Traditional Knee Replacement Versus Minimally Invasive Knee Replacement


- Slides: 22
Traditional Knee Replacement Versus Minimally Invasive Knee Replacement in the Treatment of Osteoarthritis Jeremy Waddell, PA-S Prof. David Fahringer, Advisor 3/23/2006
Objectives n n Understand the basic pathophysiology of osteoarthritis of the knee. Understand how osteoarthritis affects the patient. Know the differences between traditional and minimally invasive knee replacement surgery. Understand why this information is important to the future PA.
Osteoarthritis (OA) Also known as “Degenerative Joint Disease” n Causes intense pain which decreases the patient’s activity. n Affects more than 20 million people in the U. S. and 10% of adults over the age of 50. n
A myth about OA is that it is a process of aging resulting in “wear and tear” of articular cartilage. n Studies show that OA is not just a result of aging, but instead is a disease process. n – Denatured type II collagen is found in both normal and OA cartilage. – Degradative enzyme activity is increased with OA vs. normal aging cartilage.
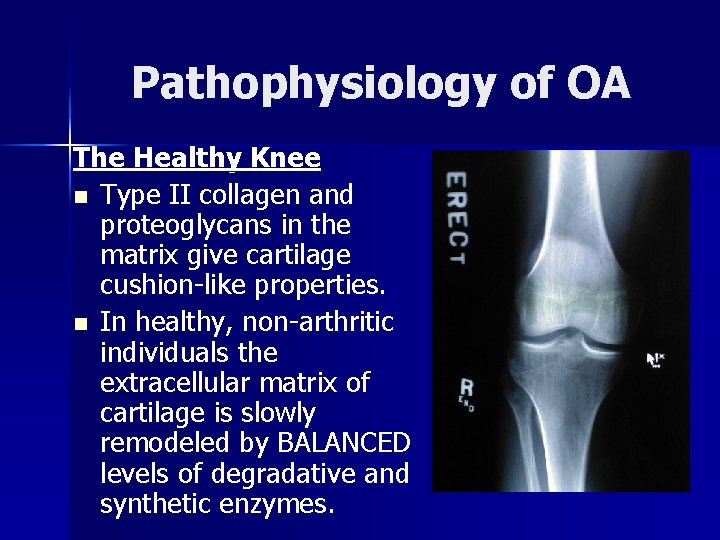
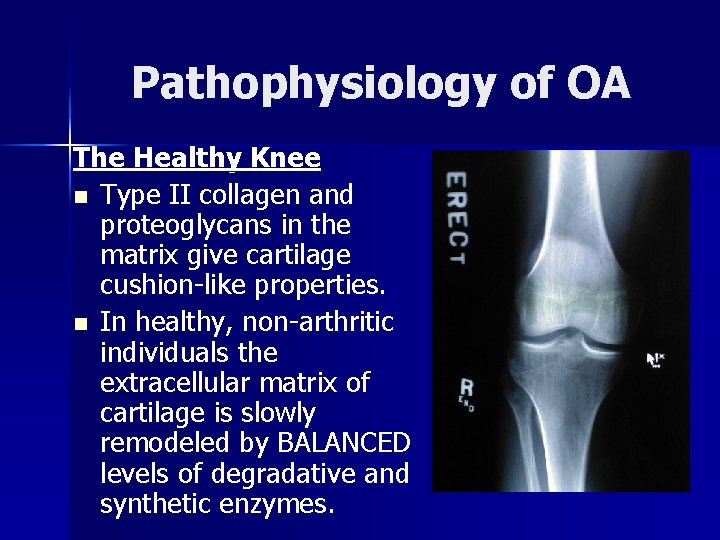
Pathophysiology of OA The Healthy Knee n Type II collagen and proteoglycans in the matrix give cartilage cushion-like properties. n In healthy, non-arthritic individuals the extracellular matrix of cartilage is slowly remodeled by BALANCED levels of degradative and synthetic enzymes.
