Assessing Suicide Risk Jennifer Warner MA NCC Resources













- Slides: 66
Assessing Suicide Risk Jennifer Warner, MA, NCC Resources for Human Development

Welcome and Introductions

Demographics and Statistics “After cancer and heart disease, suicide accounts for more years of life lost than any other cause of death. ”* *Understanding suicide facts and figures; http: //www. afsp. org
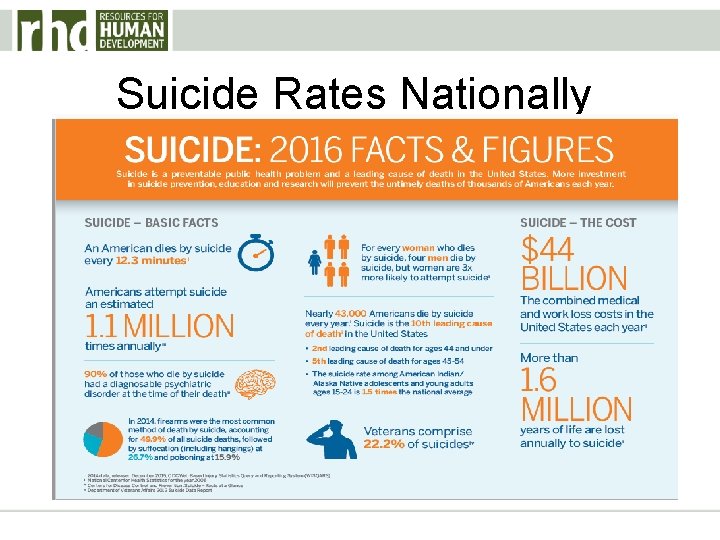
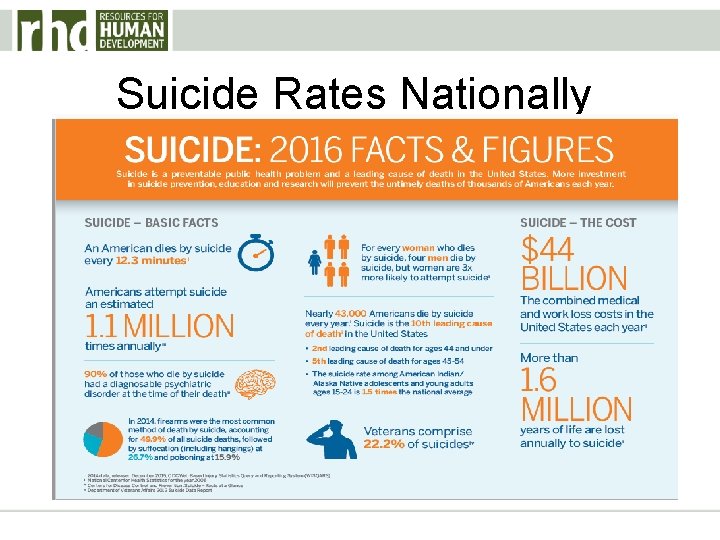
Suicide Rates Nationally

• Suicide was the tenth leading cause of death overall in the United States, claiming the lives of more than 44, 000 people. • Suicide was the third leading cause of death among individuals between the ages of 10 and 14, and the second leading cause of death among individuals between the ages of 15 and 34. • There were more than twice as many suicides (44, 193) in the United States as there were homicides (17, 793). • Centers for Disease Control and Prevention (CDC), 2015
• More people die annually by suicide than by automobile accidents. • The annual suicide rate in the United States has been increasing over the past decade. • Now, a majority of the suicides by Americans occurred among both men and women between the ages of 45 and 54. * *SAMHSA. gov


• Every day, approximately 105 Americans die by suicide. * • There is 1 suicide for every estimated 25 attempts. * • There is 1 suicide for every estimated 4 suicide attempts in the elderly. * *CDC – Center for Disease Control, WHO - World Health Organization, AAS – American Association of Suicidology, NAMI- National Alliance on Mental Illness, NIMH – National Institute of Mental Health, SMH – Screening for Mental Health
Suicide rates in Pennsylvania
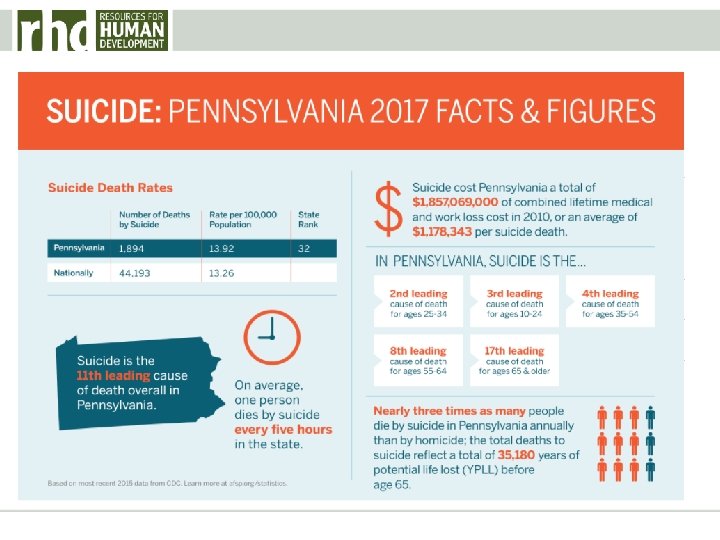
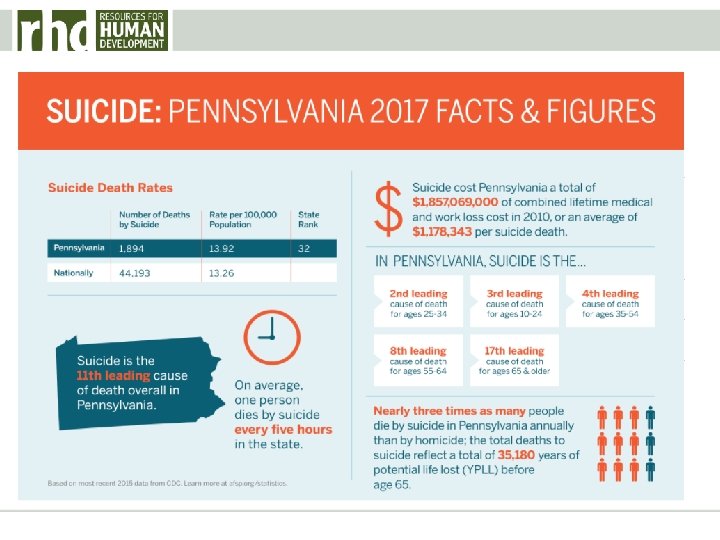
Year Pennsylvania 2012 12. 5 2013 12. 2 2014 12. 6 • Number of deaths due to intentional self-harm per 100, 000 population.
• Pennsylvania is currently ranked 13 th in the nation with an average of 13. 26 deaths per 100, 000 residents annually. (An increase from 12. 0 in 2013)* • This number ranks Pennsylvania with Iowa, Michigan, and Wisconsin. *http: //www. americashealthrankings. org/PA/Suicide
Understanding Suicidality
Suicidality • Suicidal ideation and suicide-related behaviors including completed suicide.
What is Ideation vs. Plan vs. Intent? • Suicidal Ideation – Any self-reported thoughts of engaging in suicide-related behavior. • Suicidal Plan – An individual or personalized strategy inclusive of time frame and means to complete suicide. • Suicidal Intent – The aim, purpose, or goal of self-killing as one’s purpose.
Suicide-related behaviors include: • Completed suicide: self-inflicted behavior with intention to die • Suicidal attempts: self-inflicted potentially harmful behavior without fatal issue but with intention to die • Self-harm: deliberate self-inflicted and potentially harmful acts regardless of motive
What Factors Contribute to Suicide Risk?
• • Age Mental Health and/or Substance Use Disorders Family history Trauma (physical, emotional, mental, psychological) • Biopsychosocial factors (Family, Medical, Bullying, etc. ) • Prior attempts • Impulsivity
Age • Suicide risk increases rapidly during adolescence and young adulthood and stabilizes in early midlife • Greatest risk for suicide attempts is in adolescence and early adulthood • Females tend to have more frequent suicide attempts but males tend to outnumber females in completed suicide (14. 2 in males and 12. 0 in females per 100, 000) between 15 -24 year olds
