Primary Sclerosing Cholangitis and Cholangiocarcinoma A Multidisciplinary Approach






- Slides: 59
Primary Sclerosing Cholangitis and Cholangiocarcinoma A Multidisciplinary Approach KV Narayanan Menon, MD, FRCP, FAASLD Medical Director of Liver Transplantation Digestive Disease Institute Cleveland Clinic
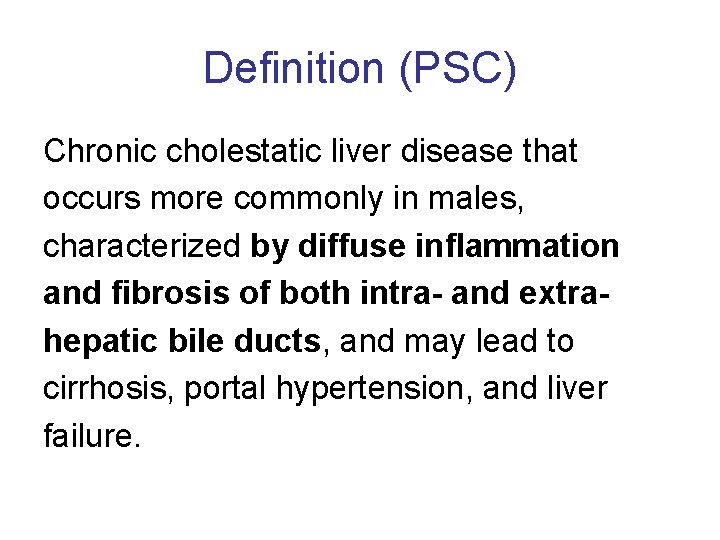
Definition (PSC) Chronic cholestatic liver disease that occurs more commonly in males, characterized by diffuse inflammation and fibrosis of both intra- and extrahepatic bile ducts, and may lead to cirrhosis, portal hypertension, and liver failure.
Diagnosis of PSC • Cholestatic biochemical profile • Characteristic cholangiography (multifocal strictures with segmental dilatations) • Exclusion of secondary causes • Autoantibodies have no role in the diagnosis of PSC
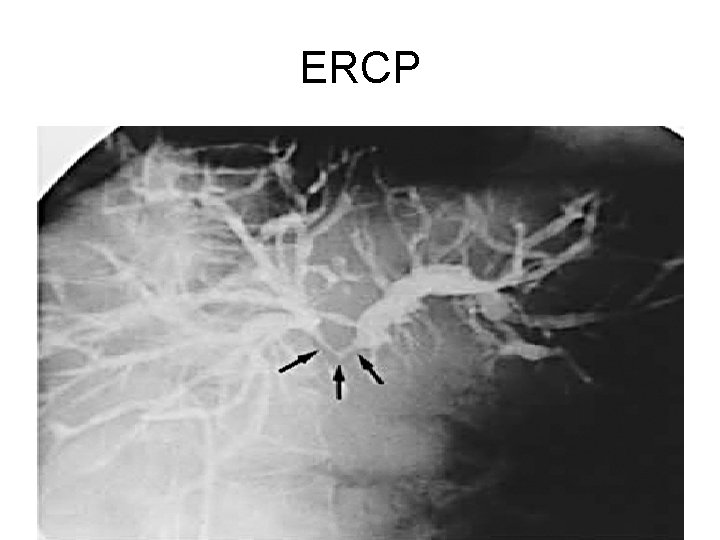
Imaging - MRCP : Sensitivity is around 80% and specificity is around 87% Early changes may be missed on MRCP and ERCP may be necessary A small group of paitents may not have extrahepatic disease (25%) Very unusual to get only extrahepatic disease (<5%)