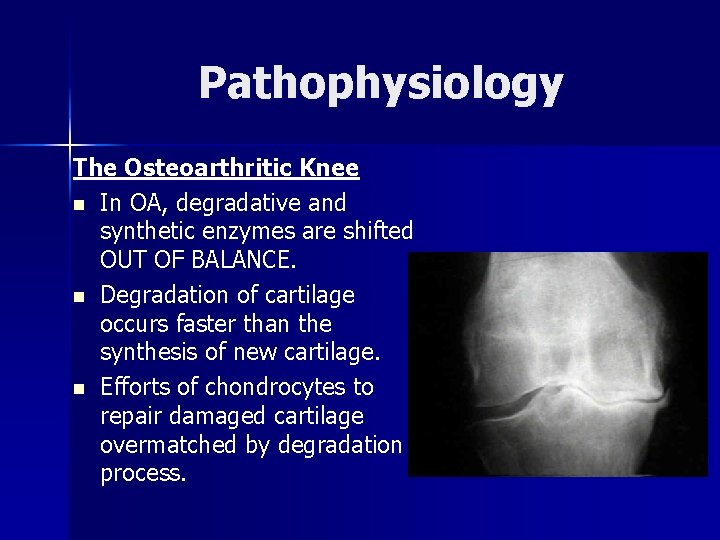
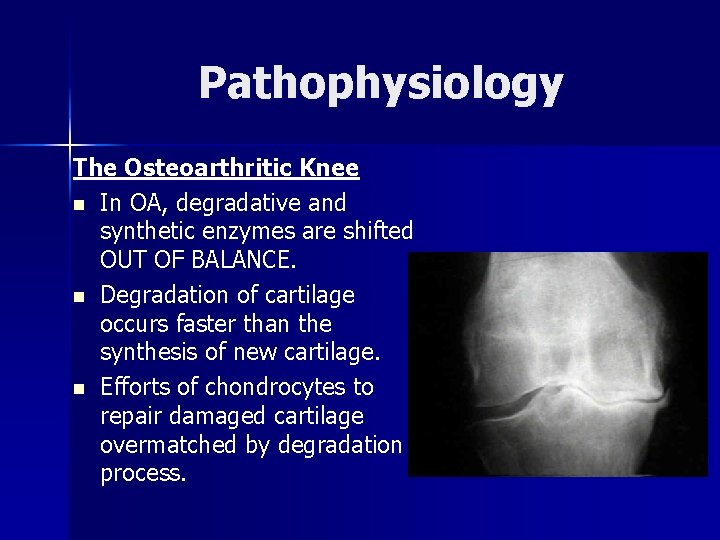
Pathophysiology The Osteoarthritic Knee n In OA, degradative and synthetic enzymes are shifted OUT OF BALANCE. n Degradation of cartilage occurs faster than the synthesis of new cartilage. n Efforts of chondrocytes to repair damaged cartilage overmatched by degradation process.
How does OA affect the patient? Loss of cartilage leaves the joint without its protective cartilage. n Patient is left with a “grinding” between the femur and tibia causing pain. n Patients complain that they are no longer able to participate in activities they enjoy. n
How does OA affect the patient? n Patient may experience depression, muscle atrophy, and social withdrawal due to inactivity. n OA can cause great amounts of stress to the patient and the patient’s family.
Treatments for OA Many treatment modalities are available to the patient with OA. n Treatments include: analgesia, supplementation, injections, strengthening exercises, physical therapy, and yoga. n BUT, there is only one definitive cure for OA…joint replacement therapy. n
Why do patients seek joint replacement? When the patient is unable to participate in chosen activities, they feel that their quality of life is affected. n Patients who “can’t sleep, can’t work, and can’t walk” are good candidates for joint replacement surgery n
Traditional Knee Replacement n n Developed in the 1950 s Currently, performed on over 300, 000 people each year Large 18 -20 cm incision gives surgeon a great view of the joint and provides large workspace for prosthesis placement. Anesthesia times average approximately 1. 5 hours.
