Reducing Internal Waits Nottingham University Hospitals Liz Williamson


- Slides: 42
Reducing Internal Waits Nottingham University Hospitals Liz Williamson- Deputy Programme Director Scott Purser- Project Lead
What we plan to cover today • The NUH improvement programme • Why this was important • Getting started • Discovery • Toolkit • Rollout • How we captured the benefits • Developing the toolkit • What the Future holds • Reflections
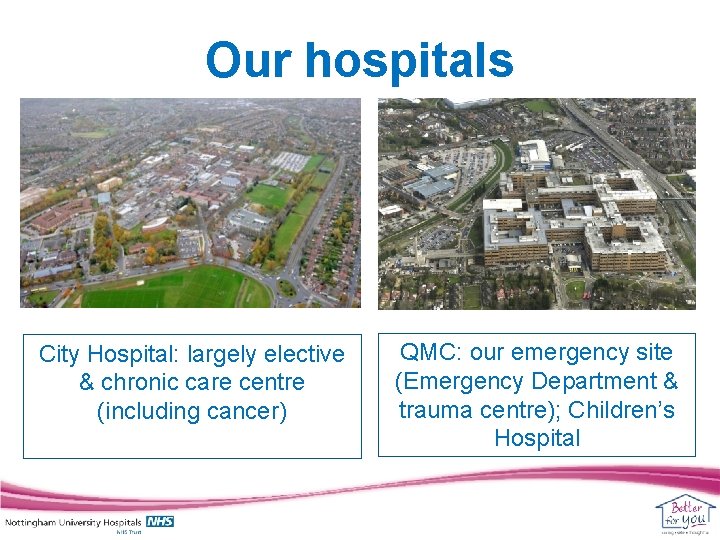
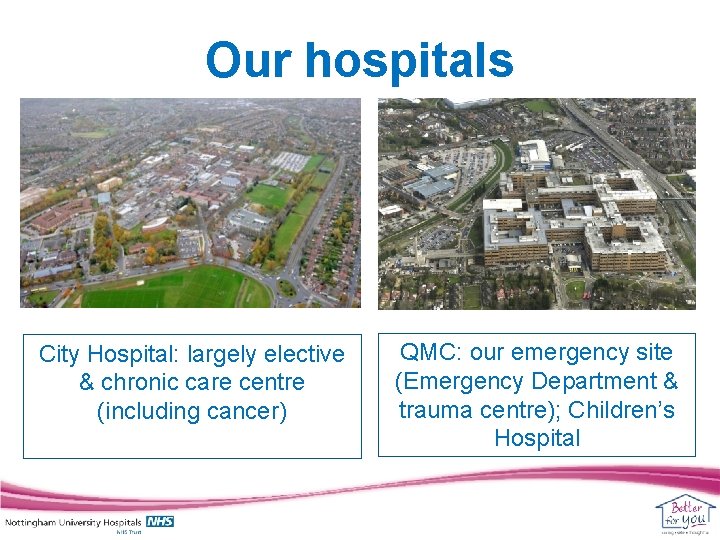
Our hospitals City Hospital: largely elective & chronic care centre (including cancer) QMC: our emergency site (Emergency Department & trauma centre); Children’s Hospital
Our vital statistics • Turnover £ 755 million • Circa 1, 700 beds and 87 wards • Over 13, 000 staff & 1, 200 volunteers • 180, 000 A&E attendances and 96, 000 admissions • 66, 000 day cases and 24, 000 elective operations

Our whole hospital improvement programme is called “Better for You” • Started in 2009/10, Better for You is our most comprehensive improvement programme • It is a quality driven programme, which releases financial savings • Currently, 250+ projects across the organisation, directly involving 2000+ staff • Change, which is caring, safe and thoughtful • The key feature is staff and patient engagement
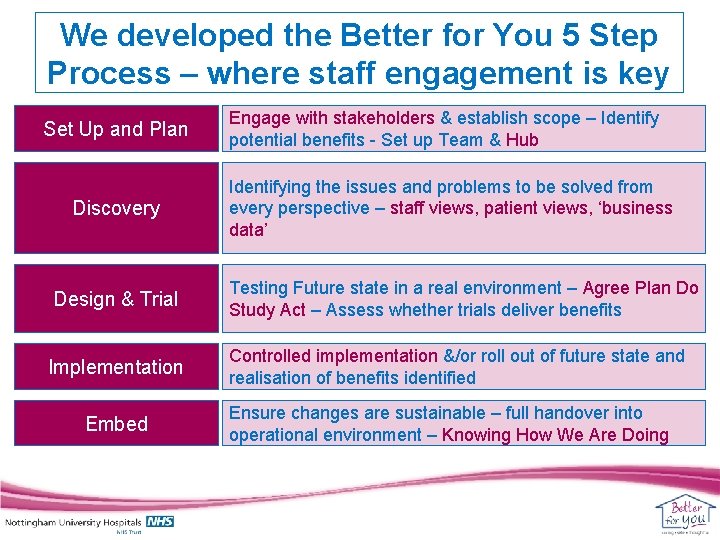
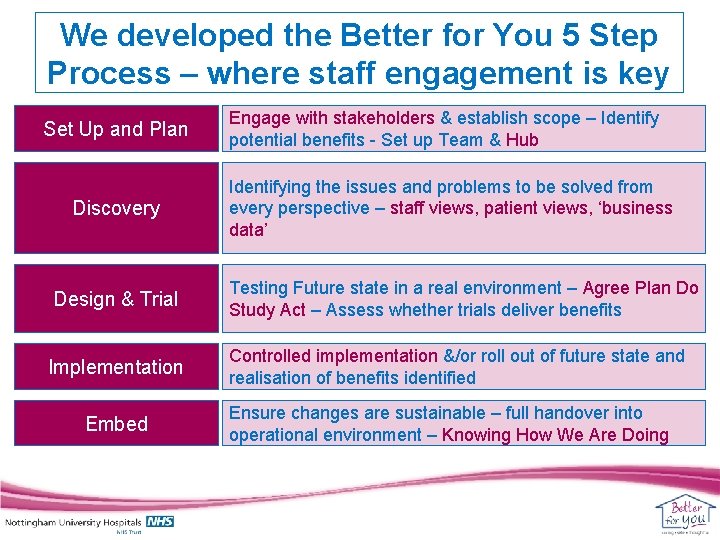
We developed the Better for You 5 Step Process – where staff engagement is key Set Up and Plan Discovery Design & Trial Implementation Embed Engage with stakeholders & establish scope – Identify potential benefits - Set up Team & Hub Identifying the issues and problems to be solved from every perspective – staff views, patient views, ‘business data’ Testing Future state in a real environment – Agree Plan Do Study Act – Assess whether trials deliver benefits Controlled implementation &/or roll out of future state and realisation of benefits identified Ensure changes are sustainable – full handover into operational environment – Knowing How We Are Doing
Why did we need to reduce patient waits? • Good quality care is helped by good patient flow – Improvements to the Emergency Pathway relies on consistent ‘pull’ from the specialties • To meet some of our formidable challenges (activity, £££) – We needed to shrink our in-patient capacity (“more with less”? ) • We respect patient’s time and do not want to keep healthy people in hospital – We want patients to have a positive experience – Some staff have learnt to accept/not challenge internal waits • Research says hospital stays can create safety issues • In-patient/hospital care is a scarce and expensive resource
