2017 American Academy of Neurology Practice Guideline Sudden













































- Slides: 45

© 2017 American Academy of Neurology

Practice Guideline Sudden Unexpected Death in Epilepsy Incidence Rates and Risk Factors Report by: Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Epilepsy Society © 2017 American Academy of Neurology

Practice Guideline Endorsement and Funding This practice guideline was co-developed with the American Epilepsy Society and endorsed by the International Child Neurology Association. This practice guideline was developed with financial support from the American Academy of Neurology (AAN). Authors who serve as AAN subcommittee members or methodologists (C. H. , D. G. , J. A. F. ) were reimbursed by the AAN for expenses related to travel to subcommittee meetings where drafts of manuscripts were reviewed. © 2017 American Academy of Neurology Slide 2

Sharing This Information The AAN develops these presentation slides as educational tools for neurologists and other health care practitioners. You may download and retain a single copy for your personal use. Please contact guidelines@aan. com to learn about options for sharing this content beyond your personal use. © 2017 American Academy of Neurology Slide 3

Presentation Objectives • To present the evidence systematically reviewed in the AAN guideline on sudden unexpected death in epilepsy (SUDEP) § Determine incidence rates in different epilepsy populations § Address whether risk factors for SUDEP have been identified • To present practice recommendations © 2017 American Academy of Neurology Slide 4

Overview § Introduction § Clinical questions § AAN practice guideline process § Methods § Conclusions § Practice recommendations © 2017 American Academy of Neurology Slide 5

Introduction • SUDEP is a poorly understood and catastrophic risk of epilepsy • The sensitive nature of discussions of this infrequent but important risk with patients with epilepsy and their families has prompted the need for evidence-based information about SUDEP • The goal of this practice guideline is to examine evidence regarding the SUDEP incidence rate in different epilepsy populations and any prognostic factors for SUDEP occurrence © 2017 American Academy of Neurology Slide 6

Clinical Questions Clinical Question 1 • What is the incidence rate of SUDEP in different epilepsy populations? Clinical Question 2 • Are there specific risk factors for SUDEP? © 2017 American Academy of Neurology Slide 7

AAN Practice Guideline Process* • Clinical Question • Evidence • Conclusions • Modified Delphi Consensus • Recommendations *Practice guideline broadly developed using the 2004 AAN Clinical Practice Guideline Process Manual. However, 2011 process used to formulate the conclusions and recommendations. © 2017 American Academy of Neurology Slide 8

Literature Search/Review Rigorous, Comprehensive, Transparent 1, 068 abstracts Searched: EMBASE, MEDLINE Inclusion criteria: 35 rated articles © 2017 American Academy of Neurology Exclusion criteria: • Randomized studies • Studies in animals pertinent to the • Languages other than questions English • n > 10 • SUDEP definition provide by Nashef 1997, e 3, Annegers 1997, e 4, and Leetstma et al 1997 e 5 Slide 9

AAN Classification of Evidence Screening Scheme (2011) Class I § Study of a cohort of patients at risk for the outcome from a defined geographic area (i. e. , population based) § The outcome is objective § Also required: –a. Inclusion criteria defined –b. At least 80% of patients undergo the screening of interest © 2017 American Academy of Neurology Slide 10

AAN Classification of Evidence Screening Scheme (2011) Class III Class IV • A non–populationbased nonclinical cohort (e. g. , mailing list, volunteer panel) or a general medical, neurology clinic/center without a specialized interest in the outcome. Study meets criteria a and b (see Class I) • The outcome is objective • A referral cohort from a center with a potential specialized interest in the outcome • Did not include person at risk for the outcome • Did not statistically sample patients or patients specifically selected for inclusion by outcome • Undefined or unaccepted screening procedure or outcome measure • No measure of frequency or statistical precision calculable © 2017 American Academy of Neurology Slide 11

