Those Challenging Times Sick Days Holidays and Parties

- Slides: 54
Those Challenging Times: Sick Days, Holidays, and Parties Ragnar Hanas, MD, Ph. D, Department of Pediatrics, Uddevalla, Sweden Presented at the CWD conference, Orlando 2003
Pediatric and adolescent diabetes in Sweden Sparsely populated with large geographical distances High diabetes incidence (3 rd in the world after Finland Sardinia) ~6500 children and adolescents up to the age of 20 ~700 new cases/year (0 -18 years) R Hanas, CWD 2003
How do we care for our patients? Almost everyone is cared for at pediatric departments, the majority by a pediatric diabetologist None are seen by GP: s 40 centers, the largest with ~ 500 patients, but most have 75 -150 Some travel 150 - 200 km to see their diabetologist 50 -100 patients / diabetologist 75 - 150 patients / diabetes nurse Teams with dietician, psychologist, counselor (social worker) R Hanas, CWD 2003
Modern treatment of childhood diabetes Traditional approach Insulin, diet, and exercise Diabetes treatment today Insulin, love and care - Prof. Johnny Ludvigsson Knowledge There is nothing that is forbidden, you can always try something and find out what works for you ”To dare is to lose foothold for a short while - not to dare is to lose yourself” Sören Kierkegaard Danish philosopher 1813 -55 R Hanas, CWD 2003
What goals do we have? The family is encouraged to take active part in diabetes and adjusting doses ”It is no fun having diabetes - but you must be able to have fun even if you have diabetes” - Prof. Johnny Ludvigsson Must know more than the average doctor to manage your diabetes Become an expert on your own diabetes R Hanas, CWD 2003
Important to learn for life. . . After one year you will have experienced most things “Then we want to learn from you!” The clinic will function as an “intelligence center” with input from all families ”Give a man a fish and he will not go hungry that day. Teach him how to fish and he will not be hungry for the rest of his life. ” Chinese saying R Hanas, CWD 2003
Try to keep on living as usual in the family. . . It is our job to adjust the insulin doses to the child, not the other way around Your job is to continue with important things you used to do, like mountain-biking, going for skiing vacation or a trip on the sea It is important to come back to your ordinary parent-child rules in the family R Hanas, CWD 2003
Healthy or sick? Healthy Start with the need of food in your body Take insulin to the food Adjust the dose according to the carbohydrate content Sick Start with the need of insulin in your body Take food and drink to the insulin Eat and drink to give the insulin sugar “to work with”, for example sweet drinks in small but frequent sips. R Hanas, CWD 2003
Sick with fever The child usually eats less but the fever requires more insulin Begin by taking the same insulin doses as usual 100° F often 25% increase of doses 102° F up to 50% increase of doses BG tests before and after each meal Urine ketones at every voiding & in blood if positive Check blood ketones if vomiting or nauseous R Hanas, CWD 2003
