Radiological Category Vascular and Interventional Radiology Principal Modality

- Slides: 20
Radiological Category: Vascular and Interventional Radiology Principal Modality (1): Fluroscopy Principal Modality (2): CT Case Report 0951 Submitted by: Lori Sedrak, D. O. Faculty reviewer: Jonathan Liaw, M. D. Date accepted: 15 January 2013

Case History • 36 year-old female presenting with massive (800 cc) hemoptysis requiring 4 units of p. RBCs. • Bronchoscopy shows massive hemorrhage with inability to identify source. • Interventional Radiology was consulted with CT of the chest obtained in-route to the angiography suite.
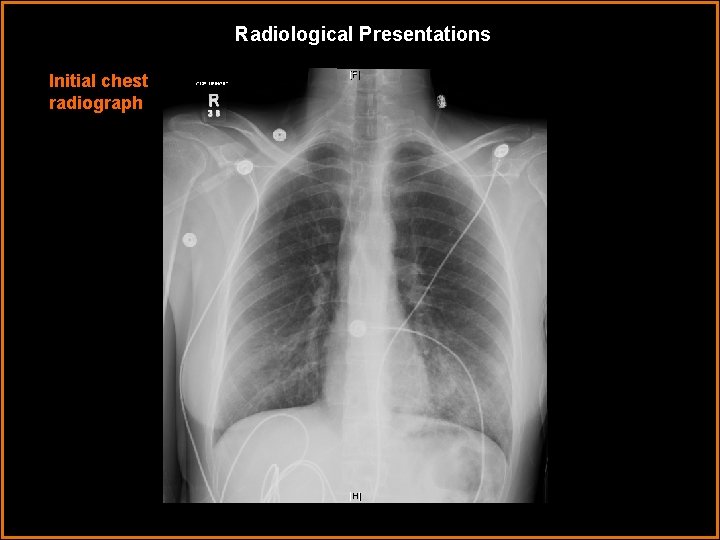
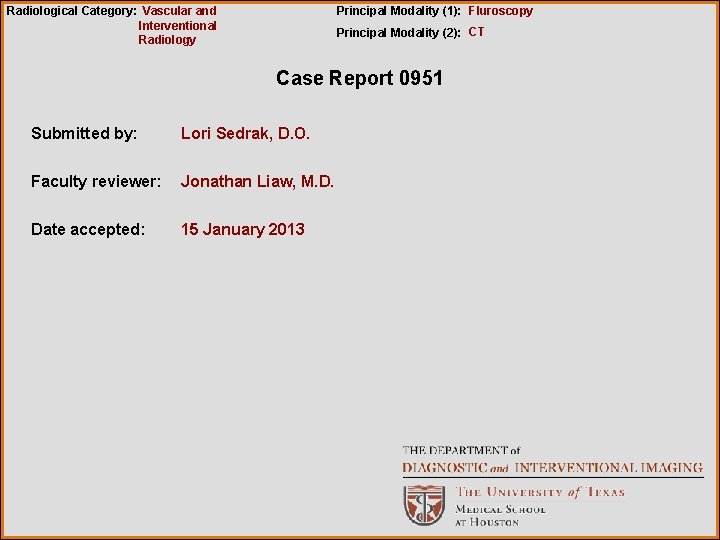
Radiological Presentations Initial chest radiograph
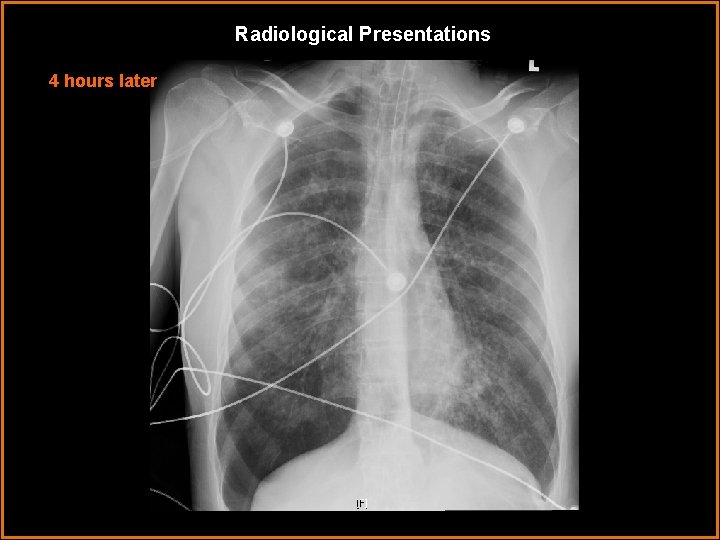
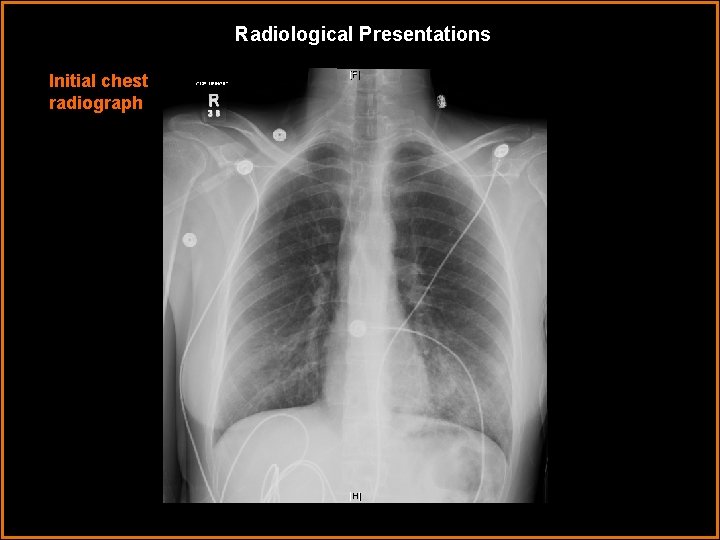
Radiological Presentations 4 hours later
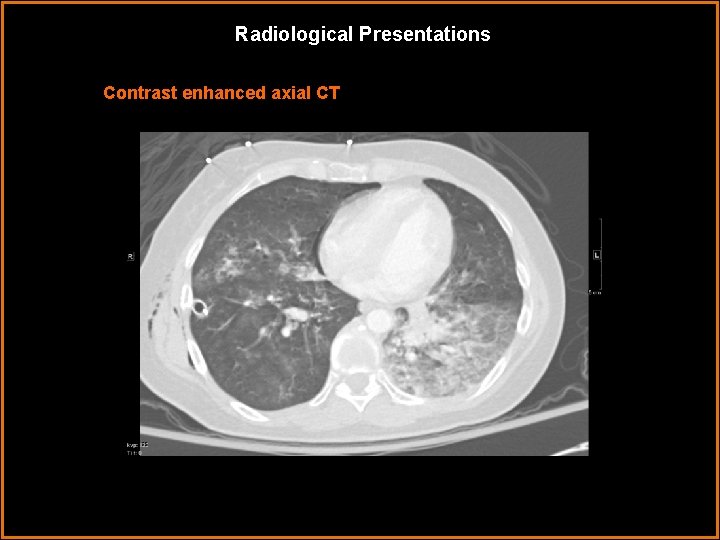
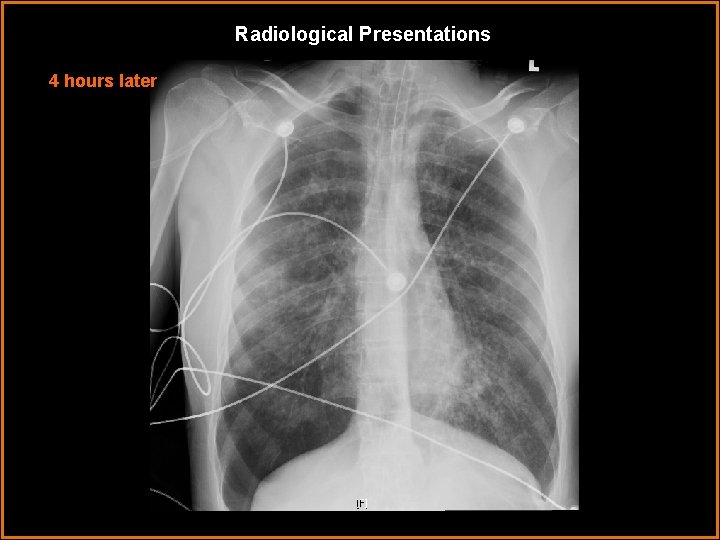
Radiological Presentations Contrast enhanced axial CT
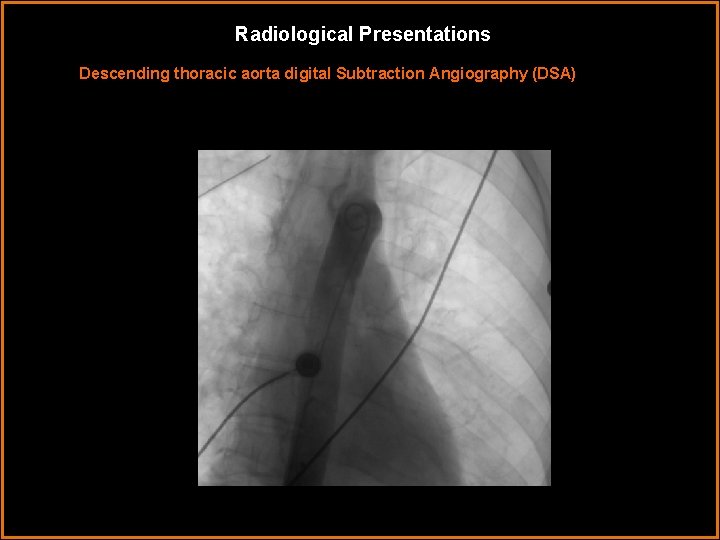
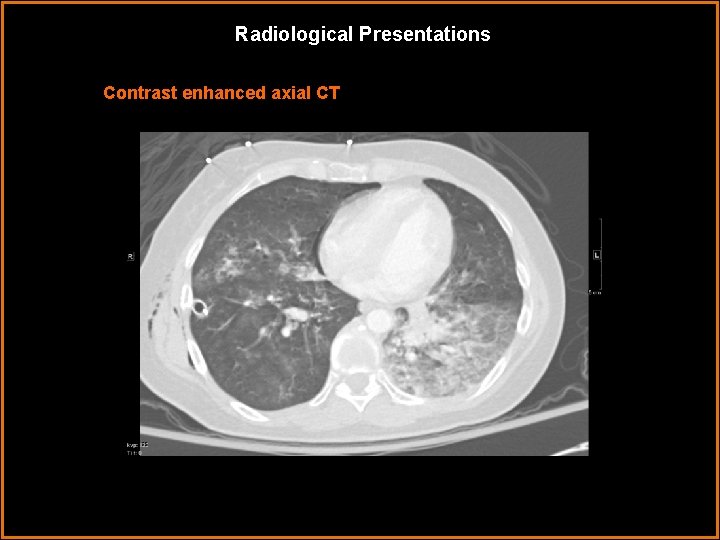
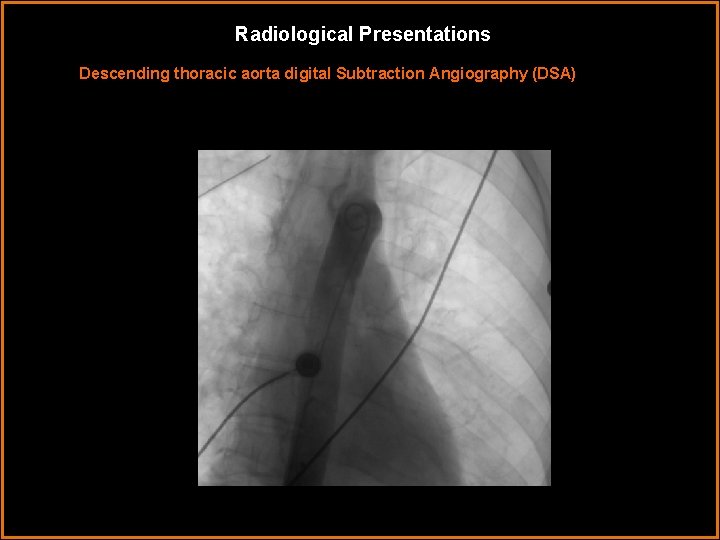
Radiological Presentations Descending thoracic aorta digital Subtraction Angiography (DSA)
