Texas Medicaid and Health Care Reform 2010 Health


- Slides: 32
Texas Medicaid and Health Care Reform 2010 Health Law Conference Houston, TX - Four Seasons Hotel April 9, 2010 Bryan Sperry, bryansperry@childhealthtx. org Children's Hospital Association of Texas (CHAT) – www. childhealthtx. org Anne Dunkelberg, Associate Director, dunkelberg@cppp. org Center for Public Policy Priorities – www. cppp. org www. texasvoiceforhealthreform. org
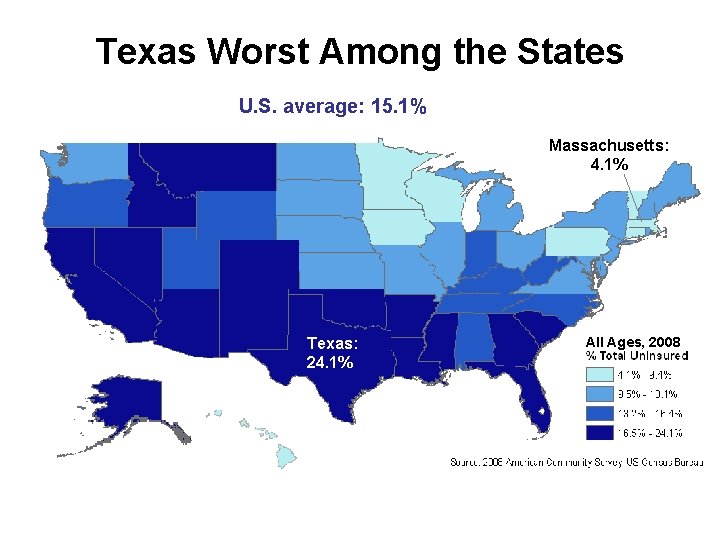
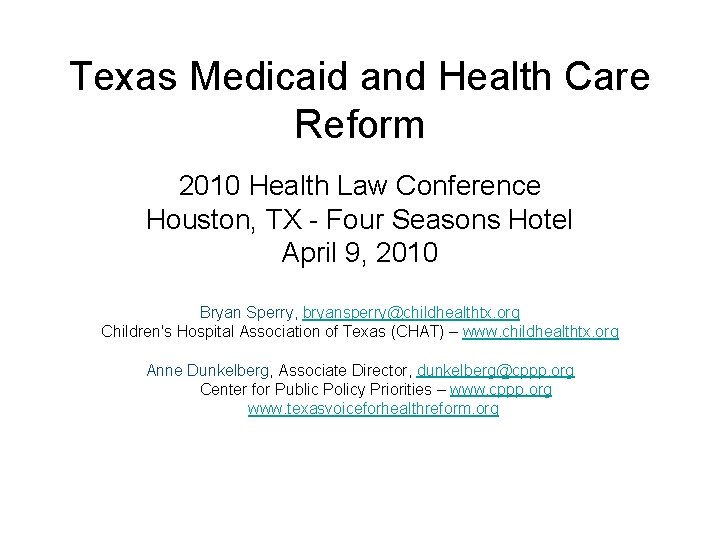
Texas Worst Among the States U. S. average: 15. 1% Massachusetts: 4. 1% Texas: 24. 1% All Ages, 2008
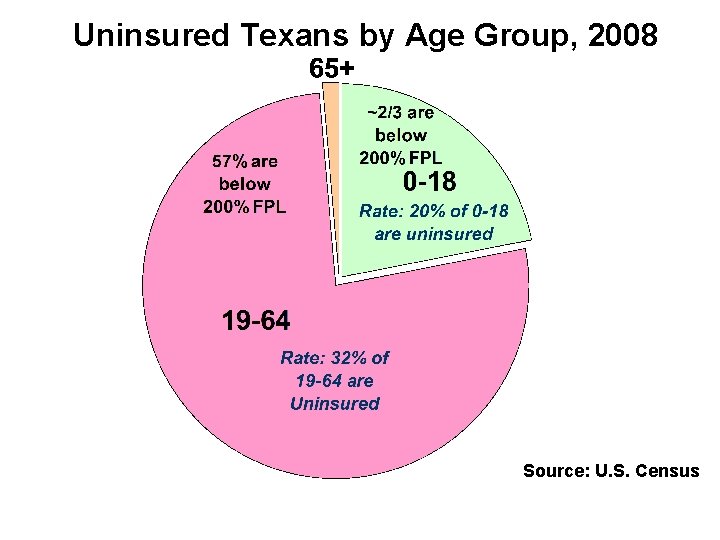
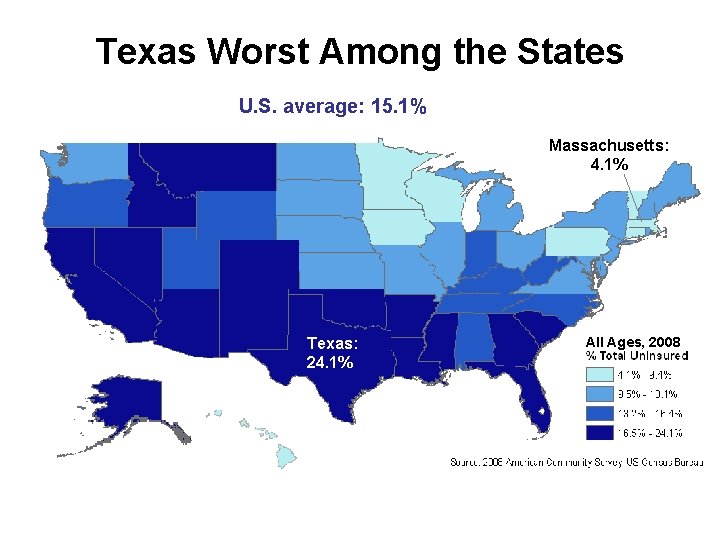
Uninsured Texans by Age Group, 2008 Source: U. S. Census
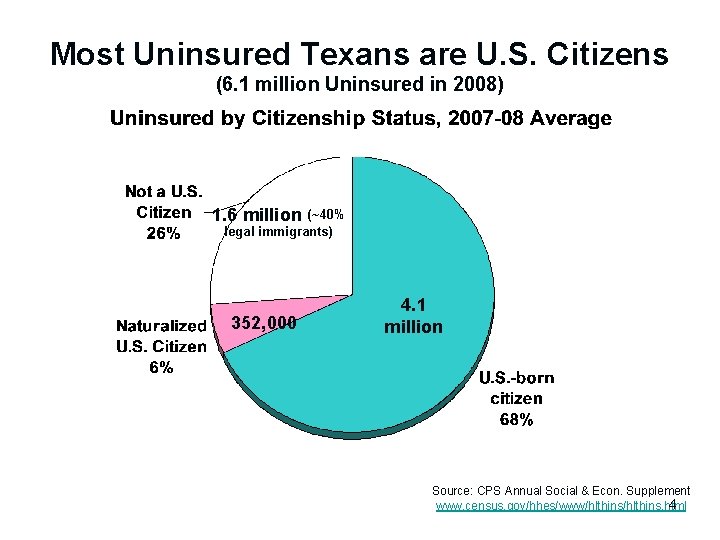
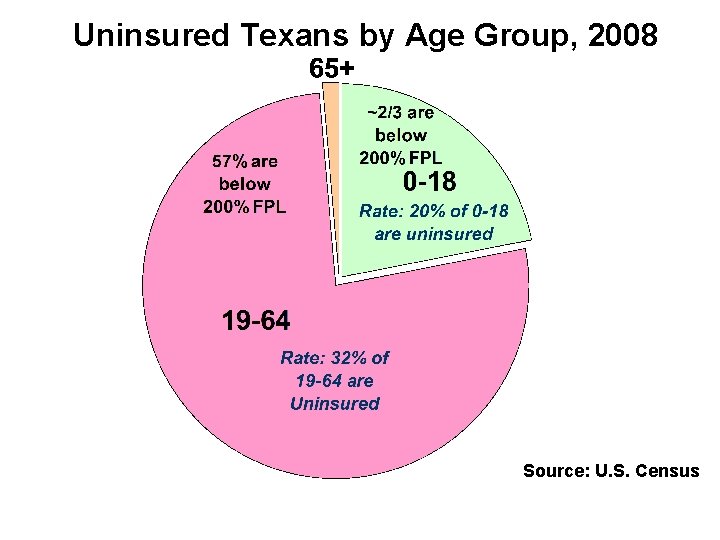
Most Uninsured Texans are U. S. Citizens (6. 1 million Uninsured in 2008) 1. 6 million (~40% legal immigrants) 352, 000 4. 1 million Source: CPS Annual Social & Econ. Supplement 4 www. census. gov/hhes/www/hlthins. html
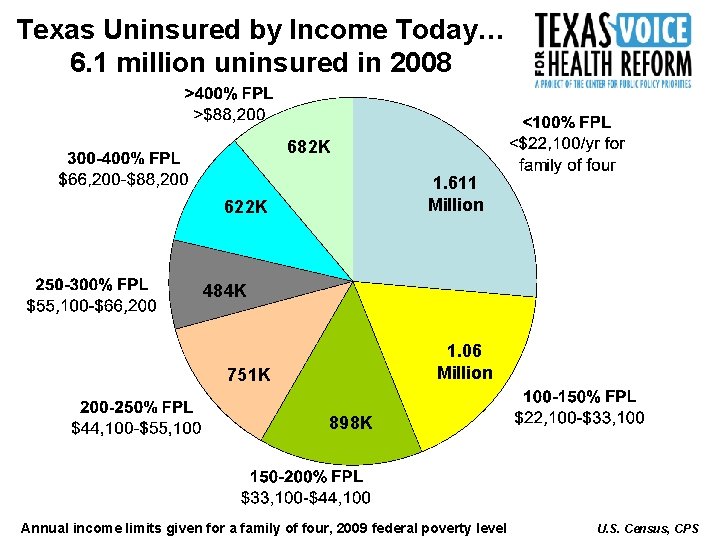
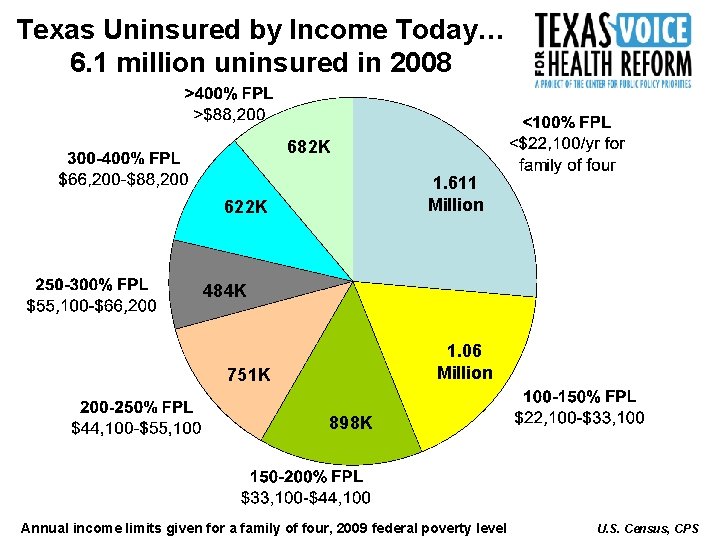
Texas Uninsured by Income Today… 6. 1 million uninsured in 2008 682 K 1. 611 Million 622 K 484 K 1. 06 Million 751 K 898 K Annual income limits given for a family of four, 2009 federal poverty level U. S. Census, CPS
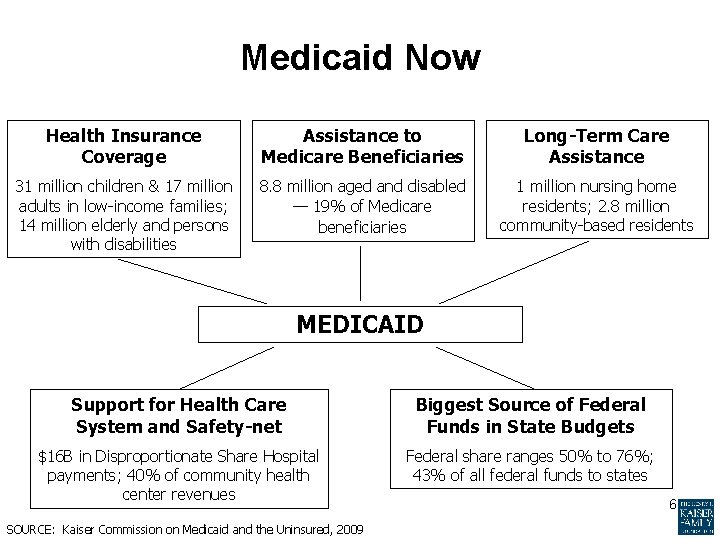
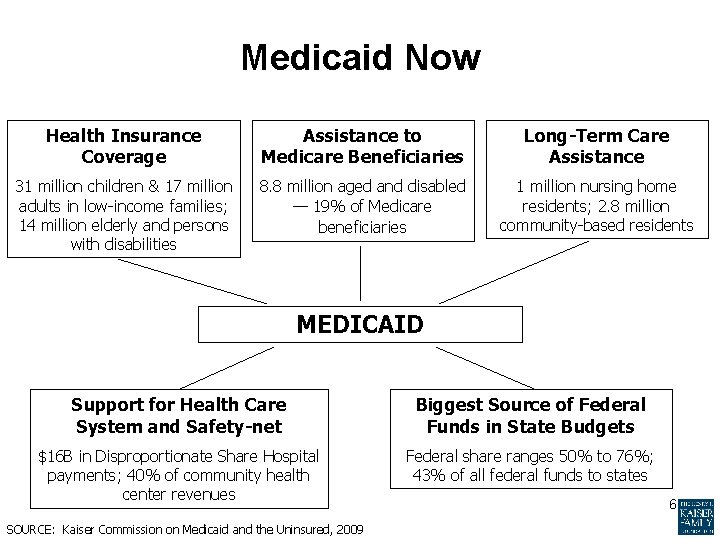
Medicaid Now Health Insurance Coverage Assistance to Medicare Beneficiaries Long-Term Care Assistance 31 million children & 17 million adults in low-income families; 14 million elderly and persons with disabilities 8. 8 million aged and disabled — 19% of Medicare beneficiaries 1 million nursing home residents; 2. 