Mental Health vs. Drug and Alcohol Issues • Most people who die by suicide have an undiagnosed, untreated, or undertreated mental health and/or substance use disorder. • 30 – 70% of suicide victims suffer from Major Depression or Bipolar Disorder.
• 2 -15% of persons who have been diagnosed with major depression die by suicide. * • An estimated 3 -20% of persons who have been diagnosed with Bipolar Disorder die by suicide. * • An estimated 6 -15% of persons diagnosed with Schizophrenia die by suicide. * *http: //depts. washington. edu/mhreport/facts_suicide. php

Suicide is the leading cause of premature death in those diagnosed with Schizophrenia and between 7595% of those individuals are male.
• Individuals with Personality Disorders are approximately three times as likely to die by suicide than those without. • 25 – 50% of these individuals also have a substance use or Major Depressive disorder. * *http: //depts. washington. edu/mhreport/facts_suicide. php
• Substance abuse is another factor in suicide and may account for over half of all cases reported. * • About 20% of suicides involve people with alcohol problems. • The lifetime rate of suicide among people with alcohol-use disorders is at least 3 -4 times the average. * *http: //www. mentalhealthamerica. net/suicide
• Completed suicides are more likely to be men over 45 who have experienced depression or alcohol abuse. • Alcohol and drug abuse are second only to depression and other mood disorders as the most frequent risk factors for suicide. * • Those with substance abuse disorders are six times more likely to complete suicide than those without. *http: //www. samhsa. gov/suicide-prevention
• The rate of completed suicide among men with substance abuse issues is 2 -3 times higher than among those without. * • Women with substance abuse issues are at 6 -9 times higher risk of suicide compared to women who do not have issues. * *http: //www. mentalhealthamerica. net/suicide

Family History • Family history of suicide can contribute to a person’s vulnerability or resiliency to suicide. • Research has shown that the risk for suicide can be inherited (Juel. Nielsen & Videbech, 1970; Roy, et al. , 1991; Lester, 2002). • Identical twins have been found to have a higher correlation for suicide than fraternal twins • Exposure to completed and attempted suicide in the family has also been found to increase suicide risk among family members
Trauma can result from any of the following: • Disasters (fires, earthquakes, floods, hurricanes, etc. ) • Victimization and severe psychological abuse • Physical assault and/or bodily injury • Surgery • Serious accidents • Exposure to fatalities (homicide, suicide) • Devastating interpersonal losses

The effects of trauma may include: • • • Anxiety Depression Hopelessness/despair/helplessness Anger/hostility Social isolation Impulsiveness Alcohol/Substance abuse Shame/guilt/lessened self-esteem Feelings of distrust or feeling threatened Loss of personal beliefs

• A significant number of individuals who attempt suicide have a background of some kind of trauma. • It may make those affected feel less connected or that they are a burden to their families and friends. • This may generate feelings of hopelessness and depression which may produce a desire to die.
