RACGP Victoria Faculty Supporting Recovery and Return To

- Slides: 49
RACGP Victoria Faculty Supporting Recovery and Return To Work For patients with pain and mental health conditions Presented by Dr Ben Barresi, General Practitioner A/Prof Carolyn Arnold, Pain Management Specialist Dr Dielle Felman, Consultant Psychiatrist Dr Peter Cotton, Clinical Psychologist Facilitated by Dr Michael Aufgang, RACGP Victoria Faculty Board Member
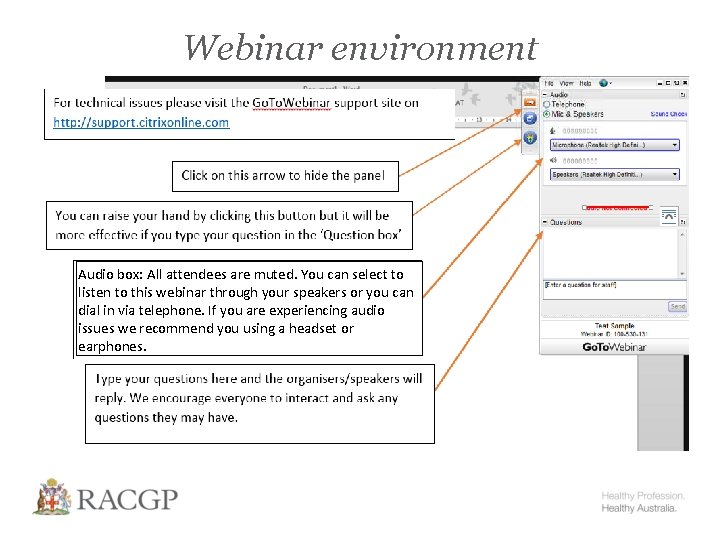
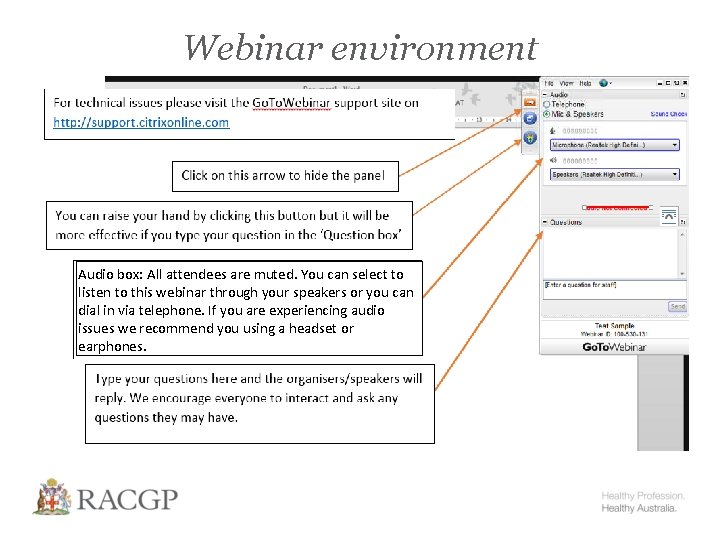
Webinar environment Audio box: All attendees are muted. You can select to listen to this webinar through your speakers or you can dial in via telephone. If you are experiencing audio issues we recommend you using a headset or earphones.
Supporting recovery and return to work for patients with pain and mental health conditions Wednesday 19 August 6. 30 pm

Speakers Dr Ben Barresi, General Practitioner A/Prof Carolyn Arnold, Pain Management Specialist Dr Dielle Felman, Consultant Psychiatrist Dr Peter Cotton, Clinical Psychologist
Learning Outcomes 1. Increase awareness of the relationship between mental health, acute and persistent pain and work related injury 2. Identify key principles and provide practical strategies for assessing and managing comorbid pain and mental health conditions in relation to work related injuries 3. Increase awareness of the important role of GPs and other health providers in setting recovery and treatment expectations for their patients 4. Increase awareness of services to support GPs in management of these patients
Supporting recovery and return to work for patients with pain and mental health conditions 6
Pain and Mental Health Setting the Scene 7
Pain …an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage …pain is always subjective, each individual learns the application of the word through experiences related to injury in early life Merskey & Bogduk (1994)
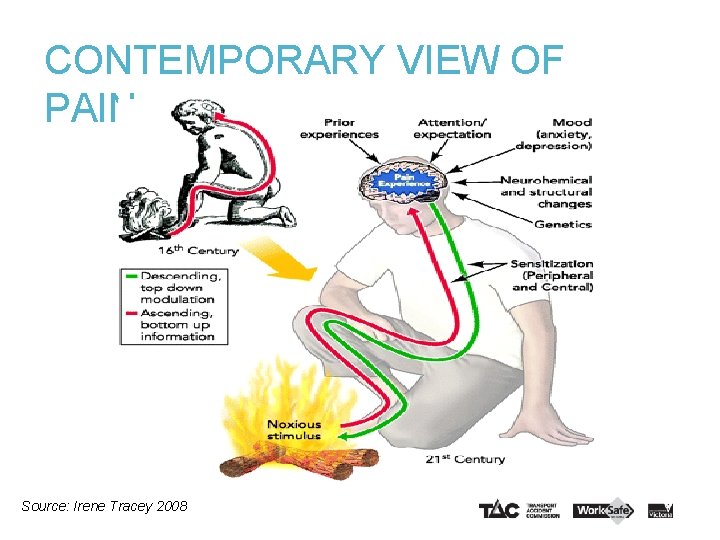
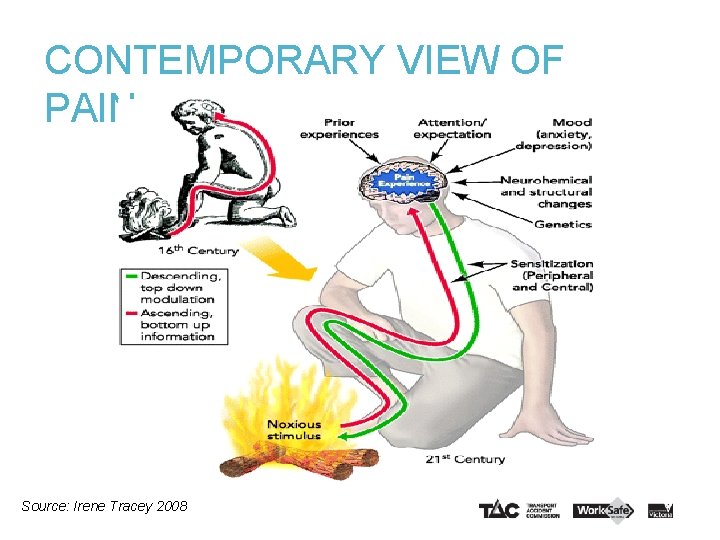
CONTEMPORARY VIEW OF PAIN Source: Irene Tracey 2008
Pain theories • Pain is no longer seen as a linear relationship between stimulus, or injury and response • New thinking supported by research shows pain experience is a complex phenomena with sophisticated central processing, learning and plasticity in play • In Chronic Pain the dynamic balance between excitation and inhibition has become maladaptive, often leading to excessive pain response, and pain appears disproportionate to the underlying condition.
