Zero Suicide Concept and Challenges Oscar Donnelly NHSCT




- Slides: 29
Zero Suicide – Concept and Challenges Oscar Donnelly NHSCT Professor Siobhan O’Neill UU
l Suicide - Worldwide Every 40 secs. a person dies by Suicide 800 k die due to suicide each year l Second leading cause of death in 15 -29 yrs old l In the UK, suicide is the leading cause of death among woman under 35 and men under 50 l 2% of the global burden of disease ‘Health Care Services need to incorporate suicide prevention as a core component’ WHO 2014 l
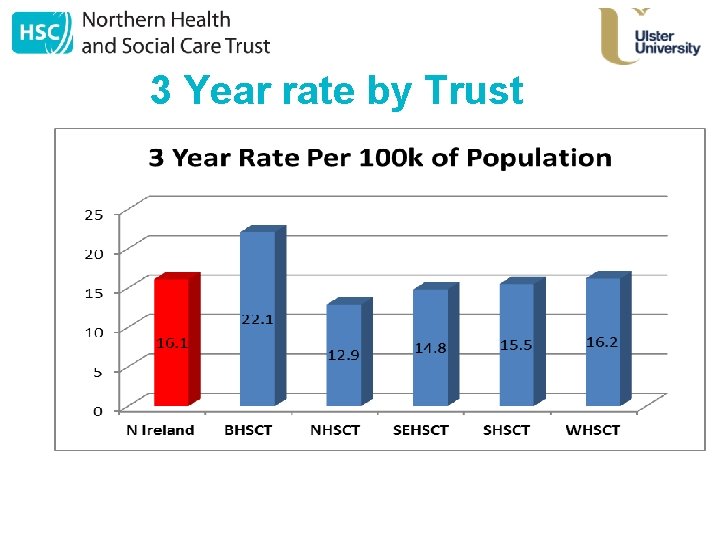
Suicide – N Ireland • • • 2015 – 318 Deaths Registered N Ireland has the highest rate in these islands Single biggest cause of death in the under 40 s Higher mortality due to suicide (0. 4 years) is the largest contributor to the NI-England male life expectancy gap (1. 1 years). NI has Rate 16. 1 per 100, 000 2013/15 (up from 15. 5) Approx 70% not known to mental health services
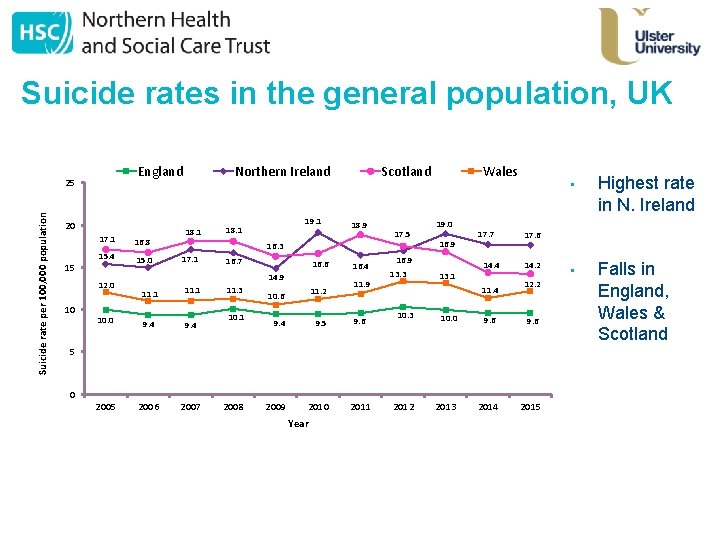
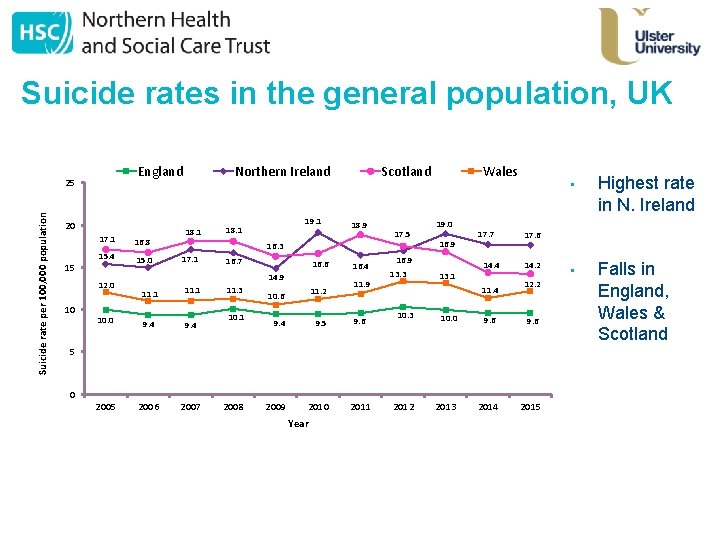
