The Liver in Sickle Cell Disease Cage S





- Slides: 34

The Liver in Sickle Cell Disease Cage S. Johnson, M. D. Professor Emeritus of Medicine and of Physiology and Biophysics Director, Comprehensive Sickle Cell Center Keck School of Medicine, University of Southern California, Los Angeles, California, USA
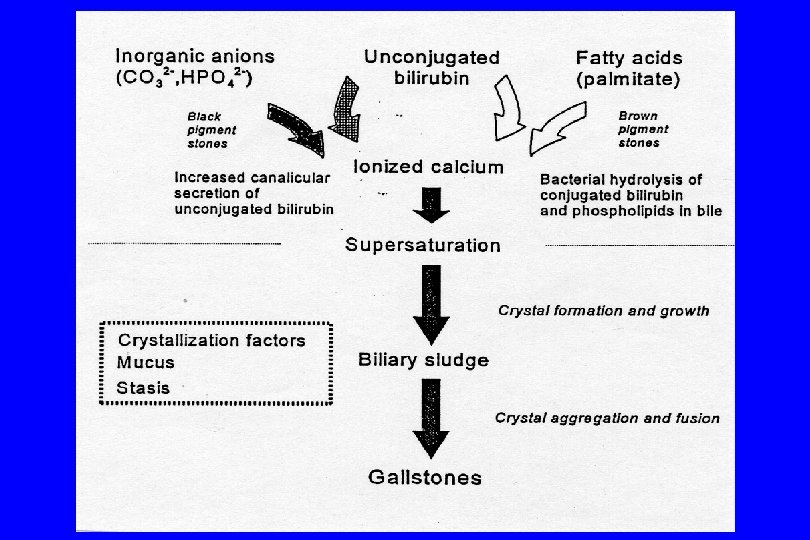
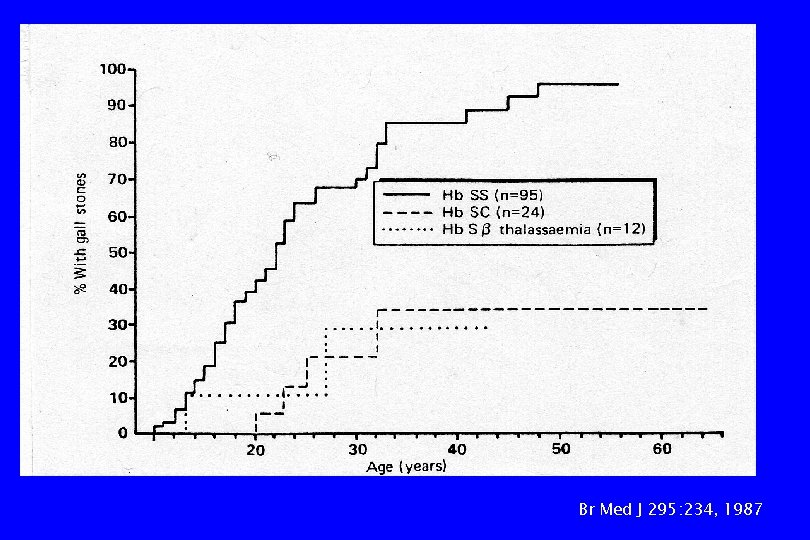
Hepato. Biliary Complications • • • hemolysis & accelerated bilirubin catabolism Transfusion therapy Vaso-occlusion Disorders unrelated to the hemoglobinopathy SS> SC> S-thalassemias
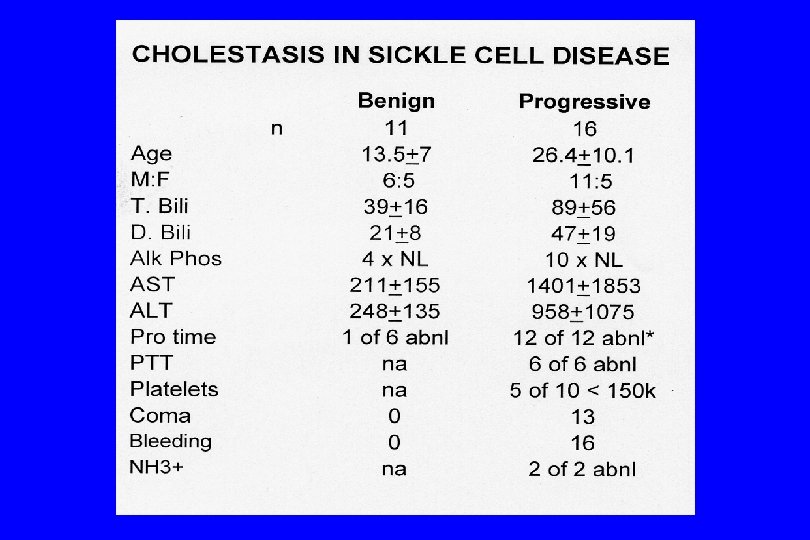
Hepato. Biliary Complications: • • • Hepatomegaly Hepatic ‘crisis’ (RUQ syndrome) Hepatitis: viral, drug-induced, auto-immune Hemosiderosis Cholestasis: benign, progressive, drug-induced Hepatic sequestration Cirrhosis Inspissated bile/Choledocholithiasis Wide differential diagnosis
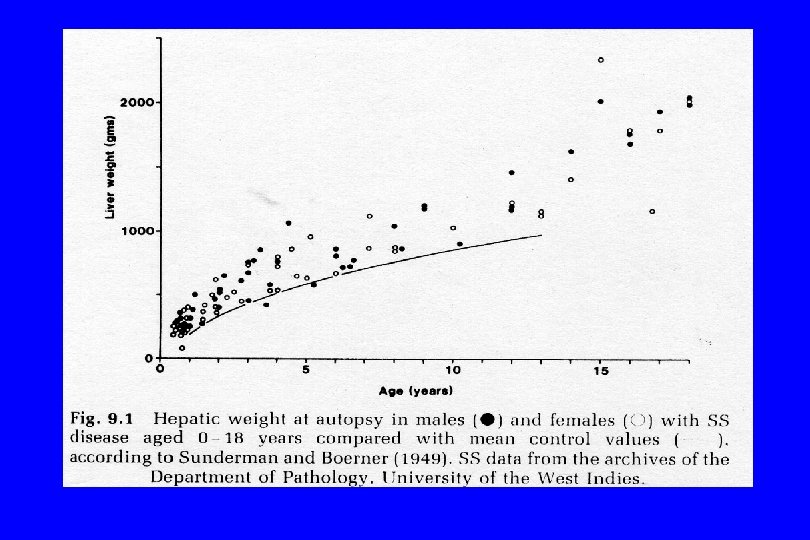
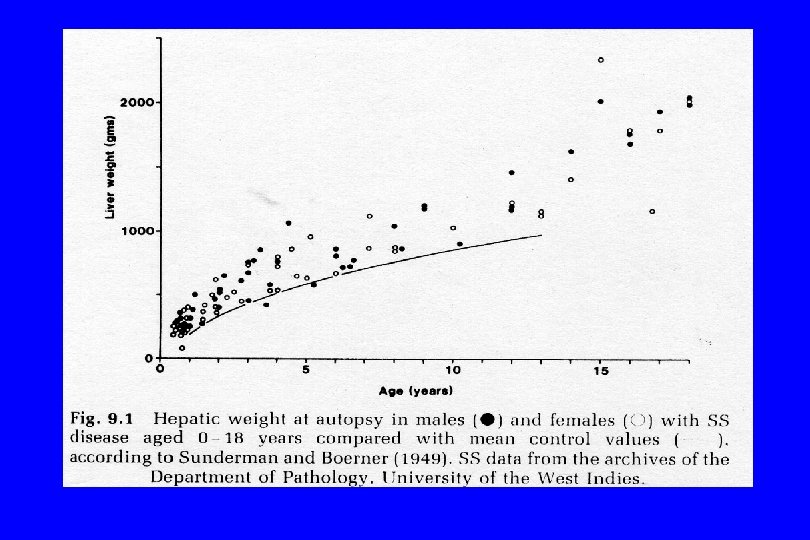
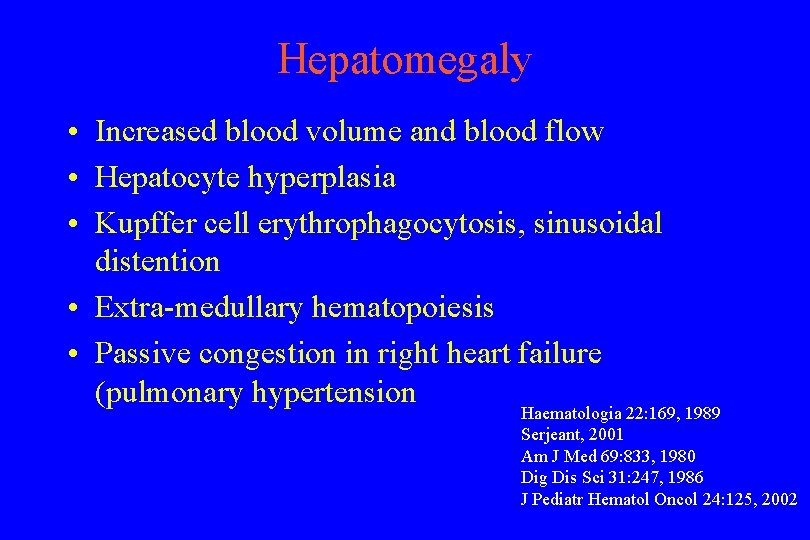
