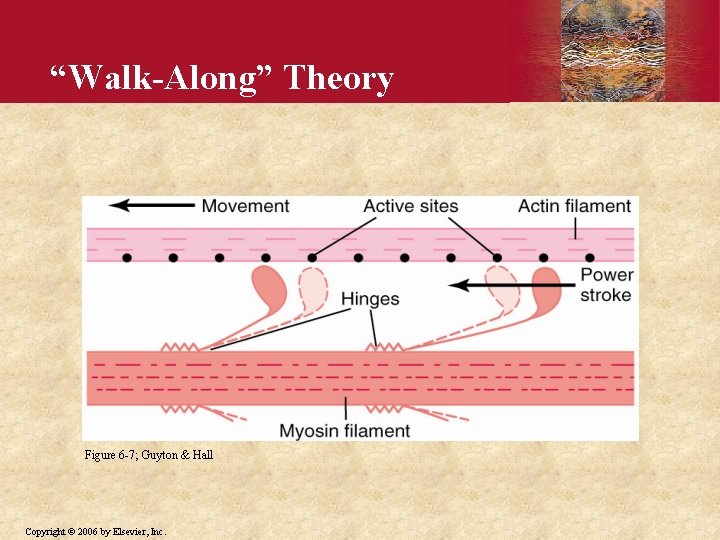
WalkAlong Theory Figure 6 7 Guyton Hall Copyright
![Frequency Summation of Twitches and Tetanus Myoplasmic [Ca 2+] Fused tetanus Force AP Time Frequency Summation of Twitches and Tetanus Myoplasmic [Ca 2+] Fused tetanus Force AP Time](https://slidetodoc.com/presentation_image_h2/5746c7037bef48ecc756b3ab9f29f915/image-29.jpg)
- Slides: 38
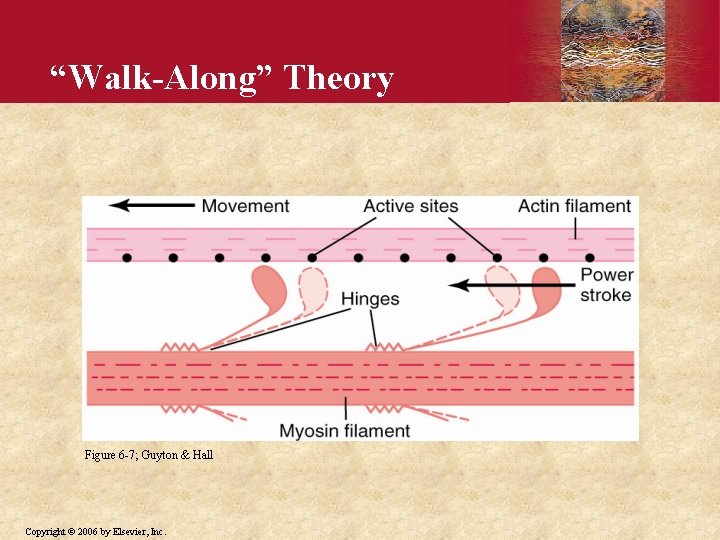
“Walk-Along” Theory Figure 6 -7; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
U N I T II Textbook of Medical Physiology, 11 th Edition Chapter 6: Contraction of Skeletal Muscle Slides by Thomas H. Adair, Ph. D GUYTON & HALL Copyright © 2006 by Elsevier, Inc.
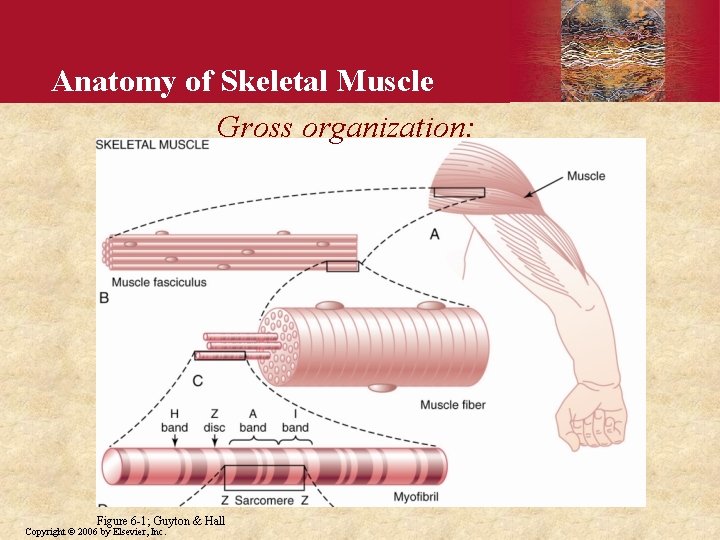
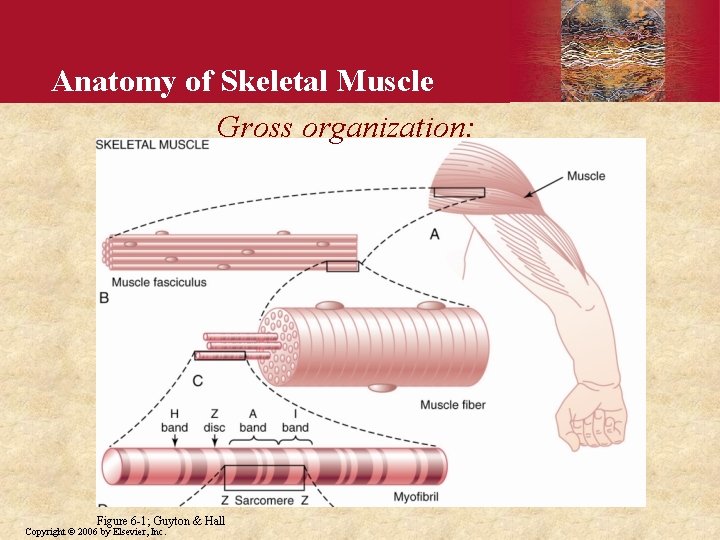
Anatomy of Skeletal Muscle Gross organization: Figure 6 -1; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
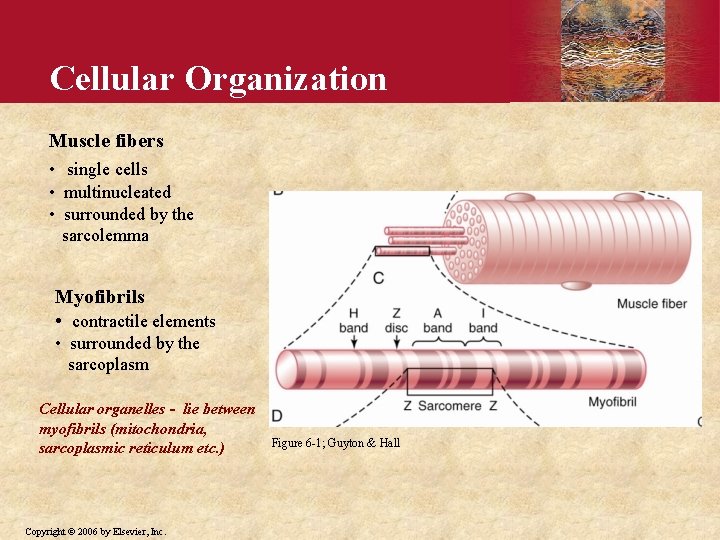
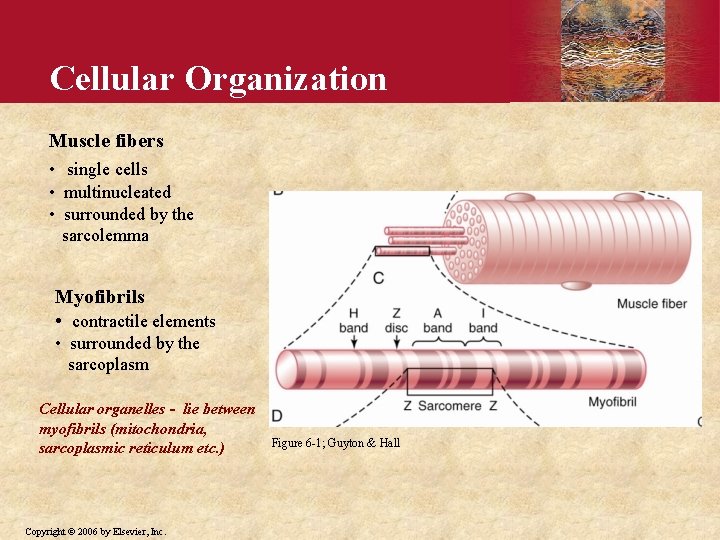
Cellular Organization Muscle fibers • single cells • multinucleated • surrounded by the sarcolemma Myofibrils • contractile elements • surrounded by the sarcoplasm Cellular organelles - lie between myofibrils (mitochondria, sarcoplasmic reticulum etc. ) Copyright © 2006 by Elsevier, Inc. Figure 6 -1; Guyton & Hall
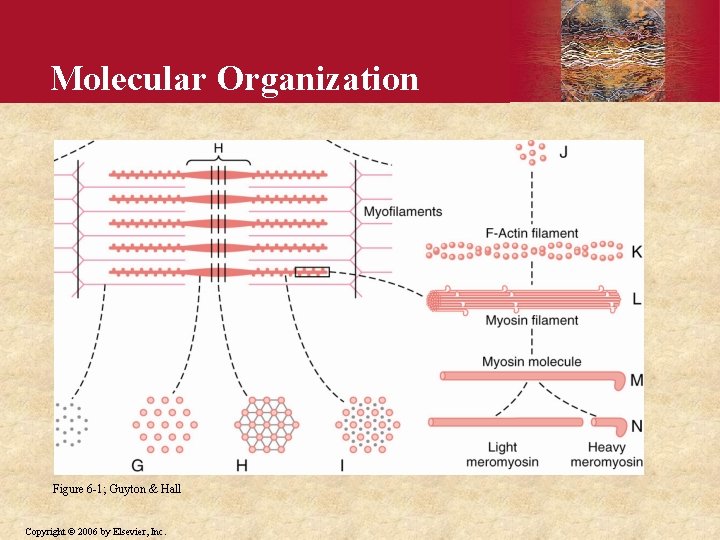
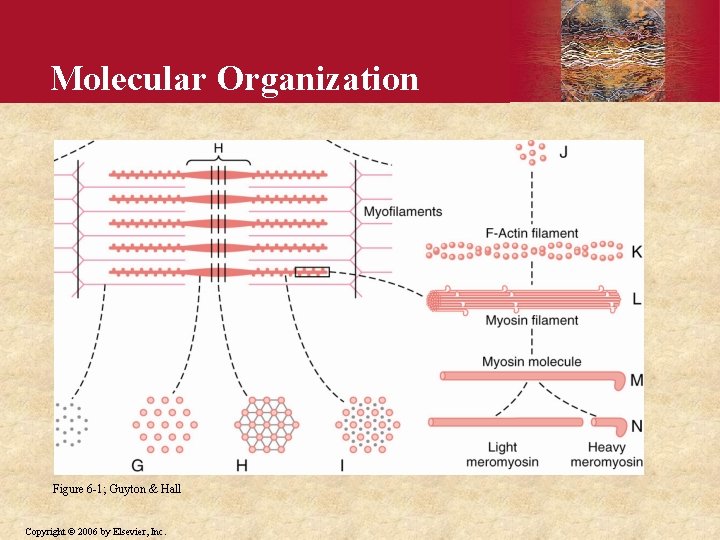
Molecular Organization Figure 6 -1; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
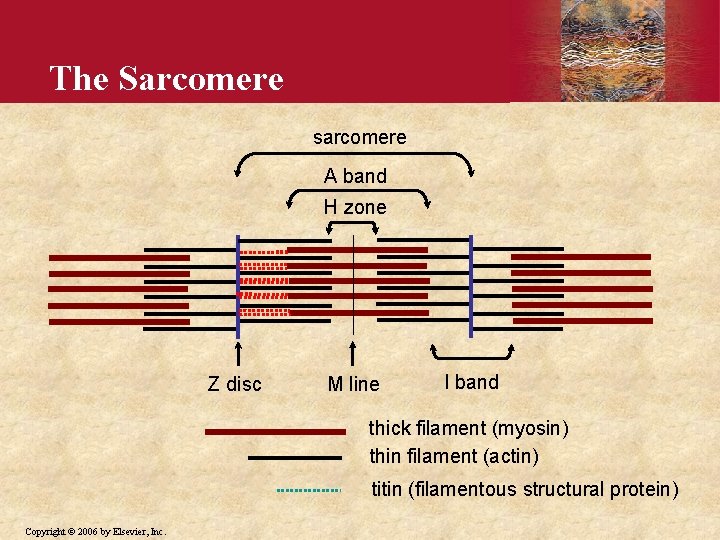
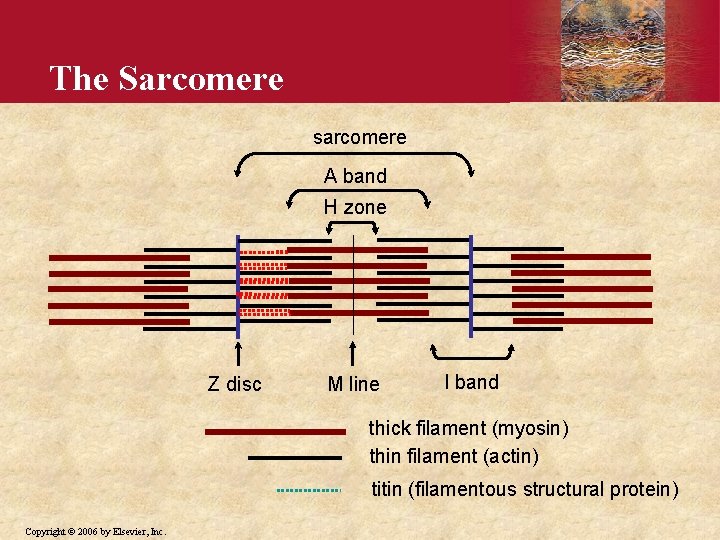
The Sarcomere sarcomere A band H zone Z disc M line I band thick filament (myosin) thin filament (actin) titin (filamentous structural protein) Copyright © 2006 by Elsevier, Inc.