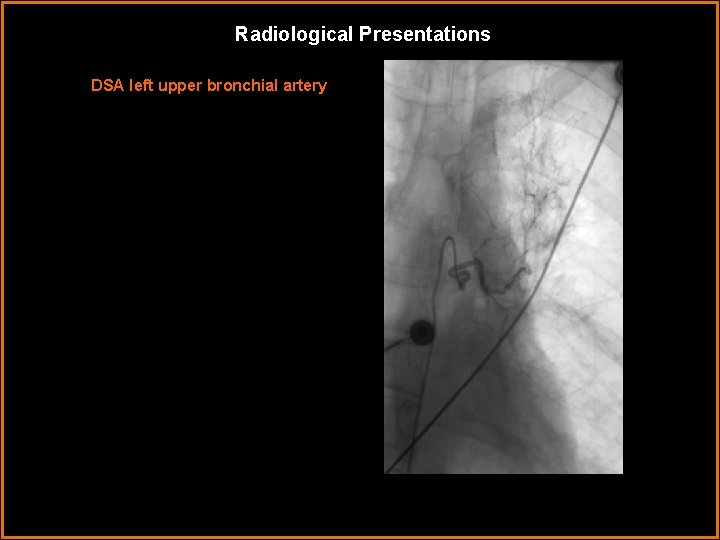
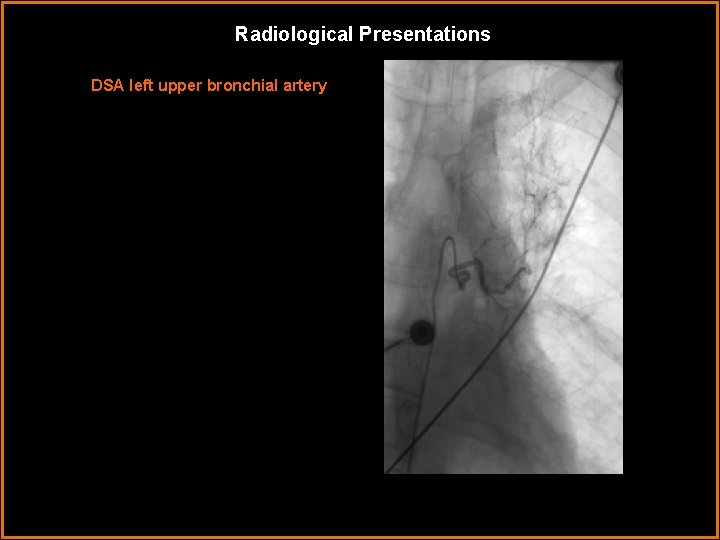
Radiological Presentations DSA left upper bronchial artery
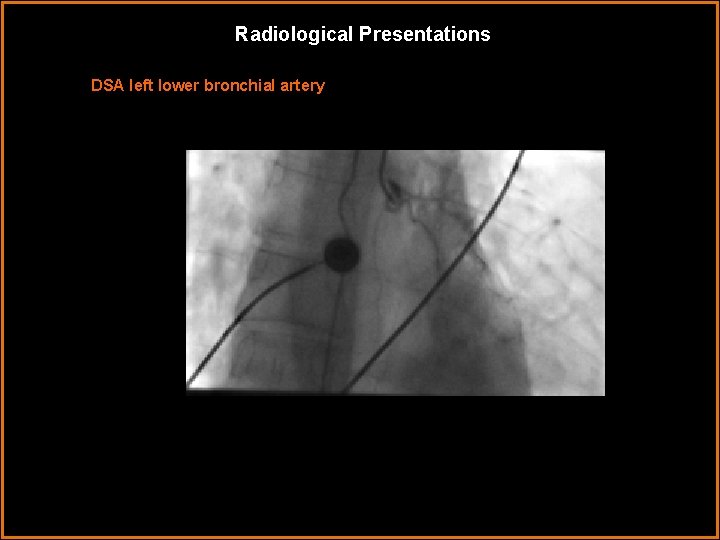
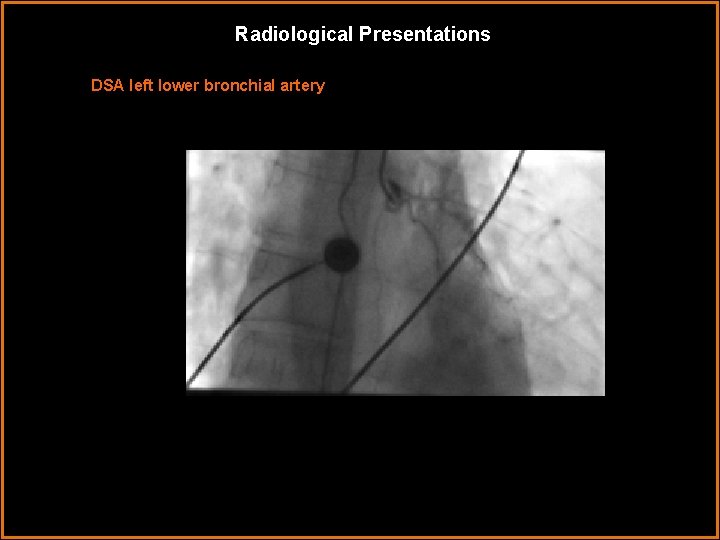
Radiological Presentations DSA left lower bronchial artery
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Traumatic tension pneumothorax • Multifocal pneumonia • Pulmonary Hemorrhage • Primary pulmonary malignancy
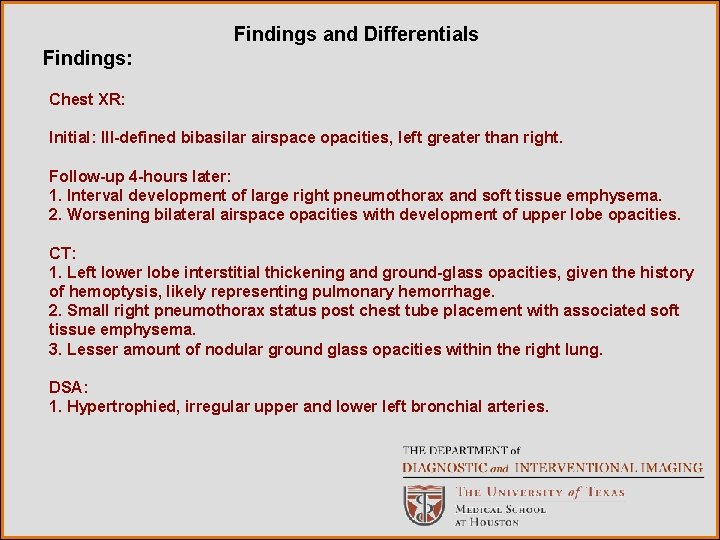
Findings and Differentials Findings: Chest XR: Initial: Ill-defined bibasilar airspace opacities, left greater than right. Follow-up 4 -hours later: 1. Interval development of large right pneumothorax and soft tissue emphysema. 2. Worsening bilateral airspace opacities with development of upper lobe opacities. CT: 1. Left lower lobe interstitial thickening and ground-glass opacities, given the history of hemoptysis, likely representing pulmonary hemorrhage. 2. Small right pneumothorax status post chest tube placement with associated soft tissue emphysema. 3. Lesser amount of nodular ground glass opacities within the right lung. DSA: 1. Hypertrophied, irregular upper and lower left bronchial arteries.
