Transfemoral TAVI using the selfexpanding Acurate neo prosthesis
![Predictors of paravalvular leak ≥ 2° Odds ratio [95% CI] p Threshold Calcium volume Predictors of paravalvular leak ≥ 2° Odds ratio [95% CI] p Threshold Calcium volume](https://slidetodoc.com/presentation_image_h/73c3aa0e69e3e14c7b83aee593df5598/image-8.jpg)
- Slides: 11
Transfemoral TAVI using the self-expanding Acurate neo prosthesis: a comprehensive analysis of anatomic and procedure related predictors of more-than-mild paravalvular leakage Won-Keun Kim*a, b, c, Helge Möllmann*d, Christoph Liebetraua, c, Matthias Renkera, Andreas Rolfa, c, Mirko Dossb, Christian Hamma, c, Thomas Walthere Kerckhoff Heart Center, a. Dep. of Cardiology, b. Dep. of Cardiac Surgery, Bad Nauheim, Germany c. Justus-Liebig University of Giessen, Dep. of Cardiology, Giessen, Germany d. St. Johannes Hospital, Dep. of Cardiology, Dortmund, Germany e. Johann-Wolfgang-Goethe Universität, Dep. of Cardiac Surgery, Frankfurt, Germany
Conflicts of interest • W. K. : Proctor for Symetis SA, St. Jude Medical/Abbott, lecture honoraria from Symetis SA, St. Jude Medical/Abbott • C. L. : lecture honoraria from Abbott, Astra Zeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Daiichi-Sankyio, and Pfizer – Bristol-Myers Squibb; travel accommodation/meeting