Radiological Category Genitourinary Principal Modality Ultrasound Principal Modality





- Slides: 22
Radiological Category: Genitourinary Principal Modality: Ultrasound Principal Modality: None Case Report #0625 Submitted by: Joshua Franklin , M. D. Faculty reviewer: Verghese George, M. D. Date accepted: 28 April 2009
Case History A 26 year old female presents to the ER with nausea, vomiting, decreased oral intake and shortness of breath for the past 2 days. She also complains of increasing abdominal pain and bloating over the past week. No fever or chills. - The patient recently began treatment for a condition, the details of the same are concealed for this case. - Her physical exam is unremarkable except for diffuse abdominal tenderness and abdominal distention. - Pertinent labs: Urine Pregnancy Test: Negative WBC 21. 8 Hemoglobin 18. 3 Creatinine 1. 1 Hematocrit 54

Radiological Presentations Figure 1: Longitudinal U/S image of the RUQL
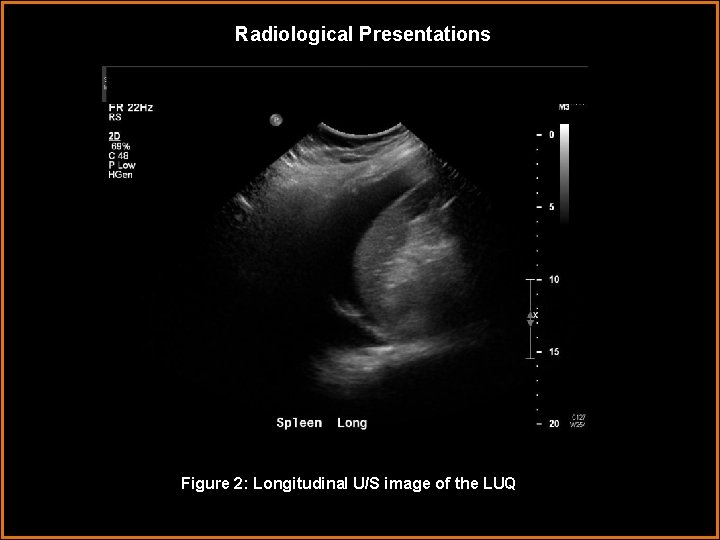
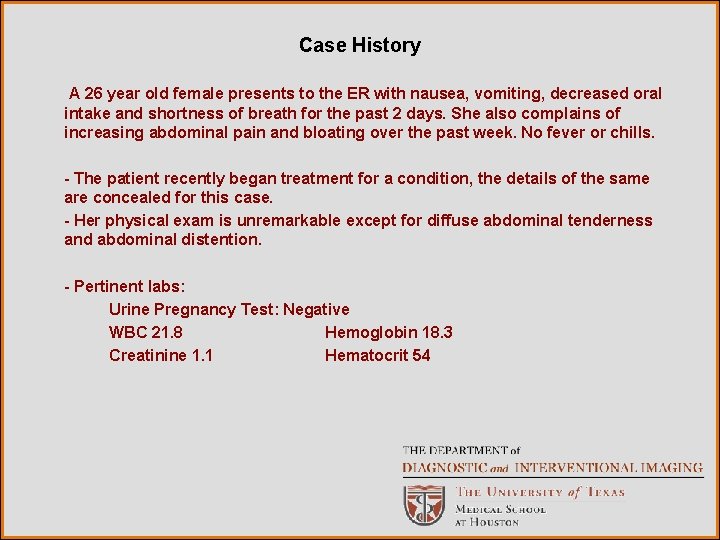
Radiological Presentations Figure 2: Longitudinal U/S image of the LUQL