Hepatomegaly • Increased blood volume and blood flow • Hepatocyte hyperplasia • Kupffer cell erythrophagocytosis, sinusoidal distention • Extra-medullary hematopoiesis • Passive congestion in right heart failure (pulmonary hypertension Haematologia 22: 169, 1989 Serjeant, 2001 Am J Med 69: 833, 1980 Dig Dis Sci 31: 247, 1986 J Pediatr Hematol Oncol 24: 125, 2002
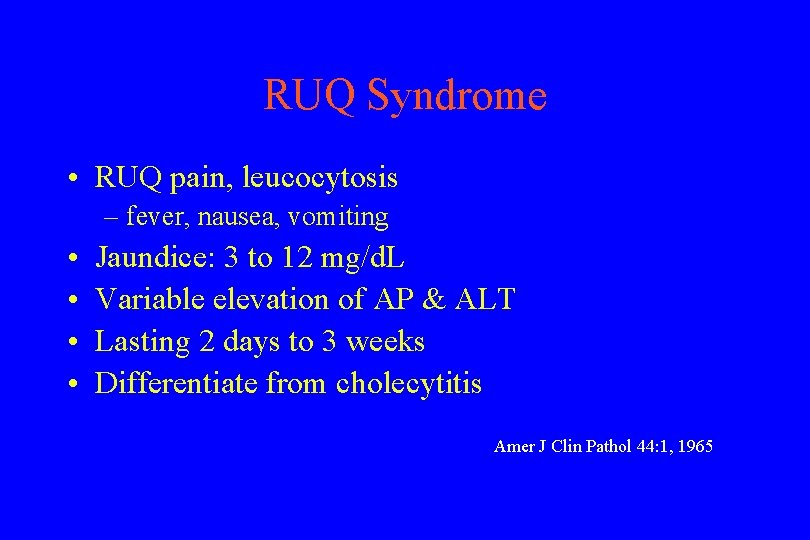
RUQ Syndrome • RUQ pain, leucocytosis – fever, nausea, vomiting • • Jaundice: 3 to 12 mg/d. L Variable elevation of AP & ALT Lasting 2 days to 3 weeks Differentiate from cholecytitis Amer J Clin Pathol 44: 1, 1965
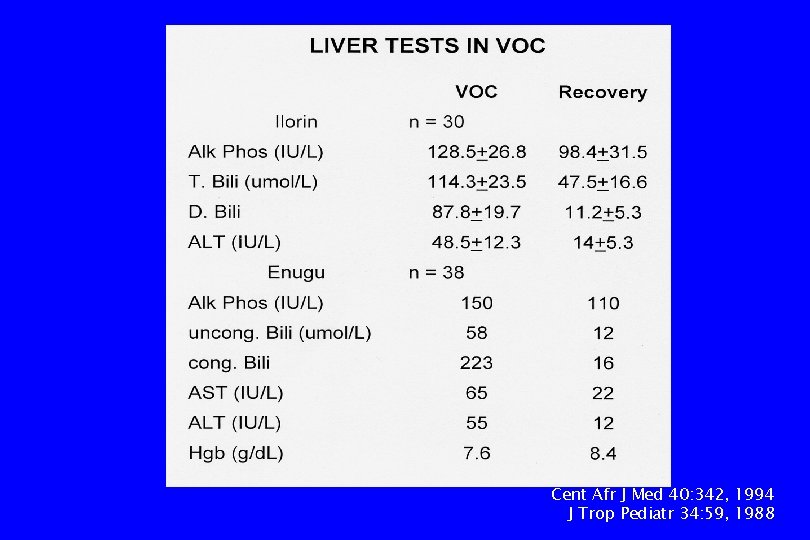
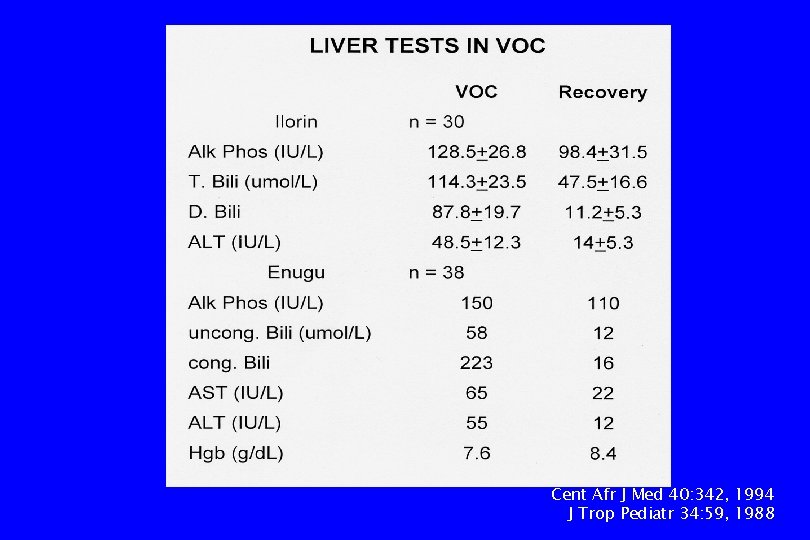
Cent Afr J Med 40: 342, 1994 J Trop Pediatr 34: 59, 1988
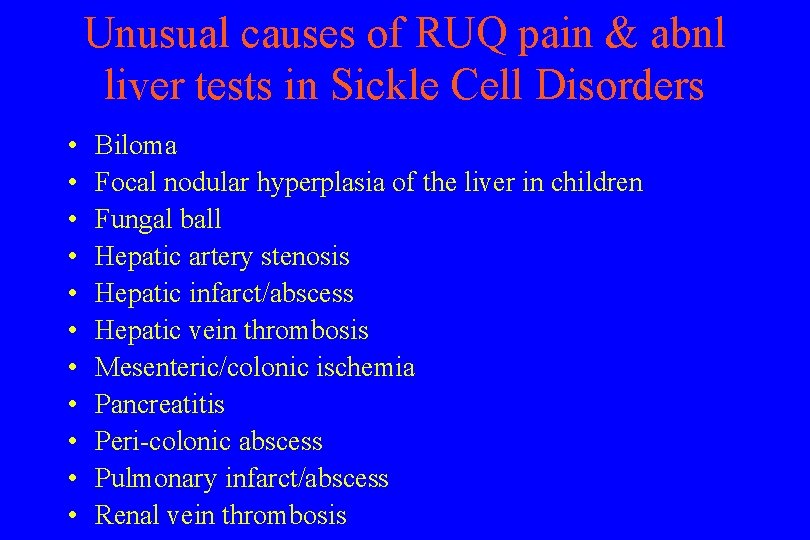
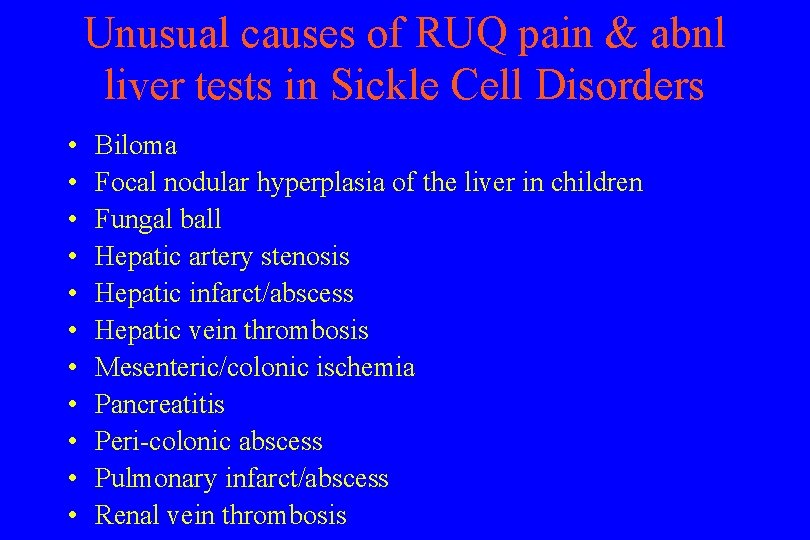
Unusual causes of RUQ pain & abnl liver tests in Sickle Cell Disorders • • • Biloma Focal nodular hyperplasia of the liver in children Fungal ball Hepatic artery stenosis Hepatic infarct/abscess Hepatic vein thrombosis Mesenteric/colonic ischemia Pancreatitis Peri-colonic abscess Pulmonary infarct/abscess Renal vein thrombosis
