Psychiatric Mental Health Nursing Mood Disorders West Coast
- Slides: 38
Psychiatric / Mental Health Nursing Mood Disorders West Coast University NURS 204
Learning Objectives Compare and contrast the similarities and differences between major depressive disorder and bipolar disorder Describe the elements of the biopsychosocial theories discussed here that contribute most to the current Explain the principles upon which the various biologic therapies for clients with mood disorders are based Systematically conduct a nursing assessment of a client with a mood disorder Implement an understanding of suicide prevention and safety promotion in the plan of care for clients with mood disorders Educate clients and families about biologic treatment for mood disorders such medications and electroconvulsive therapy Assess personal feelings, values, and attitudes toward clients with mood disorders that may provide challenges to professional practice
Mood Disorders Severe and painful sadness Abnormal elation known clinically as a “High” Changes a person’s physical, mental and social being Mood disorders vary in frequency, intensity, and duration Most common psychiatric diagnosis
Major Depression Characterize by a change in several aspects of a person’s life and emotional state consistently throughout at least 14 days Mood state described as down, sad, or feeling “blah” The person experiences one or more episodes of depression with no manic or hypomanic episode Affects twice as many women as men Onset usually occurs in the person’s mid-30’s
Types of Depression Chronic depression Endogenous depression Postpartum depression Seasonal depression Drug-induced depression Psychotic depression Involutional depression Agitated depression Anxious depression
Dysthymic Disorder Chronic depression for the majority of most days for at least 2 years Symptoms are less severe than major depression with fewer physiologic symptoms Predispose people to develop major depression Often occur in childhood and adolescence
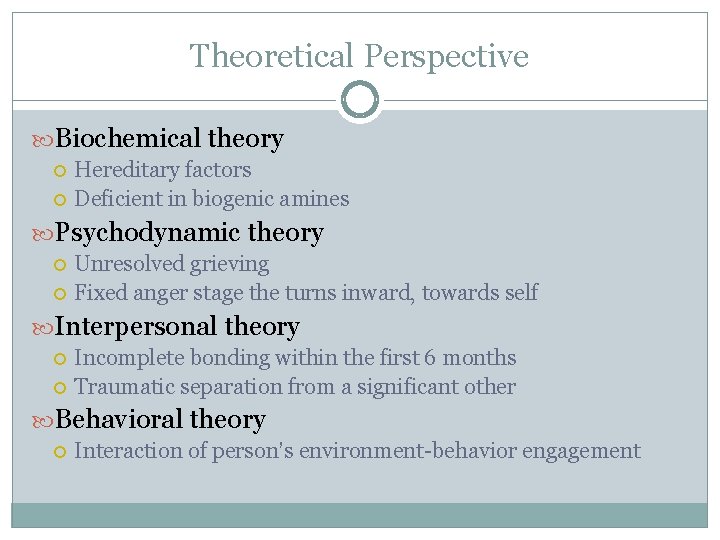
Theoretical Perspective Biochemical theory Hereditary factors Deficient in biogenic amines Psychodynamic theory Unresolved grieving Fixed anger stage the turns inward, towards self Interpersonal theory Incomplete bonding within the first 6 months Traumatic separation from a significant other Behavioral theory Interaction of person’s environment-behavior engagement
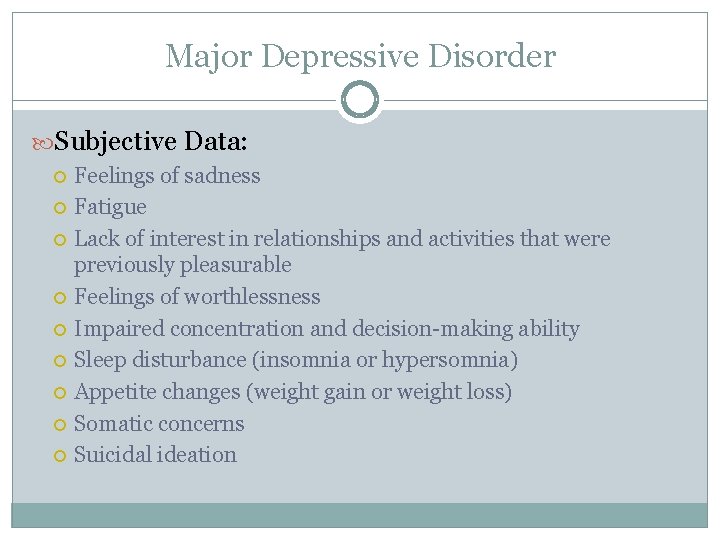
Major Depressive Disorder Subjective Data: Feelings of sadness Fatigue Lack of interest in relationships and activities that were previously pleasurable Feelings of worthlessness Impaired concentration and decision-making ability Sleep disturbance (insomnia or hypersomnia) Appetite changes (weight gain or weight loss) Somatic concerns Suicidal ideation
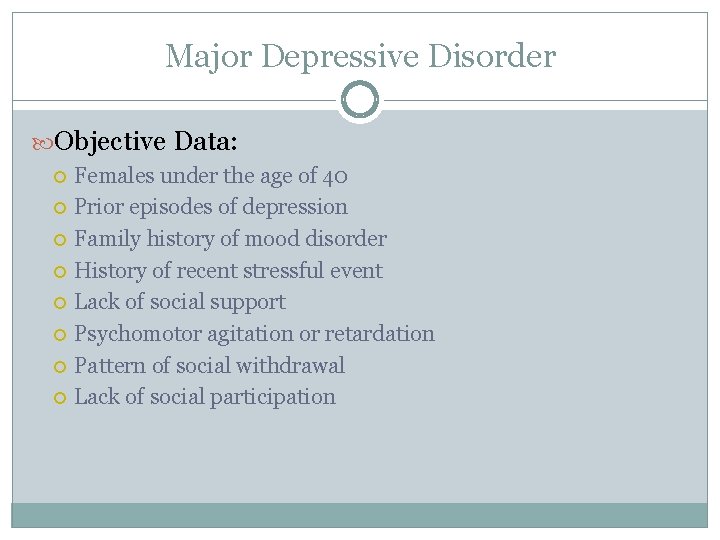
Major Depressive Disorder Objective Data: Females under the age of 40 Prior episodes of depression Family history of mood disorder History of recent stressful event Lack of social support Psychomotor agitation or retardation Pattern of social withdrawal Lack of social participation
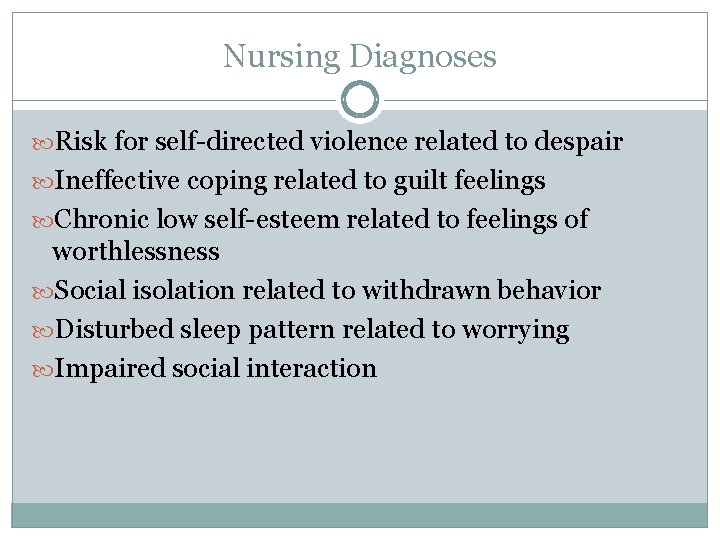
