Pulmonary circulation Physiological anatomy the Pul Artery is
![Blood flow �Effect of alveolar [O 2]: when [O 2] decreases below 70% of Blood flow �Effect of alveolar [O 2]: when [O 2] decreases below 70% of](https://slidetodoc.com/presentation_image_h2/beeca8b5d5c4df5f10adc8e4d214a868/image-8.jpg)
- Slides: 26
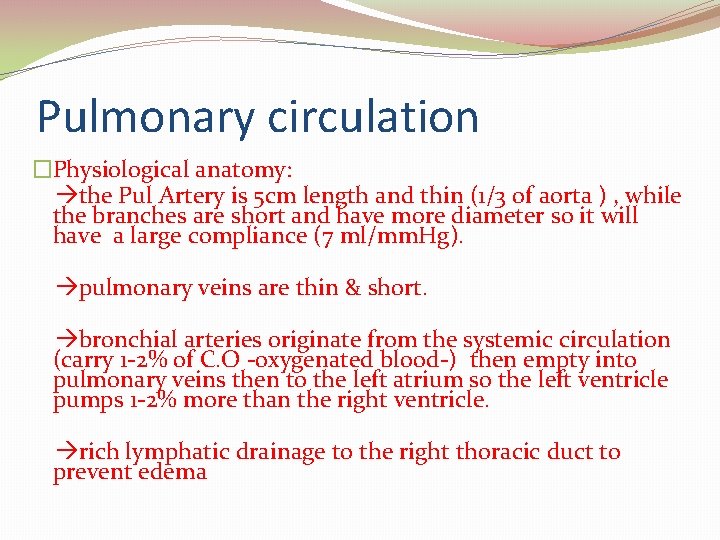
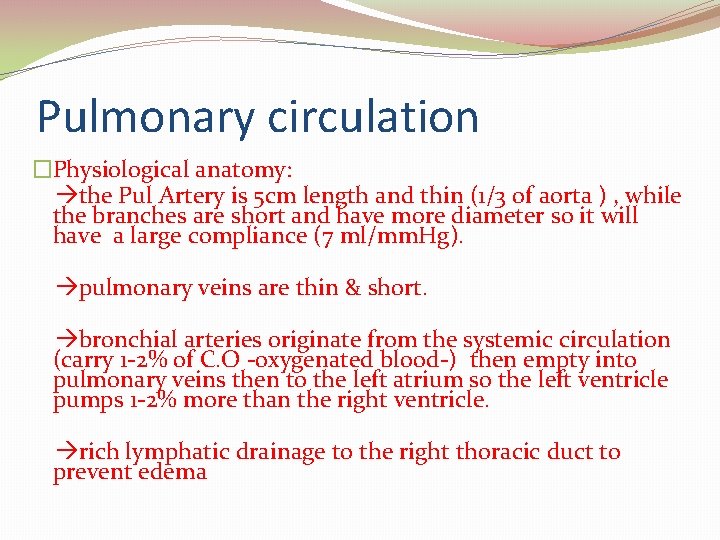
Pulmonary circulation �Physiological anatomy: the Pul Artery is 5 cm length and thin (1/3 of aorta ) , while the branches are short and have more diameter so it will have a large compliance (7 ml/mm. Hg). pulmonary veins are thin & short. bronchial arteries originate from the systemic circulation (carry 1 -2% of C. O -oxygenated blood-) then empty into pulmonary veins then to the left atrium so the left ventricle pumps 1 -2% more than the right ventricle. rich lymphatic drainage to the right thoracic duct to prevent edema