Trauma survivors with an increased risk of suicide include: • Those who self-injure, make non-fatal attempts or frequent threats of suicide • Veterans and members of the military • Physicians • Emergency responders • Sexual assault survivors • Individuals with a brain injury • Physically/developmentally disabled persons
Biopsychosocial Factors • Brain studies of people who have died by suicide have shown a number of visible differences compared to those who died from other causes (Mann & Currier, 2012). • Suicide Contagion – the imitative behavior of suicide. Media coverage of suicide is connected to the increase, or decrease, in subsequent suicides, particularly among adolescents (Sisask & Varnik, 2012). • Internet is also a concern due to its worldwide reach and ability to communicate information about notorious and celebrity suicides.

Medical Conditions and Pain • Individuals with serious medical conditions such as cancer, HIV, Lupus, and traumatic brain injury may be at an increased risk for suicide. • Chronic pain, insomnia, and adverse reactions to medications may also be contributing factors.
Bullying Most likely to precipitate suicidal thinking and suicide attempts in youth who are already depressed, or who have prolonged involvement as both victims and bullies.
Prior Attempts • 20% of people who die by suicide have had a prior attempt. • Suicide risk increases during the days/weeks following a hospitalization for a suicide attempt. • 7 -10% of individuals who have at least 1 attempted suicide previously die by suicide within the next decade