Differentials • Traumatic tension pneumothorax • Multifocal pneumonia • Pulmonary Hemorrhage • Primary pulmonary malignancy
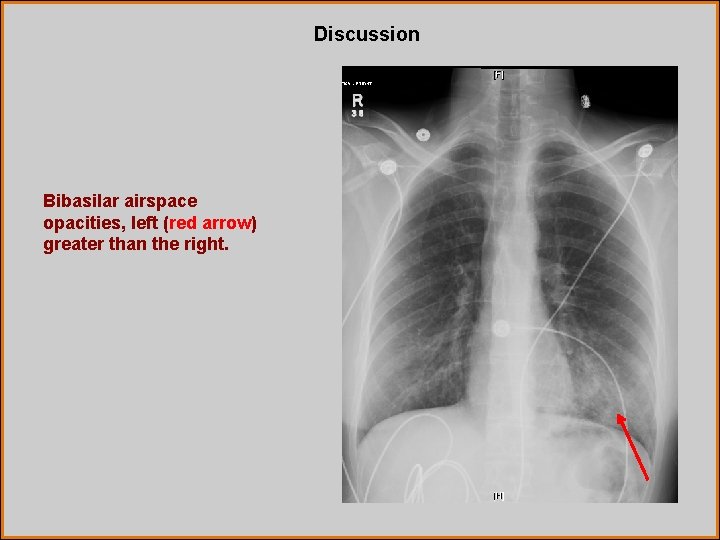
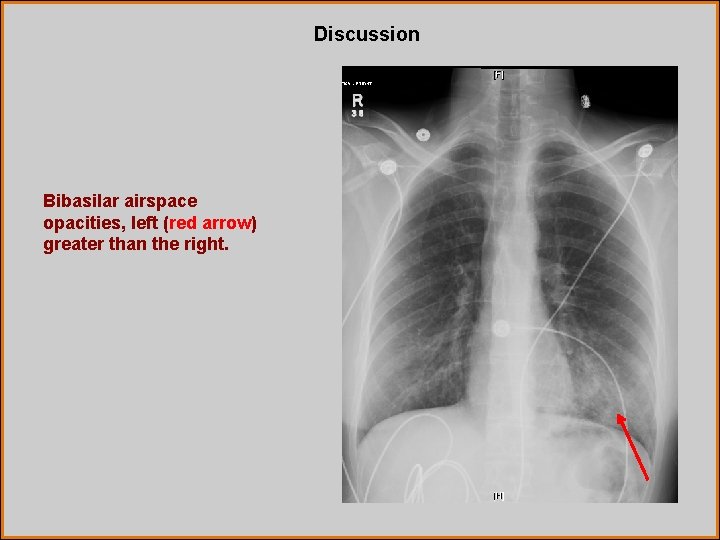
Discussion Bibasilar airspace opacities, left (red arrow) greater than the right.