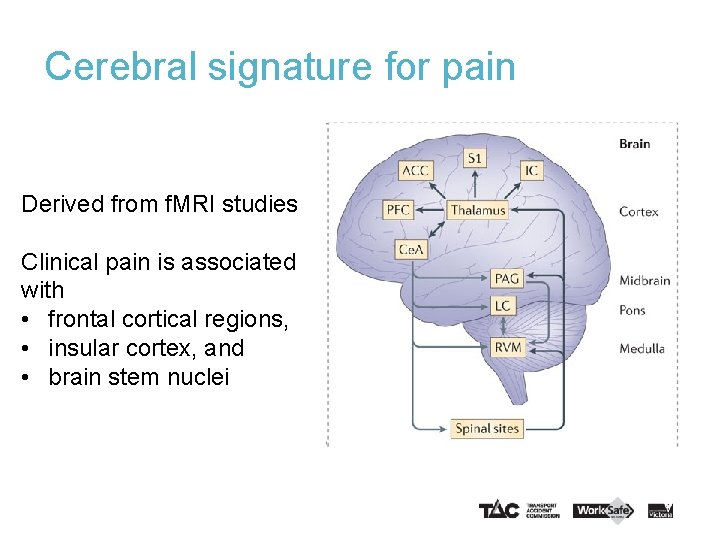
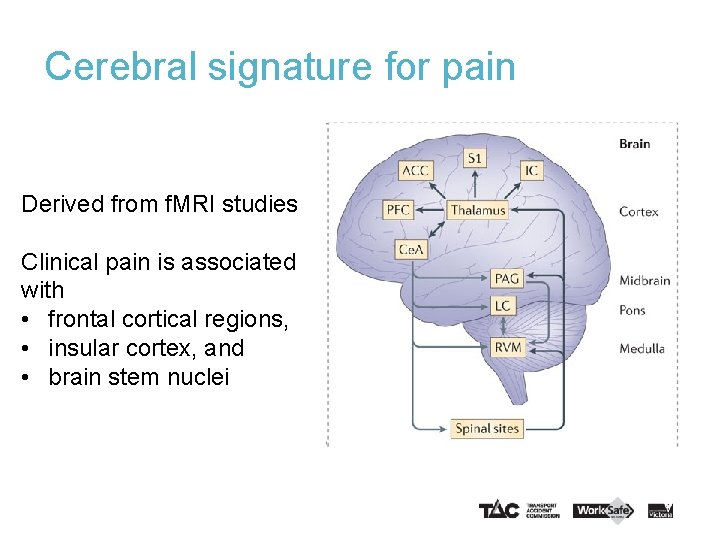
Cerebral signature for pain Derived from f. MRI studies Clinical pain is associated with • frontal cortical regions, • insular cortex, and • brain stem nuclei
Treatment for chronic pain • Given the complexity involved, monotherapy is rarely going to be an effective treatment • If medication or a procedure give a “window“ of analgesia or partly reduced pain – Use it to restore physical function – Address psychological and social factors – Facilitate return to usual roles including work
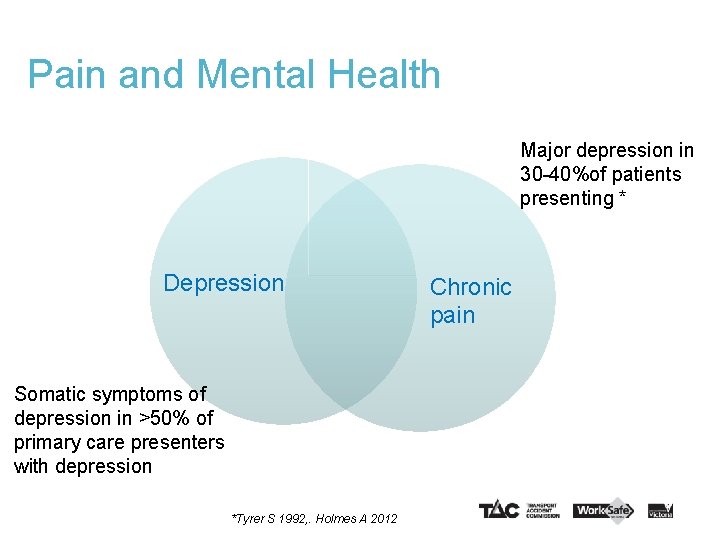
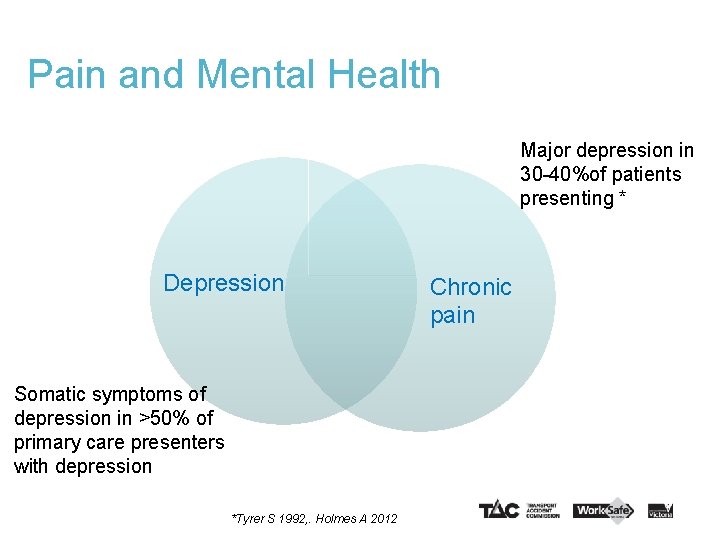
Pain and Mental Health Major depression in 30 -40%of patients presenting * Depression Somatic symptoms of depression in >50% of primary care presenters with depression *Tyrer S 1992, . Holmes A 2012 Chronic pain
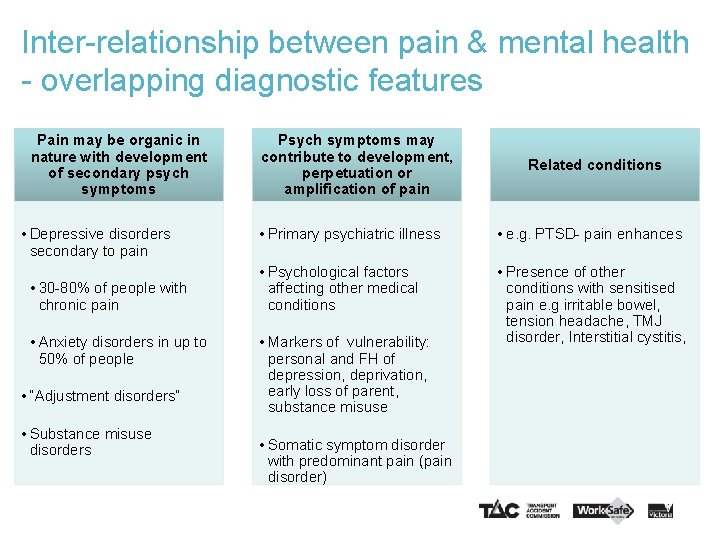
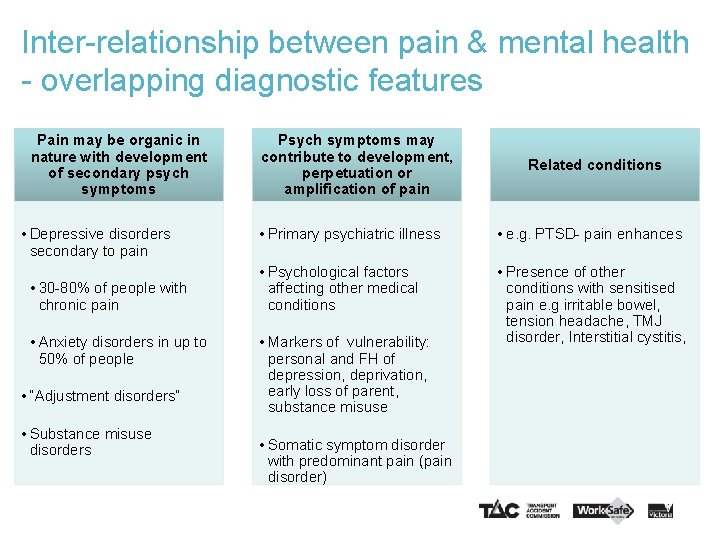
Inter-relationship between pain & mental health - overlapping diagnostic features Pain may be organic in nature with development of secondary psych symptoms • Depressive disorders secondary to pain • 30 -80% of people with chronic pain • Anxiety disorders in up to 50% of people • “Adjustment disorders” • Substance misuse disorders Psych symptoms may contribute to development, perpetuation or amplification of pain Related conditions • Primary psychiatric illness • e. g. PTSD- pain enhances • Psychological factors affecting other medical conditions • Presence of other conditions with sensitised pain e. g irritable bowel, tension headache, TMJ disorder, Interstitial cystitis, • Markers of vulnerability: personal and FH of depression, deprivation, early loss of parent, substance misuse • Somatic symptom disorder with predominant pain (pain disorder)
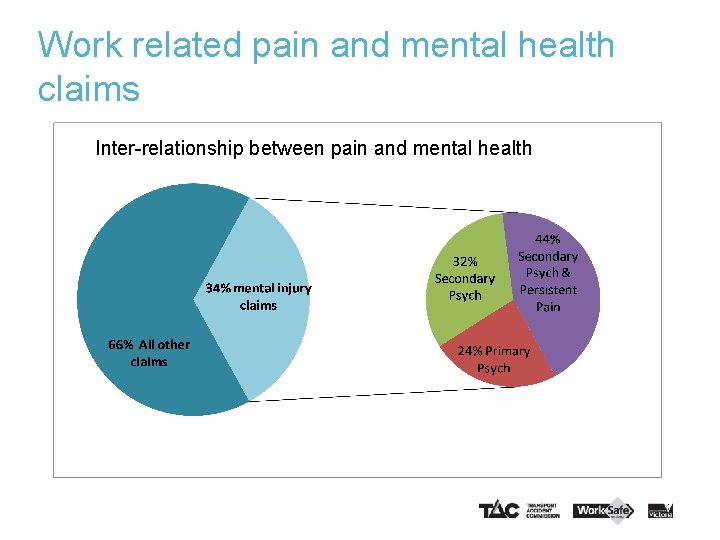
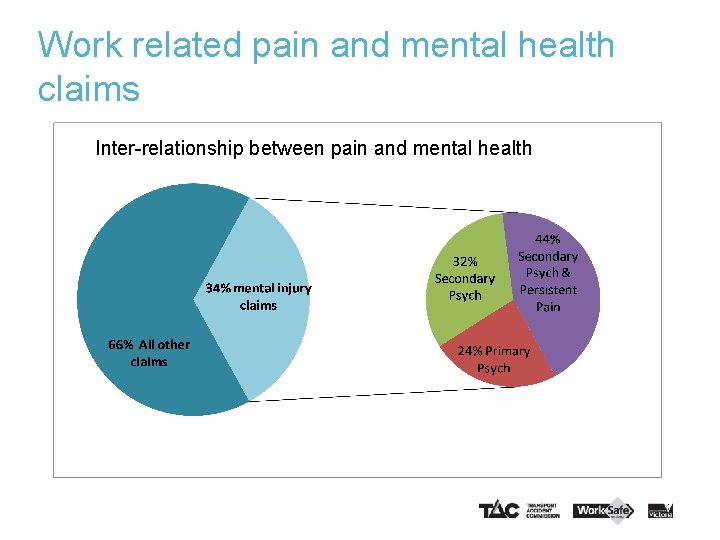
Work related pain and mental health claims Inter-relationship between pain and mental health
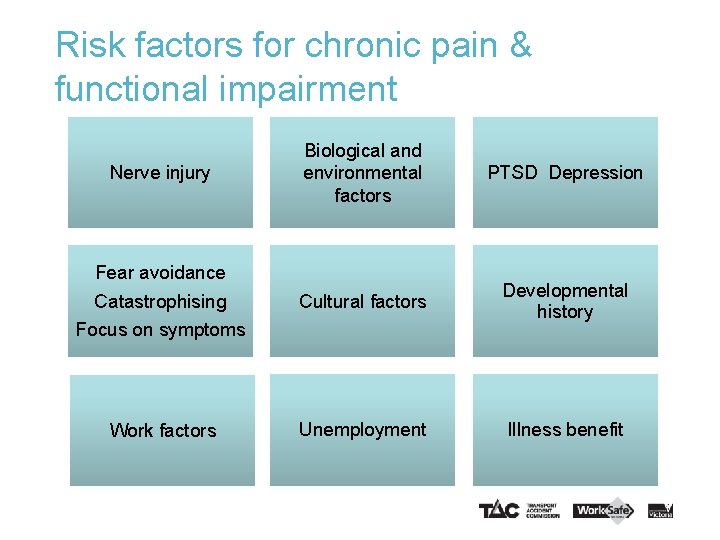
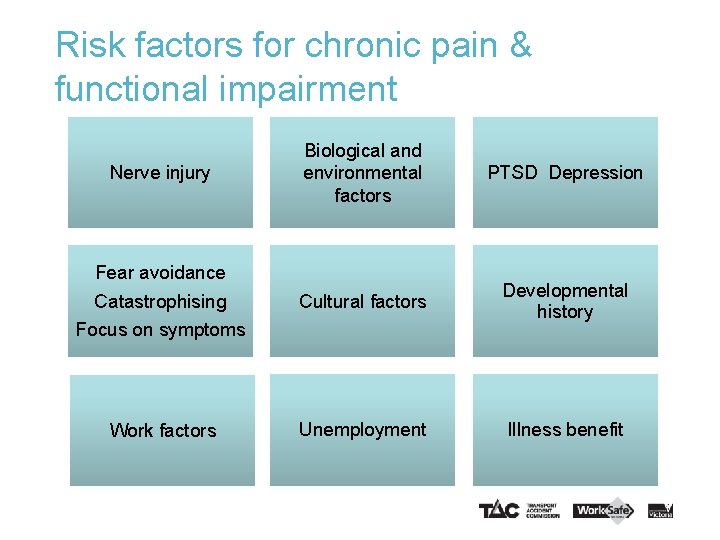
Risk factors for chronic pain & functional impairment Biological and environmental factors PTSD Depression Catastrophising Focus on symptoms Cultural factors Developmental history Work factors Unemployment Illness benefit Nerve injury Fear avoidance