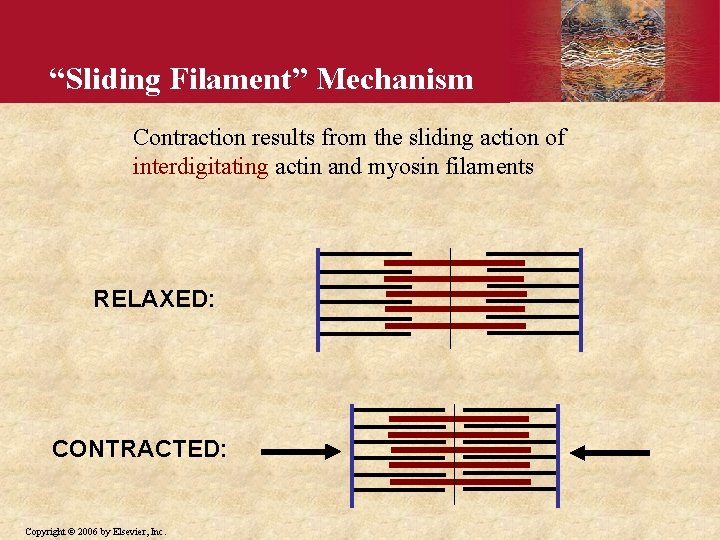
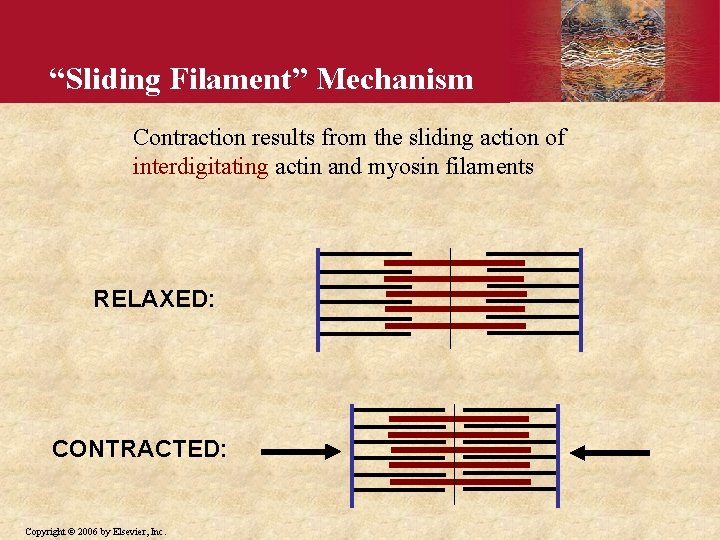
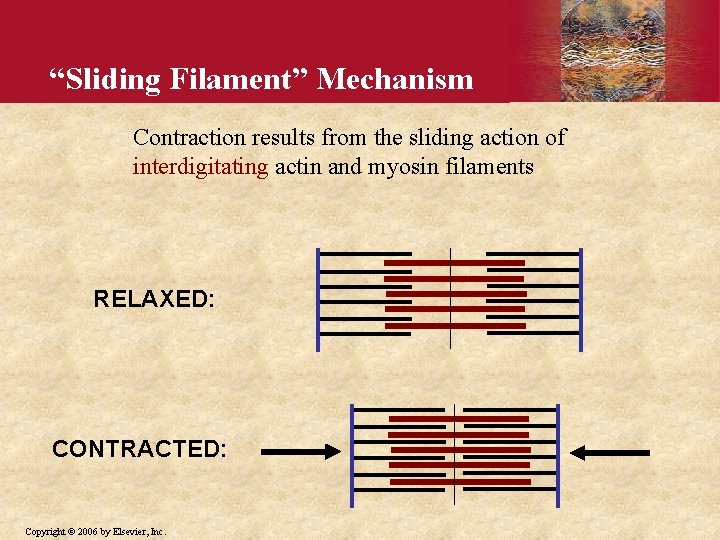
“Sliding Filament” Mechanism Contraction results from the sliding action of interdigitating actin and myosin filaments RELAXED: CONTRACTED: Copyright © 2006 by Elsevier, Inc.
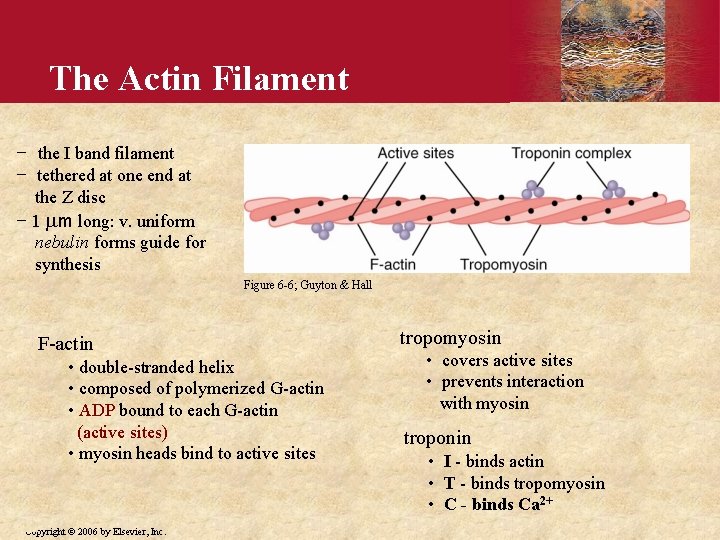
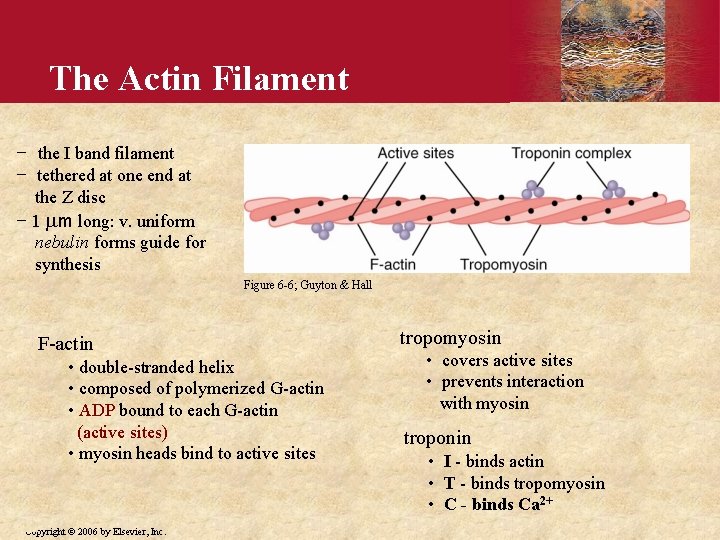
The Actin Filament − the I band filament − tethered at one end at the Z disc − 1 mm long: v. uniform nebulin forms guide for synthesis Figure 6 -6; Guyton & Hall F-actin • double-stranded helix • composed of polymerized G-actin • ADP bound to each G-actin (active sites) • myosin heads bind to active sites Copyright © 2006 by Elsevier, Inc. tropomyosin • covers active sites • prevents interaction with myosin troponin • I - binds actin • T - binds tropomyosin • C - binds Ca 2+
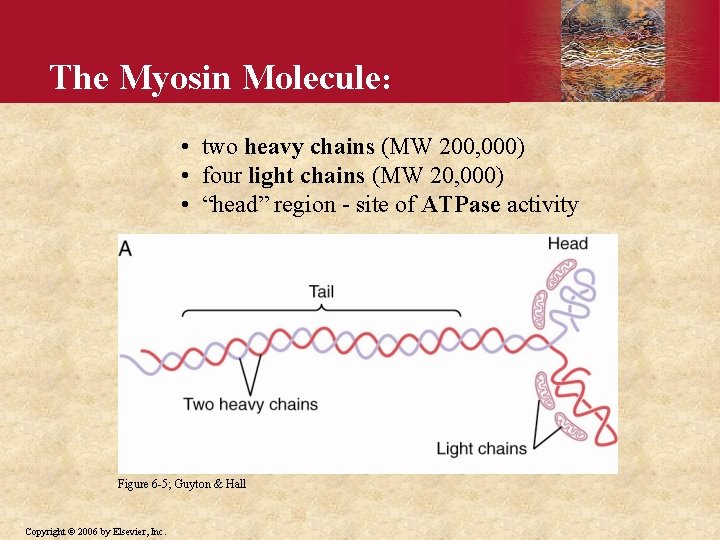
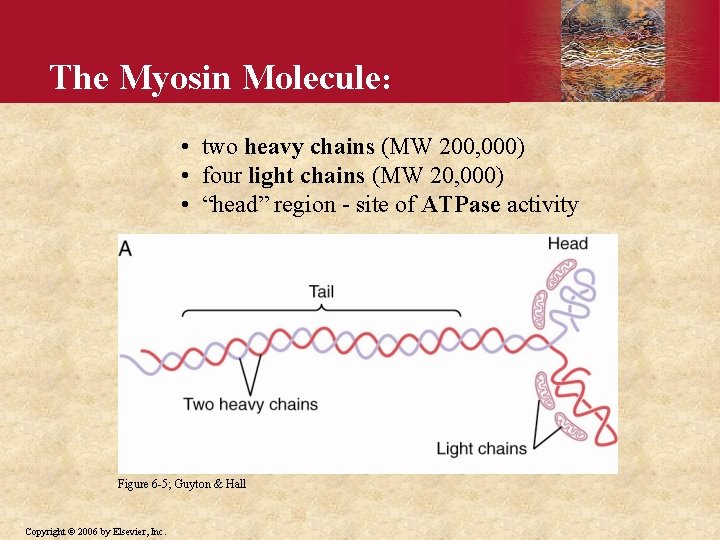
The Myosin Molecule: • two heavy chains (MW 200, 000) • four light chains (MW 20, 000) • “head” region - site of ATPase activity Figure 6 -5; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
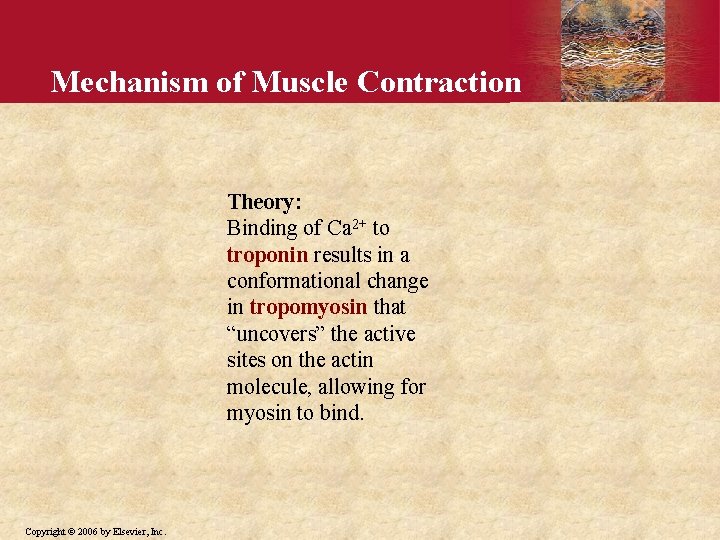
Mechanism of Muscle Contraction Theory: Binding of Ca 2+ to troponin results in a conformational change in tropomyosin that “uncovers” the active sites on the actin molecule, allowing for myosin to bind. Copyright © 2006 by Elsevier, Inc.
