Techniques of examination of the thorax and lungs
- Slides: 14
Techniques of examination of the thorax and lungs Dr. Szathmári Miklós Semmelweis University First Department of Medicine 27. Sept. 2011.
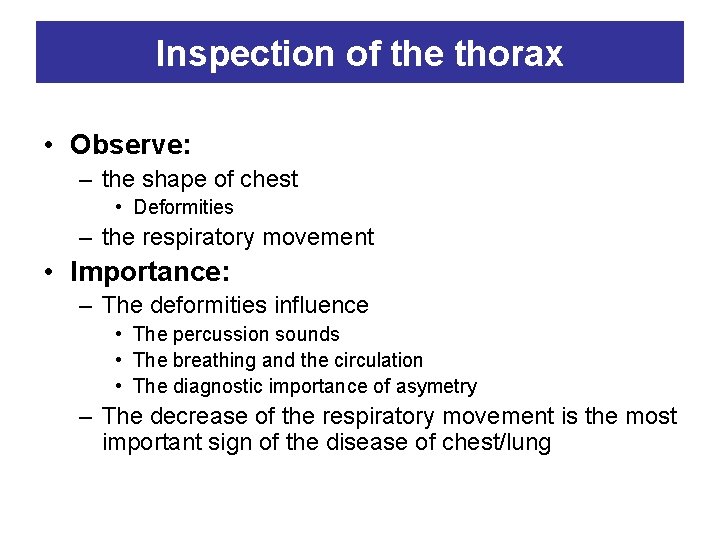
Inspection of the thorax • Observe: – the shape of chest • Deformities – the respiratory movement • Importance: – The deformities influence • The percussion sounds • The breathing and the circulation • The diagnostic importance of asymetry – The decrease of the respiratory movement is the most important sign of the disease of chest/lung
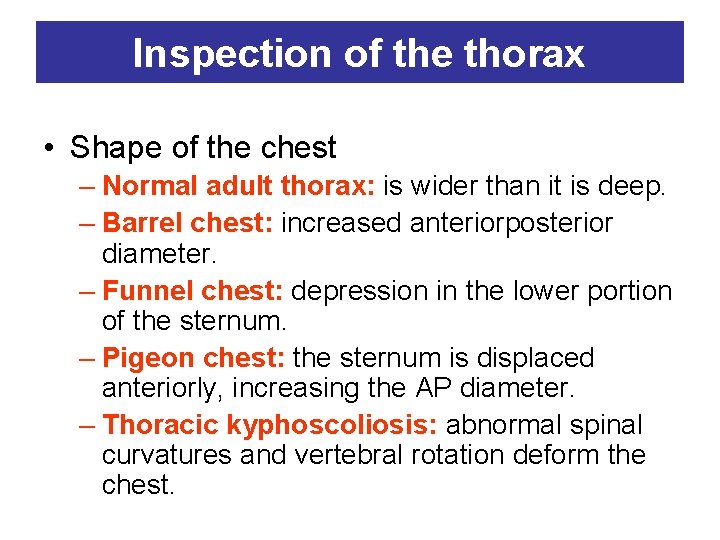
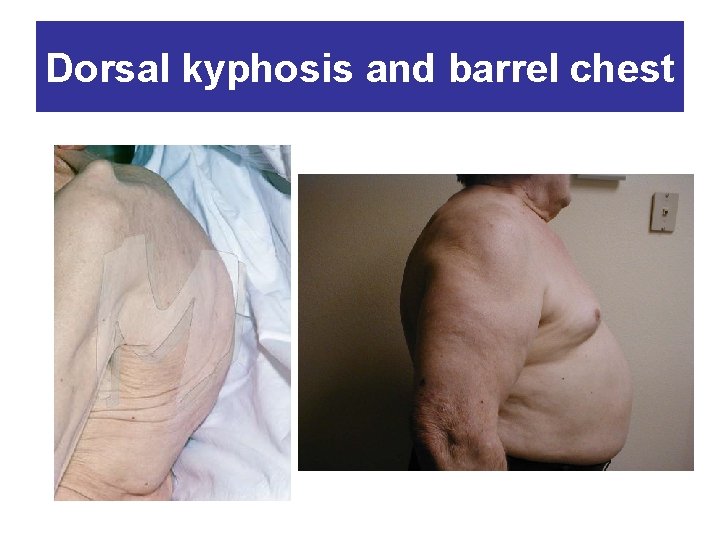
Inspection of the thorax • Shape of the chest – Normal adult thorax: is wider than it is deep. – Barrel chest: increased anteriorposterior diameter. – Funnel chest: depression in the lower portion of the sternum. – Pigeon chest: the sternum is displaced anteriorly, increasing the AP diameter. – Thoracic kyphoscoliosis: abnormal spinal curvatures and vertebral rotation deform the chest.