Impulsivity • Impulsivity is highlighted for its role in facilitating suicidal actions in those individuals with suicidal ideation. • Impulsivity make individuals more likely to act on suicidal feelings. • Impulsivity may also be more of a significant indicator of suicide attempt than the presence of a specific suicidal plan.
• Impulsivity has been adopted as a risk factor and warning sign for suicide. • The amount of suicide attempts estimated to be impulsive has ranged from a low of 20% to a high of 85%. • Impulsivity can be both a chronic and acute suicide risk.
Assessing Suicide Risk in the Mental Health/Substance Abuse Population
Assessing Suicide • “Suicidal Assessments should be conducted at first contact, with any subsequent suicidal behavior, increased ideation, or pertinent clinical change; for inpatients, prior to increasing privileges and at discharge. ”* *Substance Abuse and Mental Health Services Administration SAFE-T guidelines; http: //www. samhsa. gov
What do I do if I think someone may be suicidal? 1. Ask • Ask the person directly if he/she is having suicidal thoughts/ideas, a plan to act on those thoughts/ideas, and has access to ANY lethal means.
• You should ask questions like: – “Are you thinking about killing yourself? ” – “Have you ever tried to hurt yourself before? ” – “Do you think you may try to hurt yourself today? ” – “Have you thought about ways in which to hurt yourself? ” – “Do you have access to any pills, substances, or anything which may be considered a weapon? ”