8 million community-based residents MEDICAID Support for Health Care System and Safety-net Biggest Source of Federal Funds in State Budgets $16 B in Disproportionate Share Hospital payments; 40% of community health center revenues Federal share ranges 50% to 76%; 43% of all federal funds to states SOURCE: Kaiser Commission on Medicaid and the Uninsured, 2009 6
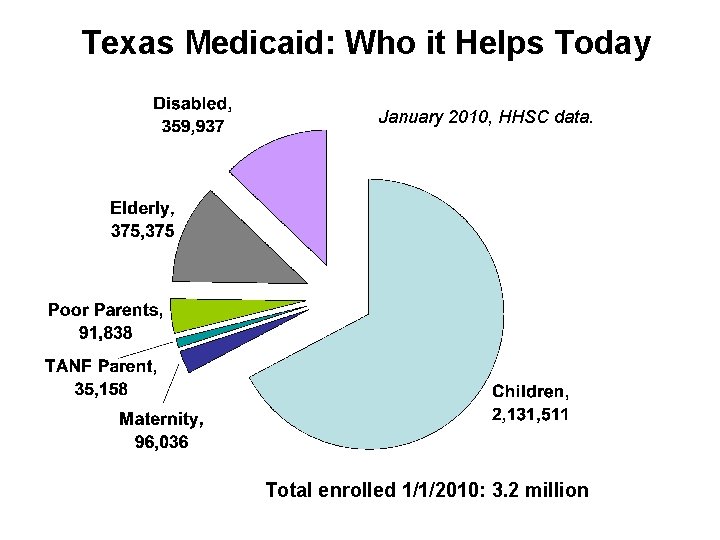
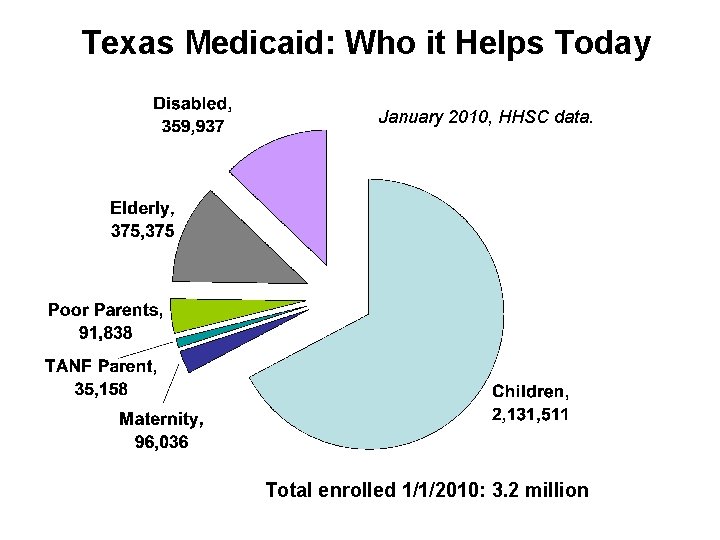
Texas Medicaid: Who it Helps Today January 2010, HHSC data. Total enrolled 1/1/2010: 3. 2 million

8
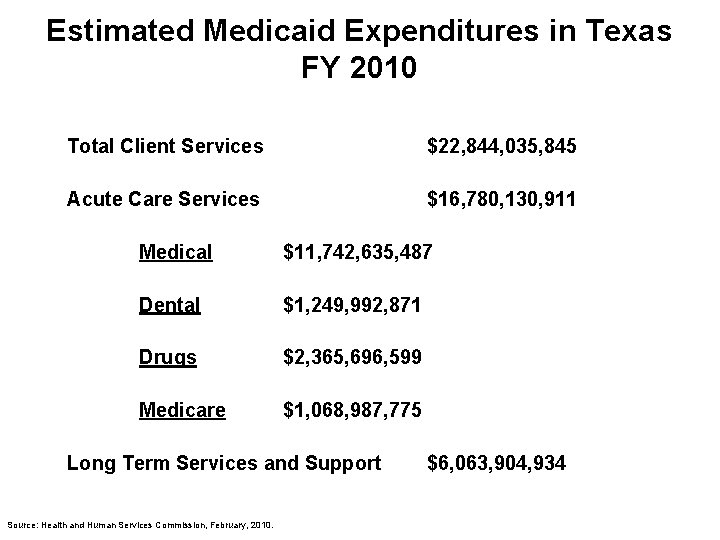
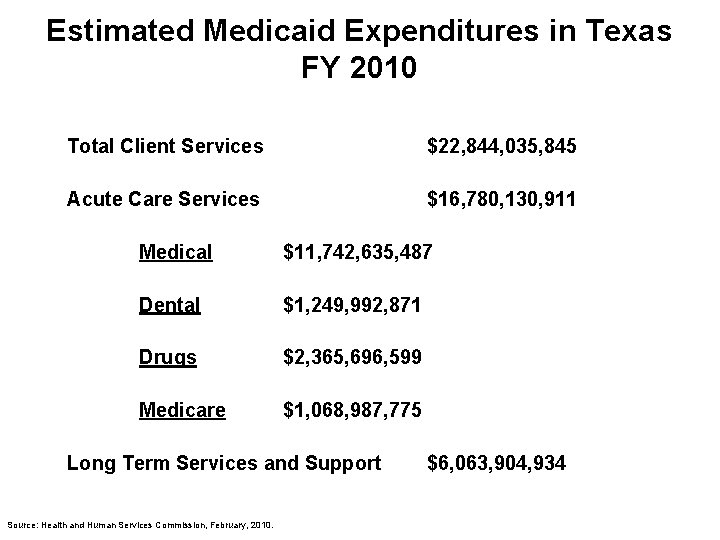
Estimated Medicaid Expenditures in Texas FY 2010 Total Client Services $22, 844, 035, 845 Acute Care Services $16, 780, 130, 911 Medical $11, 742, 635, 487 Dental $1, 249, 992, 871 Drugs $2, 365, 696, 599 Medicare $1, 068, 987, 775 Long Term Services and Support Source: Health and Human Services Commission, February, 2010. $6, 063, 904, 934
Medicaid Caseload and Cost Proportions 10

11
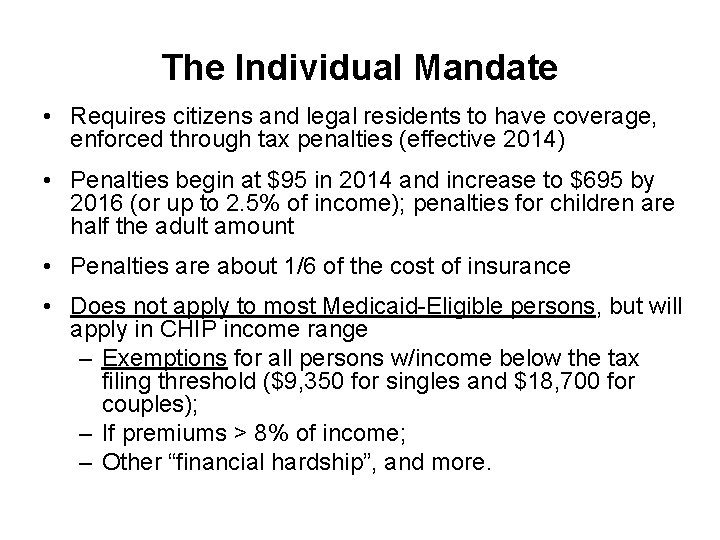
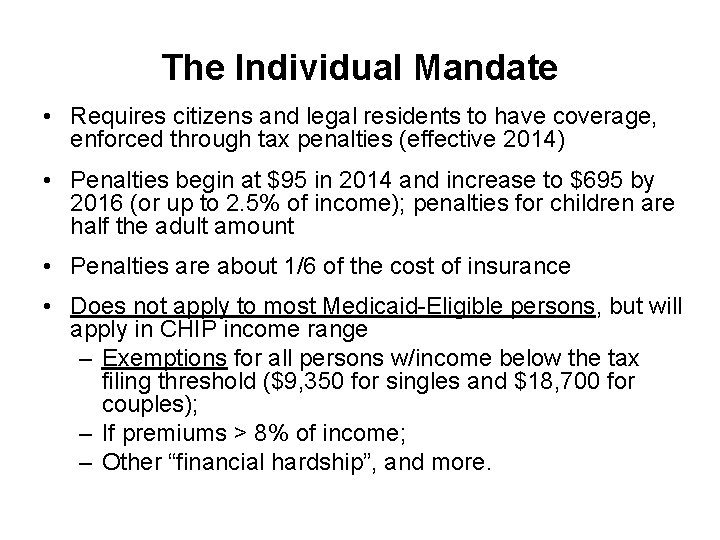
The Individual Mandate • Requires citizens and legal residents to have coverage, enforced through tax penalties (effective 2014) • Penalties begin at $95 in 2014 and increase to $695 by 2016 (or up to 2. 5% of income); penalties for children are half the adult amount • Penalties are about 1/6 of the cost of insurance • Does not apply to most Medicaid-Eligible persons, but will apply in CHIP income range – Exemptions for all persons w/income below the tax filing threshold ($9, 350 for singles and $18, 700 for couples); – If premiums > 8% of income; – Other “financial hardship”, and more.