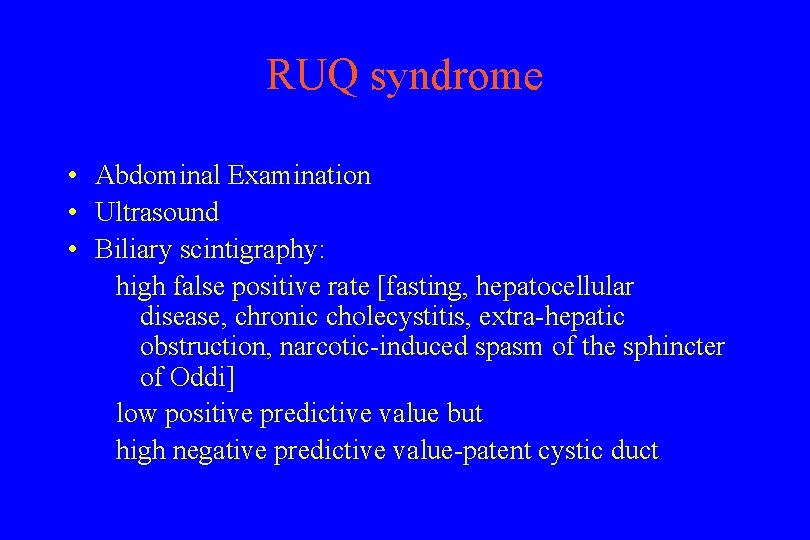
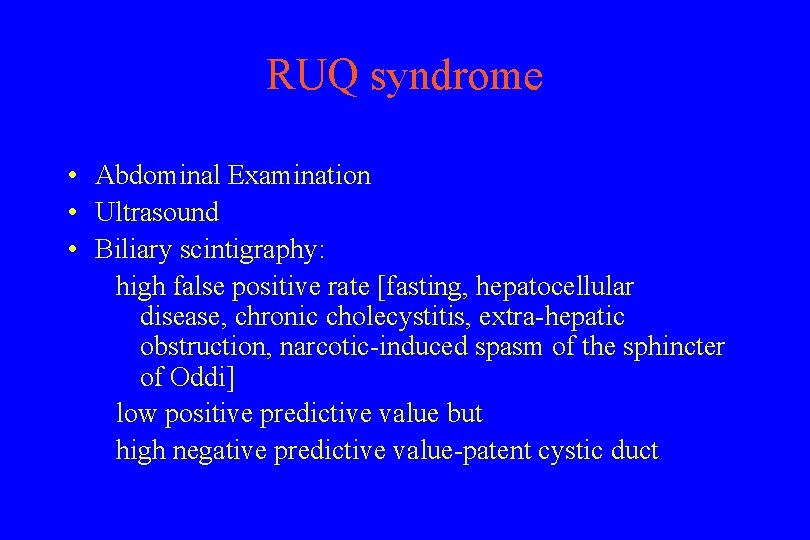
RUQ syndrome • Abdominal Examination • Ultrasound • Biliary scintigraphy: high false positive rate [fasting, hepatocellular disease, chronic cholecystitis, extra-hepatic obstruction, narcotic-induced spasm of the sphincter of Oddi] low positive predictive value but high negative predictive value-patent cystic duct
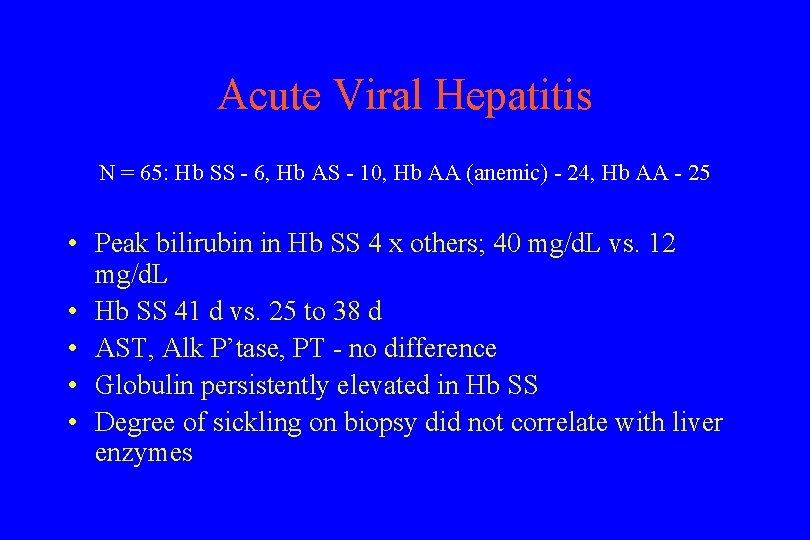
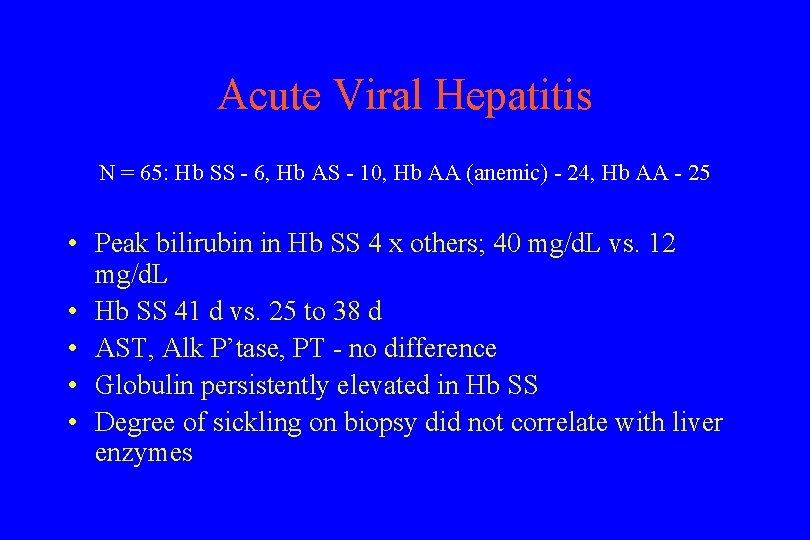
Acute Viral Hepatitis N = 65: Hb SS - 6, Hb AS - 10, Hb AA (anemic) - 24, Hb AA - 25 • Peak bilirubin in Hb SS 4 x others; 40 mg/d. L vs. 12 mg/d. L • Hb SS 41 d vs. 25 to 38 d • AST, Alk P’tase, PT - no difference • Globulin persistently elevated in Hb SS • Degree of sickling on biopsy did not correlate with liver enzymes
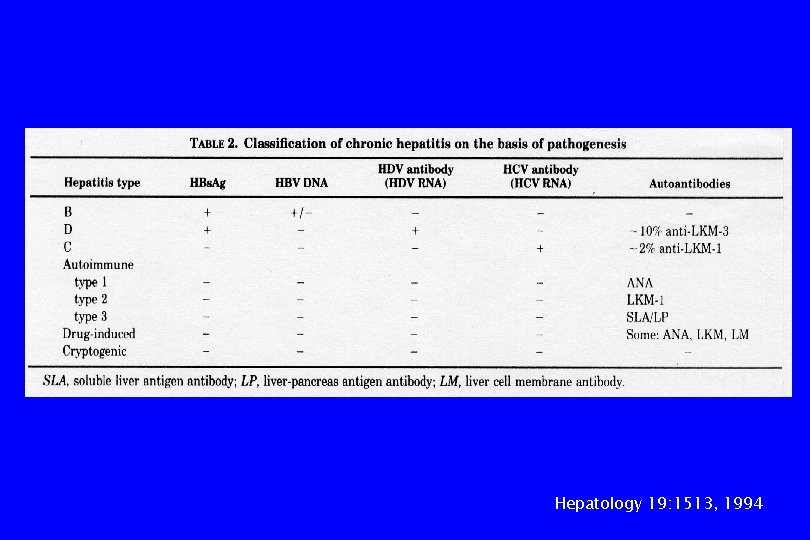
Hepatology 19: 1513, 1994
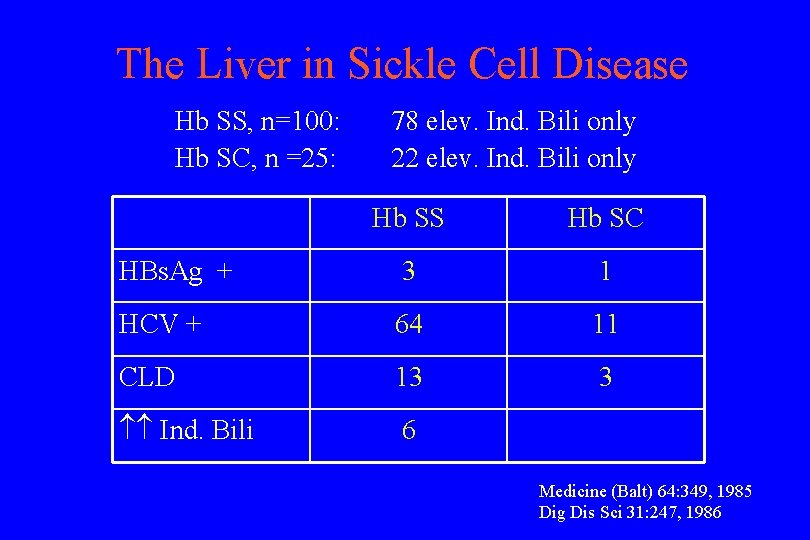
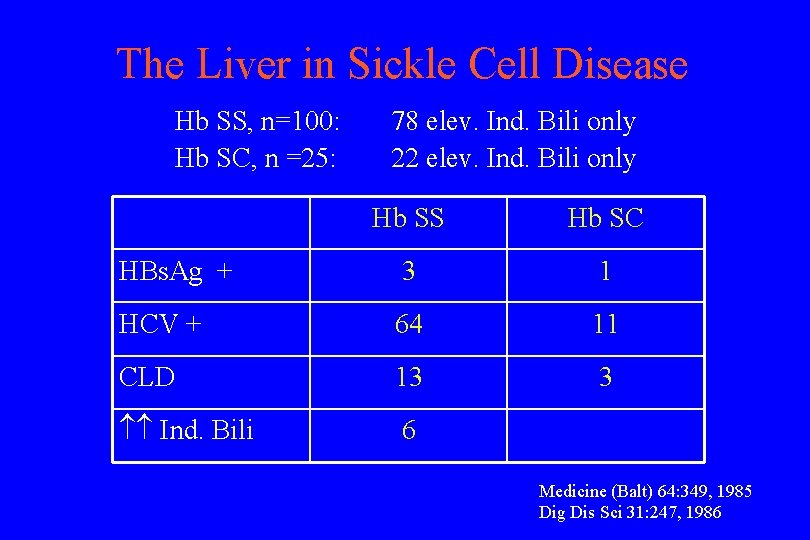