Aim and Scope of the project • Identify where and why waits occurred – Identify opportunities to work differently and/or smarter – Support directorate CIP plans • Reducing LOS • Reducing in-patient beds • Reduce the number of waits by 5080% • All adult wards Point us in the direction of where the opportunities for improvement might be
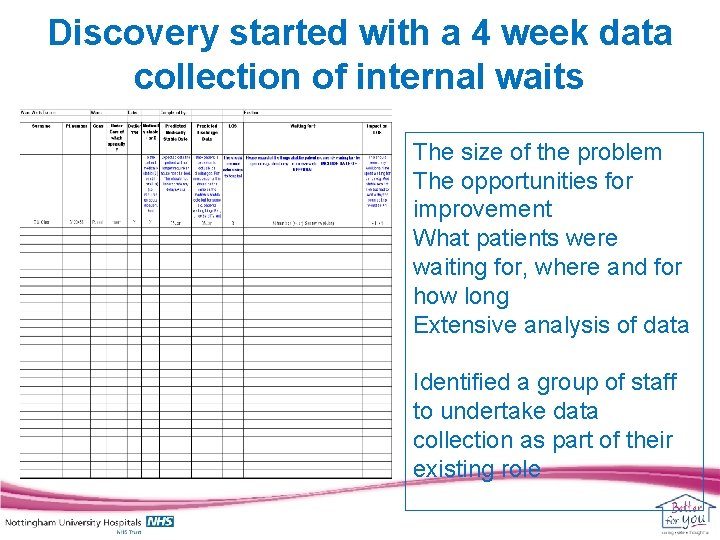
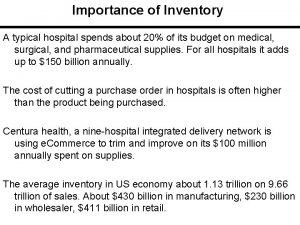
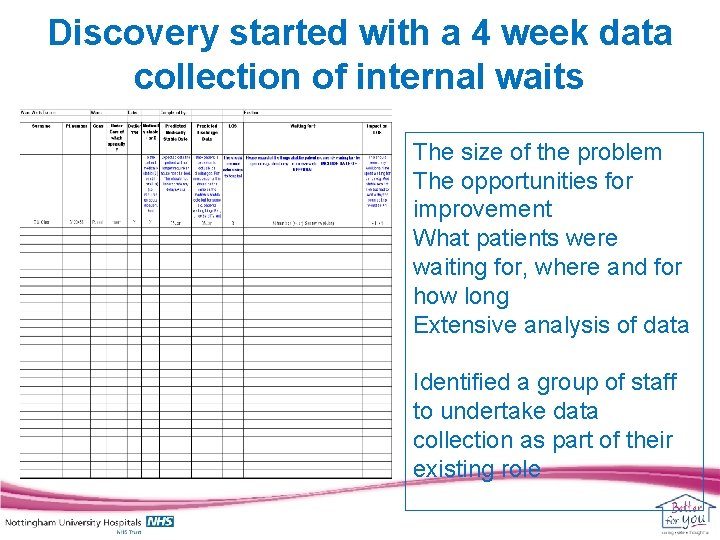
Discovery started with a 4 week data collection of internal waits The size of the problem The opportunities for improvement What patients were waiting for, where and for how long Extensive analysis of data Identified a group of staff to undertake data collection as part of their existing role
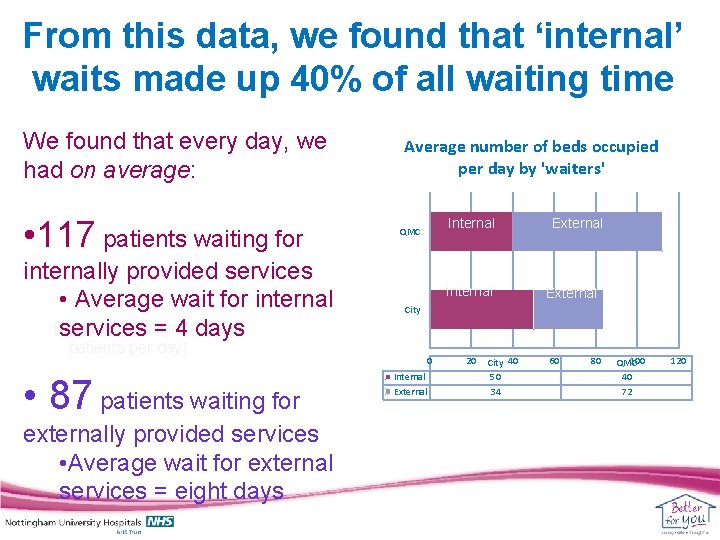
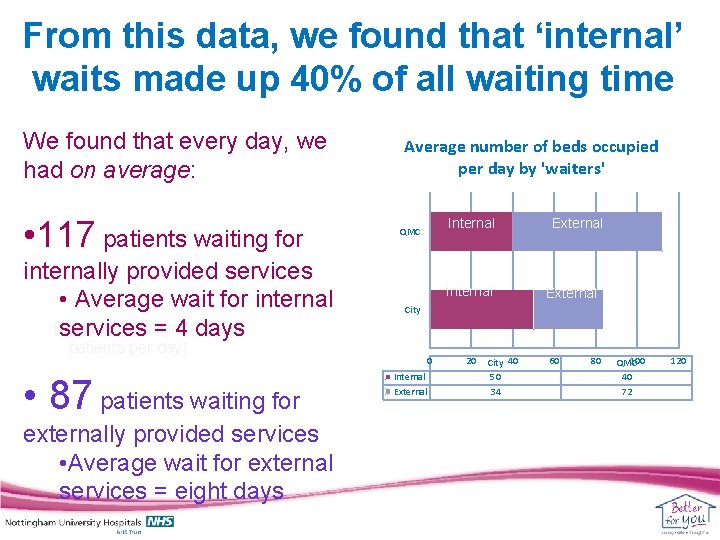
From this data, we found that ‘internal’ waits made up 40% of all waiting time We found that every day, we had on average: • 117 patients waiting for Internal (average 117 patients per day) internally provided services day) • Average wait for internal External (average services = 487 days Average number of beds occupied per day by 'waiters' externally provided services • Average wait for external services = eight days External Internal (476 bed Internal External days) City patients per day) • 87 patients waiting for Internal QMC 0 Internal External 20 City 40 50 34 60 80 100 QMC 40 72 120
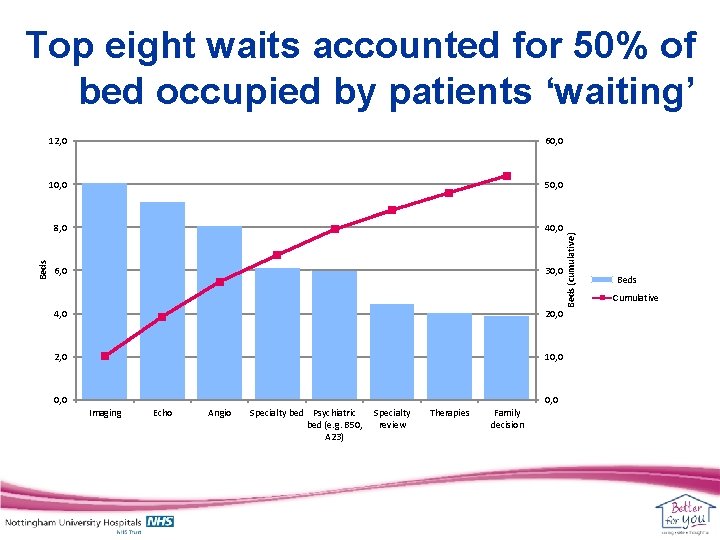
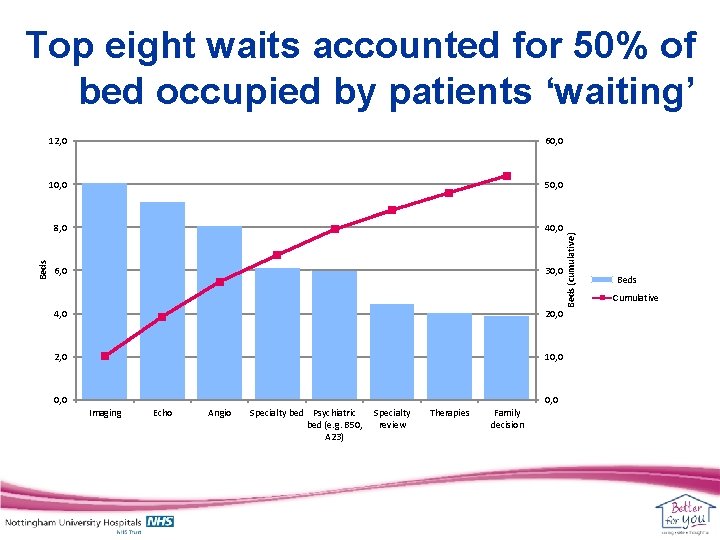
12, 0 60, 0 10, 0 50, 0 8, 0 40, 0 6, 0 30, 0 4, 0 20, 0 2, 0 10, 0 Imaging Echo Angio Specialty bed Psychiatric bed (e. g. B 50, A 23) Specialty review Therapies Family decision Beds (cumulative) Beds Top eight waits accounted for 50% of bed occupied by patients ‘waiting’ Beds Cumulative
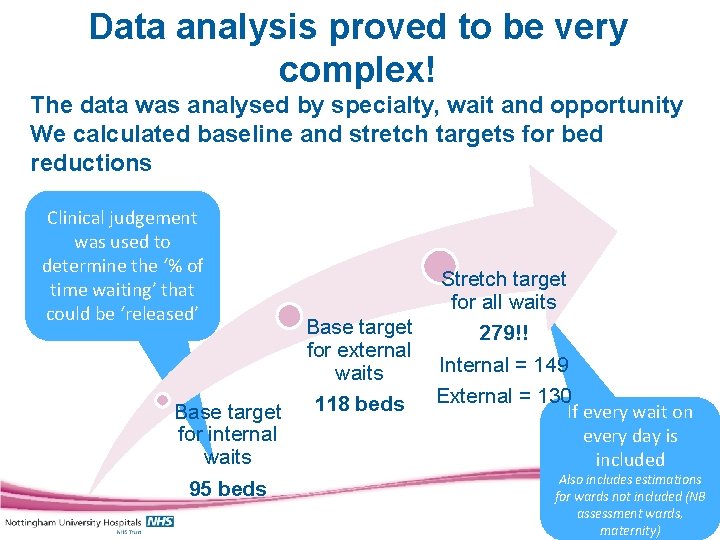
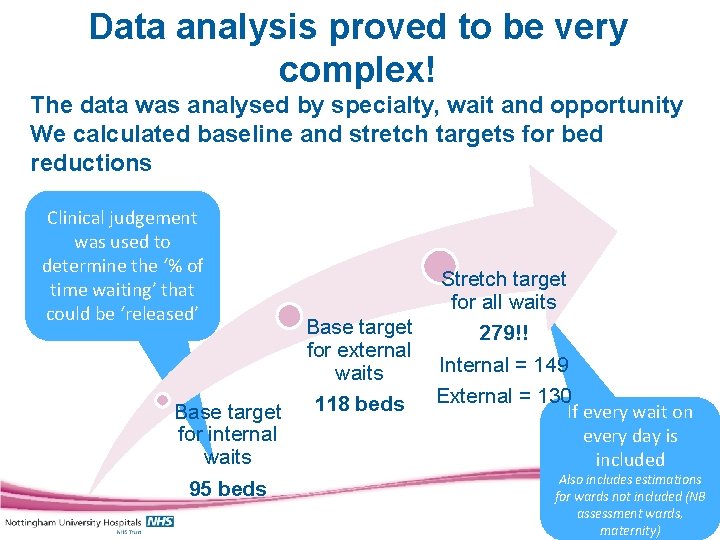
Data analysis proved to be very complex! The data was analysed by specialty, wait and opportunity We calculated baseline and stretch targets for bed reductions Clinical judgement was used to determine the ‘% of time waiting’ that could be ‘released’ Base target for internal waits 95 beds Base target for external waits 118 beds Stretch target for all waits 279!! Internal = 149 External = 130 If every wait on every day is included Also includes estimations for wards not included (NB assessment wards, maternity)
We needed a message which created shared drive for (the need for) change • Patient safety is paramount • Financial imperative to reduce costs An in-patient wait is a wasted resource and exposes patients to unnecessary risk
We took the decision early on that we needed to ‘do something’ across the trust and at pace • Set up a Steering Group – initially chaired by the Deputy CEO/Do. N • Key involvement – Medical Director, senior nurses • Early involvement with other improvement projects (imaging, heart services) 14
