior authorization if the provider is out of network – Complete all required elements on the appropriate claim form – Submit claim to appropriate MDwise delivery system claims payer -21 -
Claims Tips Prior to rendering services: • Verify their following eligibility information – – IHCP program Managed Care Entity (MCE) What delivery system they are assigned to Assigned PMP • Confirm if the services to be rendered require PA and request a PA if appropriate – Non-Urgent PA requests: 7 day turn around – Urgent PA requests: 3 day turn around -22 -
Claims Tips Claim Form Requirements • IHCP outlines all required fields for the CMS 1500 and UB-04 claims forms in the Provider Modules • Follow correct coding guidelines for claims submission • Verify that the correct place of service codes are submitted • Confirm appropriate modifiers are included • Check for proper diagnosis code(s) • Include the rendering provider NPI -23 -
Claims Tips Claim Form Submission • Make sure you submit the claim to the correct payer • Be sure claims are submitted timely: – Contracted providers must submit claims to MDwise within 90 days of the date of rendering the service – When MDwise is secondary, claim must be submitted within 90 days of the date on the primary EOB • Claim must be submitted with a copy of the EOB -24 -
Claims Tips Hoosier Healthwise • Paper claims should be submitted to: MDwise HHW Claims P. O. Box 331550 Corpus Christi, TX 78463 -1550 • CMCS pays Hoosier Healthwise claims for: - St. Vincent - Select Health - St. Catherine • All Electronic Data Interchange (EDI) • Change Health/Emdeon/Web MD Payer ID: 35191 Please note: Paper claims must be on red/white form with black ink -25 -
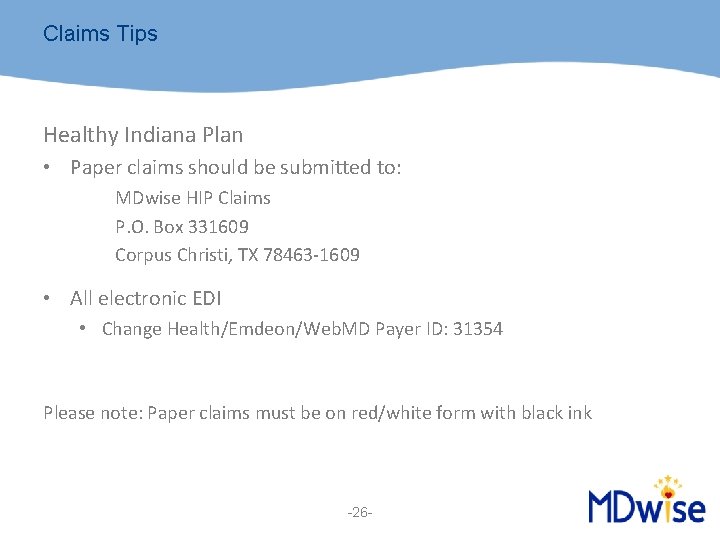
Claims Tips Healthy Indiana Plan • Paper claims should be submitted to: MDwise HIP Claims P. O. Box 331609 Corpus Christi, TX 78463 -1609 • All electronic EDI • Change Health/Emdeon/Web. MD Payer ID: 31354 Please note: Paper claims must be on red/white form with black ink -26 -
Claims Tips If you would like an update on your claim status, please complete the following steps: 1. Check the Evolent Claims Portal a) https: //mdwportal. valence. care/Logon. jsp 2. Contact the MDwise Claims department – 1 -800 -356 -1204 3. Notify your Provider Relations Representative if you see trending denials or have additional questions -27 -
Claims Tips If you would like to dispute a claim, please complete the following steps: 1. Submit a dispute to the claims department a. Complete one Claim Dispute Form for each claim i. Claim Dispute Form b. Submit one Claim Dispute Form per email to cdticket@mdwise. org c. Completely fill out the form and include all supporting documentation in the email d. Be sure you send the email securely -28 -
Claims Tips Items that do no constitute a dispute include: Corrected Claims New Claims Medical Records Attachments, including but not limited to: – Consent forms – MSRP on IHCP website – Invoices • Recoupments • • -29 -
Contact Information Claims Quick Contact Guide • Includes Delivery System claim submission information Provider Relations Contact List • Includes Deliver System Provider Relations contact information MDwise Excel PR Territory Map • Provider Relations Territory Map -30 -
Resources • MDwise Provider Manuals – http: //www. mdwise. org/for-providers/manual-and-overview/ • MDwise Provider Page — http: //www. mdwise. org/for-providers • MDwise Customer Service — 1. 800. 356. 1204 • IHCP Provider Modules – Indianamedicaid. com -31 -

Questions -32 -