Toxicology Phytotxicity Phytotoxicity refers to poisoning with poisonous




- Slides: 48
Toxicology
Phytotxicity Phytotoxicity refers to poisoning with poisonous plants. Why do animals consume plants which may harm them or their offsprings?
Phytotoxicity cont…. § Browsing or grazing animals may have limited access to high-quality forage at certain times of the year and are forced to survive by grazing some poisonous species. § Hay or forages harvested in areas where poisonous plants are abundant may be contaminated with a high percentage of poisonous plants.
Phytotoxicity cont…. § Phytotoxicity is often exacerbated during periods of below normal rainfall when the abundance of grasses is reduced. § Poisoning by plants only occurs when animals eat too much or too fast or graze over a prolonged period of time. § Management strategies to control these factors can minimize losses from poisonous plants.
Cyanide toxicity § Cyanide, hydrocyanic acid, hydrogen cyanide (HCN) and prussic acid are all terms relating to the same toxic principle. § Various cyanogenic glycosides, which can hydrolyze to form HCN are present in a number of plant species. § All animal species are susceptible to cyanide poisoning. § The ability of rumen microbial flora to rapidly hydrolyze cyanogenic glycosides makes ruminants particularly at risk.
Cyanade toxicity § Rumen microflora rapidly hydrolyze cyanogenic glycosides releasing HCN which is quickly absorbed and distributed to the tissues. § Cyanide ion combines with ferric iron in the cytochrome oxidase system, blocking electron transport and molecular oxygen transfer from oxyhemoglobin to tissues.
Cyanade toxicity § This is a reversible action. § The effect is cellular hypoxia or histotoxic anoxia. § Oxygen is not released from oxyhemoglobin to the tissues and the bright red color remains in venous blood. § The process, from ingestion of a toxic dose to onset of clinical signs can occur within a few minutes.
Cyanade toxicity clinical signs § Ruminants may exhibit signs within minutes to less an hour after ingestion of toxic plant material. § Onset of clinical signs is peracute and includes apprehension, pronounced polypnea then dyspnea. Initially there is stimulation of chemoreceptors in the carotid body and respiratory centers. § The pupils dilate, mucous membranes may be pink and venous blood a bright cherry red. weakness, voiding of urine, collapse, paddling and death follow within a few minutes.
Cyanade toxicity §Lesions are few. §Acute toxicosis §Mucous membranes may be pink §Venous blood bright red. § Subendocardial and subepicardial petecchial and ecchymotic hemorrhages typical of an agonal death may be present. § Chronic toxicosis § Degeneration of the white matter of the spinal cord, cerebellar peduncles and cerebellum
Cyanade toxicity Differential diagnosis of cyanide toxicosis in ruminants may include acute toxicoses nitrate–nitrites, urea–ammonia
Treatment The opportunity to treat cyanade toxicity is rare because of the peracute nature of the poisoning. Antidote - sodium nitrate in combination with sodium thiosulfate. Ruminants- sodium thiosulfate alone
Nitrate and nitrite poisoning §Ruminants are particularly at risk of acute, fatal nitrate/nitrite poisoning §Microorganisms in the rumen reduce nitrates to nitrites then ammonia for microbial growth. §Excess intake of nitrates may cause toxic levels of nitrite to accumulate and be absorbed into the blood. §Cattle graze a variety of grasses and weeds which, under certain conditions, especially excessive fertilization, can accumulate levels of nitrate that may prove toxic to
Nitrate cont… § Monogastric species are susceptible to the toxic effects of nitrites ingested as nitrites from non plant sources. § Nitrates and nitrites are water soluble and may contaminate water sources. § Forages and weeds growing in soil rich in manure waste or in holding pens are a potential source of poisoning. § Nitrate fertilizers are commonly found on farms and ranches and accidental ingestion or feed contamination does occasionally occur.
Nitrate cont… § During periods of drought the growth of forages and weeds is reduced but the roots may continue to collect and store nitrate in the stems. § Well-fertilized species, forages grown for temporary summer grazing and for hay production. Fertilized pastures of ryegrass (Lolium multiflorum), oats (Avena spp. ), turnips (Brassica rapa)
Nitrate. . § Action of the rumen flora reduces nitrate to the much more toxic nitrite which normally is converted to ammonia and further utilized by the microorganisms. § Nitrite is absorbed into the blood when the intake of nitrates and the production of nitrite exceed the capacity of the rumen flora to further reduce nitrite.
