Role of Amylin and Glucagon in Postprandial Glycemic







- Slides: 19

Role of Amylin and Glucagon in Postprandial Glycemic Excursions in Pediatric Type 1 Diabetes. Rubina Heptulla MD, Luisa M. Rodriguez MD and Morey W. Haymond MD. Baylor College of Medicine Houston, TX.
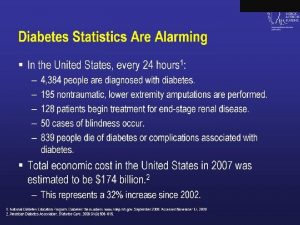
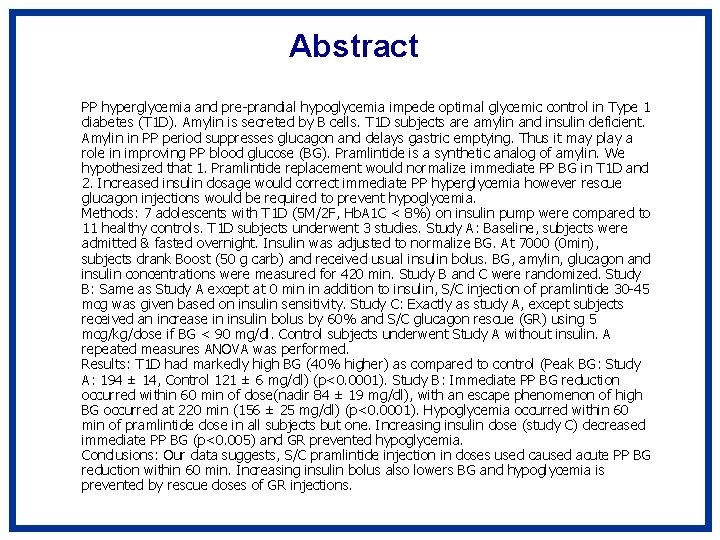
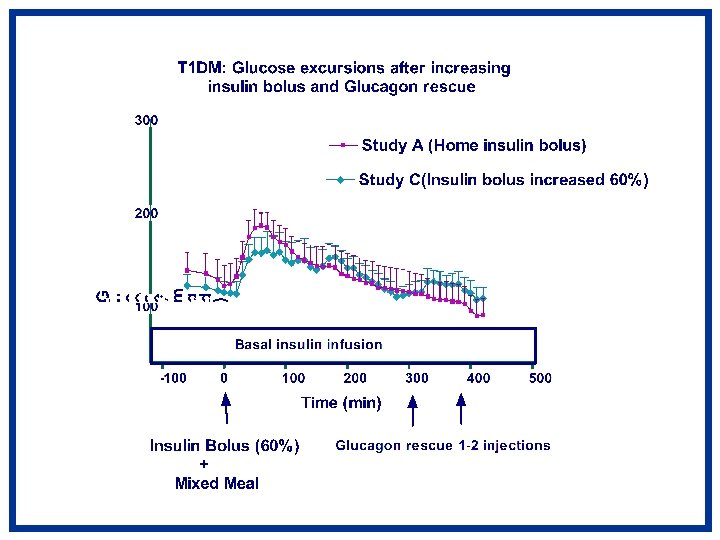
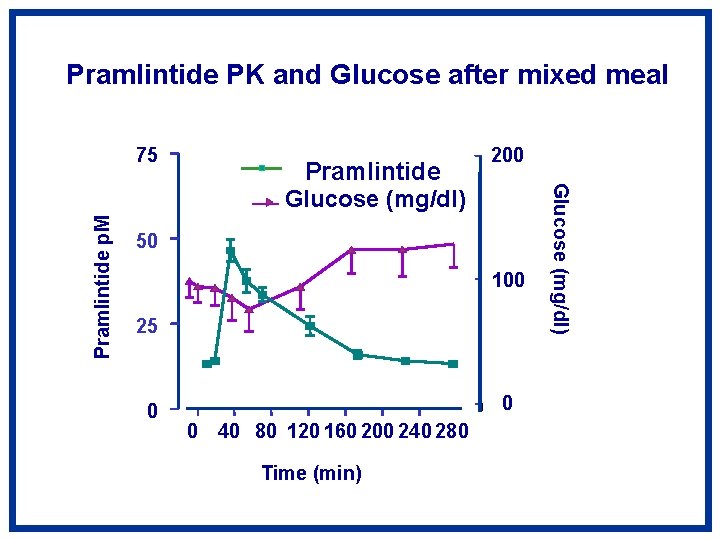
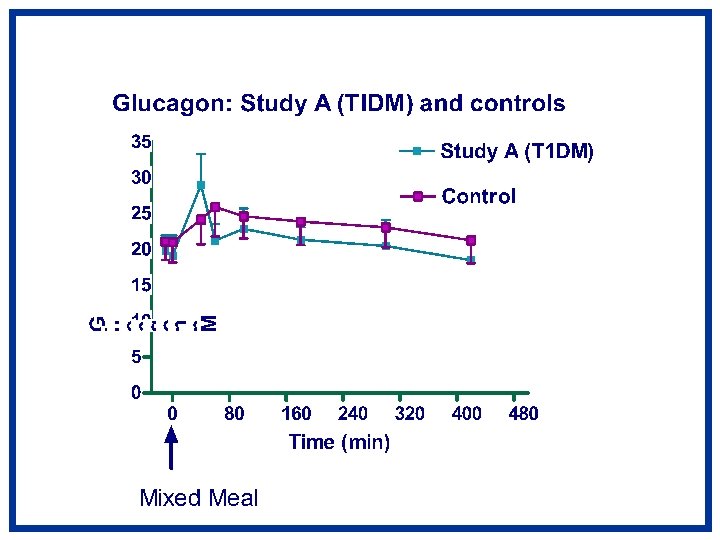
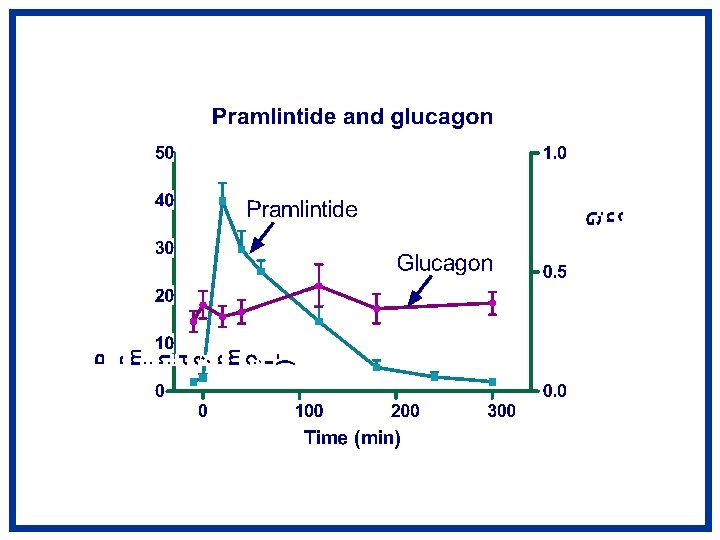
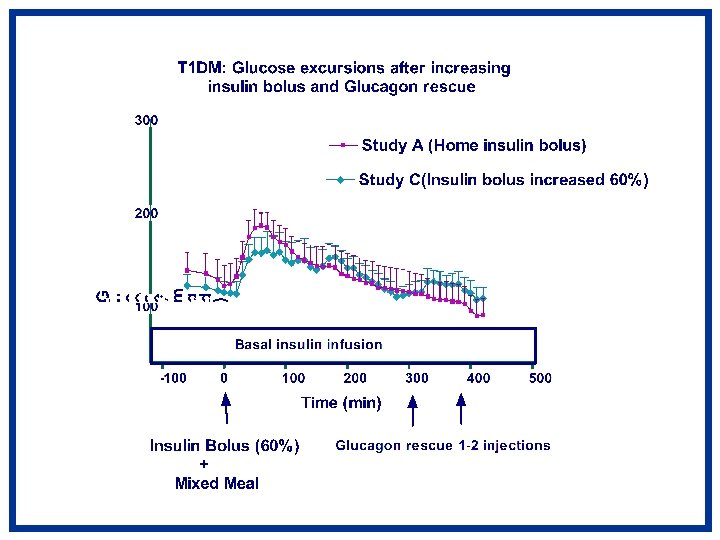
Abstract PP hyperglycemia and pre-prandial hypoglycemia impede optimal glycemic control in Type 1 diabetes (T 1 D). Amylin is secreted by Β cells. T 1 D subjects are amylin and insulin deficient. Amylin in PP period suppresses glucagon and delays gastric emptying. Thus it may play a role in improving PP blood glucose (BG). Pramlintide is a synthetic analog of amylin. We hypothesized that 1. Pramlintide replacement would normalize immediate PP BG in T 1 D and 2. Increased insulin