AAN Classification of Evidence Prognostic Scheme (2011 amended in 2015) Class I § Cohort survey with prospective data collection § Includes a broad spectrum of persons at risk for developing the outcome § Outcome measurement is objective or determined without knowledge of risk factor status § Also required: –a. Inclusion criteria defined –b. At least 80 percent of enrolled subjects have both the risk factor and outcome measured © 2017 American Academy of Neurology Slide 12

AAN Classification of Evidence Prognostic Scheme (2011 amended in 2015) Class III Class IV • Cohort study with retrospective data collection or case-control study. Study meets criteria a and b (see Class I) • Includes a broad spectrum of persons with and without the risk factor and the outcome • The presence of the risk factor and outcome are determined objectively or without knowledge of one another • Cohort or case control study • Narrow spectrum of persons with or without the disease • The presence of the risk factor and outcome are determined objectively, without knowledge of the other or by different investigators • Did not include persons at risk for the outcome • Did not include patients with and without the risk factor • Undefined or unaccepted measures of risk factors or outcomes • No measures of association or statistical precision presented or calculable *Objective outcome measurement: an outcome measure that is unlikely to be affected by an observer’s (patient, treating physician, investigator) expectation or bias (e. g. , blood tests, administrative outcome data). © 2017 American Academy of Neurology Slide 13

AAN Conclusions and Recommendation • Confidence in evidence anchored to the studies’ risk of bias § § Highly likely or highly probable* = high confidence level Likely or probable = moderate confidence level Possibly = low confidence level Insufficient evidence = very low confidence level § § Evidence systematically reviewed Strong evidence derived from related conditions Axiomatic principles of care Inferences made from one or more statements in the recommendation rationale § § § Must (or must not) = Level A (strong) Should (or should not) = Level B (moderate) May (or may not) = Level C (weak) Should not = Level R (restricted to research setting only) No recommendation made = Level U (insufficient evidence) • Recommendations informed by premises • Clinician level of obligation assigned (modified Delphi) *Italics denotes language that would appear in the conclusions or recommendations © 2017 American Academy of Neurology Slide 14

Clinical Question 1 What is the incidence of SUDEP in different epilepsy populations? © 2017 American Academy of Neurology Slide 15

Conclusions • Because of imprecision in the incidence results for general populations of persons with epilepsy, authors performed a random-effects meta-analysis for several subpopulations • To explore reasons for heterogeneity in the absolute risk, the panel conducted a meta-analysis of subgroups of studies including different groups of persons with epilepsy © 2017 American Academy of Neurology Slide 16

Conclusions What is the incidence of SUDEP in childhood? Based on moderate confidence in the evidence from 3 Class I studies, SUDEP risk in children with epilepsy is 0. 22/1, 000 patient-years (95% CI 0. 16– 0. 31). © 2017 American Academy of Neurology Slide 17

Conclusions What is the incidence of SUDEP in people with childhood-onset epilepsy, including SUDEP occurrences after adulthood? Based on low confidence in the evidence due to considerable imprecision across 5 Class I studies, e 6, e 7 – e 9, e 16 SUDEP risk increases in adults to 1. 2/1, 000 patient-years (95% CI 0. 64– 2. 32). © 2017 American Academy of Neurology Slide 18

Conclusions What is the incidence of SUDEP in the general epilepsy population? Based on low confidence in the evidence owing to considerable imprecision across 12 Class I studies, the overall SUDEP risk is 0. 58/1, 000 patient-years (95% CI 0. 31– 1. 08). © 2017 American Academy of Neurology Slide 19

Conclusions What is the incidence of SUDEP in the general population of persons with epilepsy who at some point in the course of their disease were likely difficult to treat? Based on moderate confidence in the evidence from 1 Class I study, the general population of people with epilepsy who at some point in the course of their disease were likely difficult to treat, the overall SUDEP incidence rate is 1. 5/1, 000 patient-years (95% CI, 0. 8– 2. 7). © 2017 American Academy of Neurology Slide 20

Conclusions What is the incidence of SUDEP in pregnant women with epilepsy? Based on moderate confidence in the evidence from 1 Class I study, the SUDEP incidence rate for pregnant women with epilepsy is 0. 79/1, 000 pregnancies (95% CI 0. 6– 1. 0). © 2017 American Academy of Neurology Slide 21