Nitrate… §The nitrite anion causes vasodilation and oxidizes ferrous iron in hemoglobin to the ferric (trivalent) state forming methemoglobin which cannot accept molecular oxygen. §As the percentage of methemoglobinemia rises oxygen starvation to tissues increases and blood becomes chocolate brown in color.
Nitrate … Clinical signs Weakness, cyanosis of mucous membranes, ataxia, increased respiratory rate, collapse and death within minutes. Blood is dark and may have brown color. Treatment- methylene blue
Photosensitization §Photosensitization is a severe dermatitis resulting from a complex reaction induced by photoreactive molecules exposed to ultraviolet (UV) sunlight in the skin of animals that have eaten certain plants. §The photoreactive molecule, also called a photosensitizer, functions as an energy transducer, facilitating the change of light energy into molecular electronic energy in the form of excited chemical species.
Photosensitization cont…. §Primary photosensitization is associated with photodynamic compounds in certain plants, which react in the non-pigmented skin with UV light to cause a severe dermatitis. §Secondary photosensitization results when an animal’s liver is sufficiently diseased and unable to remove plant by-products that can react with UV light to cause photosensitization.
Photosensitization cont. . • Secondary photosensitization is primarily caused by a variety of compounds toxic to the liver pyrrolizidine alkaloids (PAs). • Certain plant species cause secondary photosensitization through inflammation and obstruction of the biliary system. e. g. saponins cause inflammation and obstruction of the bile ducts. Phylloerythrin accumulates in the liver, the blood, and subsequently the skin, causing photosensitivity.
Clinical signs §Resembles severe sunburn of the areas of the skin that have little or no hair (nose, udder) and of areas that have light-colored skin andwhite hair. The tongue, especially the tip and the underside can be affected. §The progressive clinical manifestation of photosensitization consists of lacrimation, photophobia, erythema, pruritus, cutaneous edema, fissuring of the epithelium, necrosis, and sloughing of nonpigmented exposed skin. Corneal edema also is evident in some cases.
Diagnosis and treatment § Diagnosis of photosensitization is based on typical clinical signs and lesions restricted to lightly pigmented areas with sparse hair covering. § Treatment. Supportive and symptomatic care the only options. Secondary skin infections may be prevented with antibiotics. Animals should be provided ample shade
OXALATE POISONING § The poisoning is due to soluble (oxalic acid, acid oxalate and oxalate ion) and Insoluble (Calcium oxalate ) oxalate. § All species including man, are susceptible to intoxication: sheep and cattle succumb from nephropathy; Horses develop osteodystrophia fibrosa. § Two acute syndromes occur: death in 8– 12 h due to oxalate ion poisoning or death due to hypocalcaemia in acid oxalate and oxalic acid poisoning. § Subacute to chronic poisoning
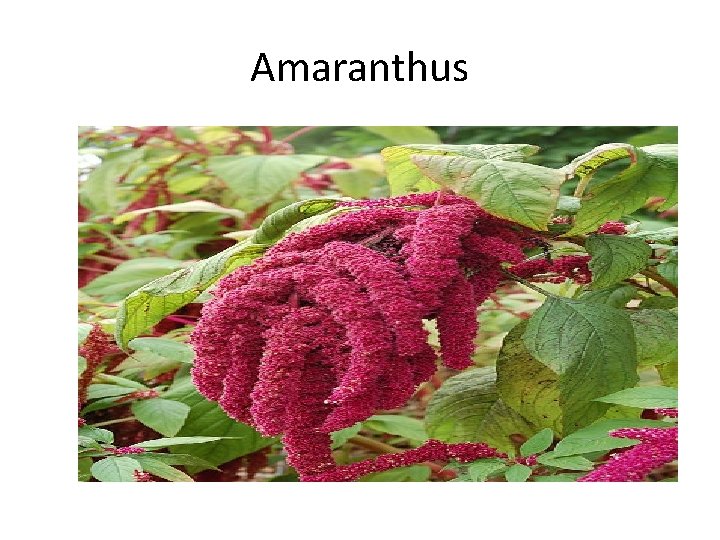
OXALATE cont § The families and genera which are of toxicological significance differ from country to country but any plant high in oxalates and eaten by animals in large quantity could be toxic. § It is often a problem in low rainfall areas where some plants are dominant and animals have to browse. § e. g. amaranthus, setaria, rumex, chenopodium
Oxalate cont… • In the normal healthy rumen , a portion of the oxalic acid and soluble oxalates can combine with calcium and become insoluble. This is in contrast to non-ruminants with a gastric p. H of 1– 2 • If the rumen is adapted by gradual exposure to oxalic acid and oxalates, microorganisms (such as Oxalobacter formigenes) can use oxalic acid as an energy source. It is only when the microbes are unable to break down oxalic acid that toxicity results