expenses from Bayer and Daiichi-Sankyo • M. R. : lecture honoraria from St. Jude Medical/Abbott, travel accomodation/meeting expenses from Daiichi-Sankyo • A. R. : lecture honoraria from Astra Zeneca, Boehringer, Pfizer, MSD, Bristol Myers Squibb. • M. D. : Proctor for St. Jude Medical/Abbott. • C. H. : Advisory board Medtronic. • H. M. : Proctor fees and/or speaker honoraria from Abbott, Biotronic, Edwards Lifesciences, St. Jude Medical, Symetis SA. • All other authors declare that they have no conflict of interest.
Background & Aims • The Acurate neo TAVI prosthesis is increasingly used, but anatomic and procedural factors of paravalvular leakage ≥ 2° (around 4%)1 are poorly understood. We present • a large single center experience (n=500) using this device • a comprehensive analysis of anatomic and procedure related predictors of paravalvular leakage ≥ 2° • learning curve effect 1 Möllmann et al, Eurointervention 2017; 13, 7.
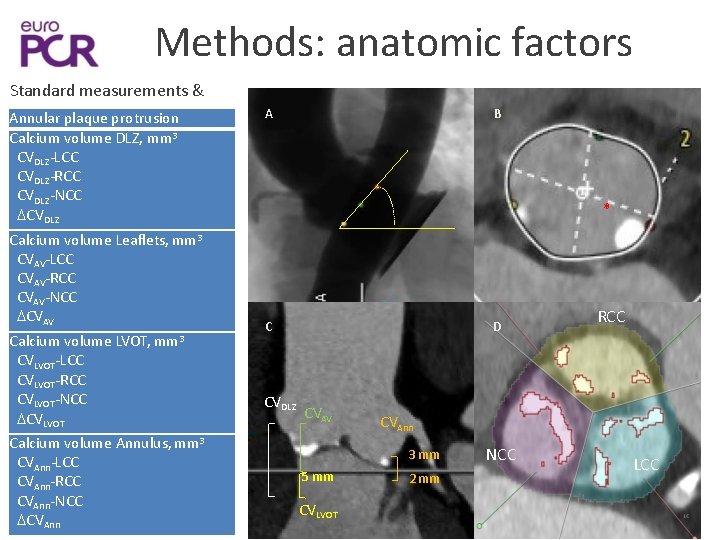
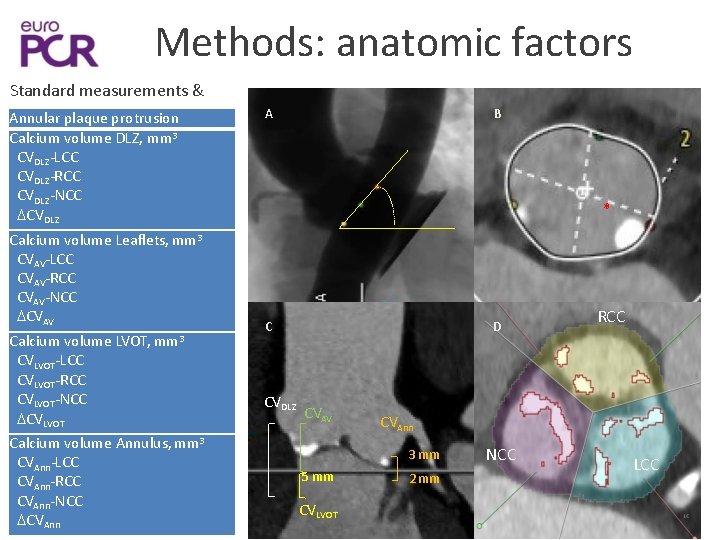
Methods: anatomic factors Standard measurements & Annular plaque protrusion Calcium volume DLZ, mm 3 CVDLZ-LCC CVDLZ-RCC CVDLZ-NCC CVDLZ Calcium volume Leaflets, mm 3 CVAV-LCC CVAV-RCC CVAV-NCC CVAV Calcium volume LVOT, mm 3 CVLVOT-LCC CVLVOT-RCC CVLVOT-NCC CVLVOT Calcium volume Annulus, mm 3 CVAnn-LCC CVAnn-RCC CVAnn-NCC CVAnn A B * C CVDLZ D CVAV CVAnn 3 mm 5 mm CVLVOT RCC 2 mm NCC LCC