Nursing Diagnoses Risk for self-directed violence related to despair Ineffective coping related to guilt feelings Chronic low self-esteem related to feelings of worthlessness Social isolation related to withdrawn behavior Disturbed sleep pattern related to worrying Impaired social interaction
General Nursing Intervention Identify the patient’s potential for suicide Create a safe environment Formulate verbal contract with patient to notify staff members when feelings begin to get out of control Encourage patient to express anger in acceptable ways Assists patient in recognizing strengths and accomplishments Assist patient in performing activities of daily living
Suicide Prevention Assess for suicide risk by direct questioning about suicidal thinking, history of suicide attempts, and whether the client has a specific suicide plan The more organized the plan is, the more concern it generated as safety is a priority Suicidal clients should be placed under suicide precautions Close staff supervision Remove items such as sharps, belts, shoe laces, mirror etc. No-suicide contract
Dysfunctional Grieving Bereavement is a term that refers to the state of loss Dysfunctional grieving is a term that describes the failure of an individual to follow the course of normal grieving to a point of resolution
Bipolar Disorder Symptoms of at least one episodes of mania, often accompanied by major depressive episodes Bipolar Disorders are a group of mood disorders that include manic episodes, hypomanic episodes, mixed episodes, depressed episodes, and cyclothymic disorder Clients with bipolar disorder experience the elevated mood symptoms seen in mania and hypomania
Types Bipolar I disorder, manic: characterized by elation or irritability with excessive motor activity Bipolar I disorder, mixed: characterized by mood swings ranging from depression to euphoria, with intervening periods of normal behavior Bipolar II disorder: characterized by no manic or mixed episode but at least one hypomanic episode Cyclothymic disorder: characterized by a chronic, fluctuating mood disturbance with frequent periods of hypomania and depression
Theoretical Perspective Biological theory: Genetic predisposition exists Increased levels of norepinephrine Psychoanalytic theory: Cyclic behaviors of depression and mania are responses to conditional love from the significant caregiver Ego development is disruptive because the child is in a dependent role, resulting in a punitive superego or strong id
Myths and Facts Myth: People with bipolar disorder can’t get better or lead a normal life. Fact: Many people with bipolar disorder have successful careers, happy family lives, and satisfying relationships. Living with bipolar disorder is challenging. But with treatment, healthy coping skills, and a solid support system, people can live fully while managing symptoms. Myth: People with bipolar disorder swing back and forth between mania and depression. Fact: Some people alternate between extreme episodes of mania and depression, but most are depressed more often than they are manic. Mania may also be so mild that it goes unrecognized. People with bipolar disorder can also go for long stretches without symptoms.