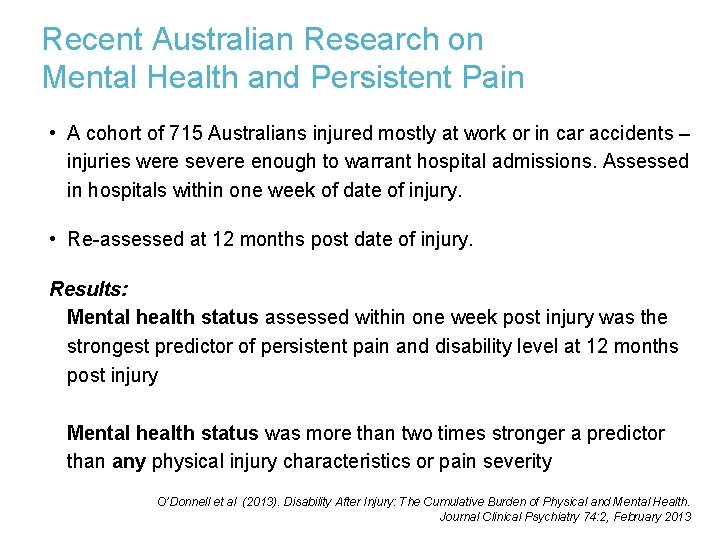
Recent Australian Research on Mental Health and Persistent Pain • A cohort of 715 Australians injured mostly at work or in car accidents – injuries were severe enough to warrant hospital admissions. Assessed in hospitals within one week of date of injury. • Re-assessed at 12 months post date of injury. Results: Mental health status assessed within one week post injury was the strongest predictor of persistent pain and disability level at 12 months post injury Mental health status was more than two times stronger a predictor than any physical injury characteristics or pain severity O’Donnell et al (2013). Disability After Injury: The Cumulative Burden of Physical and Mental Health. Journal Clinical Psychiatry 74: 2, February 2013
Assessing pain and mental health conditions in relation to work related injury 18
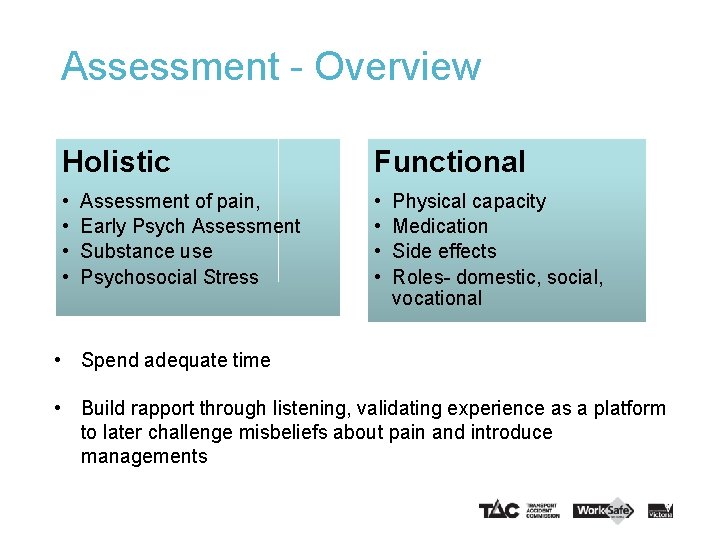
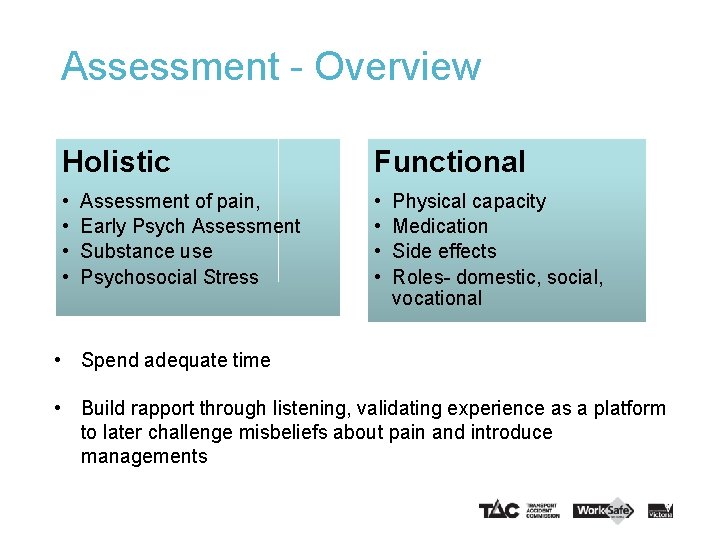
Assessment - Overview Holistic Functional • • Assessment of pain, Early Psych Assessment Substance use Psychosocial Stress Physical capacity Medication Side effects Roles- domestic, social, vocational • Spend adequate time • Build rapport through listening, validating experience as a platform to later challenge misbeliefs about pain and introduce managements
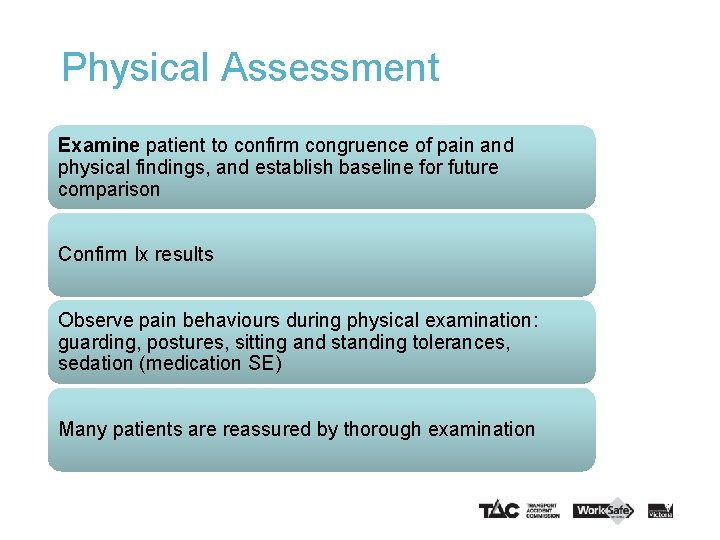
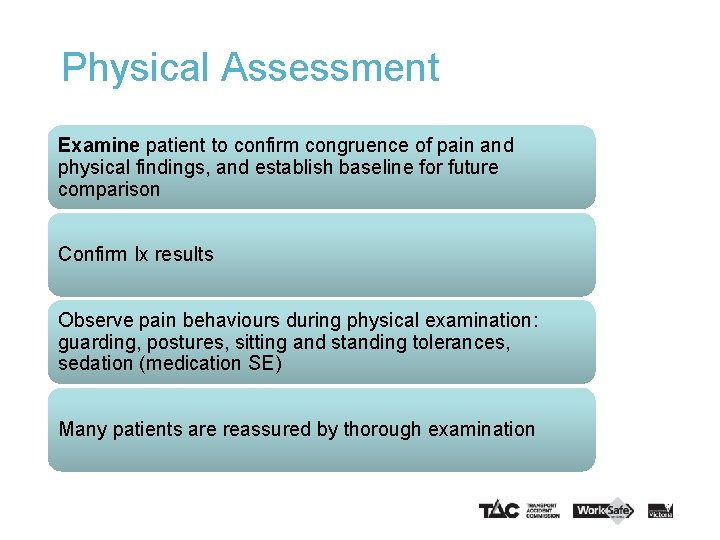
Physical Assessment Examine patient to confirm congruence of pain and physical findings, and establish baseline for future comparison Confirm Ix results Observe pain behaviours during physical examination: guarding, postures, sitting and standing tolerances, sedation (medication SE) Many patients are reassured by thorough examination
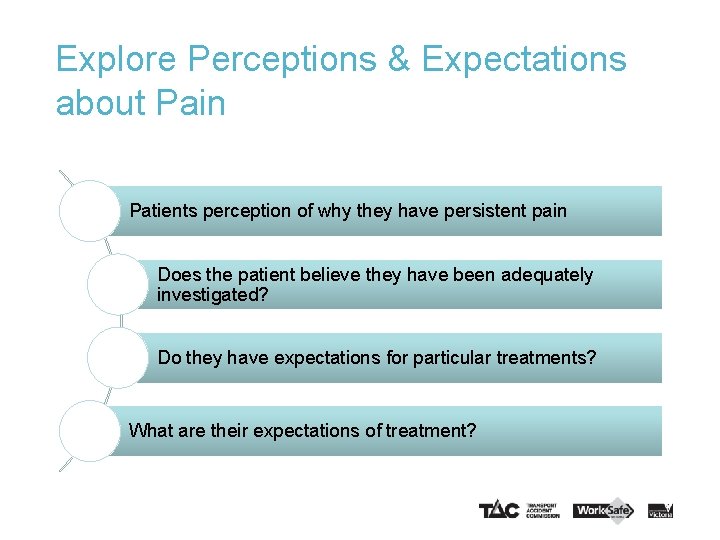
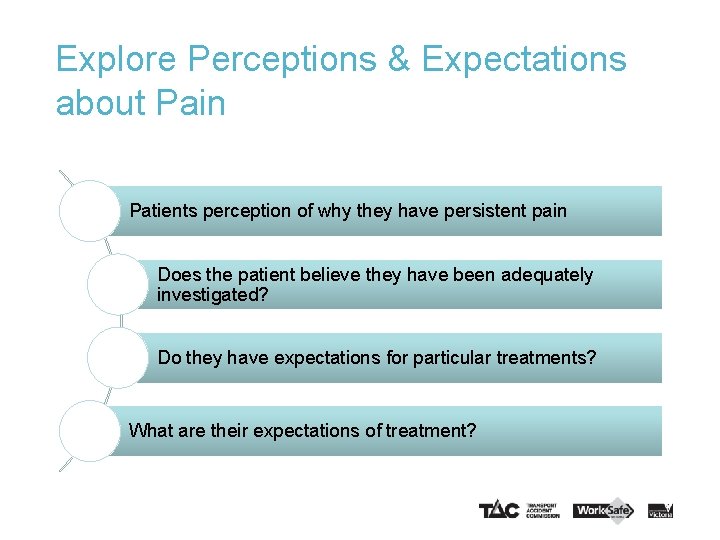
Explore Perceptions & Expectations about Pain Patients perception of why they have persistent pain Does the patient believe they have been adequately investigated? Do they have expectations for particular treatments? What are their expectations of treatment?
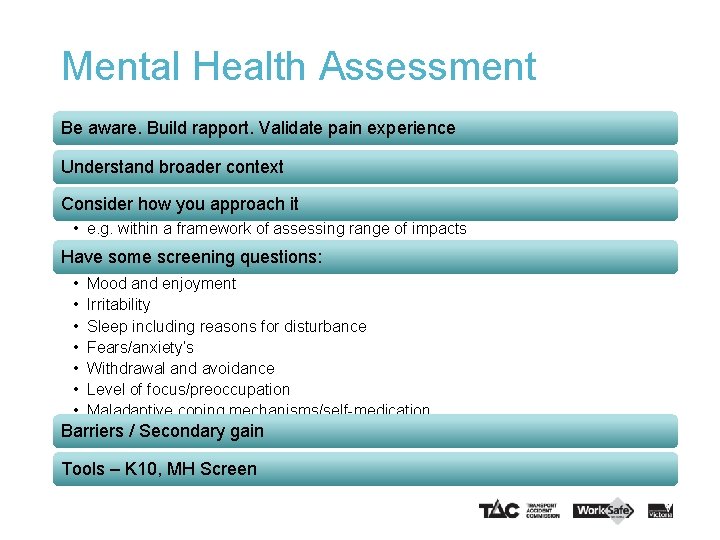
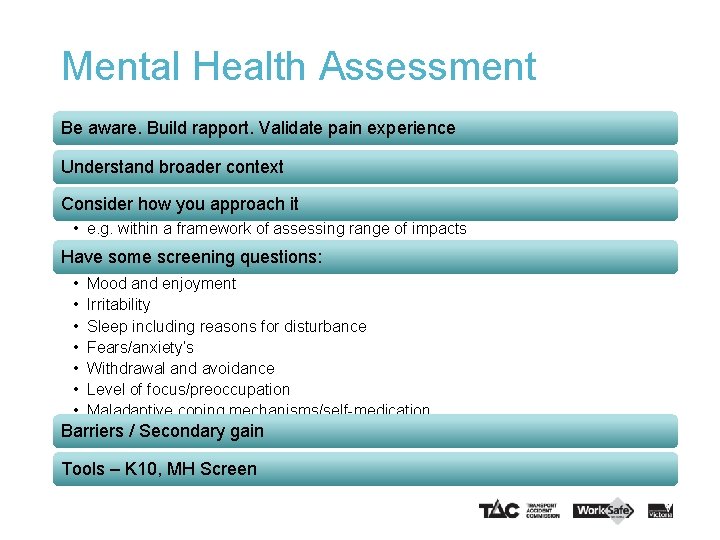