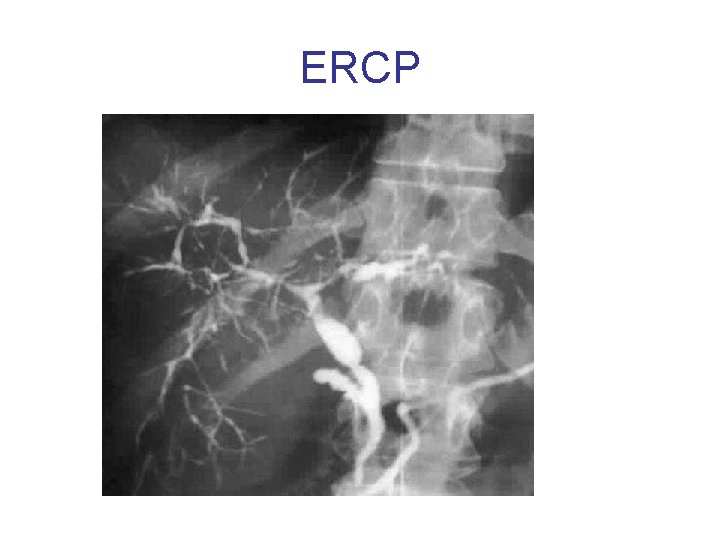
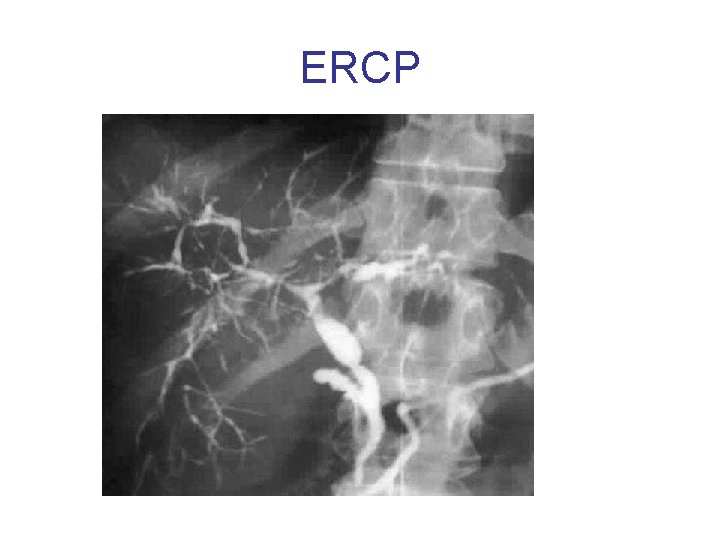
ERCP
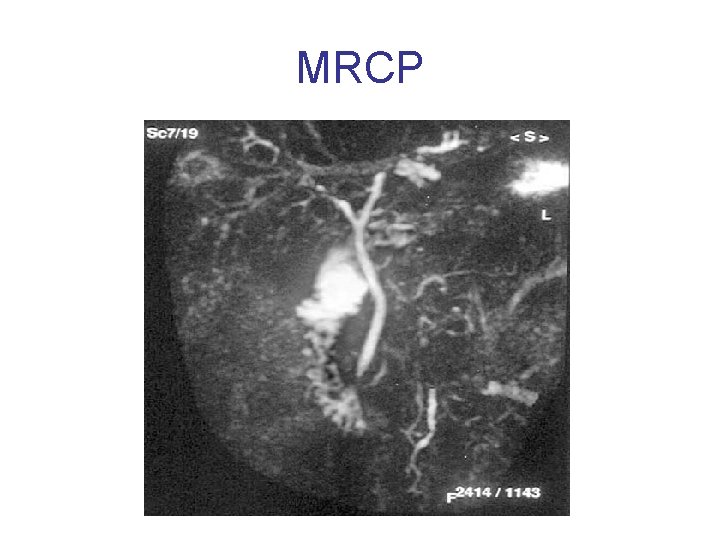
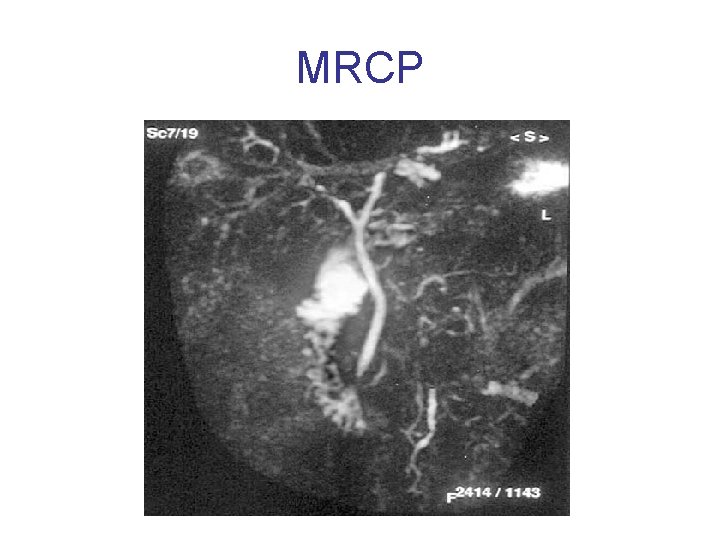
MRCP
Liver Biopsy • Not essential for the diagnosis of PSC • Classic periductal “onion peel” is seen infrequently in liver biopsy • Useful in – Determining stage of fibrosis – Presence of overlap such as autoimmune hepatitis
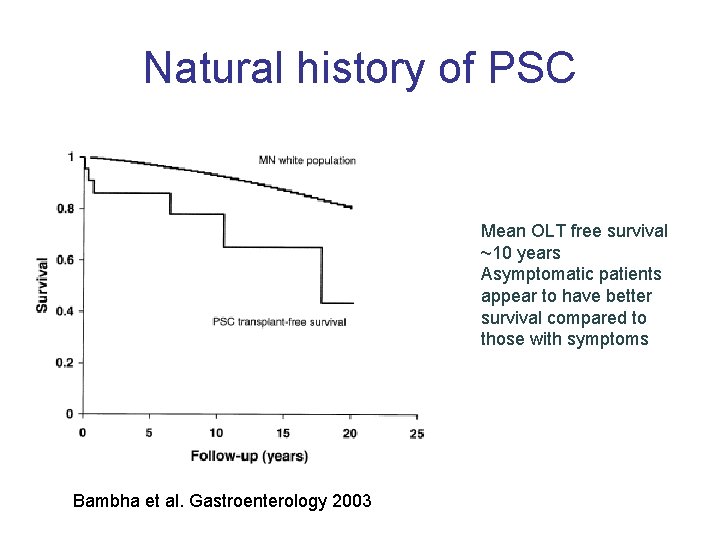
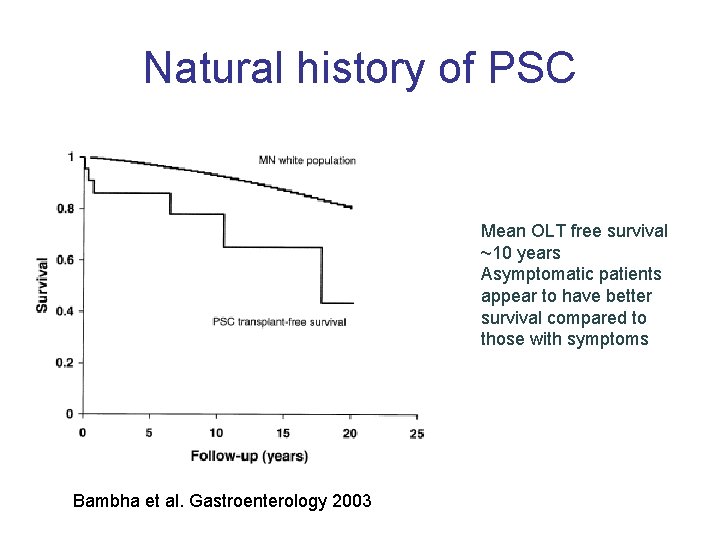
Natural history of PSC Mean OLT free survival ~10 years Asymptomatic patients appear to have better survival compared to those with symptoms Bambha et al. Gastroenterology 2003
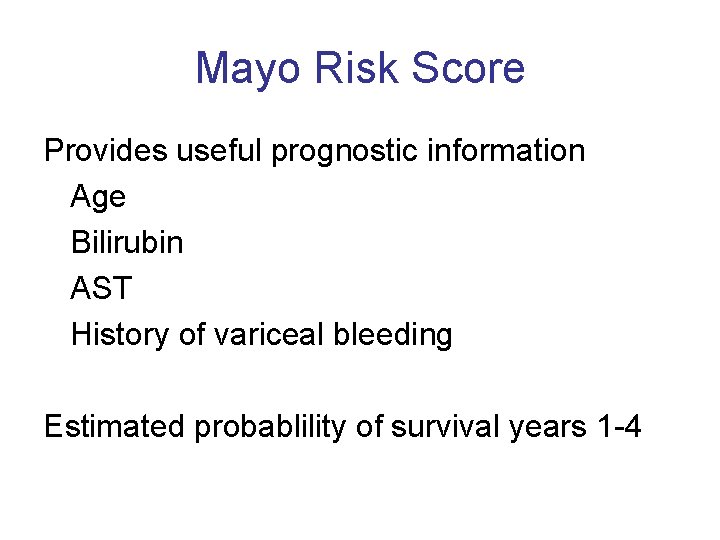
Mayo Risk Score Provides useful prognostic information Age Bilirubin AST History of variceal bleeding Estimated probablility of survival years 1 -4
Complications of PSC • Complications of cholestasis (bile stasis) • Specific complications of PSC • Complications of portal hypertension