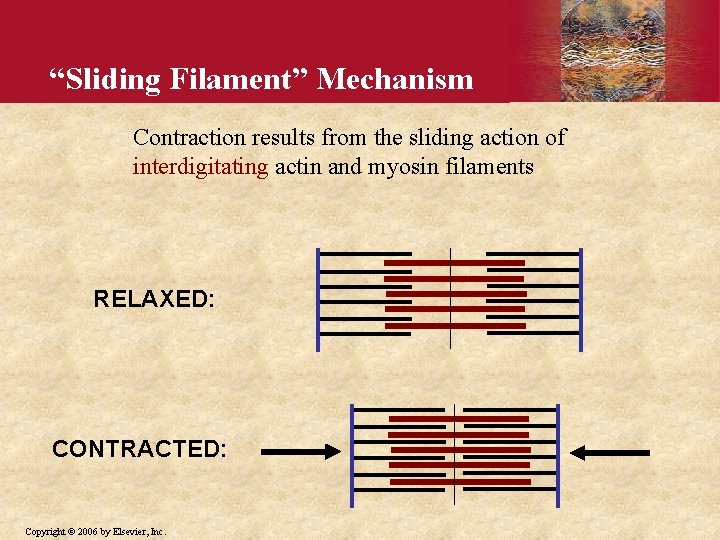
“Sliding Filament” Mechanism Contraction results from the sliding action of interdigitating actin and myosin filaments RELAXED: CONTRACTED: Copyright © 2006 by Elsevier, Inc.
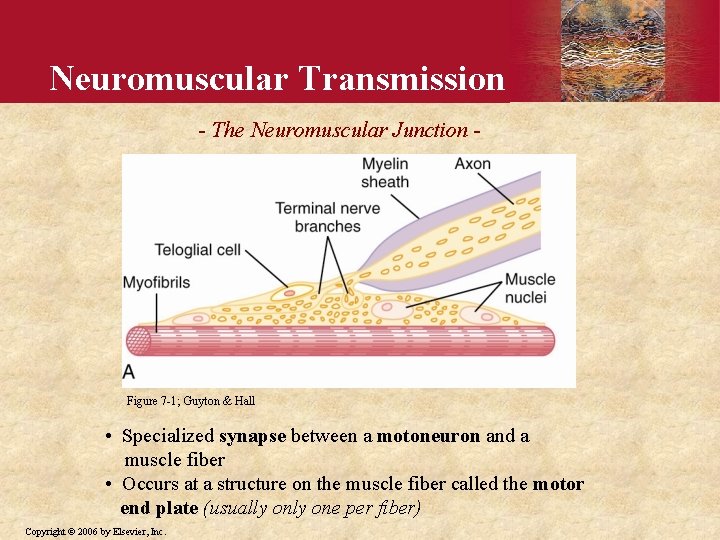
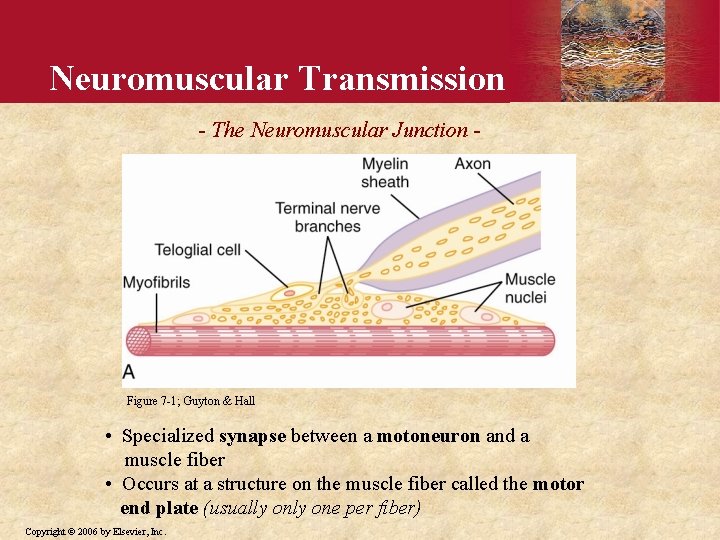
Neuromuscular Transmission - The Neuromuscular Junction - Figure 7 -1; Guyton & Hall • Specialized synapse between a motoneuron and a muscle fiber • Occurs at a structure on the muscle fiber called the motor end plate (usually one per fiber) Copyright © 2006 by Elsevier, Inc.
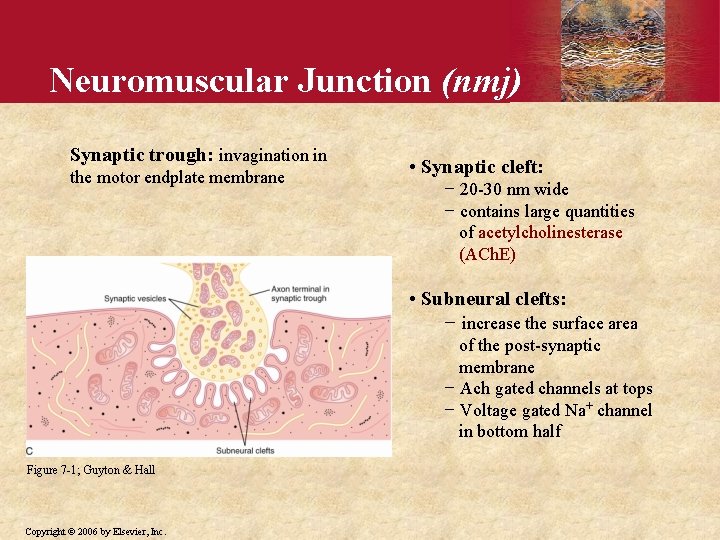
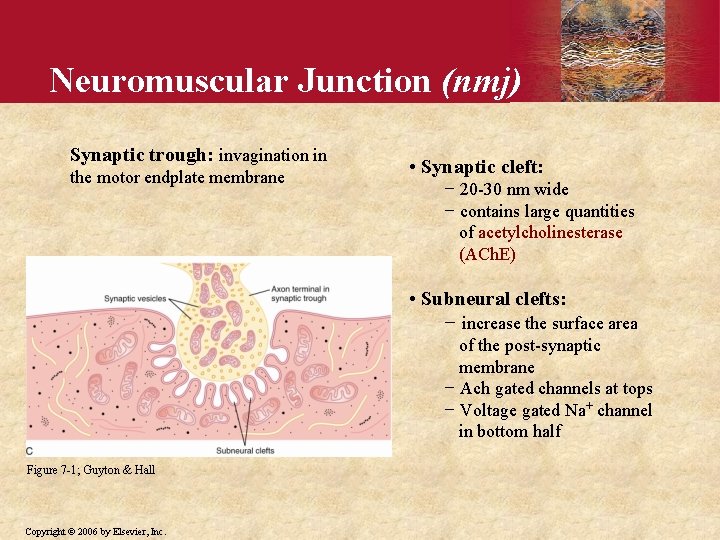
Neuromuscular Junction (nmj) Synaptic trough: invagination in the motor endplate membrane • Synaptic cleft: − 20 -30 nm wide − contains large quantities of acetylcholinesterase (ACh. E) • Subneural clefts: − increase the surface area of the post-synaptic membrane − Ach gated channels at tops − Voltage gated Na+ channel in bottom half Figure 7 -1; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
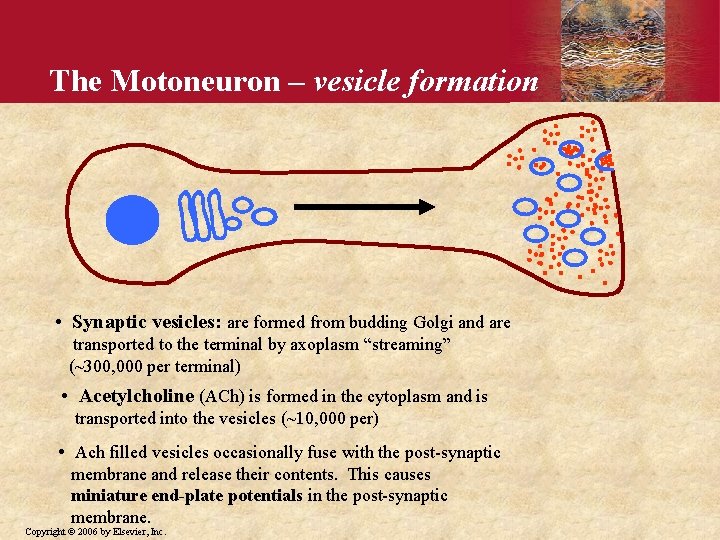
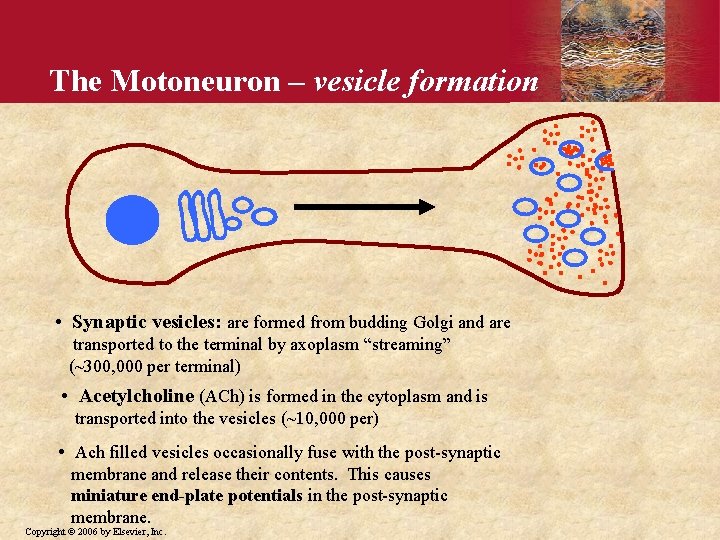
The Motoneuron – vesicle formation • Synaptic vesicles: are formed from budding Golgi and are transported to the terminal by axoplasm “streaming” (~300, 000 per terminal) • Acetylcholine (ACh) is formed in the cytoplasm and is transported into the vesicles (~10, 000 per) • Ach filled vesicles occasionally fuse with the post-synaptic membrane and release their contents. This causes miniature end-plate potentials in the post-synaptic membrane. Copyright © 2006 by Elsevier, Inc.