Suicide rates in the general population, UK England Suicide rate per 100, 000 population 25 20 15 17. 1 16. 8 15. 4 15. 0 12. 0 10 Northern Ireland 18. 1 19. 1 18. 1 Scotland 18. 9 17. 5 16. 3 17. 1 16. 7 16. 6 14. 9 11. 1 10. 0 9. 4 2005 2006 2007 11. 3 10. 1 11. 2 10. 6 9. 4 9. 5 2009 2010 16. 4 11. 9 9. 6 Wales 19. 0 16. 9 13. 3 13. 1 17. 7 14. 4 11. 4 10. 3 10. 0 2008 Year 2011 2012 2013 Highest rate in N. Ireland • Falls in England, Wales & Scotland 17. 6 14. 2 12. 2 9. 6 2014 2015 5 0 •
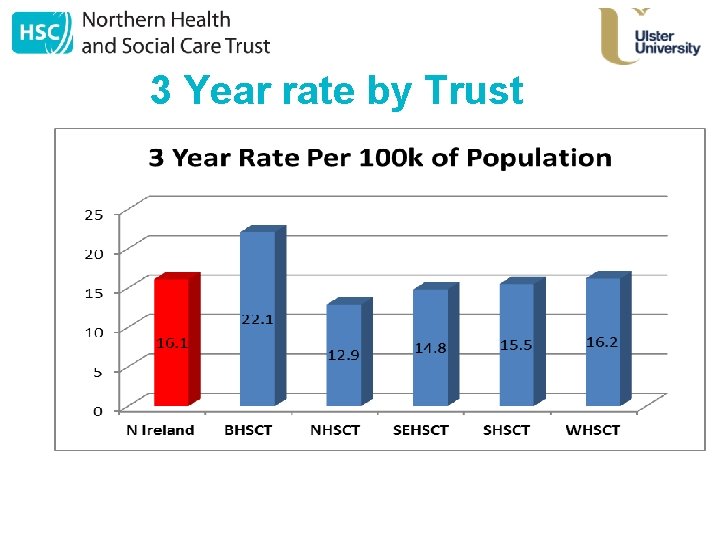
3 Year rate by Trust
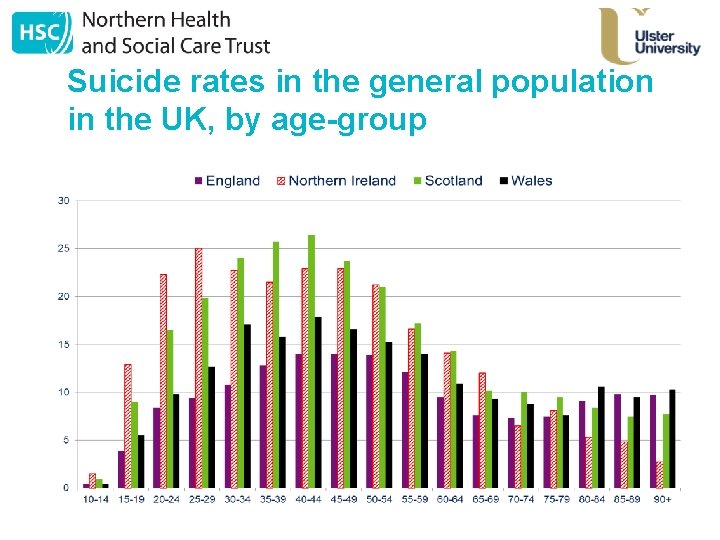
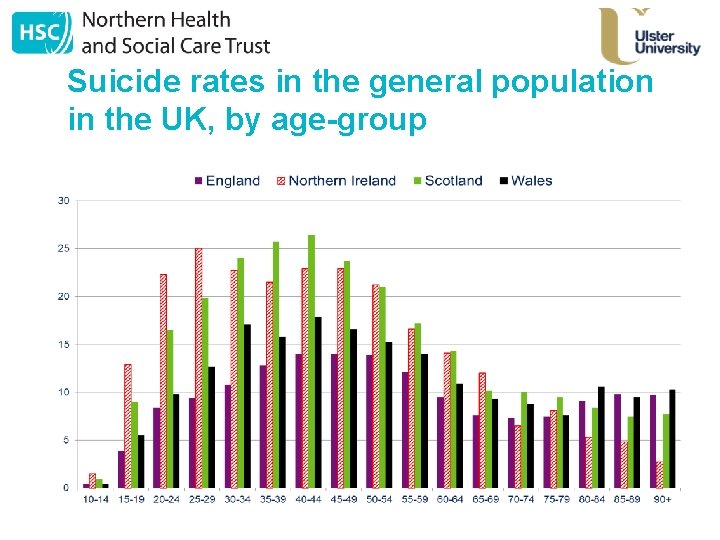
Suicide rates in the general population in the UK, by age-group
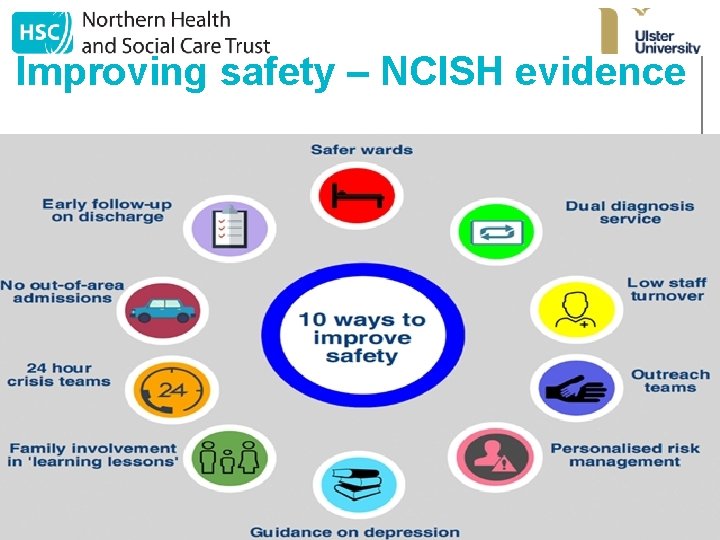
Improving safety – NCISH evidence
What is Zero Suicide • • An approach A concept A toolkit A target Zero Suicide is a commitment to suicide prevention in health and behavioural health care systems, and also a specific set of tools and strategies. It is both a concept and a practice. Fundamental question: Is suicide preventable?