Mental Health Assessment Be aware. Build rapport. Validate pain experience Understand broader context Consider how you approach it • e. g. within a framework of assessing range of impacts Have some screening questions: • • Mood and enjoyment Irritability Sleep including reasons for disturbance Fears/anxiety’s Withdrawal and avoidance Level of focus/preoccupation Maladaptive coping mechanisms/self-medication Barriers / Secondary gain Tools – K 10, MH Screen
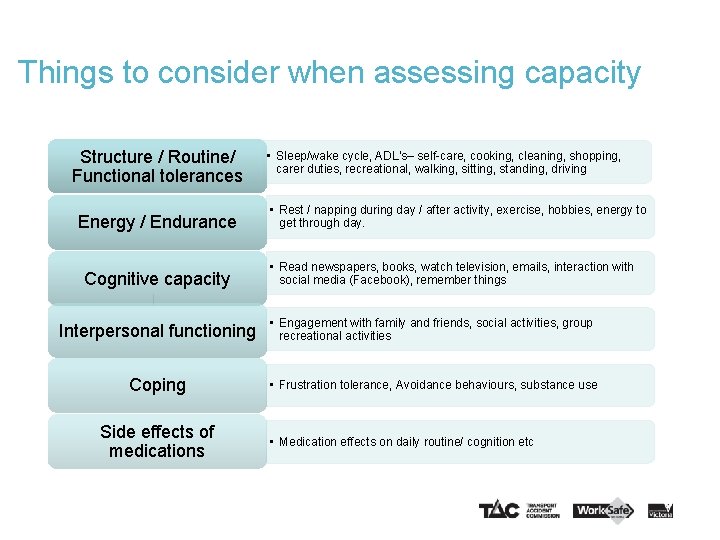
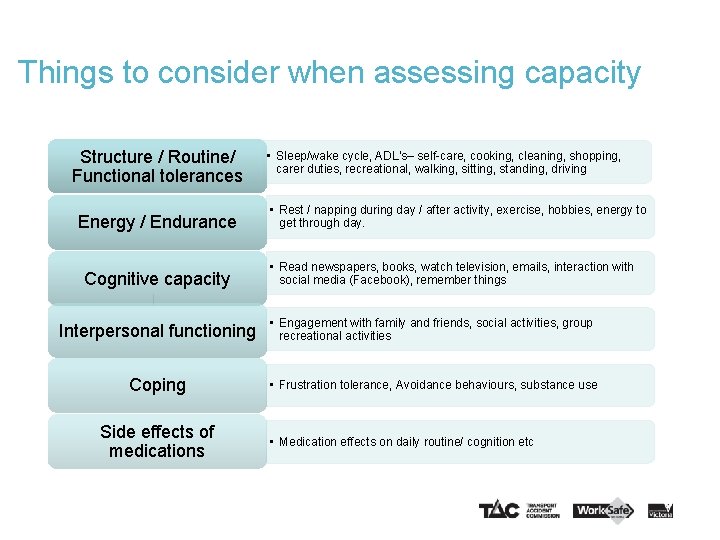
Things to consider when assessing capacity Structure / Routine/ Functional tolerances Energy / Endurance Cognitive capacity • Sleep/wake cycle, ADL’s– self-care, cooking, cleaning, shopping, carer duties, recreational, walking, sitting, standing, driving • Rest / napping during day / after activity, exercise, hobbies, energy to get through day. • Read newspapers, books, watch television, emails, interaction with social media (Facebook), remember things Interpersonal functioning • Engagement with family and friends, social activities, group recreational activities Coping • Frustration tolerance, Avoidance behaviours, substance use Side effects of medications • Medication effects on daily routine/ cognition etc
Managing pain and mental health conditions in relation to work related injury 25
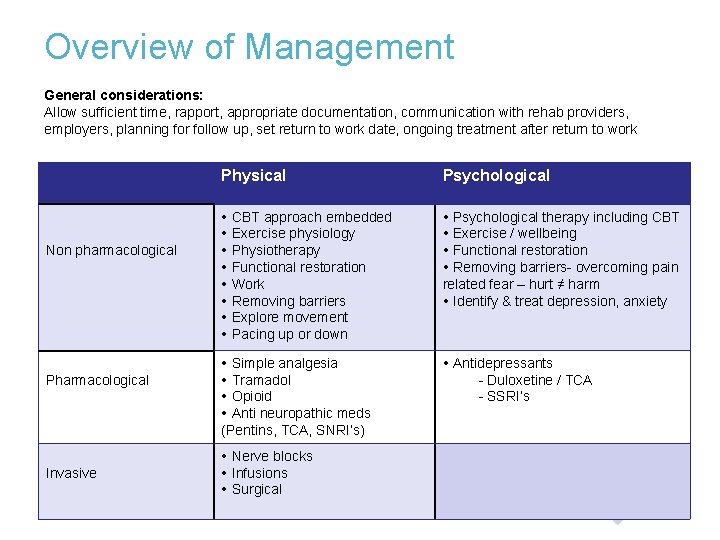
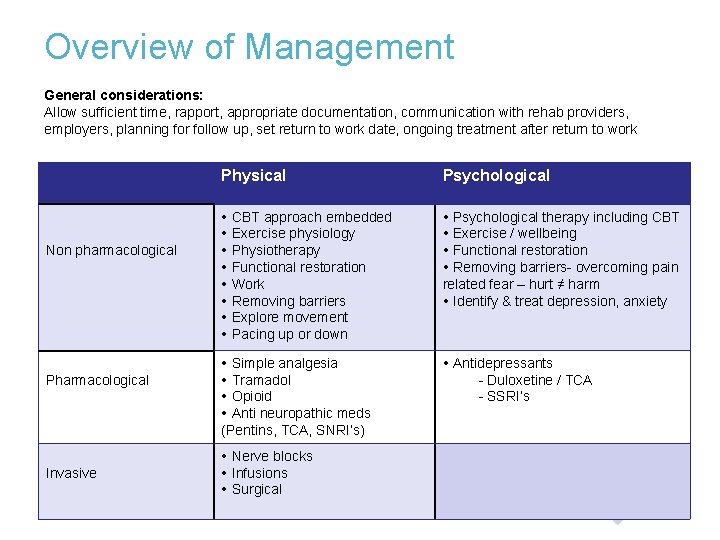
Overview of Management General considerations: Allow sufficient time, rapport, appropriate documentation, communication with rehab providers, employers, planning for follow up, set return to work date, ongoing treatment after return to work Non pharmacological Pharmacological Invasive Physical Psychological CBT approach embedded Exercise physiology Physiotherapy Functional restoration Work Removing barriers Explore movement Pacing up or down Psychological therapy including CBT Exercise / wellbeing Functional restoration Removing barriers- overcoming pain related fear – hurt ≠ harm Identify & treat depression, anxiety Simple analgesia Tramadol Opioid Anti neuropathic meds (Pentins, TCA, SNRI’s) Antidepressants - Duloxetine / TCA - SSRI’s Nerve blocks Infusions Surgical
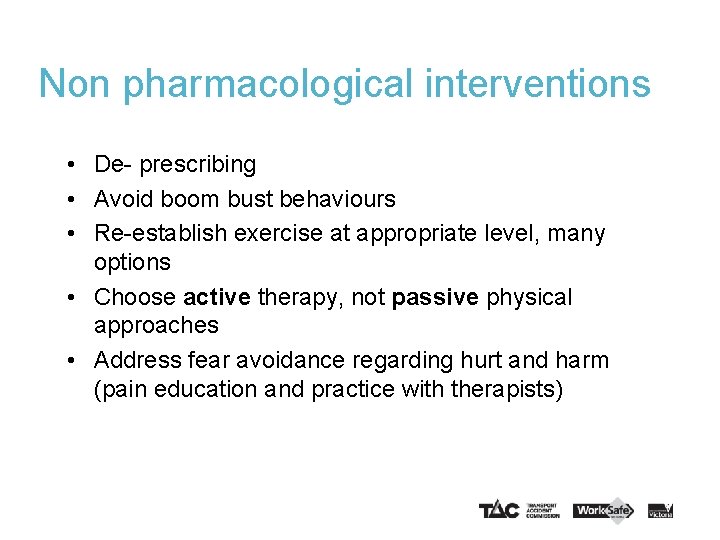
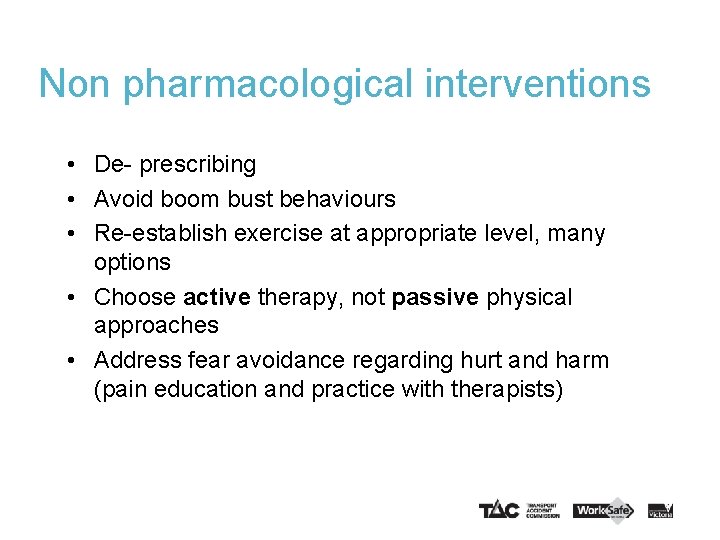