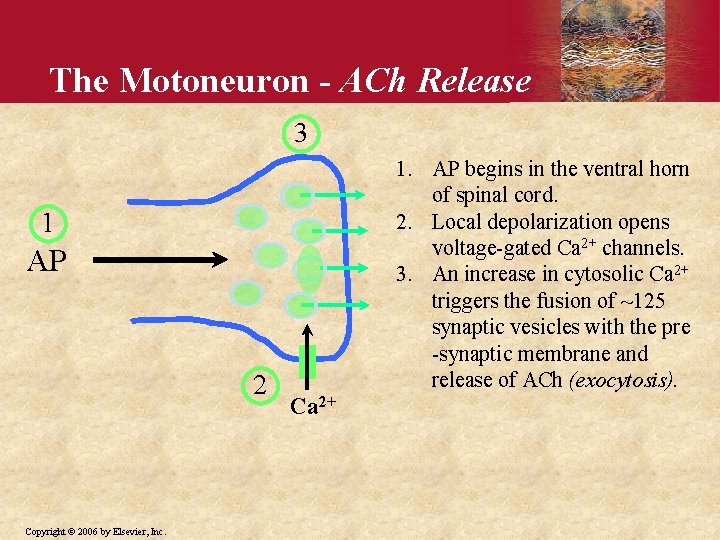
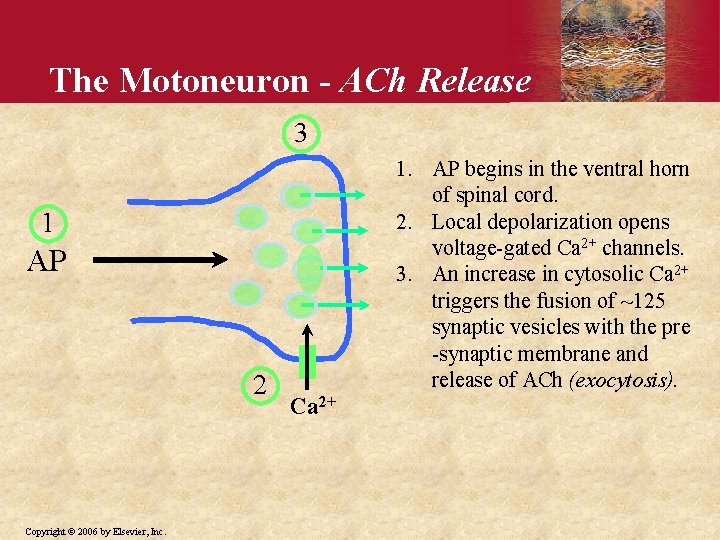
The Motoneuron - ACh Release 3 1. AP begins in the ventral horn of spinal cord. 2. Local depolarization opens voltage-gated Ca 2+ channels. 3. An increase in cytosolic Ca 2+ triggers the fusion of ~125 synaptic vesicles with the pre -synaptic membrane and release of ACh (exocytosis). 1 AP 2 Copyright © 2006 by Elsevier, Inc. Ca 2+
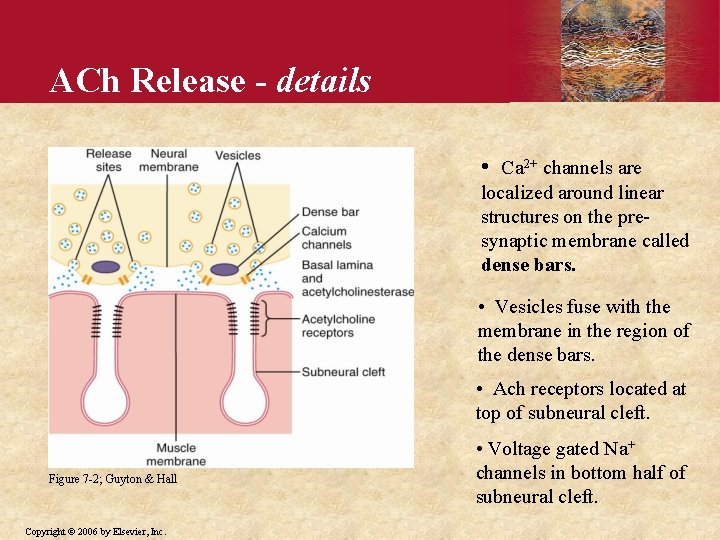
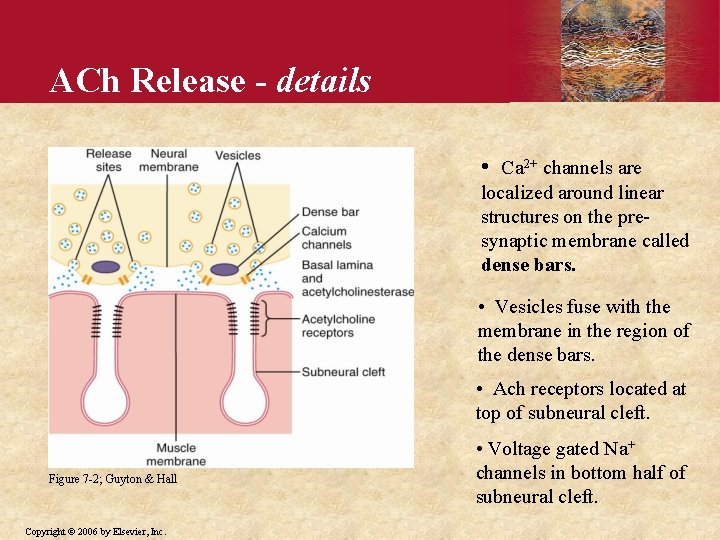
ACh Release - details • Ca 2+ channels are localized around linear structures on the presynaptic membrane called dense bars. • Vesicles fuse with the membrane in the region of the dense bars. • Ach receptors located at top of subneural cleft. Figure 7 -2; Guyton & Hall Copyright © 2006 by Elsevier, Inc. • Voltage gated Na+ channels in bottom half of subneural cleft.
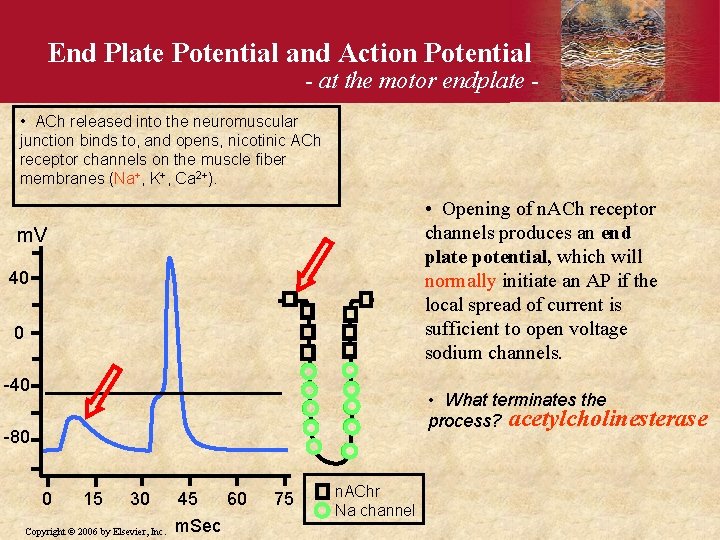
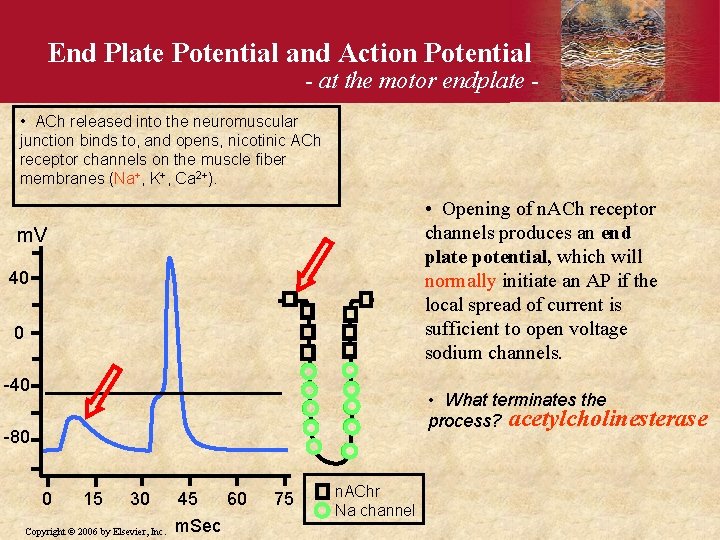
End Plate Potential and Action Potential - at the motor endplate - • ACh released into the neuromuscular junction binds to, and opens, nicotinic ACh receptor channels on the muscle fiber membranes (Na+, K+, Ca 2+). • Opening of n. ACh receptor channels produces an end plate potential, which will normally initiate an AP if the local spread of current is sufficient to open voltage sodium channels. m. V 40 0 -40 • What terminates the process? acetylcholinesterase -80 0 15 30 Copyright © 2006 by Elsevier, Inc. 45 m. Sec 60 75 n. AChr Na channel
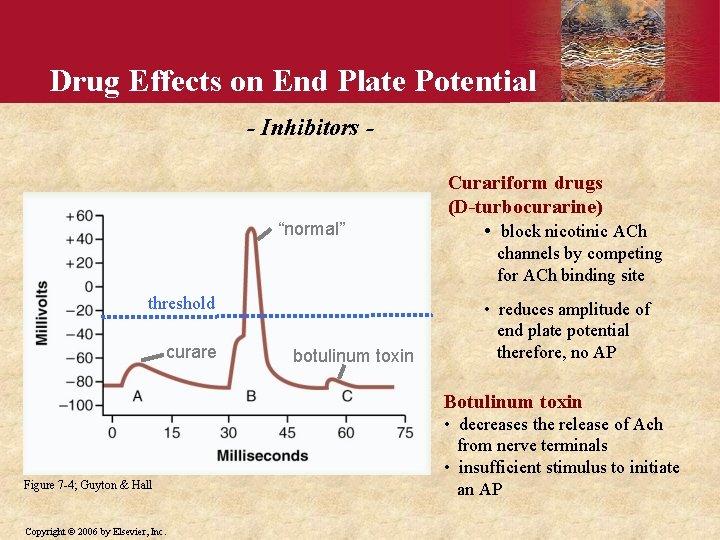
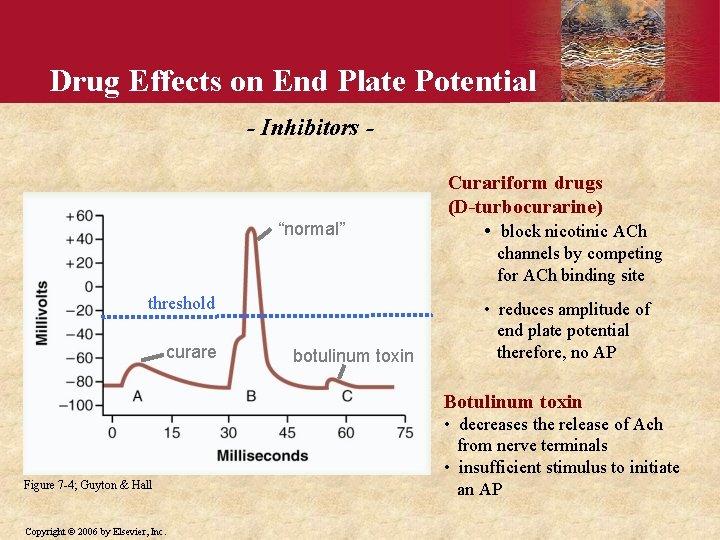
Drug Effects on End Plate Potential - Inhibitors - “normal” Curariform drugs (D-turbocurarine) • block nicotinic ACh channels by competing for ACh binding site threshold curare botulinum toxin • reduces amplitude of end plate potential therefore, no AP Botulinum toxin Figure 7 -4; Guyton & Hall Copyright © 2006 by Elsevier, Inc. • decreases the release of Ach from nerve terminals • insufficient stimulus to initiate an AP
Drug Effects on End Plate Potential - Stimulants ACh-like drugs (methacholine, carbachol, nicotine) • bind activate nicotinic ACh receptors • not destroyed by ACh. E – prolonged effect Anti-ACh. E (neostigmine, physostigmine, diisopropyl fluorophosphate or “nerve gas”) • block the degradation of ACh • prolong its effect Copyright © 2006 by Elsevier, Inc.
Myasthenia Gravis Incidence / symptoms: • paralysis - lethal in extreme cases when respiratory muscles are involved • 2 per 1, 000 people / year Cause: • autoimmune disease characterized by the presence of antibodies against the nicotinic ACh receptor which destroys them • weak end plate potentials Treatment: • usually ameliorated by anti-ACh. E (neostigmine) • increases amount of ACh in nmj Copyright © 2006 by Elsevier, Inc.
Lambert-Eaton Myasthenic Syndrome Incidence / symptoms: • 1 per 100, 000 people / year • 40% also have small cell lung cancer • muscle weakness/paralysis Cause: • LEMS results from an autoimmune attack against voltage-gated calcium channels on the presynaptic motor nerve terminal. • weak end plate potentials Treatment: • can be treated with anti-ACh. E (neostigmine) • increases amount of ACh in nmj Copyright © 2006 by Elsevier, Inc.