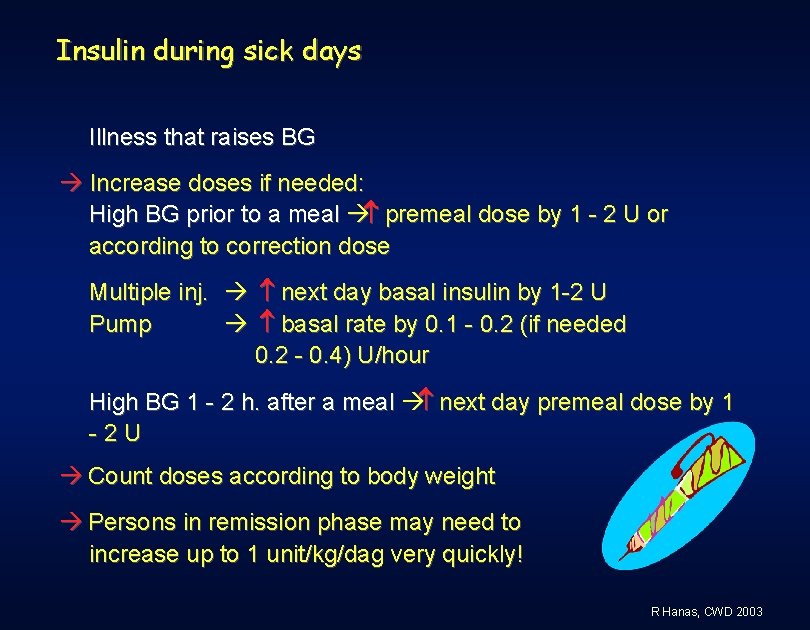
Insulin during sick days Illness that raises BG Increase doses if needed: High BG prior to a meal premeal dose by 1 - 2 U or according to correction dose Multiple inj. next day basal insulin by 1 -2 U Pump basal rate by 0. 1 - 0. 2 (if needed 0. 2 - 0. 4) U/hour High BG 1 - 2 h. after a meal next day premeal dose by 1 -2 U Count doses according to body weight Persons in remission phase may need to increase up to 1 unit/kg/dag very quickly! R Hanas, CWD 2003
Beware of vomiting when having diabetes! Vomiting or nausea? Caused by lack of insulin? !? High blood glucose? Ketones in blood or urine ? When a child with diabetes vomits it should always be considered a sign of insulin deficiency until the opposite is proven! Vomiting from gastroenteritis should be considered only when a lack of insulin has been excluded! R Hanas, CWD 2003
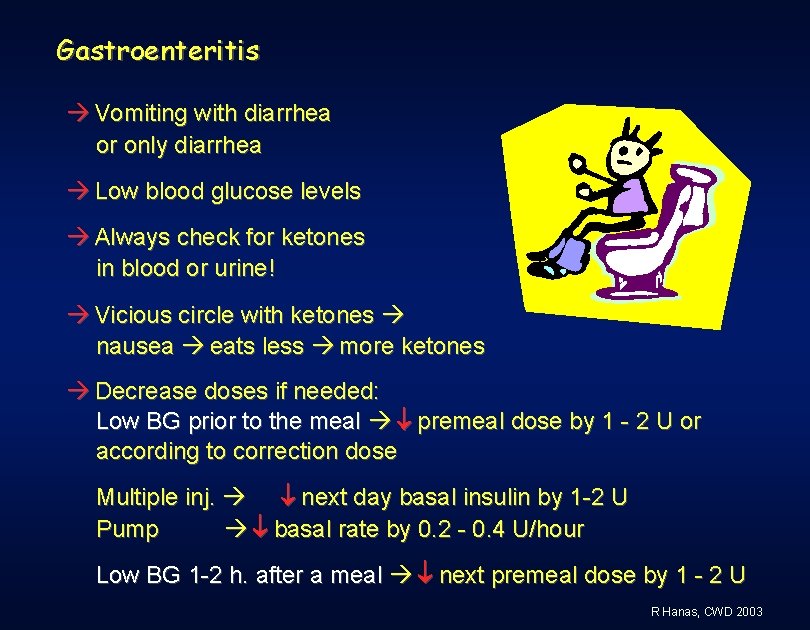
Gastroenteritis Vomiting with diarrhea or only diarrhea Low blood glucose levels Always check for ketones in blood or urine! Vicious circle with ketones nausea eats less more ketones Decrease doses if needed: Low BG prior to the meal premeal dose by 1 - 2 U or according to correction dose Multiple inj. next day basal insulin by 1 -2 U Pump basal rate by 0. 2 - 0. 4 U/hour Low BG 1 -2 h. after a meal next premeal dose by 1 - 2 U R Hanas, CWD 2003
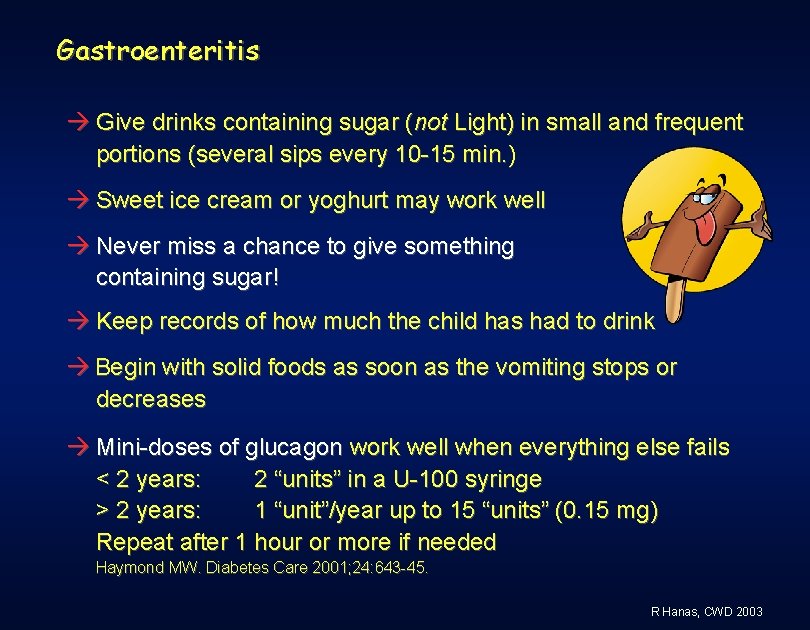
Gastroenteritis Give drinks containing sugar (not Light) in small and frequent portions (several sips every 10 -15 min. ) Sweet ice cream or yoghurt may work well Never miss a chance to give something containing sugar! Keep records of how much the child has had to drink Begin with solid foods as soon as the vomiting stops or decreases Mini-doses of glucagon work well when everything else fails < 2 years: 2 “units” in a U-100 syringe > 2 years: 1 “unit”/year up to 15 “units” (0. 15 mg) Repeat after 1 hour or more if needed Haymond MW. Diabetes Care 2001; 24: 643 -45. R Hanas, CWD 2003
Increased risk of ketoacidosis when ill Relative insulin deficiency if doses are not increased Nausea/vomiting makes it difficult to eat Therefore it may be difficult to increase insulin doses Small insulin depot with a pump insulin deficiency develops quickly if there is a pump failure when you are ill Drink more to prevent dehydration! Sugar-free fluids if BG is > ~220 mg/dl Fluids containing carbohydrates if BG < ~220 mg/dl (~12 mmol/l) R Hanas, CWD 2003
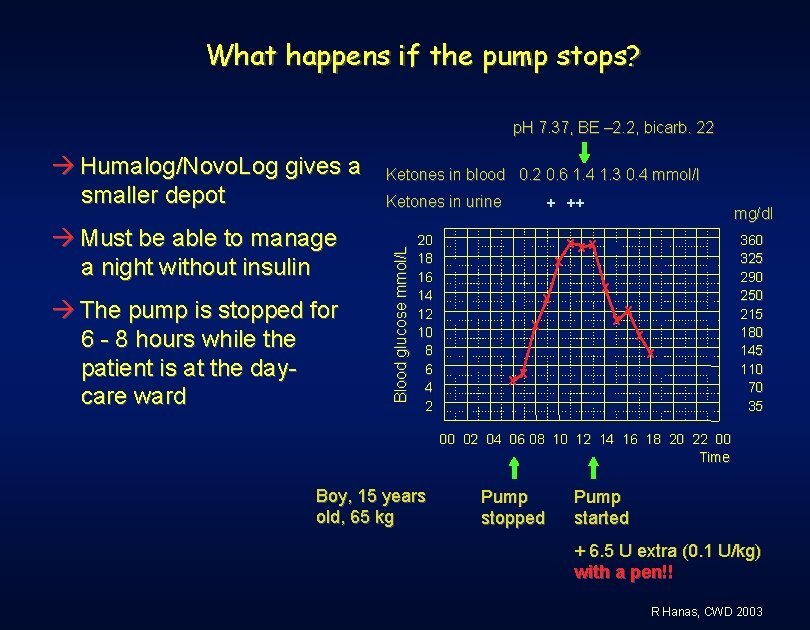
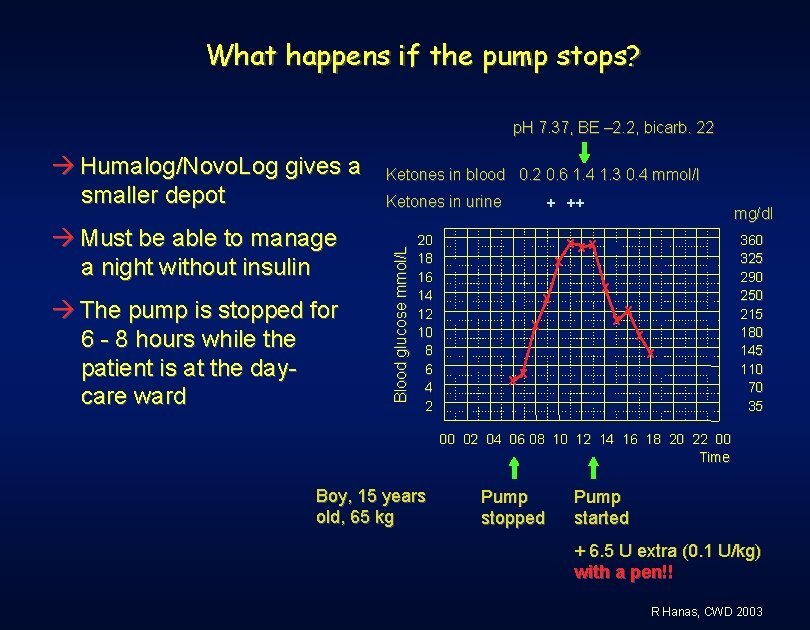
What happens if the pump stops? p. H 7. 37, BE – 2. 2, bicarb. 22 Must be able to manage a night without insulin The pump is stopped for 6 - 8 hours while the patient is at the daycare ward Ketones in blood 0. 2 0. 6 1. 4 1. 3 0. 4 mmol/l Ketones in urine Blood glucose mmol/L Humalog/Novo. Log gives a smaller depot 20 18 16 14 12 10 8 6 4 2 + ++ x x x mg/dl x xx x x xx 360 325 290 250 215 180 145 110 70 35 00 02 04 06 08 10 12 14 16 18 20 22 00 Time Boy, 15 years old, 65 kg Pump stopped Pump started + 6. 5 U extra (0. 1 U/kg) with a pen!! R Hanas, CWD 2003
