Radiological Category Interventional Radiology Principal Modality 1 Computed
- Slides: 12
Radiological Category: Interventional Radiology Principal Modality (1): Computed Tomography Principal Modality (2): None Case Report # 767 Submitted by: Lee Myers, M. D. Faculty reviewer: Kenneth Bryant, M. D. , Ph. D. , The University of Texas Medical School at Houston Date accepted: 13 February, 2011
Case History 44 year old male with history of pancreatic cancer with intractable abdominal pain. A procedure was requested to alleviate the patient’s pain and was performed by Interventional radiology.
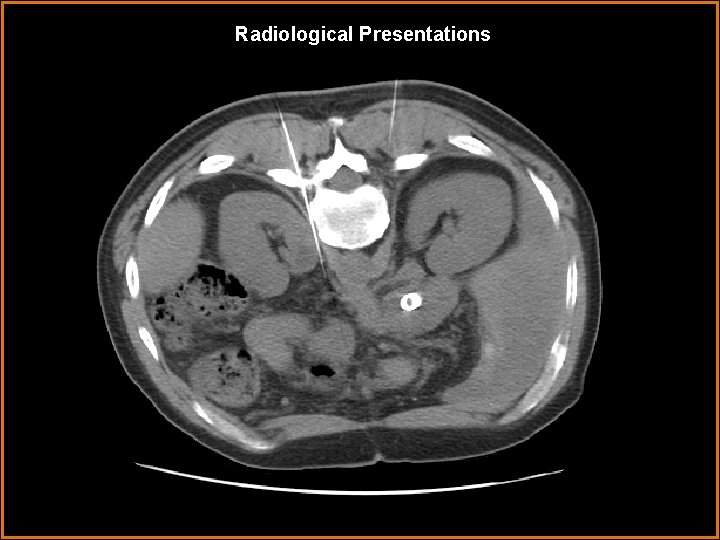
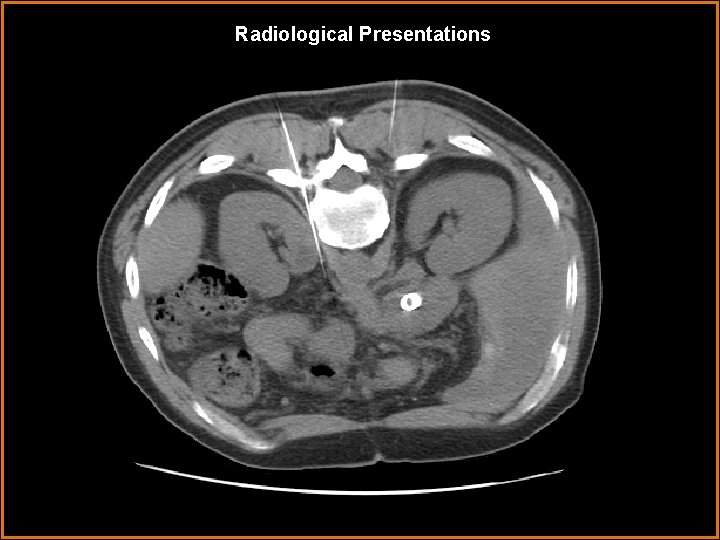
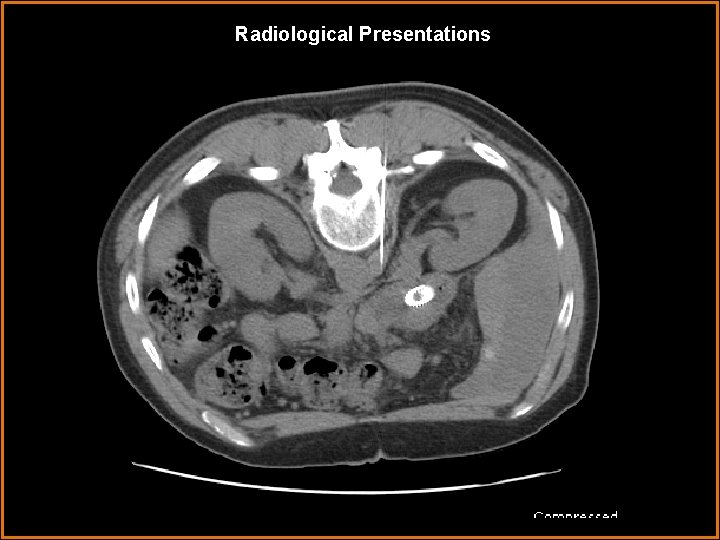
Radiological Presentations
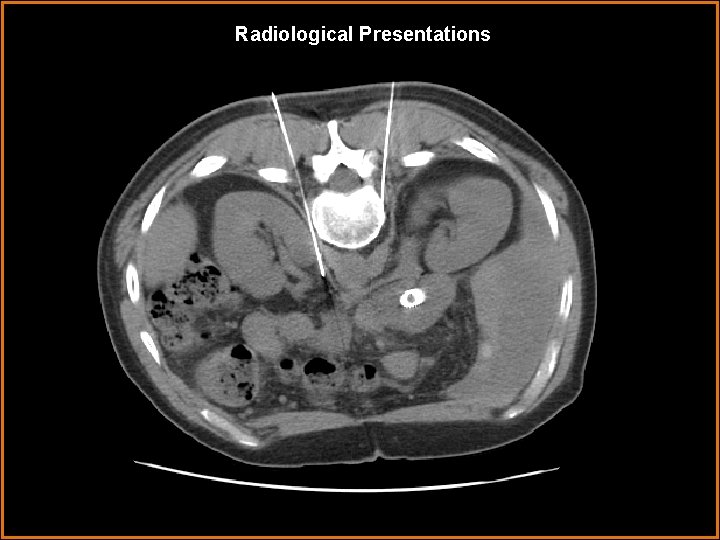
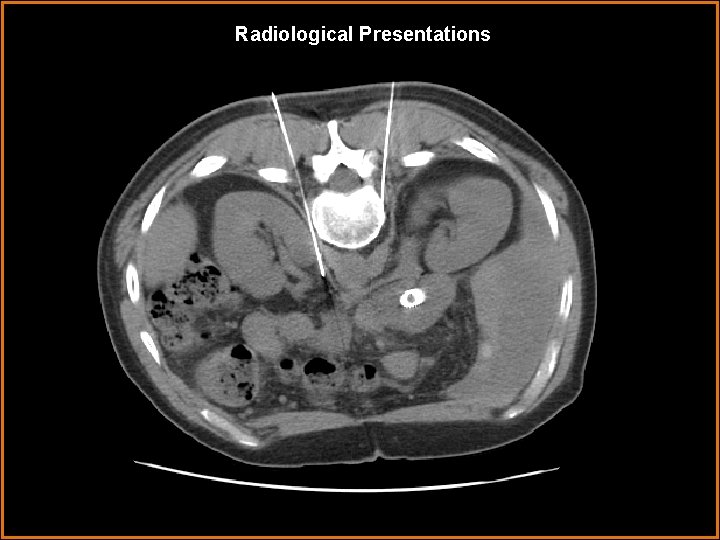
Radiological Presentations
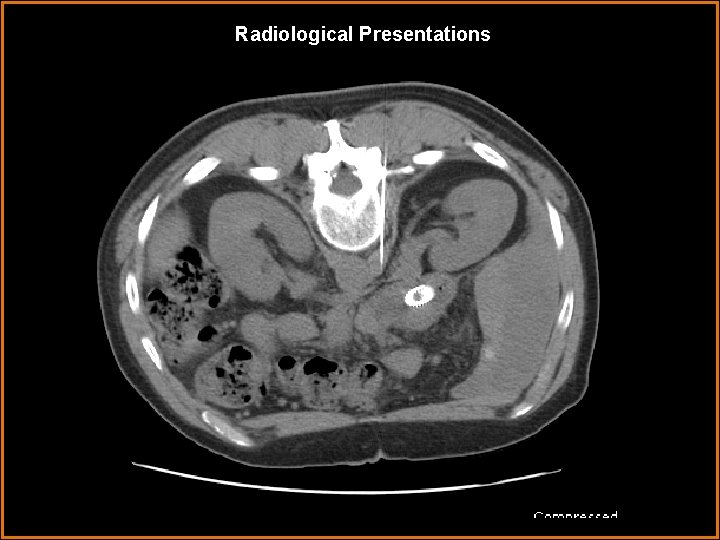
Radiological Presentations
Case History During the procedure the patient had relief of his abdominal pain. The next morning the patient was pain free.
Test Your Diagnosis Which one of the following is your choice for the procedure that was performed? After your selection, go to next page. • Removal of lymph nodes compressing on the adjacent nerves • Celiac plexus block • Biopsy of a mass
Findings and Differentials Findings: The CT images demonstrate two 20 gauge Chiba needles advanced into the region of the celiac ganglia bilaterally from a posterior approach. How is proper location confirmed? : • Inject 98% ethyl alcohol • Inject contrast • Inject lidocaine • CT resolution is adequate to confirm proper location