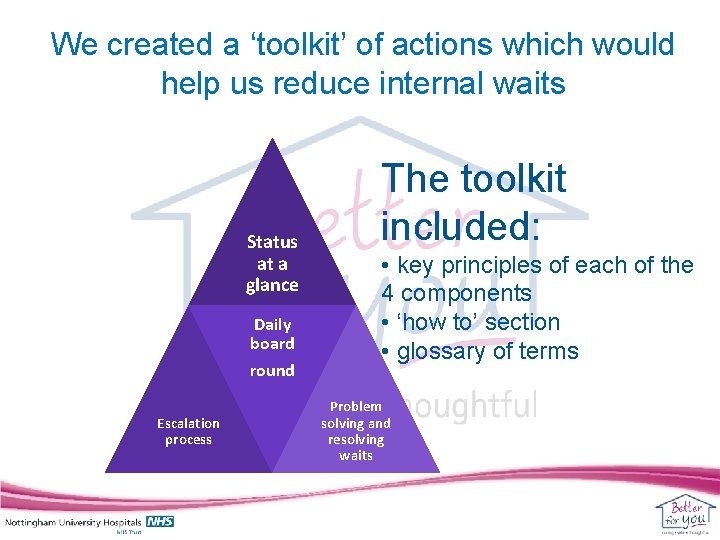
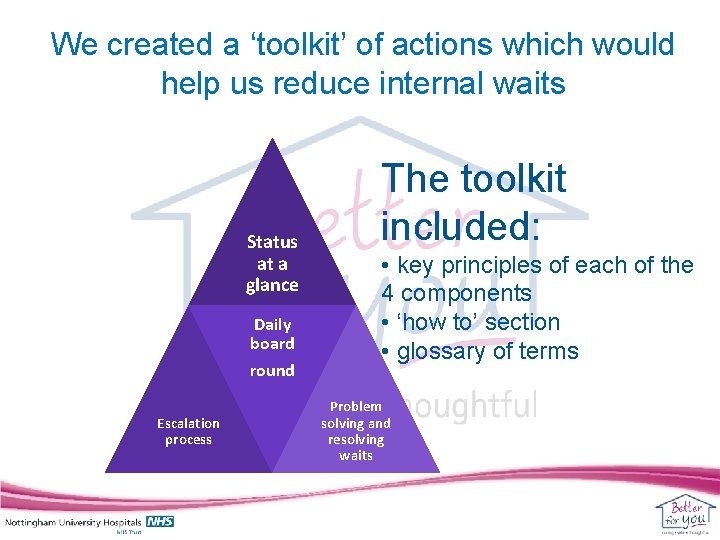
We created a ‘toolkit’ of actions which would help us reduce internal waits Status at a glance Daily board round Escalation process The toolkit included: • key principles of each of the 4 components • ‘how to’ section • glossary of terms Problem solving and resolving waits
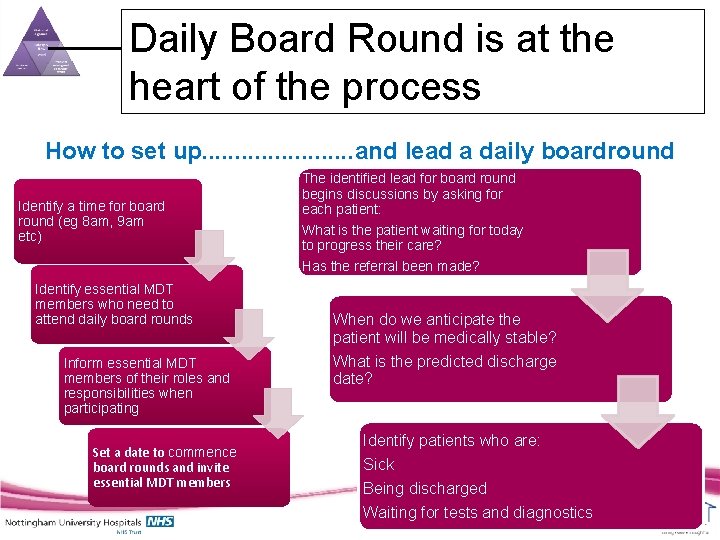
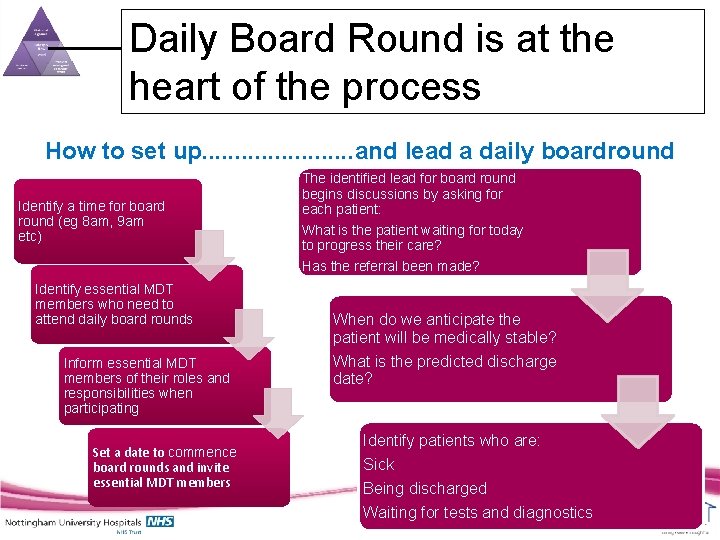
Daily Board Round is at the heart of the process How to set up. . . and lead a daily boardround Identify a time for board round (eg 8 am, 9 am etc) Identify essential MDT members who need to attend daily board rounds Inform essential MDT members of their roles and responsibilities when participating Set a date to commence board rounds and invite essential MDT members The identified lead for board round begins discussions by asking for each patient: What is the patient waiting for today to progress their care? Has the referral been made? When do we anticipate the patient will be medically stable? What is the predicted discharge date? Identify patients who are: Sick Being discharged Waiting for tests and diagnostics
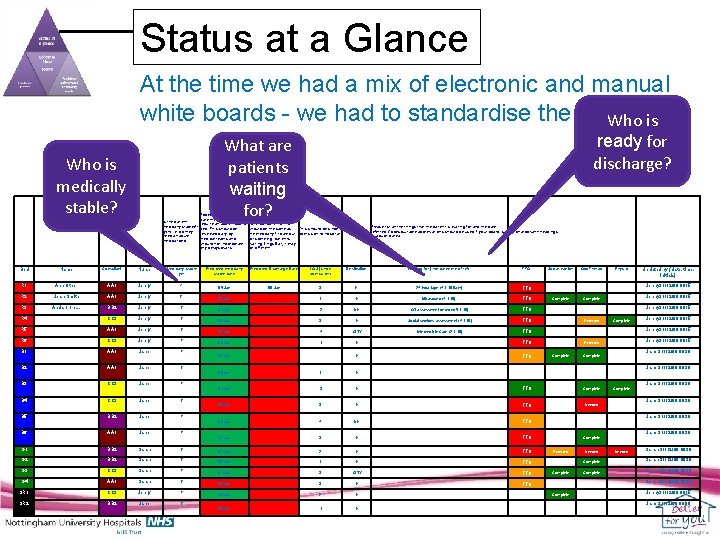
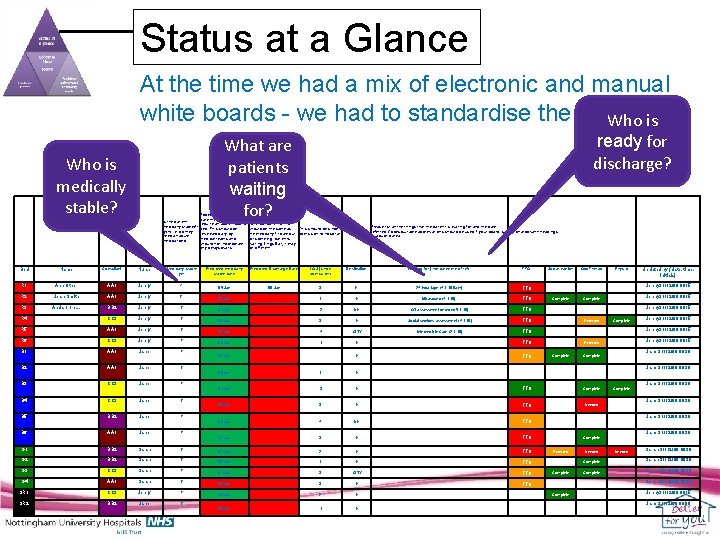
Status at a Glance At the time we had a mix of electronic and manual white boards - we had to standardise the layout Who is medically stable? Is the patient medically stable/fit (y/n) i. e. do they need an acute medical bed Expected date the patient will no longer require an acute hospital bed. This should be reviewed daily by medical teams and should not incorporate any delays/waits Medically stable y/n Predicted medically stable date Predicted Discharge Date LOS (since admission) Destination Waiting for (incl date/time of ref) TTO Social worker Occ Therap Physio 05 -Jan 06 -Jan 3 H 24 hour tape (4. 1. 10 9 am) TTO Needed Complete Name Consultant Nurse R 1 Ann Other AA 1 Jenny X R 2 Jean Smith AA 1 Jenny y R 3 And so on…. BB 2 Jenny y R 4 CC 3 Jenny y R 5 AA 1 Jenny y R 6 CC 3 Jenny n B 1 AA 1 Jane n Jane y Bed ready for discharge? What are patients waiting for? Date patient is expected to actually be discharged. For most patients this should be the same as This should be since the medically fit date but admission to hospital for some e. g. patients waiting Lings Bar, it may be different 02 -Jan 1 H Ultrasound (4. 1. 10) TTO 01 -Jan 2 NH OT assessment (referred 5. 1. 10) TTO 03 -Jan 3 H Social services assessment (4. 1. 10) TTO 02 -Jan 4 CITY Internediate Care (2. 1. 