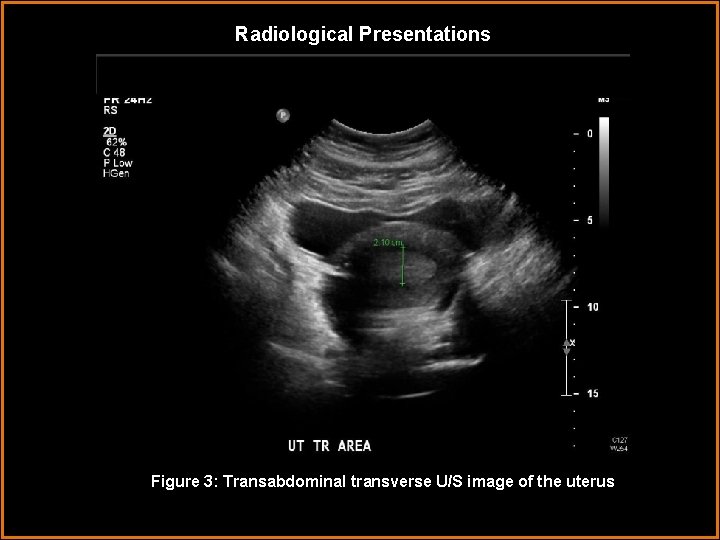
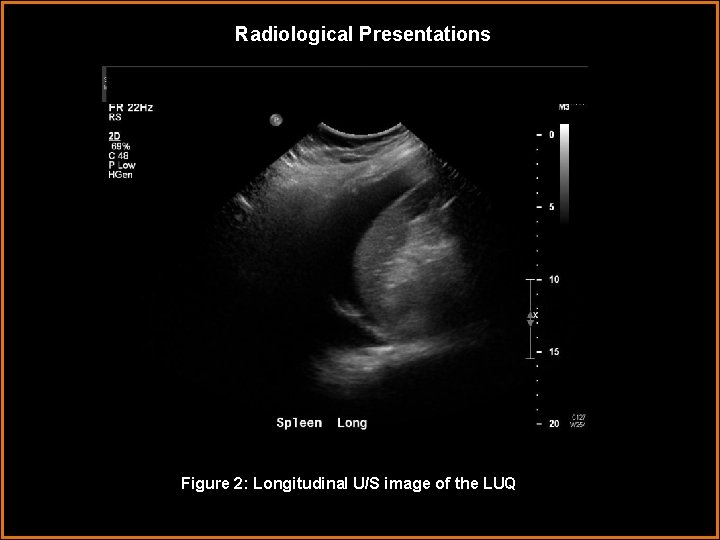
Radiological Presentations Figure 3: Transabdominal transverse U/S image of the uterus
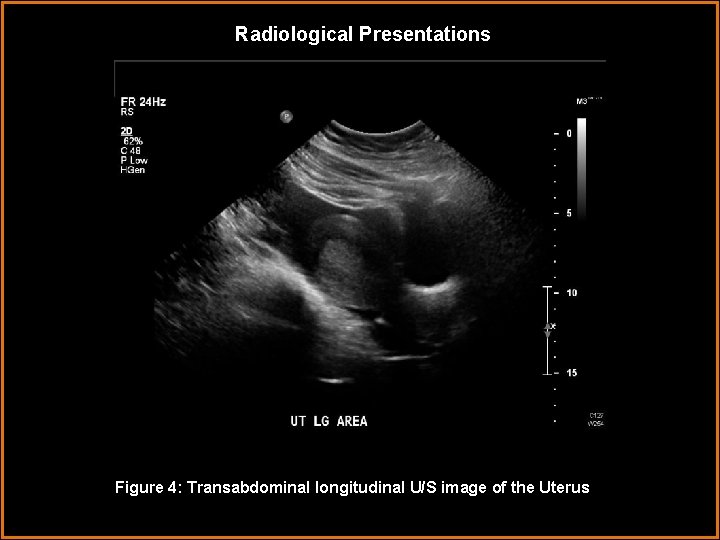
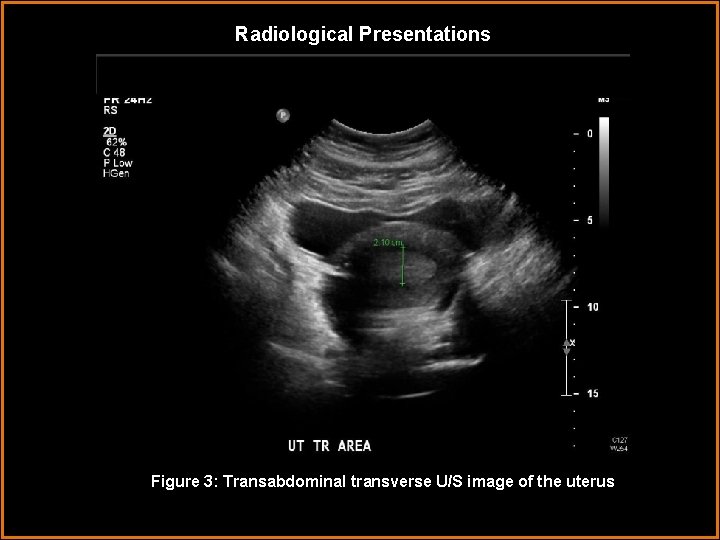
Radiological Presentations Figure 4: Transabdominal longitudinal U/S image of the Uterus
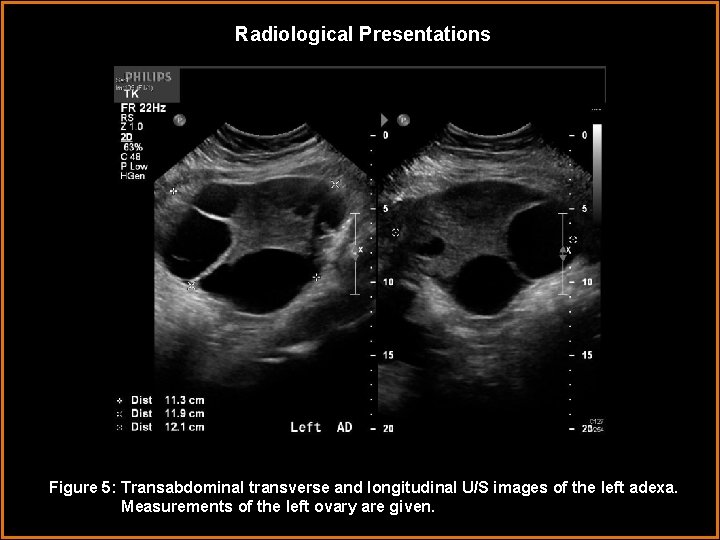
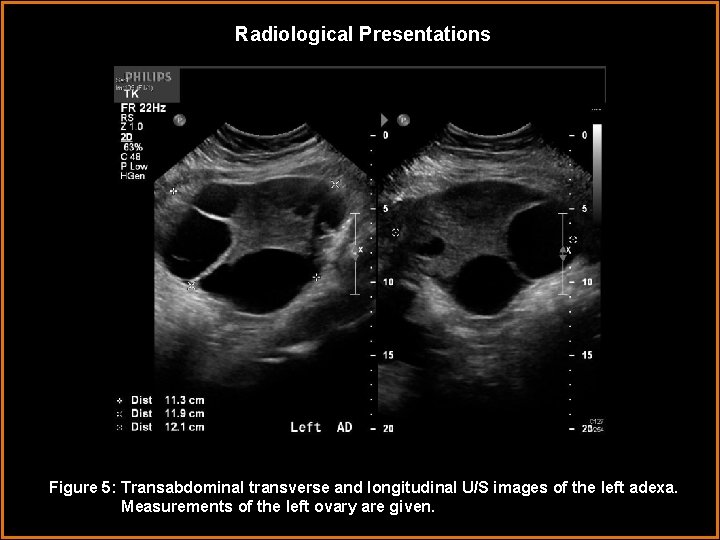
Radiological Presentations Figure 5: Transabdominal transverse and longitudinal U/S images of the left adexa. Measurements of the left ovary are given.