dosage would correct immediate PP hyperglycemia however rescue glucagon injections would be required to prevent hypoglycemia. Methods: 7 adolescents with T 1 D (5 M/2 F, Hb. A 1 C < 8%) on insulin pump were compared to 11 healthy controls. T 1 D subjects underwent 3 studies. Study A: Baseline, subjects were admitted & fasted overnight. Insulin was adjusted to normalize BG. At 7000 (0 min), subjects drank Boost (50 g carb) and received usual insulin bolus. BG, amylin, glucagon and insulin concentrations were measured for 420 min. Study B and C were randomized. Study B: Same as Study A except at 0 min in addition to insulin, S/C injection of pramlintide 30 -45 mcg was given based on insulin sensitivity. Study C: Exactly as study A, except subjects received an increase in insulin bolus by 60% and S/C glucagon rescue (GR) using 5 mcg/kg/dose if BG < 90 mg/dl. Control subjects underwent Study A without insulin. A repeated measures ANOVA was performed. Results: T 1 D had markedly high BG (40% higher) as compared to control (Peak BG: Study A: 194 ± 14, Control 121 ± 6 mg/dl) (p<0. 0001). Study B: Immediate PP BG reduction occurred within 60 min of dose(nadir 84 ± 19 mg/dl), with an escape phenomenon of high BG occurred at 220 min (156 ± 25 mg/dl) (p<0. 0001). Hypoglycemia occurred within 60 min of pramlintide dose in all subjects but one. Increasing insulin dose (study C) decreased immediate PP BG (p<0. 005) and GR prevented hypoglycemia. Conclusions: Our data suggests, S/C pramlintide injection in doses used caused acute PP BG reduction within 60 min. Increasing insulin bolus also lowers BG and hypoglycemia is prevented by rescue doses of GR injections.
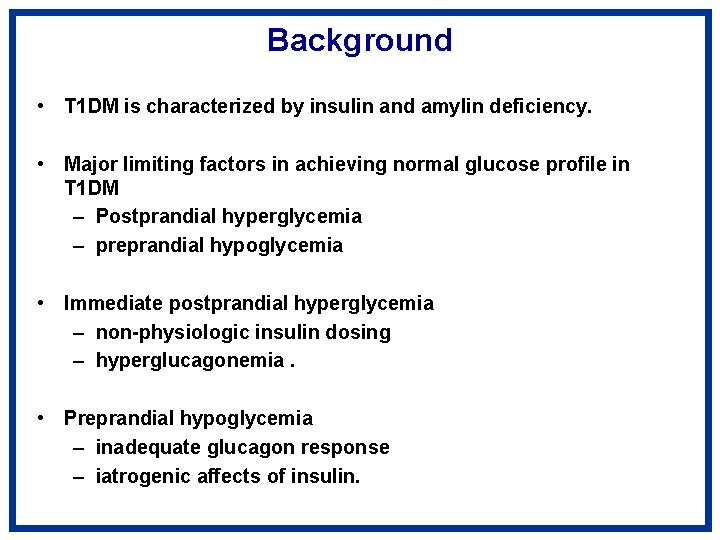
Background • T 1 DM is characterized by insulin and amylin deficiency. • Major limiting factors in achieving normal glucose profile in T 1 DM – Postprandial hyperglycemia – preprandial hypoglycemia • Immediate postprandial hyperglycemia – non-physiologic insulin dosing – hyperglucagonemia. • Preprandial hypoglycemia – inadequate glucagon response – iatrogenic affects of insulin.