10) TTO 03 -Jan 1 H TTO 02 -Jan B 2 B 3 B 4 B 5 B 6 AA 1 CC 3 BB 2 AA 1 Jane Please list all the things that the patient is waiting for and the date referred. Codes/suitable abbreviations should be used if your board is Optional column headings in a public area Jenny 31/12/08 0815 Referred Complete Jenny 31/12/08 0815 Jane 31/12/08 0830 Complete Jane 31/12/08 0830 09 -Jan 1 H 01 -Jan 3 H TTO Complete 03 -Jan 3 H TTO Needed 03 -Jan 4 NH TTO 02 -Jan 3 H TTO 04 -Jan 2 H TTO 02 -Jan 1 H TTO 01 -Jan 3 CITY TTO 03 -Jan 3 H TTO 10 -Jan 2 H 06 -Jan 1 H Jane 31/12/08 0830 Complete Jane 31/12/08 0830 n BB 2 Sarah y G 3 CC 3 Sarah n G 4 AA 1 Sarah y SR 1 CC 3 Jenny n SR 2 BB 2 Jane y Jenny 31/12/08 0815 Referred y G 2 Jenny 31/12/08 0815 n G 1 Updated by (date, time, initials) Jane 31/12/08 0830 Complete Referred Complete Needed Sarah 31/12/08 0830 Complete Jenny 31/12/08 0815 Jane 31/12/08 0830
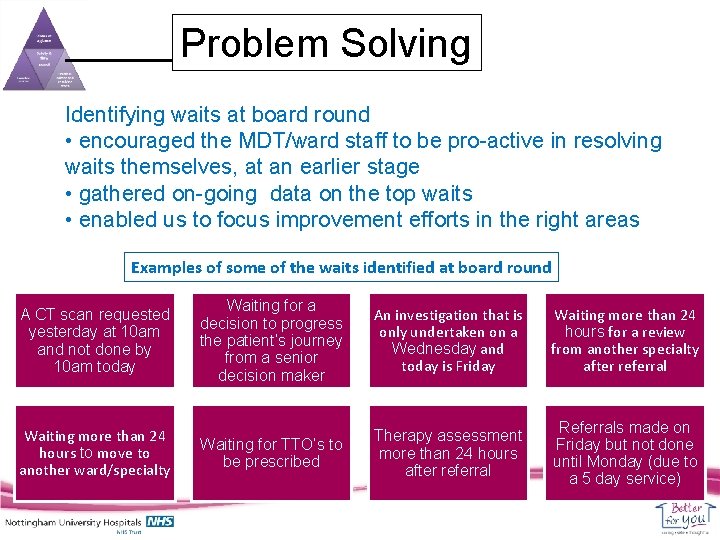
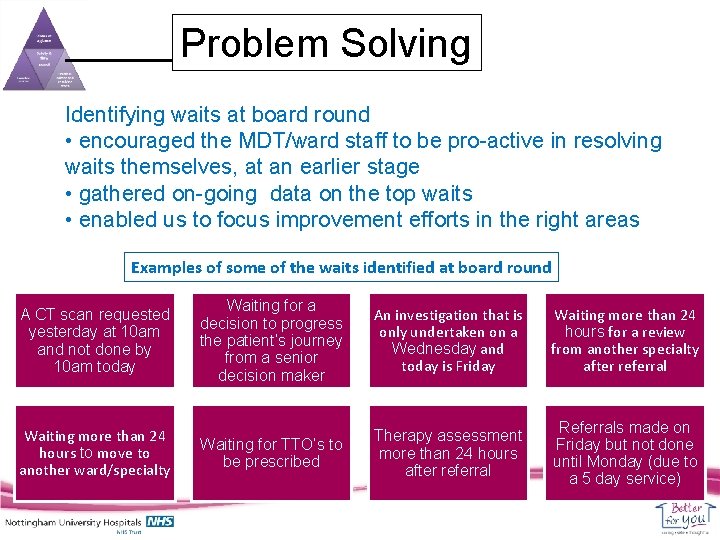
Problem Solving Identifying waits at board round • encouraged the MDT/ward staff to be pro-active in resolving waits themselves, at an earlier stage • gathered on-going data on the top waits • enabled us to focus improvement efforts in the right areas Examples of some of the waits identified at board round A CT scan requested yesterday at 10 am and not done by 10 am today Waiting more than 24 hours to move to another ward/specialty Waiting for a decision to progress the patient’s journey from a senior decision maker An investigation that is only undertaken on a Wednesday and today is Friday Waiting more than 24 hours for a review from another specialty after referral Waiting for TTO’s to be prescribed Therapy assessment more than 24 hours after referral Referrals made on Friday but not done until Monday (due to a 5 day service)
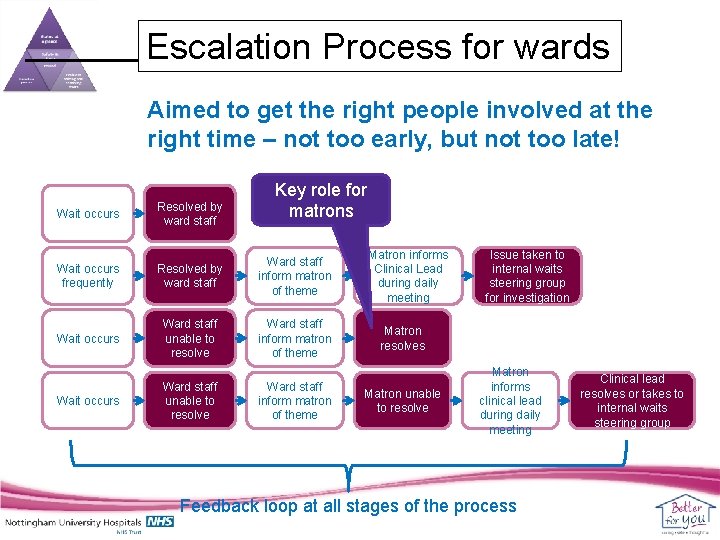
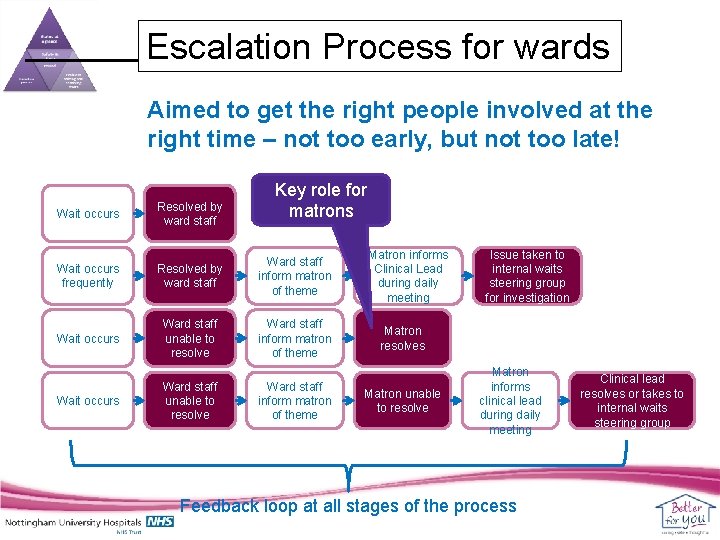
Escalation Process for wards Aimed to get the right people involved at the right time – not too early, but not too late! Wait occurs Resolved by ward staff Key role for matrons Wait occurs frequently Resolved by ward staff Ward staff inform matron of theme Wait occurs Ward staff unable to resolve Ward staff inform matron of theme Matron informs Clinical Lead during daily meeting Issue taken to internal waits steering group for investigation Matron resolves Matron unable to resolve Matron informs clinical lead during daily meeting Feedback loop at all stages of the process Clinical lead resolves or takes to internal waits steering group
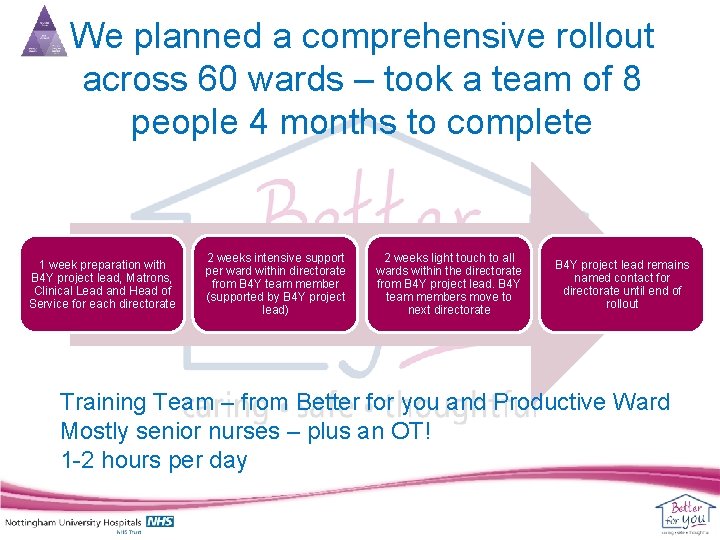
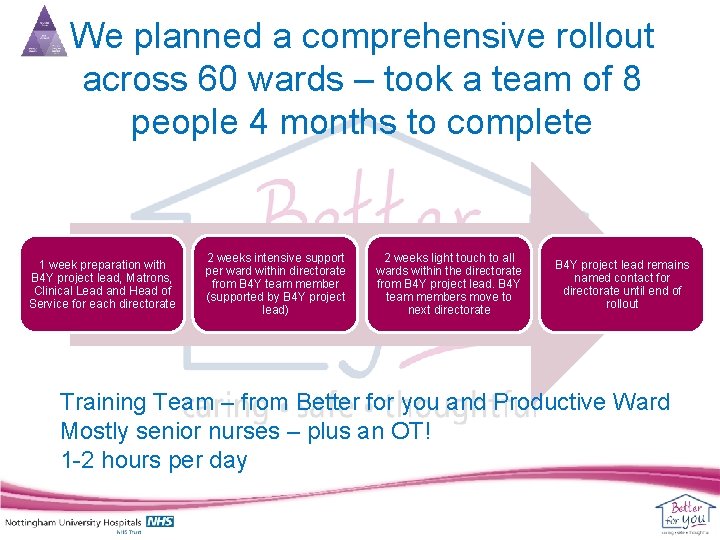