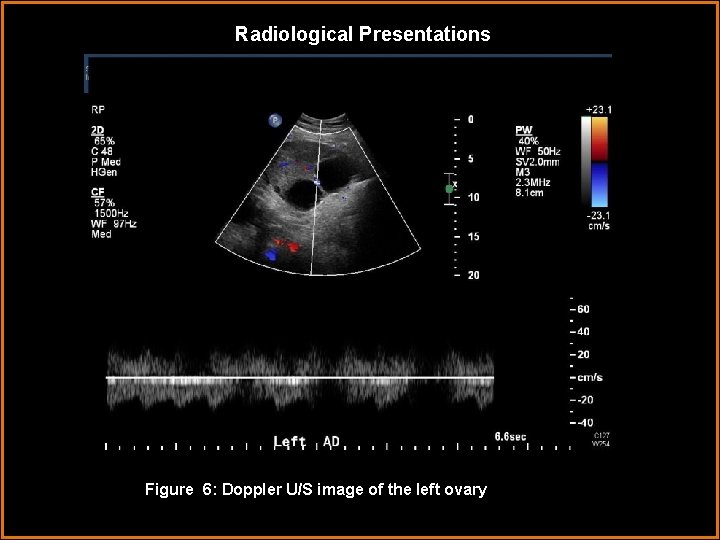
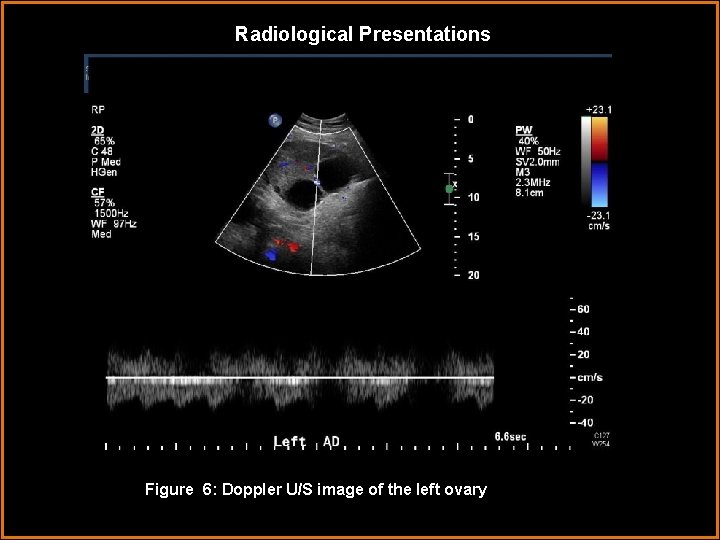
Radiological Presentations Figure 6: Doppler U/S image of the left ovary. L
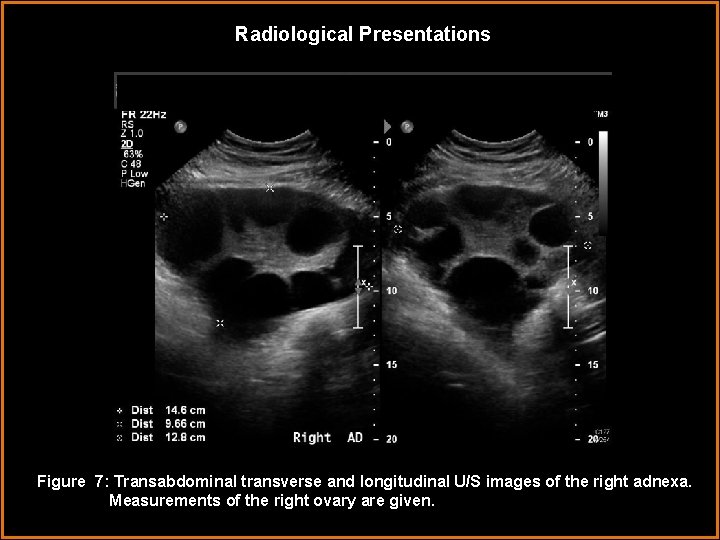
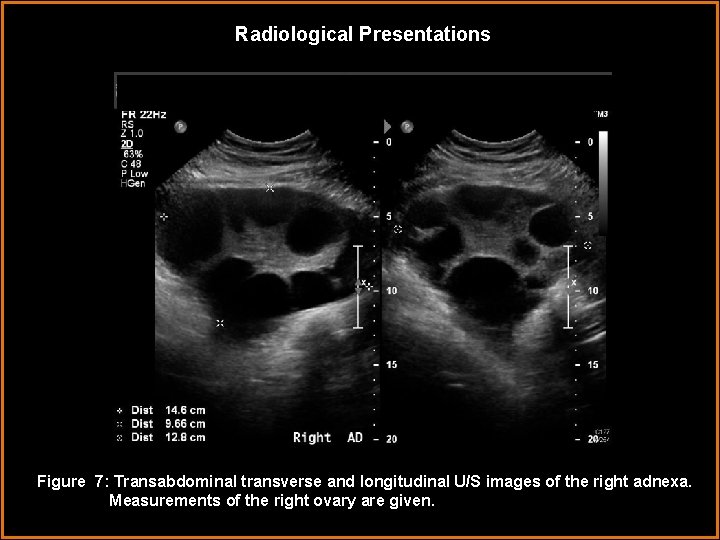
Radiological Presentations Figure 7: Transabdominal transverse and longitudinal U/S images of the right adnexa. Measurements of the right ovary are given.