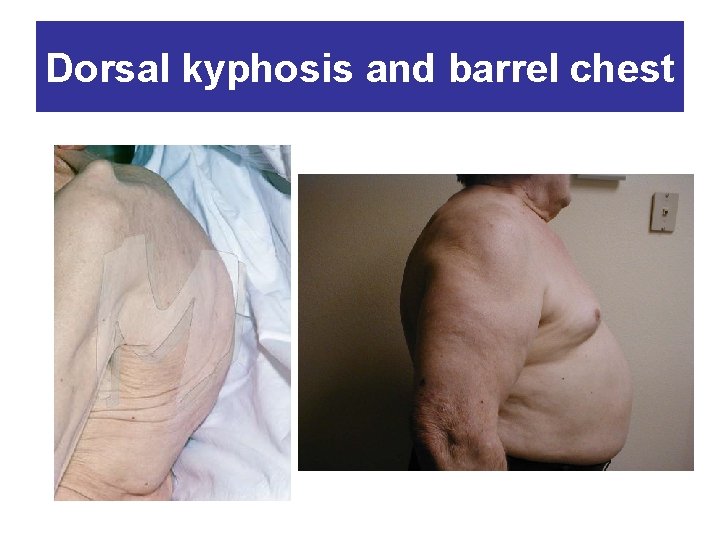
Dorsal kyphosis and barrel chest
Inspection of the thorax • Abnormal retraction of the interspaces during inspiration (severe asthma, COPD or upper airway obstraction). • Inspection of movement of chest wall during inspiration (unilateral impairment or delay of respiratory movement suggests disease of the underlying lung or pleura.
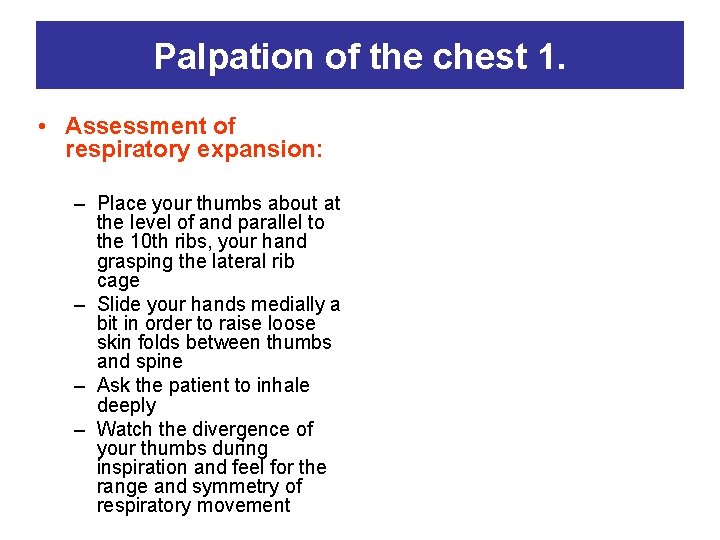
Palpation of the chest 1. • Assessment of respiratory expansion: – Place your thumbs about at the level of and parallel to the 10 th ribs, your hand grasping the lateral rib cage – Slide your hands medially a bit in order to raise loose skin folds between thumbs and spine – Ask the patient to inhale deeply – Watch the divergence of your thumbs during inspiration and feel for the range and symmetry of respiratory movement
Palpation of the chest 2. Tactile fremitus – refers to the palpable vibrations transmitted through the bronchopulmonary system to the chest wall when the patiens speaks • Palpate and compare symmetrical areas of the lungs • Use the ulnar surface of your hand. Ask the patient to repeat ninety-nine or „harminchárom”. • If fremitus is faint, ask the patient to speak more loudly or in a deeper voice. Pleural rub • Normal pleural surfaces move smoothly and noiselessly against each other during respiration • When pleural surfaces become inflamed, they move jerkily as they are repetedly delayed by increased friction. • The sounds may be discrete, but sometimes are so numerous that they merge into an apparently continuous sound. It is localized to a relatively small area of the chest wall
Palpation of the thorax • intercostal tenderness: over inflammed pleura. Bruises over a fractured rib. • chest expansion: decreased expansion in case of pleural effusion, lobar pneumonia, chronic fibrotic disease of the underlying lung • tactile fremitus: Decreased pectoral fremitus is in case of pleural effusion or pleural thickening or PTX.