Specific complications of PSC • • Bacterial cholangitis Bile duct strictures Cholangioarcinoma Hepatocellular carcinoma
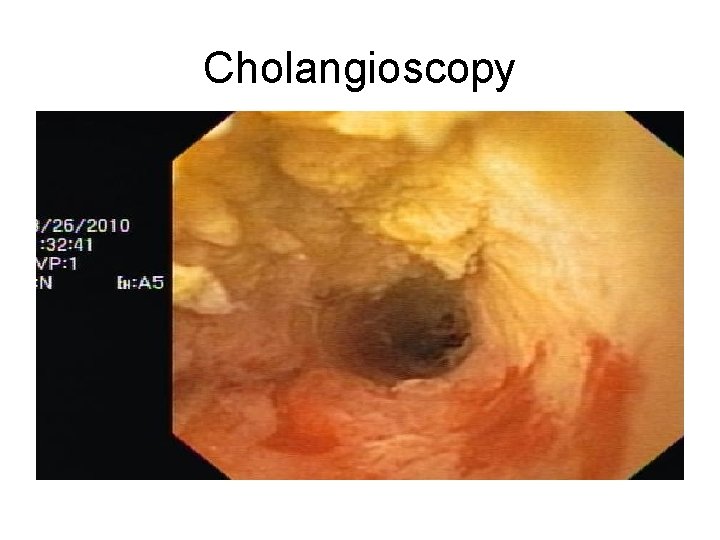
Endoscopic therapy • Most patients will develop dominant strictures – Stenosis with diameter <1. 5 mm in the CBD or <1 mm in HD • Repeated endoscopic interventions are often needed – Antibiotic therapy mandatory – Stents tend to occlude earlier –exchange in 2 – 3 months – Balloon dilatation alone may be preferred – Brush cytology and biopsy before endoscopic therapy to exclude malignancy • Limitations – High grade stenosis >2 cm above the bifurcation –consider percutaneous cholangiography
Liver transplantation • Only effective therapy – Excellent survival rates (>90% at 1 year) – However, PSC recurs in 15 -20% of cases and recurrence may be often associated with loss of the graft – These patients also have a higher frequency of other post OLT complications including hepatic artery thrombosis (HAT)
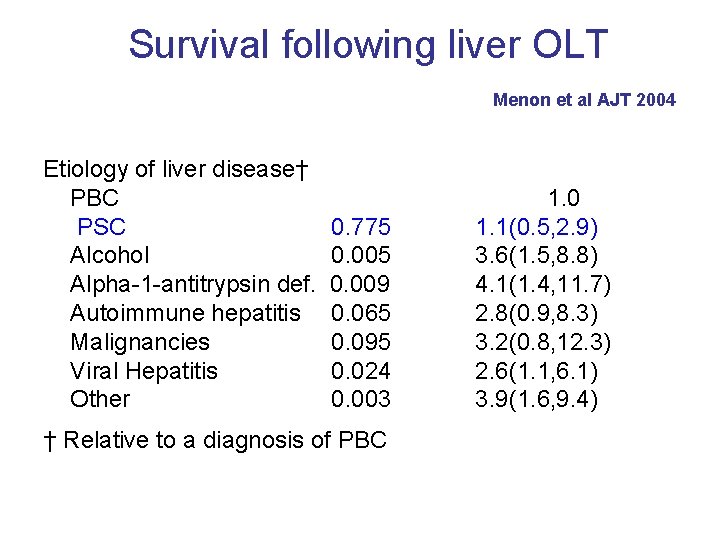