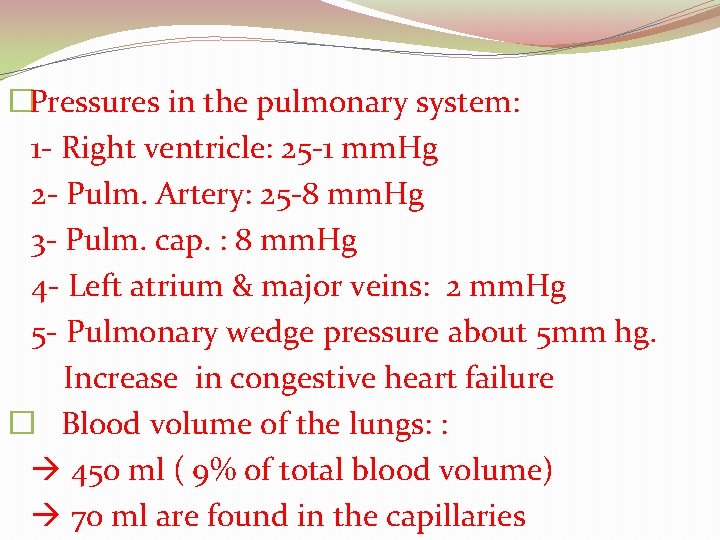
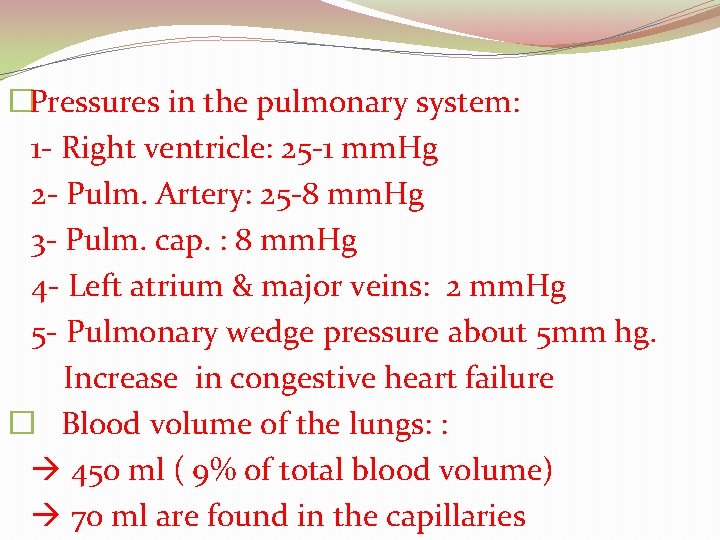
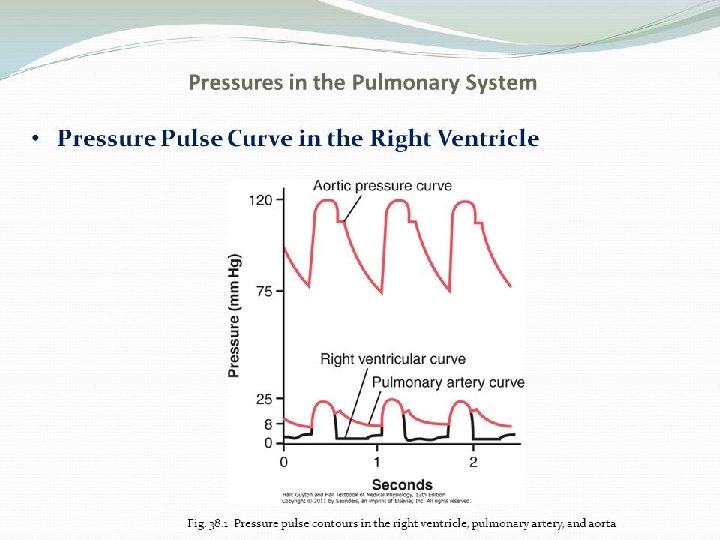
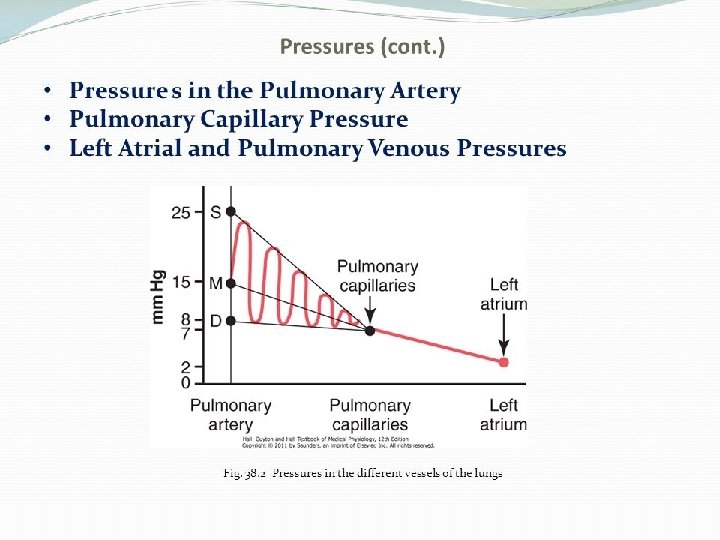
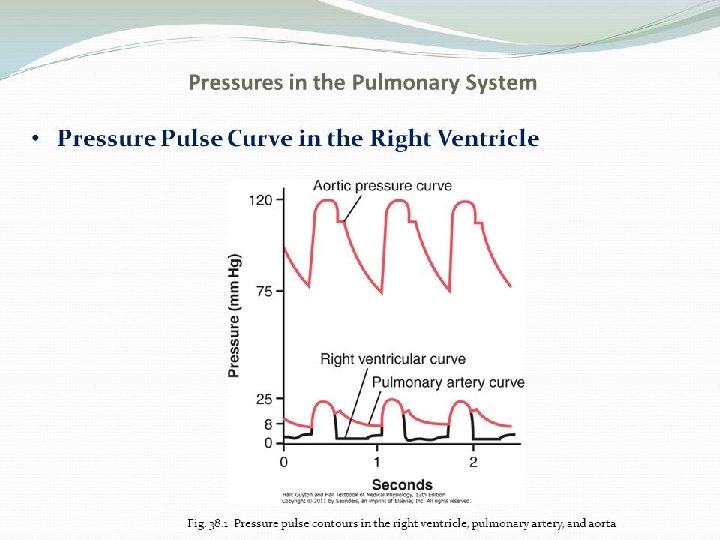
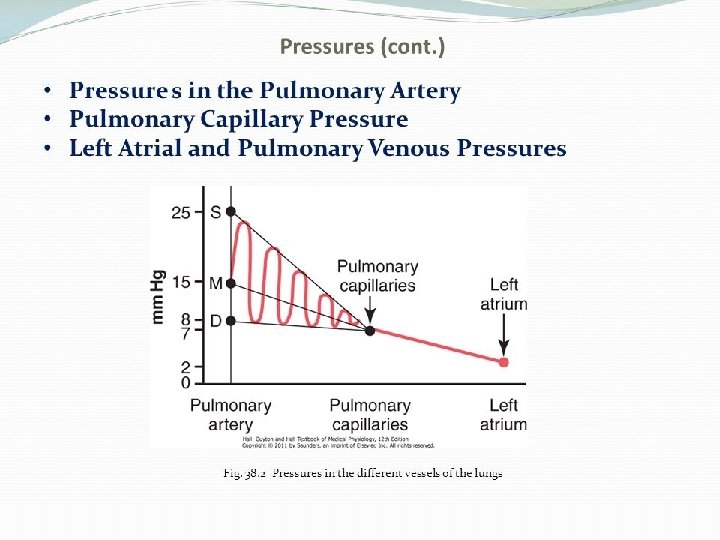
�Pressures in the pulmonary system: 1 - Right ventricle: 25 -1 mm. Hg 2 - Pulm. Artery: 25 -8 mm. Hg 3 - Pulm. cap. : 8 mm. Hg 4 - Left atrium & major veins: 2 mm. Hg 5 - Pulmonary wedge pressure about 5 mm hg. Increase in congestive heart failure � Blood volume of the lungs: : 450 ml ( 9% of total blood volume) 70 ml are found in the capillaries
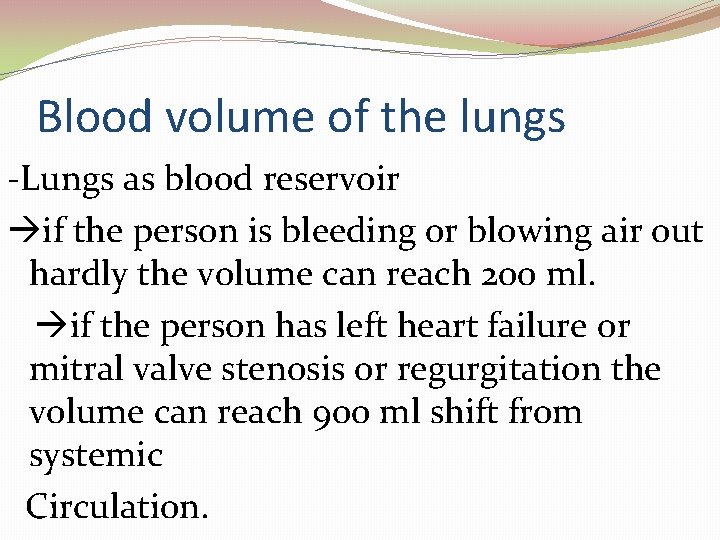
Blood volume of the lungs -Lungs as blood reservoir if the person is bleeding or blowing air out hardly the volume can reach 200 ml. if the person has left heart failure or mitral valve stenosis or regurgitation the volume can reach 900 ml shift from systemic Circulation.