The Liver in Sickle Cell Disease Hb SS, n=100: Hb SC, n =25: 78 elev. Ind. Bili only 22 elev. Ind. Bili only Hb SS Hb SC HBs. Ag + 3 1 HCV + 64 11 CLD 13 3 Ind. Bili 6 Medicine (Balt) 64: 349, 1985 Dig Dis Sci 31: 247, 1986
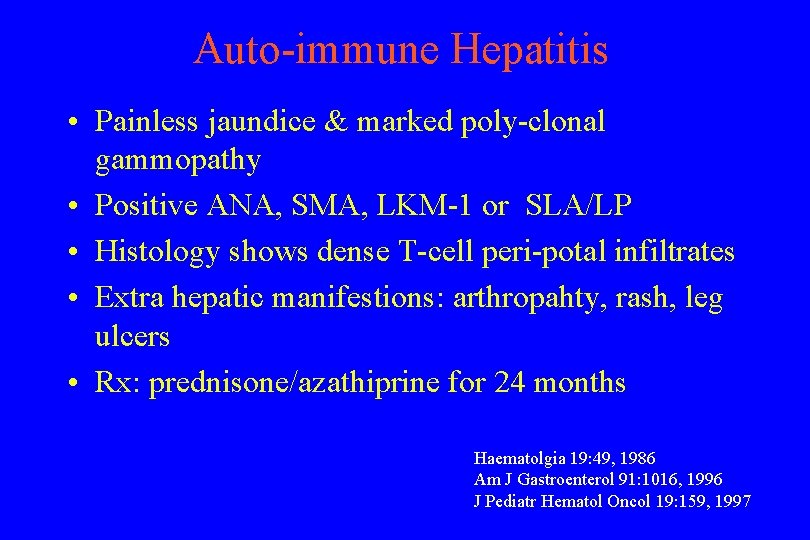
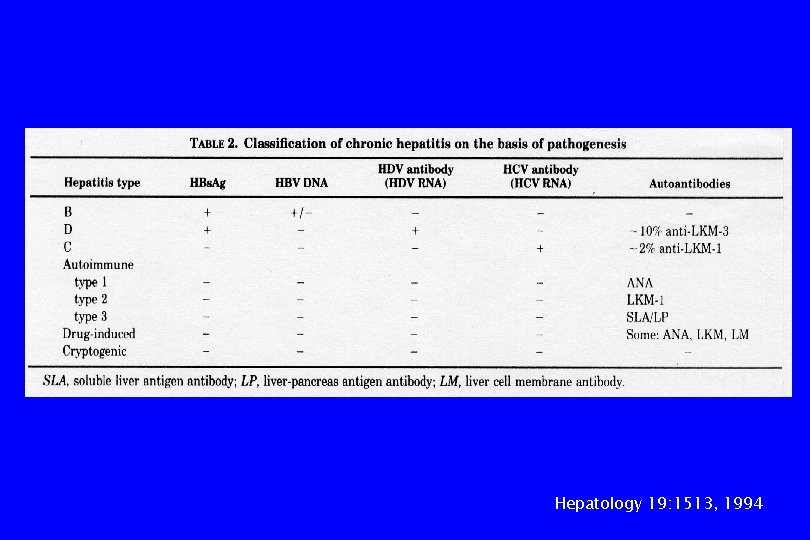
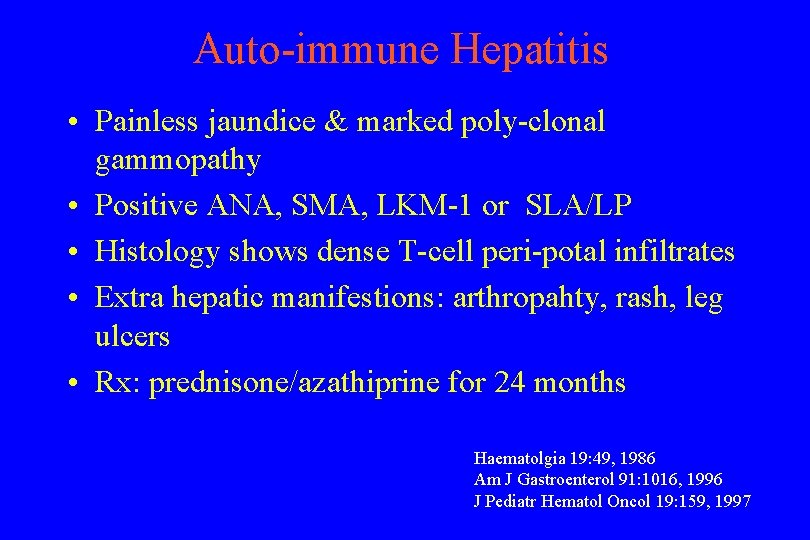
Auto-immune Hepatitis • Painless jaundice & marked poly-clonal gammopathy • Positive ANA, SMA, LKM-1 or SLA/LP • Histology shows dense T-cell peri-potal infiltrates • Extra hepatic manifestions: arthropahty, rash, leg ulcers • Rx: prednisone/azathiprine for 24 months Haematolgia 19: 49, 1986 Am J Gastroenterol 91: 1016, 1996 J Pediatr Hematol Oncol 19: 159, 1997
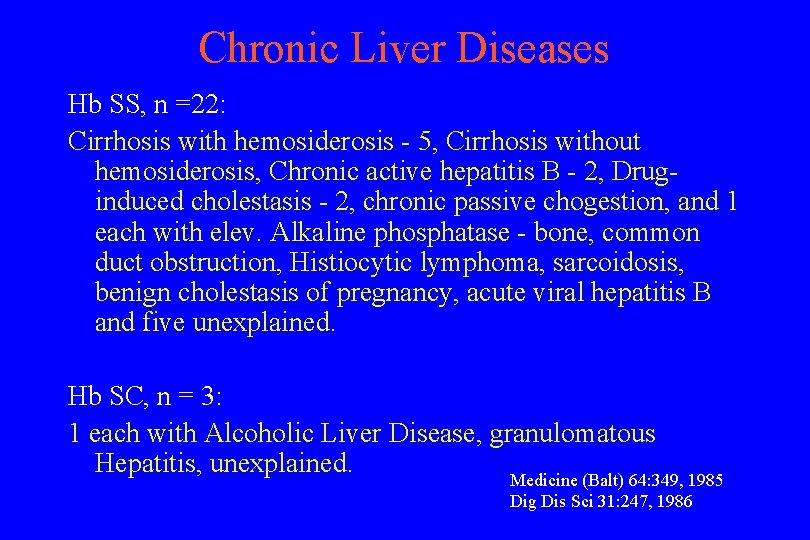
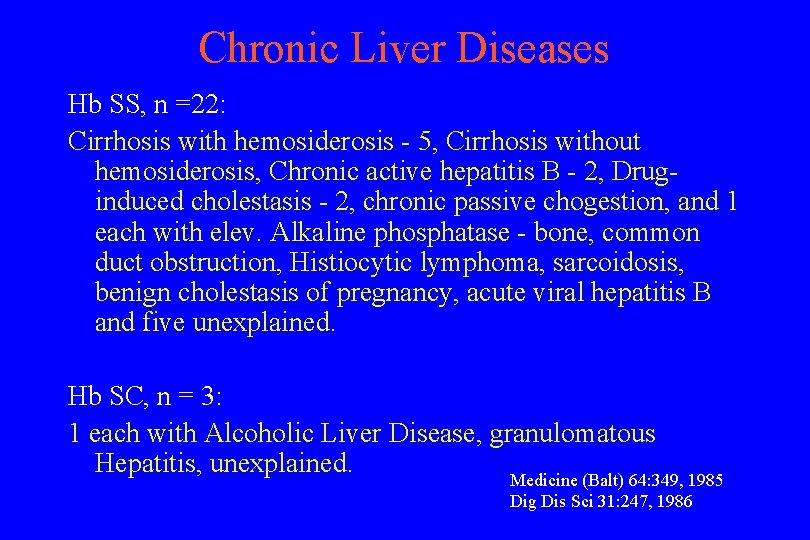
Chronic Liver Diseases Hb SS, n =22: Cirrhosis with hemosiderosis - 5, Cirrhosis without hemosiderosis, Chronic active hepatitis B - 2, Druginduced cholestasis - 2, chronic passive chogestion, and 1 each with elev. Alkaline phosphatase - bone, common duct obstruction, Histiocytic lymphoma, sarcoidosis, benign cholestasis