Myths and Facts Myth: Bipolar disorder only affects mood. Fact: Bipolar disorder also affects your energy level, judgment, memory, concentration, appetite, sleep patterns, sex drive, and self-esteem. Additionally, bipolar disorder has been linked to anxiety, substance abuse, and health problems such as diabetes, heart disease, migraines, and high blood pressure. Myth: Aside from taking medication, there is nothing you can do to control bipolar disorder. Fact: While medication is the foundation of bipolar disorder treatment, therapy and self-help strategies also play important roles. You can help control your symptoms by exercising regularly, getting enough sleep, eating right, monitoring your moods, keeping stress to a minimum, and surrounding yourself with supportive people.
Nursing Diagnosis Risk for injury related to agitation Ineffective health maintenance related to hyperactivity Disturbed sleep pattern related to restlessness Self-care deficit related to inattention to personal needs Impaired social interaction related to decreased attention span Disturbed thought process related to the psychotic process
Nursing Interventions Reduce environmental stimuli Limit patient’s participation in group activities Create a safe environment Provide physical exercise as a substitute for increased motor activity Avoid arguments or confrontations with the patient Restrict caffeine intake Limit the selection of clothing available Keep the patient oriented to reality Assist patient in focusing on a single task
Psychopharmacology Antidepressants: Possible indications Depression Eating disorder Chronic pain Panic disorder Enuresis Obsessive compulsive disorder (OCD) Generalized anxiety disorder (GAD) Post traumatic stress disorder (PTSD) Pre-menstural syndrome (PMS)
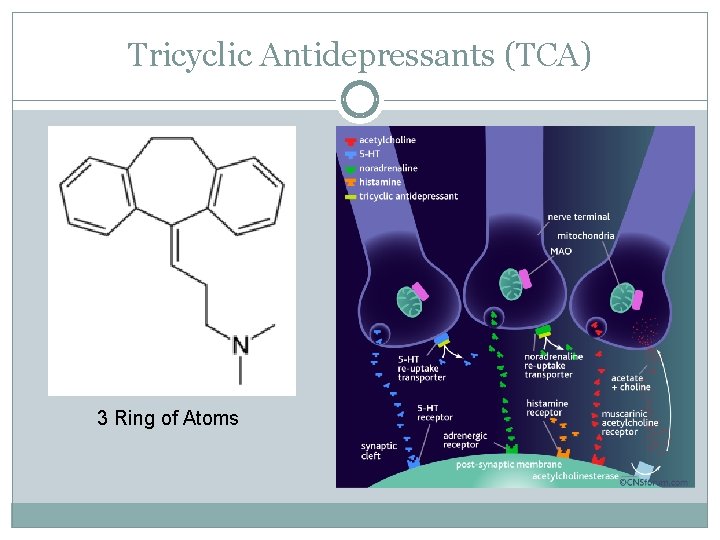
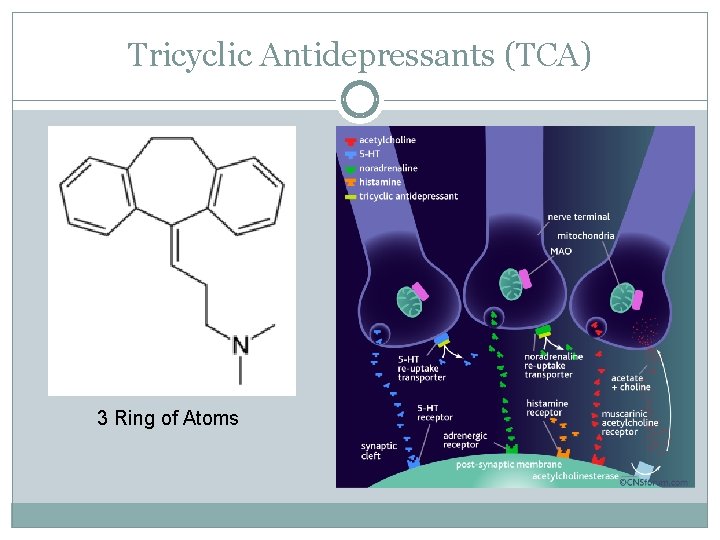
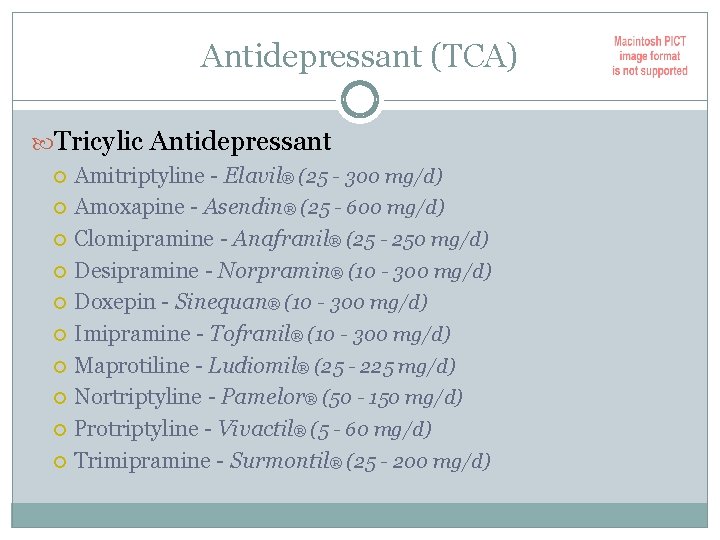
Tricyclic Antidepressants (TCA) 3 Ring of Atoms
Antidepressant (TCA) Tricylic Antidepressant Amitriptyline - Elavil® (25 - 300 mg/d) Amoxapine - Asendin® (25 - 600 mg/d) Clomipramine - Anafranil® (25 - 250 mg/d) Desipramine - Norpramin® (10 - 300 mg/d) Doxepin - Sinequan® (10 - 300 mg/d) Imipramine - Tofranil® (10 - 300 mg/d) Maprotiline - Ludiomil® (25 - 225 mg/d) Nortriptyline - Pamelor® (50 - 150 mg/d) Protriptyline - Vivactil® (5 - 60 mg/d) Trimipramine - Surmontil® (25 - 200 mg/d)
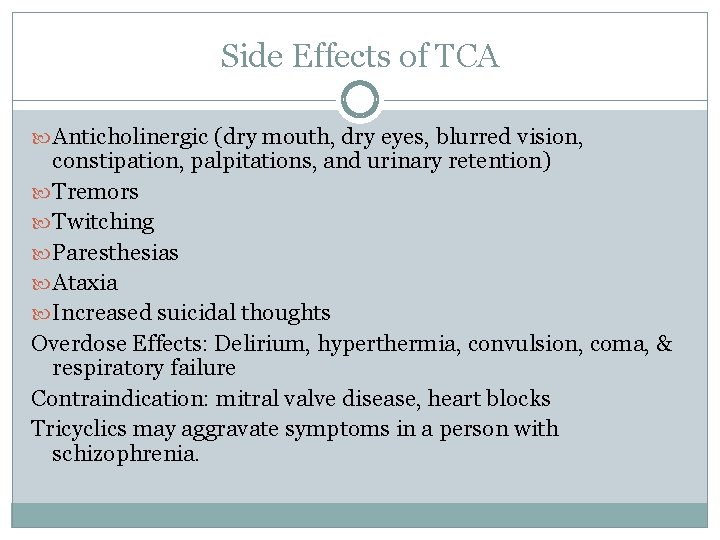
Side Effects of TCA Anticholinergic (dry mouth, dry eyes, blurred vision, constipation, palpitations, and urinary retention) Tremors Twitching Paresthesias Ataxia Increased suicidal thoughts Overdose Effects: Delirium, hyperthermia, convulsion, coma, & respiratory failure Contraindication: mitral valve disease, heart blocks Tricyclics may aggravate symptoms in a person with schizophrenia.