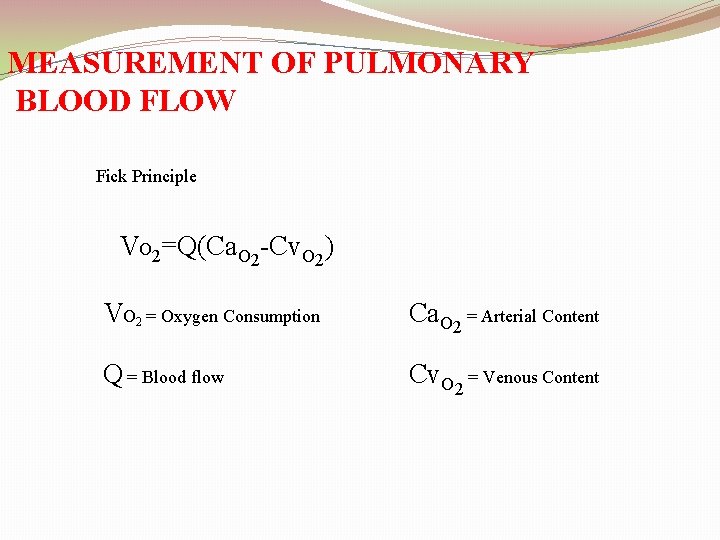
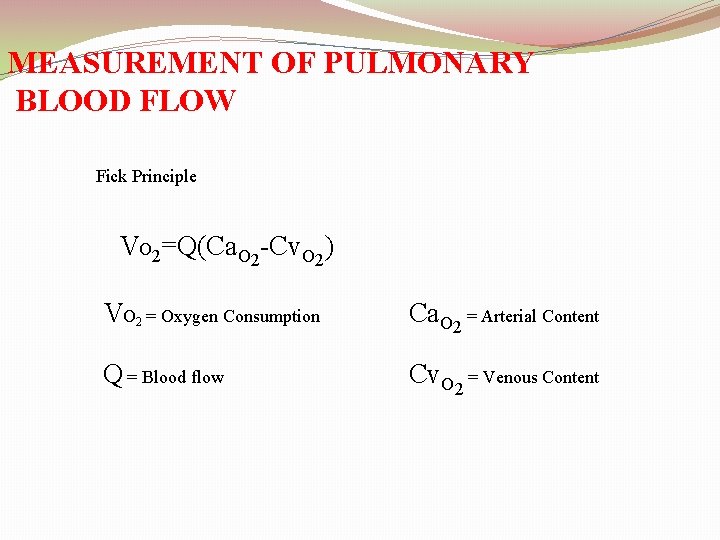
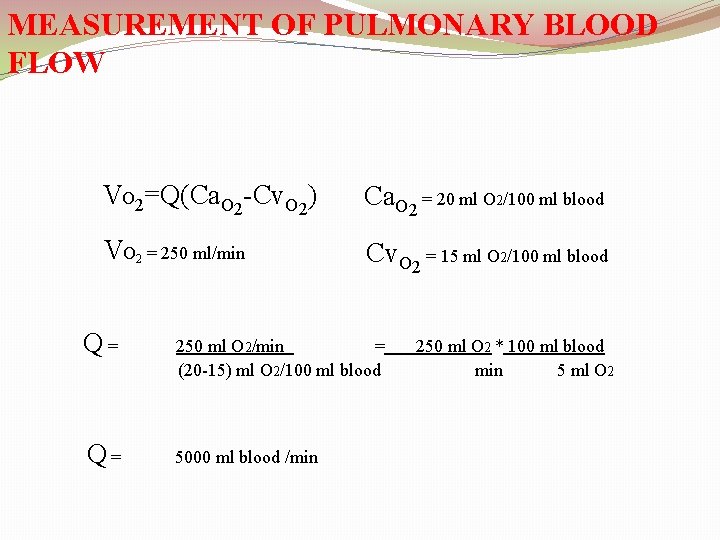
MEASUREMENT OF PULMONARY BLOOD FLOW Fick Principle VO 2=Q(Ca. O 2 -Cv. O 2) VO 2 = Oxygen Consumption Ca. O 2 = Arterial Content Q = Blood flow Cv. O 2 = Venous Content
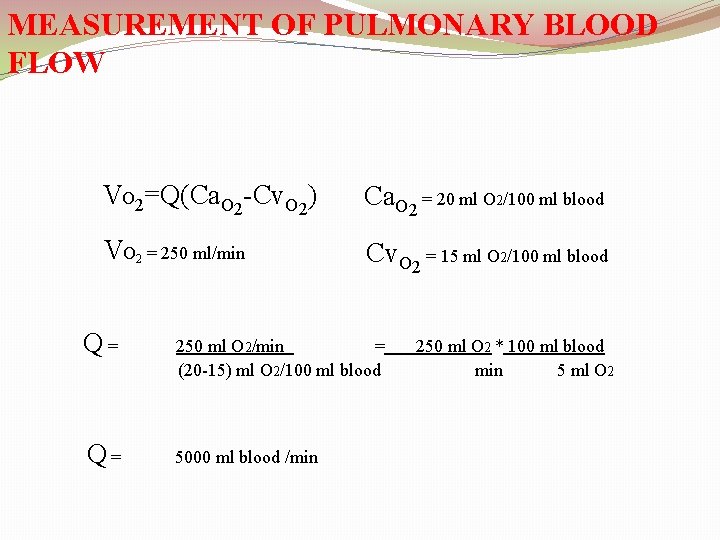
MEASUREMENT OF PULMONARY BLOOD FLOW VO 2=Q(Ca. O 2 -Cv. O 2) Ca. O 2 = 20 ml O 2/100 ml blood VO 2 = 250 ml/min Cv. O 2 = 15 ml O 2/100 ml blood Q= 250 ml O 2/min = (20 -15) ml O 2/100 ml blood Q= 5000 ml blood /min 250 ml O 2 * 100 ml blood min 5 ml O 2
![Blood flow Effect of alveolar O 2 when O 2 decreases below 70 of Blood flow �Effect of alveolar [O 2]: when [O 2] decreases below 70% of](https://slidetodoc.com/presentation_image_h2/beeca8b5d5c4df5f10adc8e4d214a868/image-8.jpg)
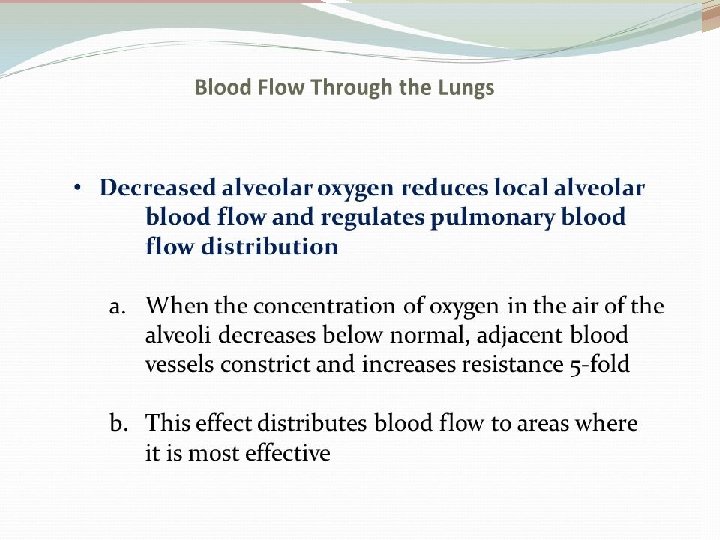
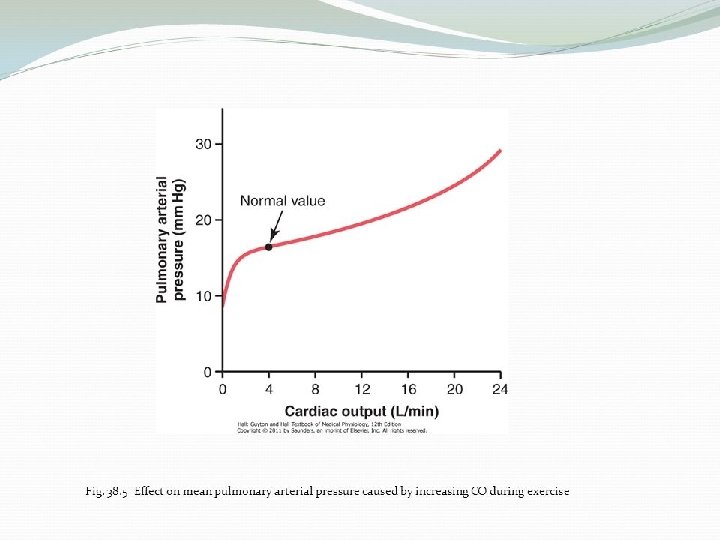