2. Listen and Look • Listen and look for red flags for suicidal behavior by identifying risk factors present and/or using one of the following mnemonic devices:
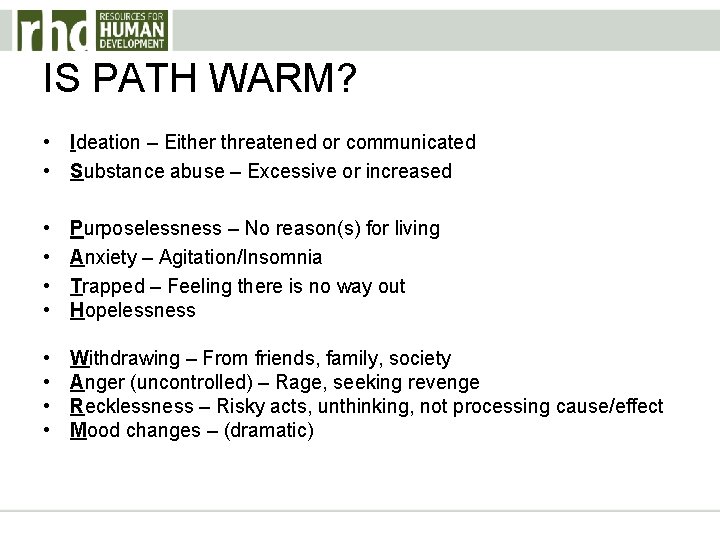
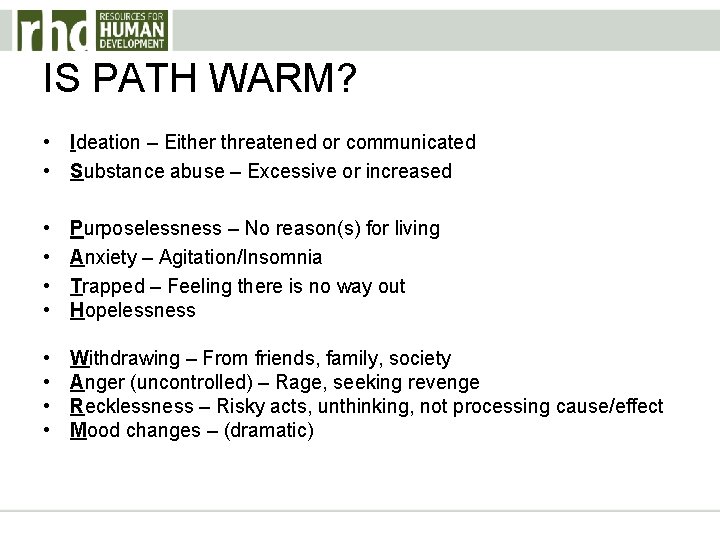
IS PATH WARM? • Ideation – Either threatened or communicated • Substance abuse – Excessive or increased • • Purposelessness – No reason(s) for living Anxiety – Agitation/Insomnia Trapped – Feeling there is no way out Hopelessness • • Withdrawing – From friends, family, society Anger (uncontrolled) – Rage, seeking revenge Recklessness – Risky acts, unthinking, not processing cause/effect Mood changes – (dramatic)
SAFE-T • Suicide Assessment Five-step Evaluation Tool • Draws upon the American Psychiatric Association Practice Guidelines for the Assessment and Treatment of Patients with Suicidal Behaviors.
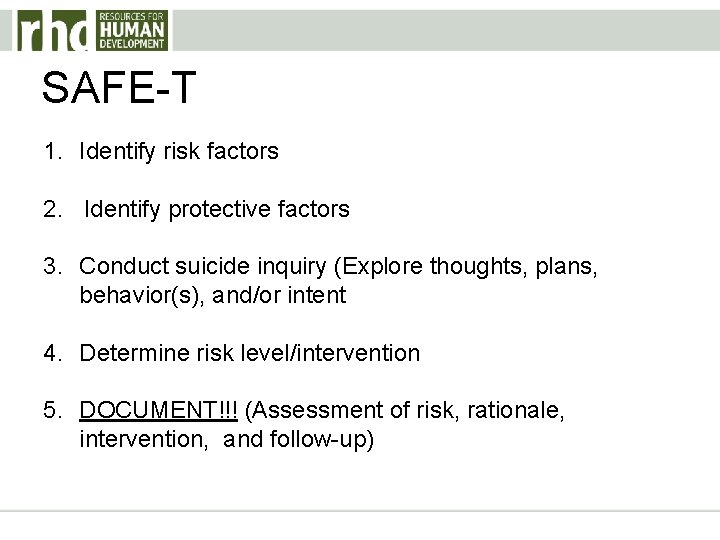
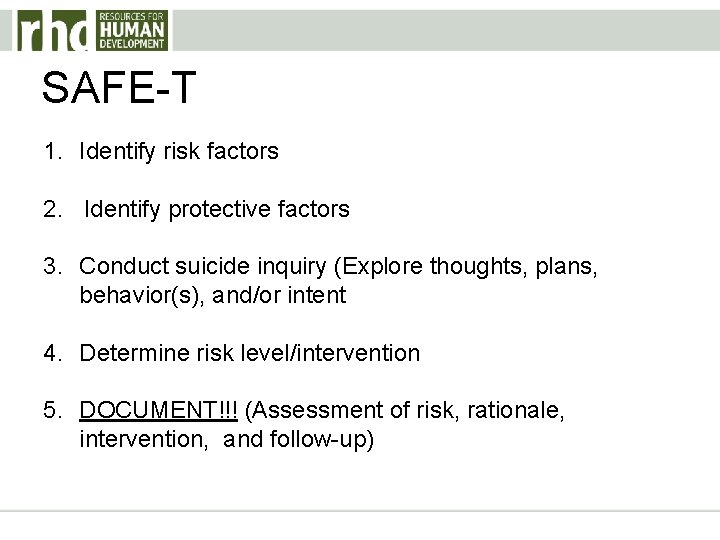
SAFE-T 1. Identify risk factors 2. Identify protective factors 3. Conduct suicide inquiry (Explore thoughts, plans, behavior(s), and/or intent 4. Determine risk level/intervention 5. DOCUMENT!!! (Assessment of risk, rationale, intervention, and follow-up)
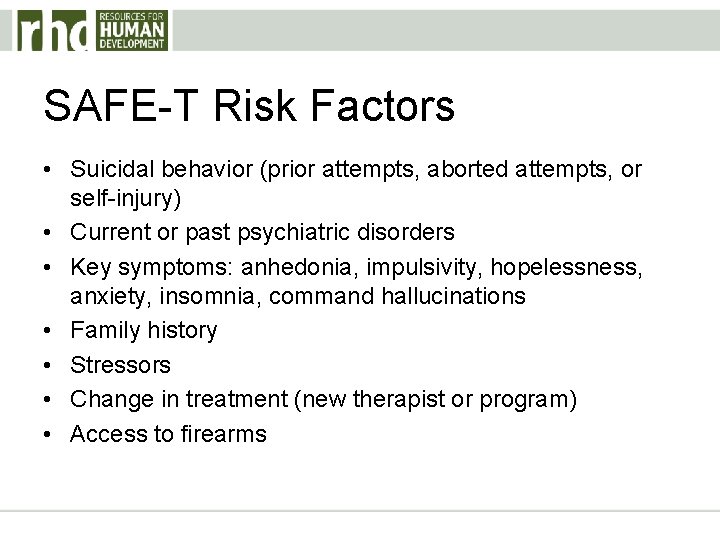
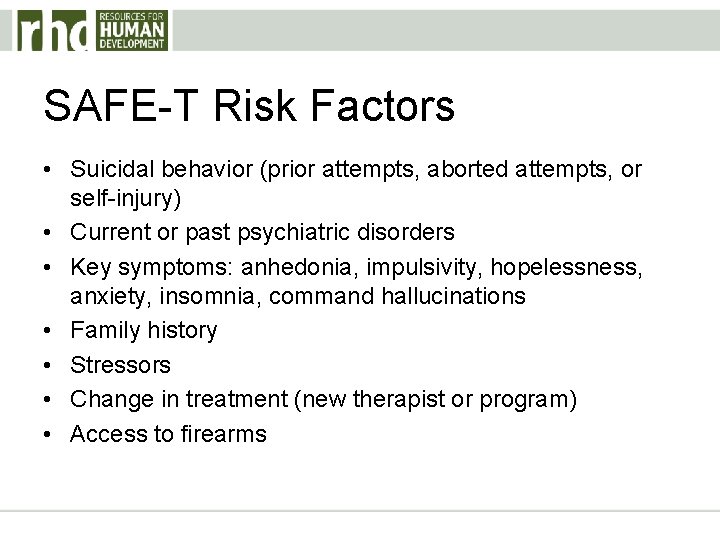
SAFE-T Risk Factors • Suicidal behavior (prior attempts, aborted attempts, or self-injury) • Current or past psychiatric disorders • Key symptoms: anhedonia, impulsivity, hopelessness, anxiety, insomnia, command hallucinations • Family history • Stressors • Change in treatment (new therapist or program) • Access to firearms