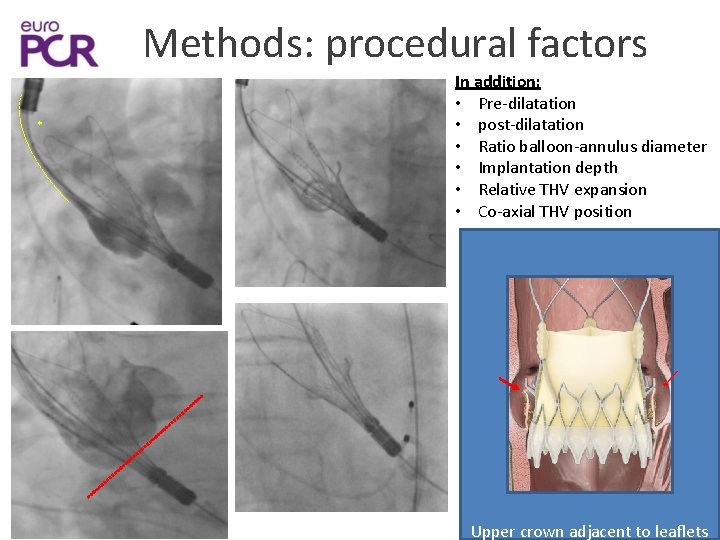
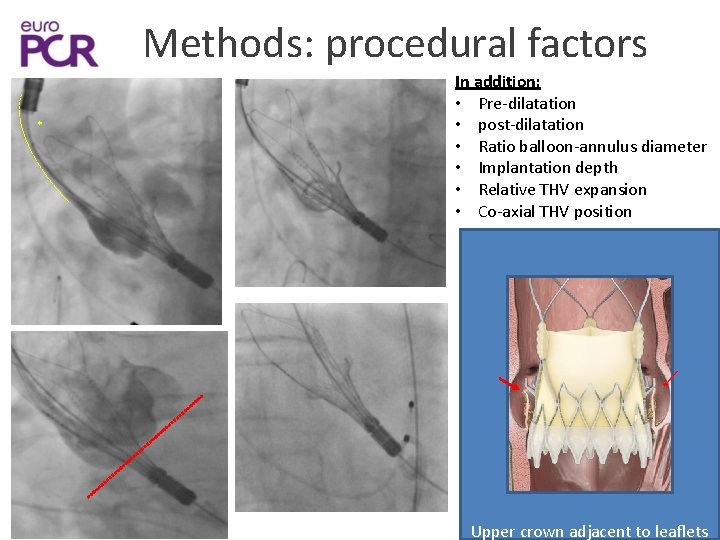
Methods: procedural factors * In addition: • Pre-dilatation • post-dilatation • Ratio balloon-annulus diameter • Implantation depth • Relative THV expansion • Co-axial THV position Upper crown adjacent to leaflets
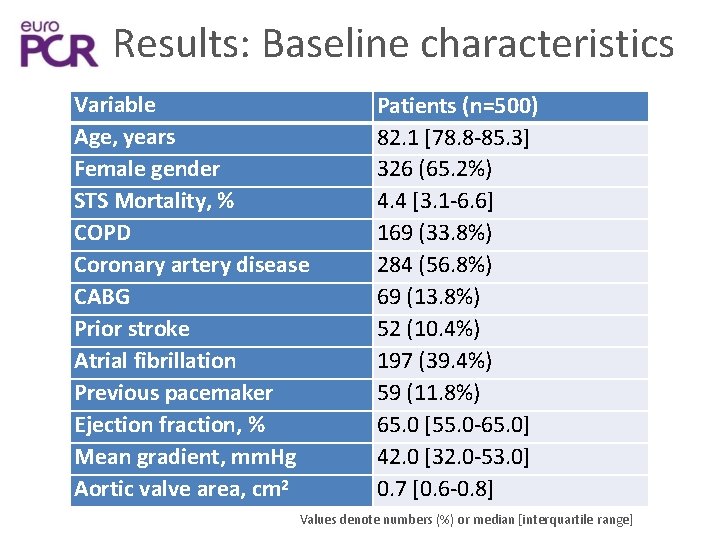
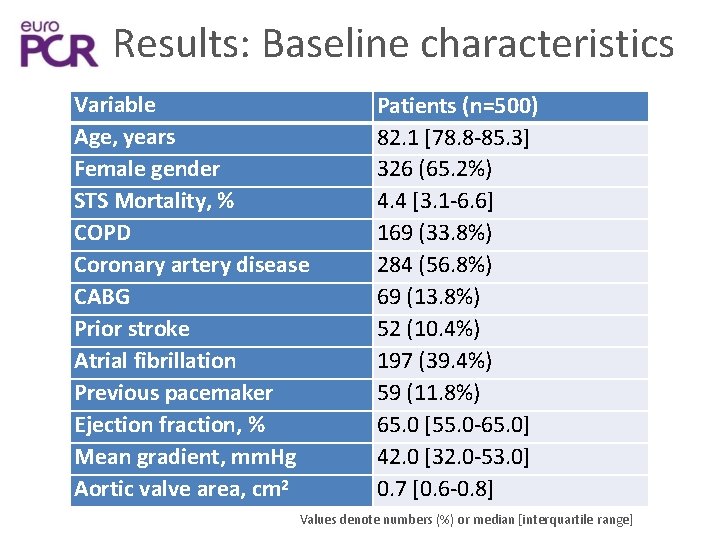
Results: Baseline characteristics Variable Age, years Female gender STS Mortality, % COPD Coronary artery disease CABG Prior stroke Atrial fibrillation Previous pacemaker Ejection fraction, % Mean gradient, mm. Hg Aortic valve area, cm 2 Patients (n=500) 82. 1 [78. 8 -85. 3] 326 (65. 2%) 4. 4 [3. 1 -6. 6] 169 (33. 8%) 284 (56. 8%) 69 (13. 8%) 52 (10. 4%) 197 (39. 4%) 59 (11. 8%) 65. 0 [55. 0 -65. 0] 42. 0 [32. 0 -53. 0] 0. 7 [0. 6 -0. 8] Values denote numbers (%) or median [interquartile range]
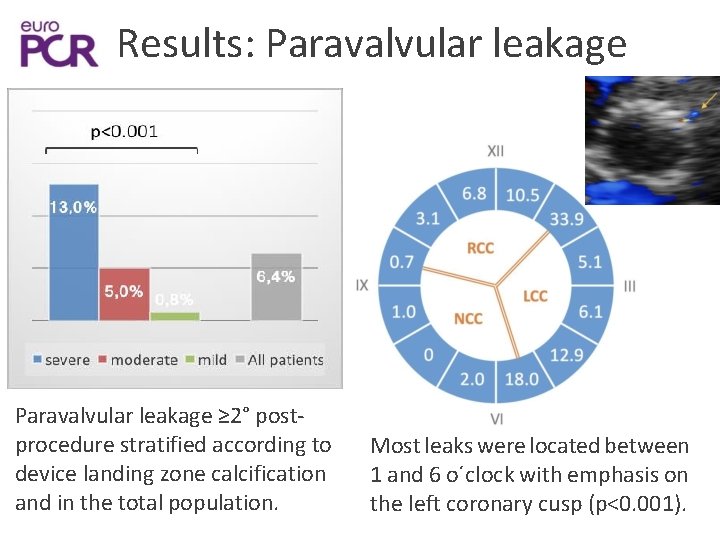
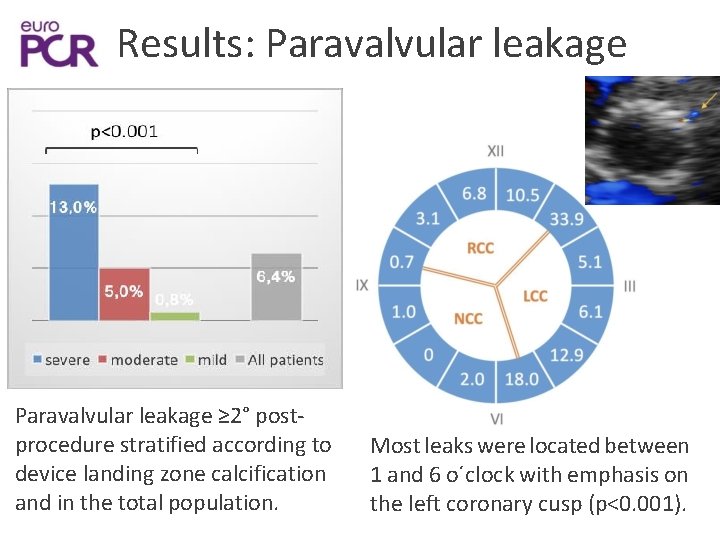
Results: Paravalvular leakage ≥ 2° postprocedure stratified according to device landing zone calcification and in the total population. Most leaks were located between 1 and 6 o´clock with emphasis on the left coronary cusp (p<0. 001).