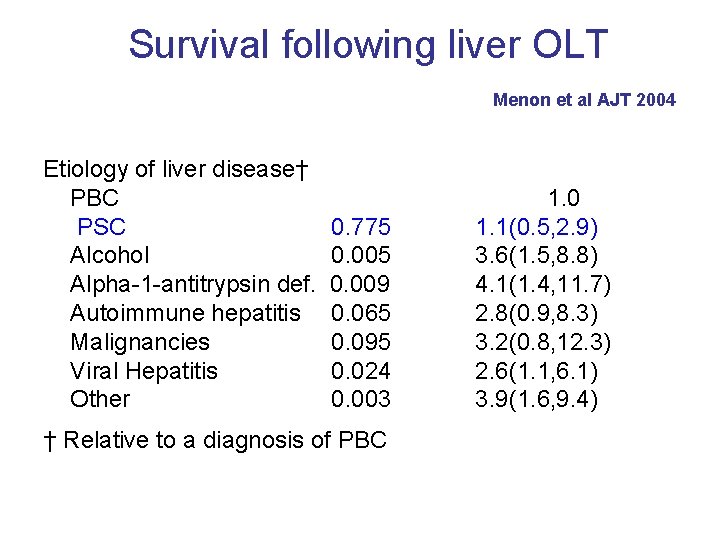
Survival following liver OLT Menon et al AJT 2004 Etiology of liver disease† PBC PSC Alcohol Alpha-1 -antitrypsin def. Autoimmune hepatitis Malignancies Viral Hepatitis Other 0. 775 0. 009 0. 065 0. 095 0. 024 0. 003 † Relative to a diagnosis of PBC 1. 0 1. 1(0. 5, 2. 9) 3. 6(1. 5, 8. 8) 4. 1(1. 4, 11. 7) 2. 8(0. 9, 8. 3) 3. 2(0. 8, 12. 3) 2. 6(1. 1, 6. 1) 3. 9(1. 6, 9. 4)
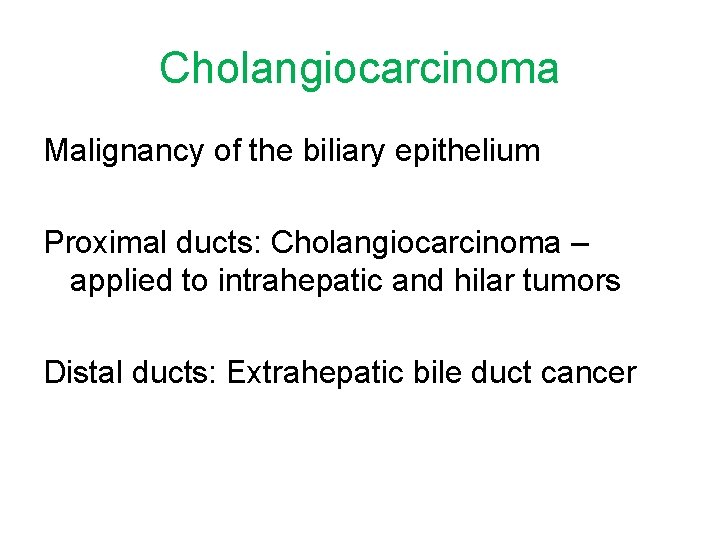
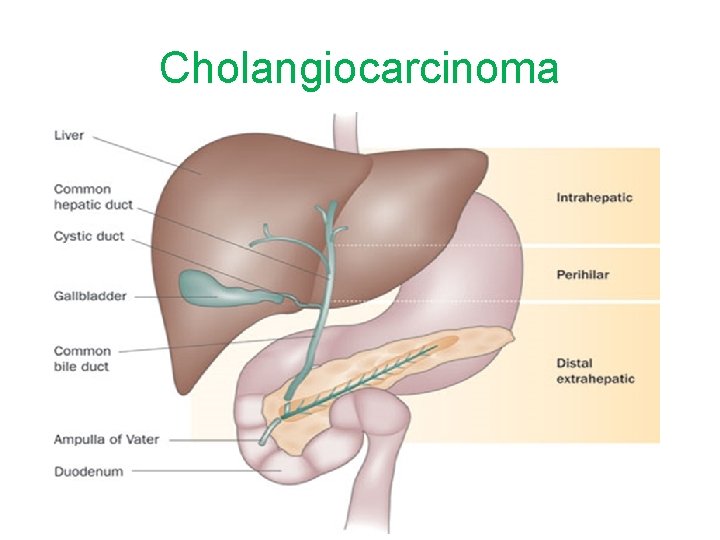
Cholangiocarcinoma Malignancy of the biliary epithelium Proximal ducts: Cholangiocarcinoma – applied to intrahepatic and hilar tumors Distal ducts: Extrahepatic bile duct cancer
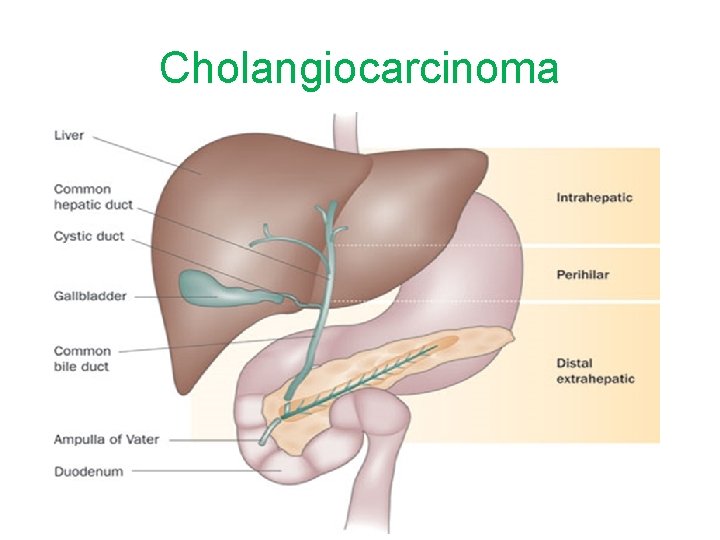
Cholangiocarcinoma
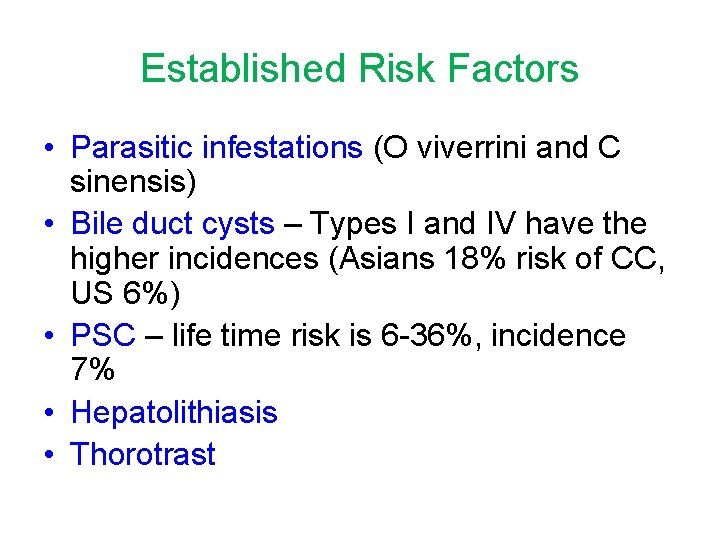
Established Risk Factors • Parasitic infestations (O viverrini and C sinensis) • Bile duct cysts – Types I and IV have the higher incidences (Asians 18% risk of CC, US 6%) • PSC – life time risk is 6 -36%, incidence 7% • Hepatolithiasis • Thorotrast