Oxalate cont… • The organ systems most commonly affected are the kidneys, GIT and neural tissue due to precipitation of calcium oxalate crystals • Inactivation of vitally essential Ca- and Mgdependent enzymes and consequent cell damage. • Oxalate competitively inhibits oxidation of lactate and non-competitively interferes with pyruvate reduction. • The exact cellular pathophysiology for cellular toxicity, has not been elucidated
Oxalate cont… • Binds to Mg that it is an essential co-factor to catalyze several enzymatic reactions, particularly those involving ATP production. • Nephrotoxicity and crystal formation, urolithiasis • Vascular damage and crystal formation in small arteries of the rumen • Hypocalcemia Hypomagnesimia • Reduced absorption of calcium and magnesium
Oxalate cont… Clinical signs • Acute toxicity in Sheep - dullness, head held low, anorexia, white froth from mouth, weakness, stiffness, rapid respiration, ataxia, comatose with extensive jerky extensor rigidity; acute toxicity in cattle is similar with sheep • Subacute incoordination, apprehension, belligerence, excess salivation, recumbency, coma, bloat, cyanosis and death. Subacute locomotor disturbances are mainly evident when animals are forced to move and start with the forelimbs.
Oxalate cont… Necropsy • Marked edema and hemorrhages in the rumen which is caused by severe rumenitis with vascular damage. • Kidneys are pale edematous and enlarged; hyalinization of the glomeruli and marked tubular dilation. • Calcium oxalate crystals are encountered in both the ruminal wall around the damaged vasculature as well as in the kidneys.
Oxalate cont… Treatment • Calcium borogluconate • Limewater/milk • Activated charcoal • Prophylaxis • inclusion of dicalcium phospahate • Adaptation • Heat treatment
Insoluble oxalates • Calcium oxalate is found in several plants. • these substances may play a role in protection from chemicals produced by other plants, protection from herbivores/insects or could be the plant’s natural calcium sink • Clinical signs include salivation, gagging, colic, bloody diarrhea, depression, prostration and rarely death
Bracken fern (Pteridium aquilinum) §Several species most found in the tropics §Wide range of syndromes have been described §Neurological condition -thiamine deficiency §Bone marrow aplasia §Ulceration of the upper GI tract, §bright blindness -progressive retinal degeneration
Bracken fern cont. . Thiaminase§ polioencephalomalacia in monogastrics impaired thiamine metabolism in sheep. § Poisoning in non-ruminants is due to a thiaminase; the effects are essentially those of vitamin B 1 deficiency, with myelin degeneration of the peripheral nerves.
Bracken fern cont… • Aplastic anemia factor -Acute hemorrhagic disease in cattle is characterized by extensive hemorrhage of the mucous membranes, and subcutaneous hemorrhage and edema • The compound ptaquiloside has been suggested as cause of death of precursor cells in the marrow so that cells with a shorter life span (the platelets) are affected first. • An initial leukocytosis is followed by granulocytopenia and thrombocytopenia with resultant increased susceptibility to infection and tendency to spontaneous hemorrhage.
Bracken fern cont… Clinical signs • Horses— include anorexia, weight loss, incoordination, and a crouching stance with back and neck arched and feet placed wide apart. tachycardia and arrhythmias are present, death. • Cattle, acute bracken poisoning causes an acute hemorrhagic syndrome or, in some cases, sudden death. • Affected cattle are weak, lose weight, and pyrexic; many have difficulty breathing and have icteric or pale mucosae with petechiae; clots of blood in the feces, and bleeding from body orifices.