![Predictors of paravalvular leak 2 Odds ratio 95 CI p Threshold Calcium volume Predictors of paravalvular leak ≥ 2° Odds ratio [95% CI] p Threshold Calcium volume](https://slidetodoc.com/presentation_image_h/73c3aa0e69e3e14c7b83aee593df5598/image-8.jpg)
Predictors of paravalvular leak ≥ 2° Odds ratio [95% CI] p Threshold Calcium volume annulus, mm 3 1. 006 [1. 003 -1. 010] <0. 001 97 mm 3 Annular plaque protrusion 2. 895 [1. 212 -6. 913] 0. 017 NA Cover index. Perimeter 0. 881 [0. 781 -0. 994] 0. 04 4. 4% Sinotubular junction height, mm 1. 169 [1. 022 -1. 337] 0. 04 21. 5 mm Aortic movement of the delivery 5. 593 [1. 299 -24. 071] 0. 02 system after deployment NA Peri-annular region Cover Index. Perimeter=100 × (prosthesis diameter-perimeter derived annulus)/prosthesis diameter)
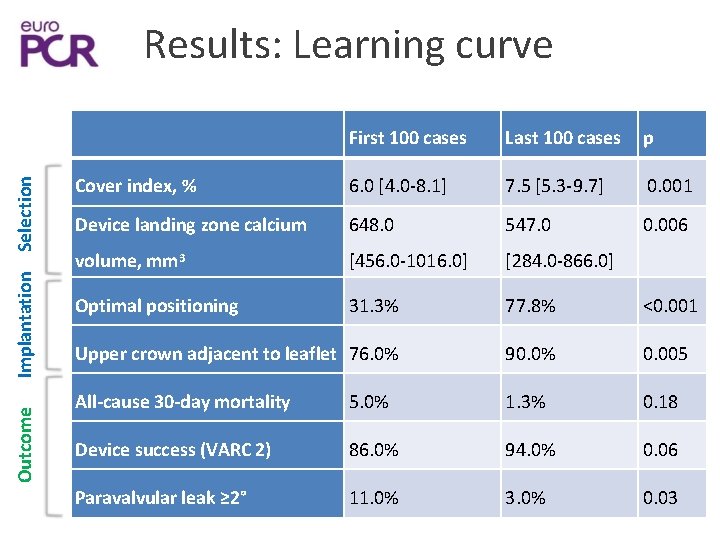
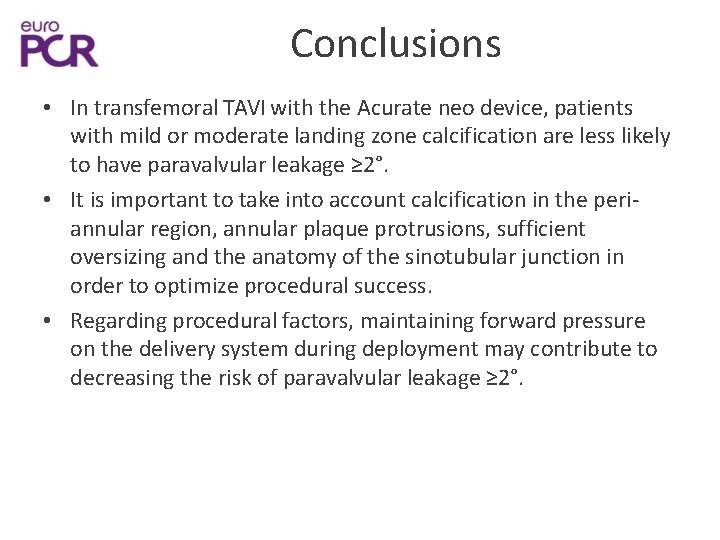
Outcome Implantation Selection Results: Learning curve First 100 cases Last 100 cases p Cover index, % 6. 0 [4. 0 -8. 1] 7. 5 [5. 3 -9. 7] 0. 001 Device landing zone calcium 648. 0 547. 0 0. 006 volume, mm 3 [456. 0 -1016. 0] [284. 0 -866. 0] Optimal positioning 31. 3% 77. 8% <0. 001 Upper crown adjacent to leaflet 76. 0% 90. 0% 0. 005 All-cause 30 -day mortality 5. 0% 1. 3% 0. 18 Device success (VARC 2) 86. 0% 94. 0% 0. 06 Paravalvular leak ≥ 2° 11. 0% 3. 0% 0. 03
Conclusions • In transfemoral TAVI with the Acurate neo device, patients with mild or moderate landing zone calcification are less likely to have paravalvular leakage ≥ 2°. • It is important to take into account calcification in the periannular region, annular plaque protrusions, sufficient oversizing and the anatomy of the sinotubular junction in order to optimize procedural success. • Regarding procedural factors, maintaining forward pressure on the delivery system during deployment may contribute to decreasing the risk of paravalvular leakage ≥ 2°.