What is Zero Suicide? l l l A priority of the National Action Alliance for Suicide Prevention A goal of the National Strategy for Suicide Prevention A project of the Suicide Prevention Resource Center A framework for systematic, clinical suicide prevention in behavioral health and health care systems A focus on safety and error reduction in healthcare A set of best practices and tools for health systems and providers
The case for Zero Suicide in healthcare systems • • Many of those who have died by suicide have been in contact with health services. Suicidal individuals often fall through multiple cracks in a fragmented health care system. Systematic approach to quality improvement. Builds on work done in the Henry Ford Health System (HFHS) in Michigan. HFHS applied a rigorous quality improvement process to problems such as inpatient falls and medication errors. Perfect Depression Care A comprehensive approach that includes suicide prevention as an explicit goal. The approach incorporates both best and promising practices in quality improvement and evidence-based care. Demonstrated an 80% reduction in the suicide rate among health plan members.
Elements of Suicide Prevention in health care systems Clinical Care and Intervention Task Force of the National Action Alliance for Suicide Prevention • LEAD: Create a leadership-driven, safety-oriented culture committed to dramatically reducing suicide among people under care. Include suicide attempt and loss survivors in leadership and planning roles. • TRAIN: Workforce development and training. Develop a competent, confident, and caring workforce. • IDENTIFY: Systematically identify and assess suicide risk. Standardized screening and risk assessment.
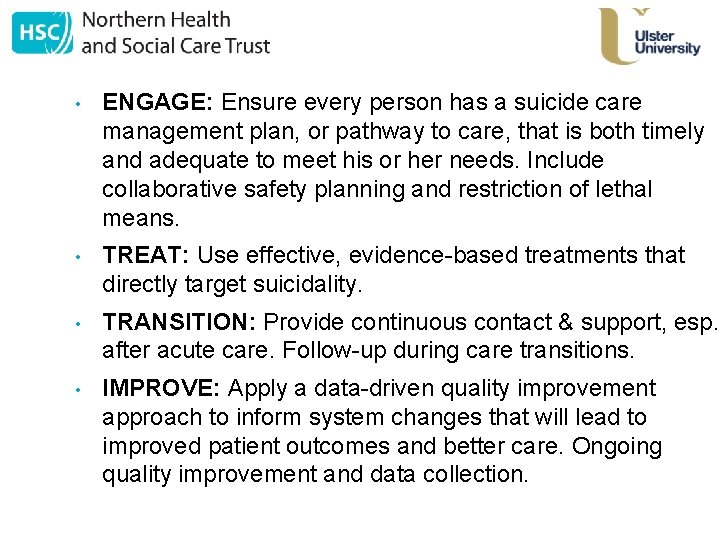
• ENGAGE: Ensure every person has a suicide care management plan, or pathway to care, that is both timely and adequate to meet his or her needs. Include collaborative safety planning and restriction of lethal means. • TREAT: Use effective, evidence-based treatments that directly target suicidality. • TRANSITION: Provide continuous contact & support, esp. after acute care. Follow-up during care transitions. • IMPROVE: Apply a data-driven quality improvement approach to inform system changes that will lead to improved patient outcomes and better care. Ongoing quality improvement and data collection.
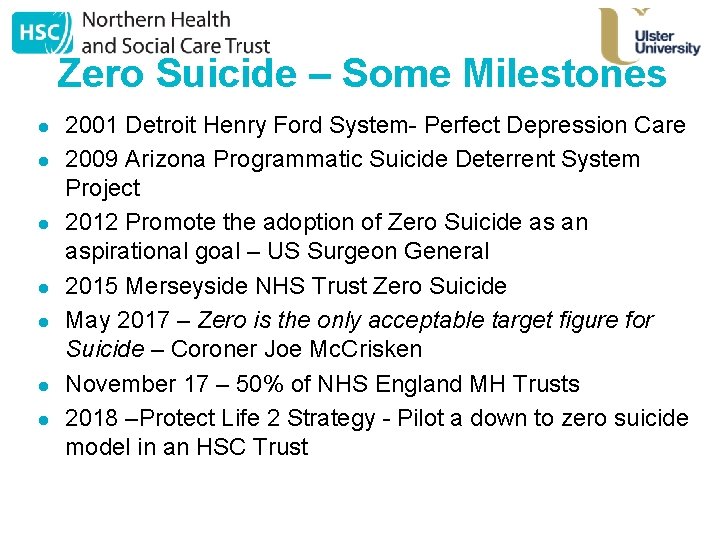
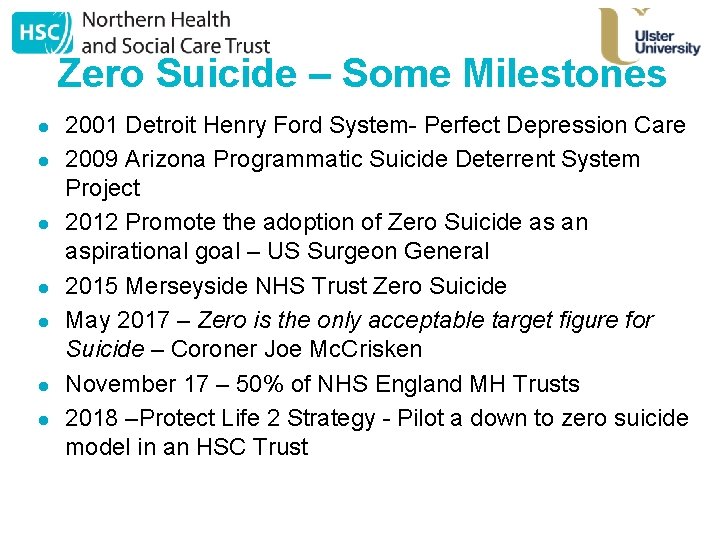