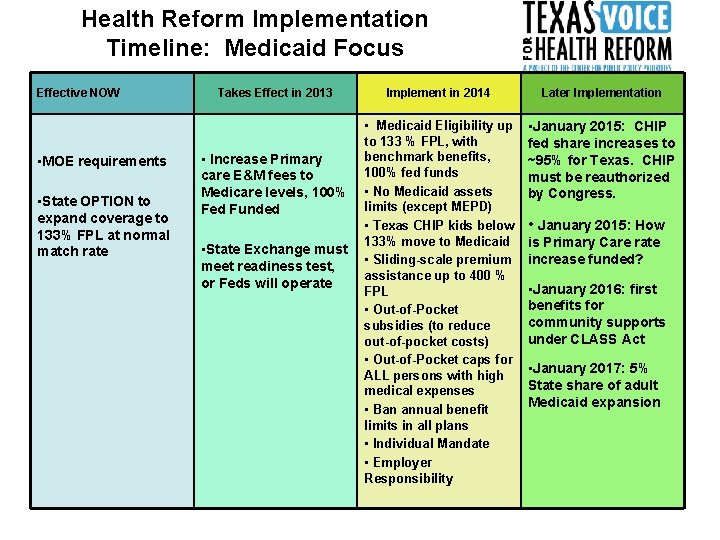
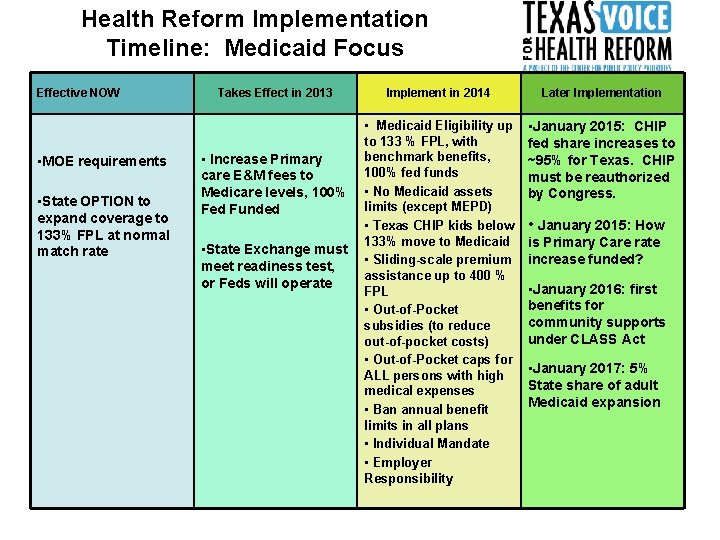
Health Reform Implementation Timeline: Medicaid Focus Effective NOW • MOE requirements • State OPTION to expand coverage to 133% FPL at normal match rate Takes Effect in 2013 • Increase Primary care E&M fees to Medicare levels, 100% Fed Funded • State Exchange must meet readiness test, or Feds will operate Implement in 2014 Later Implementation • Medicaid Eligibility up to 133 % FPL, with benchmark benefits, 100% fed funds • No Medicaid assets limits (except MEPD) • Texas CHIP kids below 133% move to Medicaid • Sliding-scale premium assistance up to 400 % FPL • Out-of-Pocket subsidies (to reduce out-of-pocket costs) • Out-of-Pocket caps for ALL persons with high medical expenses • Ban annual benefit limits in all plans • Individual Mandate • Employer Responsibility • January 2015: CHIP fed share increases to ~95% for Texas. CHIP must be reauthorized by Congress. • January 2015: How is Primary Care rate increase funded? • January 2016: first benefits for community supports under CLASS Act • January 2017: 5% State share of adult Medicaid expansion
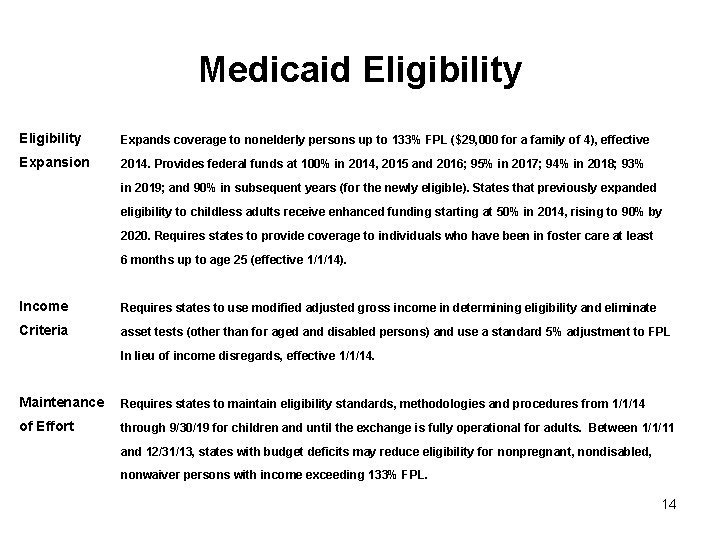
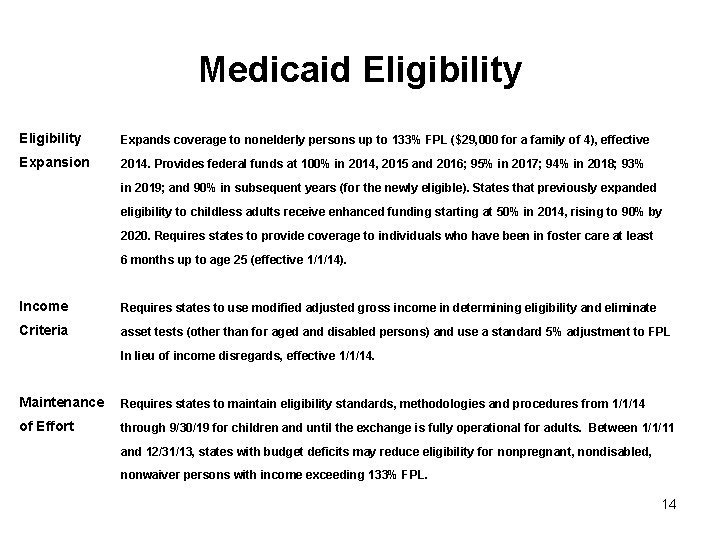
Medicaid Eligibility Expands coverage to nonelderly persons up to 133% FPL ($29, 000 for a family of 4), effective Expansion 2014. Provides federal funds at 100% in 2014, 2015 and 2016; 95% in 2017; 94% in 2018; 93% in 2019; and 90% in subsequent years (for the newly eligible). States that previously expanded eligibility to childless adults receive enhanced funding starting at 50% in 2014, rising to 90% by 2020. Requires states to provide coverage to individuals who have been in foster care at least 6 months up to age 25 (effective 1/1/14). Income Requires states to use modified adjusted gross income in determining eligibility and eliminate Criteria asset tests (other than for aged and disabled persons) and use a standard 5% adjustment to FPL In lieu of income disregards, effective 1/1/14. Maintenance Requires states to maintain eligibility standards, methodologies and procedures from 1/1/14 of Effort through 9/30/19 for children and until the exchange is fully operational for adults. Between 1/1/11 and 12/31/13, states with budget deficits may reduce eligibility for nonpregnant, nondisabled, nonwaiver persons with income exceeding 133% FPL. 14
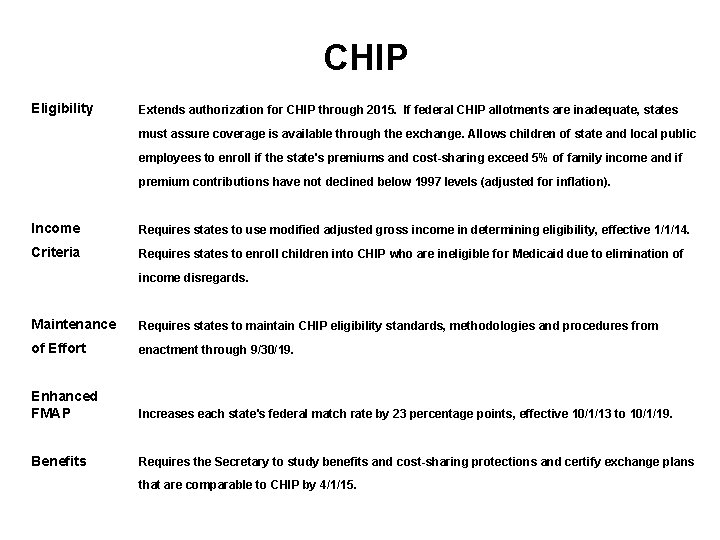
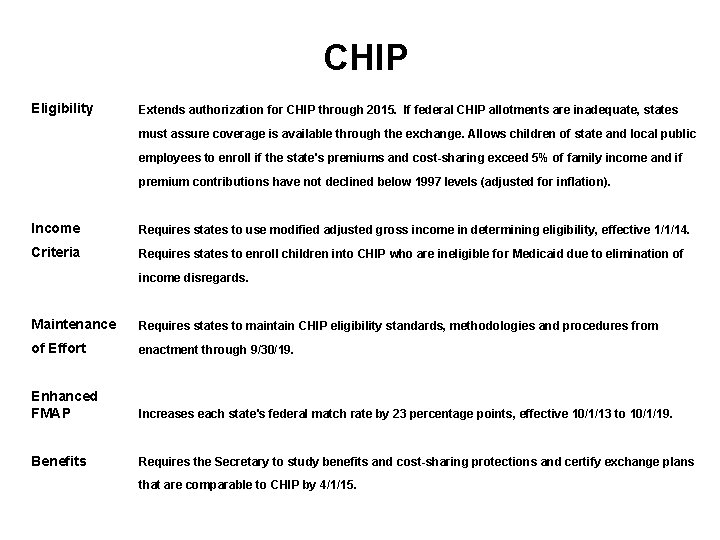
CHIP Eligibility Extends authorization for CHIP through 2015. If federal CHIP allotments are inadequate, states must assure coverage is available through the exchange. Allows children of state and local public employees to enroll if the state's premiums and cost-sharing exceed 5% of family income and if premium contributions have not declined below 1997 levels (adjusted for inflation). Income Requires states to use modified adjusted gross income in determining eligibility, effective 1/1/14. Criteria Requires states to enroll children into CHIP who are ineligible for Medicaid due to elimination of income disregards. Maintenance Requires states to maintain CHIP eligibility standards, methodologies and procedures from of Effort enactment through 9/30/19. Enhanced FMAP Increases each state's federal match rate by 23 percentage points, effective 10/1/13 to 10/1/19. Benefits Requires the Secretary to study benefits and cost-sharing protections and certify exchange plans that are comparable to CHIP by 4/1/15.