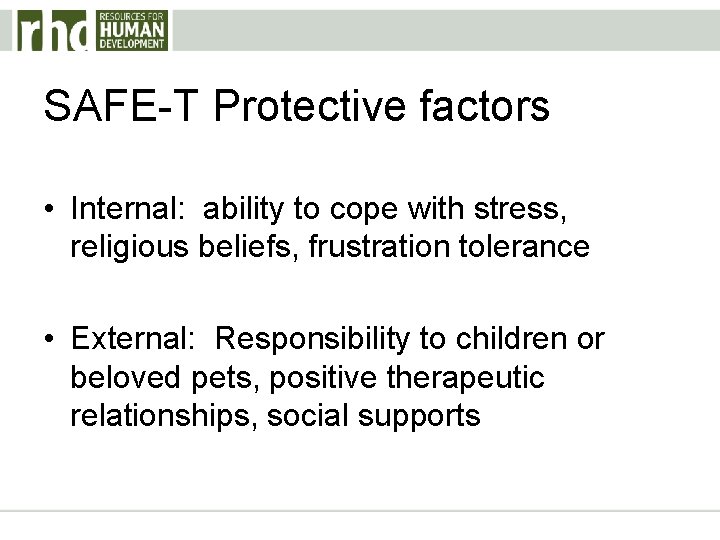
SAFE-T Protective factors • Internal: ability to cope with stress, religious beliefs, frustration tolerance • External: Responsibility to children or beloved pets, positive therapeutic relationships, social supports
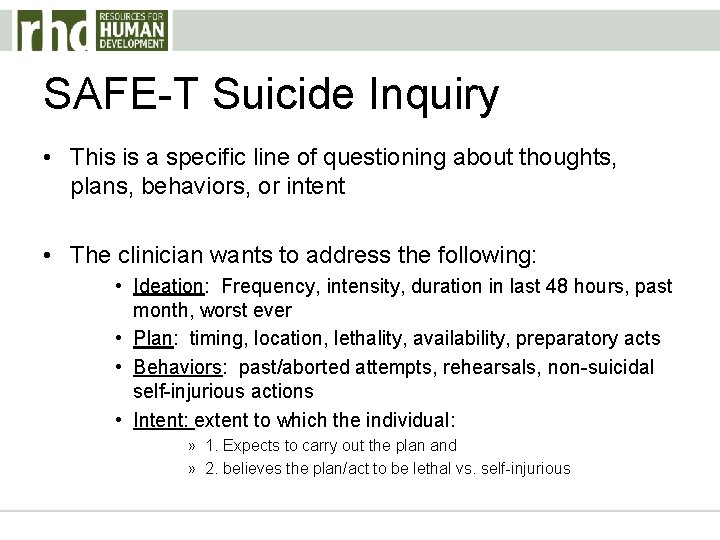
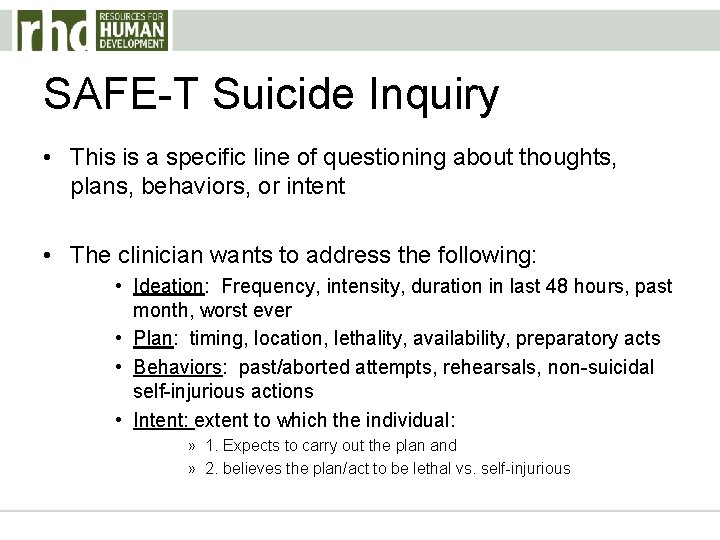
SAFE-T Suicide Inquiry • This is a specific line of questioning about thoughts, plans, behaviors, or intent • The clinician wants to address the following: • Ideation: Frequency, intensity, duration in last 48 hours, past month, worst ever • Plan: timing, location, lethality, availability, preparatory acts • Behaviors: past/aborted attempts, rehearsals, non-suicidal self-injurious actions • Intent: extent to which the individual: » 1. Expects to carry out the plan and » 2. believes the plan/act to be lethal vs. self-injurious
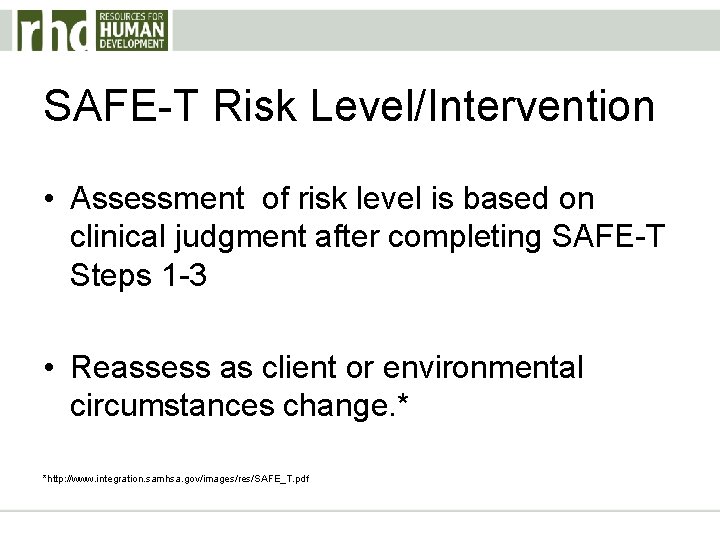
SAFE-T Risk Level/Intervention • Assessment of risk level is based on clinical judgment after completing SAFE-T Steps 1 -3 • Reassess as client or environmental circumstances change. * *http: //www. integration. samhsa. gov/images/res/SAFE_T. pdf
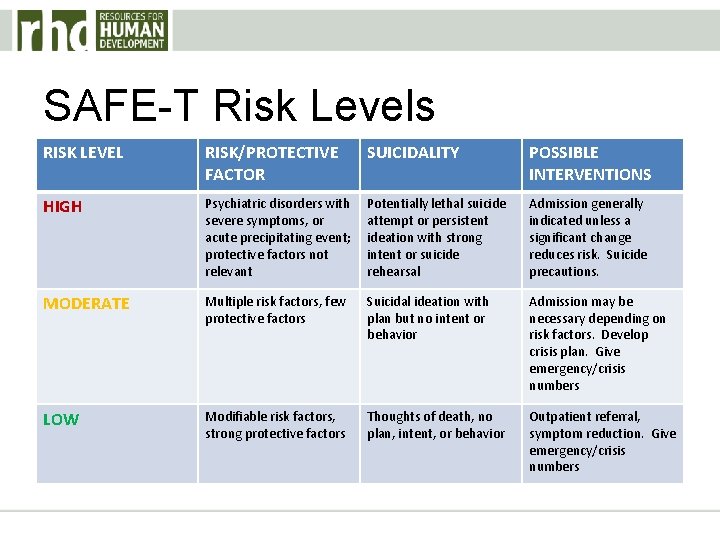
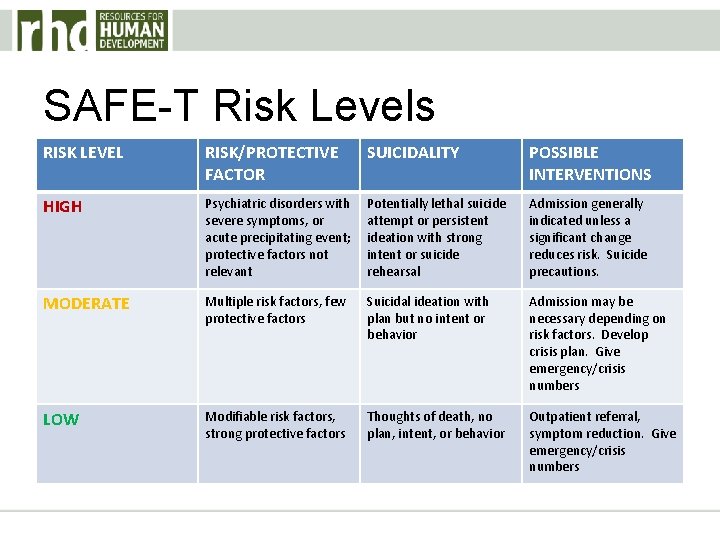