Clinical Features • Obstructive jaundice • Cholangitis • In patients with PSC • Worseing jaundice • Weight loss
Diagnosis Biochemical Radiological Endoscopic Pathological
Biochemical Diagnosis CA 19 -9 > 100 may have predictive value 7% of the population are red blood cell Lewis phenotye negative and will have non-detectable CA 19 -9 also elevated in Cancers of the stomach, colon and pancreas Bacterial cholangitis Smoking Gynecological malignancies
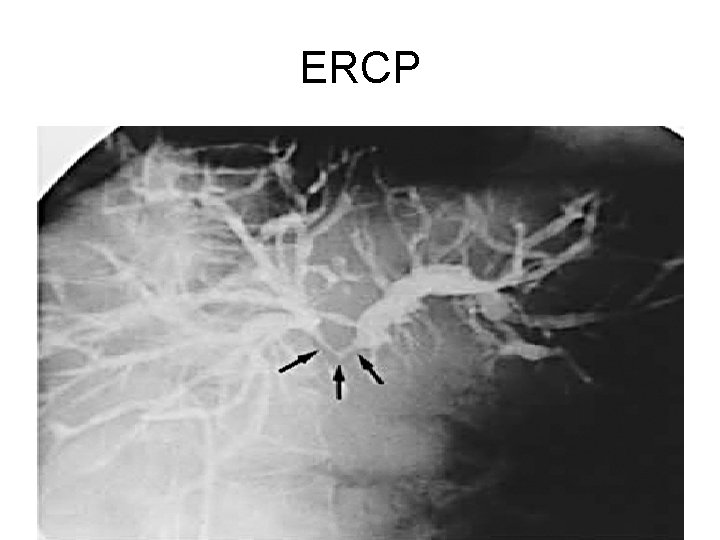
ERCP
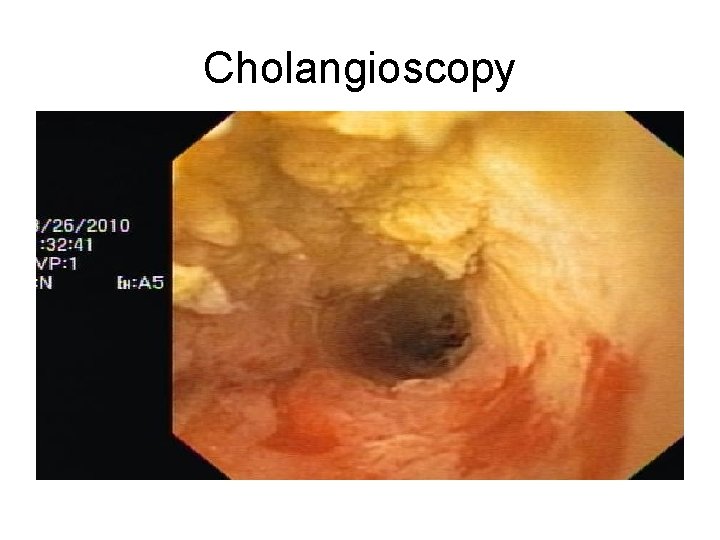
Cholangioscopy

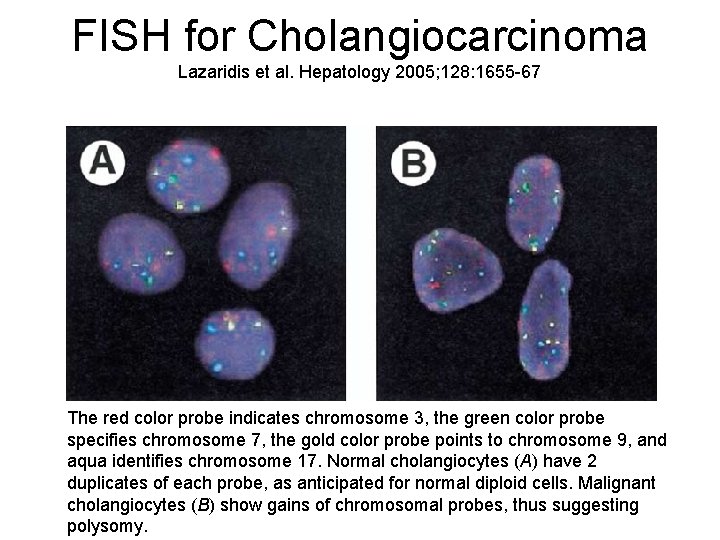
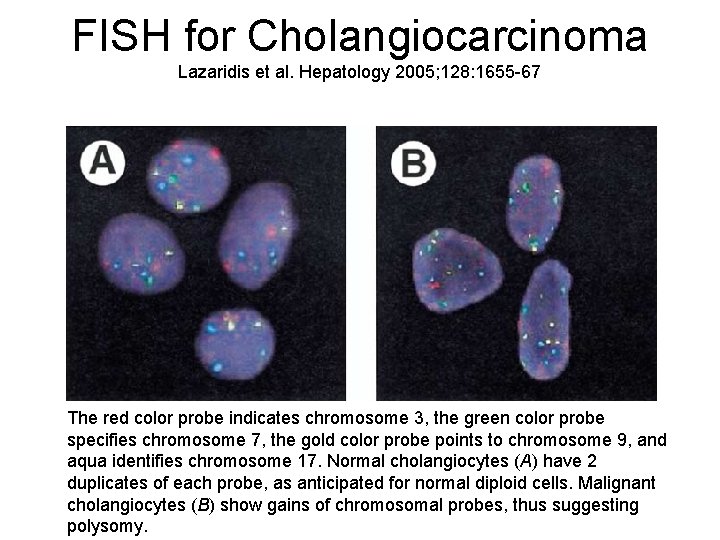
FISH for Cholangiocarcinoma Lazaridis et al. Hepatology 2005; 128: 1655 -67 The red color probe indicates chromosome 3, the green color probe specifies chromosome 7, the gold color probe points to chromosome 9, and aqua identifies chromosome 17. Normal cholangiocytes (A) have 2 duplicates of each probe, as anticipated for normal diploid cells. Malignant cholangiocytes (B) show gains of chromosomal probes, thus suggesting polysomy.