Other bony landmarks on the chest wall • Posteriorly, with the fingers of one hand, press inward and up against the lower border of the rib cage you can identify the 12 th rib • The inferior angle of the scapula lies approximately at the level of the 7 th rib • When the patient flexes the neck forward, the most prominent process is usually that of the 7 th cervical
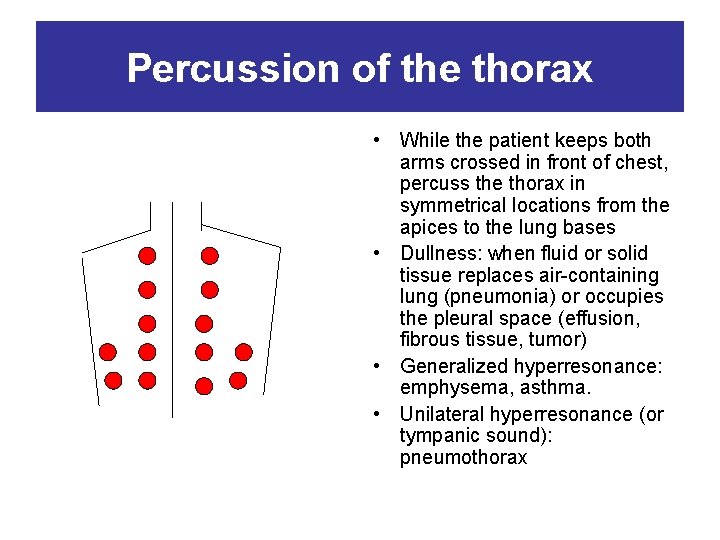
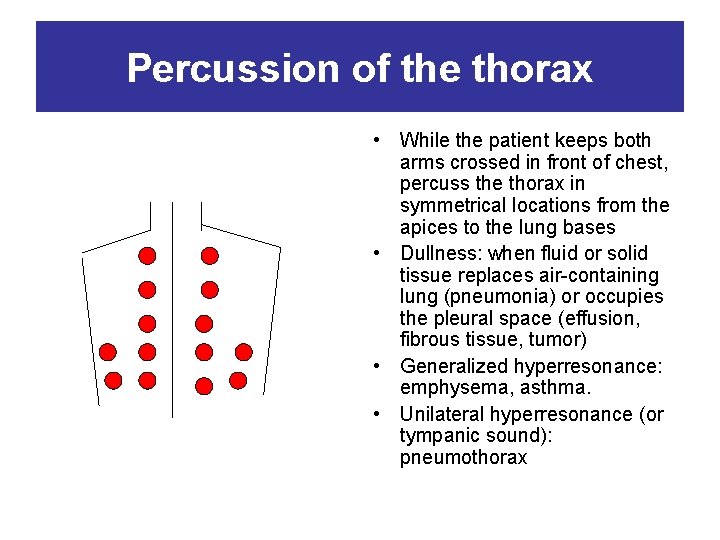
Percussion of the thorax • While the patient keeps both arms crossed in front of chest, percuss the thorax in symmetrical locations from the apices to the lung bases • Dullness: when fluid or solid tissue replaces air-containing lung (pneumonia) or occupies the pleural space (effusion, fibrous tissue, tumor) • Generalized hyperresonance: emphysema, asthma. • Unilateral hyperresonance (or tympanic sound): pneumothorax
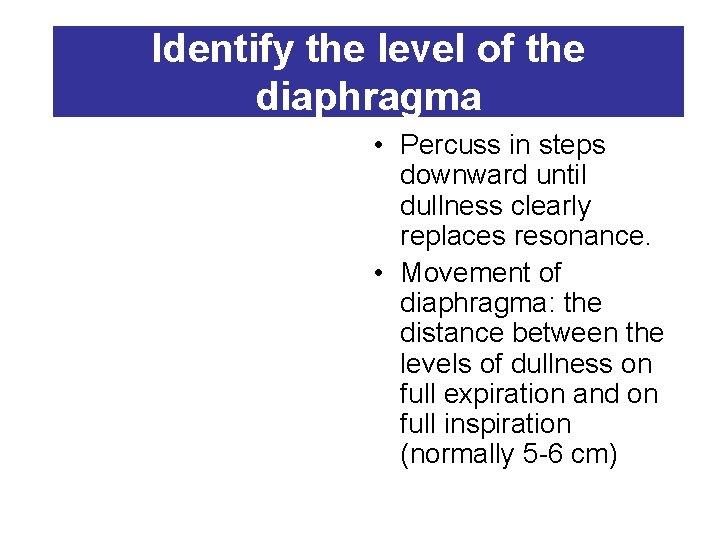
Identify the level of the diaphragma • Percuss in steps downward until dullness clearly replaces resonance. • Movement of diaphragma: the distance between the levels of dullness on full expiration and on full inspiration (normally 5 -6 cm)