SAFE-T Risk Levels RISK LEVEL RISK/PROTECTIVE FACTOR SUICIDALITY POSSIBLE INTERVENTIONS HIGH Psychiatric disorders with severe symptoms, or acute precipitating event; protective factors not relevant Potentially lethal suicide attempt or persistent ideation with strong intent or suicide rehearsal Admission generally indicated unless a significant change reduces risk. Suicide precautions. MODERATE Multiple risk factors, few protective factors Suicidal ideation with plan but no intent or behavior Admission may be necessary depending on risk factors. Develop crisis plan. Give emergency/crisis numbers LOW Modifiable risk factors, strong protective factors Thoughts of death, no plan, intent, or behavior Outpatient referral, symptom reduction. Give emergency/crisis numbers
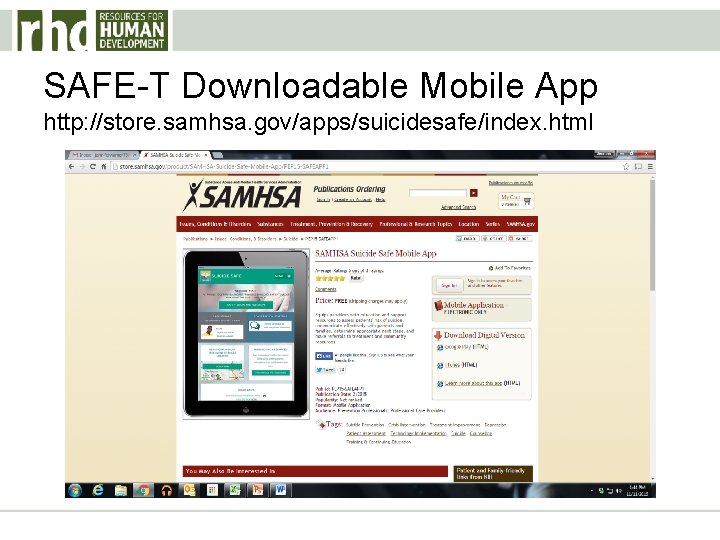
SAFE-T Downloadable Mobile App http: //store. samhsa. gov/apps/suicidesafe/index. html
S. L. A. P. and D. I. R. T. • SLAP – An assessment of degree of risk • After there is a realization that the client may be at risk, assess the degree of risk. • Always begin questions with “how? ” such as, “How do you plan to harm yourself? ” • If the person has a plan, use SLAP
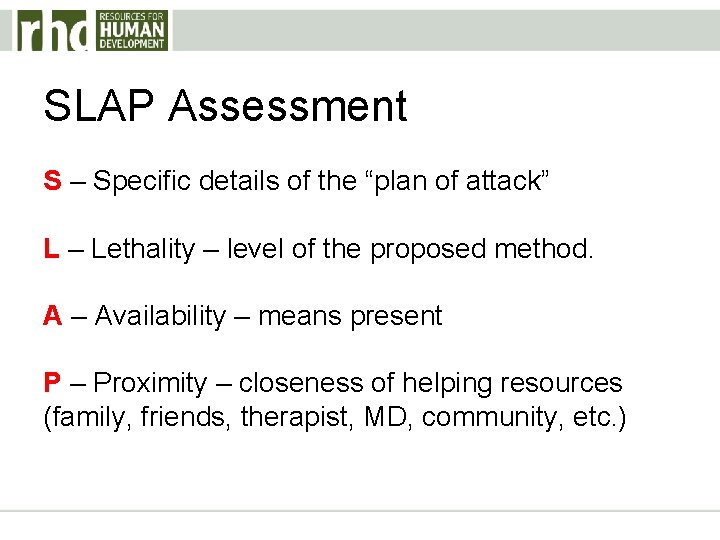
SLAP Assessment S – Specific details of the “plan of attack” L – Lethality – level of the proposed method. A – Availability – means present P – Proximity – closeness of helping resources (family, friends, therapist, MD, community, etc. )
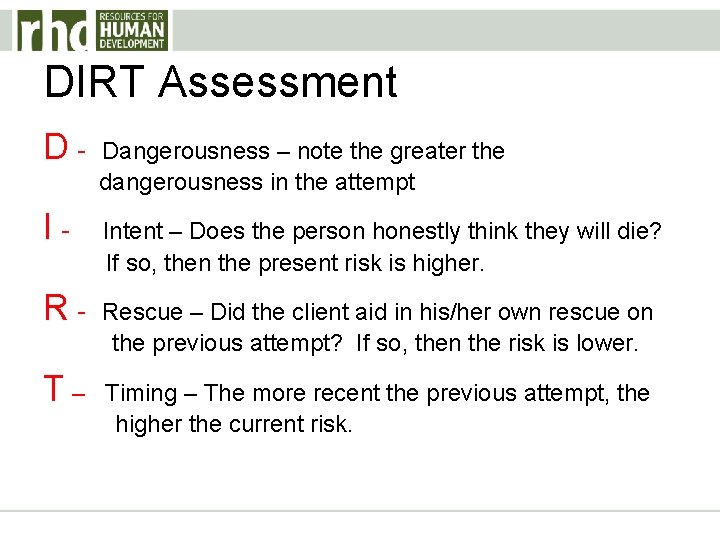
DIRT Assessment • This is an assessment of past suicide attempts • Keep in mind any unexplainable deviation from an ingrained behavioral pattern or sudden/unexplainable recovery from a severe depression or other negative factor(s).