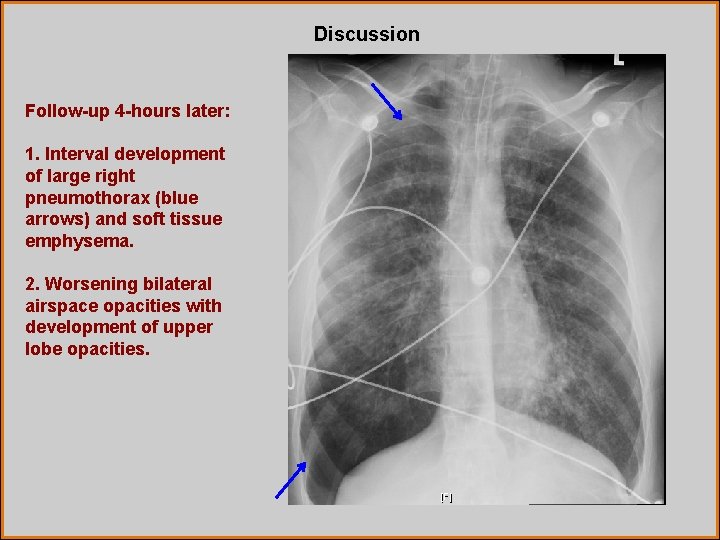
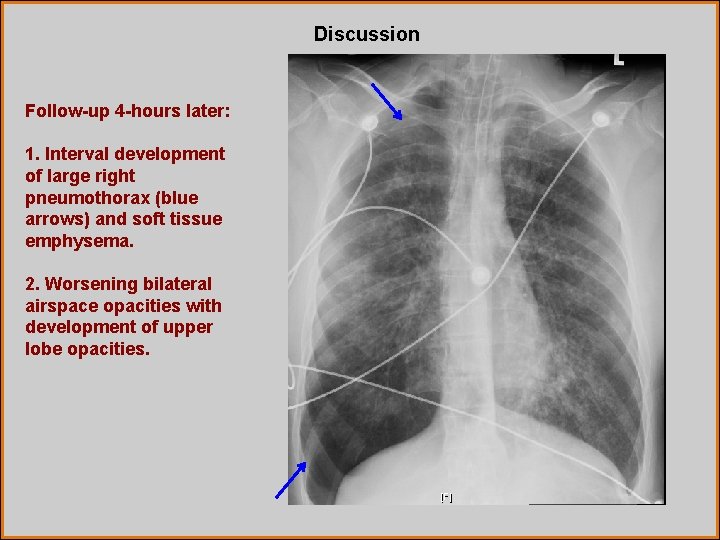
Discussion Follow-up 4 -hours later: 1. Interval development of large right pneumothorax (blue arrows) and soft tissue emphysema. 2. Worsening bilateral airspace opacities with development of upper lobe opacities.
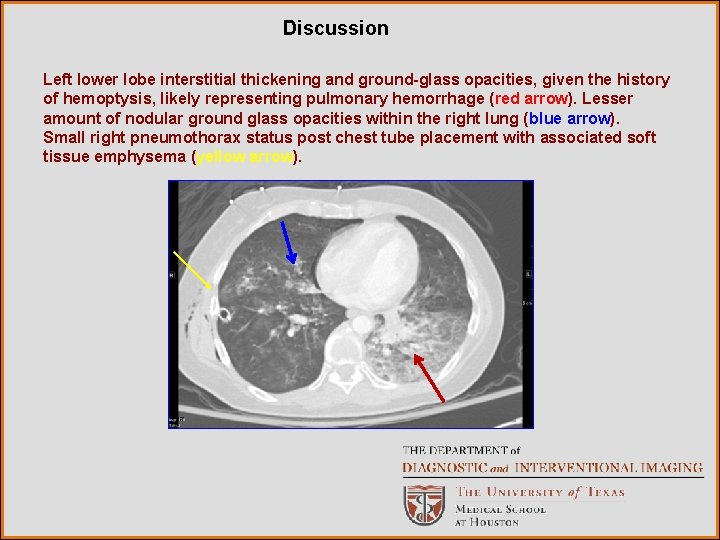
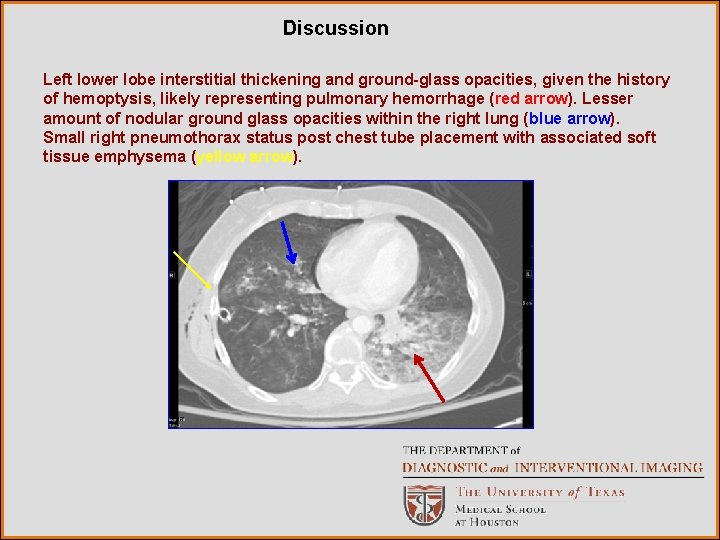
Discussion Left lower lobe interstitial thickening and ground-glass opacities, given the history of hemoptysis, likely representing pulmonary hemorrhage (red arrow). Lesser amount of nodular ground glass opacities within the right lung (blue arrow). Small right pneumothorax status post chest tube placement with associated soft tissue emphysema (yellow arrow).