We planned a comprehensive rollout across 60 wards – took a team of 8 people 4 months to complete 1 week preparation with B 4 Y project lead, Matrons, Clinical Lead and Head of Service for each directorate 2 weeks intensive support per ward within directorate from B 4 Y team member (supported by B 4 Y project lead) 2 weeks light touch to all wards within the directorate from B 4 Y project lead. B 4 Y team members move to next directorate B 4 Y project lead remains named contact for directorate until end of rollout Training Team – from Better for you and Productive Ward Mostly senior nurses – plus an OT! 1 -2 hours per day
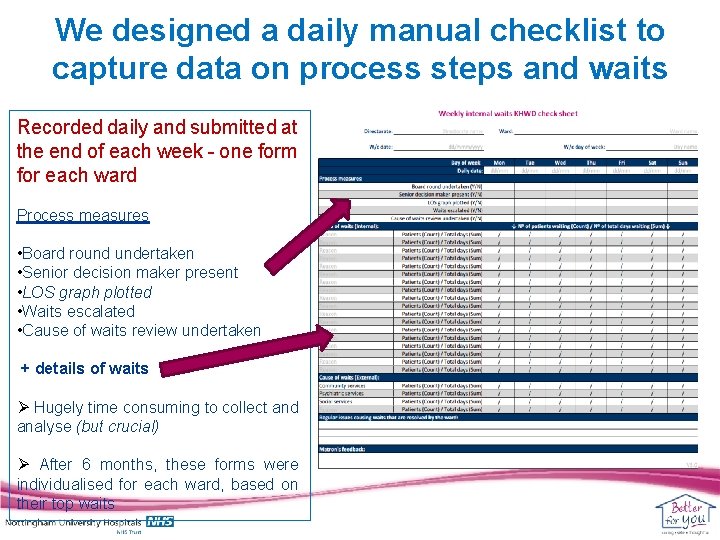
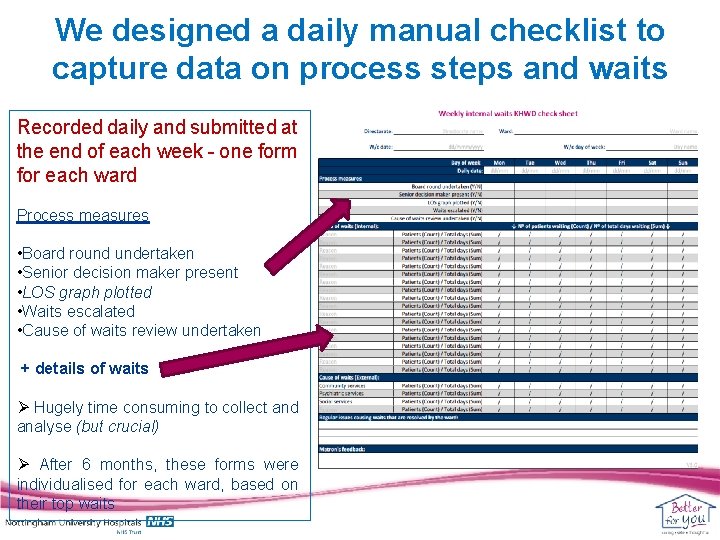
We designed a daily manual checklist to capture data on process steps and waits Recorded daily and submitted at the end of each week - one form for each ward Process measures • Board round undertaken • Senior decision maker present • LOS graph plotted • Waits escalated • Cause of waits review undertaken + details of waits Ø Hugely time consuming to collect and analyse (but crucial) Ø After 6 months, these forms were individualised for each ward, based on their top waits
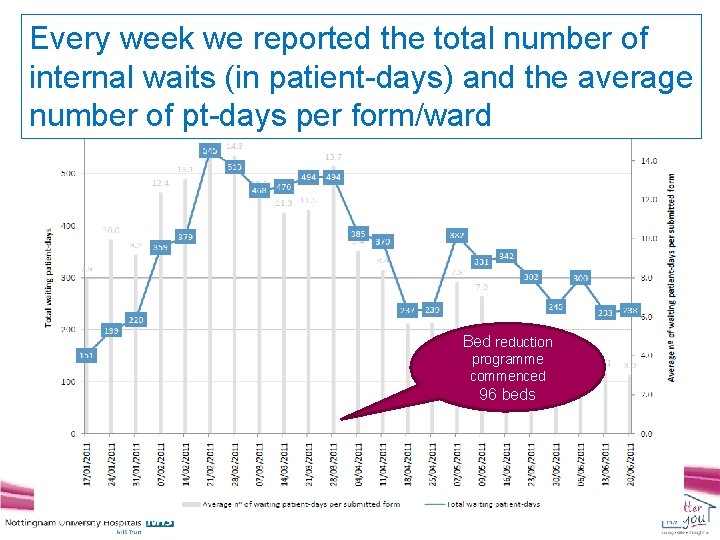
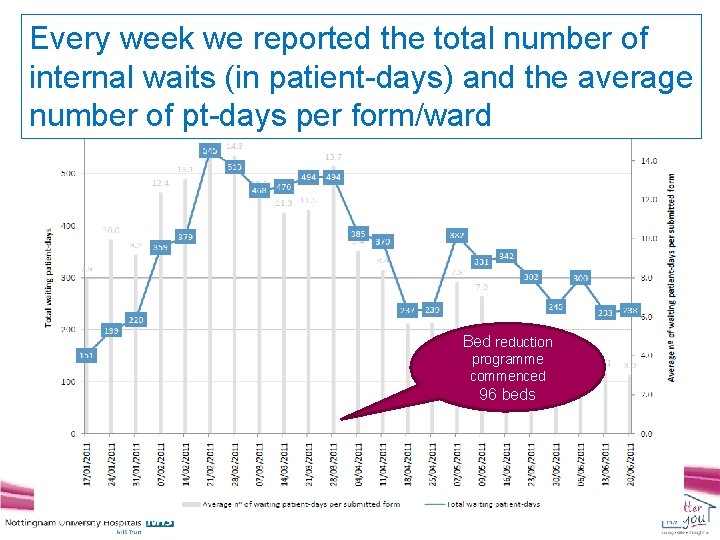
Every week we reported the total number of internal waits (in patient-days) and the average number of pt-days per form/ward Bed reduction programme commenced 96 beds
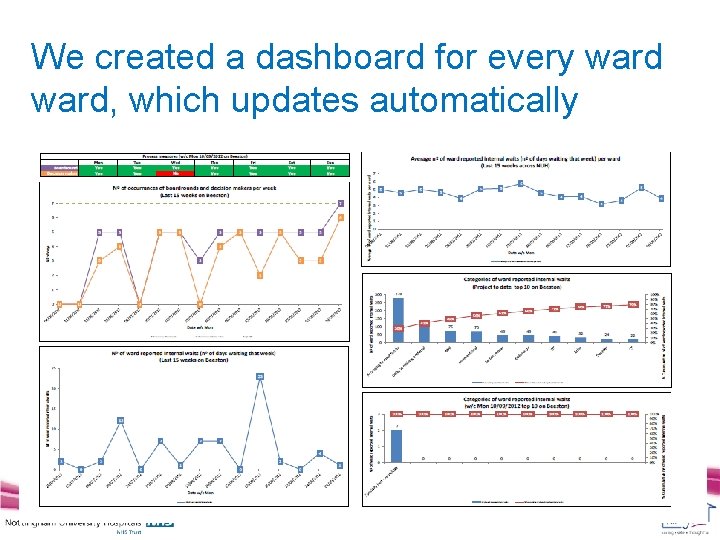
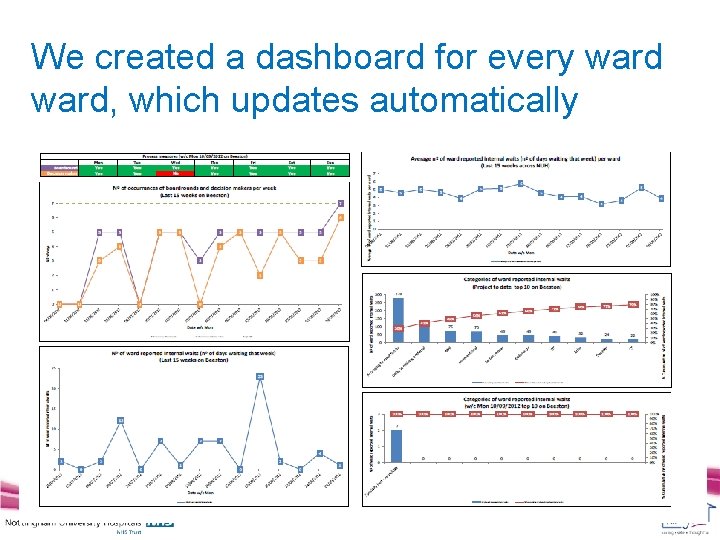
We created a dashboard for every ward, which updates automatically
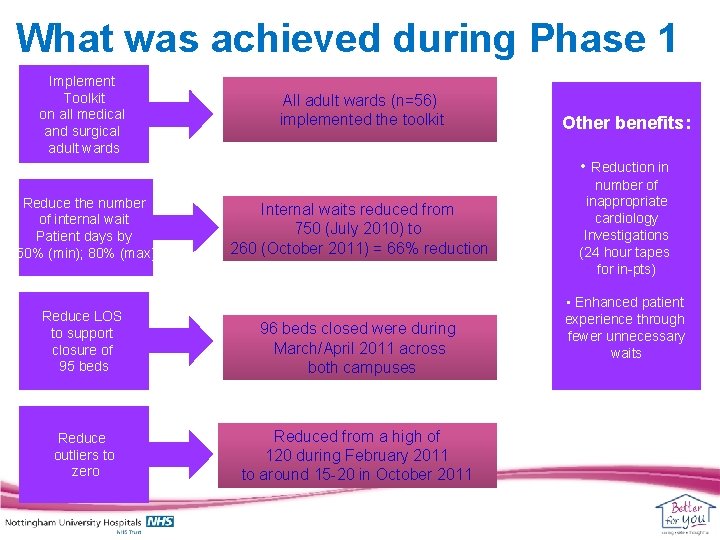
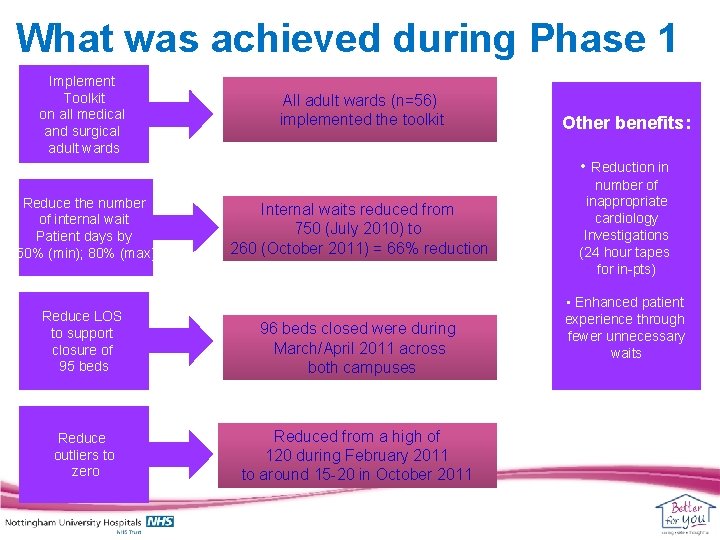
What was achieved during Phase 1 Implement Toolkit on all medical and surgical adult wards Reduce the number of internal wait Patient days by 50% (min); 80% (max) All adult wards (n=56) implemented the toolkit Other benefits: • Reduction in Internal waits reduced from 750 (July 2010) to 260 (October 2011) = 66% reduction Reduce LOS to support closure of 95 beds 96 beds closed were during March/April 2011 across both campuses Reduce outliers to zero Reduced from a high of 120 during February 2011 to around 15 -20 in October 2011 number of inappropriate cardiology Investigations (24 hour tapes for in-pts) • Enhanced patient experience through fewer unnecessary waits
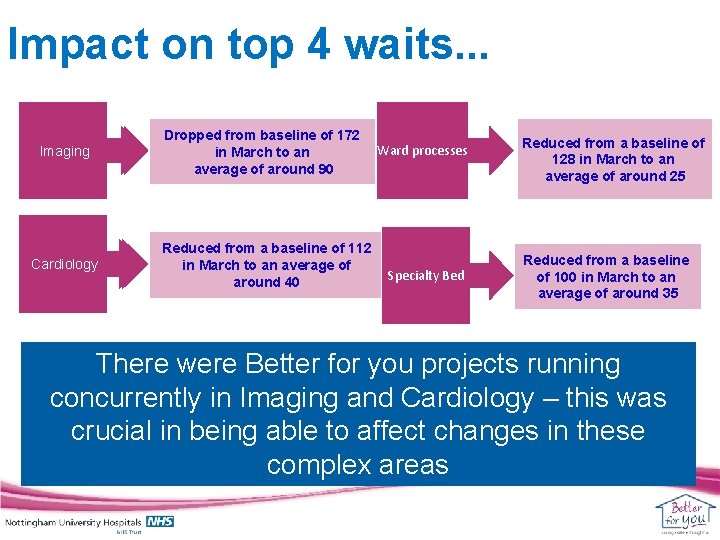
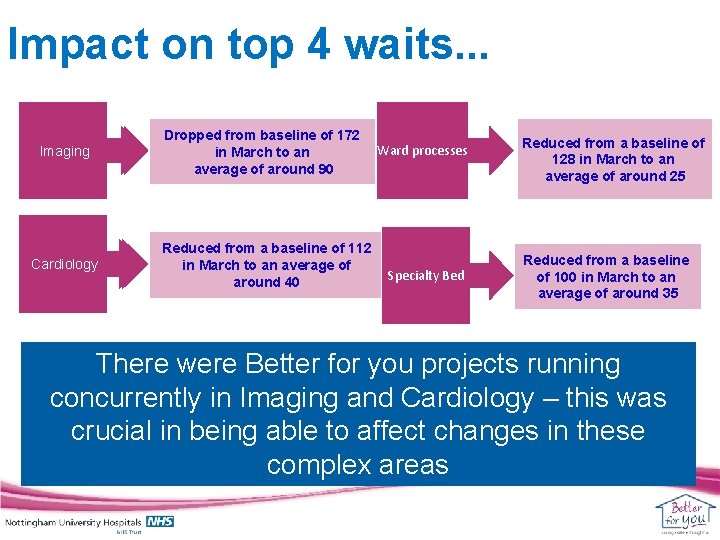
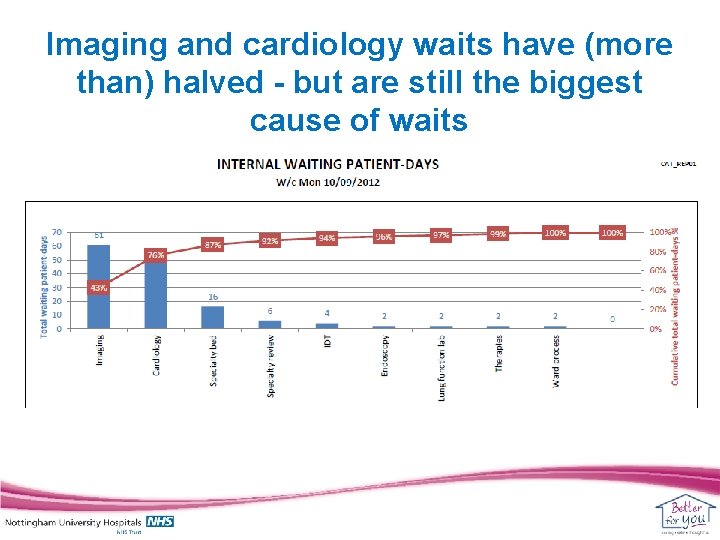
Impact on top 4 waits. . . Imaging Cardiology Droppedfrom baseline of of 172 in. March to to an an in averageof ofaround 90 90 average Reducedfromaabaselineof of 112 in. March to to an an average of of in around 40 40 around Ward processes Specialty Bed Reduced from a baseline of 128 in March to an average of around 25 Reduced from a baseline of 100 in March to an average of around 35 There were Better for you projects running concurrently in Imaging and Cardiology – this was crucial in being able to affect changes in these complex areas