Radiological Presentations Figure 8: Doppler U/S image of the right ovary.
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Ovarian Torsion • Polycystic Ovaries • Primary Ovarian Malignancy • Pelvic Inflammatory Disease • Metastatic Disease involving the ovaries • None of the above
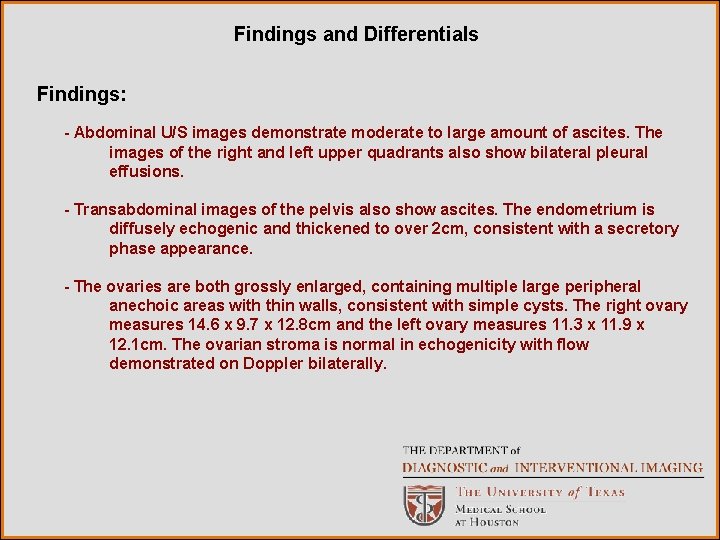
Findings and Differentials Findings: - Abdominal U/S images demonstrate moderate to large amount of ascites. The images of the right and left upper quadrants also show bilateral pleural effusions. - Transabdominal images of the pelvis also show ascites. The endometrium is diffusely echogenic and thickened to over 2 cm, consistent with a secretory phase appearance. - The ovaries are both grossly enlarged, containing multiple large peripheral anechoic areas with thin walls, consistent with simple cysts. The right ovary measures 14. 6 x 9. 7 x 12. 8 cm and the left ovary measures 11. 3 x 11. 9 x 12. 1 cm. The ovarian stroma is normal in echogenicity with flow demonstrated on Doppler bilaterally.
Findings and Differentials: • Ovarian hyperstimulation syndrome • Polycystic ovary syndrome • Ovarian Torsion • Primary ovarian malignancy • Metastatic Disease
Discussion The combination of ascites, pleural effusions, and symmetrically enlarged ovaries containing peripherally arranged cysts is highly suggestive of ovarian hyperstimulation syndrome, and a history of fertility treatment with gonadotropins should be sought for. Indeed, in this case, the patient had a 6 year history of infertility for which she had recently commenced treatment. Unlikely considerations in the differential include polycystic ovary syndrome and cystic ovarian neoplasia. Although the entire constellation of findings is not consistent with torsion alone, ovarian torsion should always be considered in a patient with enlarged ovaries and pelvic pain. Ovarian hyperstimulation syndrome (OHSS) is an exaggerated response to ovulation induction therapy. It is most commonly associated with administration of exogenous gonadotropins, and only rarely with administration of other fertility drugs such as clomiphene or gonadotropin releasing hormone 1. Multiple follicles enlarge as they are stimulated to develop by the administration of gonadotropins. The large peripheral cysts in this represent the stimulated follicles – a hyperstimulated ovary is essentially an “Aunt Minnie”. Ovulation is then induced, usually by administration of h. CG at mid-cycle. History of ovulation induction is important, as OHSS develops only if ovulation is induced 3.