Bracken fern cont… Diagnosis • Blood thiamine and pyruvate levels, platelet count • Differential Dx • Rabies in horses • Acute toxicity in cattle –Anthrax, mycotoxicicosis • Chronic toxicity-Babesiosis, bacillary haemoglobinuria • Retinal changes-infectious keratoconjuctivitis, cataracts, pregnancy toxemia
Treatment • Administration of thiamine • Antimicrobials • Good nursing care
Teratogenic plants § Alkaloids (e. g. cyclopamine) have been associated with the occurrence of cyclops lambs and other developmental abnormalities in sheep. § The mechanism of action is the inhibition of neuroepithelial cell mitosis and migration during neurulation and decreased proliferation of chondrocytes.
Veratrum cont. . • Defects before days 12 to 36 of pregnancy • Cyclops lambs • prolonged gestation (associated with the absence of pituitary gland) • embryonic death • cleft palate • metacarpal, metatarsal and tracheal cartilage defects
Abortion • Ingestion by cattle of pine needles possibly present in some junipers • isocupressic acid — Inhibition of the catechol estrogen induced blockade of Ca channels by isocupressic acid • Increaesd influx of divalent calcium into arterial smooth muscle cells supplying the gravid uterus and vasoconstriction • Reduction in the blood flow reaching the fetal circulation and causes fetal stress, leading to the induction of premature parturition or abortion.

ZEA mays

Sorghum