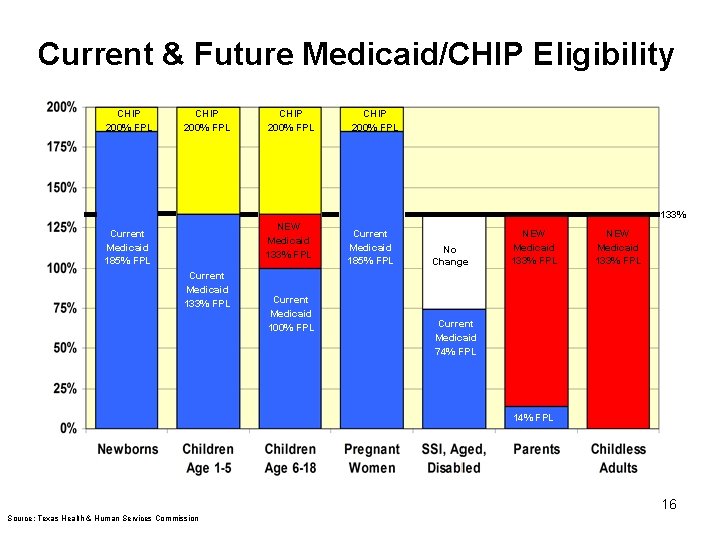
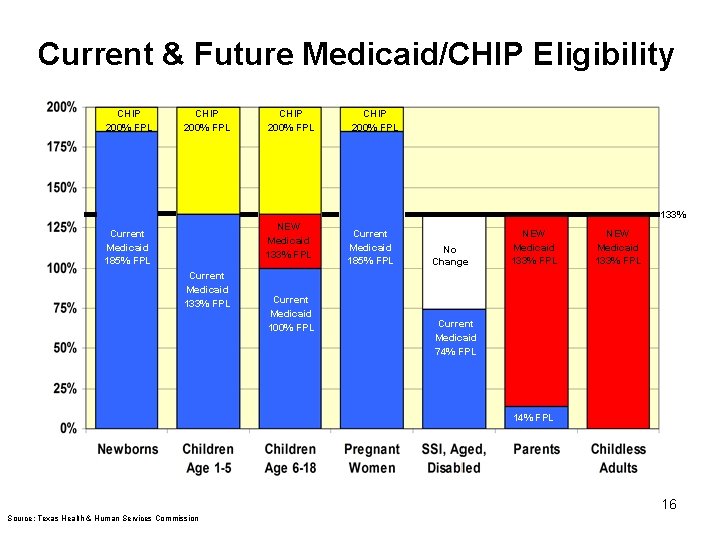
Current & Future Medicaid/CHIP Eligibility CHIP 200% FPL 133% NEW Medicaid 133% FPL Current Medicaid 185% FPL Current Medicaid 133% FPL Current Medicaid 100% FPL Current Medicaid 185% FPL No Change NEW Medicaid 133% FPL Current Medicaid 74% FPL 16 Source: Texas Health & Human Services Commission
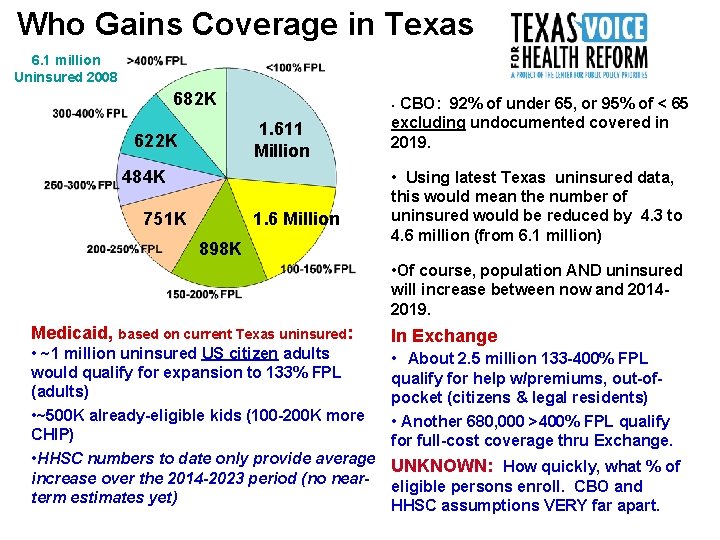
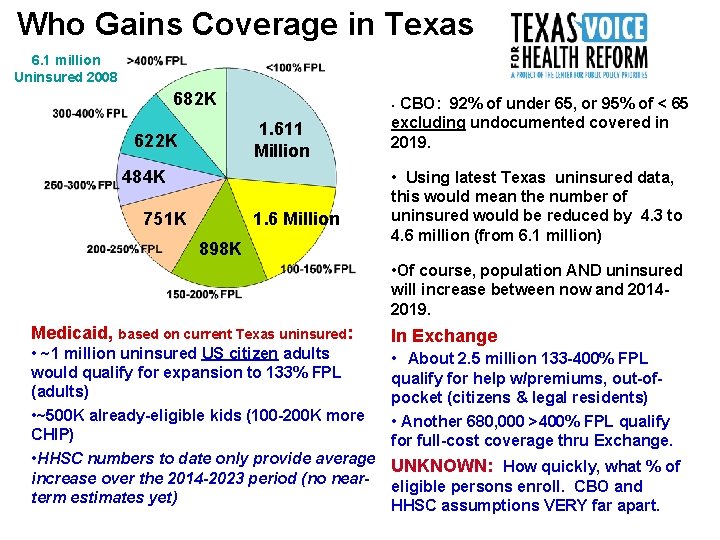
Who Gains Coverage in Texas 6. 1 million Uninsured 2008 682 K 1. 611 Million 622 K 484 K 751 K CBO: 92% of under 65, or 95% of < 65 excluding undocumented covered in 2019. • 1. 6 Million 898 K • Using latest Texas uninsured data, this would mean the number of uninsured would be reduced by 4. 3 to 4. 6 million (from 6. 1 million) • Of course, population AND uninsured will increase between now and 20142019. Medicaid, based on current Texas uninsured: • ~1 million uninsured US citizen adults would qualify for expansion to 133% FPL (adults) • ~500 K already-eligible kids (100 -200 K more CHIP) • HHSC numbers to date only provide average increase over the 2014 -2023 period (no nearterm estimates yet) In Exchange • About 2. 5 million 133 -400% FPL qualify for help w/premiums, out-ofpocket (citizens & legal residents) • Another 680, 000 >400% FPL qualify for full-cost coverage thru Exchange. UNKNOWN: How quickly, what % of eligible persons enroll. CBO and HHSC assumptions VERY far apart.