Discussion Risk factors for development of OHSS include young age, low body weight, polycystic ovary syndrome, high doses of exogenous gonadotropins, high or rapidly rising estradiol levels, and previous episodes of OHSS 1. The hallmark of the pathophysiology of OHSS is an increase in capillary permeability, resulting in third spacing of fluid from the intravascular space. Several factors produced by the developing follicles are implicated as having a role in the increased vascular permeability including prorenin and renin, multiple cytokines, and vascular endothelial growth factor (VEGF)1, 3. Many of the clinical symptoms of OHSS are related to the increased vascular permeability. Abdominal distention and discomfort results from ascites, rapid weight gain is caused by the third spacing, and respiratory difficulty is caused by the development of pleural effusions or in severe cases ARDS. Hypotension, tachycardia and decreased renal perfusion with oliguria and risk of renal failure may develop as the intravascular volume is contracted. Decreased intravascular volume also leads to hemoconcentration and increased risk of thromboembolism. In the case presented, the patient’s hematocrit was elevated at 54% indicating hemoconcentration. 1

Discussion There exist several classification schemes for OHSS. The commonly used classification by Golan describes mild, moderate, and severe forms of OHSS which are subdivided into five grades. Grade 1 and 2 are mild, grade 3 is moderate, and grade 4 and 5 are severe. Each grade incorporates the findings of the lower grades and adds one or more characteristics. 2, 3 - Grade 1: Abdominal distention and discomfort. MILD - Grade 2: Grade 1 + nausea, vomiting, diarrhea, and enlarged ovaries to 5 - 12 cm. MODERATE SEVERE - Grade 3: Mild characteristics + ultrasound evidence of ascites. - Grade 4: Moderate characteristics + clinical evidence of ascites and/or hydrothorax or breathing difficulties. - Grade 5: All of the above + change in blood volume, hemoconcentration, coagulation abnormalities, and decreased renal perfusion/function.

Discussion More recently, Rizk and Aboulghar proposed another classification, which aims to place patients into clinical groups that better correlate with prognosis so as to help guide treatment. The mild category described in earlier classifications such as the one proposed by Golan has been eliminated since nearly all patients undergoing ovarian stimulation therapy experience these mild symptoms which require no specific therapy. 2, 3 -Moderate OHSS: Abdominal distention and discomfort, nausea, normal labs, U/S evidence of ascites and enlarged ovaries but no clinical evidence of ascites. -Severe OHSS: -Grade A: Inpatient or outpatient treatment depending on clinical judgement. Nausea, vomiting, diarrhea, abdominal pain, oliguria, dyspnea, clinical evidence of ascites or hydrothorax. -Grade B: Requires inpatient treatment. Grade A + massive ascites, massively enlarged ovaries, severe dyspnea, marked oliguria, increased Hct, creatinine, LFTs. -Grade C: Requires ICU treatment: OHSS + ARDS, renal failure, or venous thromboembolism
Discussion OHSS is generally a self-limiting disorder that resolves spontaneously in less than 2 weeks and requires only symptomatic therapy. It should be noted, however, that when the patient with OHSS is pregnant, the disorder may persist and is often more severe 3. Other differental considerations include polycystic ovary syndrome. These patient are in a hyperandrogenic state with associated problems including amenorrhea or oligomenorrhea, infertility, insulin resistance, obesity, and hirsutism. The ultrasound appearance of the ovaries in these patients is variable. Some are normal in appearance, some are solid but enlarged, and some demonstrate the classic appearance of enlargement with numerous small cysts lined up peripherally in a string of pearls configuration. Polycystic ovary syndrome is not likely in this case as there is no association of polycystic ovaries with ascites or pleural effusions. Also, the cysts in polycystic ovary syndrome are usually small and relatively uniform whereas those seen in the case presented here are large and of variable size and shape. 4