Lolium temulantum
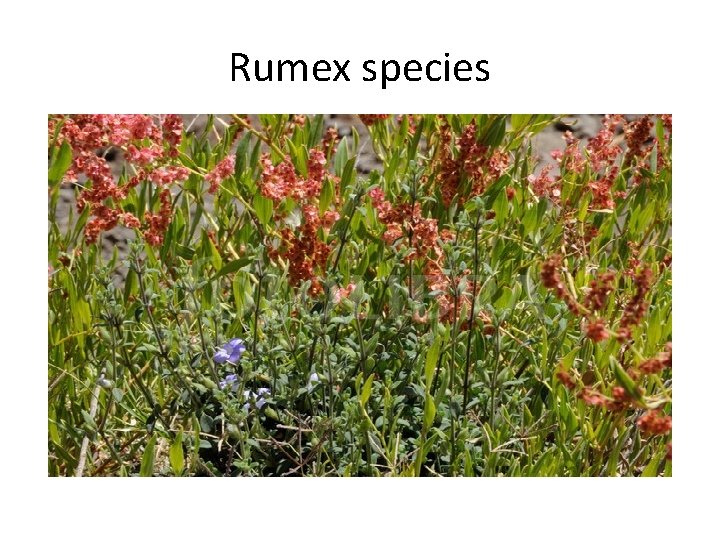
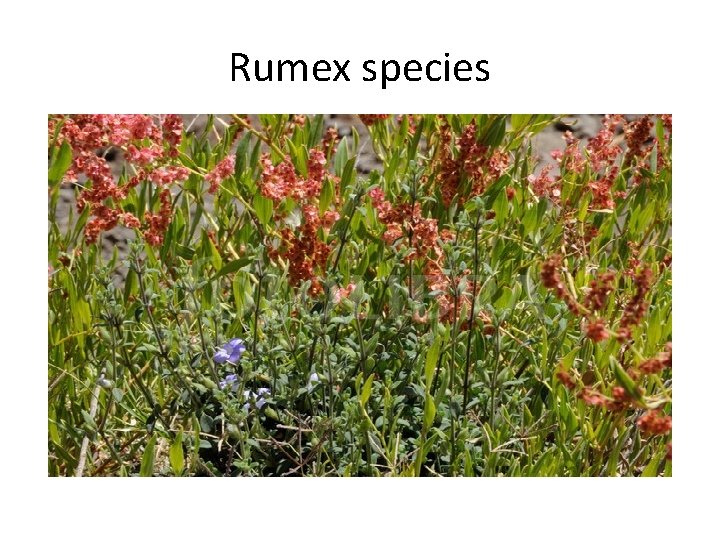
Rumex species
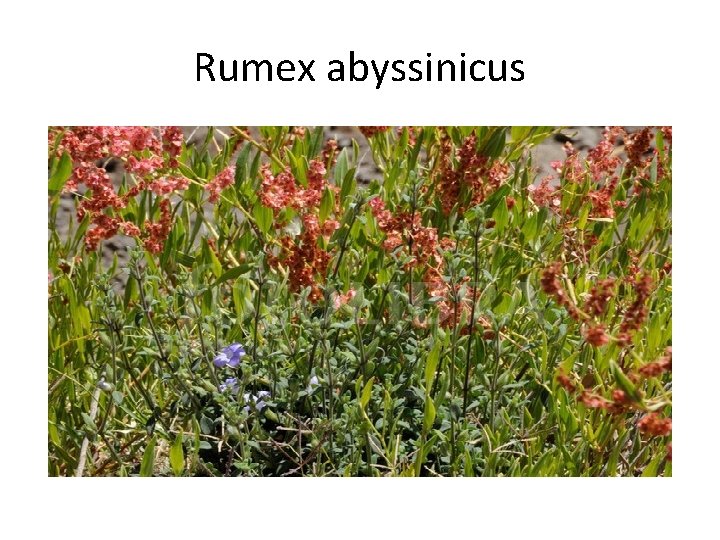
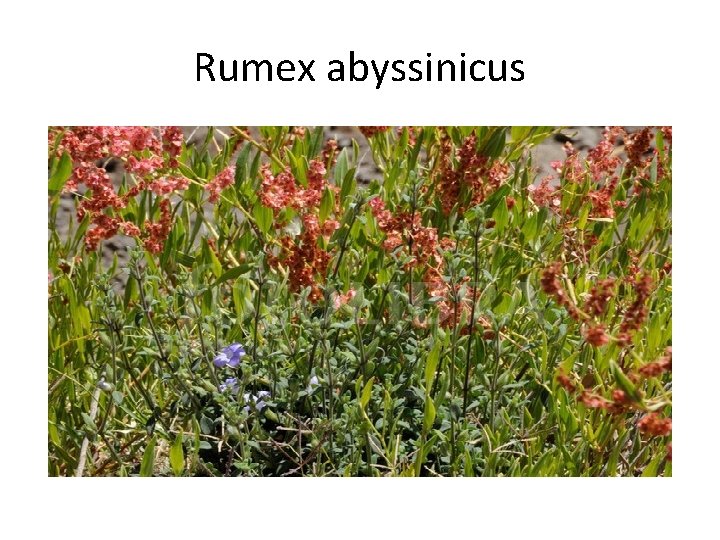
Rumex abyssinicus
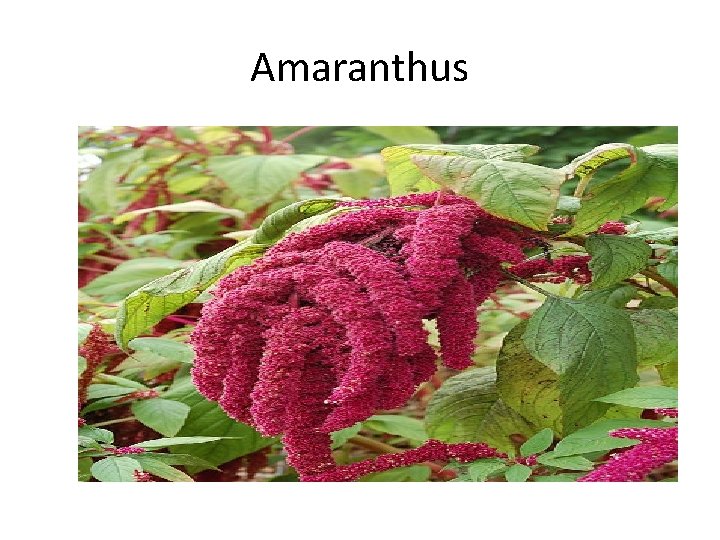
Amaranthus

Bracken fern
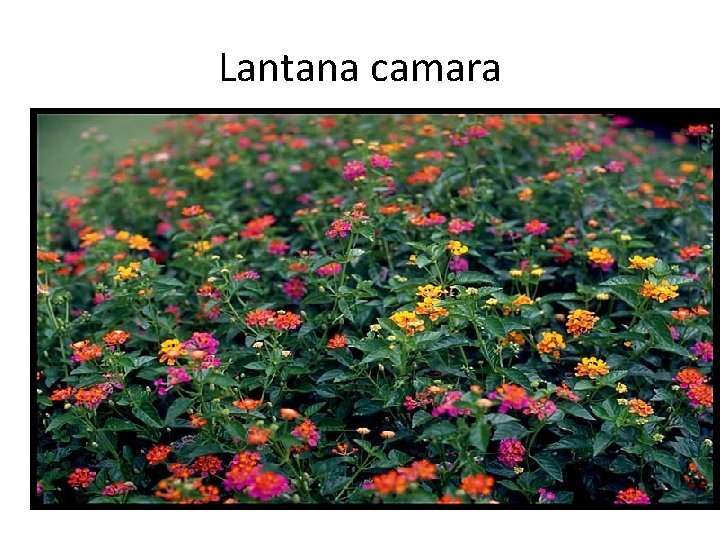
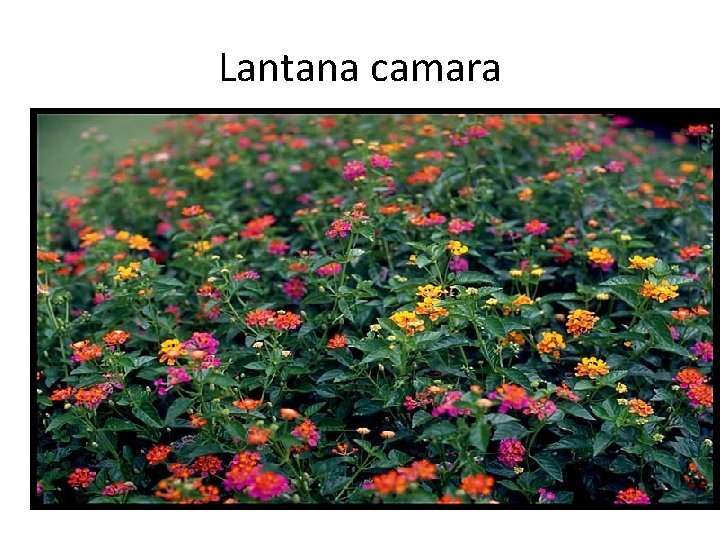
Lantana camara
 Hhps symbols
Hhps symbols Wel kaduru
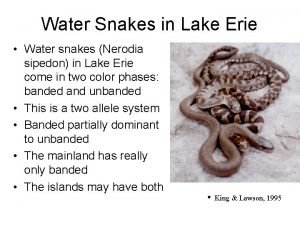
Wel kaduru Allelic diversity
Allelic diversity Asv vial dose
Asv vial dose Poisonous gas leaked in bhopal gas tragedy
Poisonous gas leaked in bhopal gas tragedy Platypus poison
Platypus poison Poison dart frog adaptation
Poison dart frog adaptation Urinal cake poisonous
Urinal cake poisonous Sand dollar anatomy
Sand dollar anatomy Technic
Technic Echinoderm meaning
Echinoderm meaning Poisonous coral snake
Poisonous coral snake Reason for bhopal gas tragedy
Reason for bhopal gas tragedy Forensic toxicology vocabulary
Forensic toxicology vocabulary Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Forensic toxicology lab activity
Forensic toxicology lab activity Forensic toxicologist definition
Forensic toxicologist definition Ld50 examples
Ld50 examples Toxicology
Toxicology Toxicology
Toxicology Toxicology types
Toxicology types Drug identification and toxicology
Drug identification and toxicology What is toxicology?
What is toxicology? Importance of toxicology