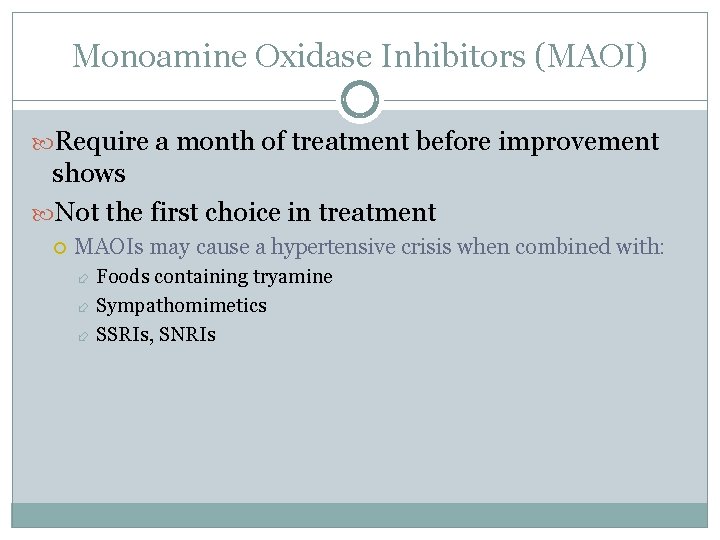
Monoamine Oxidase Inhibitors (MAOI) Require a month of treatment before improvement shows Not the first choice in treatment MAOIs may cause a hypertensive crisis when combined with: Foods containing tryamine Sympathomimetics SSRIs, SNRIs
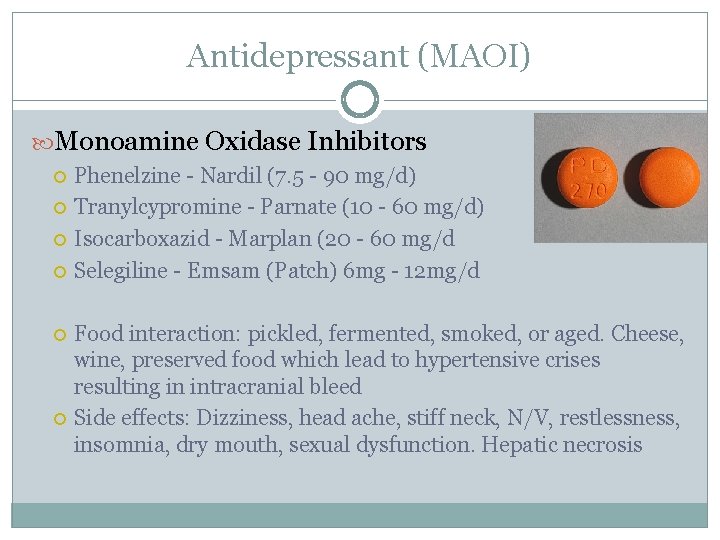
Antidepressant (MAOI) Monoamine Oxidase Inhibitors Phenelzine - Nardil (7. 5 - 90 mg/d) Tranylcypromine - Parnate (10 - 60 mg/d) Isocarboxazid - Marplan (20 - 60 mg/d Selegiline - Emsam (Patch) 6 mg - 12 mg/d Food interaction: pickled, fermented, smoked, or aged. Cheese, wine, preserved food which lead to hypertensive crises resulting in intracranial bleed Side effects: Dizziness, head ache, stiff neck, N/V, restlessness, insomnia, dry mouth, sexual dysfunction. Hepatic necrosis
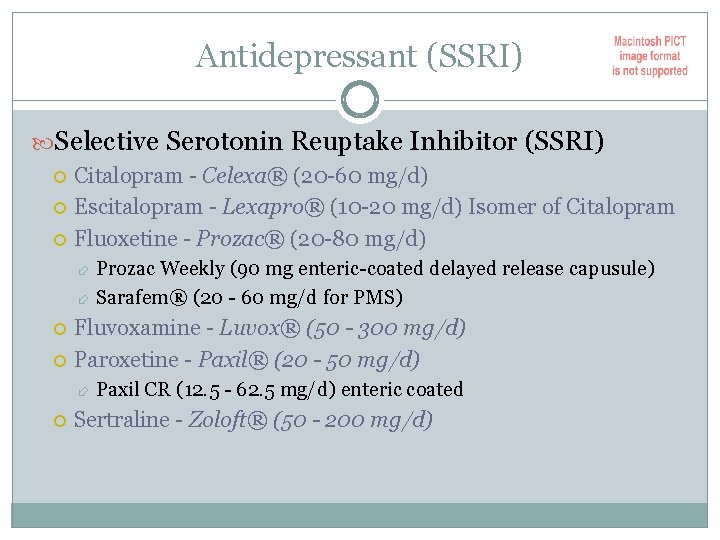
Antidepressant (SSRI) Selective Serotonin Reuptake Inhibitor (SSRI) Citalopram - Celexa® (20 -60 mg/d) Escitalopram - Lexapro® (10 -20 mg/d) Isomer of Citalopram Fluoxetine - Prozac® (20 -80 mg/d) Prozac Weekly (90 mg enteric-coated delayed release capusule) Sarafem® (20 - 60 mg/d for PMS) Fluvoxamine - Luvox® (50 - 300 mg/d) Paroxetine - Paxil® (20 - 50 mg/d) Paxil CR (12. 5 - 62. 5 mg/d) enteric coated Sertraline - Zoloft® (50 - 200 mg/d)
Antidepressant (SSRI) Possible Side Effects Nausea and Vomiting Nervousness Insomnia Somnolence Constipation Sexual dysfunction
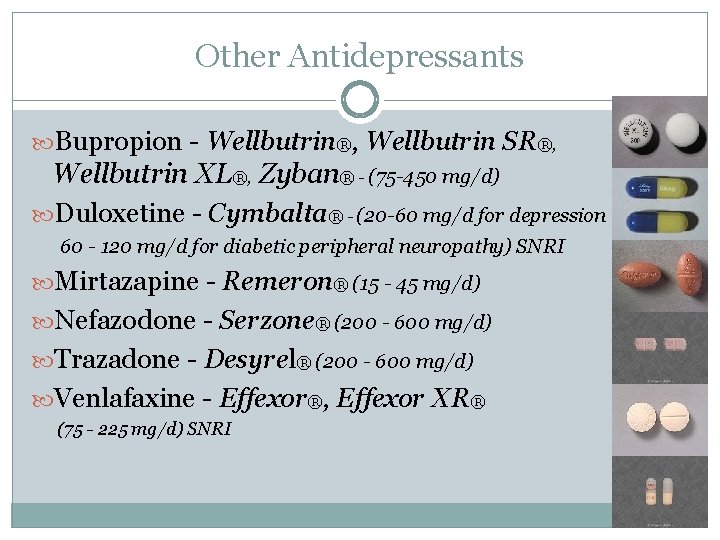
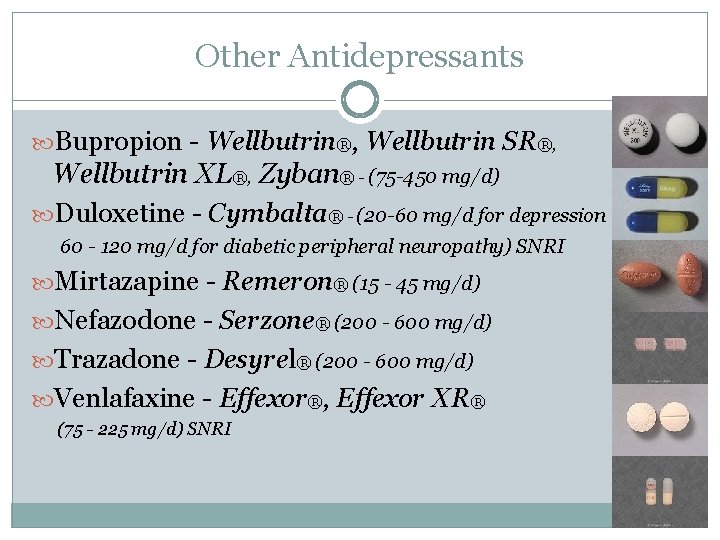
Other Antidepressants Bupropion - Wellbutrin®, Wellbutrin SR®, Wellbutrin XL®, Zyban® - (75 -450 mg/d) Duloxetine - Cymbalta® - (20 -60 mg/d for depression 60 - 120 mg/d for diabetic peripheral neuropathy) SNRI Mirtazapine - Remeron® (15 - 45 mg/d) Nefazodone - Serzone® (200 - 600 mg/d) Trazadone - Desyrel® (200 - 600 mg/d) Venlafaxine - Effexor®, Effexor XR® (75 - 225 mg/d) SNRI