of pregnancy, acute viral hepatitis B and five unexplained. Hb SC, n = 3: 1 each with Alcoholic Liver Disease, granulomatous Hepatitis, unexplained. Medicine (Balt) 64: 349, 1985 Dig Dis Sci 31: 247, 1986
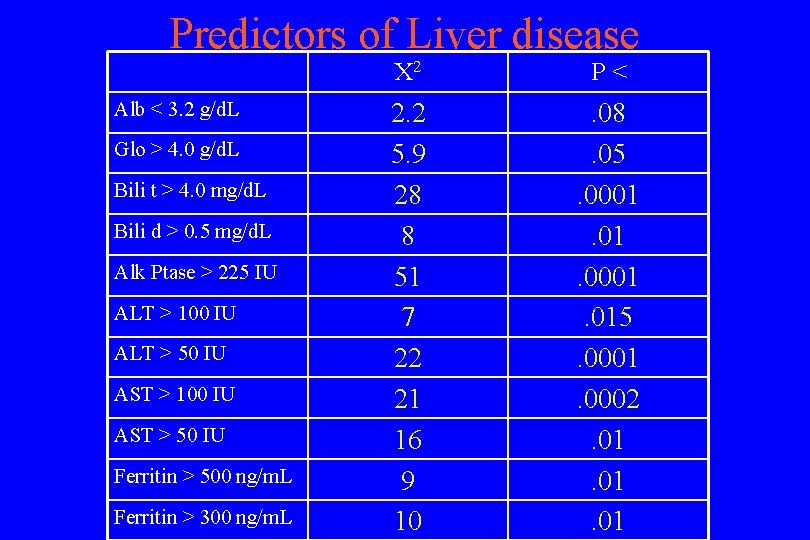
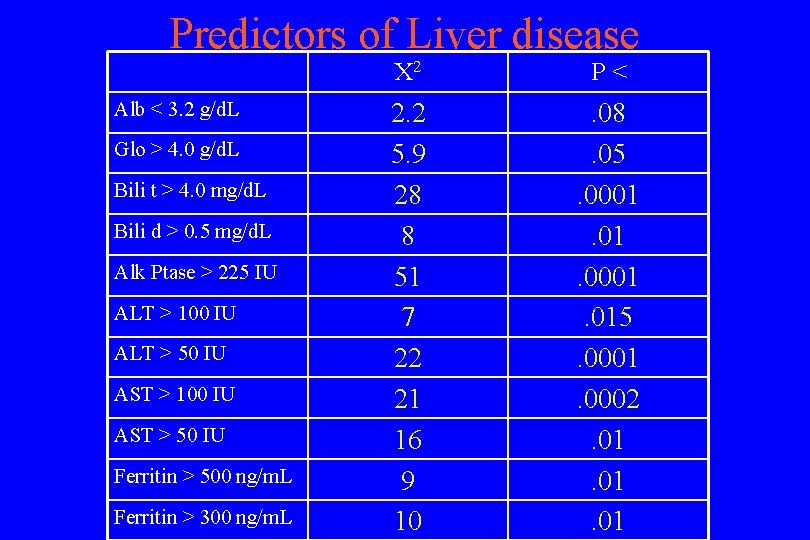
Predictors of Liver disease Alb < 3. 2 g/d. L Glo > 4. 0 g/d. L Bili t > 4. 0 mg/d. L Bili d > 0. 5 mg/d. L Alk Ptase > 225 IU ALT > 100 IU ALT > 50 IU AST > 100 IU AST > 50 IU Ferritin > 500 ng/m. L Ferritin > 300 ng/m. L X 2 P< 2. 2 5. 9 28 8 51 7 22 21 16 9 10 . 08. 05. 0001. 015. 0001. 0002. 01. 01
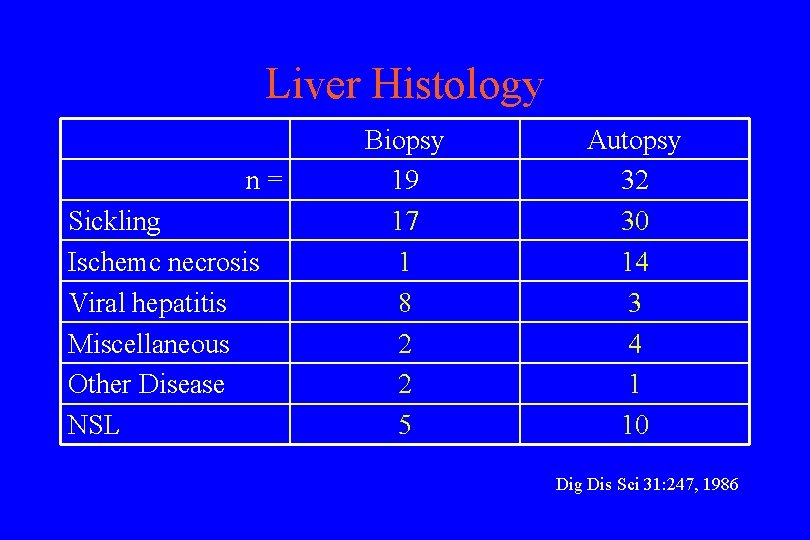
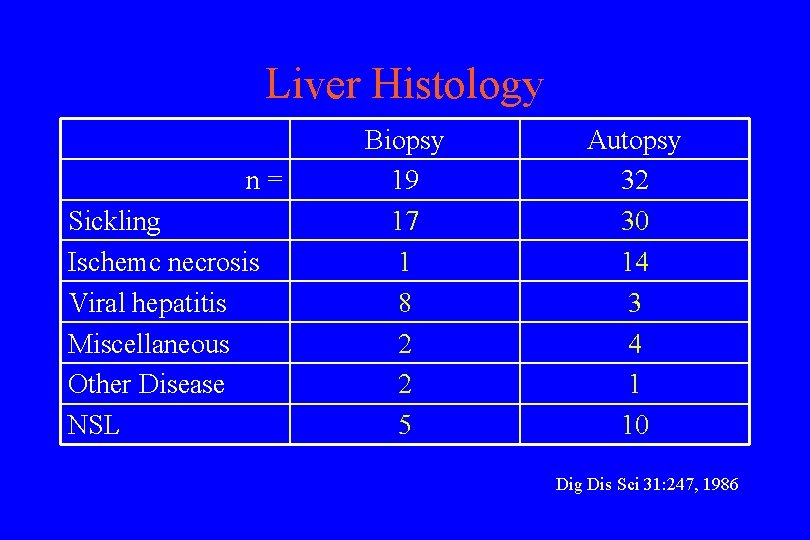
Liver Histology n= Sickling Ischemc necrosis Viral hepatitis Miscellaneous Other Disease NSL Biopsy 19 17 1 8 2 2 5 Autopsy 32 30 14 3 4 1 10 Dig Dis Sci 31: 247, 1986
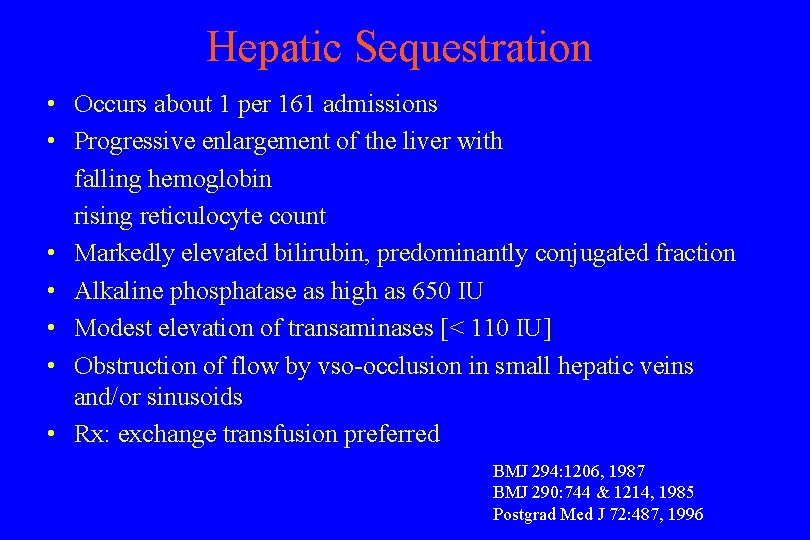
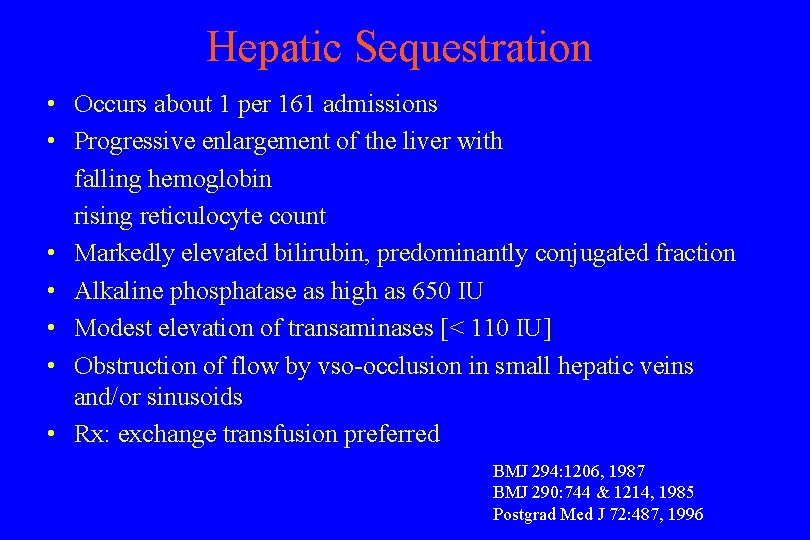
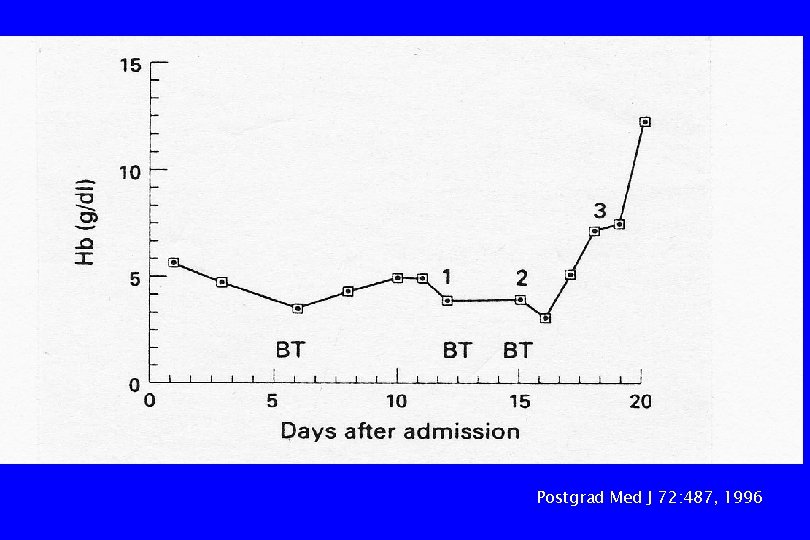