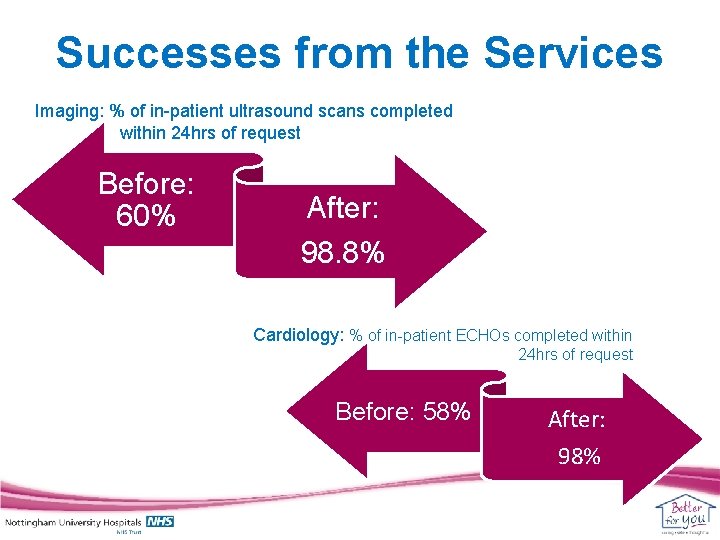
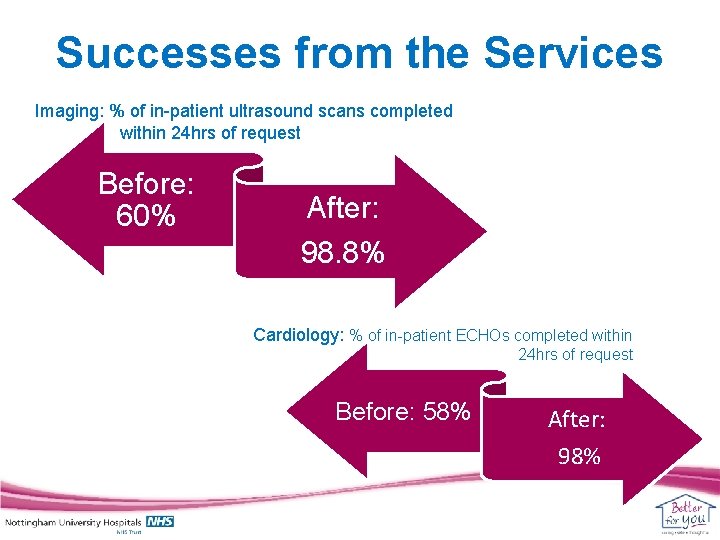
Successes from the Services Imaging: % of in-patient ultrasound scans completed within 24 hrs of request Before: 60% After: 98. 8% Cardiology: % of in-patient ECHOs completed within 24 hrs of request Before: 58% After: 98%
How staff felt about the project. . . You have won me over! I didn’t think it would make a difference but it has! Being able to see how long patients have been in hospital is a real eye opener I can now tell my patients what’s going to happen next and when we’re planning for them to go home We have tried to improve our communication as a team for a while now - a daily board round has given us the ability to progress this
Reducing Internal Waits The Future
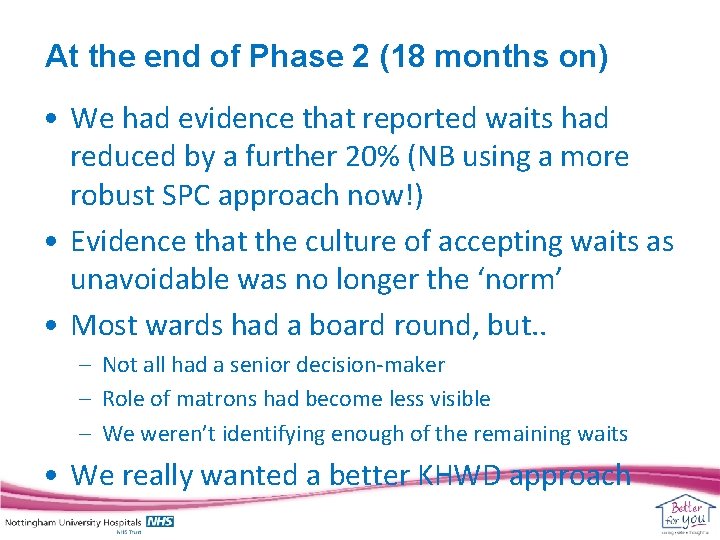
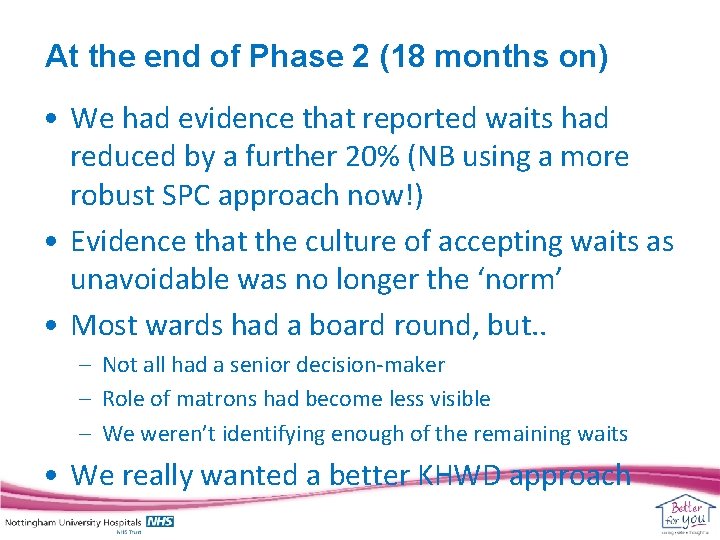
At the end of Phase 2 (18 months on) • We had evidence that reported waits had reduced by a further 20% (NB using a more robust SPC approach now!) • Evidence that the culture of accepting waits as unavoidable was no longer the ‘norm’ • Most wards had a board round, but. . – Not all had a senior decision-maker – Role of matrons had become less visible – We weren’t identifying enough of the remaining waits • We really wanted a better KHWD approach
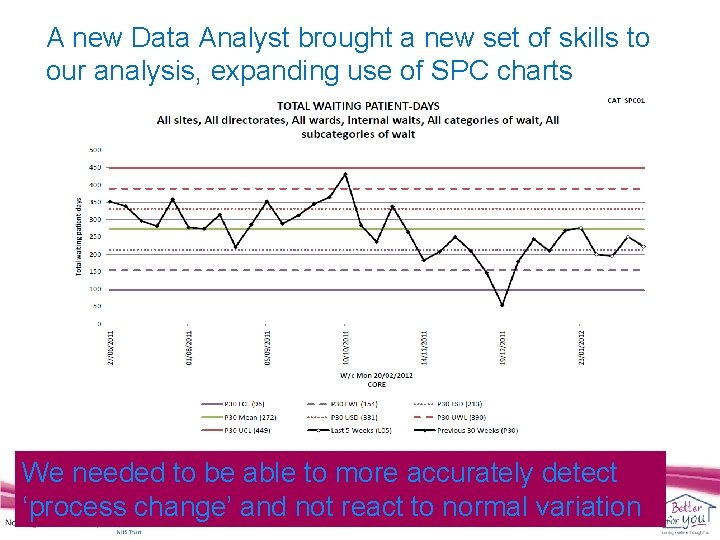
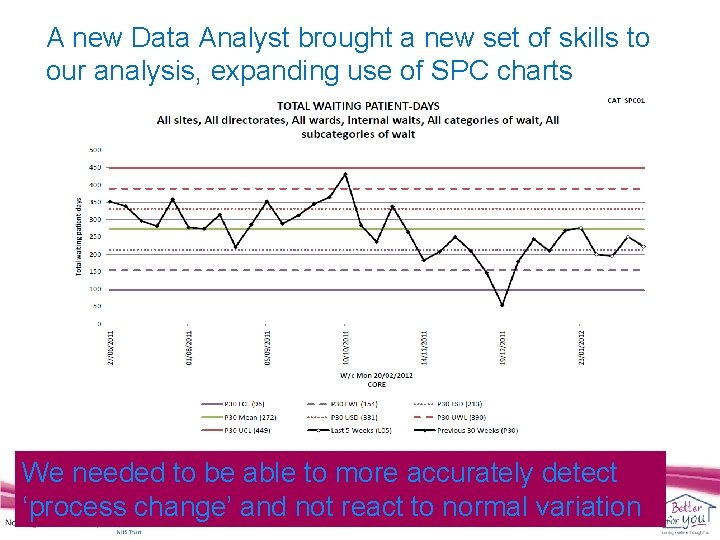
A new Data Analyst brought a new set of skills to our analysis, expanding use of SPC charts We needed to be able to more accurately detect ‘process change’ and not react to normal variation
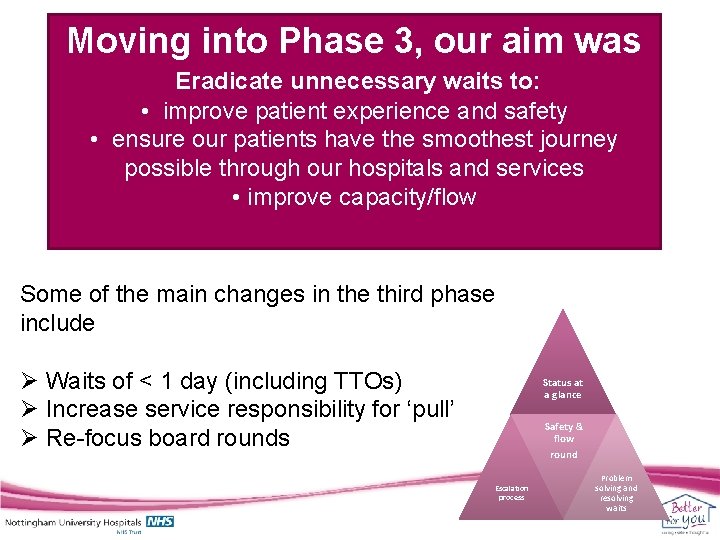
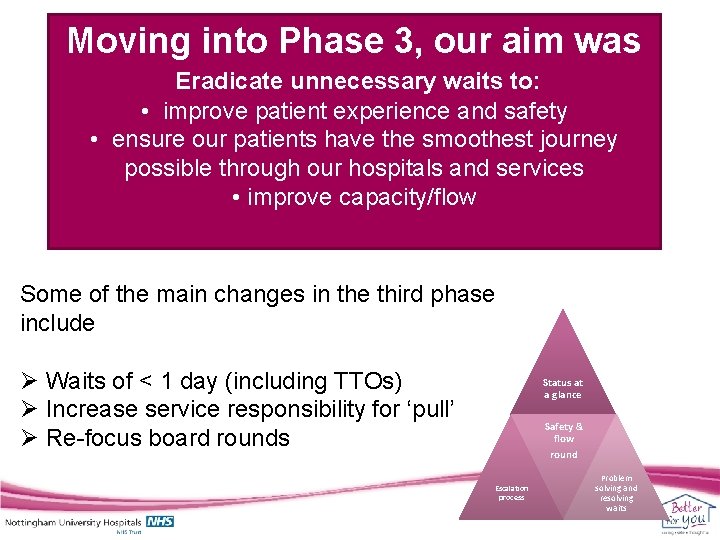
Moving into Phase 3, our aim was Eradicate unnecessary waits to: • improve patient experience and safety • ensure our patients have the smoothest journey possible through our hospitals and services • improve capacity/flow Some of the main changes in the third phase include Ø Waits of < 1 day (including TTOs) Ø Increase service responsibility for ‘pull’ Ø Re-focus board rounds Status at a glance Safety & flow round Escalation process Problem solving and resolving waits
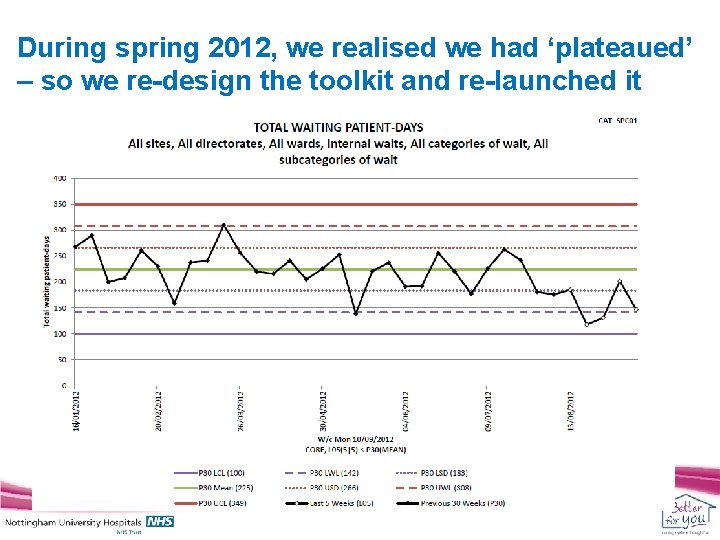
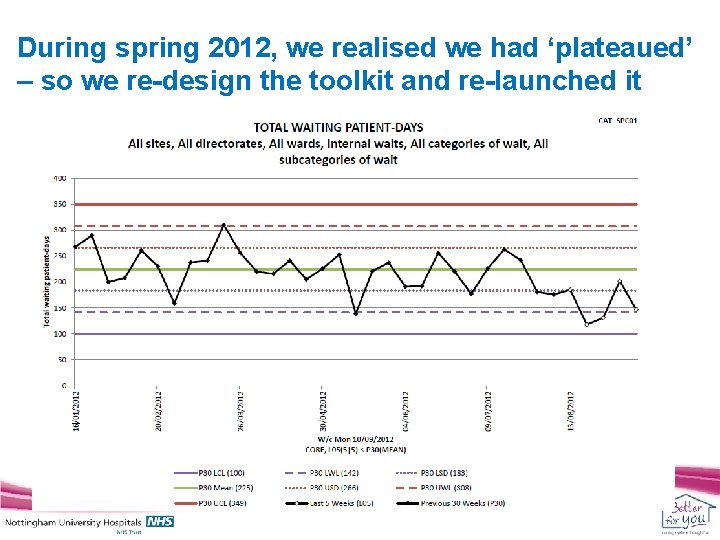
During spring 2012, we realised we had ‘plateaued’ – so we re-design the toolkit and re-launched it
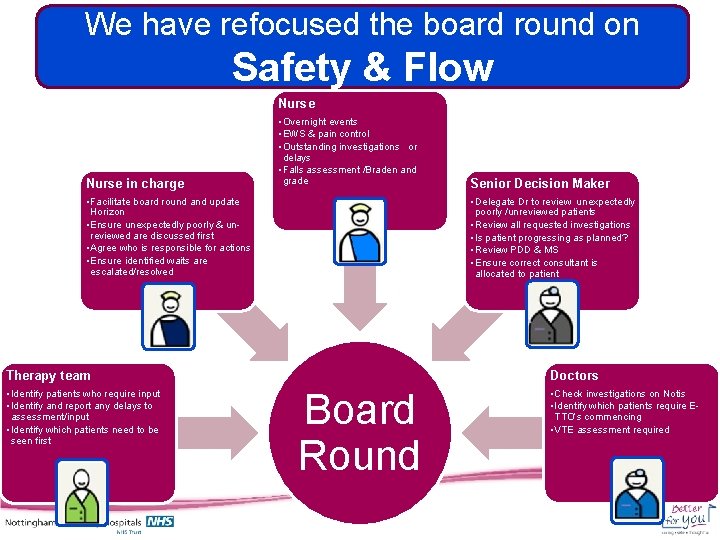
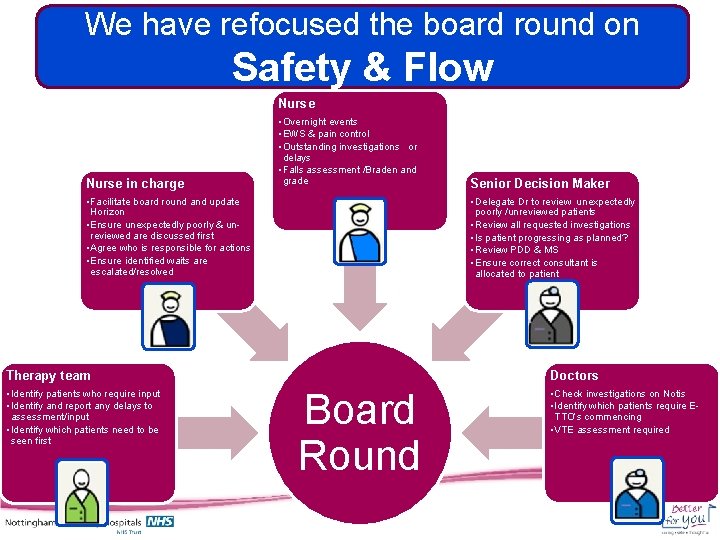