Non pharmacological interventions • De- prescribing • Avoid boom bust behaviours • Re-establish exercise at appropriate level, many options • Choose active therapy, not passive physical approaches • Address fear avoidance regarding hurt and harm (pain education and practice with therapists)
Is work a pain management strategy? Significant differences seen in the “at work” group: • Lower fear avoidance • Less pain catastrophising • Lower perceived workload • Higher pain acceptance • Higher life control Comparison of workers at work and not at work with chronic musculoskeletal pain Haitze, J, et el Workers who safety at work despite chronic nonspecific musculoskletal pain: Do they differ from workers with sick leave? Journal Occup Rehabil (2012) 22: 489 -502
The role of GPs in realising the Health Benefits of Work Evidence-based messages: Work is an important part of rehabilitation Work is a therapeutic intervention Typically, waiting for recovery, delays recovery Staying away from work may lead to poorer health Employer-supported, early return to work helps recovery
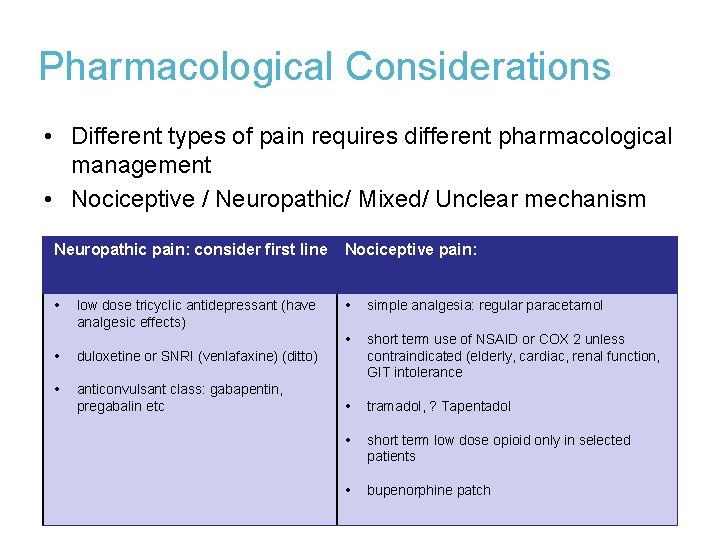
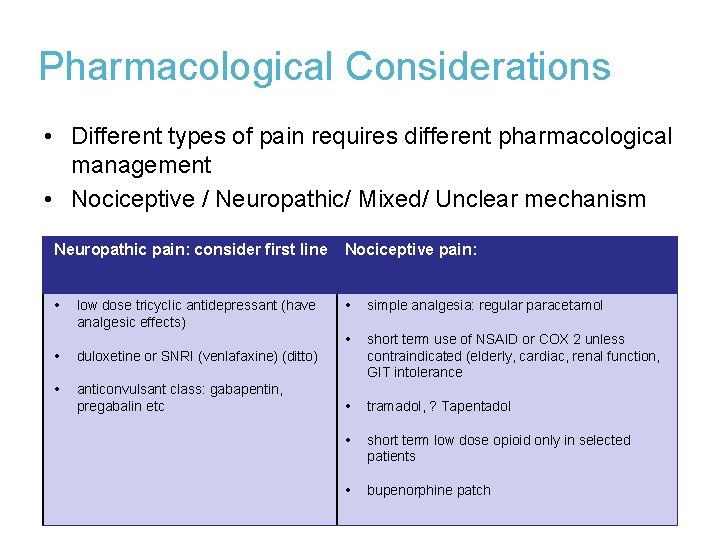
Pharmacological Considerations • Different types of pain requires different pharmacological management • Nociceptive / Neuropathic/ Mixed/ Unclear mechanism Neuropathic pain: consider first line Nociceptive pain: simple analgesia: regular paracetamol short term use of NSAID or COX 2 unless contraindicated (elderly, cardiac, renal function, GIT intolerance tramadol, ? Tapentadol short term low dose opioid only in selected patients bupenorphine patch low dose tricyclic antidepressant (have analgesic effects) duloxetine or SNRI (venlafaxine) (ditto) anticonvulsant class: gabapentin, pregabalin etc
Pharmacological Considerations Opioids 1. Opioids commenced for Rx of acute pain should not be continued if pain persists without careful re-assessment of risks /benefits 2. Be wary of opioids in “sensitized” pain conditions e. g fibromyalgia 3. Long term opioids for chronic pain are being reconsidered due to – – tolerance (loss of effect) and lack of evidence of effectiveness in chronic pain
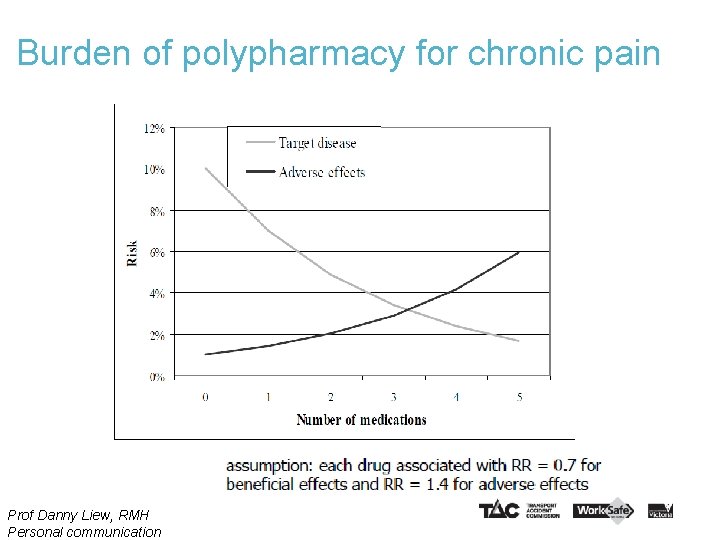
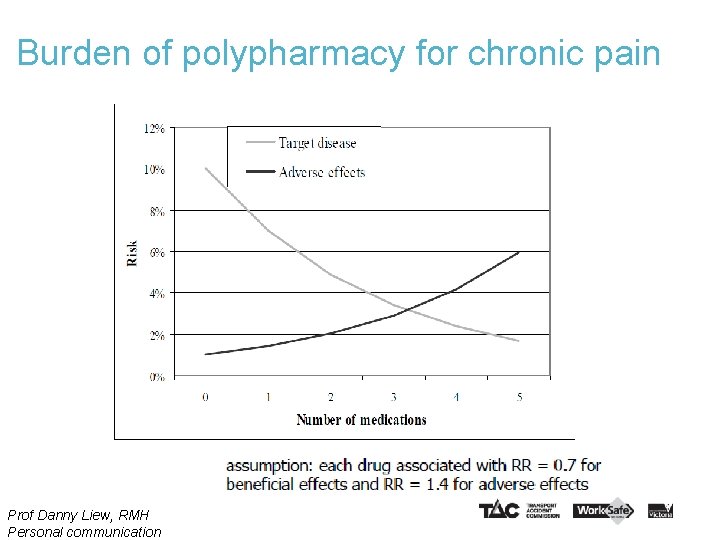
Burden of polypharmacy for chronic pain Prof Danny Liew, RMH Personal communication