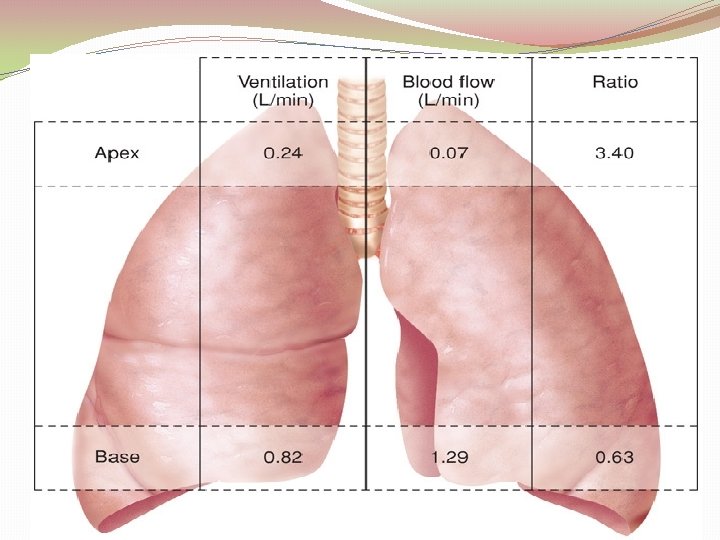
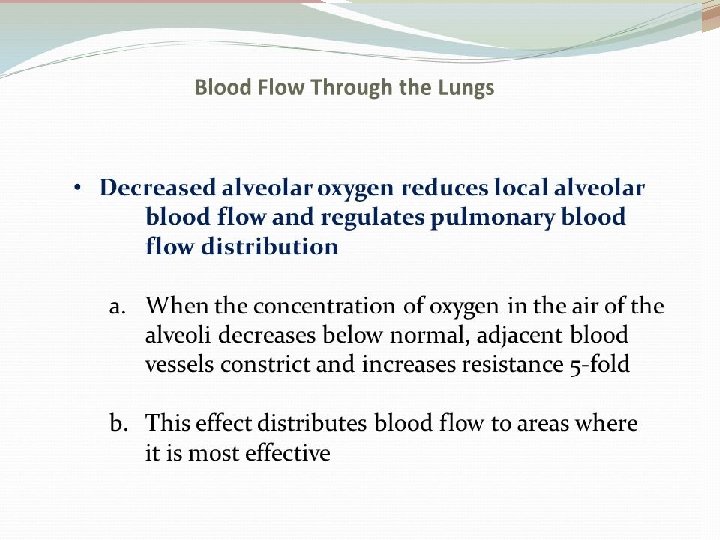
Blood flow �Effect of alveolar [O 2]: when [O 2] decreases below 70% of normal alveolar epithelial cells secrete vasoconstrictors adjacent blood vessels constrict blood flows to better aerated alveoli (extreme low [O 2] 5 x resistance) �Effect of hydrostatic pressure: in normal upright adult there’s a difference between the lowest and highest points of the lung the gradient is 23 mm. Hg (15 mm. Hg above the heart & 8 mm. Hg below it)
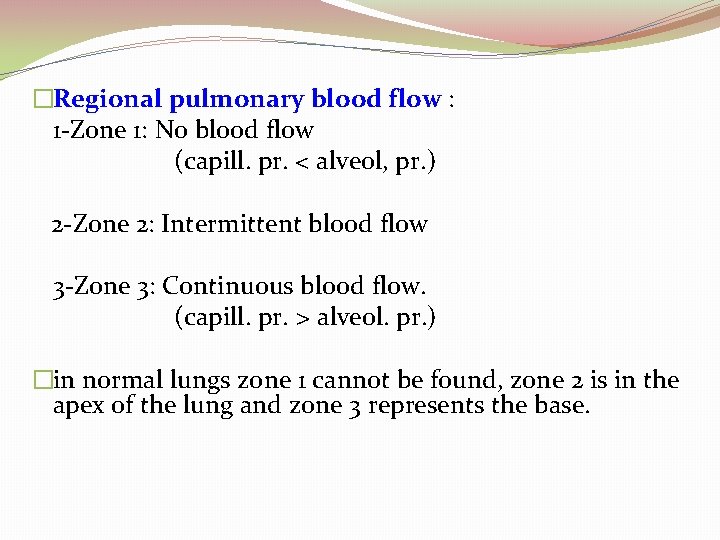
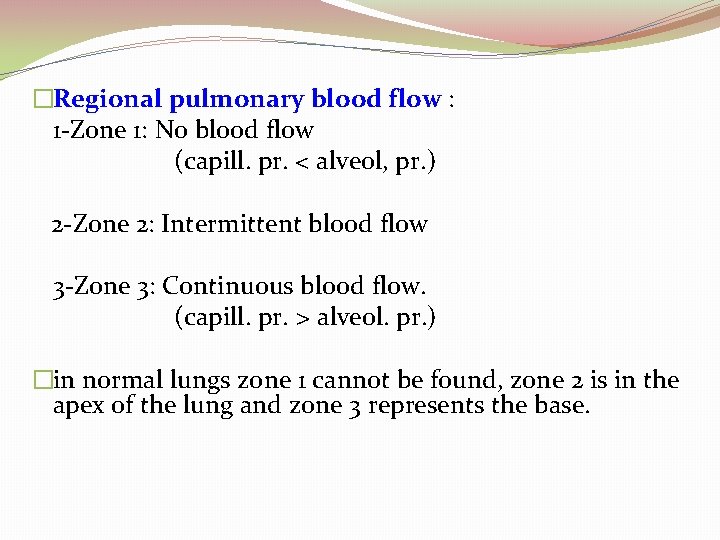
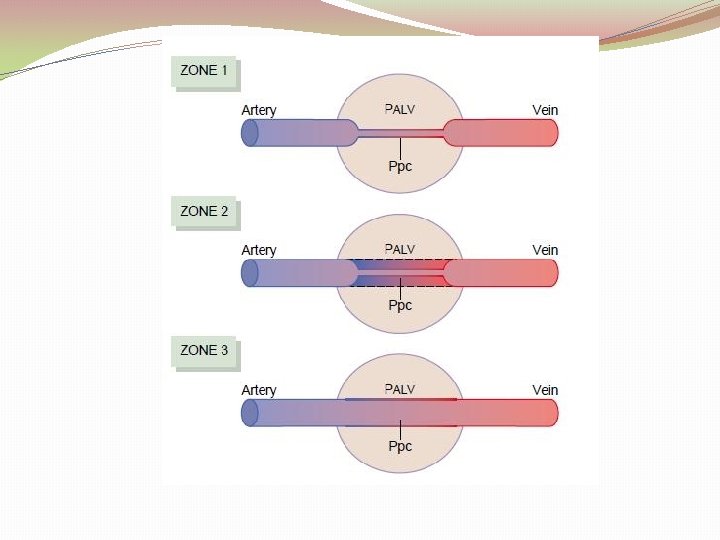
�Regional pulmonary blood flow : 1 -Zone 1: No blood flow (capill. pr. < alveol, pr. ) 2 -Zone 2: Intermittent blood flow 3 -Zone 3: Continuous blood flow. (capill. pr. > alveol. pr. ) �in normal lungs zone 1 cannot be found, zone 2 is in the apex of the lung and zone 3 represents the base.