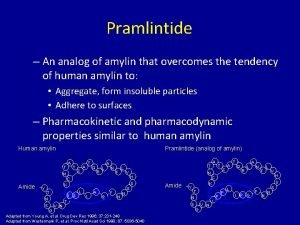
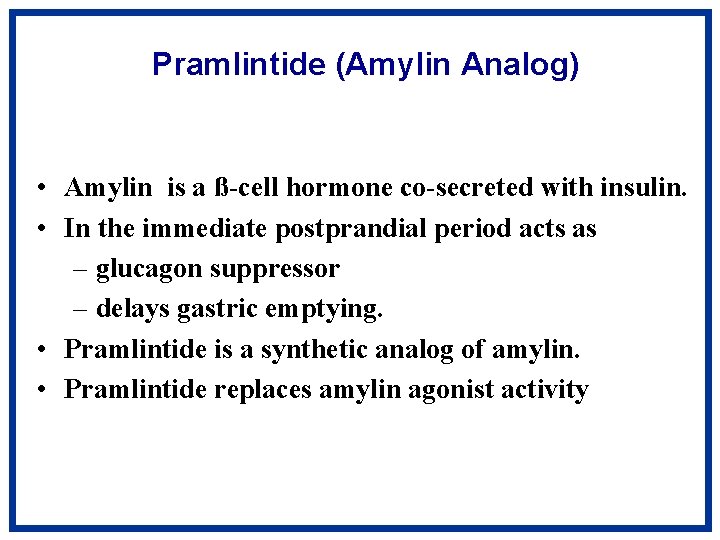
Pramlintide (Amylin Analog) • Amylin is a ß-cell hormone co-secreted with insulin. • In the immediate postprandial period acts as – glucagon suppressor – delays gastric emptying. • Pramlintide is a synthetic analog of amylin. • Pramlintide replaces amylin agonist activity
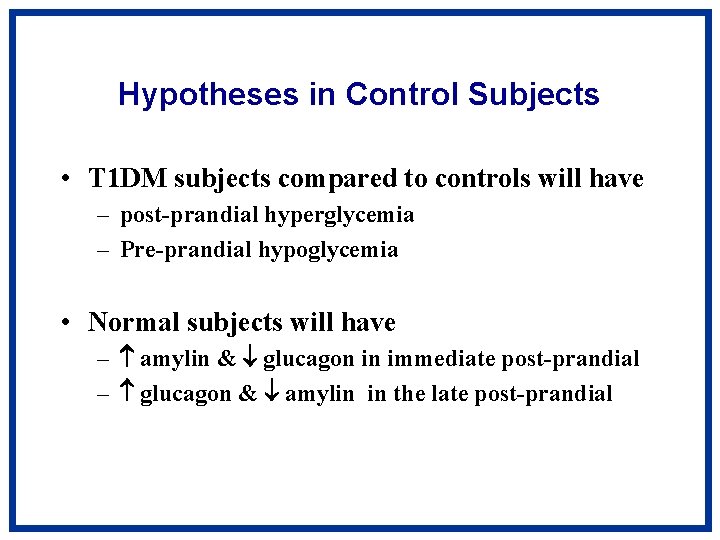
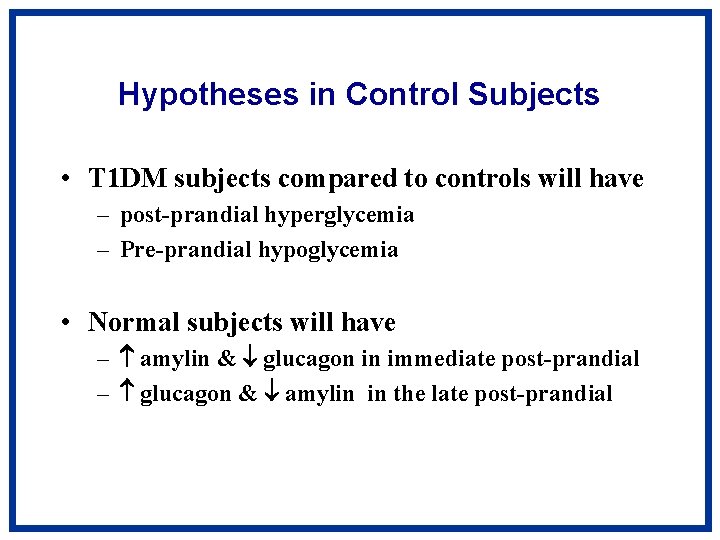
Hypotheses in Control Subjects • T 1 DM subjects compared to controls will have – post-prandial hyperglycemia – Pre-prandial hypoglycemia • Normal subjects will have – amylin & glucagon in immediate post-prandial – glucagon & amylin in the late post-prandial
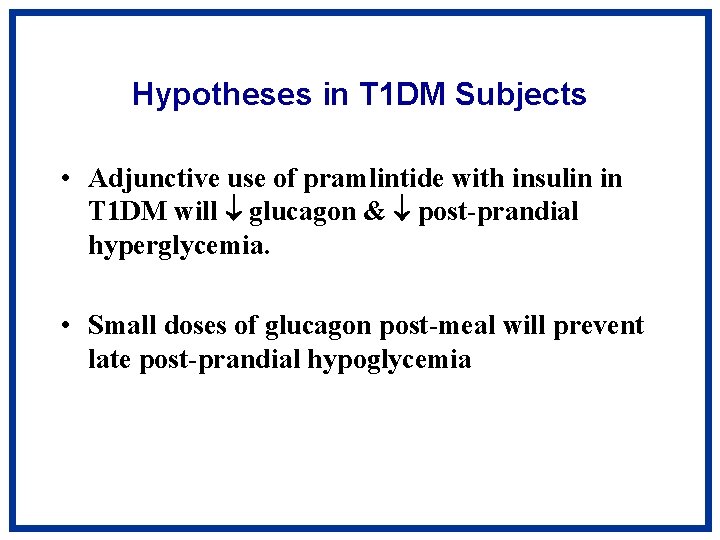