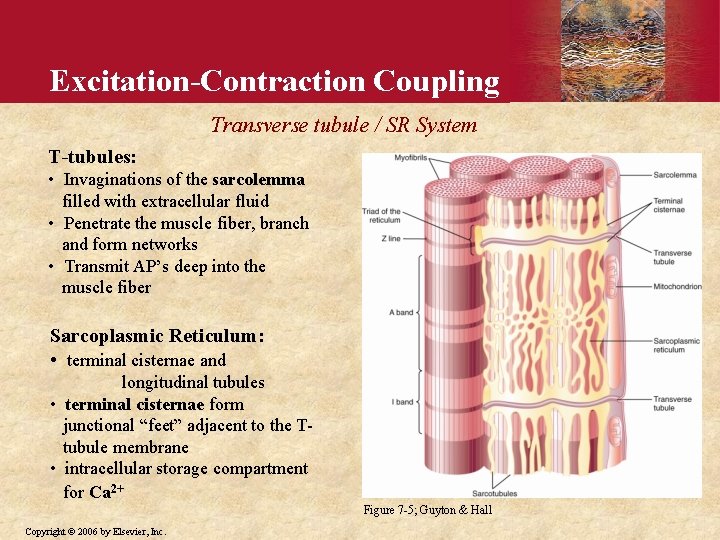
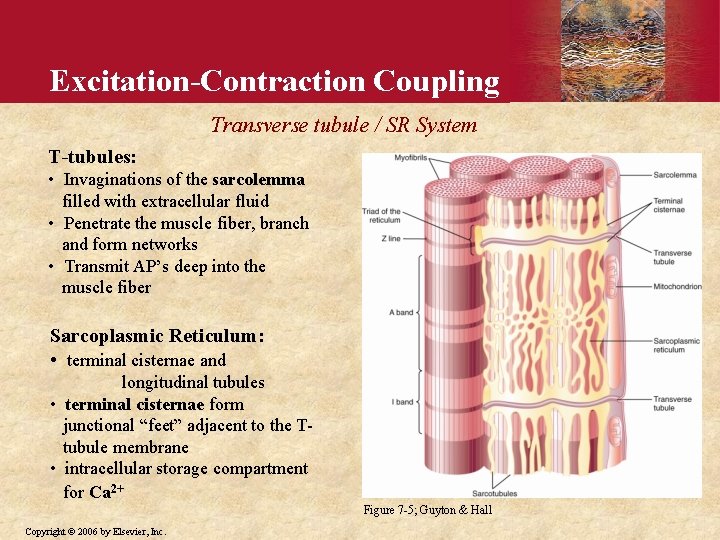
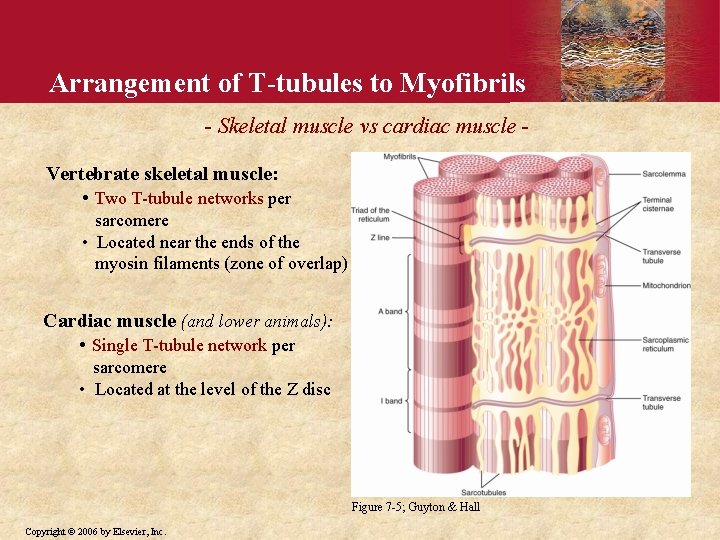
Excitation-Contraction Coupling Transverse tubule / SR System T-tubules: • Invaginations of the sarcolemma filled with extracellular fluid • Penetrate the muscle fiber, branch and form networks • Transmit AP’s deep into the muscle fiber Sarcoplasmic Reticulum: • terminal cisternae and longitudinal tubules • terminal cisternae form junctional “feet” adjacent to the Ttubule membrane • intracellular storage compartment for Ca 2+ Figure 7 -5; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
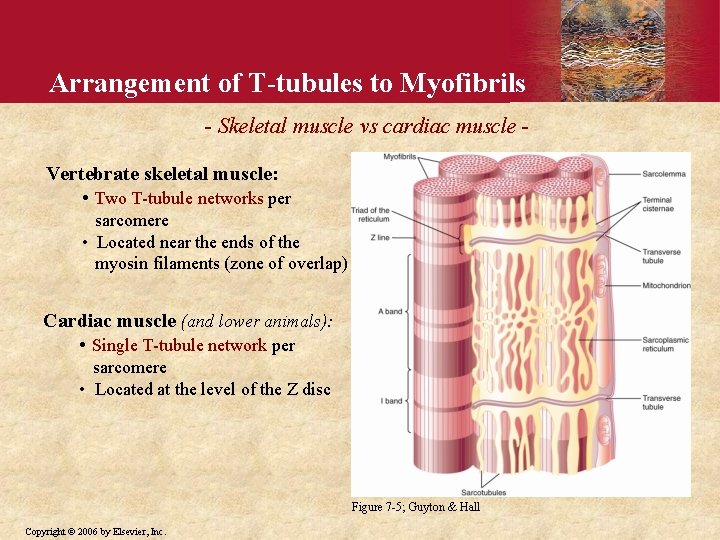
Arrangement of T-tubules to Myofibrils - Skeletal muscle vs cardiac muscle Vertebrate skeletal muscle: • Two T-tubule networks per sarcomere • Located near the ends of the myosin filaments (zone of overlap) Cardiac muscle (and lower animals): • Single T-tubule network per sarcomere • Located at the level of the Z disc Figure 7 -5; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
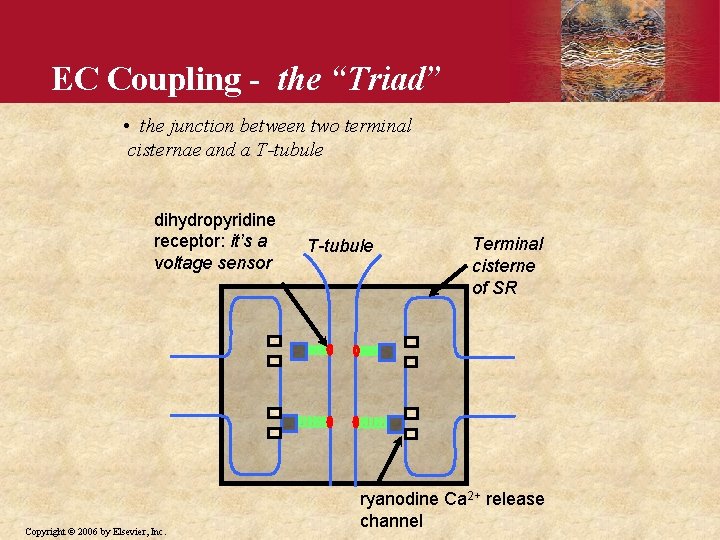
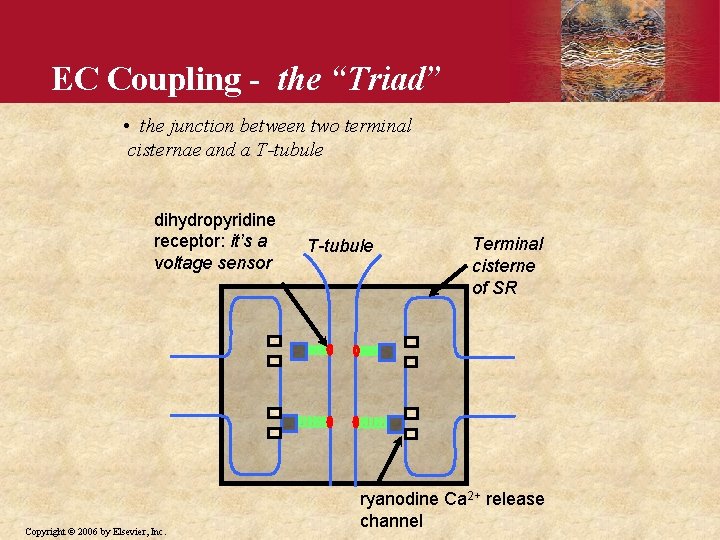
EC Coupling - the “Triad” • the junction between two terminal cisternae and a T-tubule dihydropyridine receptor: it’s a voltage sensor Copyright © 2006 by Elsevier, Inc. T-tubule Terminal cisterne of SR ryanodine Ca 2+ release channel
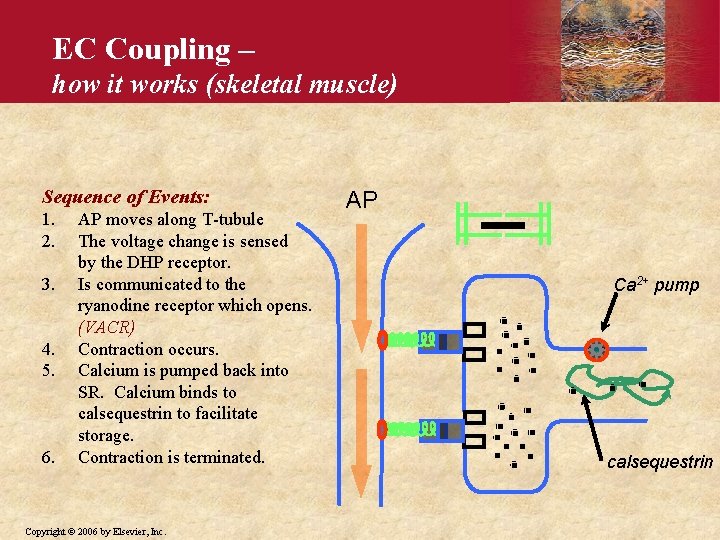
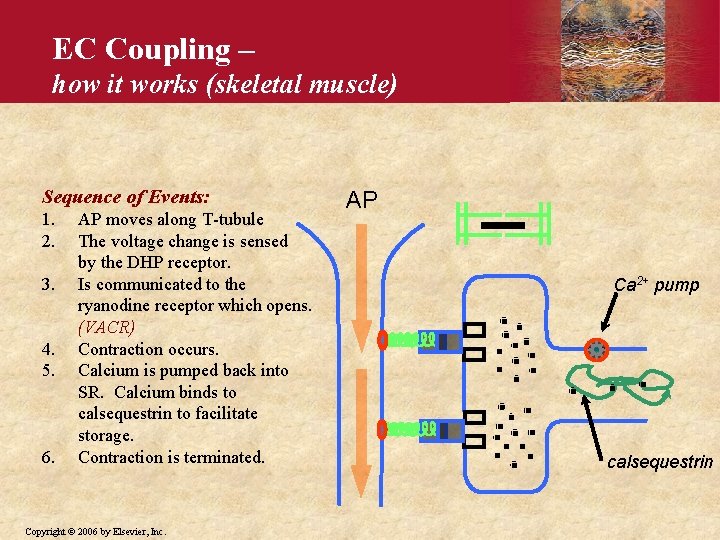
EC Coupling – how it works (skeletal muscle) Sequence of Events: 1. 2. 3. 4. 5. 6. AP moves along T-tubule The voltage change is sensed by the DHP receptor. Is communicated to the ryanodine receptor which opens. (VACR) Contraction occurs. Calcium is pumped back into SR. Calcium binds to calsequestrin to facilitate storage. Contraction is terminated. Copyright © 2006 by Elsevier, Inc. AP Ca 2+ pump calsequestrin
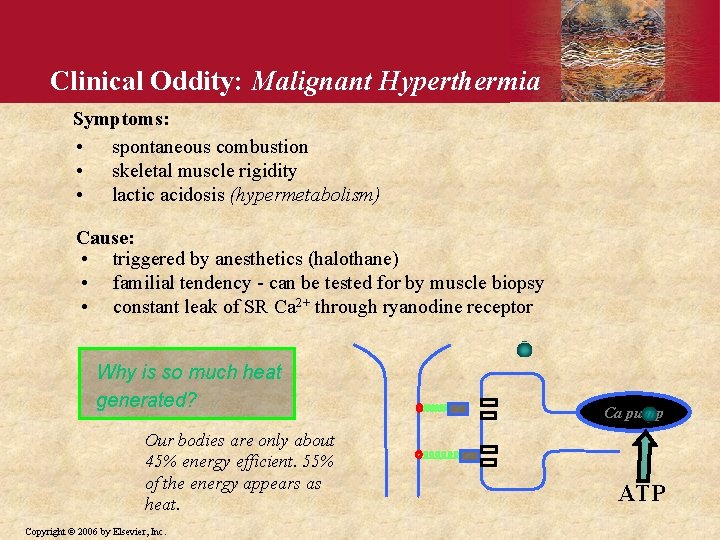
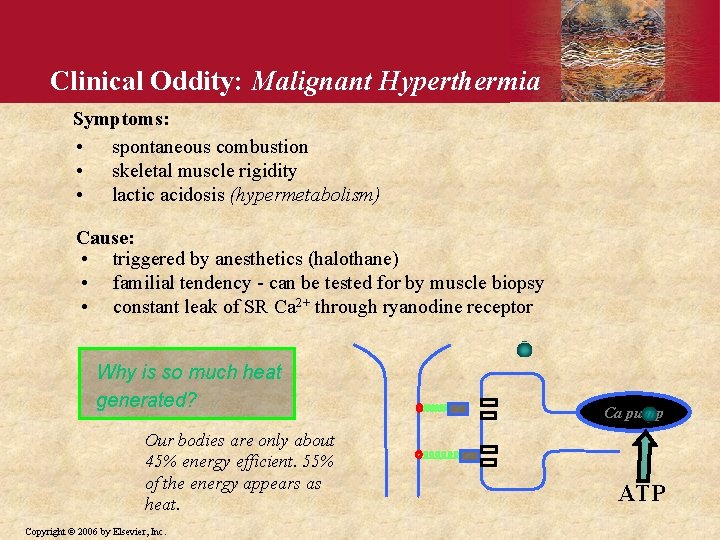
Clinical Oddity: Malignant Hyperthermia Symptoms: • spontaneous combustion • skeletal muscle rigidity • lactic acidosis (hypermetabolism) Cause: • triggered by anesthetics (halothane) • familial tendency - can be tested for by muscle biopsy • constant leak of SR Ca 2+ through ryanodine receptor Why is so much heat generated? Our bodies are only about 45% energy efficient. 55% of the energy appears as heat. Copyright © 2006 by Elsevier, Inc. Ca pump ATP
Muscle Mechanics Copyright © 2006 by Elsevier, Inc.