Case Study Discussion • John (JM) 46 yr • Cleaner in local shopping centre • Injured R shoulder when emptying bin into a skip 33
Case study – John (JM) • You see him 10 weeks after his initial injury. • He attended a colleague of yours (now left the practice). • Diagnosis: right sternoclavicular joint sprain (confirmed CT and MRI) • JM was told by he would have acute pain for approx 2 weeks and could then RTW with recovery expected to take 6 weeks. • Your colleague arranged a specialist appointment for JM (no surgery required) • He has had a cortisone injection and notes indicated he developed flushing of the face. He was also prescribed anti-inflammatory medication but made him feel “weak & tired”. John reluctant to take simple analgesics. • He was off work initially for two weeks, then returned to modified duties. Your colleague referred him to a psychologist prior to leaving your practice. He tells you he didn’t attend. • He has been on modified duties since week 2 post injury. • He has had an Occupational Rehabilitation Provider assessment and you read in the notes that “JM is very pain focused”
Case Study – Following your first assessment • John speaks for 5 -10 minutes about the severity of his pain. • He is reluctant to consider any alternatives you offer citing the previous reaction to an injection. • He has tried anti inflammatory medication and that mad him feel “weak and unwell” • He spontaneously reports feelings of pain from time to time which can last between 1 -20 mins • He has no difficulty with activities of daily living. He can undertake household cleaning tasks including wiping benches, sweeping, carry rubbish to the bin outside and push the bins to the kerb once a week for collection. • He tells you that he is now starting to worry about lots of different things involving his two children, his wife, his pain and what is going to happen to him? • Your examination findings reveal mild tenderness of the sterno-clavicular joint, a full range of motion and sufficient strength on manual muscle testing of the shoulder girdle. He grimaces every time you palpate any part of the shoulder girdle and lateral side of the neck. • He has been on restricted duties for six weeks folding envelopes in the office and is “bored” and wants to consider a return to more active duties.