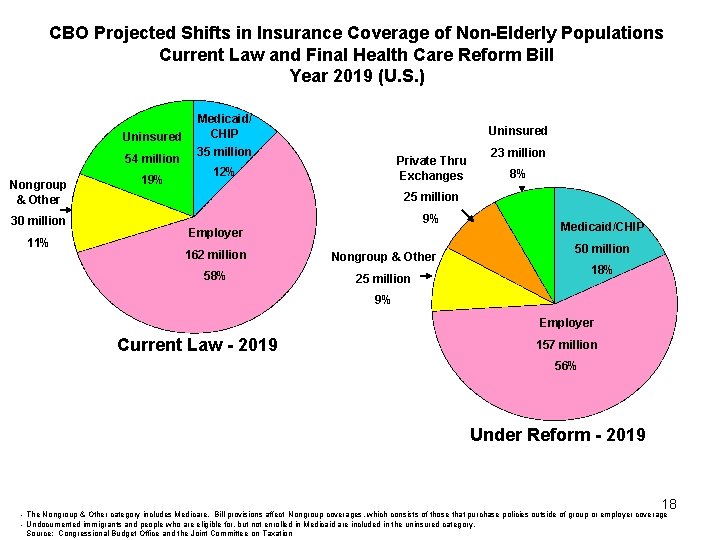
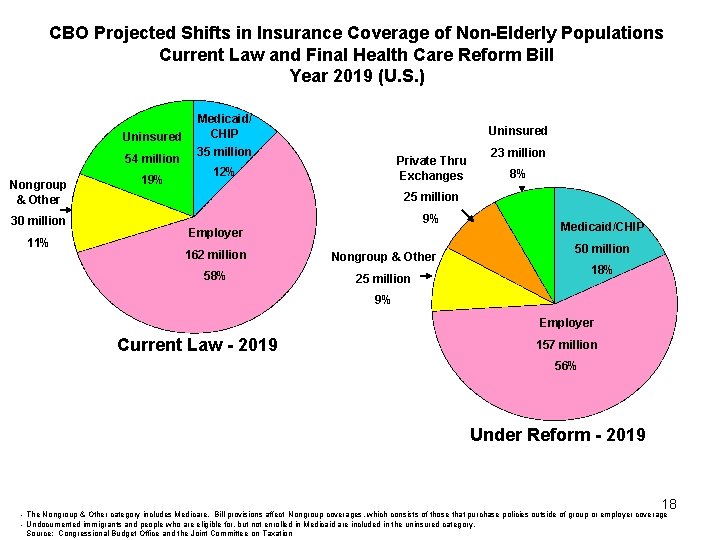
CBO Projected Shifts in Insurance Coverage of Non-Elderly Populations Current Law and Final Health Care Reform Bill Year 2019 (U. S. ) Uninsured 54 million Nongroup & Other 30 million 11% 19% Medicaid/ CHIP Uninsured 35 million Private Thru Exchanges 12% 23 million 8% 25 million 9% Employer 162 million Nongroup & Other 58% 25 million Medicaid/CHIP 50 million 18% 9% Employer Current Law - 2019 157 million 56% Under Reform - 2019 18 - The Nongroup & Other category includes Medicare. Bill provisions affect Nongroup coverages, which consists of those that purchase policies outside of group or employer coverage - Undocumented immigrants and people who are eligible for, but not enrolled in Medicaid are included in the uninsured category. Source: Congressional Budget Office and the Joint Committee on Taxation
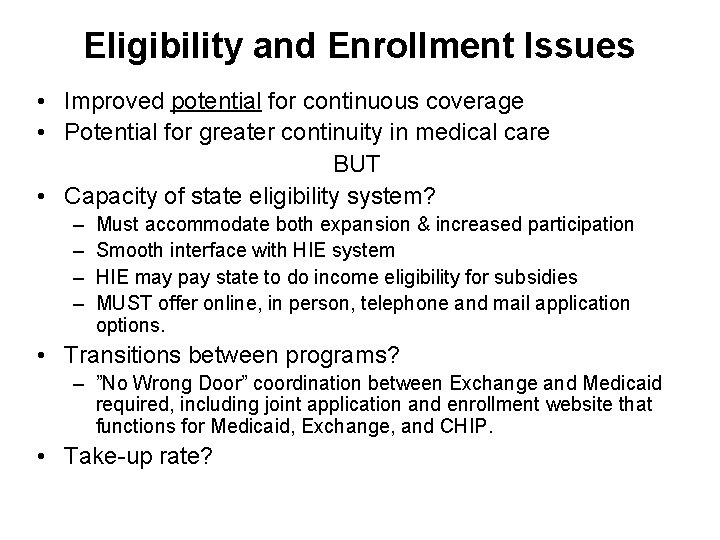
Eligibility and Enrollment Issues • Improved potential for continuous coverage • Potential for greater continuity in medical care BUT • Capacity of state eligibility system? – – Must accommodate both expansion & increased participation Smooth interface with HIE system HIE may pay state to do income eligibility for subsidies MUST offer online, in person, telephone and mail application options. • Transitions between programs? – ”No Wrong Door” coordination between Exchange and Medicaid required, including joint application and enrollment website that functions for Medicaid, Exchange, and CHIP. • Take-up rate?
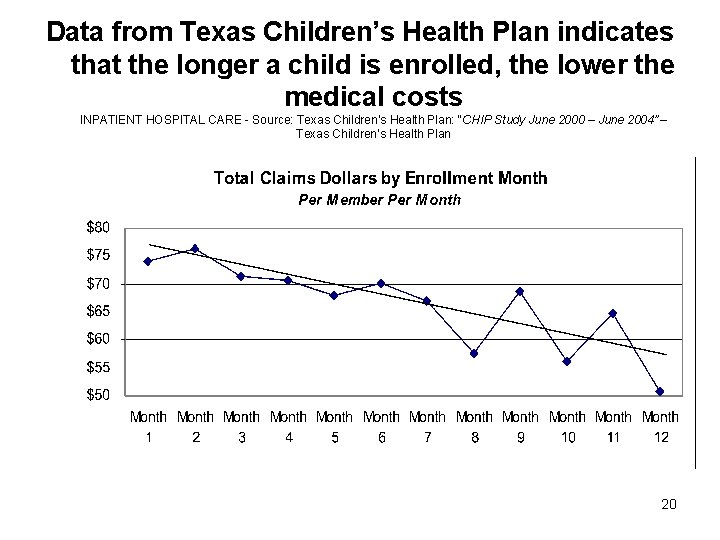
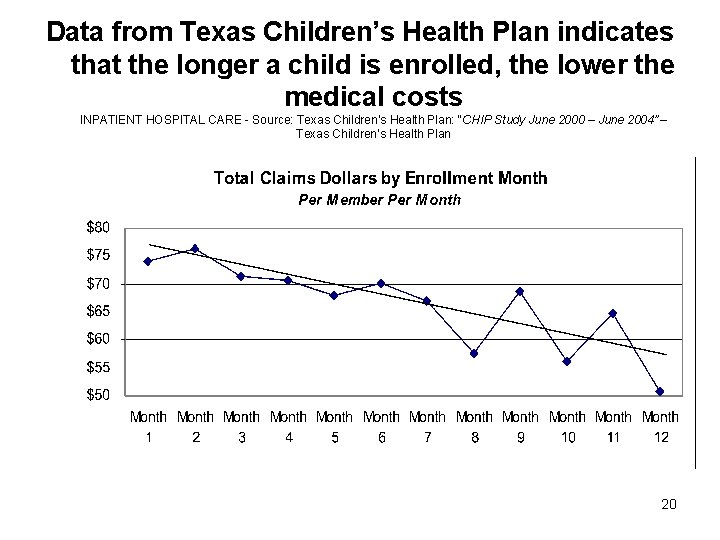
Data from Texas Children’s Health Plan indicates that the longer a child is enrolled, the lower the medical costs INPATIENT HOSPITAL CARE - Source: Texas Children’s Health Plan: “CHIP Study June 2000 – June 2004” – Texas Children’s Health Plan 20
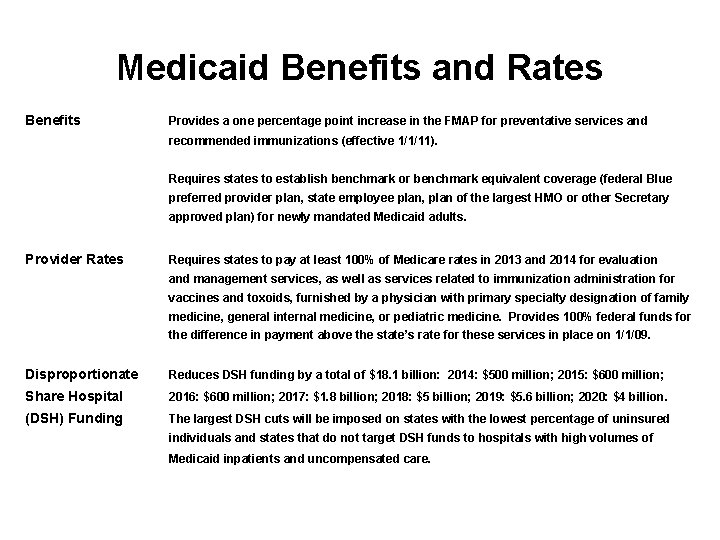
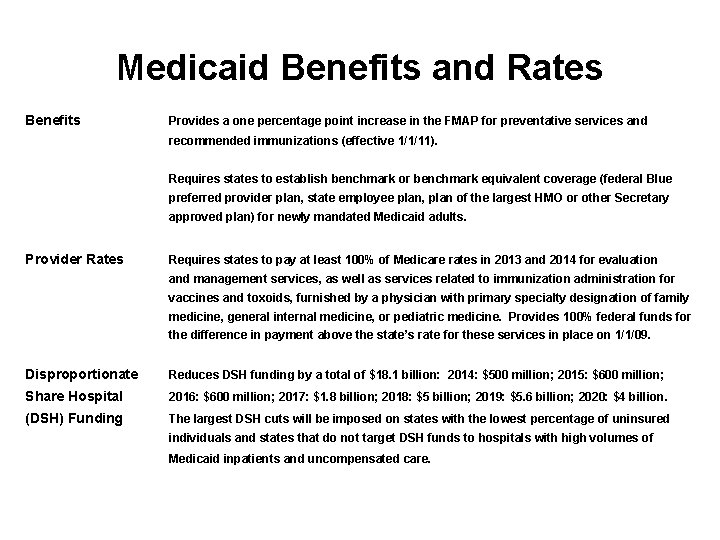
Medicaid Benefits and Rates Benefits Provides a one percentage point increase in the FMAP for preventative services and recommended immunizations (effective 1/1/11). Requires states to establish benchmark or benchmark equivalent coverage (federal Blue preferred provider plan, state employee plan, plan of the largest HMO or other Secretary approved plan) for newly mandated Medicaid adults. Provider Rates Requires states to pay at least 100% of Medicare rates in 2013 and 2014 for evaluation and management services, as well as services related to immunization administration for vaccines and toxoids, furnished by a physician with primary specialty designation of family medicine, general internal medicine, or pediatric medicine. Provides 100% federal funds for the difference in payment above the state’s rate for these services in place on 1/1/09. Disproportionate Reduces DSH funding by a total of $18. 1 billion: 2014: $500 million; 2015: $600 million; Share Hospital 2016: $600 million; 2017: $1. 8 billion; 2018: $5 billion; 2019: $5. 6 billion; 2020: $4 billion. (DSH) Funding The largest DSH cuts will be imposed on states with the lowest percentage of uninsured individuals and states that do not target DSH funds to hospitals with high volumes of Medicaid inpatients and uncompensated care.