© 2017 American Academy of Neurology Slide 22

Table e-2. Conclusions for SUDEP incidence Population Confidence level Overall SUDEP/1, 000 patient-years (CI) 0. 58 (0. 31– 1. 08) Childhood 0. 22 (0. 16– 0. 31) Moderate Adulthood 1. 2 (0. 64– 2. 32) Low © 2017 American Academy of Neurology Low Slide 23

Recommendations: Clinical Question 1 SUDEP incidence in children Level B © 2017 American Academy of Neurology • Clinicians caring for children with epilepsy should inform the children’s parents or guardians that There is a rare risk of SUDEP In 1 year, SUDEP typically affects 1 in 4, 500 children with epilepsy; in other words, annually, 4, 499 of 4, 500 children will not be affected by SUDEP Slide 24

Recommendations: Clinical Question 1 SUDEP incidence in adults Level B © 2017 American Academy of Neurology • Clinicians should inform their adult persons with epilepsy that There is a small risk of SUDEP In 1 year, SUDEP typically affects 1 in 1, 000 adults with epilepsy; in other words, annually, 999 of 1, 000 adults will not be affected by SUDEP Slide 25

Clinical Question 2 Are there any risk factors for SUDEP? © 2017 American Academy of Neurology Slide 26

Most concerning risk factors Factor Presence of GTCS vs lack of GTCS Odds ratio (CI) 10 (7– 14) Confidence level Moderate Frequency of GTCS OR 5. 07 (2. 94– 8. 76) for 1– 2 GTCS per y, and OR 15. 46 (9. 92– 24. 10) for >3 GTCS per y High Not being seizure free for 1– 5 y 4. 7 (1. 4– 16) Moderate Not adding an AED when patients are medically refractory 6 (2– 20) Moderate Nocturnal supervision (risk reduction) 0. 4 (0. 2– 0. 8) Moderate Use of nocturnal listening device (risk reduction) 0. 1 (0. 0– 0. 3) Moderate © 2017 American Academy of Neurology Slide 27

Conclusions Presence or absence of (GTCS) It is likely that GTCS occurrence (vs no GTCS occurrence) increases SUDEP risk, based on moderate confidence in the evidence from 2 Class II studies. Although 1 study shows significance and the other does not, the CI of the smaller studye 21 does not exclude an important effect encompassed by the CI of the larger study. e 20 The larger study also shows a dose-response effect of GTCS occurrence vs not having GTCS on SUDEP risk, e 20 which results in an upgrade of the conclusion to high from moderate. © 2017 American Academy of Neurology Slide 28

Conclusions Seizure-associated factors: GTCS frequency It is highly likely that GTCS frequency is associated with an increased SUDEP risk (based on 2 Class II studies upgraded to high from moderate because of magnitude of the effect). SUDEP risk increases 3 -fold at a GTCS frequency of >3/y, compared with a GTCS frequency of 1– 2/y. © 2017 American Academy of Neurology Slide 29

Conclusions Seizure-associated factors: Seizure freedom/seizure remission It is likely that having a seizure within the last year increases SUDEP risk (moderate confidence in the evidence based on 2 Class II studies), as does having a seizure in the previous 5 years (moderate confidence in the evidence based on 1 Class I study) compared with being seizure free. © 2017 American Academy of Neurology Slide 30

Conclusions Highly refractory epilepsy • There is insufficient evidence to support or refute the prognostic value of refractory epilepsy for SUDEP (vs newly diagnosed epilepsy) (very low confidence in the evidence, 2 Class I studies, both with insufficient precision to drive recommendations because 95% CIs included both important and unimportant differences). © 2017 American Academy of Neurology Slide 31

Conclusions Nocturnal supervision It is likely that nocturnal supervision defined as the presence in the bedroom of another individual of normal intelligence and at least 10 years old is associated with a decreased SUDEP risk (confidence in the evidence from 1 Class II study upgraded to moderate from low because of magnitude of the effect of 20%– 80% reduction). © 2017 American Academy of Neurology Slide 32