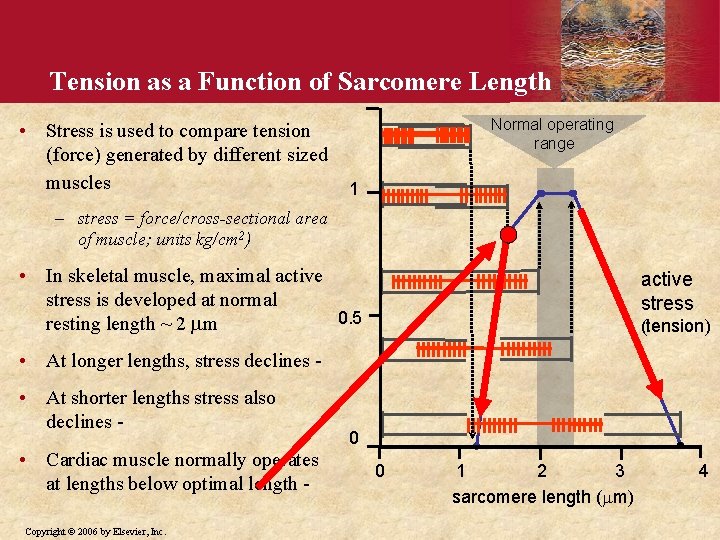
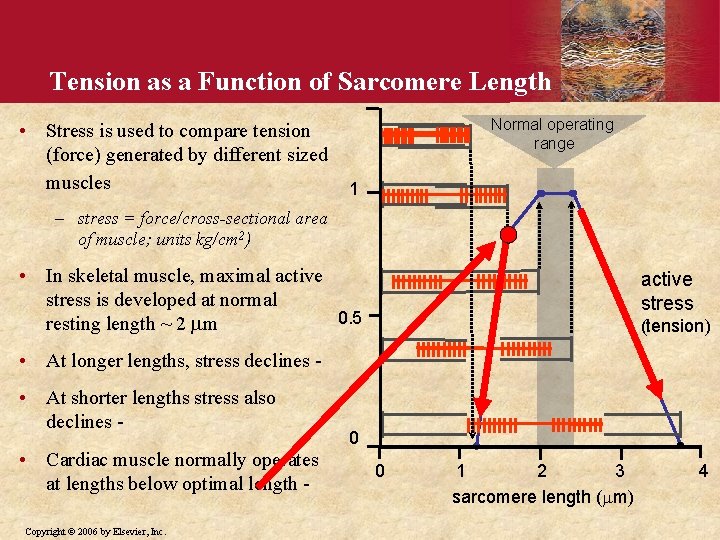
Tension as a Function of Sarcomere Length • Stress is used to compare tension (force) generated by different sized muscles Normal operating range 1 – stress = force/cross-sectional area of muscle; units kg/cm 2) • In skeletal muscle, maximal active stress is developed at normal 0. 5 resting length ~ 2 mm active stress (tension) • At longer lengths, stress declines • At shorter lengths stress also declines • Cardiac muscle normally operates at lengths below optimal length Copyright © 2006 by Elsevier, Inc. 0 0 1 2 3 sarcomere length (mm) 4
![Frequency Summation of Twitches and Tetanus Myoplasmic Ca 2 Fused tetanus Force AP Time Frequency Summation of Twitches and Tetanus Myoplasmic [Ca 2+] Fused tetanus Force AP Time](https://slidetodoc.com/presentation_image_h2/5746c7037bef48ecc756b3ab9f29f915/image-29.jpg)
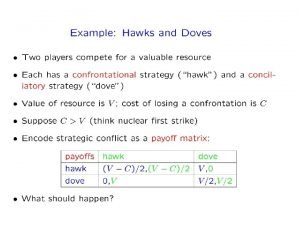
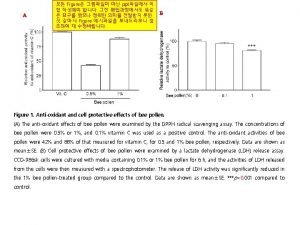
Frequency Summation of Twitches and Tetanus Myoplasmic [Ca 2+] Fused tetanus Force AP Time (1 second) • Myoplasmic Ca 2+ falls (initiating relaxation) before development of maximal contractile force • If the muscle is stimulated before complete relaxation has occurred the new twitch will sum with the previous one etc. • If action potential frequency is sufficiently high, the individual contractions are not resolved and a ‘fused tetanus’ contraction is recorded. Copyright © 2006 by Elsevier, Inc.
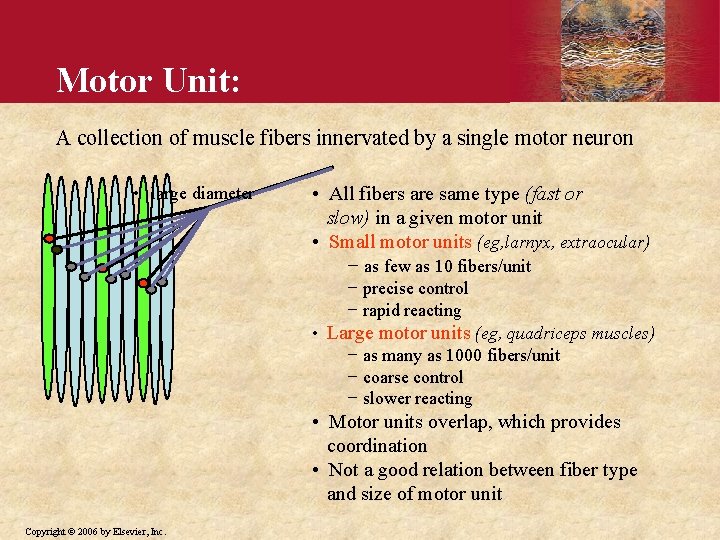
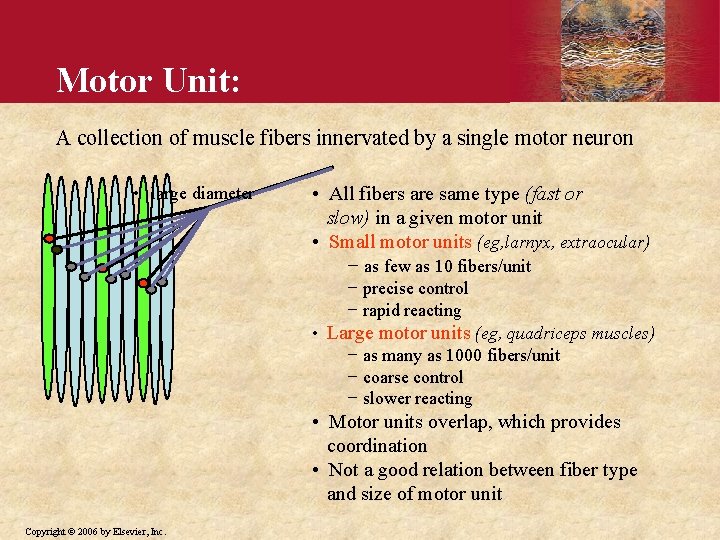
Motor Unit: A collection of muscle fibers innervated by a single motor neuron • large diameter • All fibers are same type (fast or slow) in a given motor unit • Small motor units (eg, larnyx, extraocular) − as few as 10 fibers/unit − precise control − rapid reacting • Large motor units (eg, quadriceps muscles) − as many as 1000 fibers/unit − coarse control − slower reacting • Motor units overlap, which provides coordination • Not a good relation between fiber type and size of motor unit Copyright © 2006 by Elsevier, Inc.
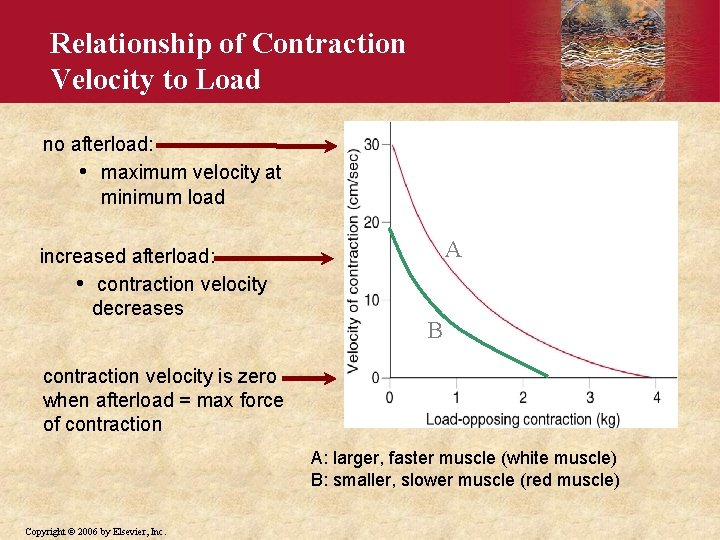
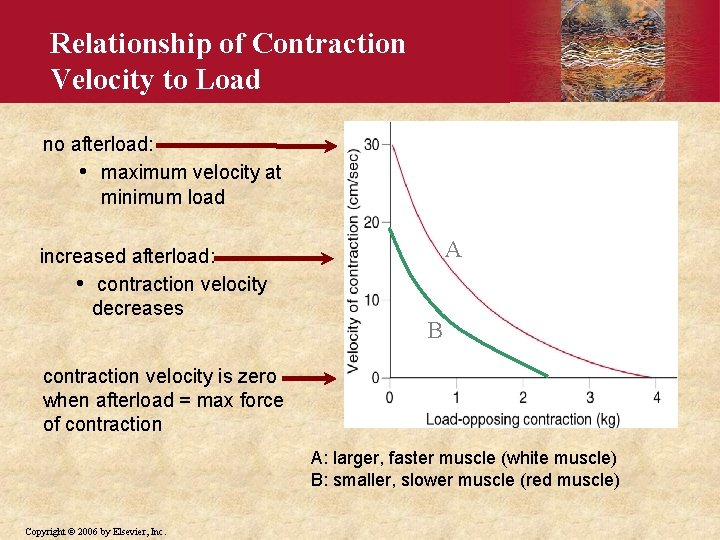
Relationship of Contraction Velocity to Load no afterload: • maximum velocity at minimum load increased afterload: • contraction velocity decreases A B contraction velocity is zero when afterload = max force of contraction A: larger, faster muscle (white muscle) B: smaller, slower muscle (red muscle) Copyright © 2006 by Elsevier, Inc.