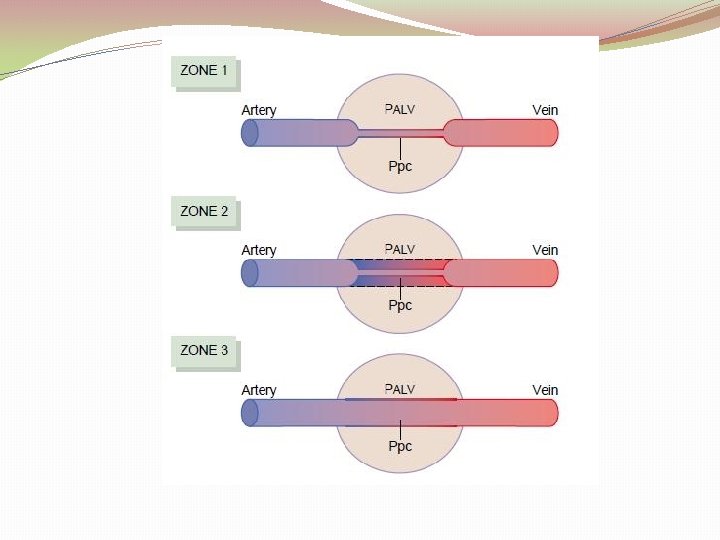
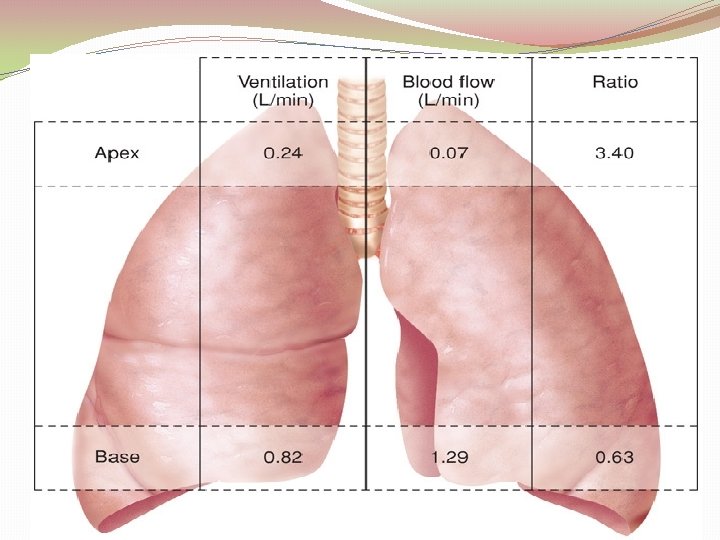
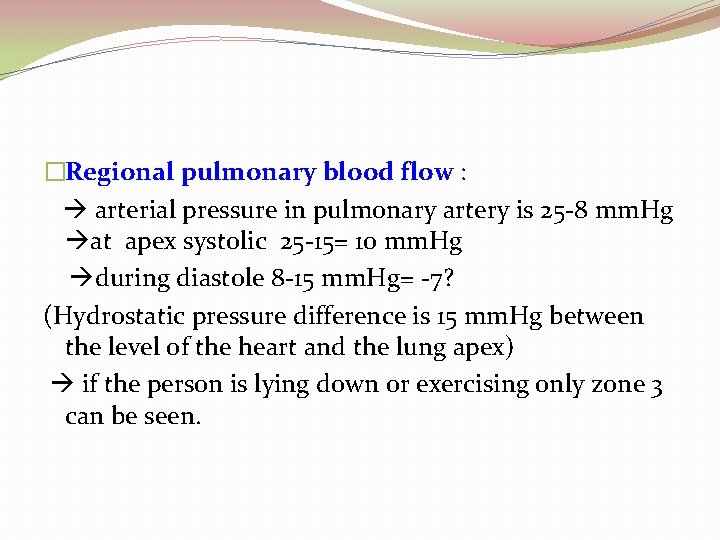
�Regional pulmonary blood flow : arterial pressure in pulmonary artery is 25 -8 mm. Hg at apex systolic 25 -15= 10 mm. Hg during diastole 8 -15 mm. Hg= -7? (Hydrostatic pressure difference is 15 mm. Hg between the level of the heart and the lung apex) if the person is lying down or exercising only zone 3 can be seen.
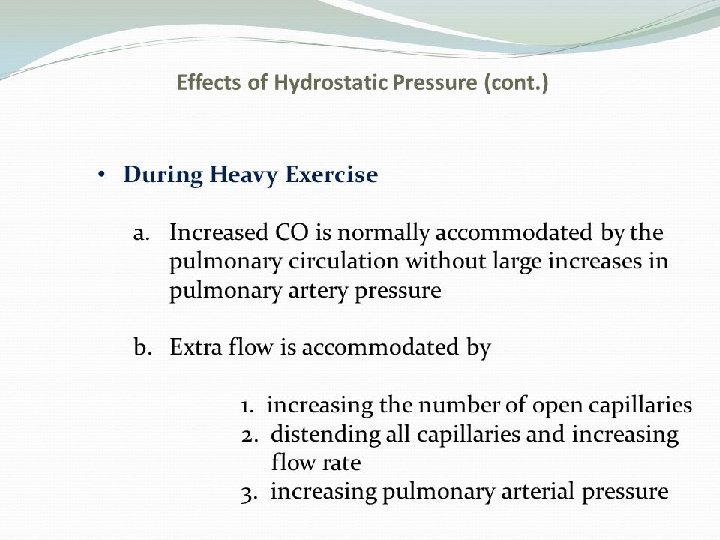
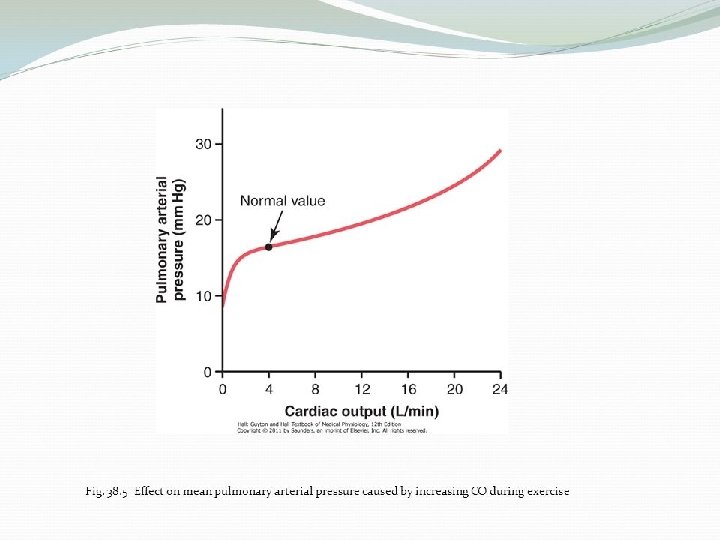
�C. Increase flow to the top by about 700 -800% and � 200 -300% in the lower part because during exercise convert apices from zone 2 to zone 3
�PULMONARY CIRCULATION IN LEFT SIDE HEART FAILURE �When the left atrial pressure increase more than 7 mmhg will cause increase of pulmonary arterial pressure which will increase the load on right ventricle.