Workplace reasonable adjustments Work. Cover legislation – The employer is obligated to make reasonable adjustments. Consider: Duties e. g. modified duties Hours e. g. reduced hours, graduated increase in hours. Expectations e. g. longer time frames, lower KPI’s Work. Safe and TAC can fund the cost of reasonable workplace modifications to assist a worker to return to suitable employment.
Case Study continues After your discussion with John, you certify him fit for suitable duties for a period of 4 weeks as listed in the RTW plan. The plan excludes any provocative activity for his shoulder and outlines John starting modified duties at 12 hrs per week, and then graduating through 8 hrs, 24 hrs, 30 hrs in the final week before your review. You see him for his scheduled review at 4 weeks and the following information emerges: • • • He didn’t attend psychologist He’s still getting pain lasting 20 mins & worried there is something seriously wrong At work some modified duties can provoke pain which causes him distress He is becoming more short tempered and irritable at home He has fears that when he is returned to full duties his employer will sack him
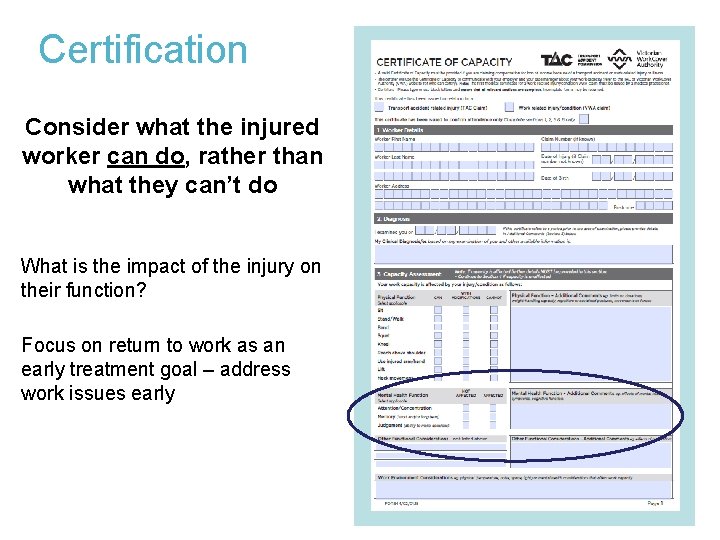
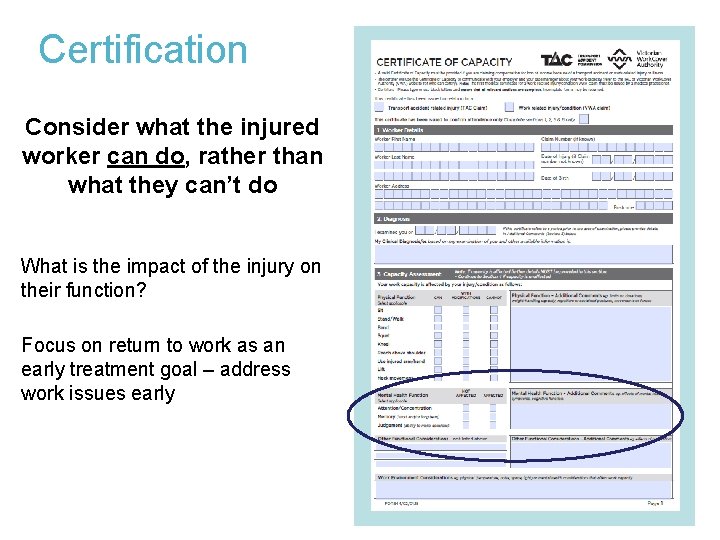
Certification Consider what the injured worker can do, rather than what they can’t do What is the impact of the injury on their function? Focus on return to work as an early treatment goal – address work issues early
Appropriate certification Certificates should: • be issued on the basis of medical reasons only - prevent iatrogenic disability • reflect the patient’s capacity rather than the availability of suitable employment • TAC or Work. Safe certificates should only be issued if the incapacity is related to a compensable injury
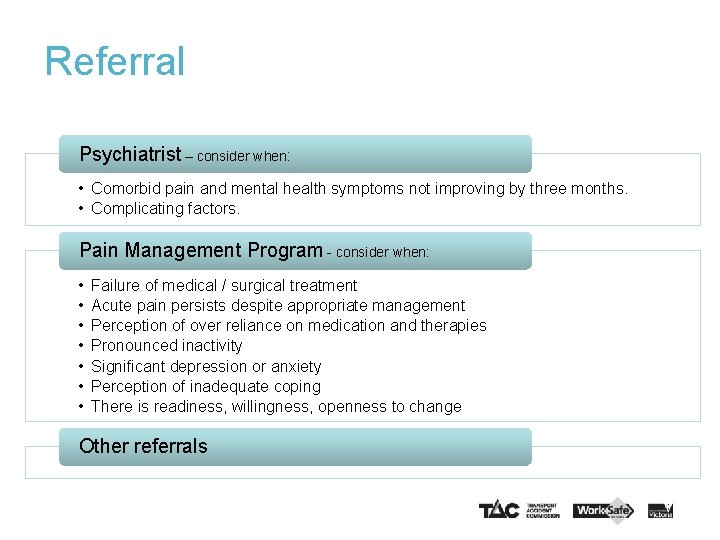
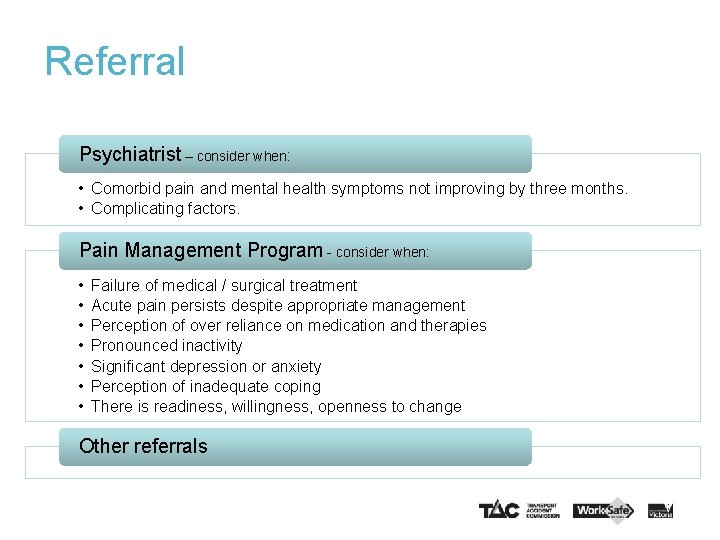
Referral Psychiatrist – consider when: • Comorbid pain and mental health symptoms not improving by three months. • Complicating factors. Pain Management Program - consider when: • • Failure of medical / surgical treatment Acute pain persists despite appropriate management Perception of over reliance on medication and therapies Pronounced inactivity Significant depression or anxiety Perception of inadequate coping There is readiness, willingness, openness to change Other referrals
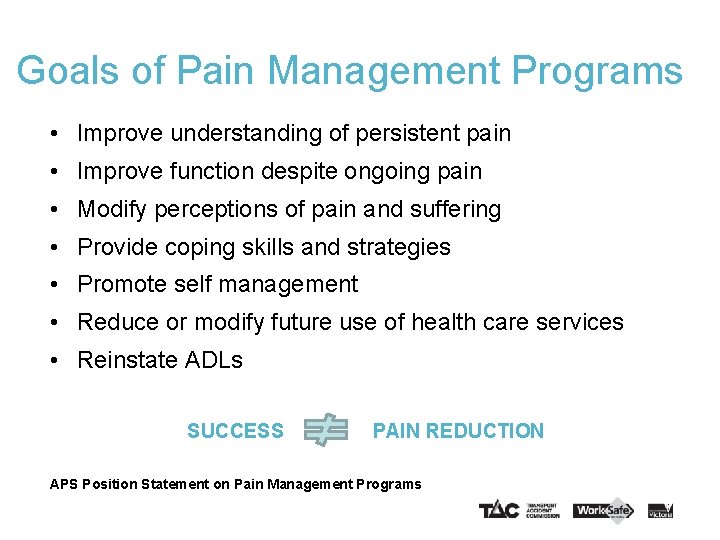
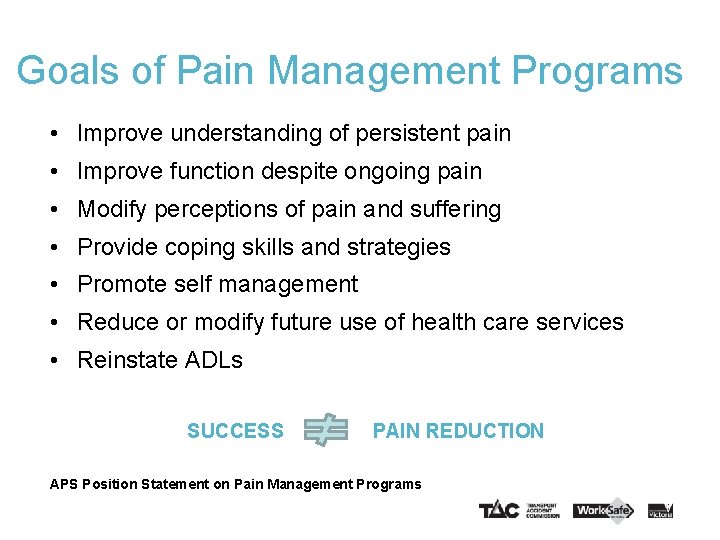
Goals of Pain Management Programs • Improve understanding of persistent pain • Improve function despite ongoing pain • Modify perceptions of pain and suffering • Provide coping skills and strategies • Promote self management • Reduce or modify future use of health care services • Reinstate ADLs SUCCESS PAIN REDUCTION APS Position Statement on Pain Management Programs
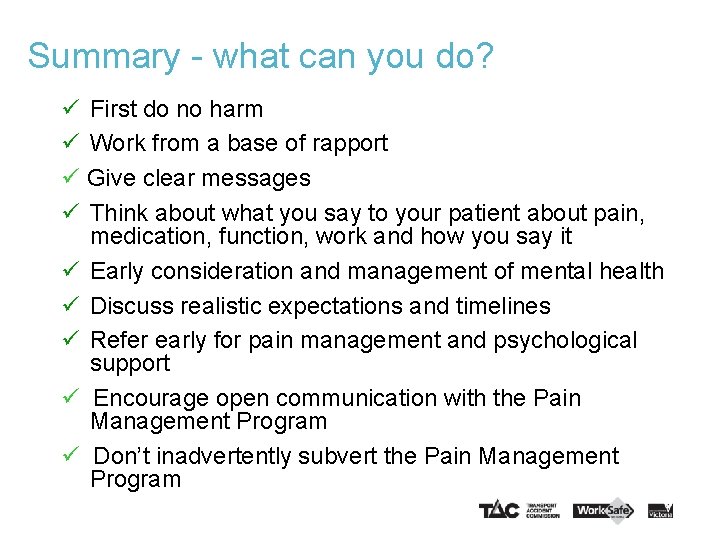
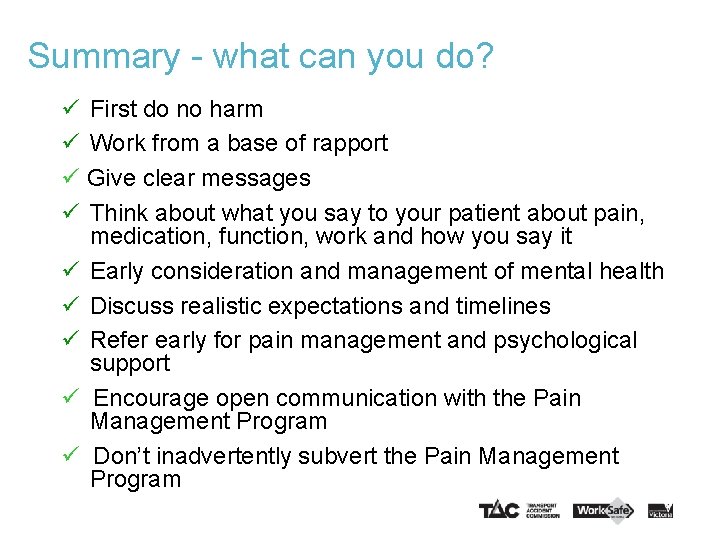
Summary - what can you do? First do no harm Work from a base of rapport Give clear messages Think about what you say to your patient about pain, medication, function, work and how you say it Early consideration and management of mental health Discuss realistic expectations and timelines Refer early for pain management and psychological support Encourage open communication with the Pain Management Program Don’t inadvertently subvert the Pain Management Program
Resources 45
Professional Development resources The following RACGP QI and CPD accredited e-learning modules are also available: Persistent Pain in the General Practice setting The Role of the GP in return to work including certification The Health Benefits of Safe Work Access the modules from the following websites: www. worksafe. vic. gov. au/certificate www. tac. vic. gov. au/certificate http: //learning. nhv. org. au/
Mental health resources • Vocational / Occupational Rehabilitation Services http: //www. worksafe. vic. gov. au/return-to-work/information-forworkers/getting-assistance-occupational-rehabilitation • Mindhealthconnect – www. mindhealthconnect. org. au – the Australian Government’s website provides up to date information and resources to assist with mental health issues including anxiety, stress and depression. The site also provides a list of endorsed online e-therapy services. • Return to Work. Net – returntowork. net. au – designed to help anyone involved in the process of returning to work after absence due to depression, an anxiety disorder or a related mental health problem • Beyondblue – New. Access – an early intervention program intended to provide easily accessible, free and quality services for people with mild to moderate depression and anxiety who are currently not accessing mental health services