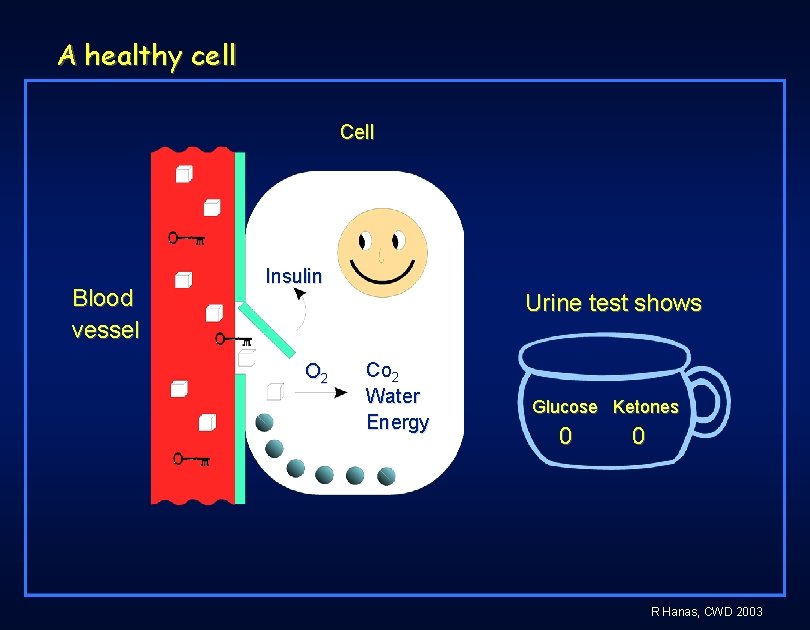
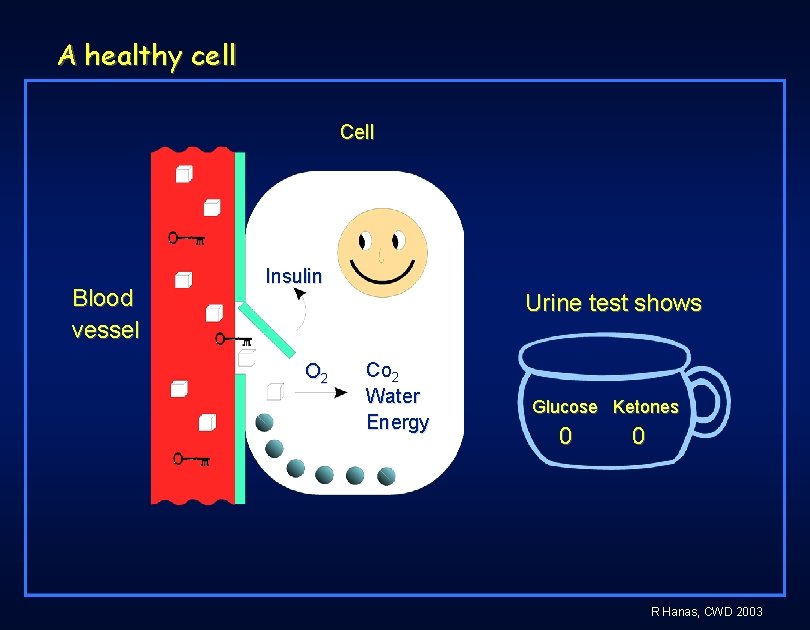
A healthy cell Cell Blood vessel Insulin Urine test shows O 2 Co 2 Water Energy Glucose Ketones 0 0 R Hanas, CWD 2003
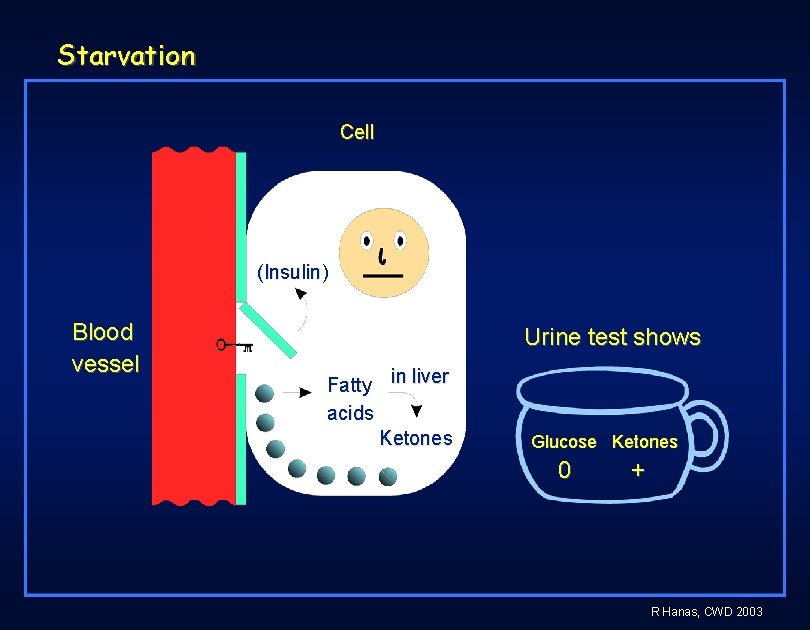
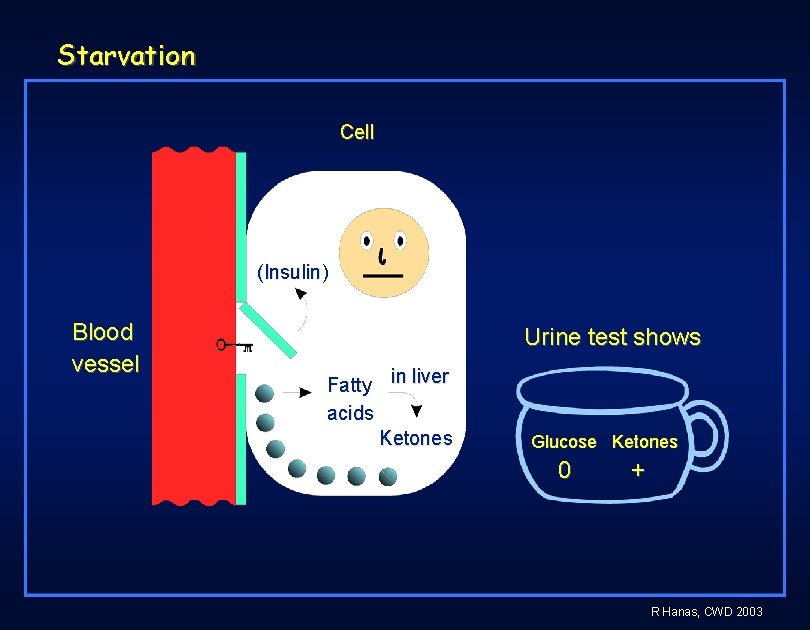
Starvation Cell (Insulin) Blood vessel Urine test shows Fatty in liver acids Ketones Glucose Ketones 0 + R Hanas, CWD 2003
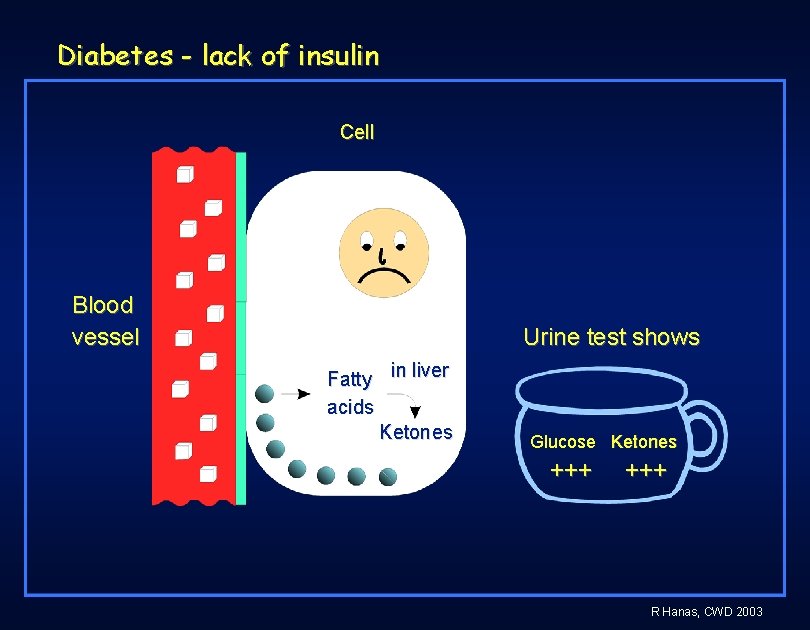
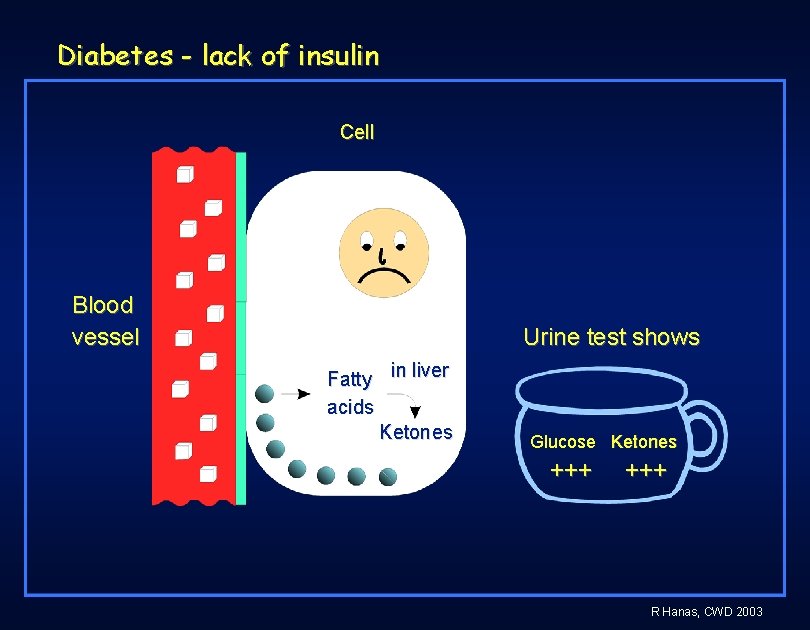
Diabetes - lack of insulin Cell Blood vessel Urine test shows Fatty in liver acids Ketones Glucose Ketones +++ R Hanas, CWD 2003
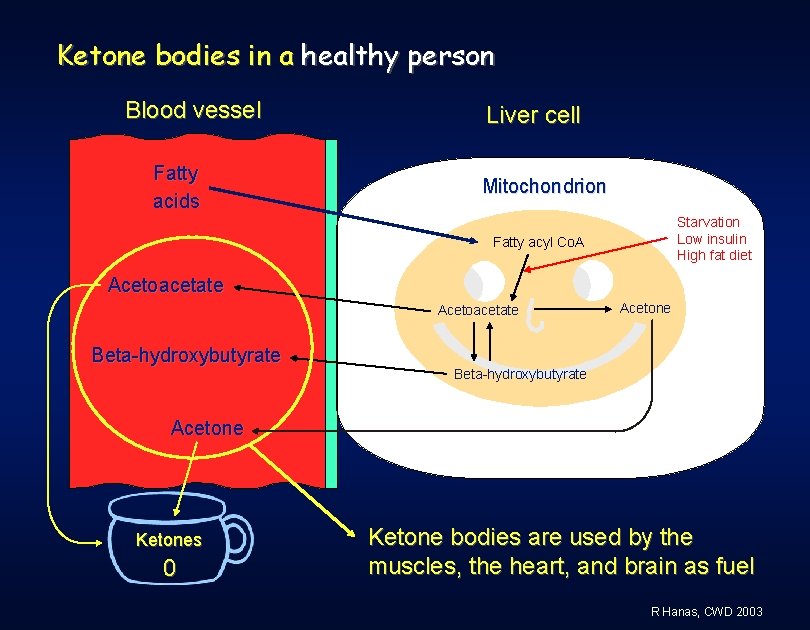
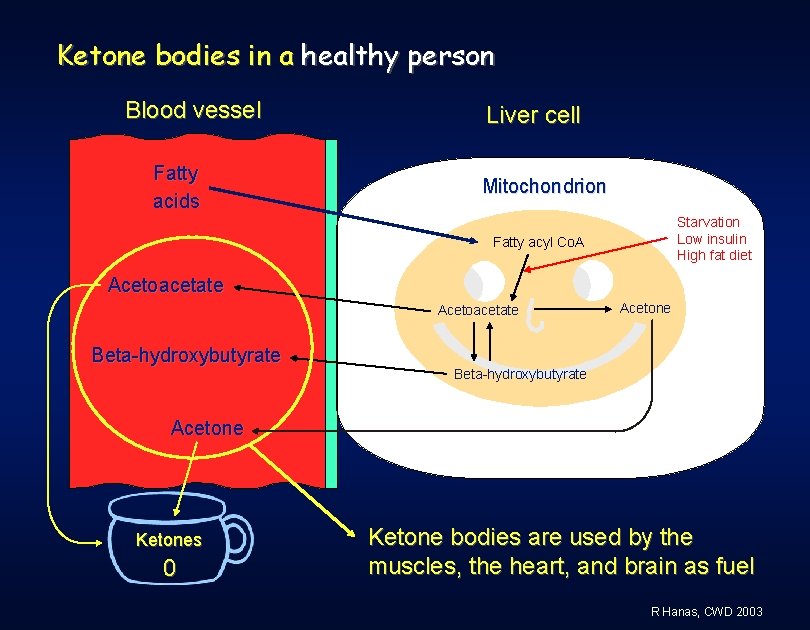
Ketone bodies in a healthy person Blood vessel Fatty acids Liver cell Mitochondrion Starvation Low insulin High fat diet Fatty acyl Co. A Acetoacetate Beta-hydroxybutyrate Acetone Ketones 0 Ketone bodies are used by the muscles, the heart, and brain as fuel R Hanas, CWD 2003
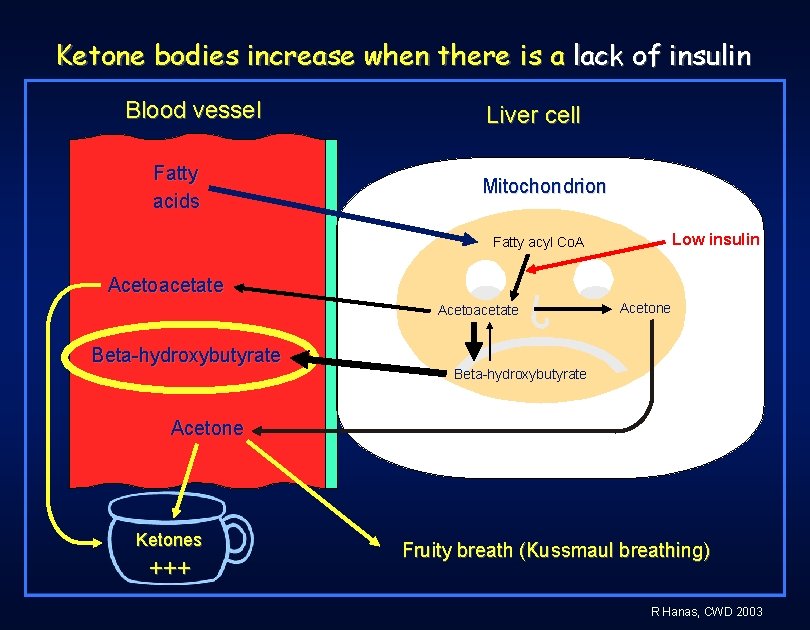
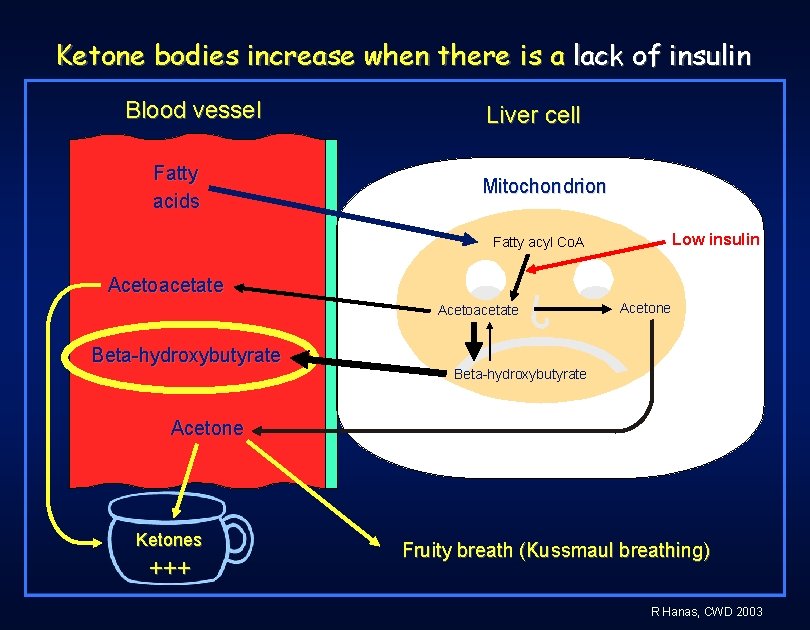
Ketone bodies increase when there is a lack of insulin Blood vessel Fatty acids Liver cell Mitochondrion Low insulin Fatty acyl Co. A Acetoacetate Beta-hydroxybutyrate Acetone Ketones +++ Fruity breath (Kussmaul breathing) R Hanas, CWD 2003
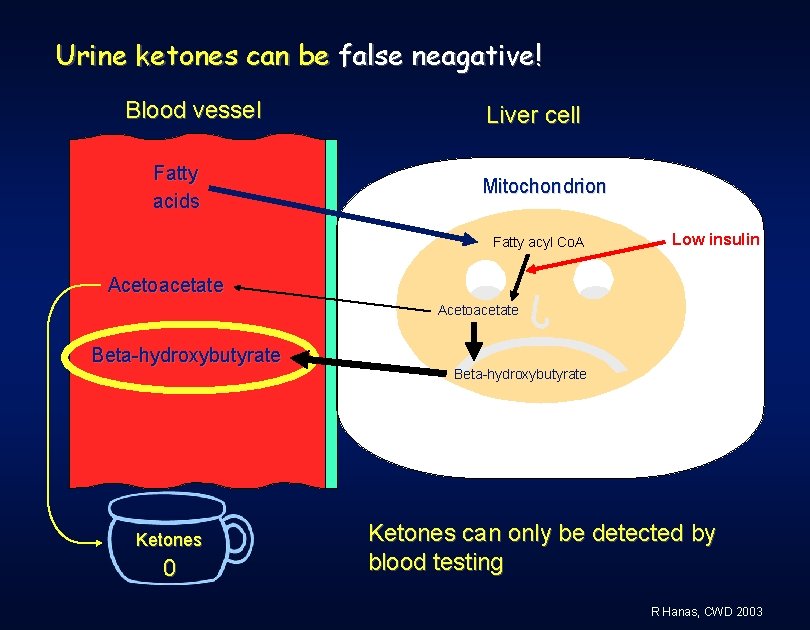
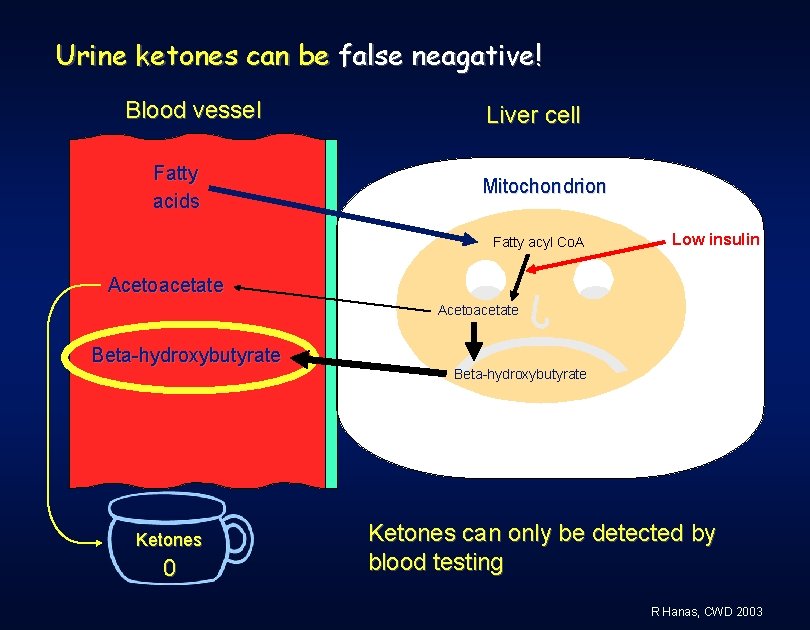
Urine ketones can be false neagative! Blood vessel Fatty acids Liver cell Mitochondrion Fatty acyl Co. A Low insulin Acetoacetate Beta-hydroxybutyrate Ketones 0 Beta-hydroxybutyrate Ketones can only be detected by blood testing R Hanas, CWD 2003
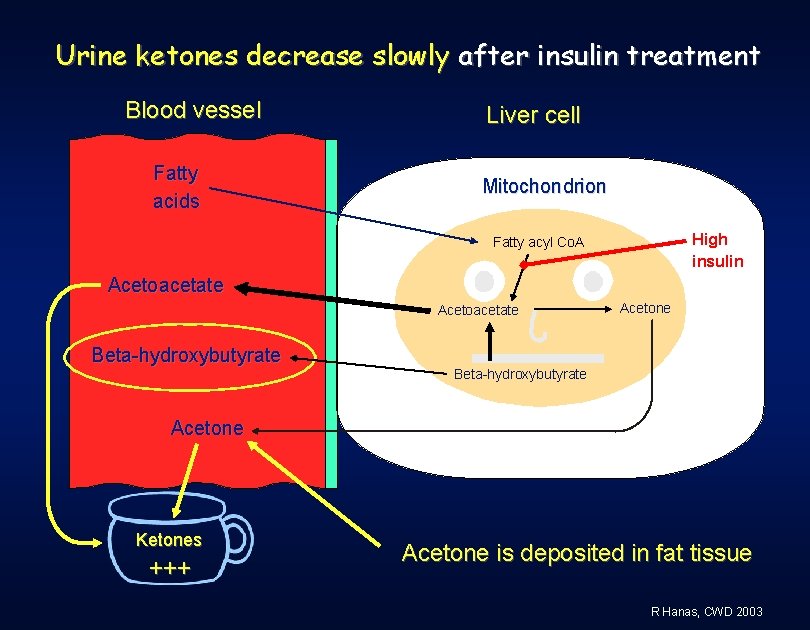
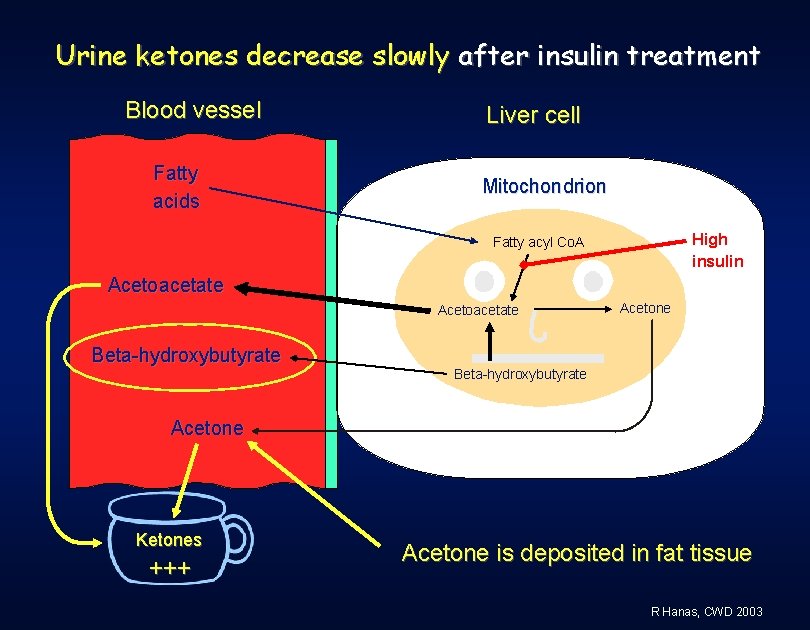
Urine ketones decrease slowly after insulin treatment Blood vessel Fatty acids Liver cell Mitochondrion High insulin Fatty acyl Co. A Acetoacetate Beta-hydroxybutyrate Acetone Ketones +++ Acetone is deposited in fat tissue R Hanas, CWD 2003
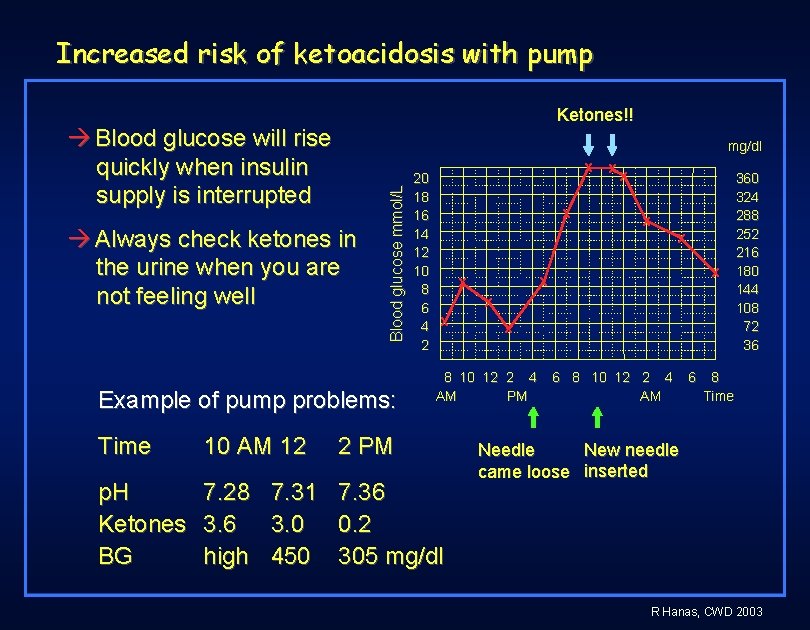
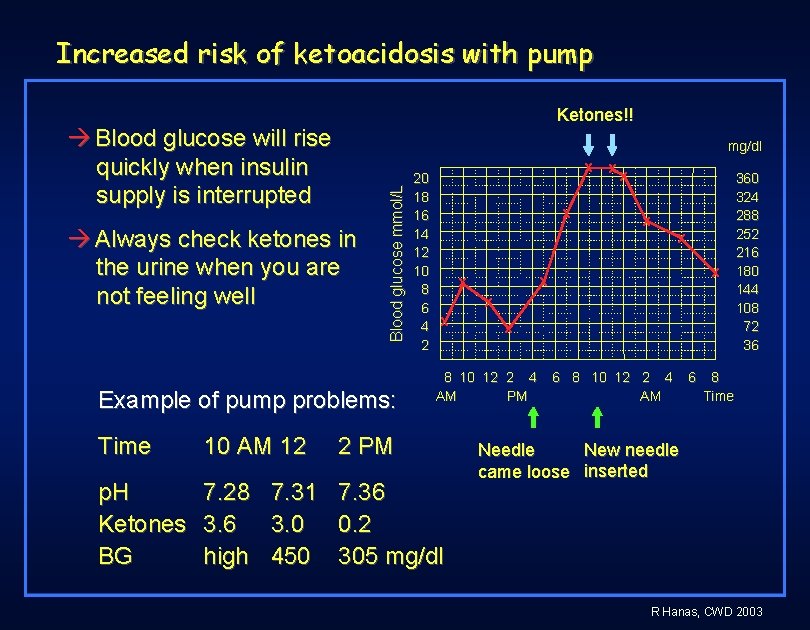
Increased risk of ketoacidosis with pump Ketones!! Blood glucose will rise quickly when insulin supply is interrupted Always check ketones in the urine when you are not feeling well Blood glucose mmol/L mg/dl Example of pump problems: 20 18 16 14 12 10 8 6 4 2 x x x 8 10 12 2 4 AM PM Time 10 AM 12 2 PM p. H Ketones BG 7. 28 3. 6 high 7. 36 0. 2 305 mg/dl 7. 31 3. 0 450 x 6 8 10 12 2 4 AM 6 360 324 288 252 216 180 144 108 72 36 8 Time New needle Needle came loose inserted R Hanas, CWD 2003
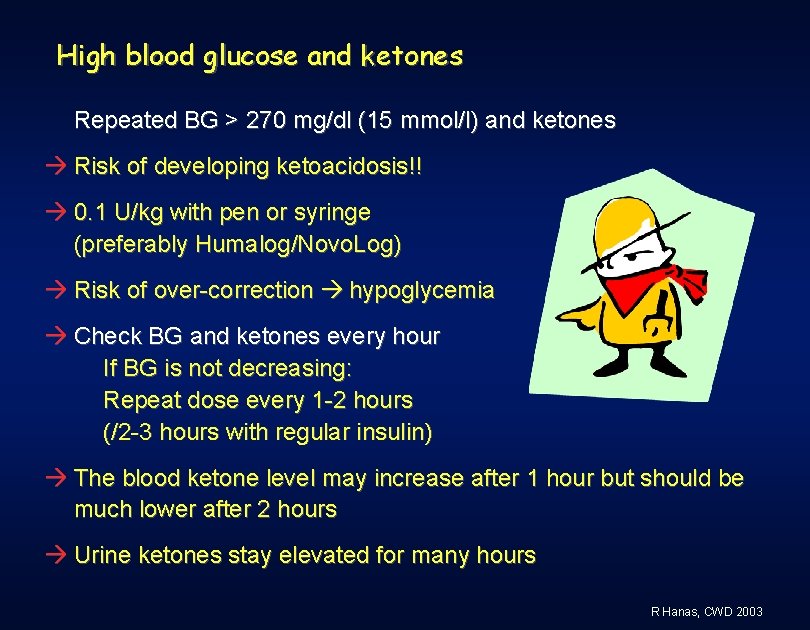
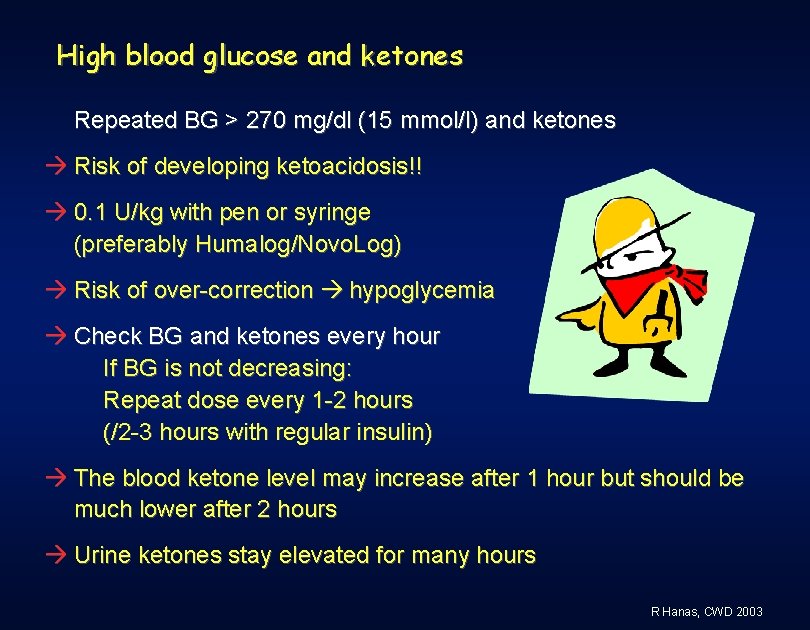
High blood glucose and ketones Repeated BG > 270 mg/dl (15 mmol/l) and ketones Risk of developing ketoacidosis!! 0. 1 U/kg with pen or syringe (preferably Humalog/Novo. Log) Risk of over-correction hypoglycemia Check BG and ketones every hour If BG is not decreasing: Repeat dose every 1 -2 hours (/2 -3 hours with regular insulin) The blood ketone level may increase after 1 hour but should be much lower after 2 hours Urine ketones stay elevated for many hours R Hanas, CWD 2003