Treatment • Surgical Resection • Liver Transplantation • Palliative • Chemotherapy (Cisplatin and gemcitabine) • Biliary stenting • Photodynamic therapy
Exclusion Criteria for Surgical Resection of Hilar CCA Extension into both sides of the liver Unilobar disease with encasement of the contralateral portal vein or hepatic artery branch Bilateral portal vein or hepatic artery branch encasement Intrahepatic or distant metastases Distant lymph node metastases Significant comorbidities
Liver Transplantation • Original protocol was performed at Nebraska • Mayo Clinic has published a number of reports on transplantation • UNOS has recently awarded patients with cholangiocarcinoma exception MELD points if they are in an accepted protocol
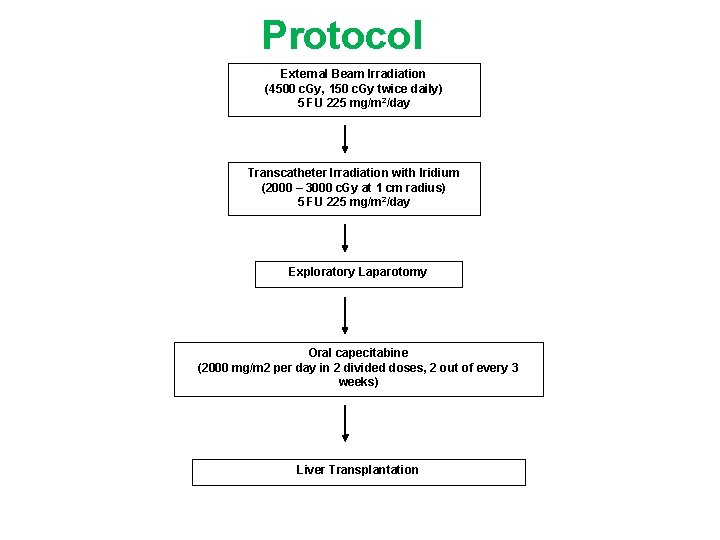
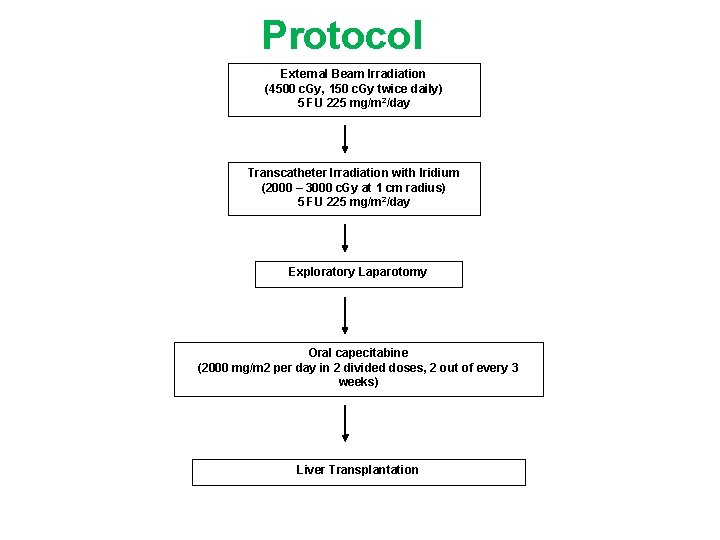
Protocol External Beam Irradiation (4500 c. Gy, 150 c. Gy twice daily) 5 FU 225 mg/m 2/day Transcatheter Irradiation with Iridium (2000 – 3000 c. Gy at 1 cm radius) 5 FU 225 mg/m 2/day Exploratory Laparotomy Oral capecitabine (2000 mg/m 2 per day in 2 divided doses, 2 out of every 3 weeks) Liver Transplantation
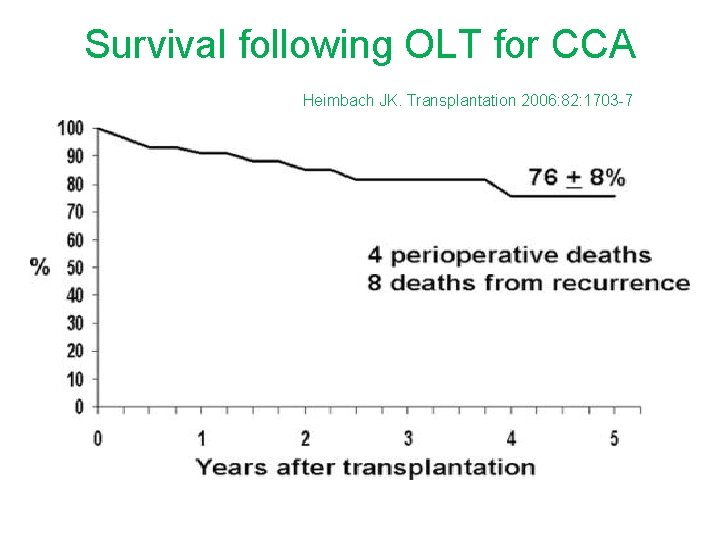
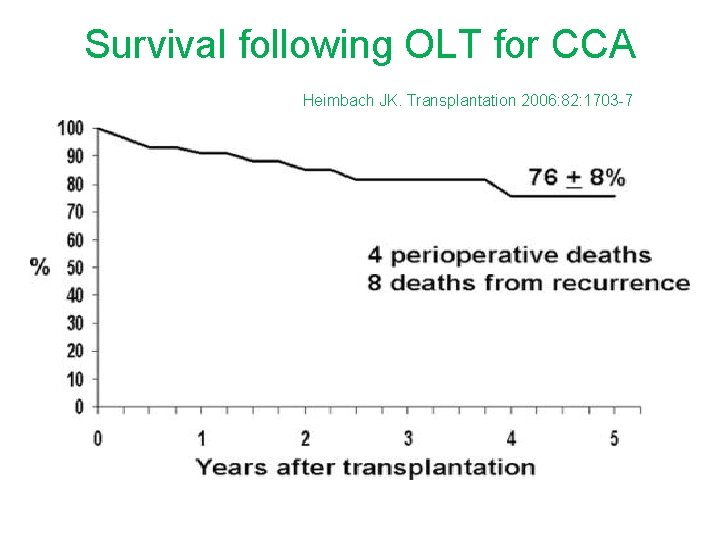
Survival following OLT for CCA Heimbach JK. Transplantation 2006: 82: 1703 -7