Zero Suicide – Some Milestones l l l l 2001 Detroit Henry Ford System- Perfect Depression Care 2009 Arizona Programmatic Suicide Deterrent System Project 2012 Promote the adoption of Zero Suicide as an aspirational goal – US Surgeon General 2015 Merseyside NHS Trust Zero Suicide May 2017 – Zero is the only acceptable target figure for Suicide – Coroner Joe Mc. Crisken November 17 – 50% of NHS England MH Trusts 2018 –Protect Life 2 Strategy - Pilot a down to zero suicide model in an HSC Trust
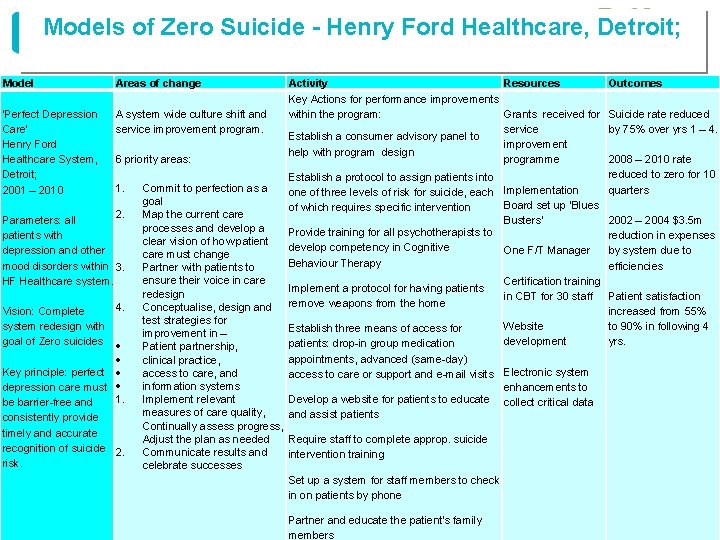
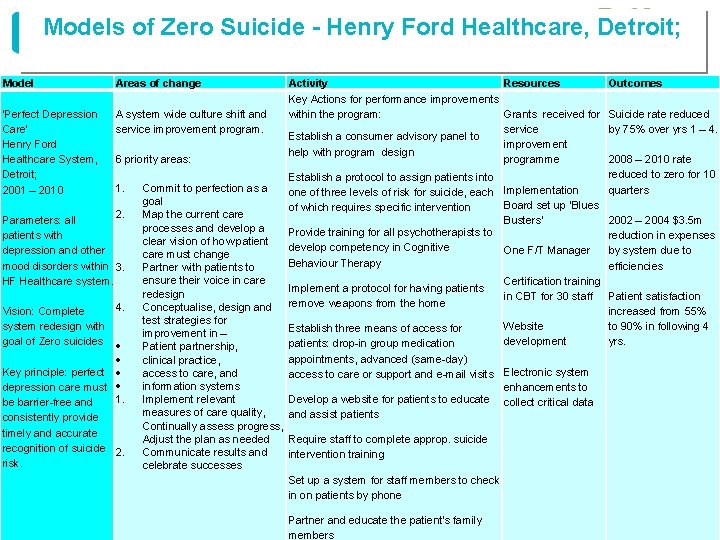
Models of Zero Suicide - Henry Ford Healthcare, Detroit; Model Areas of change Activity Resources Key Actions for performance improvements ‘Perfect Depression A system wide culture shift and within the program: Grants received for Care’ service improvement program. service Establish a consumer advisory panel to Henry Ford improvement help with program design Healthcare System, 6 priority areas: programme Detroit; Establish a protocol to assign patients into 1. Commit to perfection as a 2001 – 2010 one of three levels of risk for suicide, each Implementation goal Board set up ‘Blues of which requires specific intervention 2. Map the current care Parameters: all Busters’ processes and develop a Provide training for all psychotherapists to patients with clear vision of how patient develop competency in Cognitive depression and other One F/T Manager care must change Behaviour Therapy mood disorders within 3. Partner with patients to ensure their voice in care HF Healthcare system. Certification training Implement a protocol for having patients redesign in CBT for 30 staff remove weapons from the home 4. Conceptualise, design and Vision: Complete test strategies for system redesign with Website Establish three means of access for improvement in – goal of Zero suicides development patients: drop-in group medication Patient partnership, appointments, advanced (same-day) clinical practice, Key principle: perfect access to care, and access to care or support and e-mail visits Electronic system information systems depression care must enhancements to Develop a website for patients to educate 1. Implement relevant be barrier-free and collect critical data measures of care quality, and assist patients consistently provide Continually assess progress, timely and accurate Adjust the plan as needed Require staff to complete approp. suicide recognition of suicide 2. Communicate results and intervention training risk. celebrate successes Set up a system for staff members to check in on patients by phone Partner and educate the patient's family members Outcomes Suicide rate reduced by 75% over yrs 1 – 4. 2008 – 2010 rate reduced to zero for 10 quarters 2002 – 2004 $3. 5 m reduction in expenses by system due to efficiencies Patient satisfaction increased from 55% to 90% in following 4 yrs.