euro PCR J A CC C AR D I O V A SC U L A R I N TE R VE N T I O N S VOL. ■. N O. ■ , 2 0 18 <C>2 0 18 B Y T H E A M E R I CA N C O L L EG E OF C A RD I O L OGY F O U N D A T I ON P U B LI SHE D B Y E L SE V I ER The ACURATE Neo Transcatheter Heart Valve A Comprehensive Analysis of Predictors of Procedural Outcome Won-Keun Kim, MDa, , , bc Helge Mo llm an n, MD, PHD, <l. Christoph Liebetr au, MD, Pn. Da, , c. Matthias Renker, MD, a And reas Rolf , MD, PHD, ac • Philippe Simon / Arnaud Van Linden, MDe, Mani Arsalan, MD/ Mir ko Doss , MD, PHDb, Christia n W. Hamm, MD, Pn. Da, , c Thomas Walther, MD, PHDe ABSTRACT OBJECTIVES The aim of th is study was to perform a comprehensive analysis of factors that affect procedural outcomes of tran scathet er aortic val ve replacement using the ACURATE neo prosthesis (Symet is/Bost on, Ecublens, Switzerland). BACKGROUND Predi ctors of p rocedural outcomes usin g the ACURATE neo prosthesis ar e poorly understood. METHODS A t ot al of 500 patients underwent t ransfemoral ao rt ic val ve replacement with t he ACURATE neo prosthes is. Device lan ding zone calcificat ion was strat ified as severe, moderate, or mild. Anat omic and procedural pred ict ors of second -degree or greater paravalvular leakage and permanent pacemaker implant at ion were assessed. RESULTS Post-p rocedural second-deg ree or greater par ava l vular leakage was more frequent with increasing device landing zone cal cificat ion (mil d 0. 8% vs. moderate 5. 0% vs. severe 13. 0%, p < 0. 0 01), whereas permanent pacemaker implant at ion was indepen dent of device landing zone calcificat ion. More severe periannular cal cificat ion (odds rati o [OR] : 1. 0 0 7; 95% confidence interva l [C l ] : 1. 0 03 to 1. 010 ; p < 0. 0 01), less oversizing (OR: 0. 867; 95% Cl: 0. 773 to 0. 971; p = 0. 014), the presence of annular plaque prot rusions (OR: 2. 756; 95% Cl: 1. 138 to 6. 670 ; p of the deli very system after full deployment (OR: 5. 593; 95% Cl: 1. 299 to 24. 076; p = 0. 025), and aortic movement = 0. 02), and sinotubular junction height (OR: 1. 156; 95% Cl: 1. 007 to 1. 328; p = 0. 04) independently predict ed second-degree or greater paravalvular leakage. Predictors of permanent pacemaker implantat ion were pre -exist ing right bundle branch block (OR: 3. 122; 95% Cl: 1. 261 to 7. 731; p = 0. 01) and more oversizing (OR: 1. 111; 95% Cl: 1. 009 to 1. 222; p = 0. 0 3).