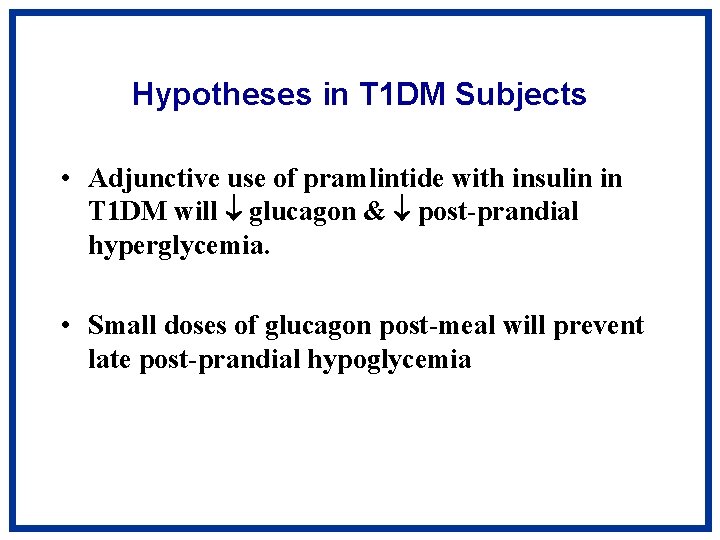
Hypotheses in T 1 DM Subjects • Adjunctive use of pramlintide with insulin in T 1 DM will glucagon & post-prandial hyperglycemia. • Small doses of glucagon post-meal will prevent late post-prandial hypoglycemia

Study Design Controls T 1 DM Study A Study B Study C
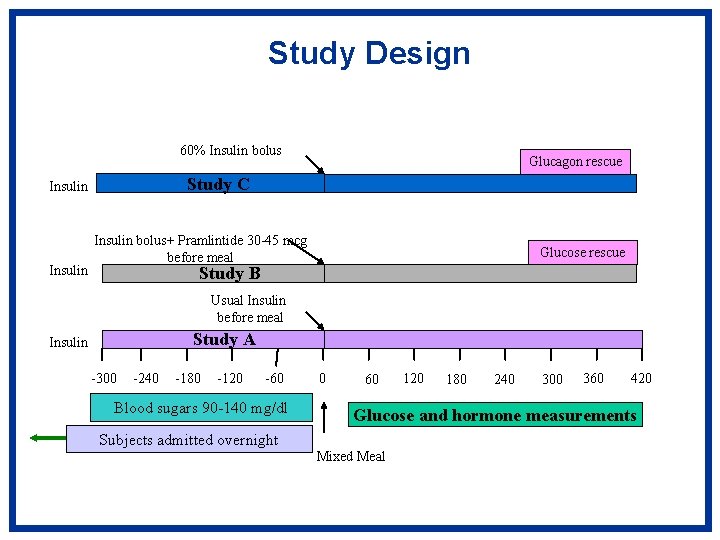
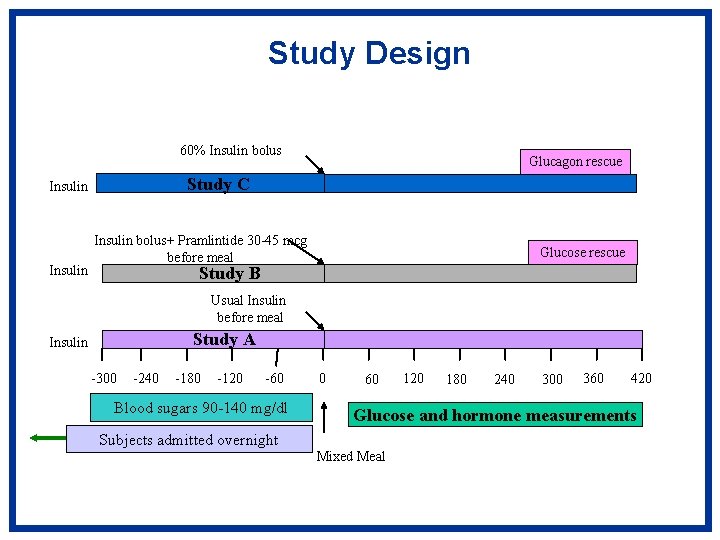
Study Design 60% Insulin bolus Study C Insulin Glucagon rescue Insulin bolus+ Pramlintide 30 -45 mcg before meal Glucose rescue Study B Usual Insulin before meal Study A Insulin -300 -240 -180 -120 -60 Blood sugars 90 -140 mg/dl 0 60 120 180 240 300 360 420 Glucose and hormone measurements Subjects admitted overnight Mixed Meal