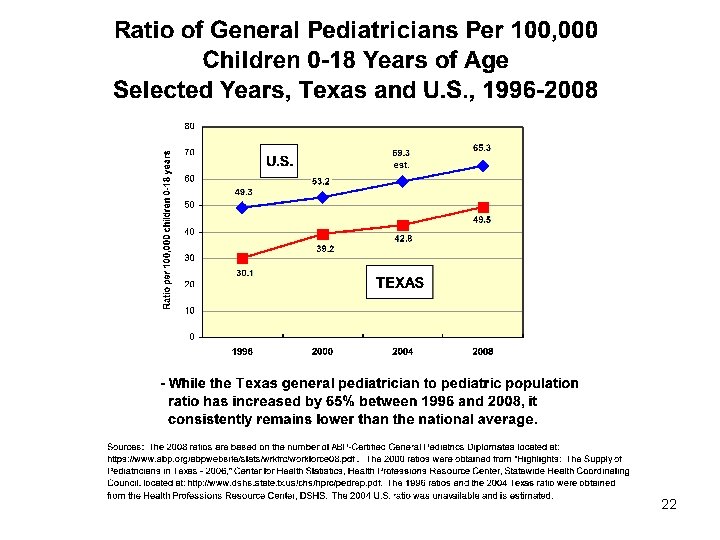
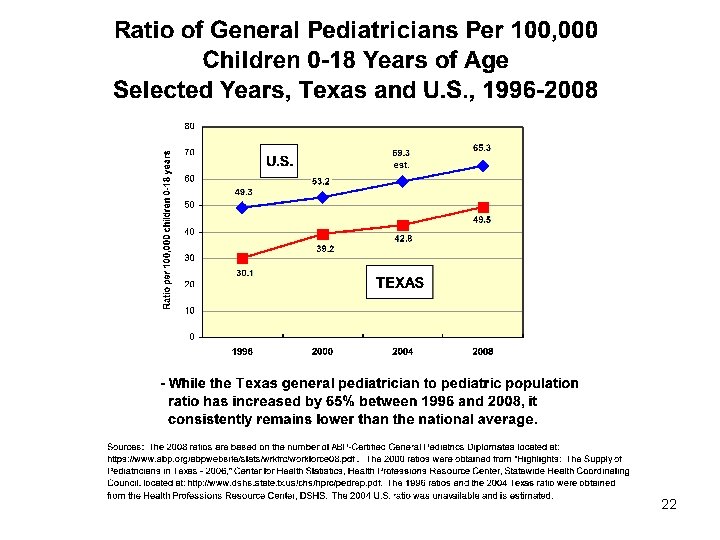
22
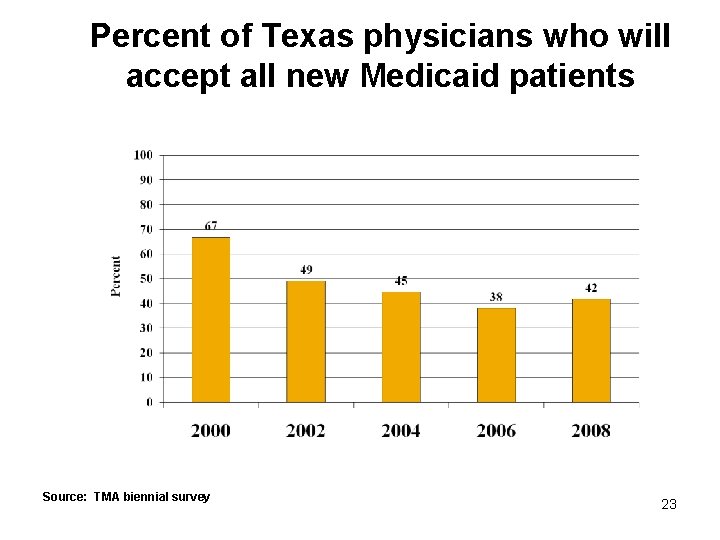
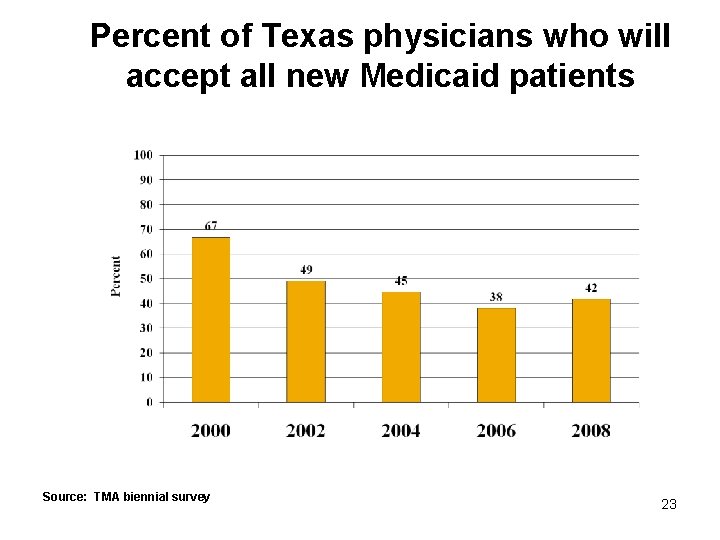
Percent of Texas physicians who will accept all new Medicaid patients Source: TMA biennial survey 23
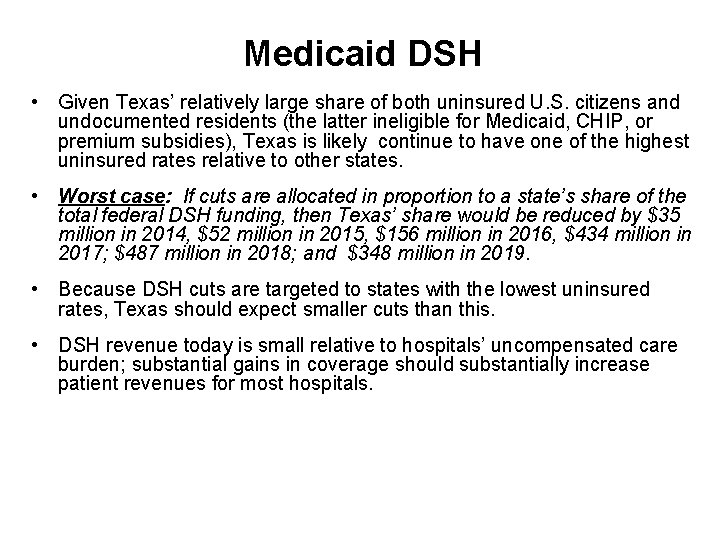
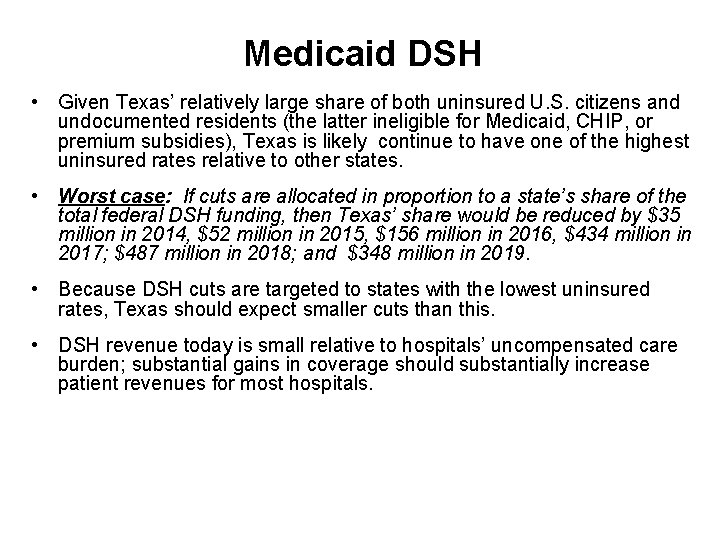
Medicaid DSH • Given Texas’ relatively large share of both uninsured U. S. citizens and undocumented residents (the latter ineligible for Medicaid, CHIP, or premium subsidies), Texas is likely continue to have one of the highest uninsured rates relative to other states. • Worst case: If cuts are allocated in proportion to a state’s share of the total federal DSH funding, then Texas’ share would be reduced by $35 million in 2014, $52 million in 2015, $156 million in 2016, $434 million in 2017; $487 million in 2018; and $348 million in 2019. • Because DSH cuts are targeted to states with the lowest uninsured rates, Texas should expect smaller cuts than this. • DSH revenue today is small relative to hospitals’ uncompensated care burden; substantial gains in coverage should substantially increase patient revenues for most hospitals.
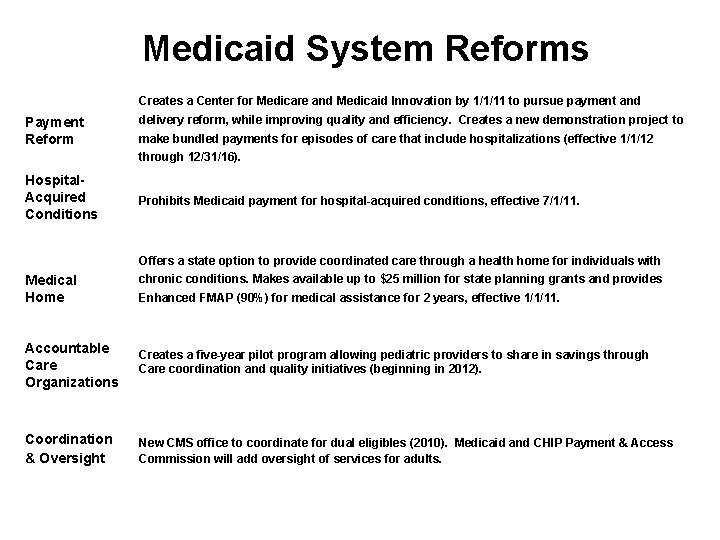
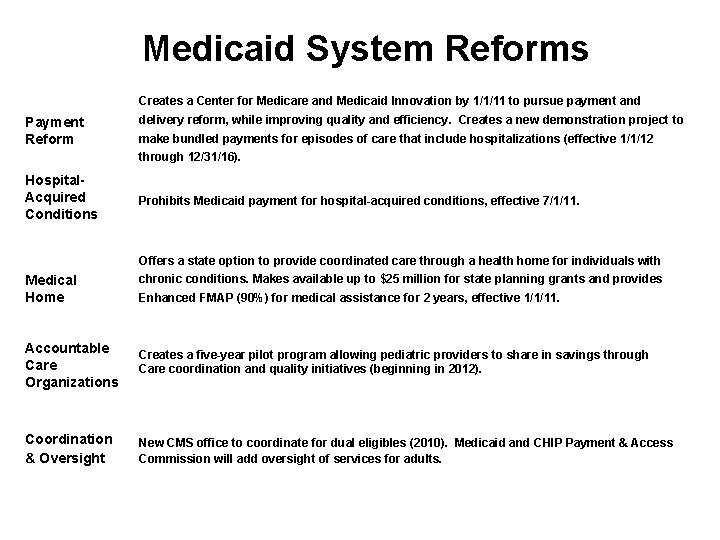
Medicaid System Reforms Creates a Center for Medicare and Medicaid Innovation by 1/1/11 to pursue payment and Payment Reform delivery reform, while improving quality and efficiency. Creates a new demonstration project to make bundled payments for episodes of care that include hospitalizations (effective 1/1/12 through 12/31/16). Hospital. Acquired Conditions Prohibits Medicaid payment for hospital-acquired conditions, effective 7/1/11. Offers a state option to provide coordinated care through a health home for individuals with Medical Home chronic conditions. Makes available up to $25 million for state planning grants and provides Enhanced FMAP (90%) for medical assistance for 2 years, effective 1/1/11. Accountable Care Organizations Creates a five-year pilot program allowing pediatric providers to share in savings through Care coordination and quality initiatives (beginning in 2012). Coordination & Oversight New CMS office to coordinate for dual eligibles (2010). Medicaid and CHIP Payment & Access Commission will add oversight of services for adults.