Conclusions Nocturnal listening device It is likely that use of regular checks throughout the night or a nocturnal listening device is associated with a decreased SUDEP risk (confidence in the evidence from 1 Class II study upgraded to moderate from low because of magnitude of the effect of at least 70% reduction). © 2017 American Academy of Neurology Slide 33

Additional Conclusions Please see manuscript for full discussion of conclusions. The evidence is low that the following factors are associated with altering SUDEP risk: • Nocturnal seizures (associated with increased risk) • Any specific AED (none associated specifically with increased risk) • LTG use in women (associated with increased risk) • Never having been treated with an AED (associated with increased risk) • Number of AEDs used overall (associated with increased risk) • Heart rate variability (not associated with increased risk) • Extratemporal epilepsy (associated with increased risk) • Intellectual disability (associated with increased risk) • Male gender (associated with increased risk) • Anxiolytic drug use (associated with increased risk) © 2017 American Academy of Neurology Slide 34

Additional Conclusions Please see manuscript for full discussion of conclusions. The evidence is very low or conflicting that the following factors are associated with altering SUDEP risk: • Overall seizure frequency when evaluated by using all seizure types • Medically refractory epilepsy vs not having well-controlled seizures defined as no seizures for the past year • Monotherapy vs polytherapy • CBZ, PHT, or VPA levels that are above, below, or within the reference range • Psychotropic drug use • Mental health disorders, lung disorders, or alcohol use • LTG use in people with highly refractory epilepsy • Frequent changes in AEDs • Therapeutic drug monitoring © 2017 American Academy of Neurology Slide 35

Additional Conclusions (continued) Please see manuscript for full discussion of conclusions. The evidence is very low or conflicting that the following factors are associated with altering SUDEP risk: • Undergoing a resective epilepsy surgical procedure (although current research does not rule out the possibility of a beneficial effect or, further, the potential effect of epilepsy surgery on reducing GTCS frequency and epilepsy severity on reducing SUDEP risk) • Engel outcome of epilepsy surgery (although current research does not rule out the possibility of a beneficial effect and, further, the potential effect of epilepsy surgery on reducing GTCS frequency and epilepsy severity on reducing SUDEP risk) • VNS use for more than 2 years (however, current research does not rule out the possibility of a beneficial effect and, further, the potential effect of epilepsy surgery on reducing GTCS frequency and epilepsy severity on reducing the risk of SUDEP) © 2017 American Academy of Neurology Slide 36

Additional Conclusions (continued) Please see manuscript for full discussion of conclusions. The evidence is very low or conflicting that the following factors are associated with altering SUDEP risk: • Epilepsy etiology, whether idiopathic or localization related • Structural lesion on MRI • Duration of epilepsy • Age at epilepsy onset • Postictal EEG suppression © 2017 American Academy of Neurology Slide 37

Recommendations: Clinical Question 2 Risk factor of GTCS Level B © 2017 American Academy of Neurology • For persons with epilepsy who continue to experience GTCS, clinicians should continue to actively manage epilepsy therapies to reduce seizure occurrences and the risk of SUDEP while incorporating patient preferences and weighing the risks and benefits of any new approach Slide 38

Recommendations: Clinical Question 2 Risk factor of lack of nocturnal supervision Level C © 2017 American Academy of Neurology • For persons with frequent GTCS and nocturnal seizures, clinicians may advise selected patients and families, if permitted by their individualized epilepsy and psychosocial circumstances, to use nocturnal supervision or other nocturnal precautions, such as the use of a remote listening device, to reduce SUDEP risk Slide 39

Recommendations: Clinical Question 2 Risk factor of uncontrolled epilepsy Level B © 2017 American Academy of Neurology • Clinicians should inform their persons with epilepsy that seizure freedom, particularly freedom from GTCS (which is more likely to occur with medication adherence), is strongly associated with a decreased risk of SUDEP Slide 40