We have refocused the board round on Safety & Flow Nurse in charge • Overnight events • EWS & pain control • Outstanding investigations or delays • Falls assessment /Braden and grade • Facilitate board round and update Horizon • Ensure unexpectedly poorly & unreviewed are discussed first • Agree who is responsible for actions • Ensure identified waits are escalated/resolved • Delegate Dr to review unexpectedly poorly /unreviewed patients • Review all requested investigations • Is patient progressing as planned? • Review PDD & MS • Ensure correct consultant is allocated to patient Therapy team • Identify patients who require input • Identify and report any delays to assessment/input • Identify which patients need to be seen first Senior Decision Maker Doctors Board Round • Check investigations on Notis • Identify which patients require ETTO’s commencing • VTE assessment required
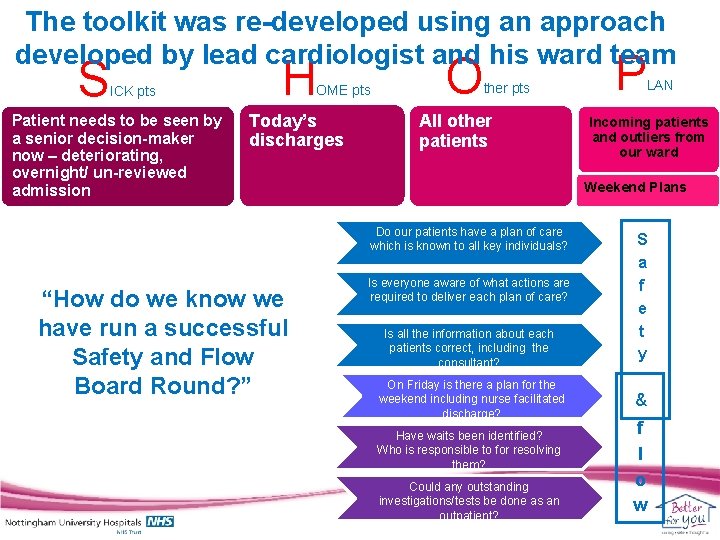
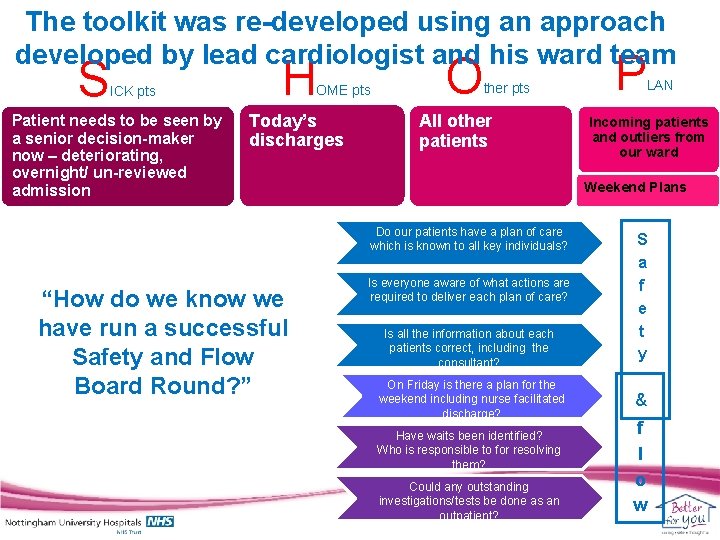
The toolkit was re-developed using an approach developed by lead cardiologist and his ward team S ICK pts Patient needs to be seen by a senior decision-maker now – deteriorating, overnight/ un-reviewed admission H OME pts Today’s discharges O ther pts All other patients LAN Incoming patients and outliers from our ward Weekend Plans Do our patients have a plan of care which is known to all key individuals? “How do we know we have run a successful Safety and Flow Board Round? ” P Is everyone aware of what actions are required to deliver each plan of care? Is all the information about each patients correct, including the consultant? On Friday is there a plan for the weekend including nurse facilitated discharge? Have waits been identified? Who is responsible to for resolving them? Could any outstanding investigations/tests be done as an outpatient? S a f e t y & f l o w
We have improved and expanded data analysis By Directorate By Ward By Service
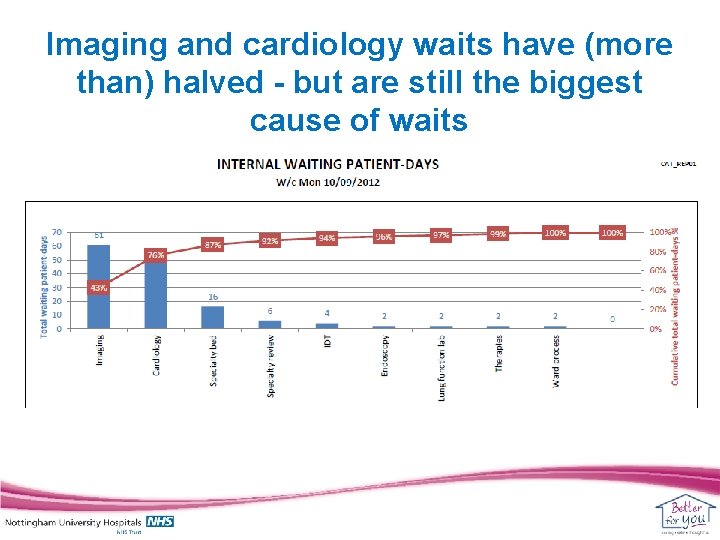
Imaging and cardiology waits have (more than) halved - but are still the biggest cause of waits
Our Current Challenges! • Reduce the number of internal waits by a further 20% in six months • Harness the opportunities of our new electronic bed management system • Waits measured in hours not days • Escalation plans for the top 5 services • Electronic data collection • Integrate Internal Waits ‘processes’ to daily capacity/flow meetings
Some reflections (or “what we would do differently if we could”!)
It was (and is) tough To get started. . . To create the drive for change. . . To get enough of the ‘right’ people involved and actually helping. . . Getting the cultural change from the bottom up. . .
But it has made a huge difference • It’s part of ‘our’ language now • Board rounds are an accepted part of everyday life (doesn’t mean they always happen though!) • Some wards have taken to the concept well and easily, others. . • Most of our services have responded very positively and pro-actively to reducing waiting times