Importance of toxicology Toxicology definition
Toxicology definition Forensics toxicology definition
Forensics toxicology definition Hormesis ne demek
Hormesis ne demek Toxicology defination
Toxicology defination Examples of toxicology
Examples of toxicology Toxicology management
Toxicology management Forensic science timeline
Forensic science timeline Chapter 21 toxicology
Chapter 21 toxicology Toxicology excellence for risk assessment
Toxicology excellence for risk assessment Toxicology effects
Toxicology effects Toxicology and applied pharmacology
Toxicology and applied pharmacology Definition of environmental toxicology
Definition of environmental toxicology Food safety and toxicology
Food safety and toxicology Which is more toxic
Which is more toxic Washington state patrol toxicology lab
Washington state patrol toxicology lab Define forensic toxicology
Define forensic toxicology A small dose of toxicology
A small dose of toxicology Toxicology effects
Toxicology effects North carolina medical examiner
North carolina medical examiner Therapeutic index
Therapeutic index Chapter 8 toxicology poisons and alcohol
Chapter 8 toxicology poisons and alcohol Atropine action
Atropine action Lesson plan on food poisoning
Lesson plan on food poisoning Seo poisoning wikipedia
Seo poisoning wikipedia Common factors that can lead to food poisoning
Common factors that can lead to food poisoning