Hepatic Sequestration • Occurs about 1 per 161 admissions • Progressive enlargement of the liver with falling hemoglobin rising reticulocyte count • Markedly elevated bilirubin, predominantly conjugated fraction • Alkaline phosphatase as high as 650 IU • Modest elevation of transaminases [< 110 IU] • Obstruction of flow by vso-occlusion in small hepatic veins and/or sinusoids • Rx: exchange transfusion preferred BMJ 294: 1206, 1987 BMJ 290: 744 & 1214, 1985 Postgrad Med J 72: 487, 1996
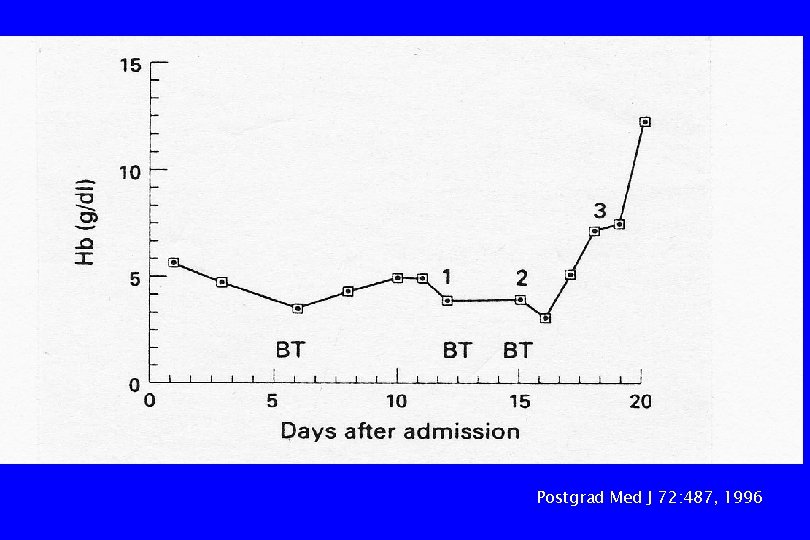
Postgrad Med J 72: 487, 1996
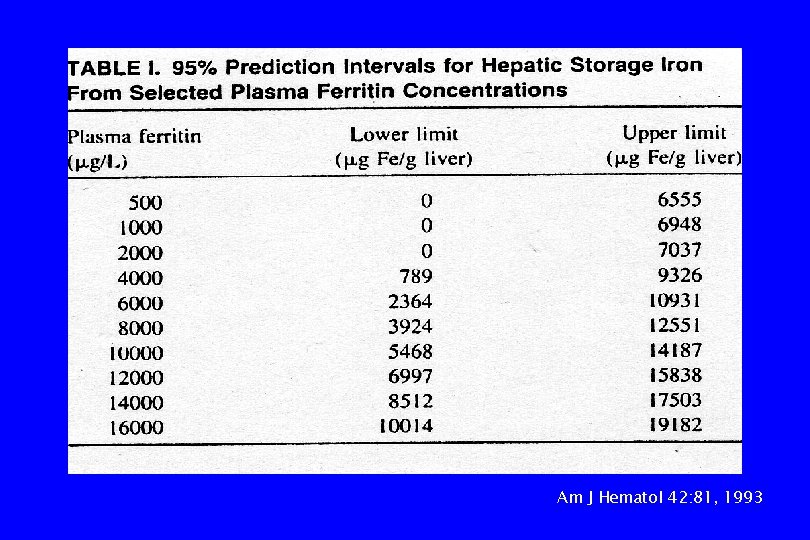
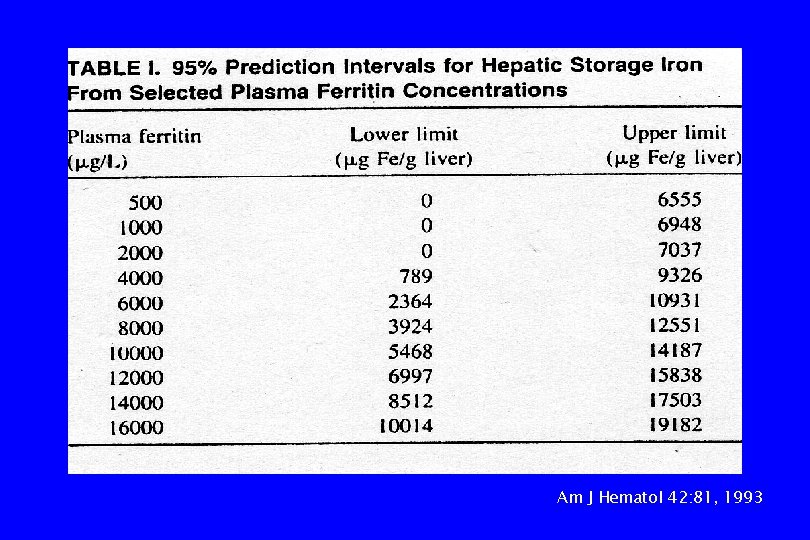
Am J Hematol 42: 81, 1993

Br J Haematol 89: 757, 1995
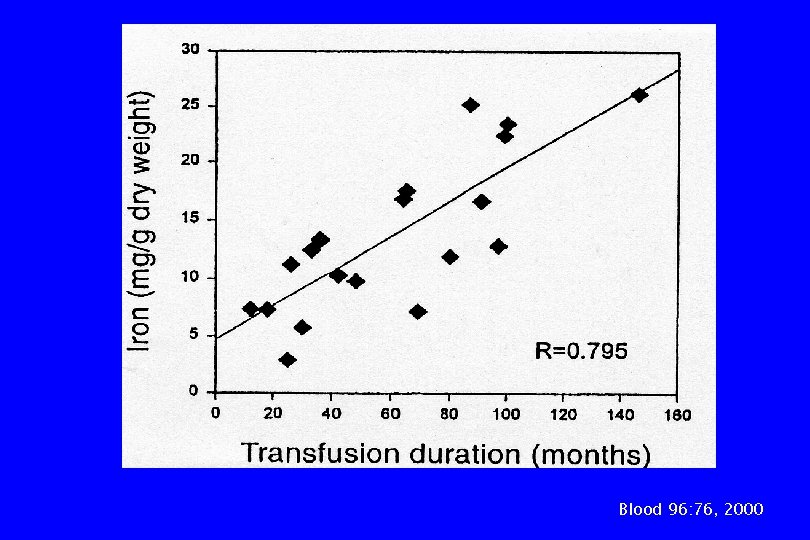
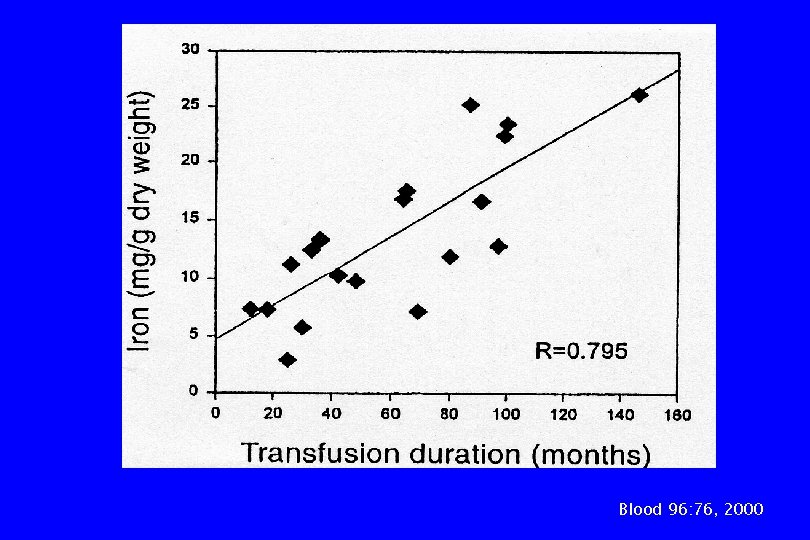
Blood 96: 76, 2000

Blood 96: 76, 2000
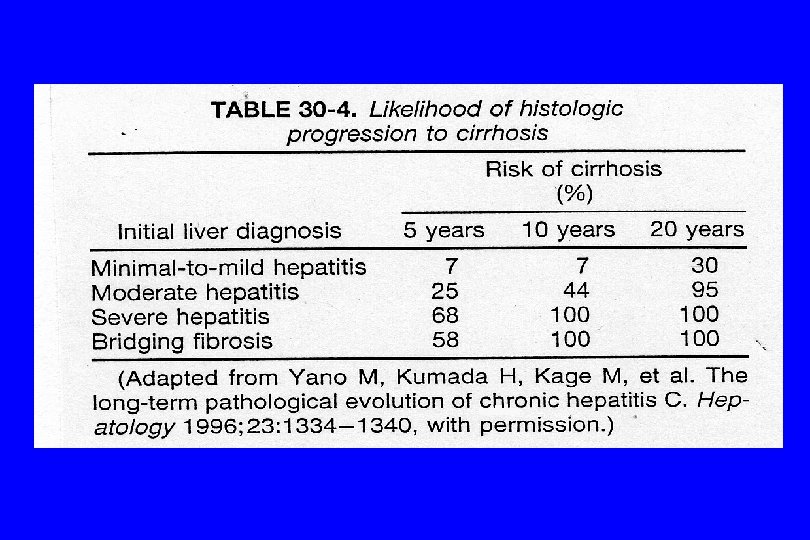
Cirrhosis • • Hepatitis B or C, auto-immune Hemochromatosis Chronic passive congestion Miscellaneous: alcohol, toxins, sarcoidosis, cryptogenic, chronic biliary obstruction
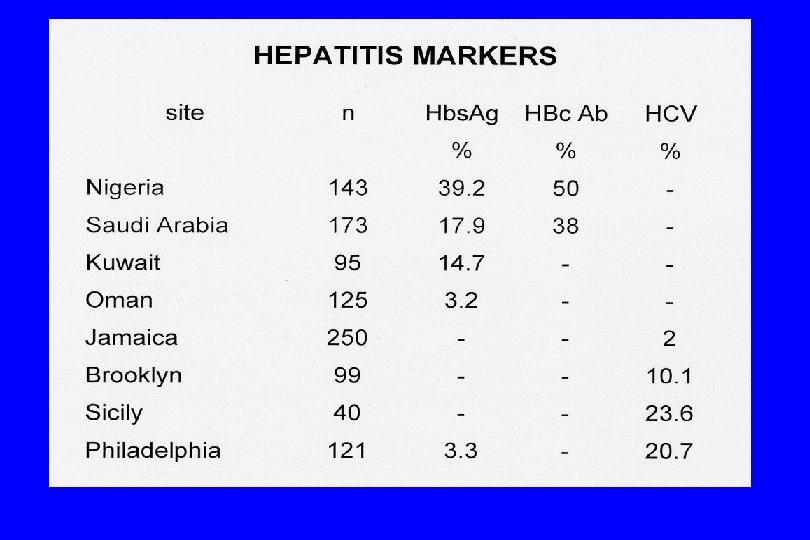
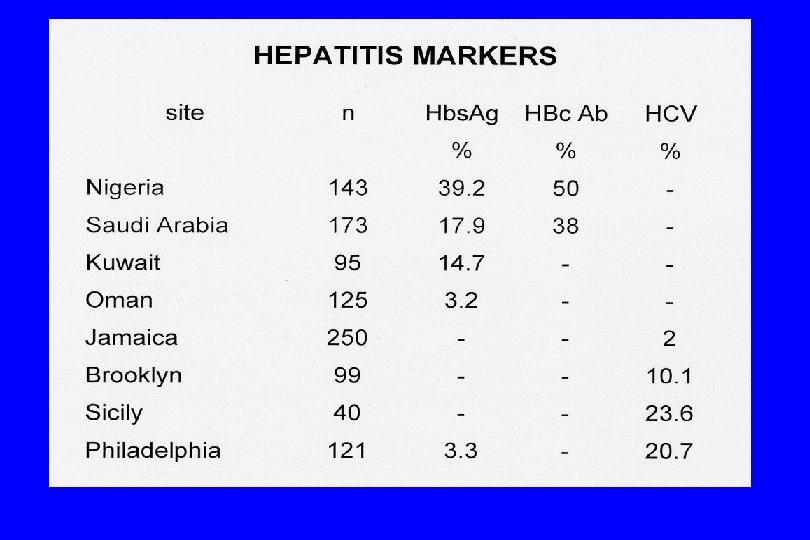
Summary 1. The majority of patients have only elevations of indirect bilirubin and LDH due to hemolysis 2. Chronic abnormalities in liver function are due to a wide variety of disorders other than the hemoglobinopathy. Judicious use of liver biopsy is often required for specific diagnosis. 3. Evidence for hepatitis B and C infection is common. Patients seropositive for hepatitis C have significantly greater serum globulin and transaminase levels than those seronegative.
Summary 4. Kuppfer cell erythrophagocytosis and intrasinusoidal sickling are universally found in hepatic histology and are not related to the degree of transaminase elevation. The absence of shrunken hepatocytes speaks against the concept of anoxic liver damage and is more consistent with the liver as the site of RBC destruction in the absence of splenic function. 5. The increasing use of transfusion therapy in this patient population is associated with a high frequency of trnasfusion transmitted viral disease and iron overload; prudence dictates ongoing surveillance for these and other liver disorders that may affect these patients.