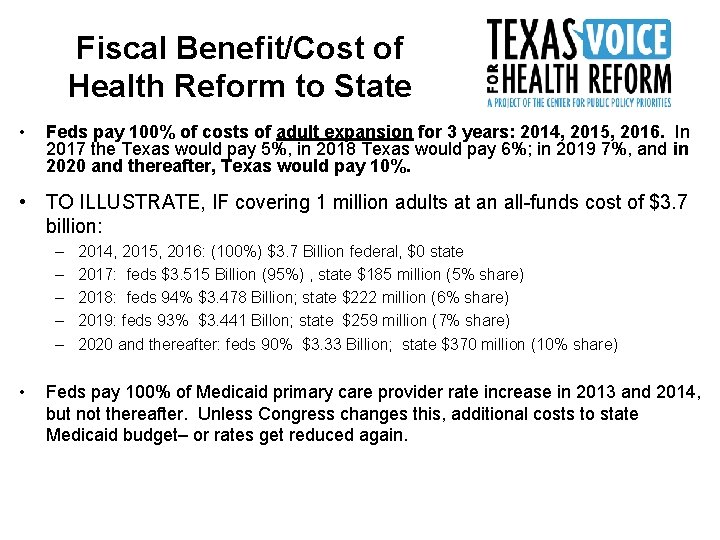
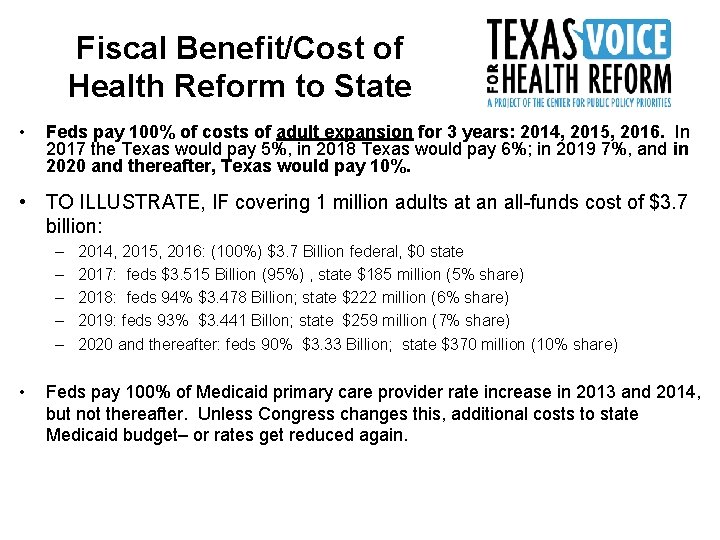
Fiscal Benefit/Cost of Health Reform to State • Feds pay 100% of costs of adult expansion for 3 years: 2014, 2015, 2016. In 2017 the Texas would pay 5%, in 2018 Texas would pay 6%; in 2019 7%, and in 2020 and thereafter, Texas would pay 10%. • TO ILLUSTRATE, IF covering 1 million adults at an all-funds cost of $3. 7 billion: – – – • 2014, 2015, 2016: (100%) $3. 7 Billion federal, $0 state 2017: feds $3. 515 Billion (95%) , state $185 million (5% share) 2018: feds 94% $3. 478 Billion; state $222 million (6% share) 2019: feds 93% $3. 441 Billon; state $259 million (7% share) 2020 and thereafter: feds 90% $3. 33 Billion; state $370 million (10% share) Feds pay 100% of Medicaid primary care provider rate increase in 2013 and 2014, but not thereafter. Unless Congress changes this, additional costs to state Medicaid budget– or rates get reduced again.
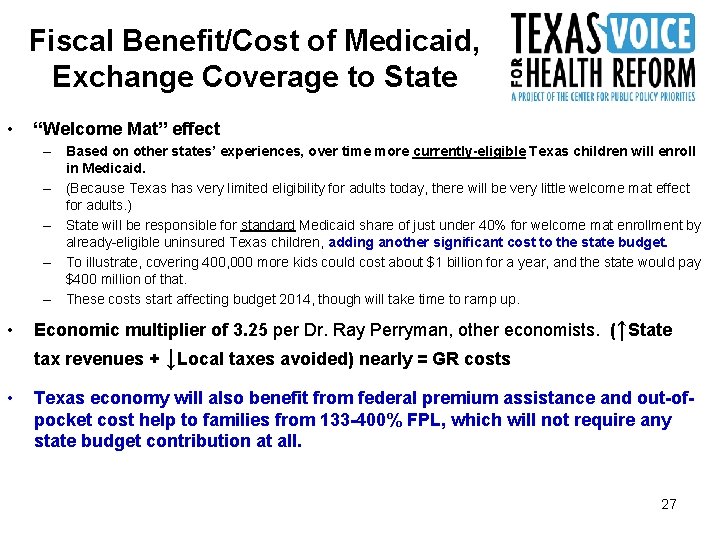
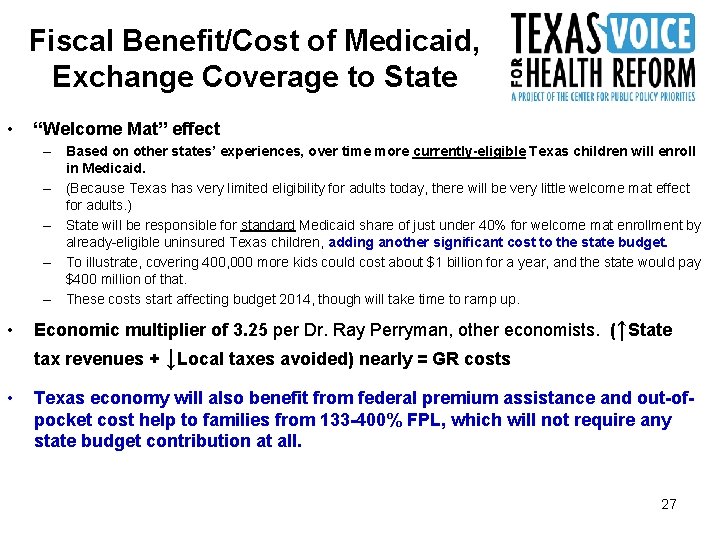
Fiscal Benefit/Cost of Medicaid, Exchange Coverage to State • “Welcome Mat” effect – Based on other states’ experiences, over time more currently-eligible Texas children will enroll in Medicaid. – (Because Texas has very limited eligibility for adults today, there will be very little welcome mat effect for adults. ) – State will be responsible for standard Medicaid share of just under 40% for welcome mat enrollment by already-eligible uninsured Texas children, adding another significant cost to the state budget. – To illustrate, covering 400, 000 more kids could cost about $1 billion for a year, and the state would pay $400 million of that. – These costs start affecting budget 2014, though will take time to ramp up. • Economic multiplier of 3. 25 per Dr. Ray Perryman, other economists. (↑State tax revenues + ↓Local taxes avoided) nearly = GR costs • Texas economy will also benefit from federal premium assistance and out-ofpocket cost help to families from 133 -400% FPL, which will not require any state budget contribution at all. 27
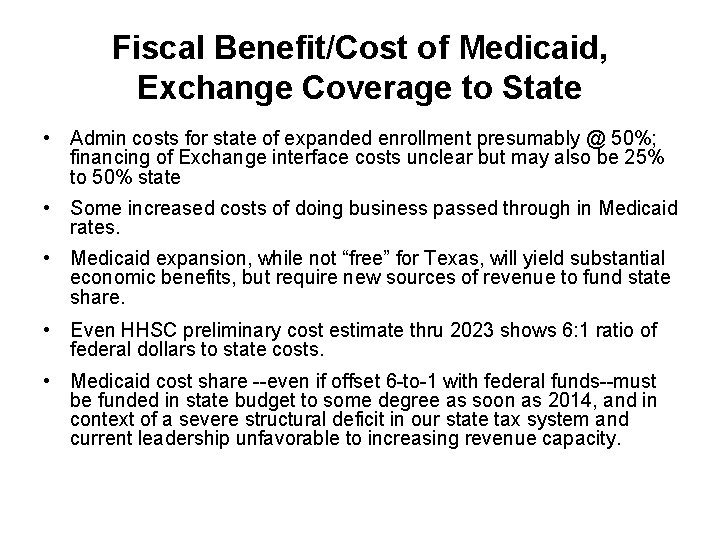
Fiscal Benefit/Cost of Medicaid, Exchange Coverage to State • Admin costs for state of expanded enrollment presumably @ 50%; financing of Exchange interface costs unclear but may also be 25% to 50% state • Some increased costs of doing business passed through in Medicaid rates. • Medicaid expansion, while not “free” for Texas, will yield substantial economic benefits, but require new sources of revenue to fund state share. • Even HHSC preliminary cost estimate thru 2023 shows 6: 1 ratio of federal dollars to state costs. • Medicaid cost share --even if offset 6 -to-1 with federal funds--must be funded in state budget to some degree as soon as 2014, and in context of a severe structural deficit in our state tax system and current leadership unfavorable to increasing revenue capacity.