Serotonin Syndrome Mild in most people, recovery within 24 - 72 hours, although it can cause death under circumstances Seen in people taking two or more medications that increase levels of serotonin in the CNS Symptoms: 3 of the following must be present Mental status changes Agitation Myoclonus Shivering Hyperreflexia Ataxia Diaphoresis hyperpyrexia
Management and Prevention of Serotonin Syndrome Supportive measures Discontinue medication Provide benzodiazepine Anti-serotonergic agents: Periactin, Sansert, Inderal Dantrium for relieving muscle rigidity and hyperthermia
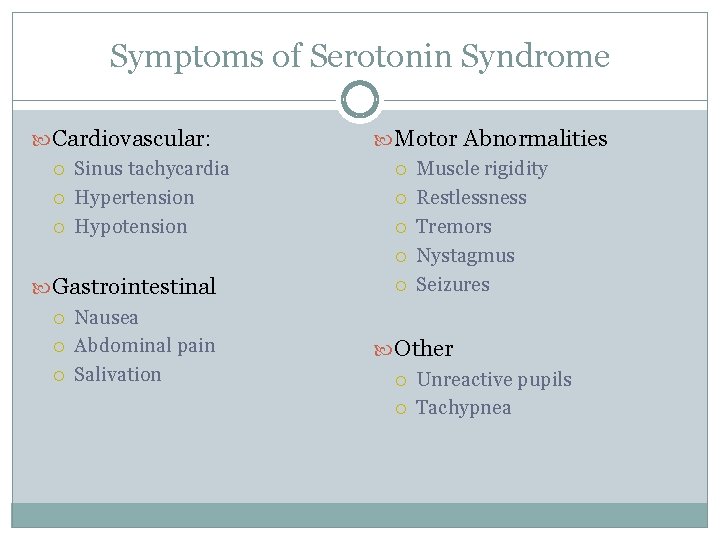
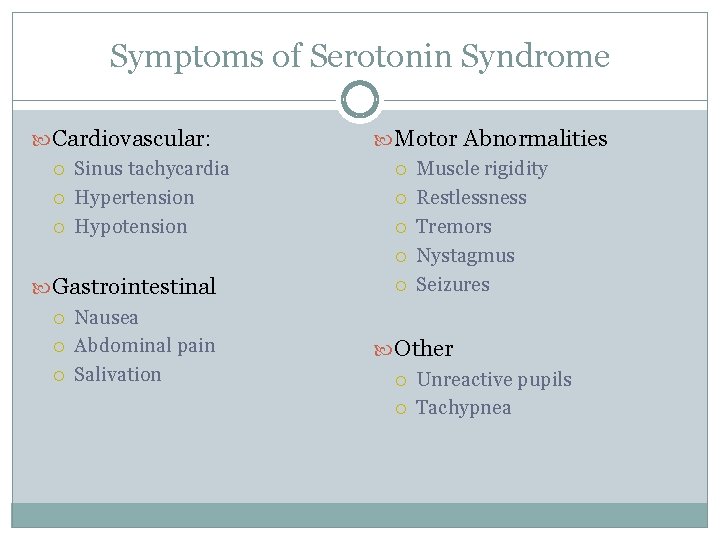
Symptoms of Serotonin Syndrome Cardiovascular: Sinus tachycardia Hypertension Hypotension Gastrointestinal Nausea Abdominal pain Salivation Motor Abnormalities Muscle rigidity Restlessness Tremors Nystagmus Seizures Other Unreactive pupils Tachypnea
Mood Stabilizers Antimanic Agents Lithium Carbonate (300 - 2, 400 mg/d) Eskalith® - fast release capsule Lithotab® - fast release tablet Lithobid, Eskalith CR® - sustained release tablet Lithium Citrate - (liquid formulation 5 ml = 8 m. Eq = 300 mg of Lithium Carbonate) Symptoms of Li Toxicity Levels > 1. 2 m. Eq/L - Course hand tremors, nausea, vomiting, diarrhea, confusion, ataxia, slurred speech, lethargy, thirst and polyuria Levels > 2. 0 to 3. 0 m. Eq/L - Profound CNS depression, arrythmia, seizures, coma
Mood Stabilizer Divalproex Sodium - Depakote® - (enteric coated) Valproic Acid Syrup - Depakene syrup Valproic Acid - Depakene (250 - 1, 500 mg/d) Side effects: GI distress N/V/D - give with food Drowsiness -give at bedtime Tremor Alopecia - zinc and selenium supplements Weight gain - diet and regular exercise Black box warnings: Hepatoxity, pancreatitis, teratogenicity
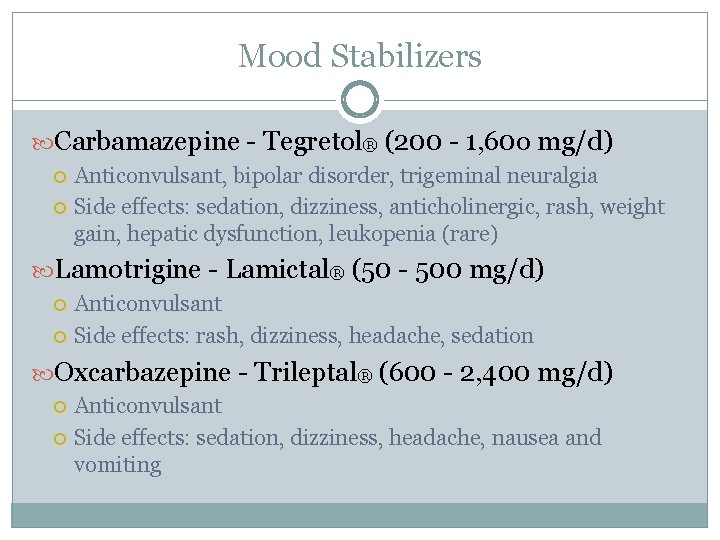