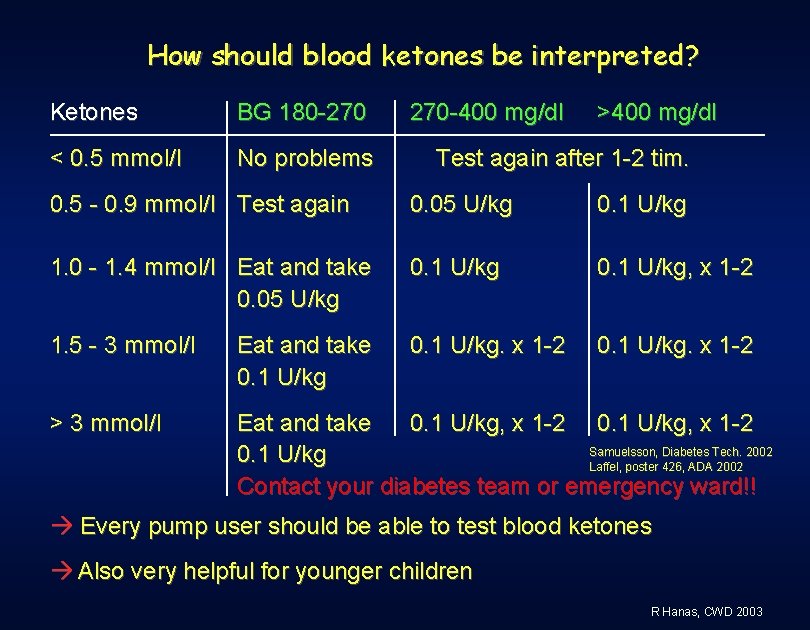
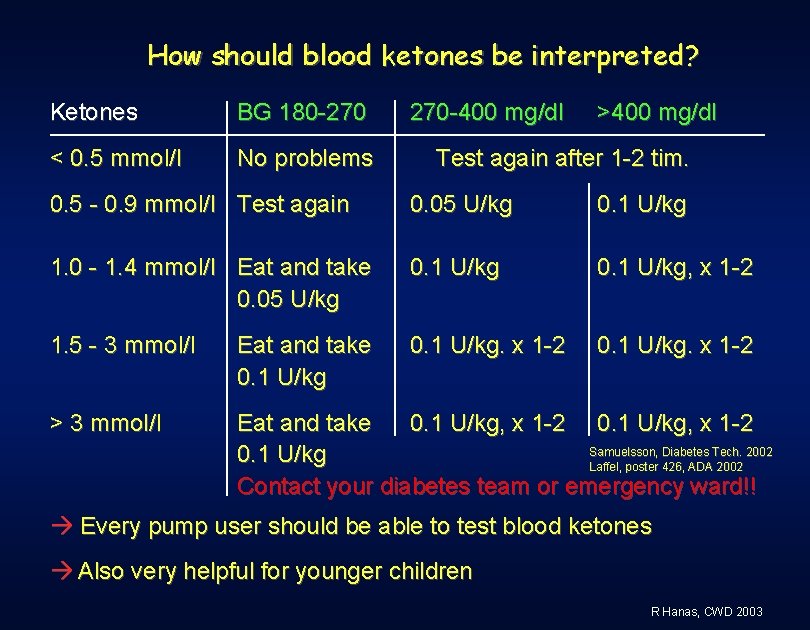
How should blood ketones be interpreted? Ketones BG 180 -270 < 0. 5 mmol/l No problems 270 -400 mg/dl >400 mg/dl Test again after 1 -2 tim. 0. 5 - 0. 9 mmol/l Test again 0. 05 U/kg 0. 1 U/kg 1. 0 - 1. 4 mmol/l Eat and take 0. 05 U/kg 0. 1 U/kg, x 1 -2 1. 5 - 3 mmol/l Eat and take 0. 1 U/kg. x 1 -2 > 3 mmol/l Eat and take 0. 1 U/kg, x 1 -2 Samuelsson, Diabetes Tech. 2002 0. 1 U/kg Laffel, poster 426, ADA 2002 Contact your diabetes team or emergency ward!! Every pump user should be able to test blood ketones Also very helpful for younger children R Hanas, CWD 2003
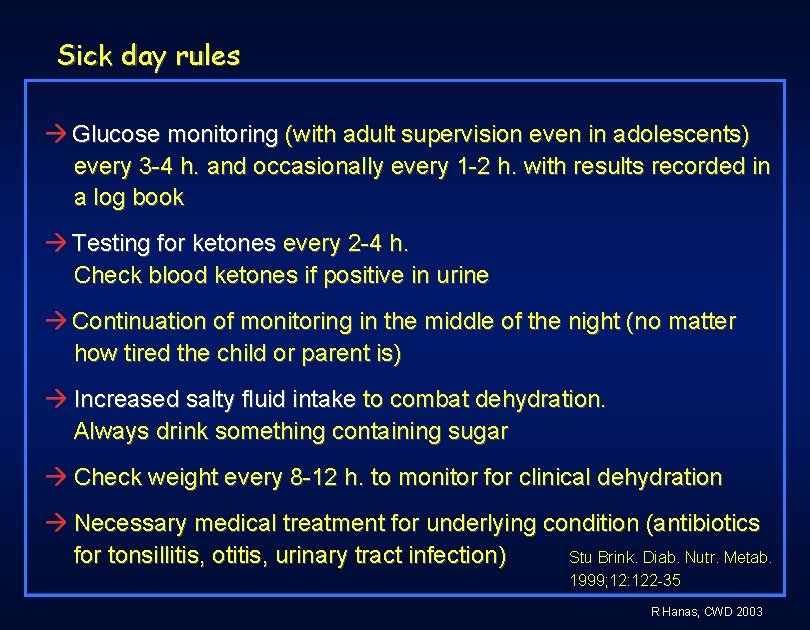
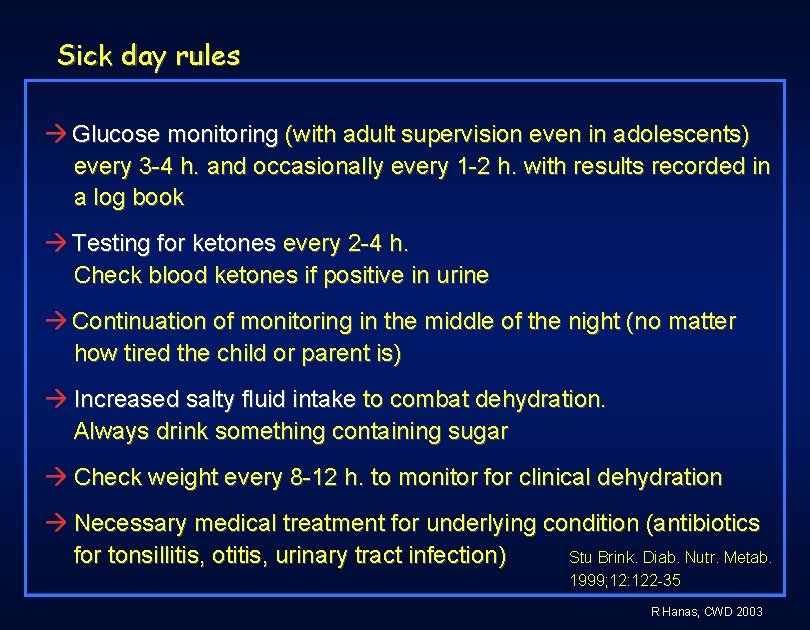
Sick day rules Glucose monitoring (with adult supervision even in adolescents) every 3 -4 h. and occasionally every 1 -2 h. with results recorded in a log book Testing for ketones every 2 -4 h. Check blood ketones if positive in urine Continuation of monitoring in the middle of the night (no matter how tired the child or parent is) Increased salty fluid intake to combat dehydration. Always drink something containing sugar Check weight every 8 -12 h. to monitor for clinical dehydration Necessary medical treatment for underlying condition (antibiotics for tonsillitis, otitis, urinary tract infection) Stu Brink. Diab. Nutr. Metab. 1999; 12: 122 -35 R Hanas, CWD 2003
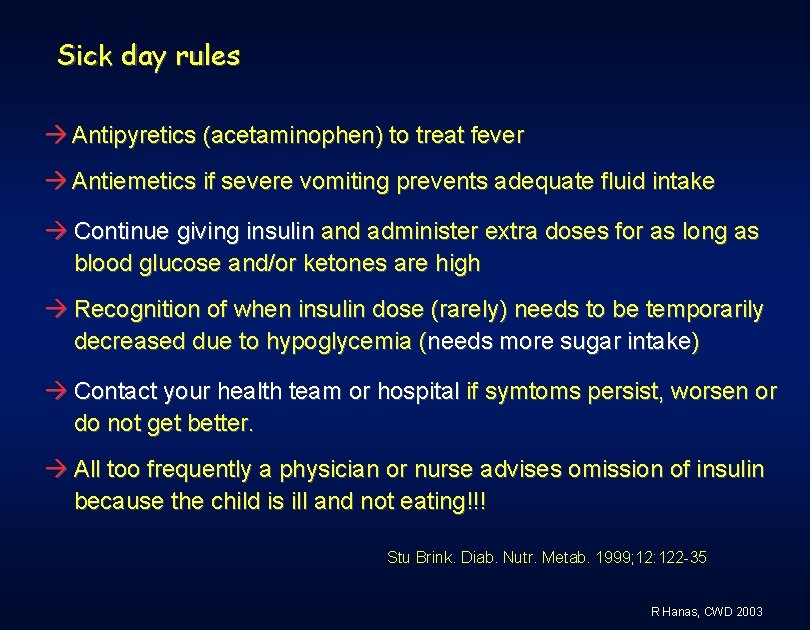
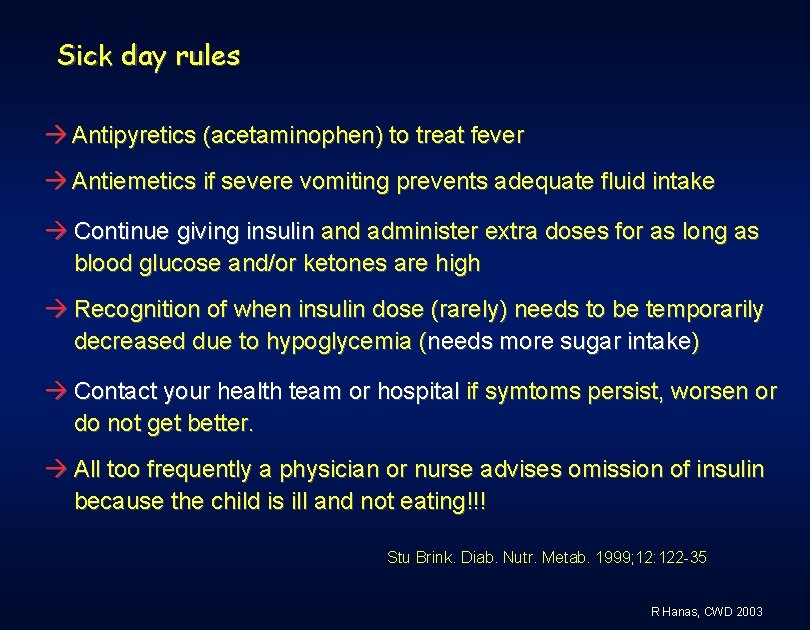
Sick day rules Antipyretics (acetaminophen) to treat fever Antiemetics if severe vomiting prevents adequate fluid intake Continue giving insulin and administer extra doses for as long as blood glucose and/or ketones are high Recognition of when insulin dose (rarely) needs to be temporarily decreased due to hypoglycemia (needs more sugar intake) Contact your health team or hospital if symtoms persist, worsen or do not get better. All too frequently a physician or nurse advises omission of insulin because the child is ill and not eating!!! Stu Brink. Diab. Nutr. Metab. 1999; 12: 122 -35 R Hanas, CWD 2003
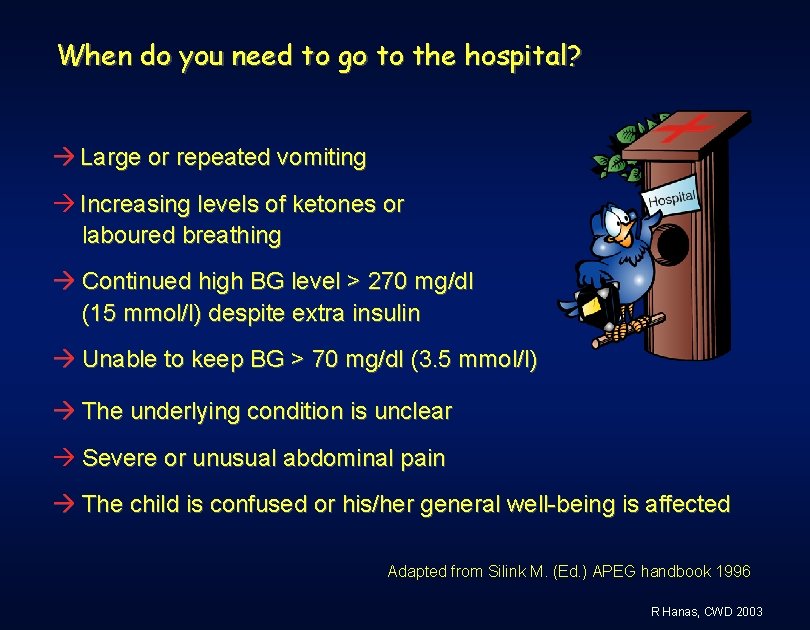
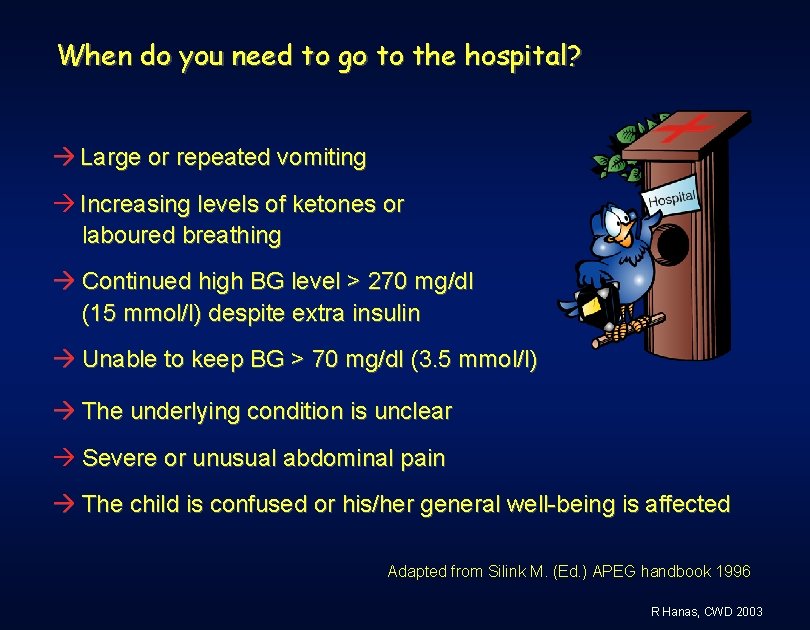
When do you need to go to the hospital? Large or repeated vomiting Increasing levels of ketones or laboured breathing Continued high BG level > 270 mg/dl (15 mmol/l) despite extra insulin Unable to keep BG > 70 mg/dl (3. 5 mmol/l) The underlying condition is unclear Severe or unusual abdominal pain The child is confused or his/her general well-being is affected Adapted from Silink M. (Ed. ) APEG handbook 1996 R Hanas, CWD 2003
When do you need to go to the hospital? The child is young (< 2 - 3 years) or has another disease besides diabetes Exhausted patients/relatives, for example due to repeated nighttime waking Always call if you are in the least unsure about how to manage the situation Adapted from Silink M. (Ed. ) APEG handbook 1996 R Hanas, CWD 2003