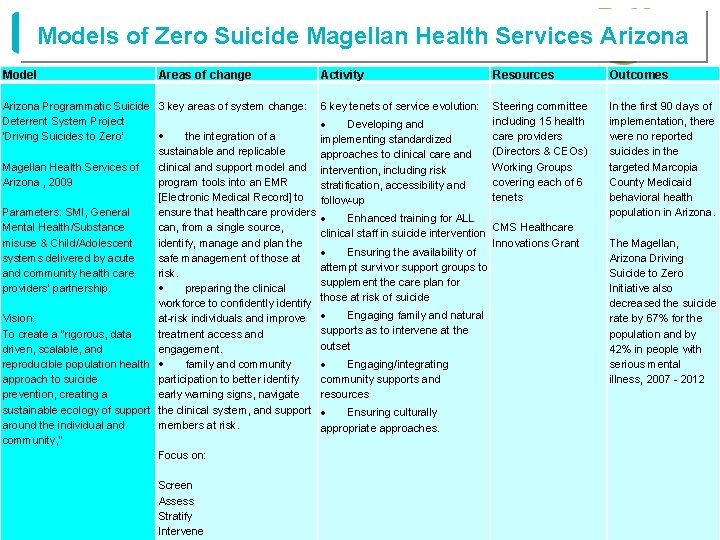
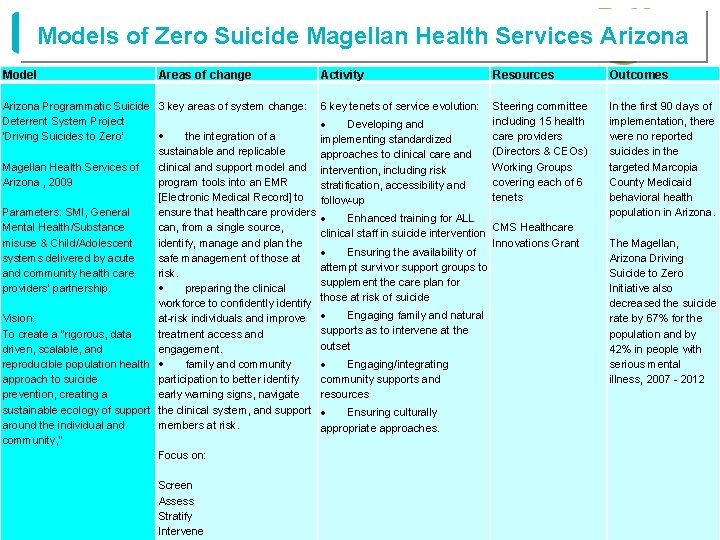
Models of Zero Suicide Magellan Health Services Arizona Model Areas of change Activity Resources Arizona Programmatic Suicide Deterrent System Project ‘Driving Suicides to Zero’ Magellan Health Services of Arizona , 2009 Parameters: SMI, General Mental Health/Substance misuse & Child/Adolescent systems delivered by acute and community health care providers’ partnership. Vision: To create a "rigorous, data driven, scalable, and reproducible population health approach to suicide prevention, creating a sustainable ecology of support around the individual and community, " 3 key areas of system change: 6 key tenets of service evolution: Steering committee including 15 health Developing and the integration of a care providers implementing standardized sustainable and replicable (Directors & CEOs) approaches to clinical care and clinical and support model and intervention, including risk Working Groups program tools into an EMR covering each of 6 stratification, accessibility and [Electronic Medical Record] to follow-up tenets ensure that healthcare providers Enhanced training for ALL can, from a single source, CMS Healthcare clinical staff in suicide intervention identify, manage and plan the Innovations Grant Ensuring the availability of safe management of those at attempt survivor support groups to risk. supplement the care plan for preparing the clinical those at risk of suicide workforce to confidently identify Engaging family and natural at-risk individuals and improve supports as to intervene at the treatment access and outset engagement. Engaging/integrating family and community supports and participation to better identify resources early warning signs, navigate the clinical system, and support Ensuring culturally members at risk. appropriate approaches. Focus on: Screen Assess Stratify Intervene Outcomes In the first 90 days of implementation, there were no reported suicides in the targeted Marcopia County Medicaid behavioral health population in Arizona. The Magellan, Arizona Driving Suicide to Zero Initiative also decreased the suicide rate by 67% for the population and by 42% in people with serious mental illness, 2007 - 2012
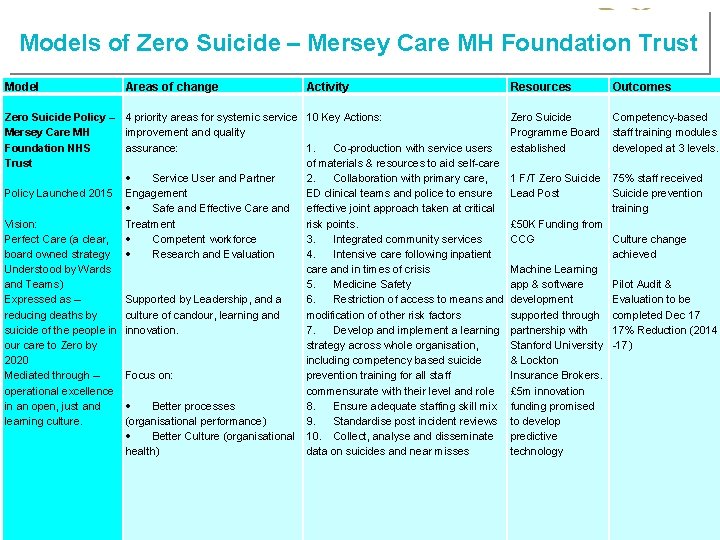
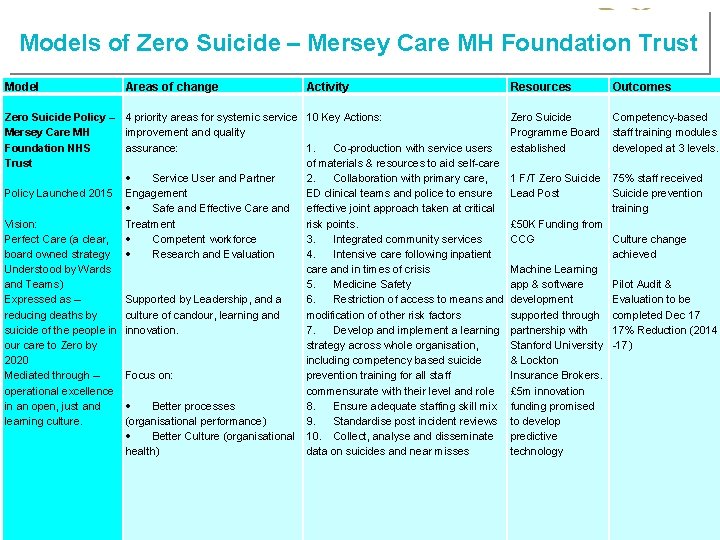