Mood Stabilizers Carbamazepine - Tegretol® (200 - 1, 60 o mg/d) Anticonvulsant, bipolar disorder, trigeminal neuralgia Side effects: sedation, dizziness, anticholinergic, rash, weight gain, hepatic dysfunction, leukopenia (rare) Lamotrigine - Lamictal® (50 - 500 mg/d) Anticonvulsant Side effects: rash, dizziness, headache, sedation Oxcarbazepine - Trileptal® (600 - 2, 400 mg/d) Anticonvulsant Side effects: sedation, dizziness, headache, nausea and vomiting
Medication Teaching Proper client education enhances the effectiveness of medication therapy and can improve client adherence and diminish non-adherence Client education begins when medication therapy begins and is repeated during the course of the client’s hospitalization Give instructions verbally and in writing Include family members or significant others if they will supervise home administration
Electroconvulsive Therapy (ECT) Treatment procedure during which an electric current is passed through the brain. Unilateral or bilateral Indication: severe depression, acute mania, psychotic symptoms, acutely suicidal Treatment is 3 times a week until the course of 12 treatments is completed Causes generalized seizure (tonic-clonic) Contraindication: ICP and recent MI Side effects: transient short-term memory loss Not a cure
Working with Clients Receiving ECT Consent forms completed Keep pt NPO for at least 4 hours Ask the patient to void and remove contact lenses, jewelry, hairpins, and dentures prior to treatment Assess vital signs Medications: Robinul®, Brevital®, Anectine® Recovery: lateral recumbent position, orient to time, place and situation Offer food Offer medication for Headache
 Chapter 11 psychiatric mental health nursin
Chapter 11 psychiatric mental health nursin Conclusion of nursing process
Conclusion of nursing process Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Neurosis vs psychosis
Neurosis vs psychosis Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Mental health disorders