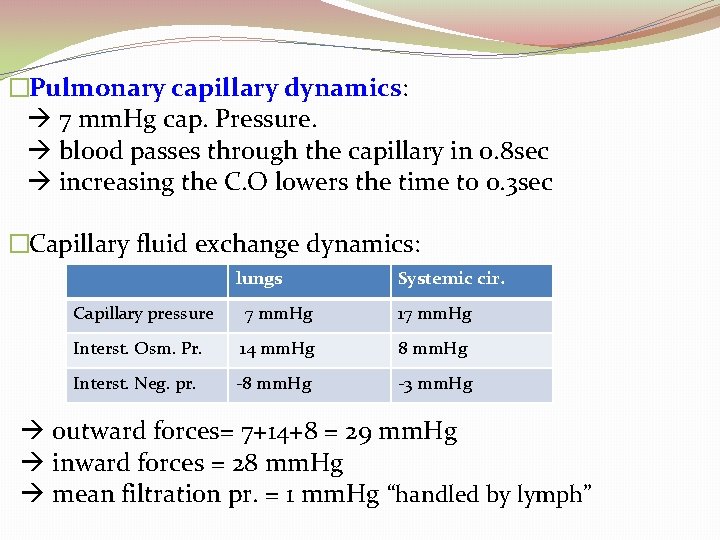
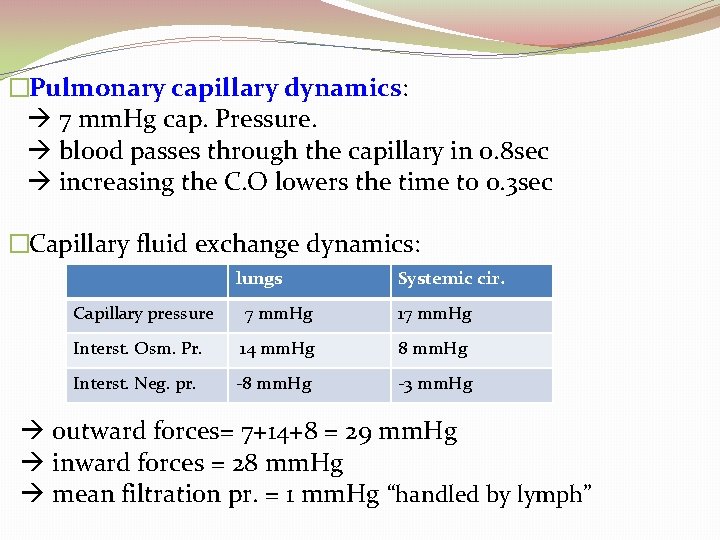
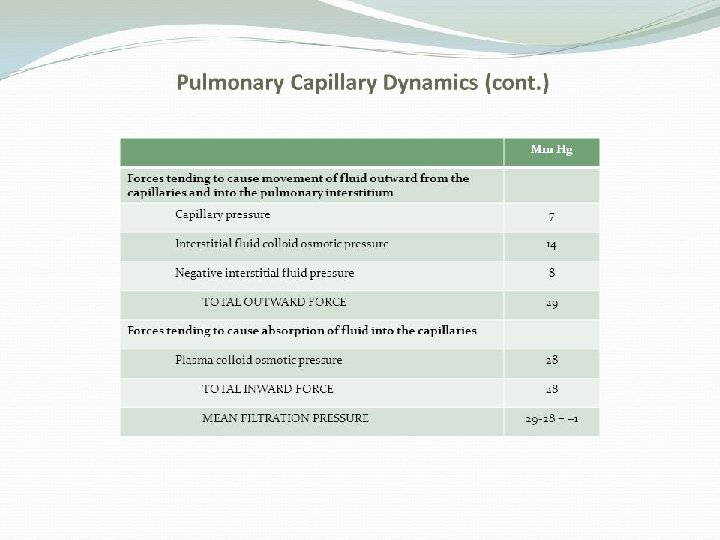
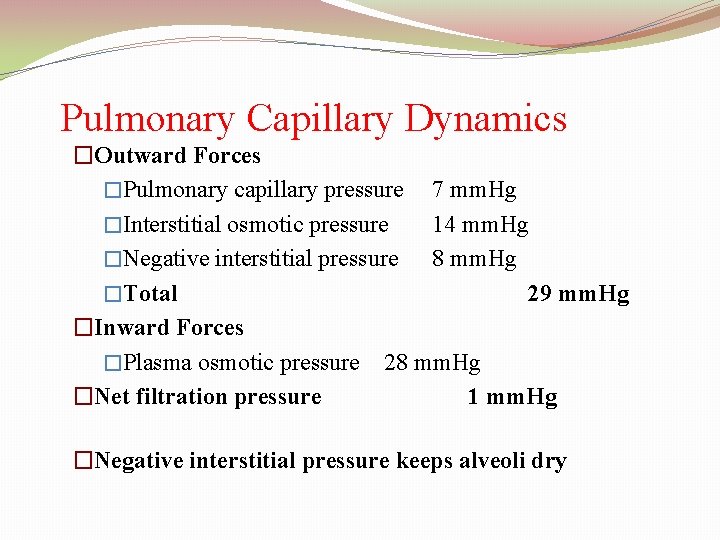
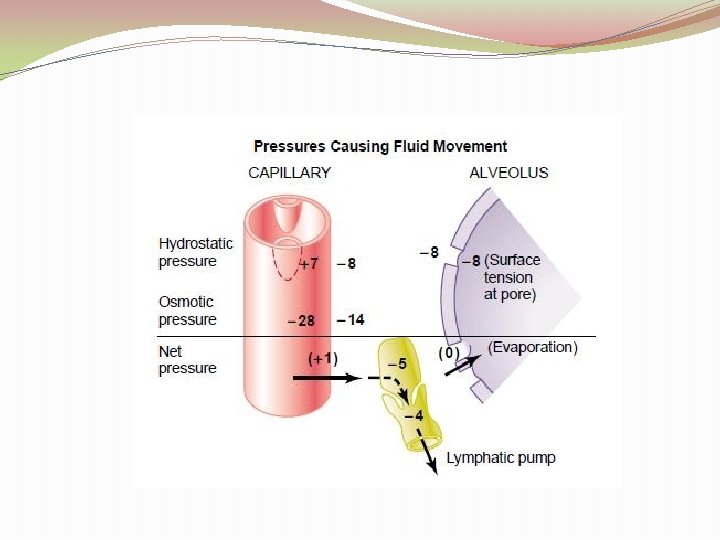
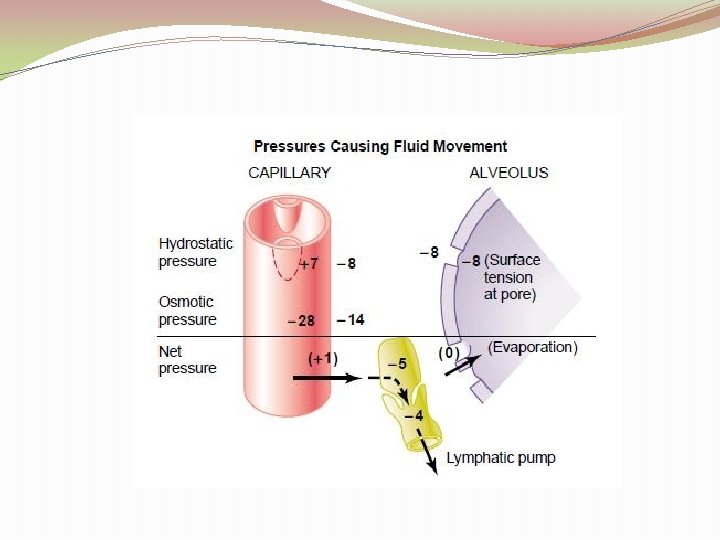
�Pulmonary capillary dynamics: 7 mm. Hg cap. Pressure. blood passes through the capillary in 0. 8 sec increasing the C. O lowers the time to 0. 3 sec �Capillary fluid exchange dynamics: lungs Systemic cir. Capillary pressure 7 mm. Hg 17 mm. Hg Interst. Osm. Pr. 14 mm. Hg 8 mm. Hg Interst. Neg. pr. -8 mm. Hg -3 mm. Hg outward forces= 7+14+8 = 29 mm. Hg inward forces = 28 mm. Hg mean filtration pr. = 1 mm. Hg “handled by lymph”
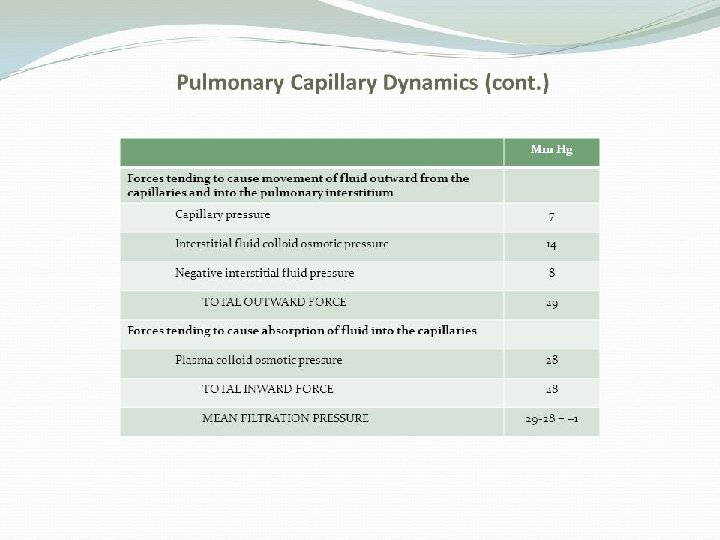
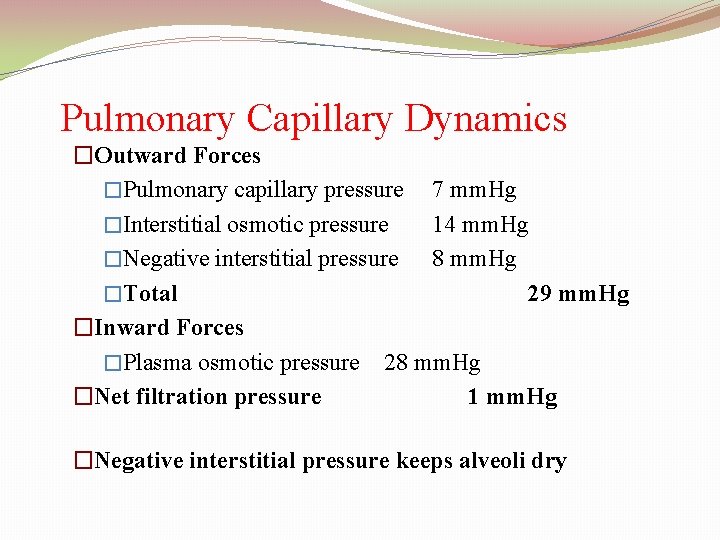
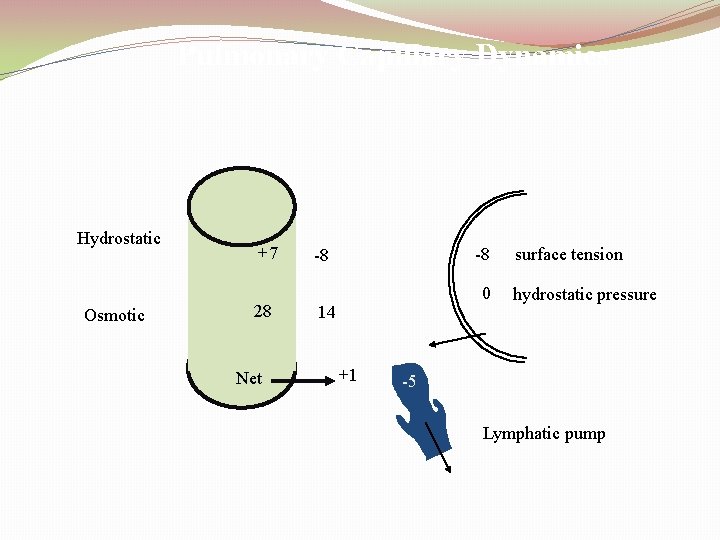