Models of Zero Suicide – Mersey Care MH Foundation Trust Model Areas of change Activity Resources Zero Suicide Policy – Mersey Care MH Foundation NHS Trust Policy Launched 2015 Vision: Perfect Care (a clear, board owned strategy Understood by Wards and Teams) Expressed as – reducing deaths by suicide of the people in our care to Zero by 2020 Mediated through – operational excellence in an open, just and learning culture. 4 priority areas for systemic service improvement and quality assurance: Service User and Partner Engagement Safe and Effective Care and Treatment Competent workforce Research and Evaluation Supported by Leadership, and a culture of candour, learning and innovation. Focus on: Better processes (organisational performance) Better Culture (organisational health) 10 Key Actions: Zero Suicide Programme Board 1. Co-production with service users established of materials & resources to aid self-care 2. Collaboration with primary care, 1 F/T Zero Suicide ED clinical teams and police to ensure Lead Post effective joint approach taken at critical risk points. £ 50 K Funding from 3. Integrated community services CCG 4. Intensive care following inpatient care and in times of crisis Machine Learning 5. Medicine Safety app & software 6. Restriction of access to means and development modification of other risk factors supported through 7. Develop and implement a learning partnership with strategy across whole organisation, Stanford University including competency based suicide & Lockton prevention training for all staff Insurance Brokers. commensurate with their level and role £ 5 m innovation 8. Ensure adequate staffing skill mix funding promised 9. Standardise post incident reviews to develop 10. Collect, analyse and disseminate predictive data on suicides and near misses technology Outcomes Competency-based staff training modules developed at 3 levels. 75% staff received Suicide prevention training Culture change achieved Pilot Audit & Evaluation to be completed Dec 17 17% Reduction (2014 -17)
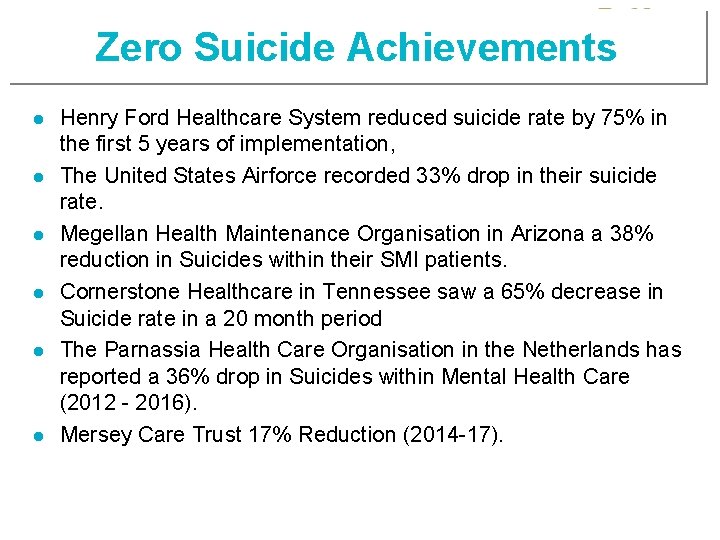
Zero Suicide Achievements l l l Henry Ford Healthcare System reduced suicide rate by 75% in the first 5 years of implementation, The United States Airforce recorded 33% drop in their suicide rate. Megellan Health Maintenance Organisation in Arizona a 38% reduction in Suicides within their SMI patients. Cornerstone Healthcare in Tennessee saw a 65% decrease in Suicide rate in a 20 month period The Parnassia Health Care Organisation in the Netherlands has reported a 36% drop in Suicides within Mental Health Care (2012 - 2016). Mersey Care Trust 17% Reduction (2014 -17).