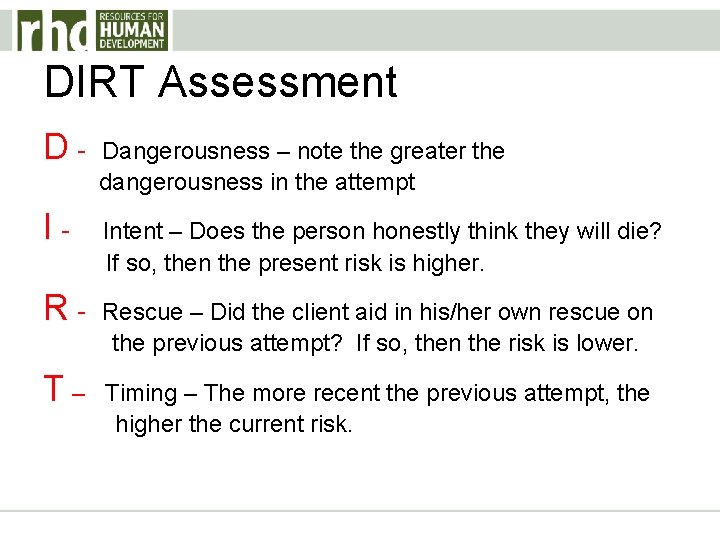
DIRT Assessment D- Dangerousness – note the greater the dangerousness in the attempt I- Intent – Does the person honestly think they will die? If so, then the present risk is higher. R- Rescue – Did the client aid in his/her own rescue on the previous attempt? If so, then the risk is lower. T– Timing – The more recent the previous attempt, the higher the current risk.
Suicide Prevention
Suicide prevention efforts seek to: • Reduce factors that increase the risk for suicidal thoughts and behaviors • Increase the factors that help strengthen, support, and protect individuals from suicide.
These efforts address: • Individual • Relationship • Community • Societal factors
DO NOT: • Accept a “Contract for Safety”. There is no evidence that “contracts” prevent suicide. In fact, they may give workers a false sense of reassurance.

Case Studies
Case Study 1 30 -year-old white male brought from his place of employment by a personnel representative. Client has been thinking of suicide “all the time” because he “can’t cope. ” Has a “knot in his stomach; sleep and appetite are down (sleeps only 3 hours per night); and plans either to shoot himself, “jump off a bridge”, or “drive recklessly”. He also reports constant fighting with his wife leading to a recent breakup (there is a long history of mutual verbal/physical abuse). He also shares a history of a serious suicide attempt when he jumped off of a ledge and fractured both legs. He reported the reason for that attempt was a previous divorce. He also reports a history of chemical dependency with two courses of treatment. He denies current problems with alcohol or drugs. He is tearful, shaking, frightened, reports feeling hopeless, and at high risk for impulsive acting out. He states that life isn’t worthwhile.

Case Study 2 49 -year-old white female brought in to you by police following threats to overdose on aspirin (initially telephoned crisis line and was willing to give her address). She reports that she feels trapped and abused, and that she “can’t cope at home with [her] schizophrenic sister”. She wants to be in the hospital and continues to state that she feels like killing herself. Her husband shares that the she has been threatening to shoot him and her daughter but “probably has no gun”. She shares that she has had a recent arrest for disorderly conduct (threatened police with a butcher knife). She also shares that she has a history of aspirin overdose 3 years ago. In the interview, she is cooperative but you note that she appears depressed, anxious, helpless, and hopeless. Her appetite and sleep are down, and so is her self-esteem. Police report that she had an alcohol level of. 12 on her field breathalyzer.
Case Study 3 23 -year-old white male, self-referred. He tells you he bought a gun 2 months ago to kill himself and claims to have the “gun and four shells” in his car. He reports having planned time and place for suicide several times in the past and shares with you that he “cannot live any more” with his “emotional pain” since his wife left him 3 years ago. He also tells you that this pain has increased during the last week, but he cannot pinpoint any reason. He also shares that he has a history of chemical dependency, but has been sober for 20 months and currently goes to AA.
Case Study 4 16 -year-old Native American female, self-referred following an overdose of 12 aspirins. She tells you that she could not tolerate rumors at school that she and another girl are “sharing the same boyfriend”. She currently denies being suicidal and states, “I won’t do it again; I learned my lesson”. She also reports that she has “always” had “difficulty expressing her feelings”. In the interview, she is quiet, appears guarded, and initially appears quite reluctant to talk.

Questions? ?
Jennifer Warner, MA, NCC jen. warner@rhd. org 412 -368 -8996 1 -800 -273 -8255 National Suicide Prevention Lifeline