Pulmonary Capillary Dynamics �Outward Forces �Pulmonary capillary pressure 7 mm. Hg �Interstitial osmotic pressure 14 mm. Hg �Negative interstitial pressure 8 mm. Hg �Total 29 mm. Hg �Inward Forces �Plasma osmotic pressure 28 mm. Hg �Net filtration pressure 1 mm. Hg �Negative interstitial pressure keeps alveoli dry
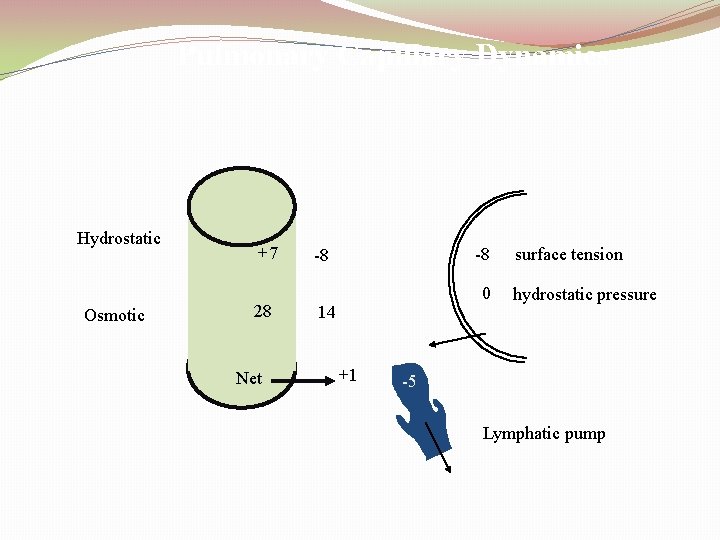
Pulmonary Capillary Dynamics Hydrostatic Osmotic +7 28 Net -8 -8 0 14 +1 surface tension hydrostatic pressure -5 Lymphatic pump
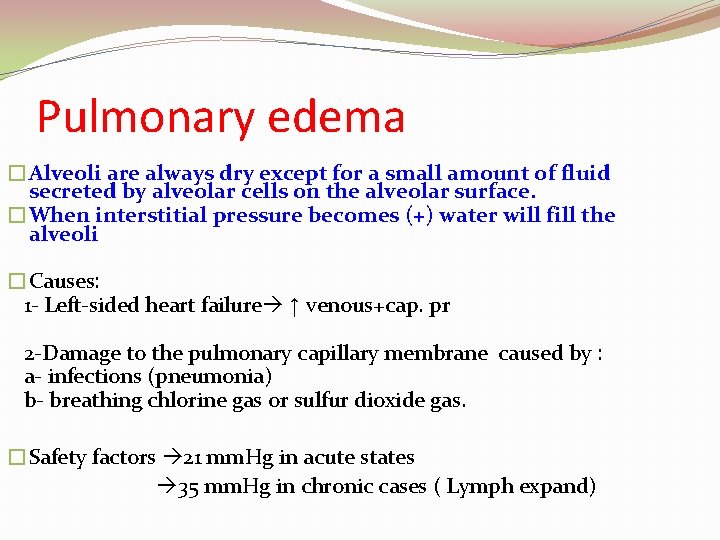
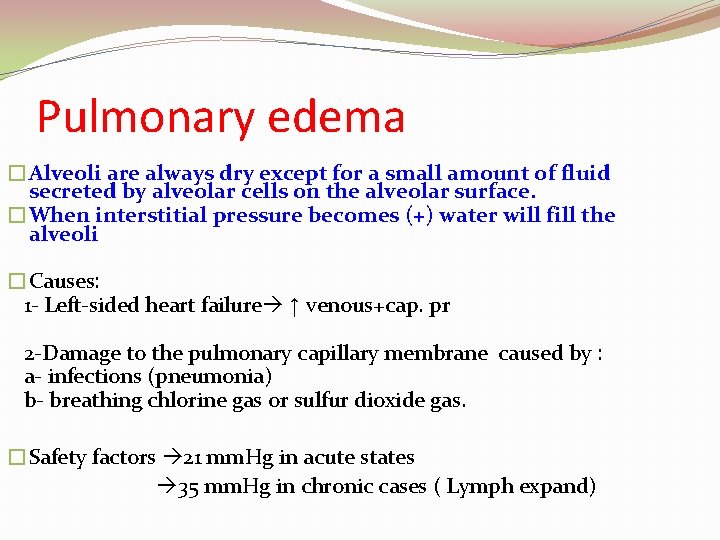
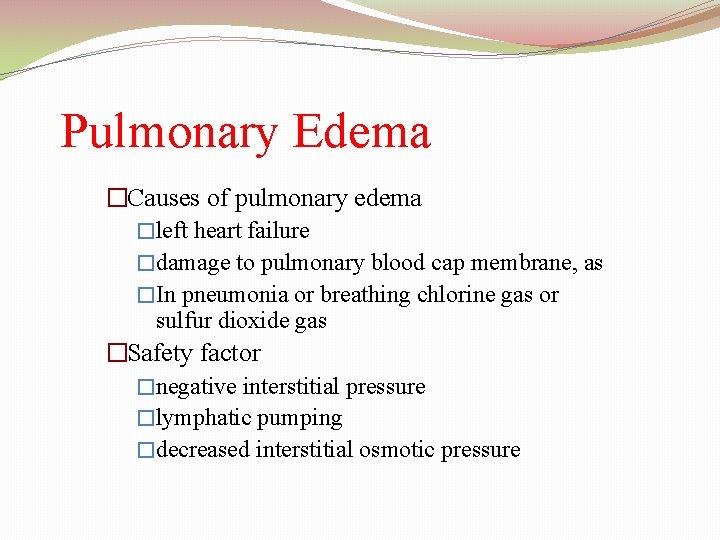
Pulmonary edema �Alveoli are always dry except for a small amount of fluid secreted by alveolar cells on the alveolar surface. �When interstitial pressure becomes (+) water will fill the alveoli �Causes: 1 - Left-sided heart failure ↑ venous+cap. pr 2 -Damage to the pulmonary capillary membrane caused by : a- infections (pneumonia) b- breathing chlorine gas or sulfur dioxide gas. �Safety factors 21 mm. Hg in acute states 35 mm. Hg in chronic cases ( Lymph expand)