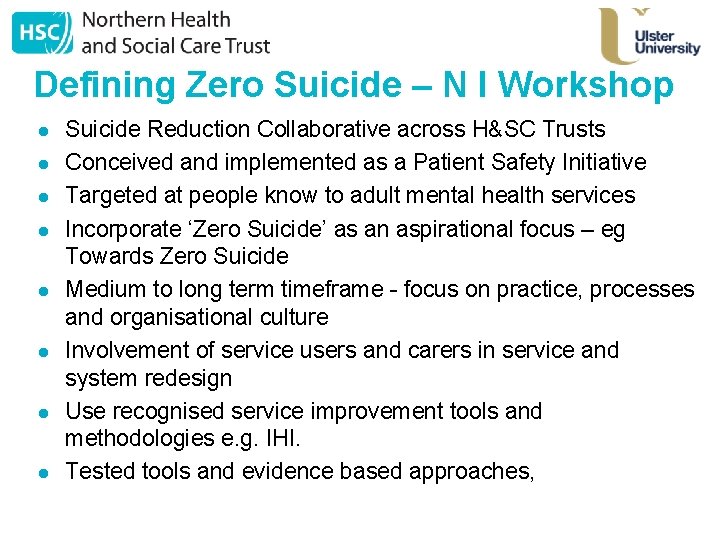
Defining Zero Suicide – N I Workshop l l l l Suicide Reduction Collaborative across H&SC Trusts Conceived and implemented as a Patient Safety Initiative Targeted at people know to adult mental health services Incorporate ‘Zero Suicide’ as an aspirational focus – eg Towards Zero Suicide Medium to long term timeframe - focus on practice, processes and organisational culture Involvement of service users and carers in service and system redesign Use recognised service improvement tools and methodologies e. g. IHI. Tested tools and evidence based approaches,
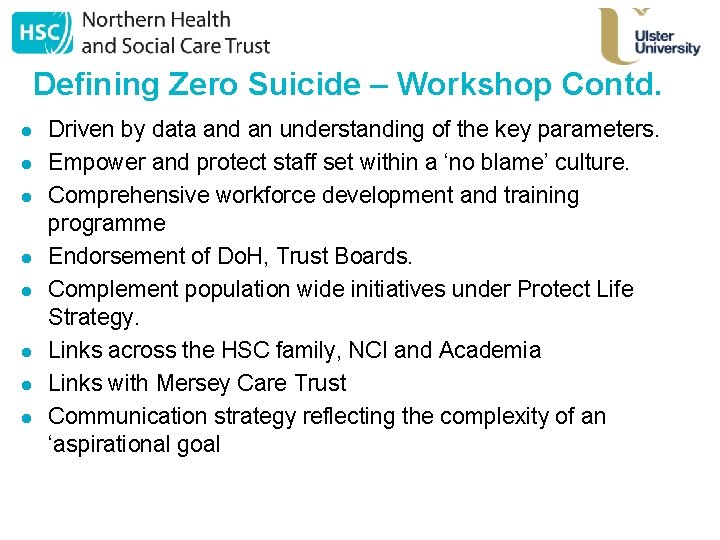
Defining Zero Suicide – Workshop Contd. l l l l Driven by data and an understanding of the key parameters. Empower and protect staff set within a ‘no blame’ culture. Comprehensive workforce development and training programme Endorsement of Do. H, Trust Boards. Complement population wide initiatives under Protect Life Strategy. Links across the HSC family, NCI and Academia Links with Mersey Care Trust Communication strategy reflecting the complexity of an ‘aspirational goal
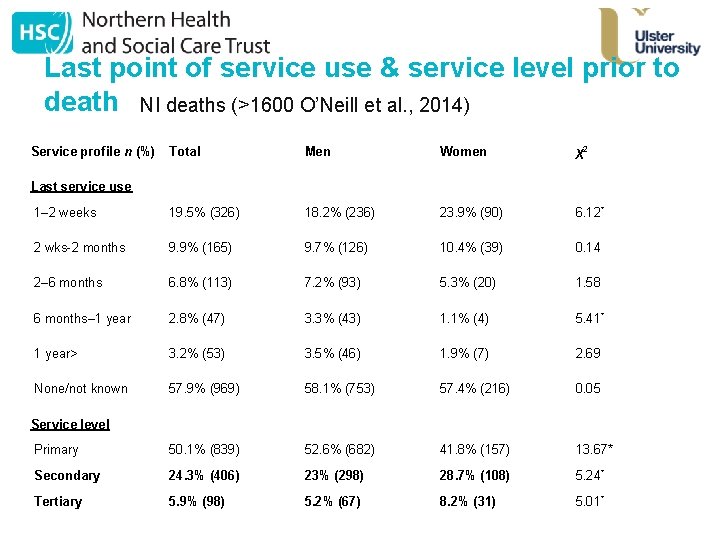
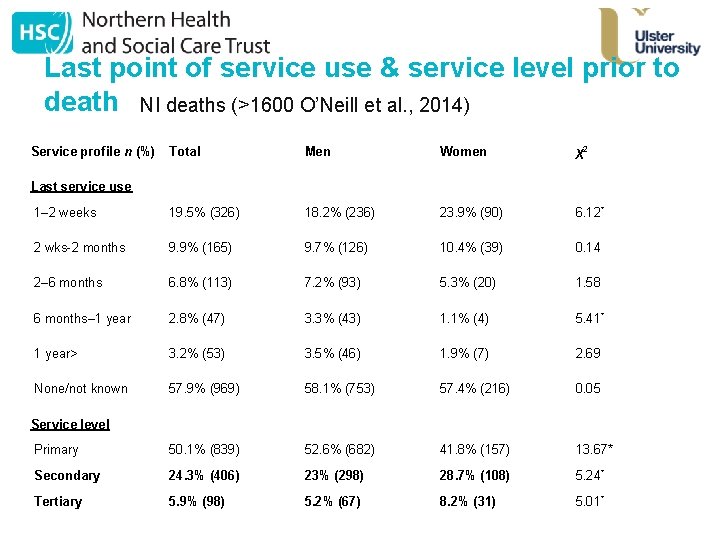
Last point of service use & service level prior to death NI deaths (>1600 O’Neill et al. , 2014) Service profile n (%) Total Men Women χ2 1– 2 weeks 19. 5% (326) 18. 2% (236) 23. 9% (90) 6. 12* 2 wks-2 months 9. 9% (165) 9. 7% (126) 10. 4% (39) 0. 14 2– 6 months 6. 8% (113) 7. 2% (93) 5. 3% (20) 1. 58 6 months– 1 year 2. 8% (47) 3. 3% (43) 1. 1% (4) 5. 41* 1 year> 3. 2% (53) 3. 5% (46) 1. 9% (7) 2. 69 None/not known 57. 9% (969) 58. 1% (753) 57. 4% (216) 0. 05 Primary 50. 1% (839) 52. 6% (682) 41. 8% (157) 13. 67* Secondary 24. 3% (406) 23% (298) 28. 7% (108) 5. 24* Tertiary 5. 9% (98) 5. 2% (67) 8. 2% (31) 5. 01* Last service use Service level

John Magowan, blogs. canterbury. ac. uk
Some critiques of ZS • • • Is suicide preventable? Risk averse practices? What is the goal of mental health care? Unintended consequences Impact on staff Piecemeal approach The importance of leadership Continuity of care and pathways between services Do the interventions that make up ZS work?