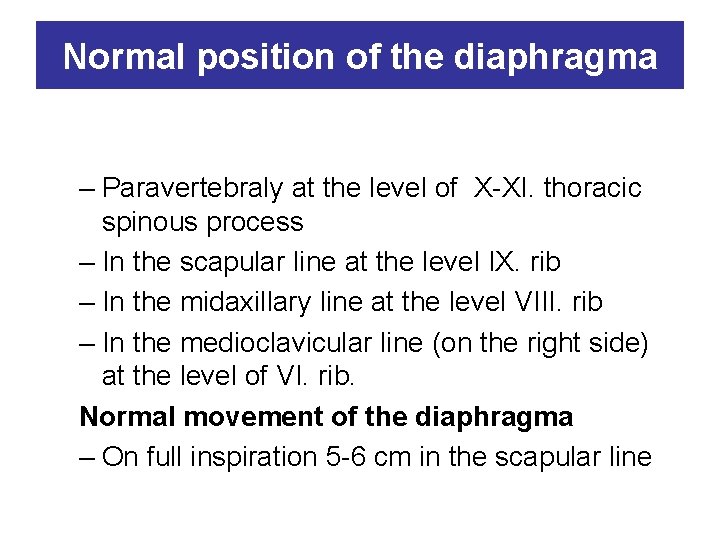
Normal position of the diaphragma – Paravertebraly at the level of X-XI. thoracic spinous process – In the scapular line at the level IX. rib – In the midaxillary line at the level VIII. rib – In the medioclavicular line (on the right side) at the level of VI. rib. Normal movement of the diaphragma – On full inspiration 5 -6 cm in the scapular line
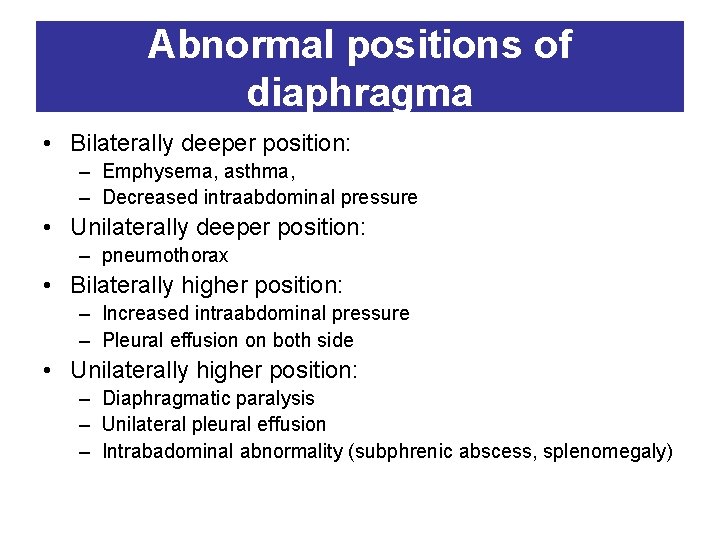
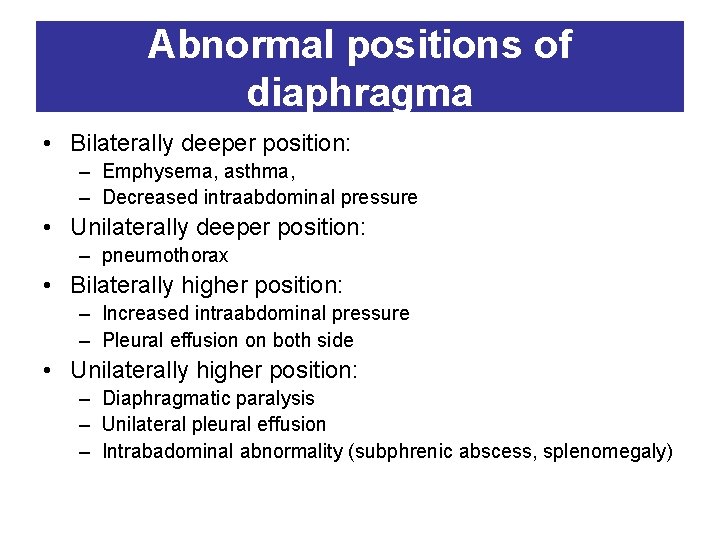
Abnormal positions of diaphragma • Bilaterally deeper position: – Emphysema, asthma, – Decreased intraabdominal pressure • Unilaterally deeper position: – pneumothorax • Bilaterally higher position: – Increased intraabdominal pressure – Pleural effusion on both side • Unilaterally higher position: – Diaphragmatic paralysis – Unilateral pleural effusion – Intrabadominal abnormality (subphrenic abscess, splenomegaly)
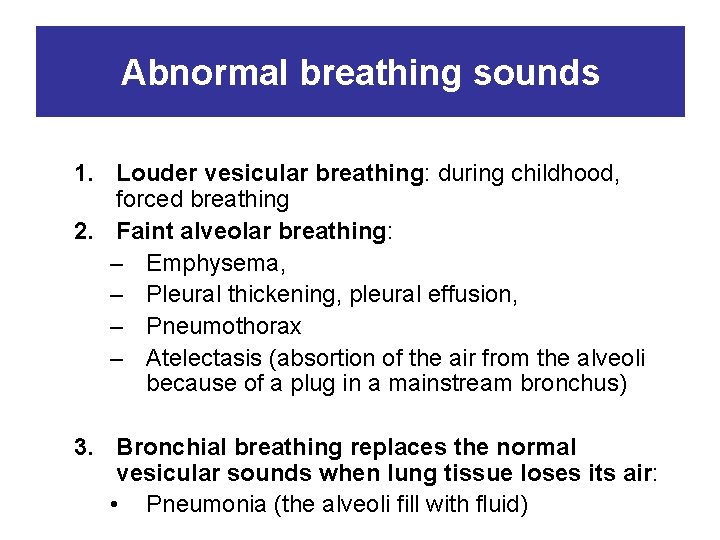
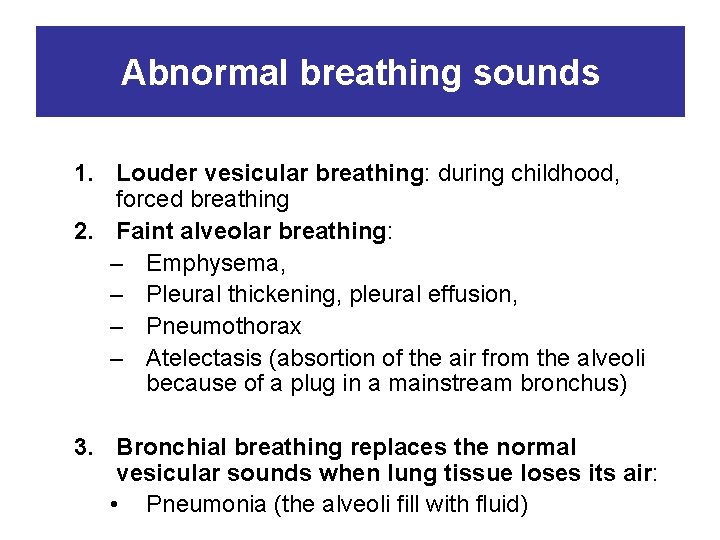
Abnormal breathing sounds 1. Louder vesicular breathing: during childhood, forced breathing 2. Faint alveolar breathing: – Emphysema, – Pleural thickening, pleural effusion, – Pneumothorax – Atelectasis (absortion of the air from the alveoli because of a plug in a mainstream bronchus) 3. Bronchial breathing replaces the normal vesicular sounds when lung tissue loses its air: • Pneumonia (the alveoli fill with fluid)
 Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Physical examination techniques
Physical examination techniques Bronchus cross section
Bronchus cross section Charting normal lung sounds examples
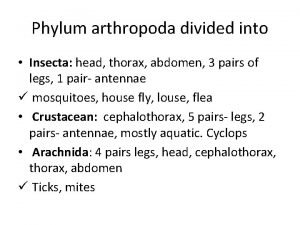
Charting normal lung sounds examples Arthropods head thorax and abdomen
Arthropods head thorax and abdomen Bucket handle movement
Bucket handle movement Hagfish cladogram
Hagfish cladogram Homeostatic responses to respiratory acidosis
Homeostatic responses to respiratory acidosis Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Oblique fissure
Oblique fissure Les fonctions techniques et les solutions techniques
Les fonctions techniques et les solutions techniques Which of the following elevates the ribs?
Which of the following elevates the ribs? Jenis jenis trauma thorax
Jenis jenis trauma thorax Ap diameter of chest
Ap diameter of chest Throax
Throax