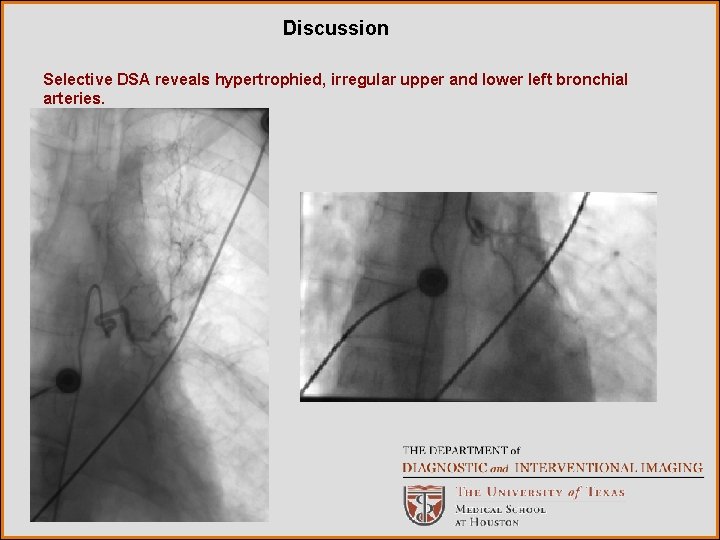
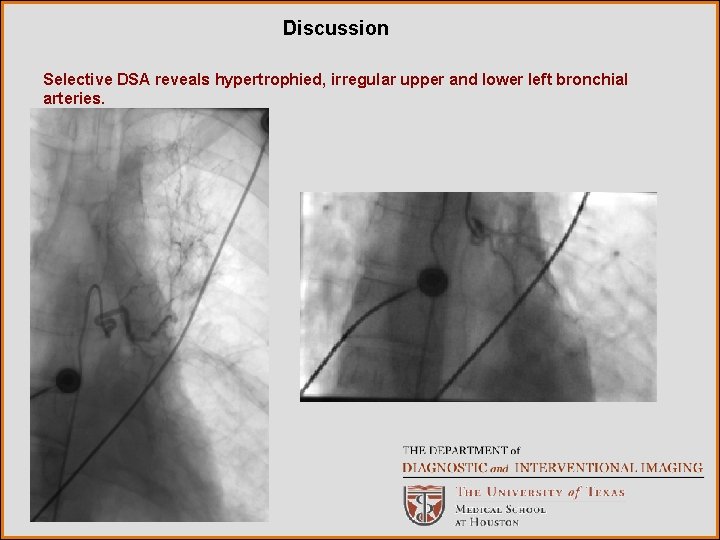
Discussion Selective DSA reveals hypertrophied, irregular upper and lower left bronchial arteries.