Discussion Primary ovarian malignancies or metastatic disease to the ovaries can potentially present with a similar constellation of findings. Ovarian cancer may be primarily cystic, as in serous and mucinous cystadenocarcinoma, and up to 20% of ovarian malignancies are bilateral. Ovarian metastases may also bilateral and some, including rectosigmoid colon cancer may be cystic. Metastatic disease to the ovaries and primary ovarian malignancies are frequently advanced at diagnosis with peritoneal metastasis, and ascites. Pleural effusions may also be seen in both metastatic disease to the ovaries and primary ovarian cancer. 4 Despite some superficial similarities of ovarian metastasis and primary ovarian malignancy to the presented case, there are several important differences. The main difference in terms of imaging is the lack of a mass in either ovary. While both metastatic disease and primary ovarian malignancies may be cystic, they usually present as complex cystic masses that distort the normal ovary, rather than as multiple peripheral anechoic simple cysts with a normal appearing ovarian stroma as seen here. Cystic malignancies are typically multiloculated with internal echoes, thick septations, and/or solid nodules. 4
Discussion Ovarian torsion must always be considered in a patient with enlarged ovaries and pelvic pain. Torsion occurs when an ovary twists on its vascular pedicle and becomes ischemic. The torsed ovary will be enlarged, with a heterogeneous stromal echotexture secondary to edema, hemorrhage, and or necrosis. Evaluation of flow to the ovary is of limited value as flow may be detected in a torsed ovary and no flow may be detected in a normal ovary. In cases of torsion, the edematous stroma pushes the normal follicles peripherally, creating an appearance of peripheral cysts similar to that seen in PCO and OHSS. In this patient’s case, flow is demonstrated, and torsion is unlikely because the visualized ovarian stroma has a homogenous echotexture and normal echogenicity. 4 Of course torsion and OHSS can coexist and it cannot be overemphasized that torsion should be considered in every case of OHSS that presents with pelvic pain.
Diagnosis Ovarian Hyperstimulation Syndrome: Clinical and ultrasound evidence of ascites, pleural effusions, symptoms of respiratory difficulty, and evidence of hemoconcentration, results in the patient being graded as below: - Severe, Grade 5 according to the Golan Classification. - Severe, Grade B according to the Rizk/Aboulghar Classification:
References 1. The Practice Committee of the American Society for Reproductive Medicine. Ovarian hyperstimulation syndrome. Fertility and Sterility 2008; 90: S 188 -193. 2. Rizk B. Ovarian Hyperstimulation Syndrome: Epidemiology, Pathophysiology, Prevention and Management. New York, NY: Cambridge University Press, 2006; 1 -10. 3. Beerendonk CCM, van Dop PA, Braat DDM, Merkus JMWM. Ovarian hyperstimulation syndrome: facts and fallacies. Obstetrical and Gynecological Survey 1998; 53(7): 439 -449. 4. Middleton WD, Kurtz AB, Hertzberg BS. Ultrasound: The Requisites. 2 nd Ed. St. Louis, MO: Mosby, 2006; 558 -563, 565 -569, 576 -581.
 Ferriman-gallwey score
Ferriman-gallwey score Erate pa
Erate pa Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Genitourinary & stds
Genitourinary & stds Male genitourinary anatomy
Male genitourinary anatomy Chapter 29 the child with a genitourinary condition
Chapter 29 the child with a genitourinary condition Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Chapter 29 the child with a genitourinary condition
Chapter 29 the child with a genitourinary condition Modality in software engineering
Modality in software engineering Characteristics of sensory neurons
Characteristics of sensory neurons Modality
Modality Medium modality
Medium modality Cardinality and modality
Cardinality and modality Epistemic modality
Epistemic modality Swd modality
Swd modality Callendreasonlocaluserinitiated
Callendreasonlocaluserinitiated One to many relationship line
One to many relationship line Modality statistics
Modality statistics Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Sodality vs modality
Sodality vs modality