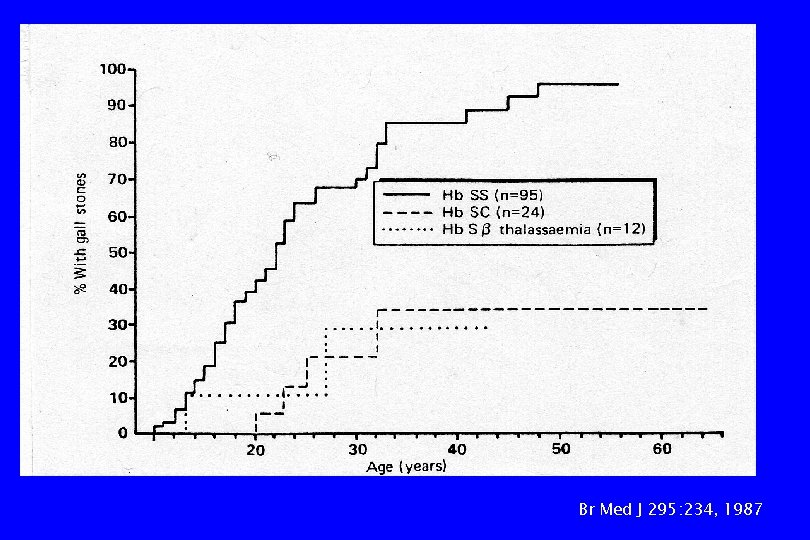
Br Med J 295: 234, 1987
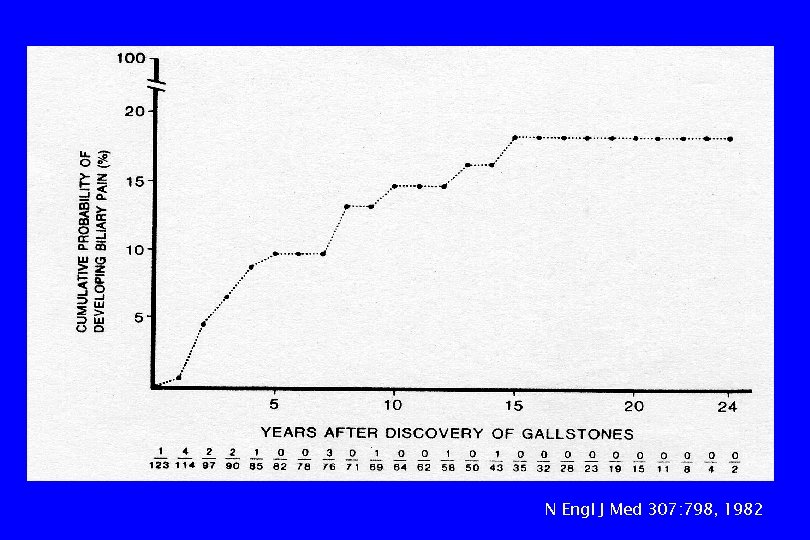
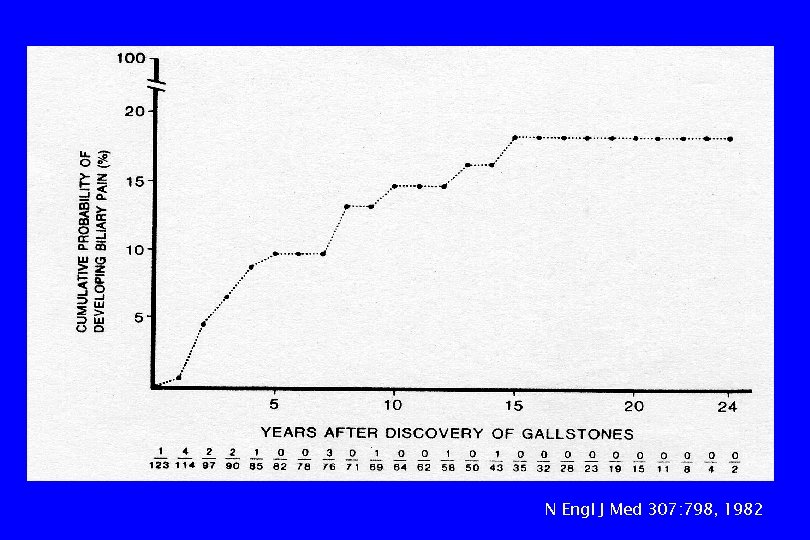
N Engl J Med 307: 798, 1982


J Pediatr 136: 80, 2000
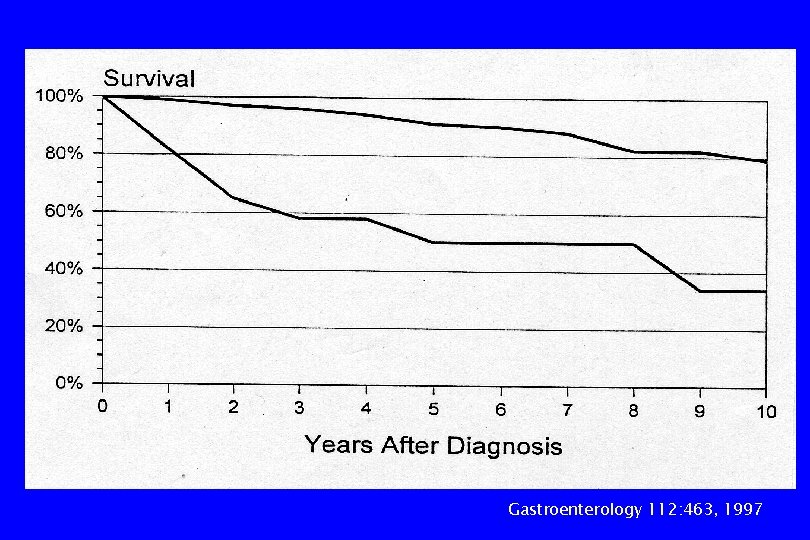
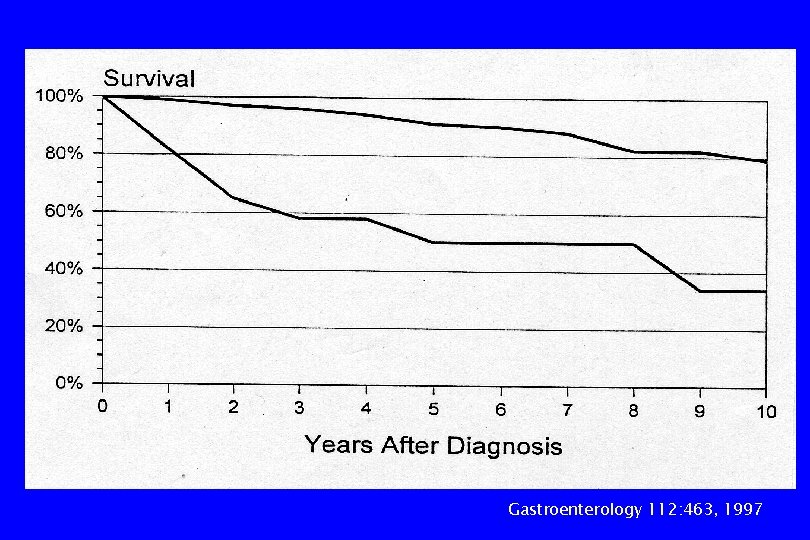
Gastroenterology 112: 463, 1997
 Gene therapy for sickle cell disease
Gene therapy for sickle cell disease Incomplete dominance
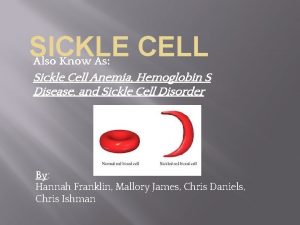
Incomplete dominance Types of sickle cell disease
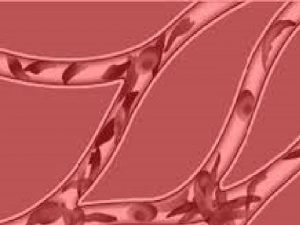
Types of sickle cell disease Sickle cells
Sickle cells Types of sickle cell disease
Types of sickle cell disease Multiple alleles example blood type
Multiple alleles example blood type Chapter 14 the human genome making karyotypes answer key
Chapter 14 the human genome making karyotypes answer key Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Sickle cell hemoglobin structure
Sickle cell hemoglobin structure Difference between sickle cell anaemia and thalassemia
Difference between sickle cell anaemia and thalassemia Sickle cell anemia lab values
Sickle cell anemia lab values Cri du chat chromosomal abnormalities
Cri du chat chromosomal abnormalities Protein synthesis and mutations
Protein synthesis and mutations Pethidine in sickle cell
Pethidine in sickle cell Hemophilia karyotype picture
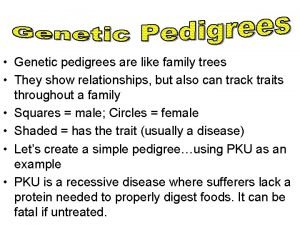
Hemophilia karyotype picture Pedigree key
Pedigree key Sickle cell hemoglobin structure
Sickle cell hemoglobin structure Sickle cell punnett square
Sickle cell punnett square Is sickle cell anemia codominant
Is sickle cell anemia codominant Sickle cell osteomyelitis
Sickle cell osteomyelitis Blood
Blood Sickle blood cell
Sickle blood cell Sickle cell anemia
Sickle cell anemia Codominance
Codominance Old world flycatchers
Old world flycatchers Nata sickle cell
Nata sickle cell Sickle cell anemia
Sickle cell anemia Sickle cell pain
Sickle cell pain Hemoglobin electrophoresis
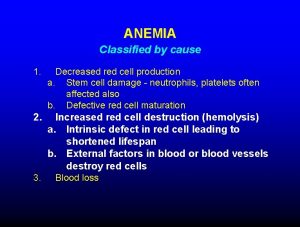
Hemoglobin electrophoresis Anemia
Anemia Everardo cobos
Everardo cobos Inheritance pattern of sickle cell anemia
Inheritance pattern of sickle cell anemia Sickle cell anemia dna sequence
Sickle cell anemia dna sequence Persilangan anemia sel sabit
Persilangan anemia sel sabit Pbs sickle cell
Pbs sickle cell