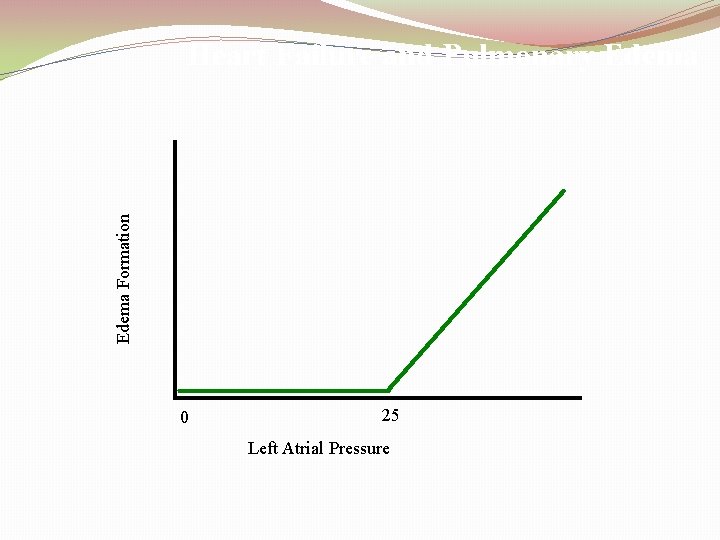
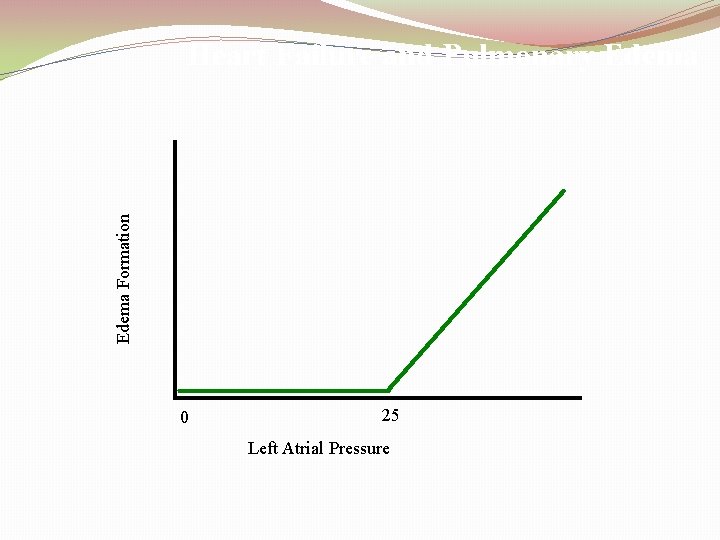
Edema Formation Heart Failure and Pulmonary Edema 0 25 Left Atrial Pressure
Pulmonary Edema �Causes of pulmonary edema �left heart failure �damage to pulmonary blood cap membrane, as �In pneumonia or breathing chlorine gas or sulfur dioxide gas �Safety factor �negative interstitial pressure �lymphatic pumping �decreased interstitial osmotic pressure
PLEURAL EFFUSION �Pleural effusion (edema) : Collection of large free fluid in the pleural space � 1 -Blockage of lymphatic drainage from pleural space � 2 - Cardiac failure (increase peripheral and pulmonary cap pressure) � 3 - Decrease plasma colloid osmotic pressure � 4 - Infection or inflammation of the surface of pleural �cavity