Mental health disorders Gulf coast center angleton texas
Gulf coast center angleton texas Mental health nursing definition according to who
Mental health nursing definition according to who History of psychiatric nursing
History of psychiatric nursing Remalteon
Remalteon Ethical and legal issues in psychiatric nursing
Ethical and legal issues in psychiatric nursing Defense mechanisms nursing
Defense mechanisms nursing West cork mental health services bantry
West cork mental health services bantry Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy questions and answers
Mental health jeopardy questions and answers Mood disorders
Mood disorders Conclusion of community mental health nursing
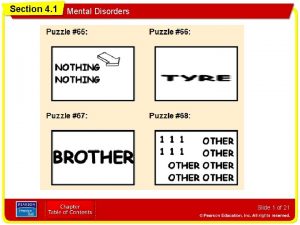
Conclusion of community mental health nursing Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Glencoe health chapter 5 assessment answers
Glencoe health chapter 5 assessment answers Chapter 5 lesson 4 getting help answer key
Chapter 5 lesson 4 getting help answer key Thought broadcasting
Thought broadcasting West coast officials
West coast officials West coast officials
West coast officials West coast officials association
West coast officials association Vegetation zone
Vegetation zone West coast neurology
West coast neurology Marine west coast
Marine west coast Characteristics of monsoon climate
Characteristics of monsoon climate Qad west coast user group
Qad west coast user group Ap style northeast
Ap style northeast West coast national park marine protected area
West coast national park marine protected area West coast windings
West coast windings West coast musculoskeletal
West coast musculoskeletal Portugal europe's west coast
Portugal europe's west coast Ocean west coast
Ocean west coast Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Myringotomy incision
Myringotomy incision Who analgesic ladder
Who analgesic ladder