Do the interventions that make up the elements of Zero Suicide work? • • Covington (2017) “They all have research-based efficacy. Erlangsen’s 2015 Lancet study showed a lower risk of deliberate self-harm and general mortality for those who received psychosocial therapy. Direct treatment of suicide is more effective and cost-efficient than statins are for heart disease. Findings are similar for routine screening for suicide risk. In 2015, Dr. Greg Simon and team concluded in Psychiatric Services that the PHQ-9 question 9 “identifies outpatients at increased risk for suicide attempt or death. ” with an accuracy about twice as predictive of future suicide as cholesterol scores are of future heart attack death. While there are few studies of safety planning, Craig Bryan’s findings in The Journal of Affective Disorders is promising. Logic and the literature base on quality improvement suggest that we need a systematic, leadership-driven quality improvement approach for a wicked and complex problem like suicide. As a scientific matter, we need more data. As a public health and quality of care matter, the evidence is already in. ”


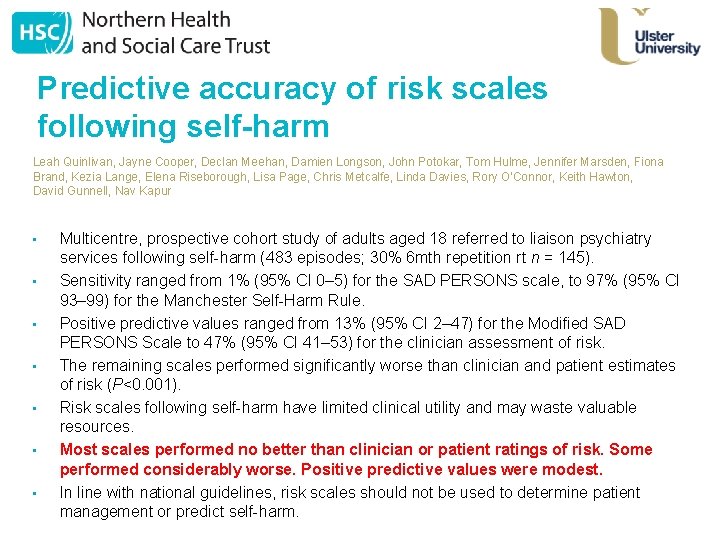
Predictive accuracy of risk scales following self-harm Leah Quinlivan, Jayne Cooper, Declan Meehan, Damien Longson, John Potokar, Tom Hulme, Jennifer Marsden, Fiona Brand, Kezia Lange, Elena Riseborough, Lisa Page, Chris Metcalfe, Linda Davies, Rory O'Connor, Keith Hawton, David Gunnell, Nav Kapur • • Multicentre, prospective cohort study of adults aged 18 referred to liaison psychiatry services following self-harm (483 episodes; 30% 6 mth repetition rt n = 145). Sensitivity ranged from 1% (95% CI 0– 5) for the SAD PERSONS scale, to 97% (95% CI 93– 99) for the Manchester Self-Harm Rule. Positive predictive values ranged from 13% (95% CI 2– 47) for the Modified SAD PERSONS Scale to 47% (95% CI 41– 53) for the clinician assessment of risk. The remaining scales performed significantly worse than clinician and patient estimates of risk (P<0. 001). Risk scales following self-harm have limited clinical utility and may waste valuable resources. Most scales performed no better than clinician or patient ratings of risk. Some performed considerably worse. Positive predictive values were modest. In line with national guidelines, risk scales should not be used to determine patient management or predict self-harm.

“It is critically important to design for zero even when it may not be theoretically possible…It’s about purposefully aiming for a higher level of performance. ” Thomas Priselac President and CEO of Cedars-Sinai Medical Center
Zero Suicide – Concept and Challenges Oscar Donnelly NHSCT Professor Siobhan O’Neill UU