Diabetes and surgery Schedule surgery first thing in the morning I. V. insulin best for major surgery with general anesthesia For minor surgery with local anesthesia, take only basal insulin (Lantus or pump) Emergency surgery: I. V. insulin to bring down BG before surgery Ketoacidosis can give abdominal pain of the same magnitude as appendicitis Parents are the “diabetes experts” when their child is at a pediatric surgery ward! R Hanas, CWD 2003
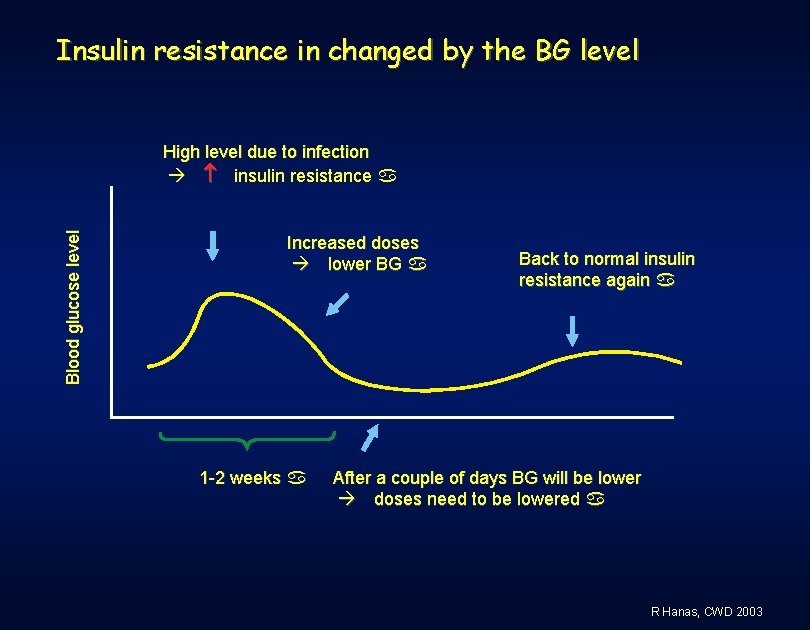
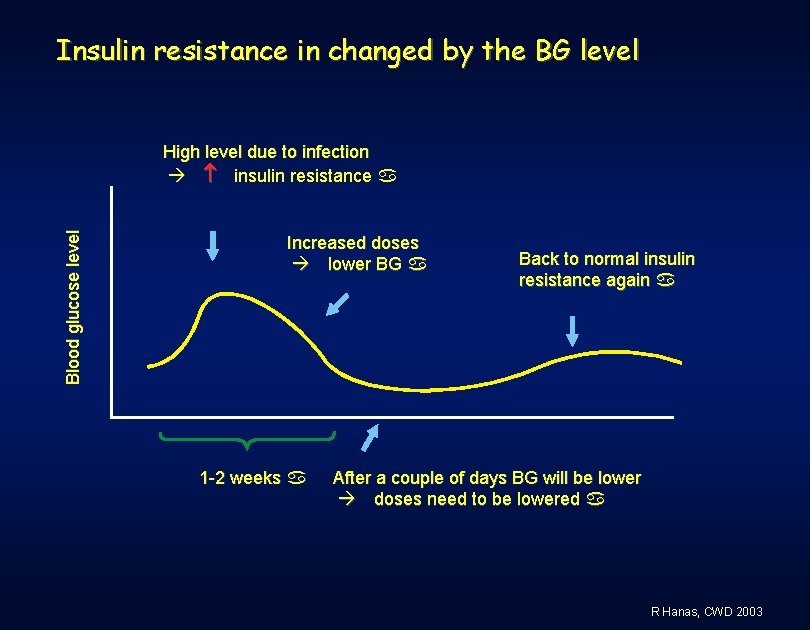
Insulin resistance in changed by the BG level Blood glucose level High level due to infection insulin resistance a Increased doses lower BG a 1 -2 weeks a Back to normal insulin resistance again a After a couple of days BG will be lower doses need to be lowered a R Hanas, CWD 2003

Insulin requirements increase with fever Insulin requirements Cold with fever a Infection cureda Increased insulin resistance due to fevera Continued insulin resistance a R Hanas, CWD 2003
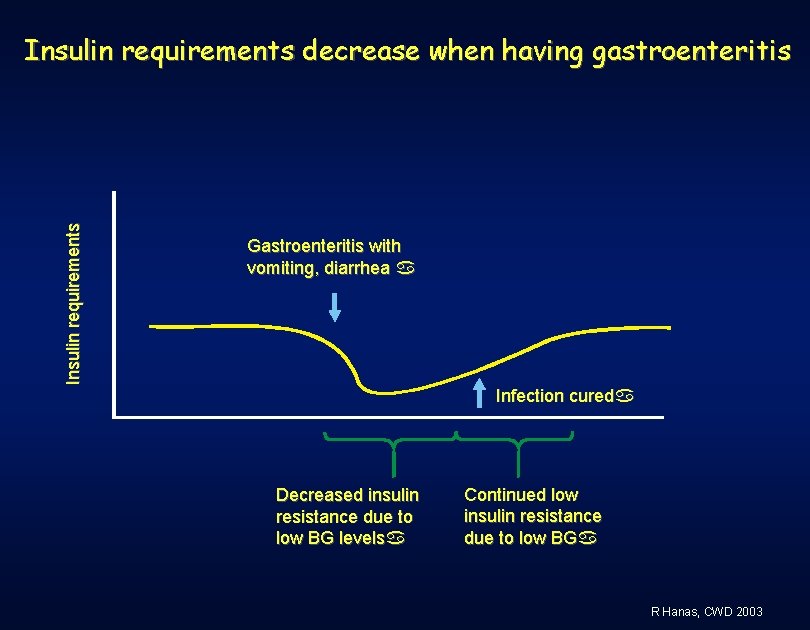
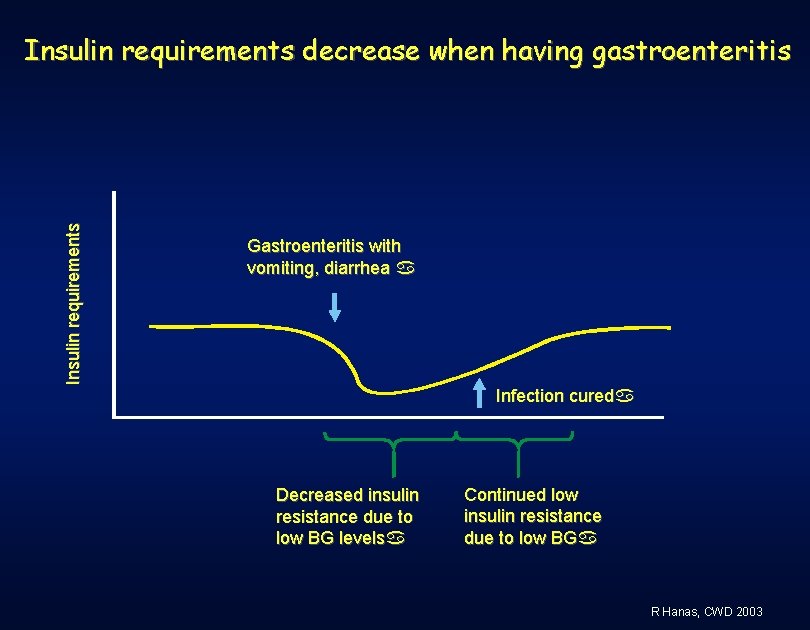
Insulin requirements decrease when having gastroenteritis Gastroenteritis with vomiting, diarrhea a Infection cureda Decreased insulin resistance due to low BG levelsa Continued low insulin resistance due to low BGa R Hanas, CWD 2003
Holidays and travelling R Hanas, CWD 2003
Isn’t it difficult to go abroad if my child has diabetes? ”When a problem is too large or seems unsolvable, don’t forget that you can eat an elephant if you cut it into small enough pieces” Slavian saying R Hanas, CWD 2003
Diabetes equipment to bring on the trip Extra insulin pen and/or syringes (pre-filled pens are handy for this) Store in separate hand luggage Thermometer to check the temperature of the refrigerator Test strips + meter Extra meter 1 mmol/l = 18 mg/dl Finger-pricking device + lancets Test strips for ketones (blood and/or urine) R Hanas, CWD 2003
Diabetes equipment to bring on the trip Dextrose/glucose tablets and gel Glucagon Clinical thermometer Fever suppressing drugs: Paracetamol/acetaminophen and/or aspirin /salicylic acid (adults only) Oral rehydration solution ID indicating that you have diabetes and a necklace/bracelet Telephone and fax. numbers for your diabetes clinic at home Insurance documents R Hanas, CWD 2003
Preventing “The Revenge of Montezuma” Antibiotics for diarrhea when travelling to Asia, Africa, Latin/South America or Southern Europe: Lexinor® (norfloxacine) Not for children younger than 12 years old or pregnant women. Dose: 200 mg twice daily for prophylactic use or 400 mg twice daily for 3 days if you are having acute diarrhea. Co-trimoxazole, Colizole® (trimethoprim + sulphamethoxazole) or similar for children younger than 12 years old. R Hanas, CWD 2003
Passing time zones Multiple injections/pump: Going west (longer day): Extra meals and doses of mealtime insulin Usual dose of bedtime insulin/pump basal rate for the “new night” Going east (shorter day): Decreased number of meals and mealtime doses Usual dose of bedtime insulin/pump basal rate for the “new night” Don’t forget to adjust the clock of the pump! R Hanas, CWD 2003