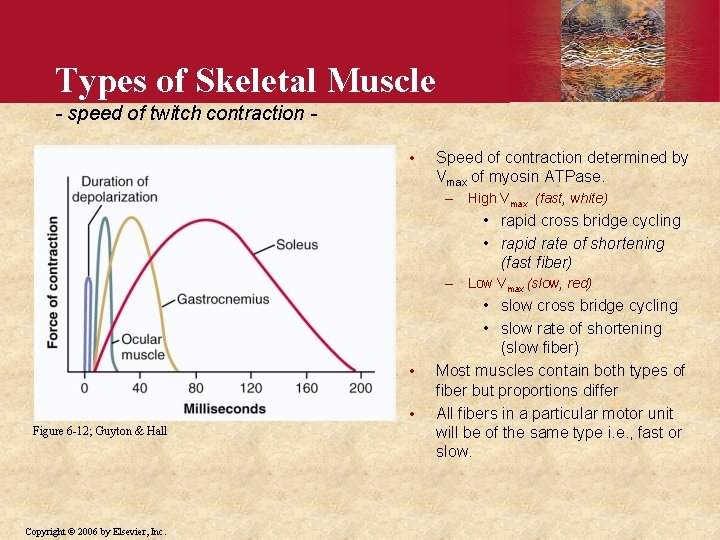
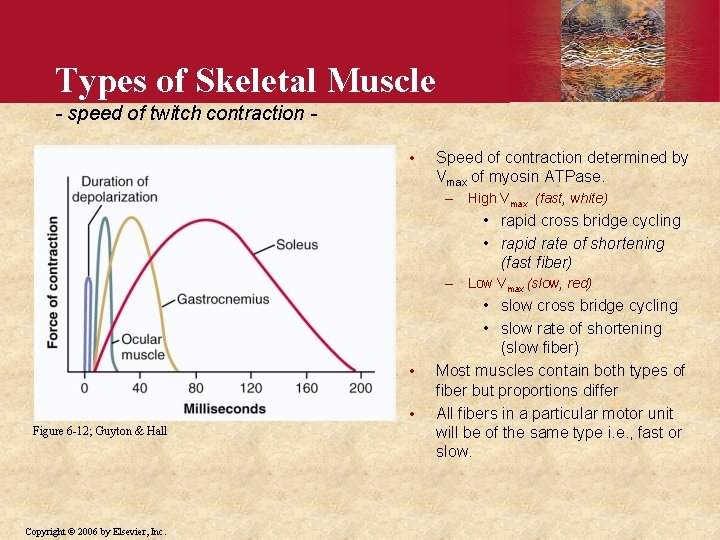
Types of Skeletal Muscle - speed of twitch contraction • Speed of contraction determined by Vmax of myosin ATPase. – High Vmax (fast, white) • rapid cross bridge cycling • rapid rate of shortening (fast fiber) – Low Vmax (slow, red) • • Figure 6 -12; Guyton & Hall Copyright © 2006 by Elsevier, Inc. • slow cross bridge cycling • slow rate of shortening (slow fiber) Most muscles contain both types of fiber but proportions differ All fibers in a particular motor unit will be of the same type i. e. , fast or slow.
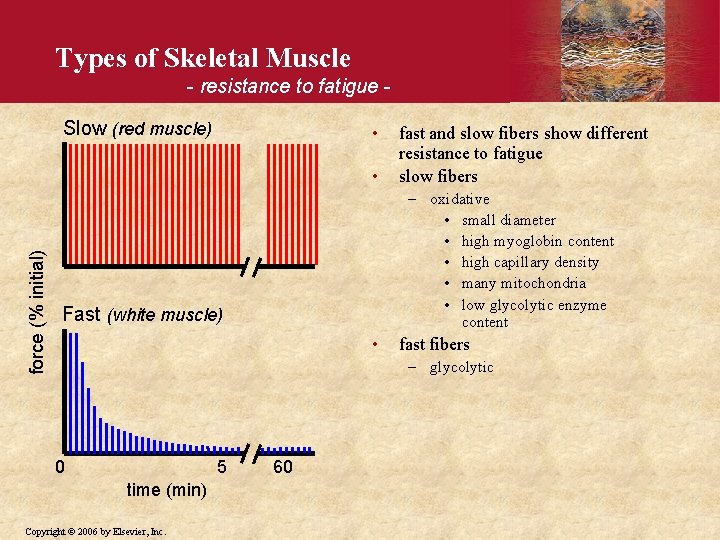
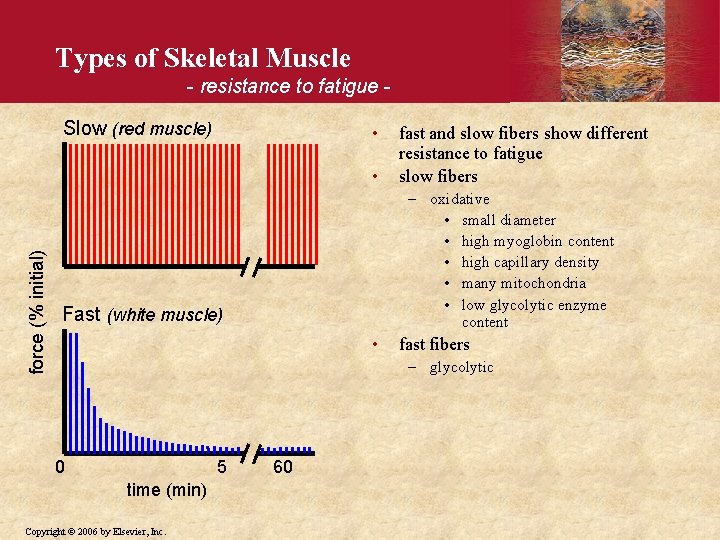
Types of Skeletal Muscle - resistance to fatigue Slow (red muscle) • force (% initial) • fast and slow fibers show different resistance to fatigue slow fibers – oxidative • small diameter • high myoglobin content • high capillary density • many mitochondria • low glycolytic enzyme content Fast (white muscle) • fast fibers – glycolytic 0 5 time (min) Copyright © 2006 by Elsevier, Inc. 60
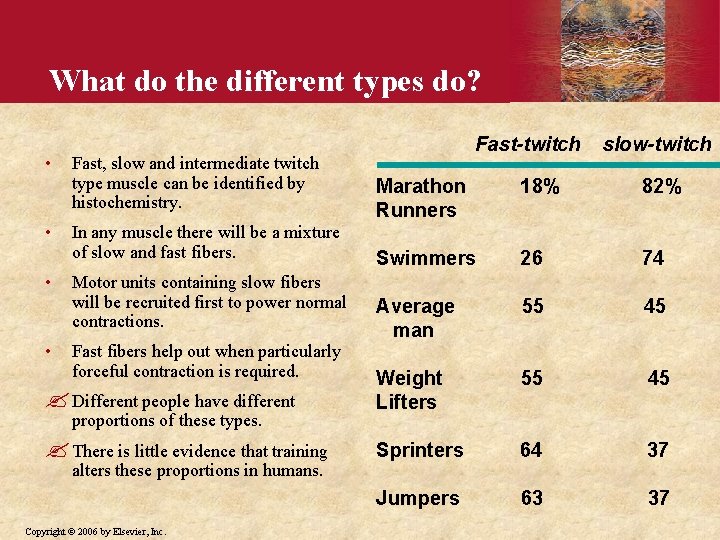
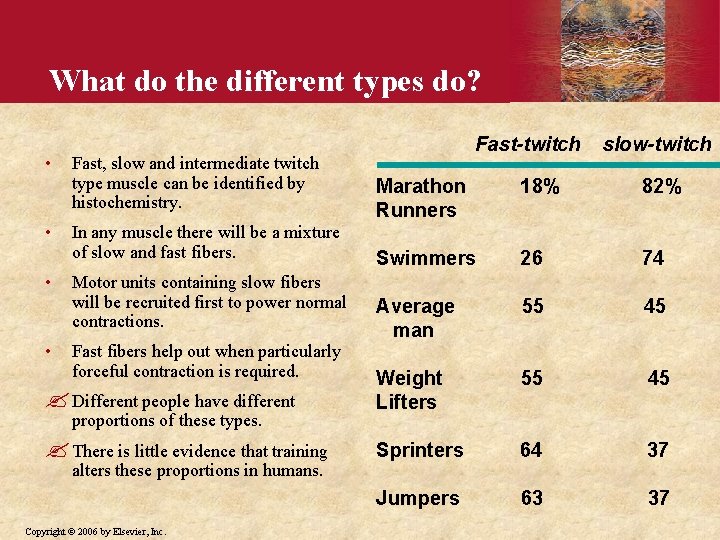
What do the different types do? • Fast, slow and intermediate twitch type muscle can be identified by histochemistry. Fast-twitch slow-twitch Marathon Runners 18% 82% Swimmers 26 74 Average man 55 45 ? Different people have different Weight Lifters 55 45 ? There is little evidence that training Sprinters 64 37 Jumpers 63 37 • • • In any muscle there will be a mixture of slow and fast fibers. Motor units containing slow fibers will be recruited first to power normal contractions. Fast fibers help out when particularly forceful contraction is required. proportions of these types. alters these proportions in humans. Copyright © 2006 by Elsevier, Inc.
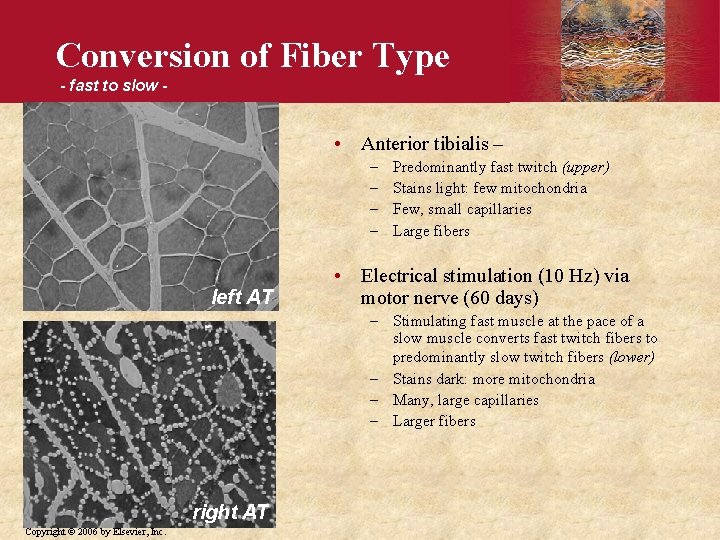
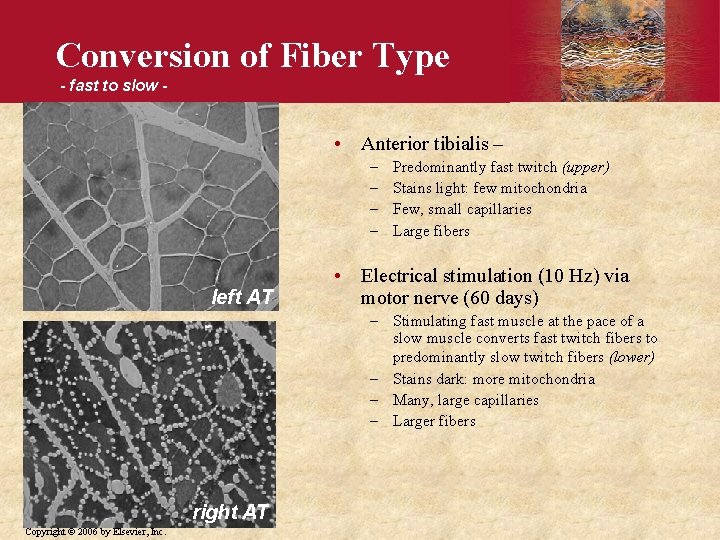
Conversion of Fiber Type - fast to slow - • Anterior tibialis – – – left AT Predominantly fast twitch (upper) Stains light: few mitochondria Few, small capillaries Large fibers • Electrical stimulation (10 Hz) via motor nerve (60 days) – Stimulating fast muscle at the pace of a slow muscle converts fast twitch fibers to predominantly slow twitch fibers (lower) – Stains dark: more mitochondria – Many, large capillaries – Larger fibers right AT Copyright © 2006 by Elsevier, Inc.