Discussion Patient selection for Celiac Plexus Block: 1. Severe, chronic visceral abdominal pain (pancreatic cancer, chronic pancreatitis, etc. ) 2. Celiac blocks are performed on patients with pain requiring narcotic analgesics, but fail to give complete relief. Procedure 1. Using CT guidance, two 20 gauge Chiba needles are advanced to the celiac plexus bilaterally from a posterior approach. 2. Confirm adequate location: Lidocaine or Marcaine is injected, which should diminish the patient’s pain almost instantly. Alternatively, a small amount of contrast can be injected to confirm location. 3. After location is confirmed, 16 - 25 m. L of 50% - 100% ethyl alcohol is injected into each needle to destroy the celiac nerves. Results 1. Ninety percent of patients have significant improvement 2. On average, the effect lasts 2 to 3 months and can be reblocked if needed.
Discussion Complications: 1. Hypotension – vasodilation of the splanchnic bed. 2. Intense abdominal pain may occur after injection of the alcohol for 3060 seconds. 3. Temporary increased bowel motility. 4. Paralysis, weakness, and nerve root pain have been described in the literature.
Diagnosis Intractable pain relieved by a celiac plexus block procedure.
References Lieberman RP, Lieberman SL, et al. “Celiac Plexus and Splanchnic Nerve Block”. Seminars in Interventional Radiology. Volume 5, Number 3. September 1988. Miller JC. “Image-Guided Pain Management, Part 1: Celiac Plexus Block for Palliative Pain Relief”. Radiology Rounds, Volume 5, Issue 9. September 2007