Recommendations for Future Research Systematic methods should be developed to identify and report the incidence of SUDEP in different epilepsy populations in order to obtain a better understanding of the incidence and causes of this devastating condition. Educational efforts are needed to improve the forensic knowledge of SUDEP among professionals such as medical examiners, coroners, and pathologists in order to help determine, and document on death certificates, the etiology in individuals, and in order to improve overall knowledge of this condition. Research to identify preventable risk factors should be supported and encouraged so that future clinical trials will be conducted to reduce SUDEP occurrence. Of particular importance is to better understand (a) the relationship between the nature, severity, and duration of epilepsy and the occurrence of SUDEP, and (b) whether current treatments affect the risk of developing SUDEP. Because of (a) risks identified with frequent GTCS, (b) the fact that one study shows more SUDEP events occur in people in placebo arms of trials, and (c) increased SUDEP risk, serious consideration should be given to avoid assigning people with frequent GTCS to placebo for long periods. © 2017 American Academy of Neurology Slide 41

References cited here can be found in the published practice guideline, available at AAN. com/guidelines. © 2017 American Academy of Neurology Slide 42

Access Practice Guideline and Summary Tools • To access the practice guideline and related summary tools, visit AAN. com/guidelines. • Practice guideline article • Summary for clinicians and summary for patients/families © 2017 American Academy of Neurology Slide 43

Questions? © 2017 American Academy of Neurology
 Asam national practice guideline
Asam national practice guideline Kdigo 2012 clinical practice guideline
Kdigo 2012 clinical practice guideline Hrayr shahinian
Hrayr shahinian American thyroid association guidelines pregnancy 2017
American thyroid association guidelines pregnancy 2017 American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 Waikato stormwater management guideline
Waikato stormwater management guideline Interview guideline template
Interview guideline template Anemia in pregnancy guideline
Anemia in pregnancy guideline Autoanamnesa
Autoanamnesa Patient safety incident definition
Patient safety incident definition Msqh standard
Msqh standard Contoh anamnesa psikologi
Contoh anamnesa psikologi East guideline
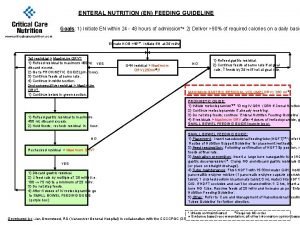
East guideline En feeding guide
En feeding guide Notching hair
Notching hair What is a guideline for hoisting a hoseline?
What is a guideline for hoisting a hoseline? Turnbull direction
Turnbull direction 5 guideline for cumbersome calculations
5 guideline for cumbersome calculations Multiplication rule for 4
Multiplication rule for 4 Who guideline on country pharmaceutical pricing policies
Who guideline on country pharmaceutical pricing policies Outside counsel guidelines
Outside counsel guidelines Canadian chiropractic guideline initiative
Canadian chiropractic guideline initiative Chronic pancreatitis guideline
Chronic pancreatitis guideline Bpfk cosmetic guideline
Bpfk cosmetic guideline Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Disconnected epidural catheter guideline
Disconnected epidural catheter guideline Escardio
Escardio Asean stability guideline
Asean stability guideline Srm process flow
Srm process flow Fmea guideline
Fmea guideline 2017 apush exam
2017 apush exam 2017 ap chemistry practice exam
2017 ap chemistry practice exam 2017 asco oncology practice conference
2017 asco oncology practice conference American academy of financial management
American academy of financial management American academy of private physicians
American academy of private physicians African american beauty academy
African american beauty academy American academy of oral and maxillofacial radiology
American academy of oral and maxillofacial radiology American academy of witchcraft arts
American academy of witchcraft arts American academy of physical medicine and rehabilitation
American academy of physical medicine and rehabilitation American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Motor strength scale
Motor strength scale Dr kirk kleinfeld
Dr kirk kleinfeld Mayzent fdo
Mayzent fdo Mary bridge pediatric neurology
Mary bridge pediatric neurology Neurology sonography
Neurology sonography