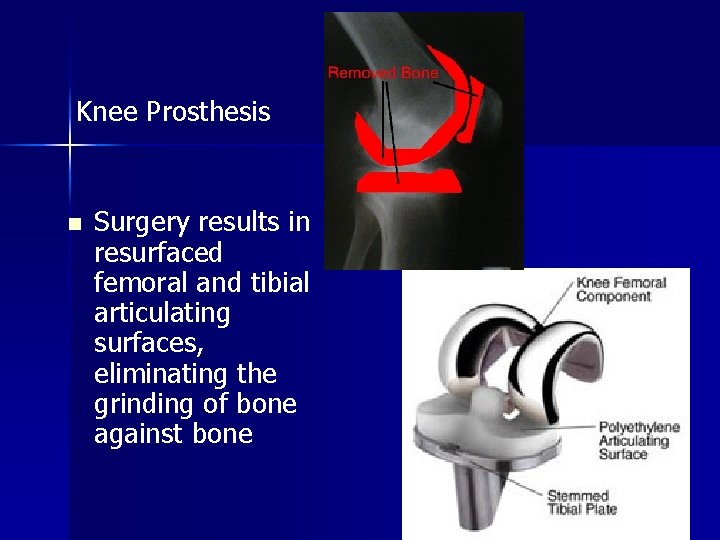
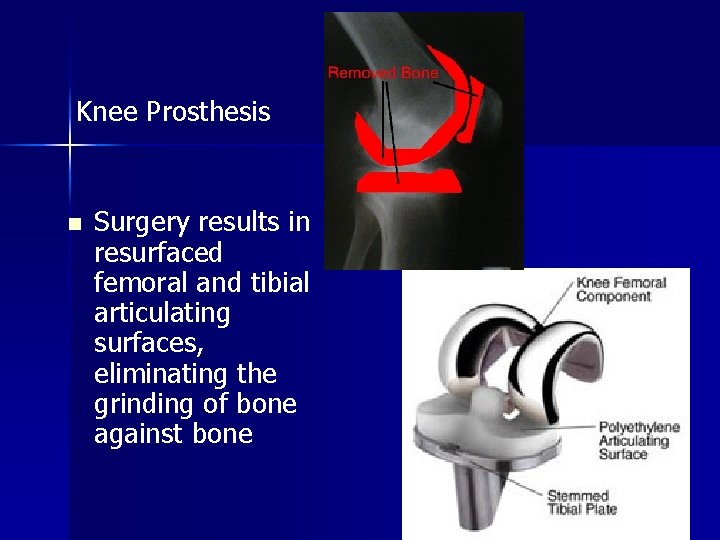
Knee Prosthesis n Surgery results in resurfaced femoral and tibial articulating surfaces, eliminating the grinding of bone against bone

Traditional Knee Replacement
Traditional Knee Replacement After reviewing 20 years of data, the NIH found that approximately 90% of patients who undergo traditional total knee replacement experience great reductions in pain. n 85% of knee replacement patients stated that they were satisfied with the outcome of their procedure n
Study conducted by Peter Thadani, M. D. n n 10 -12 year follow-up of 86 patients (49 women and 37 men; ages 45 -89), who he had performed a total knee replacement on between September 1986 and November 1988. Average preoperative functioning score of these patients’ knees was 55 on a scale of 0 -100. These patients rated their knee function as an average of 80. 6 after surgery. ROM increased 100 degrees prior to surgery to 111 degrees 10 -12 years after surgery.
Minimally Invasive Knee Replacement Heavily developed since 1991. n 4 -8 cm incision results in less damage to tissue. n A smaller incision results in faster recovery and less narcotic use for patients. n Anesthesia times average approximately 3 hours. n

Comparing Incision Sizes Minimally Invasive Traditional TKR
Study of Minimally Invasive Knee Replacements (Richard Laskin) n n n 58 TKR were performed via minimally invasive approach. Proposed that a minimally invasive approach would limit soft tissue disruption, speed recovery time, diminish blood loss, and decrease post-operative pain. Study was performed with a retrospective control group who had traditional knee replacement surgery
Pain was reported to be considerably lower in the minimally invasive group than in the traditional knee replacement group. n Total use of morphine by the minimally invasive group was 55 mg versus 118 mg by the traditional group. n Interestingly, blood loss was greater in patients undergoing minimally invasive surgery at 713 m. L compared to 573 m. L in the traditional knee replacement group n
Conclusion n n Patients report high satisfaction rates with both types of total knee replacement. Reduction of cost, hospitalization, post-op pain, and a decrease in the length of rehabilitation will push further development of minimally invasive procedures. Longer anesthesia times and increased blood loss with minimally invasive procedures are a concern. New procedures present learning curve to surgeons. Total knee replacement can greatly improve patients’ quality of life.
Why is this important to the future PA? n n n The “aging of America” will cause osteoarthritis to be one of the most common chief complaints of our future patients. Cost effectiveness and a decrease in hospitalization time will probably cause minimally invasive knee replacement to become quite popular. Knee replacement can greatly improve patients’ quality of life.
-References available upon request-