Pain resources
Pain resources Multidisciplinary pain management services are recommended in public or private settings. Network Pain Management Programs aim to help patients injured in workplace or transport accidents to manage their musculoskeletal injuries and persistent pain, and increase their independence at home, work and in the community. http: //www. worksafe. vic. gov. au/forms-andpublications/forms-and-publications/network-painmanagement-fact-sheet-gp-psychology-physiotherapy
Other useful resources General Certificate of Capacity Services • www. worksafe. vic. gov. au/gp • www. tac. vic. gov. au/gp • Resources on the role of the GP, health benefits of work, talking about a return to work – conversation starters, info on invoices, payments and policies • www. worksafe. vic. gov. au/certificate • www. tac. vic. gov. au/certificate • Resources include Medical Director and Best Practice user guides, FAQs, certificate guide and examples • • • Network pain management program Return to Work Case Conferencing Occupational Rehabilitation providers E-therapy Outreach Services (TAC)
Contact information for TAC & Work. Safe: worksafe. vic. gov. au/gp TAC: tac. vic. gov. au/gp Provider Support Phone: 5225 6013 Email: Hdsg_provider_support@tac. vic. gov. au 51
Thank you 52
 Habitos de la victoria privada
Habitos de la victoria privada Mrbs scholarship
Mrbs scholarship Lee kong chian faculty of engineering and science
Lee kong chian faculty of engineering and science Mendel university faculty of business and economics
Mendel university faculty of business and economics Elearningunideb
Elearningunideb Faculty of economics and business zagreb
Faculty of economics and business zagreb Motivated energized and capable faculty
Motivated energized and capable faculty Lee kong chian faculty of engineering and science
Lee kong chian faculty of engineering and science Pubh4401
Pubh4401 Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Asc code
Asc code Albert ward st marys
Albert ward st marys My dog romeo essay
My dog romeo essay Examples of supporting questions
Examples of supporting questions Principles of information security 5th edition pdf
Principles of information security 5th edition pdf Minor supporting details
Minor supporting details Example of major points
Example of major points Implied main idea
Implied main idea Major supporting details
Major supporting details Main idea and supporting details example paragraphs
Main idea and supporting details example paragraphs Jeopardy main idea
Jeopardy main idea What is major supporting sentence
What is major supporting sentence Primary and supporting instruments
Primary and supporting instruments Main idea and supporting details examples
Main idea and supporting details examples Instrument cross check
Instrument cross check Compelling questions definition
Compelling questions definition Topics presented in chapters
Topics presented in chapters Example of supporting details
Example of supporting details Key sentence and supporting details
Key sentence and supporting details Compelling vs supporting questions
Compelling vs supporting questions Outline supporting details
Outline supporting details Reading comprehension main idea and supporting details
Reading comprehension main idea and supporting details Main idea and supporting details
Main idea and supporting details What is the central idea?
What is the central idea? Groundwork for college reading
Groundwork for college reading Example of main idea
Example of main idea English paragraph
English paragraph Topic sentence example
Topic sentence example Supporting facility example
Supporting facility example Supporting details outline
Supporting details outline Example of paragraph with supporting details
Example of paragraph with supporting details Making an outline example
Making an outline example Main idea and supporting details
Main idea and supporting details Main idea and details
Main idea and details Balance carried down
Balance carried down Lesson 4 parameters and return make rock paper scissors
Lesson 4 parameters and return make rock paper scissors Lesson 3: parameters and return practice
Lesson 3: parameters and return practice Profit and loss acount
Profit and loss acount Data centered architecture
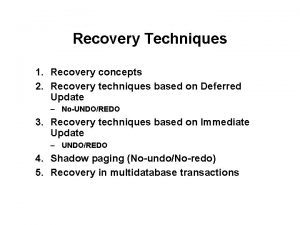
Data centered architecture Call and return architecture style
Call and return architecture style