What would we do differently? • Get matrons much more actively involved from the start – Including training & rollout • Get better and quicker feedback for wards regarding their performance • More medical staff involvement throughout • Integrate into everyday systems more quickly • Manage poor performers more robustly • Early involvement from services – creating the pull

Questions? Thoughts? Comments? Liz Williamson: liz. williamson@nuh. nhs. uk Scott Purser: scott. purser@nuh. nhs. uk 7
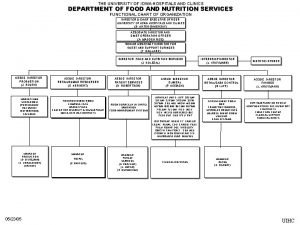
 University of iowa hospitals and clinics
University of iowa hospitals and clinics University hospitals coventry and warwickshire nhs trust
University hospitals coventry and warwickshire nhs trust Dr sue carr
Dr sue carr Bial's test reagent
Bial's test reagent Fates of glucose
Fates of glucose Osazone test diagram
Osazone test diagram Reducing vs. non-reducing sugars
Reducing vs. non-reducing sugars University of nottingham parking
University of nottingham parking University of nottingham
University of nottingham In this scheme cpu execution waits while i/o proceeds.
In this scheme cpu execution waits while i/o proceeds. God sees the truth but waits rising action
God sees the truth but waits rising action Free buffer waits
Free buffer waits Tide waits for no man
Tide waits for no man Victory waits on your fingers poster meaning
Victory waits on your fingers poster meaning The man who waits
The man who waits What does beowulf do before he swims back to land?
What does beowulf do before he swims back to land? Aldot access management manual
Aldot access management manual Difference between voluntary and mandatory
Difference between voluntary and mandatory Portsmouth trust values
Portsmouth trust values Health standards louisiana
Health standards louisiana Jci standards
Jci standards Afmsd mumbai
Afmsd mumbai What are the uses of computer in hospital
What are the uses of computer in hospital Niaho standards
Niaho standards Bcp for hospitals
Bcp for hospitals Anchorage va medical center
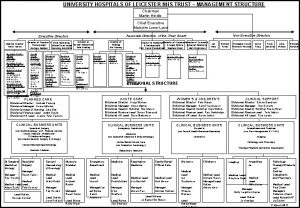
Anchorage va medical center Uhl management structure
Uhl management structure How to save pictures
How to save pictures Lean hospitals
Lean hospitals Lean hospitals mark graban
Lean hospitals mark graban Fhpl ecard
Fhpl ecard Erp for hospitals
Erp for hospitals Arogyakiranam
Arogyakiranam Bed management in hospitals
Bed management in hospitals Mghs wheelers
Mghs wheelers Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs National accreditation board for hospitals
National accreditation board for hospitals Lokmanya hospitals private limited
Lokmanya hospitals private limited Inventory cycle time
Inventory cycle time Process governance
Process governance Bethan williamson
Bethan williamson Williamson eter sentezi örnekleri
Williamson eter sentezi örnekleri Etoxiciclohexano
Etoxiciclohexano