Passing time zones 2 -dose treatment Going west (longer day): Extra meals and doses of mealtime insulin Usual dose of bedtime insulin/basal rate to the “new night” Going east (shorter day): Decreased number of meals and mealtime doses Take mealtime insulin with last meal before sleeping Short-acting insulin: no bedtime insulin Rapid-acting insulin: small dose of bedtime insulin Reduce next intermediate-acting dose with 3 -5% per time shift hour on long flights Sane T. BMJ 1990; 301: 421 -22 R Hanas, CWD 2003
Always call your home team You are never longer away from home than a telephone call Ask for a doctor’s contact before leaving home Check www. ispad. org for names of doctors Staying at a hospital where you don’t understand the language is a difficult experience Try to find a children’s hospital in an emergency situation With glucagon and frequent monitoring you can prevent most emergencies! R Hanas, CWD 2003
Diabetes camps Family camp Scout camp Skiing trip Sailing ship -9 10 -12 13 -15 16 -19 Diabetes education & camp activities R Hanas, CWD 2003
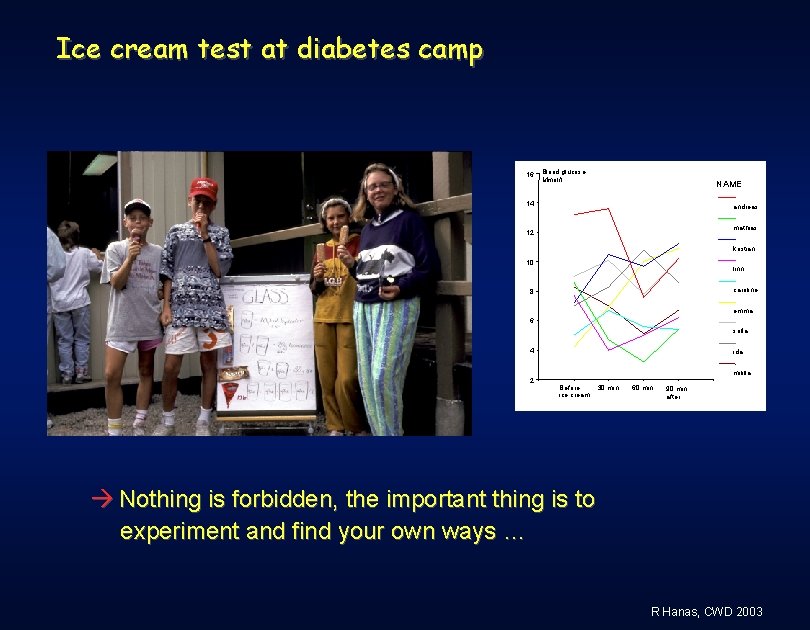
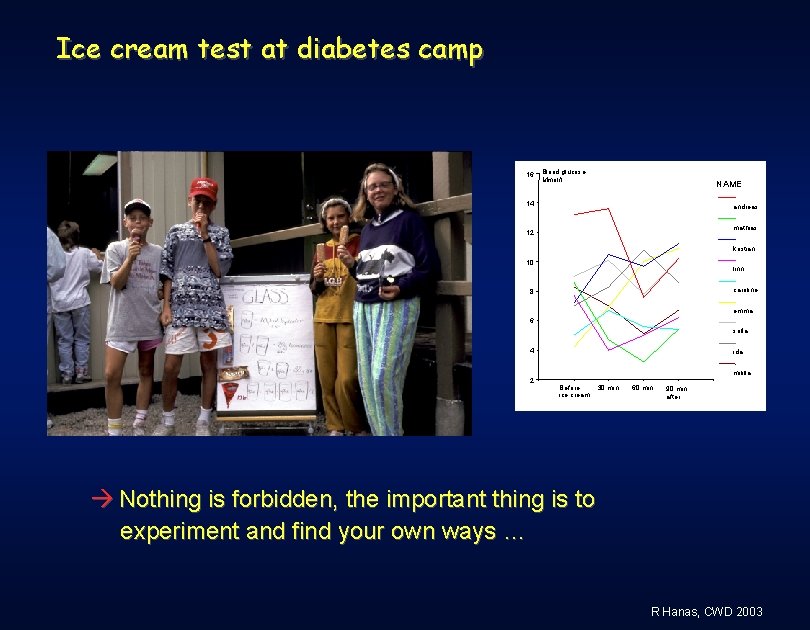
Ice cream test at diabetes camp 16 Blood glucose Mmol/l. NAME 14 andreas mathias 12 kristian 10 linn caroline 8 emma 6 sofia 4 ida mililla 2 Before ice cream 30 min. 60 min. 90 min. after Nothing is forbidden, the important thing is to experiment and find your own ways … R Hanas, CWD 2003
Diabetes camps China: 17 participants, 8 -13 years, 2 days camp Significant improvement in: - Using glucose-monitoring devices, drawing insulin, injecting insulin and choosing the right exchange of food. Lee YJ. Zhonghua Min 1992; 33: 280 -5. USA: 148 participants, 13 -17 years, 1 week camp More use of problem-focused strategies in stressful situations and less use of avoidance strategies Smith KE. Diab Educator 1991; 17: 49 -53. Sweden: 32 participants, 6 days camp Increased diabetes knowledge after using Bodylink Hanas R. Poster ISPAD 1994. R Hanas, CWD 2003
Diabetes camps USA: 86 participants, 13 -17 years, 1 week camp Significant increase in adolescents ideas on: Expressing needs and views that differ from others Expressing feelings openly Making requests Saying no to unreasonable requests Initiating and concluding conversations Smith KE. Diab Educator 1993; 19: 36 -41. Italy: 256 participants, 8 -16 years, 8 -15 days camp Significant improvement in: - Knowledge and self-management. - Hb. A 1 c improved in 74 patients that attended monthly meetings after camp. Misuraca A. Diab Res Clin Pract 1996; 32: 91 -96. R Hanas, CWD 2003
School camps Important to be able to join friends No medical staff that can handle emergencies Ask one teacher or supervisor to take responsibility Parent may need to accompany a younger child School staff can attend at a visit to the clinic Check the program for meals and activities in advance and plan together with your child Higher level of physical activity lower doses Check that hypo food is available, also at off-hours Most important is to be able to have fun, not to have a perfect BG! R Hanas, CWD 2003
Parties R Hanas, CWD 2003
What does it mean to have diabetes …? R Hanas, CWD 2003