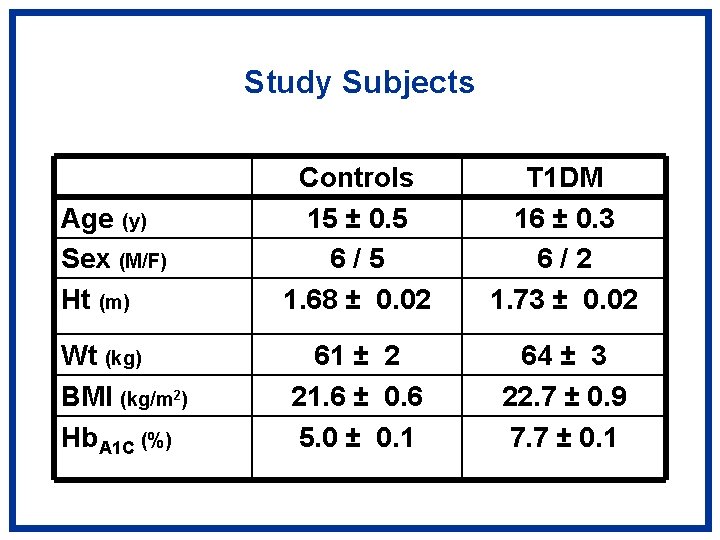
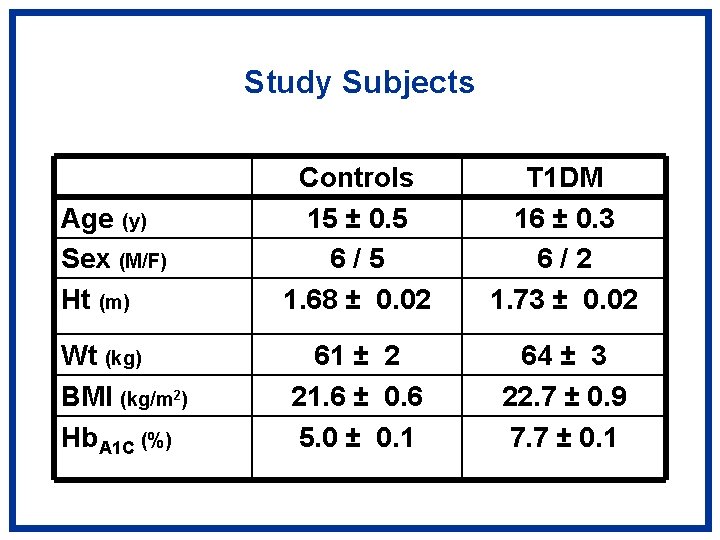
Study Subjects Age (y) Sex (M/F) Ht (m) Controls 15 ± 0. 5 6/5 1. 68 ± 0. 02 T 1 DM 16 ± 0. 3 6/2 1. 73 ± 0. 02 Wt (kg) BMI (kg/m 2) Hb. A 1 C (%) 61 ± 2 21. 6 ± 0. 6 5. 0 ± 0. 1 64 ± 3 22. 7 ± 0. 9 7. 7 ± 0. 1



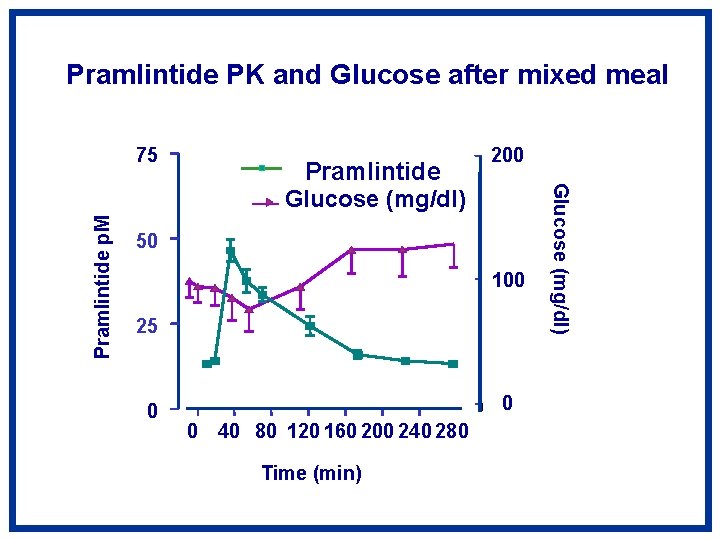
Pramlintide PK and Glucose after mixed meal Pramlintide Glucose (mg/dl) 200 50 100 25 0 0 0 40 80 120 160 200 240 280 Time (min) Glucose (mg/dl) Pramlintide p. M 75
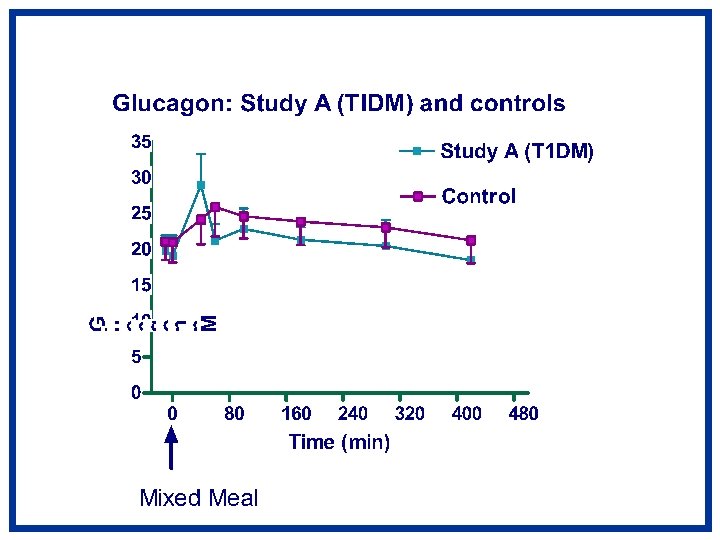
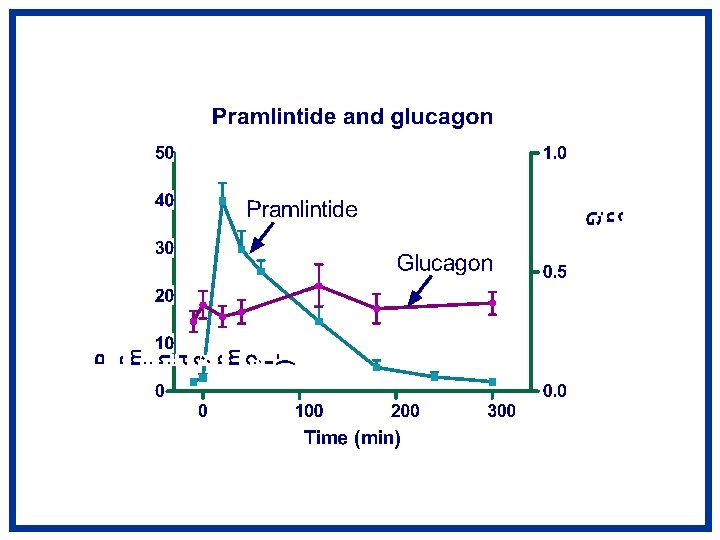


Summary • Compared to controls T 1 DM have – Immediate post-prandial hyperglycemia – Late post-prandial hypoglycemia • Adjunctive use of pre-meal pramlintide – postprandial hyperglycemia – 45 mcg dose caused immediate post-prandial hypoglycemia. • A higher insulin dose (60%) pre-meal, minimally improved postprandial hyperglycemia. • Mini dose rescue glucagon prevented late hypoglycemia
Conclusions • Pramlintide appears to have great clinical potential in decreasing post-prandial hyperglycemia • But in some patients, the higher dose can cause immediate post-prandial hypoglycemia • Gastric emptying may play in the acute suppression of glucose absorption • Pramlintide dosing and delivery may need to be modified to prevent hypoglycemia in children with T 1 DM.
 Median arcuate ligament
Median arcuate ligament B-pleated sheet
B-pleated sheet Glandula suprarrenal
Glandula suprarrenal Glucagon function
Glucagon function Glucagon training video
Glucagon training video Dan muse
Dan muse Glucagon for beta blocker overdose
Glucagon for beta blocker overdose Hormonas concepto
Hormonas concepto Glucagon training video
Glucagon training video Glucose insulin
Glucose insulin Glucagon insulin
Glucagon insulin Glucagon
Glucagon Efectos del glucagon
Efectos del glucagon Functions of glucagon
Functions of glucagon Glucagon is secreted by:
Glucagon is secreted by: Nephron
Nephron Which structure releases glucagon
Which structure releases glucagon Insuline et glucagon
Insuline et glucagon Glucagon
Glucagon Oats glycemic index
Oats glycemic index