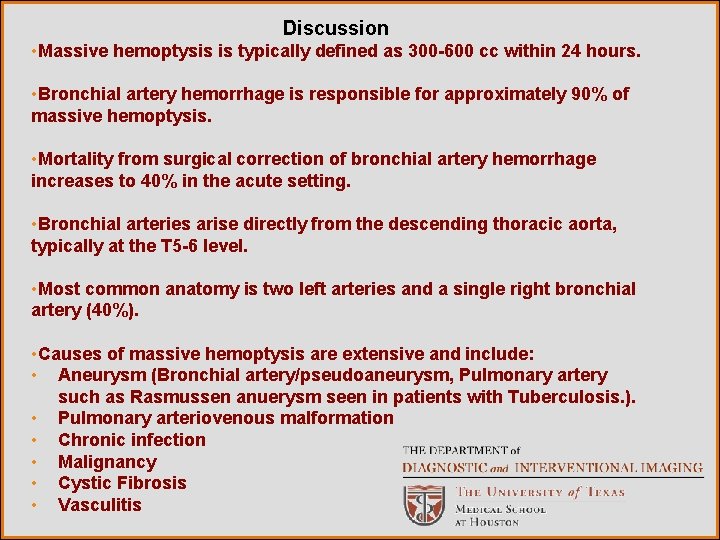
Discussion • Massive hemoptysis is typically defined as 300 -600 cc within 24 hours. • Bronchial artery hemorrhage is responsible for approximately 90% of massive hemoptysis. • Mortality from surgical correction of bronchial artery hemorrhage increases to 40% in the acute setting. • Bronchial arteries arise directly from the descending thoracic aorta, typically at the T 5 -6 level. • Most common anatomy is two left arteries and a single right bronchial artery (40%). • Causes of massive hemoptysis are extensive and include: • Aneurysm (Bronchial artery/pseudoaneurysm, Pulmonary artery such as Rasmussen anuerysm seen in patients with Tuberculosis. ). • Pulmonary arteriovenous malformation • Chronic infection • Malignancy • Cystic Fibrosis • Vasculitis
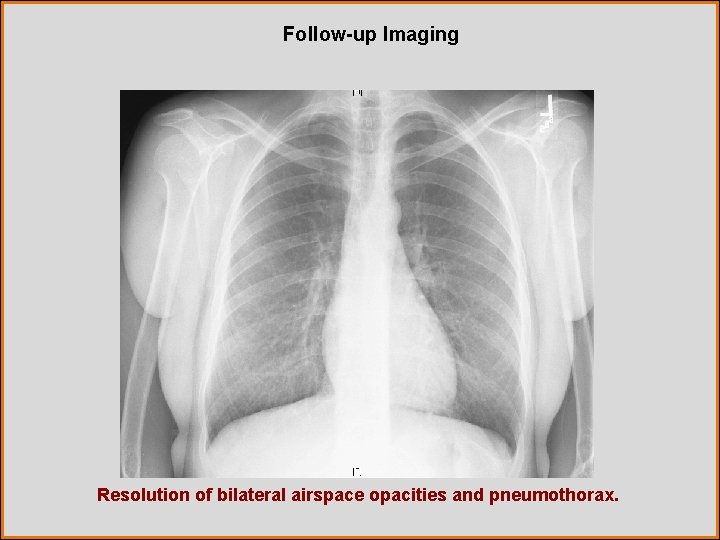
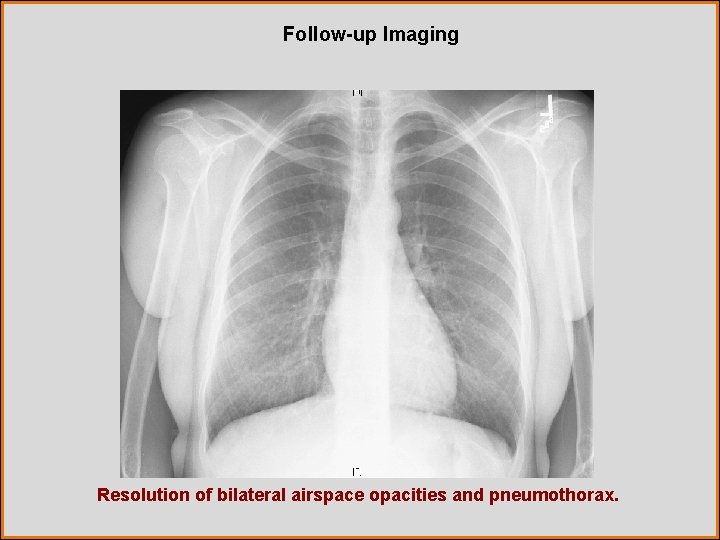
Follow-up Imaging Resolution of bilateral airspace opacities and pneumothorax.
Discussion Procedure: Initial descending thoracic angiogram. Then typically cobra-curved catheters are used to select abnormal bronchial arteries. Microcatheter placement, if feasible, provides catheter stabilization beyond origin of spinal cord braches. Complications to be aware of: Anterior spinal artery (Artery of Adamkiewicz) which has a characteristic “hairpin” configuration. Polyvinyl alcohol (PVA) particles 350 -500 μm are most frequently used worldwide. Commonly prevent recannulization and hemoptysis seen with abdorbable gelatin sponge such as gelfoam. Avoid coils due to proximal occlusion and inability to repeat embolization if needed. Liquid embolic agents should also be avoided due to distal tissue necrosis.
Diagnosis Gram negative rods cultured on bronchoscopy, consistent with pneumonia and clinical concern for vasculitis, such as polyarteritis nodosa (PAN).
References 1. Yoon W, Kim JK, Kim YH, Chung TW, and Kang HK. Bronchial and Nonbronchial Systemic Artery Embolization for Life-threatening Hemoptysis. Radio. Graphics. 2002; 22, 1395 -1409. 2. Fernando HC, Stein M, Benfield JR, Link DP. Role of bronchial artery embolization in the management of hemoptysis. Arch Surg 1998; 133: 862 -866. 3. Statdx. com