Birthday parties Learn to eat the food that is served, i. e. don’t bring a bag of ”diabetes food” Check that diet soft drinks (Light) are available The children often play around a lot risk of hypoglycemia Provide the host with hypo advice Take an extra unit for the cake if needed Bag of sweets can be brought home and eaten at suitable occasions Birthday parties should be FUN so it is better to have a slightly higher BG than a hypo! R Hanas, CWD 2003
Can you stay up all night. . . ? All night parties Temporary night work Let the pumpbasal rate run as usual or take Lantus as usual Take usual dose of NPH insulin when you go to bed if you intend to sleep ~8 -10 hours, otherwise decrease the dose Take bolus doses as usual when you eat every 4 -5 hours Take the breakfast dose when it is time to have breakfast Alcohol will make you think less clearly! R Hanas, CWD 2003
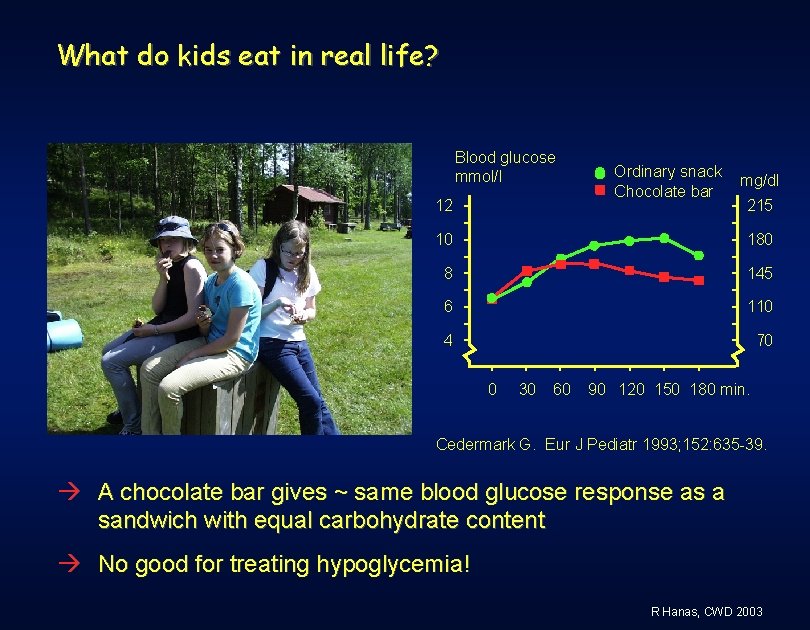
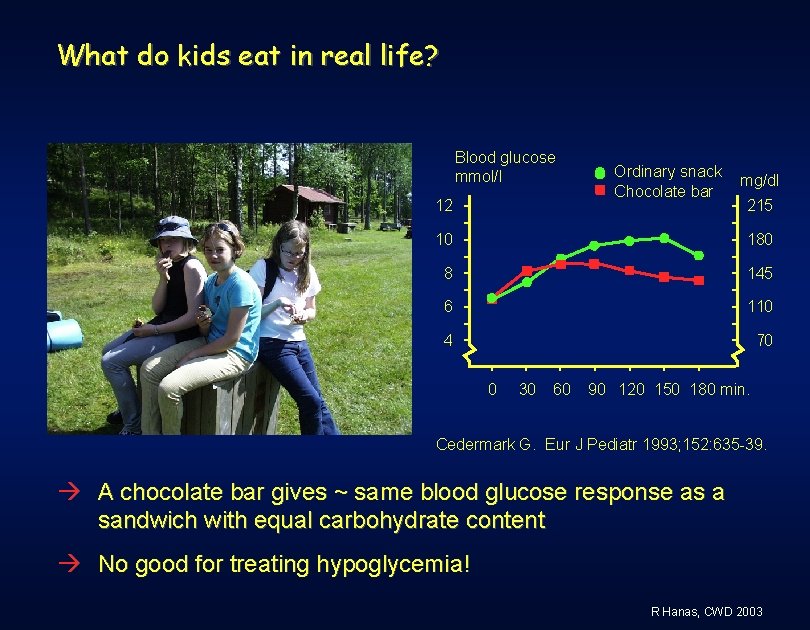
What do kids eat in real life? Blood glucose mmol/l 12 Ordinary snack Chocolate bar mg/dl 215 10 180 8 145 6 110 4 70 0 30 60 90 120 150 180 min. Cedermark G. Eur J Pediatr 1993; 152: 635 -39. A chocolate bar gives ~ same blood glucose response as a sandwich with equal carbohydrate content No good for treating hypoglycemia! R Hanas, CWD 2003
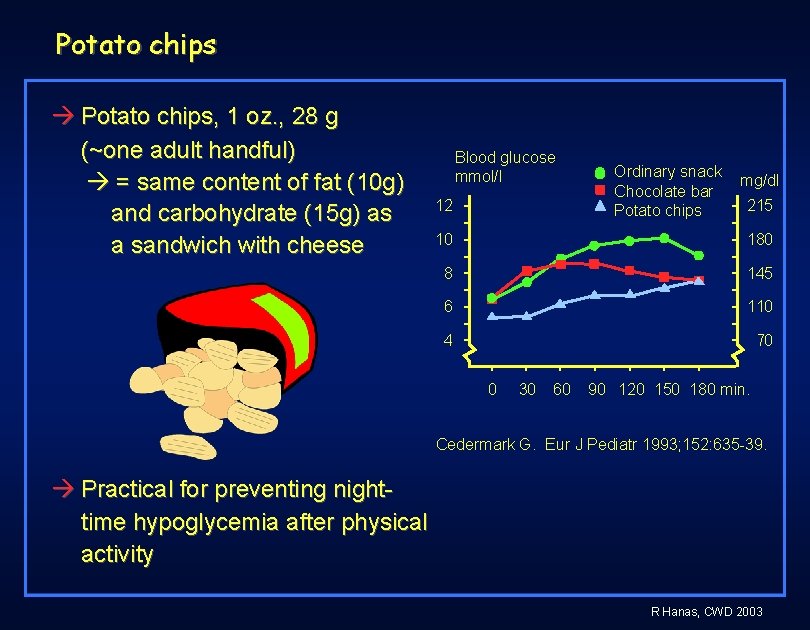
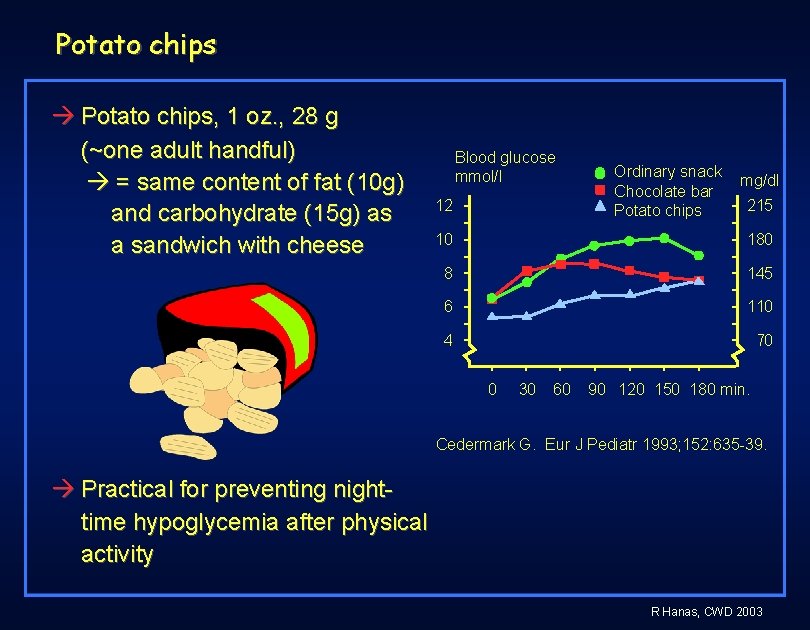
Potato chips Potato chips, 1 oz. , 28 g (~one adult handful) = same content of fat (10 g) and carbohydrate (15 g) as a sandwich with cheese Blood glucose mmol/l 12 Ordinary snack Chocolate bar Potato chips mg/dl 215 10 180 8 145 6 110 4 70 0 30 60 90 120 150 180 min. Cedermark G. Eur J Pediatr 1993; 152: 635 -39. Practical for preventing nighttime hypoglycemia after physical activity R Hanas, CWD 2003
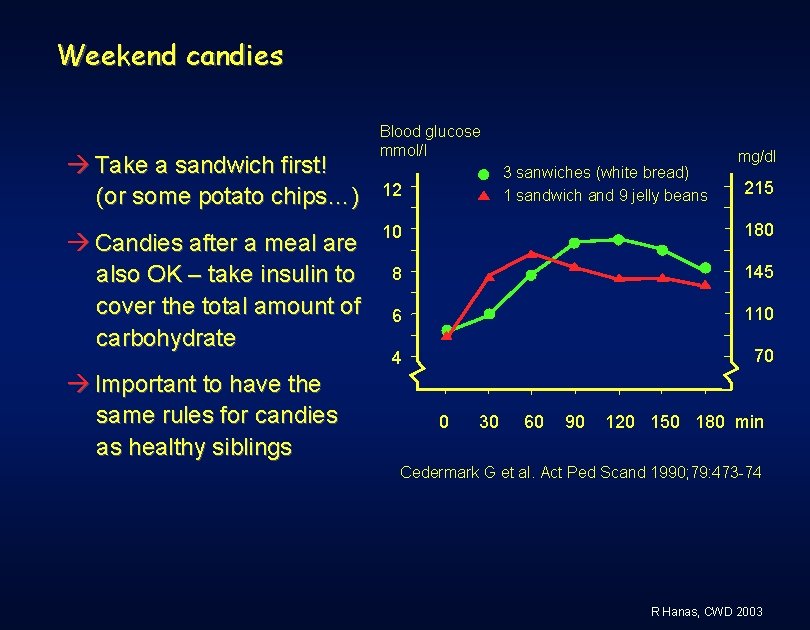
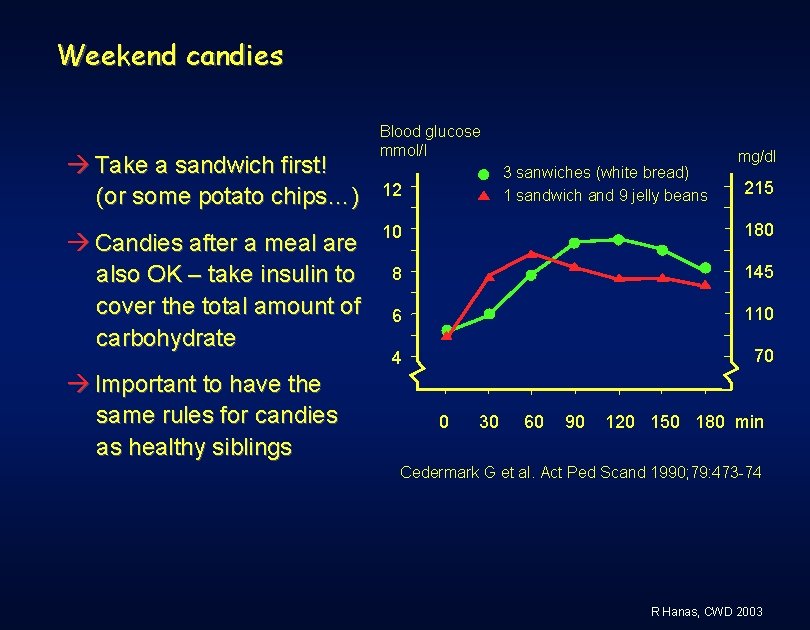
Weekend candies Take a sandwich first! (or some potato chips…) Candies after a meal are also OK – take insulin to cover the total amount of carbohydrate Important to have the same rules for candies as healthy siblings Blood glucose mmol/l 3 sanwiches (white bread) 1 sandwich and 9 jelly beans 12 mg/dl 215 10 180 8 145 6 110 4 70 0 30 60 90 120 150 180 min Cedermark G et al. Act Ped Scand 1990; 79: 473 -74 R Hanas, CWD 2003
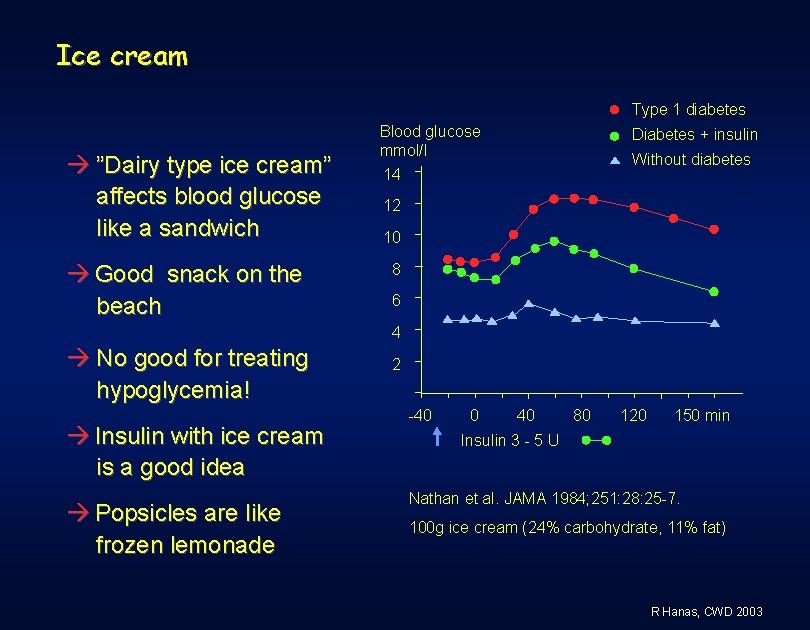
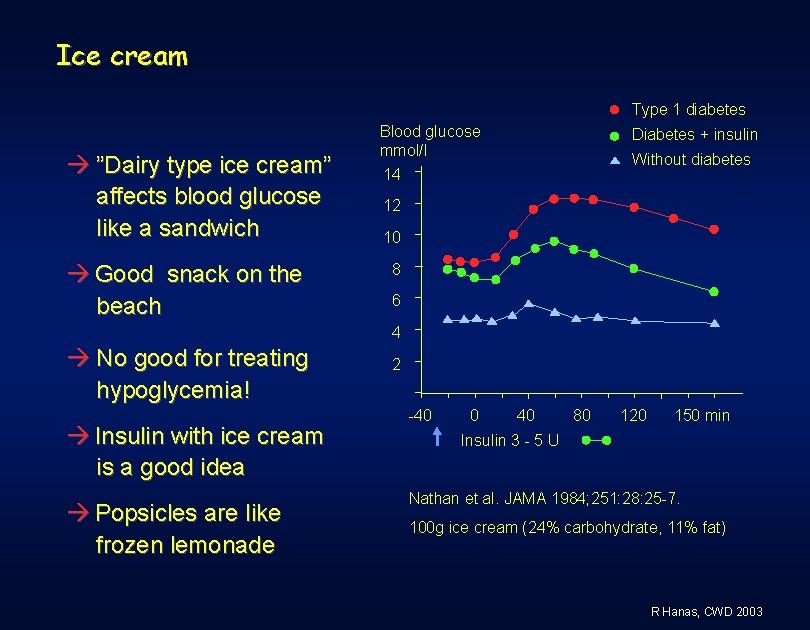
Ice cream Type 1 diabetes ”Dairy type ice cream” affects blood glucose like a sandwich Good snack on the beach Blood glucose mmol/l 14 Diabetes + insulin Without diabetes 12 10 8 6 4 No good for treating hypoglycemia! Insulin with ice cream is a good idea Popsicles are like frozen lemonade 2 -40 0 40 80 120 150 min Insulin 3 - 5 U Nathan et al. JAMA 1984; 251: 28: 25 -7. 100 g ice cream (24% carbohydrate, 11% fat) R Hanas, CWD 2003
 The sixth sick sheik's sixth sheep's sick lyrics
The sixth sick sheik's sixth sheep's sick lyrics Earss lpss
Earss lpss Those winter sundays poem analysis
Those winter sundays poem analysis In those days there was no king
In those days there was no king Caesar augustus issued a decree that a census