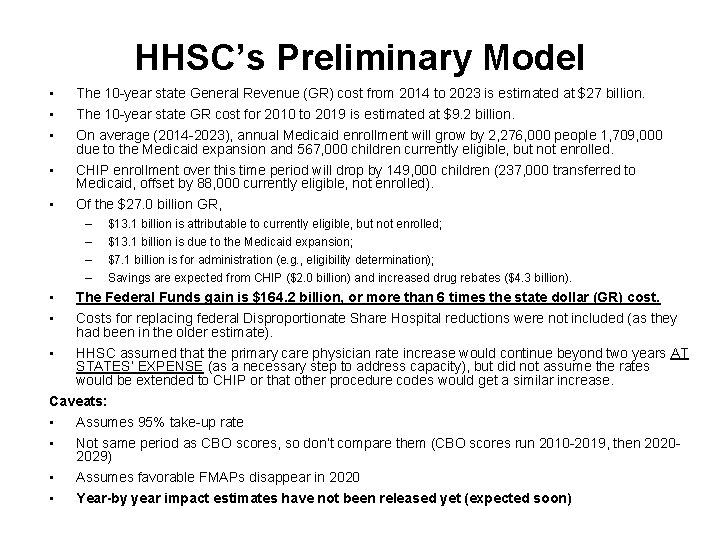
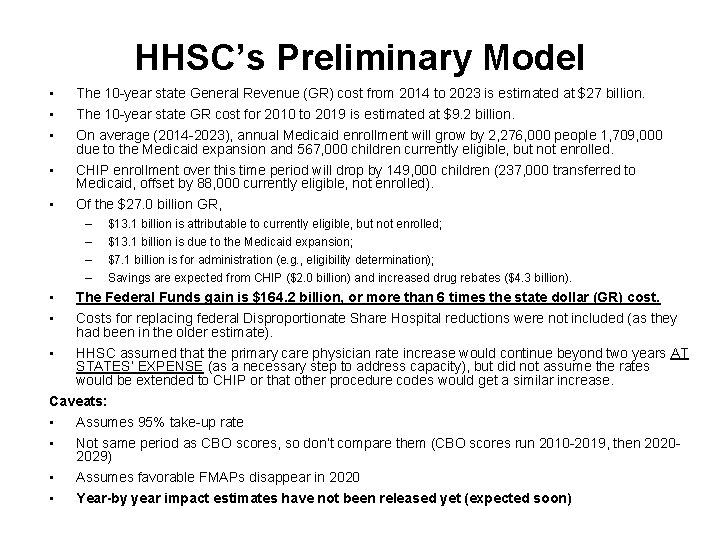
HHSC’s Preliminary Model • • • The 10 -year state General Revenue (GR) cost from 2014 to 2023 is estimated at $27 billion. The 10 -year state GR cost for 2010 to 2019 is estimated at $9. 2 billion. On average (2014 -2023), annual Medicaid enrollment will grow by 2, 276, 000 people 1, 709, 000 due to the Medicaid expansion and 567, 000 children currently eligible, but not enrolled. CHIP enrollment over this time period will drop by 149, 000 children (237, 000 transferred to Medicaid, offset by 88, 000 currently eligible, not enrolled). Of the $27. 0 billion GR, – – • • • $13. 1 billion is attributable to currently eligible, but not enrolled; $13. 1 billion is due to the Medicaid expansion; $7. 1 billion is for administration (e. g. , eligibility determination); Savings are expected from CHIP ($2. 0 billion) and increased drug rebates ($4. 3 billion). The Federal Funds gain is $164. 2 billion, or more than 6 times the state dollar (GR) cost. Costs for replacing federal Disproportionate Share Hospital reductions were not included (as they had been in the older estimate). HHSC assumed that the primary care physician rate increase would continue beyond two years AT STATES’ EXPENSE (as a necessary step to address capacity), but did not assume the rates would be extended to CHIP or that other procedure codes would get a similar increase. Caveats: • Assumes 95% take-up rate • Not same period as CBO scores, so don’t compare them (CBO scores run 2010 -2019, then 20202029) • Assumes favorable FMAPs disappear in 2020 • Year-by year impact estimates have not been released yet (expected soon)
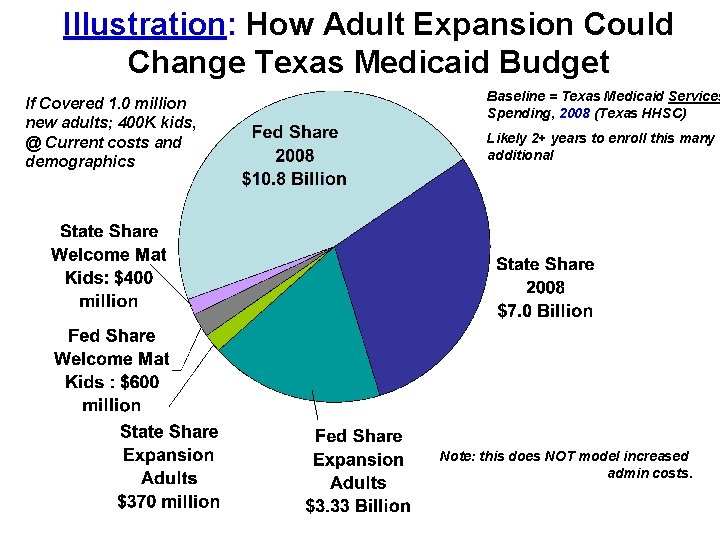
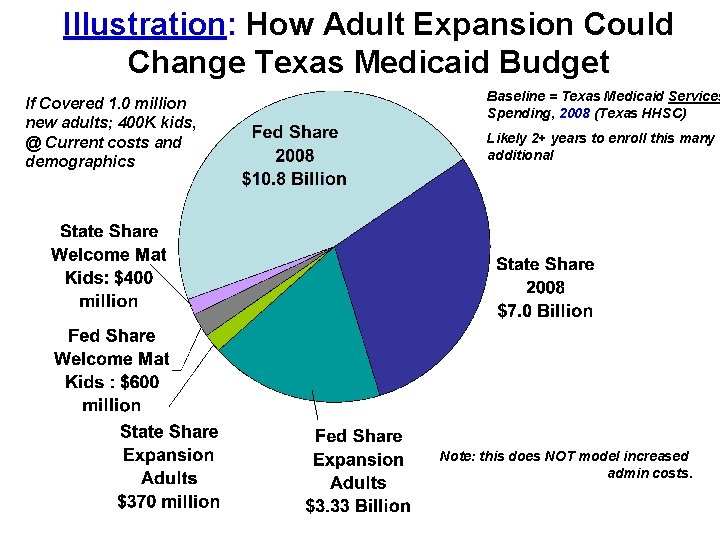
Illustration: How Adult Expansion Could Change Texas Medicaid Budget If Covered 1. 0 million new adults; 400 K kids, @ Current costs and demographics Baseline = Texas Medicaid Services Spending, 2008 (Texas HHSC) Likely 2+ years to enroll this many additional Note: this does NOT model increased admin costs.
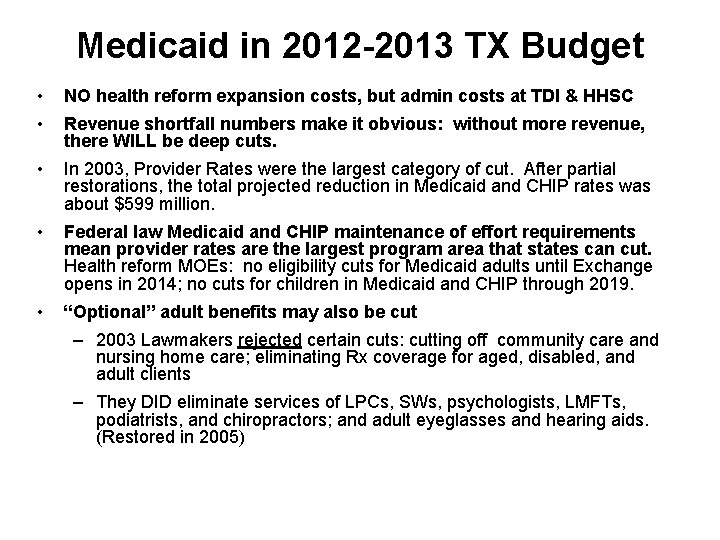
Medicaid in 2012 -2013 TX Budget • NO health reform expansion costs, but admin costs at TDI & HHSC • Revenue shortfall numbers make it obvious: without more revenue, there WILL be deep cuts. • In 2003, Provider Rates were the largest category of cut. After partial restorations, the total projected reduction in Medicaid and CHIP rates was about $599 million. • Federal law Medicaid and CHIP maintenance of effort requirements mean provider rates are the largest program area that states can cut. Health reform MOEs: no eligibility cuts for Medicaid adults until Exchange opens in 2014; no cuts for children in Medicaid and CHIP through 2019. • “Optional” adult benefits may also be cut – 2003 Lawmakers rejected certain cuts: cutting off community care and nursing home care; eliminating Rx coverage for aged, disabled, and adult clients – They DID eliminate services of LPCs, SWs, psychologists, LMFTs, podiatrists, and chiropractors; and adult eyeglasses and hearing aids. (Restored in 2005)
Use of This Presentation The Center for Public Policy Priorities encourages you to reproduce and distribute these slides, which were developed for use in making public presentations. If you reproduce these slides, please give appropriate credit to CPPP. The data presented here may become outdated; for the most recent information or to sign up for our free E-Mail Updates, visit www. cppp. org. © CPPP Center for Public Policy Priorities 900 Lydia Street Austin, TX 78702 P 512/320 -0222 32
 Non emergency medical transportation dallas tx
Non emergency medical transportation dallas tx First dental home visit documentation form
First dental home visit documentation form Continuum of care reform
Continuum of care reform Primary secondary and tertiary health care
Primary secondary and tertiary health care Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Health and social component 3
Health and social component 3 Medicare set-aside flow chart
Medicare set-aside flow chart Dshs uncompensated trauma care application
Dshs uncompensated trauma care application Chapter 10 section 1 democratic reform and activism
Chapter 10 section 1 democratic reform and activism Chapter 10 section 1 democratic reform and activism
Chapter 10 section 1 democratic reform and activism Chapter 23 lesson 3 nationalism unification and reform
Chapter 23 lesson 3 nationalism unification and reform The ferment of reform and culture
The ferment of reform and culture Revolution brings reform and terror
Revolution brings reform and terror Taxation and budget reform commission
Taxation and budget reform commission Fdr three rs
Fdr three rs Chapter 19 political reform and the progressive era
Chapter 19 political reform and the progressive era Chapter 15 the ferment of reform and culture
Chapter 15 the ferment of reform and culture What was reform darwinism?
What was reform darwinism? Chapter 7 section 2 revolution brings reform and terror
Chapter 7 section 2 revolution brings reform and terror Chapter 15 the ferment of reform and culture
Chapter 15 the ferment of reform and culture W.w. norton
W.w. norton Chapter 23 section 2 revolution brings reform and terror
Chapter 23 section 2 revolution brings reform and terror The ferment of reform and culture
The ferment of reform and culture Second great awakening
Second great awakening Church reform and the crusades
Church reform and the crusades Chapter 14 section 1 church reform and the crusades
Chapter 14 section 1 church reform and the crusades Texas health and safety code 343
Texas health and safety code 343 Wyoming medicaid provider manual
Wyoming medicaid provider manual Wyoming medicaid provider manual
Wyoming medicaid provider manual Institutional medicaid
Institutional medicaid Indiana medicaid waiver pick list
Indiana medicaid waiver pick list Unicare health plan of west virginia
Unicare health plan of west virginia Eapg medicaid
Eapg medicaid