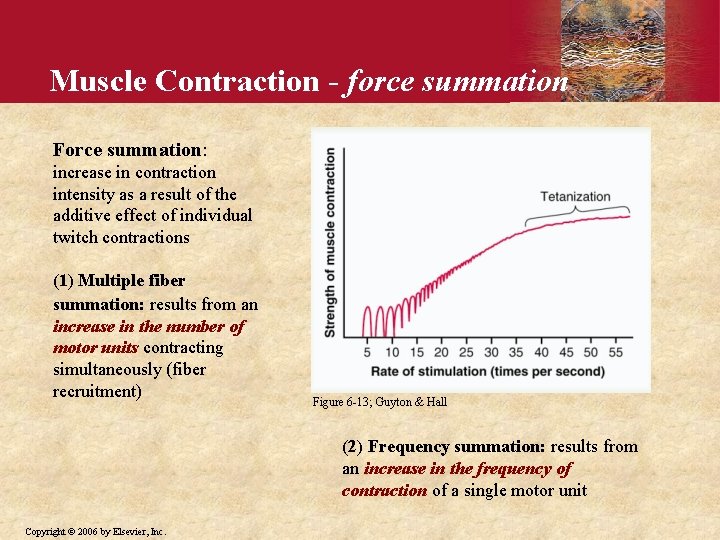
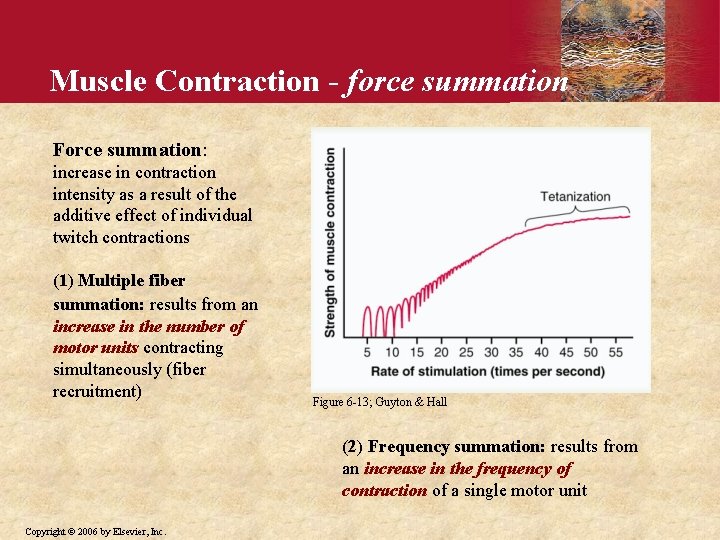
Muscle Contraction - force summation Force summation: increase in contraction intensity as a result of the additive effect of individual twitch contractions (1) Multiple fiber summation: results from an increase in the number of motor units contracting simultaneously (fiber recruitment) Figure 6 -13; Guyton & Hall (2) Frequency summation: results from an increase in the frequency of contraction of a single motor unit Copyright © 2006 by Elsevier, Inc.
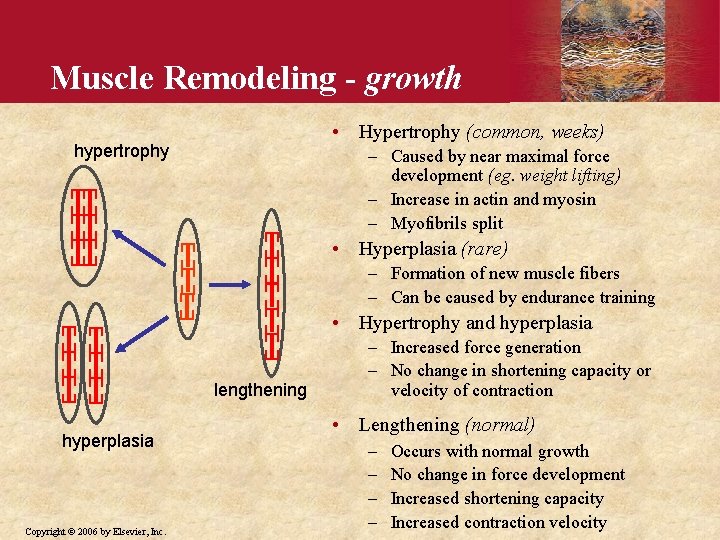
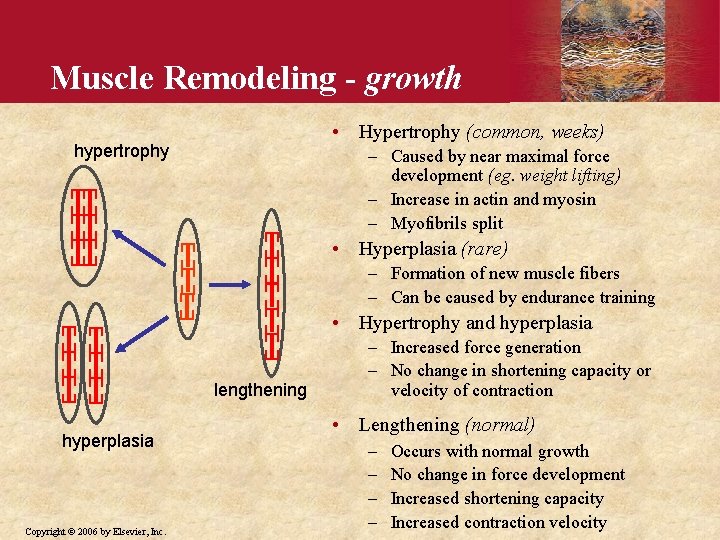
Muscle Remodeling - growth • Hypertrophy (common, weeks) hypertrophy – Caused by near maximal force development (eg. weight lifting) – Increase in actin and myosin – Myofibrils split • Hyperplasia (rare) – Formation of new muscle fibers – Can be caused by endurance training • Hypertrophy and hyperplasia lengthening hyperplasia Copyright © 2006 by Elsevier, Inc. – Increased force generation – No change in shortening capacity or velocity of contraction • Lengthening (normal) – – Occurs with normal growth No change in force development Increased shortening capacity Increased contraction velocity
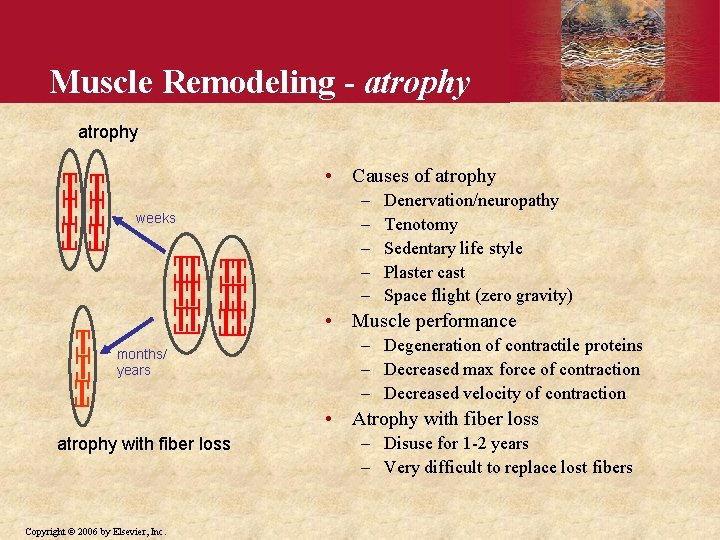
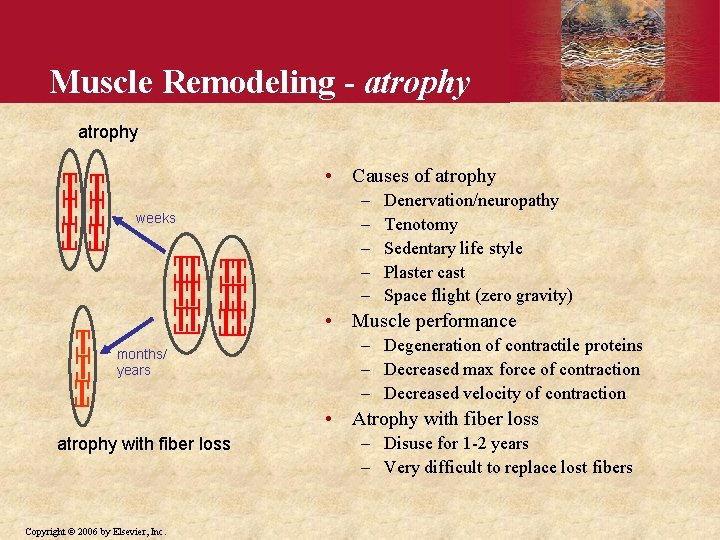
Muscle Remodeling - atrophy • Causes of atrophy weeks – – – Denervation/neuropathy Tenotomy Sedentary life style Plaster cast Space flight (zero gravity) • Muscle performance months/ years – Degeneration of contractile proteins – Decreased max force of contraction – Decreased velocity of contraction • Atrophy with fiber loss atrophy with fiber loss Copyright © 2006 by Elsevier, Inc. – Disuse for 1 -2 years – Very difficult to replace lost fibers
 Guyton
GuytonErythropoiesis guyton
 Ecg guyton
Ecg guyton Loi de starling coeur
Loi de starling coeur Blood physiology guyton
Blood physiology guyton Animal physiology guyton
Animal physiology guyton Mineralocorticoid function
Mineralocorticoid function Copyright 2005 pearson prentice hall inc
Copyright 2005 pearson prentice hall inc Stuart hall audience theory
Stuart hall audience theory Levi strauss media theory
Levi strauss media theory Identify the type of congruence transformation
Identify the type of congruence transformation 4 figure and 6 figure grid references
4 figure and 6 figure grid references Rigid transformation review
Rigid transformation review Pentagon plane figure or solid figure
Pentagon plane figure or solid figure Theory x and theory y
Theory x and theory y Convergent boundary divergent boundary transform boundary
Convergent boundary divergent boundary transform boundary Wallerstein's world systems theory
Wallerstein's world systems theory Sensation
Sensation Criticism of dependency theory
Criticism of dependency theory Continental drift theory and plate tectonics theory
Continental drift theory and plate tectonics theory Describe the trichromatic theory of color vision.
Describe the trichromatic theory of color vision. Neo classical organizational theory
Neo classical organizational theory Theory x and theory y of motivation
Theory x and theory y of motivation Hawthorne motivation
Hawthorne motivation Continuity theory vs activity theory
Continuity theory vs activity theory Continuity theory vs activity theory
Continuity theory vs activity theory Explain the keynesian theory of employment
Explain the keynesian theory of employment Opponent process theory vs trichromatic theory
Opponent process theory vs trichromatic theory Theoretical plates
Theoretical plates Lien theory vs title theory
Lien theory vs title theory Binocular cues
Binocular cues Lien theory vs title theory
Lien theory vs title theory Continuity theory vs activity theory
Continuity theory vs activity theory Classical versus keynesian economics
Classical versus keynesian economics Y management
Y management Trait theory vs social cognitive theory
Trait theory vs social cognitive theory Neoclassical growth theory vs. endogenous growth theory
Neoclassical growth theory vs. endogenous growth theory Game theory and graph theory
Game theory and graph theory Critical theory of crime
Critical theory of crime