Caesar augustus issued a decree that a census Her fancy was running riot along those days ahead of her
Her fancy was running riot along those days ahead of her 15 times 15 times 20
15 times 15 times 20 8 stages of system development life cycle
8 stages of system development life cycle Feasibility study in sdlc
Feasibility study in sdlc What i found challenging
What i found challenging Cpt abc worksheet example
Cpt abc worksheet example Challenging resistance to change
Challenging resistance to change Challenging behaviour scenarios
Challenging behaviour scenarios Examples of challenge
Examples of challenge Exciting, boring, dangerous, safe, interesting, challenging
Exciting, boring, dangerous, safe, interesting, challenging Time intensity model challenging behaviour
Time intensity model challenging behaviour Children challenging industry
Children challenging industry Periodic table sentences
Periodic table sentences Dealing with challenging patients
Dealing with challenging patients Accounting information system chapter 1
Accounting information system chapter 1 Chapter 5 section 1 parties and what they do
Chapter 5 section 1 parties and what they do Quality policy
Quality policy Sarah and pam often go to parties
Sarah and pam often go to parties Chapter 5 section 1 parties and what they do
Chapter 5 section 1 parties and what they do Political parties pros and cons
Political parties pros and cons Megan and ron ate too much and felt sick
Megan and ron ate too much and felt sick Seaside holidays then and now
Seaside holidays then and now Seaside now and then
Seaside now and then Youtube-com
Youtube-com Cultural holidays in italy
Cultural holidays in italy Seaside then and now
Seaside then and now British holidays and traditions
British holidays and traditions British holidays and festivals
British holidays and festivals Bolivia holidays and festivals
Bolivia holidays and festivals Seaside holidays then and now
Seaside holidays then and now Chapter 5 section 4: the minor parties answer key
Chapter 5 section 4: the minor parties answer key Birthday party writing
Birthday party writing Define ideological parties
Define ideological parties Food feast meaning
Food feast meaning Les parties de la lettre commerciale
Les parties de la lettre commerciale Les parties de la lettre
Les parties de la lettre Les races de dauphins
Les races de dauphins Both parties deprecated war meaning
Both parties deprecated war meaning Dear interested
Dear interested Brainpop voting
Brainpop voting Francesco redi
Francesco redi Why does gatsby stop giving parties?
Why does gatsby stop giving parties? The smallest unit of election administration
The smallest unit of election administration Cours sur le texte narratif
Cours sur le texte narratif The spoils system made political parties more powerful by
The spoils system made political parties more powerful by 4 types of minor parties
4 types of minor parties Political parties
Political parties The supreme court change
The supreme court change Political party
Political party Sistemas democraticos
Sistemas democraticos