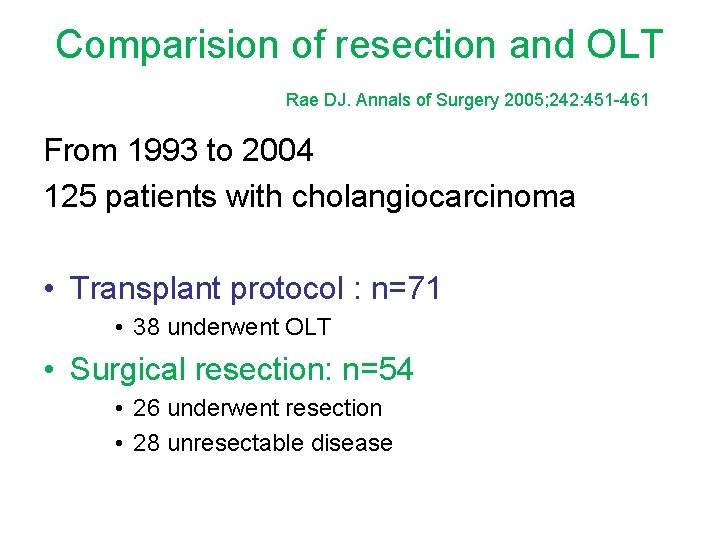
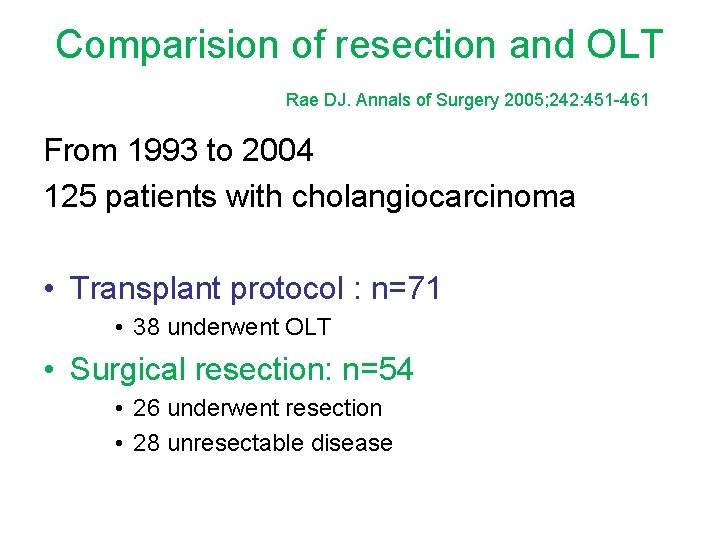
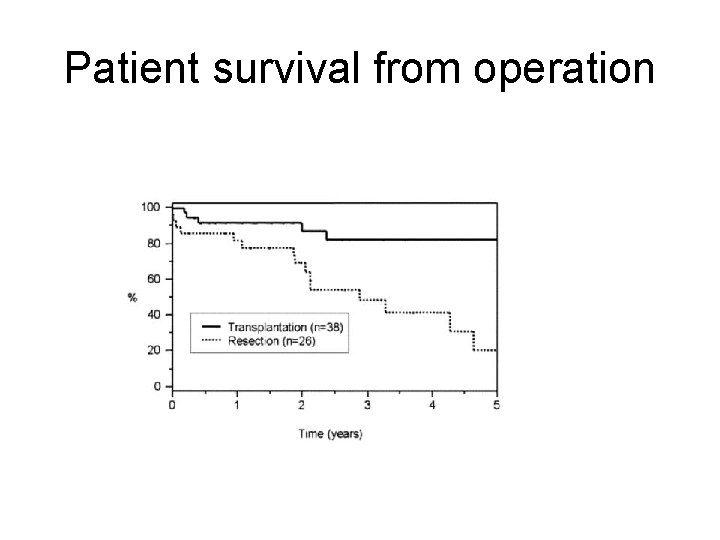
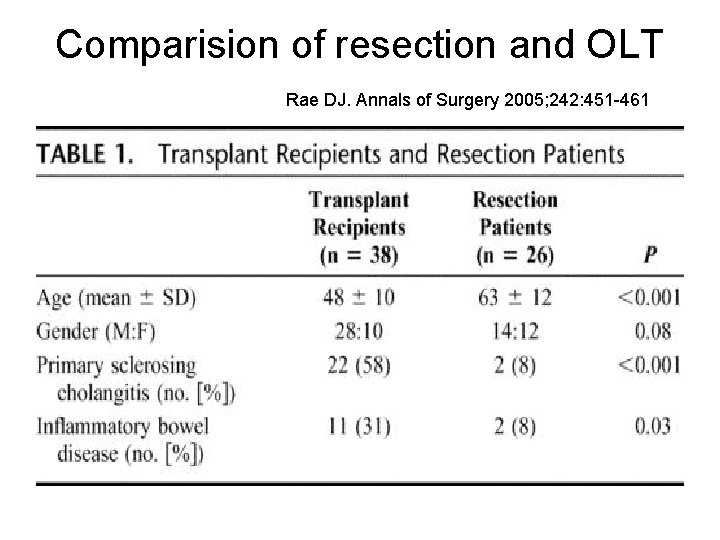
Comparision of resection and OLT Rae DJ. Annals of Surgery 2005; 242: 451 -461 From 1993 to 2004 125 patients with cholangiocarcinoma • Transplant protocol : n=71 • 38 underwent OLT • Surgical resection: n=54 • 26 underwent resection • 28 unresectable disease
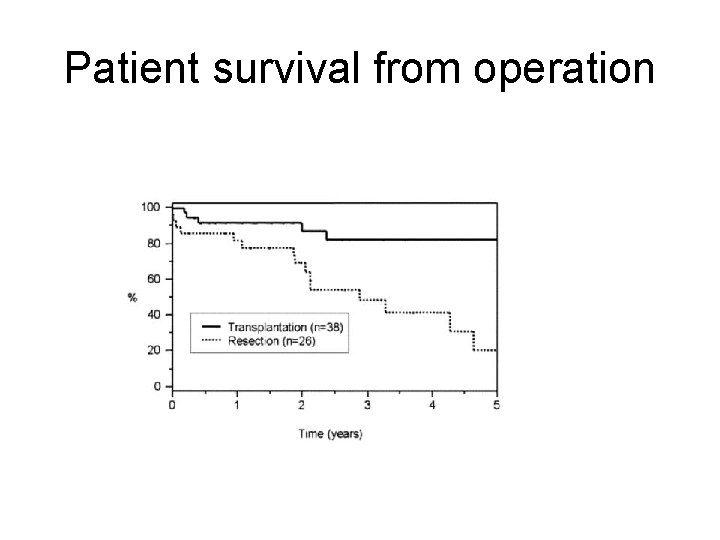
Patient survival from operation
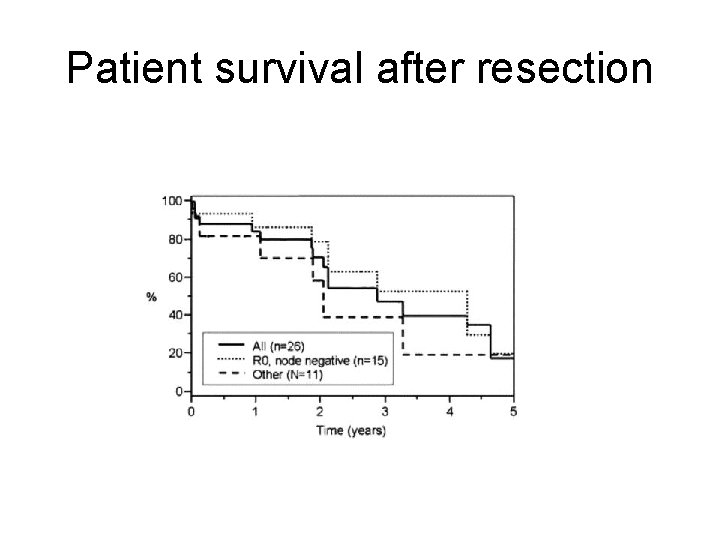
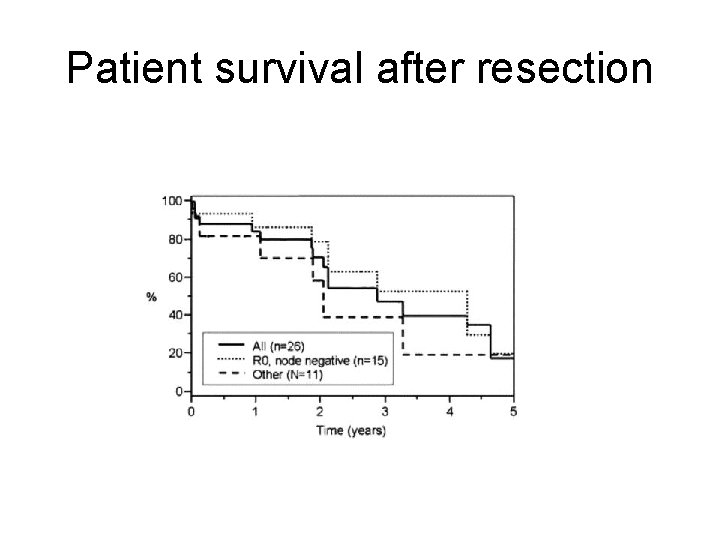
Patient survival after resection
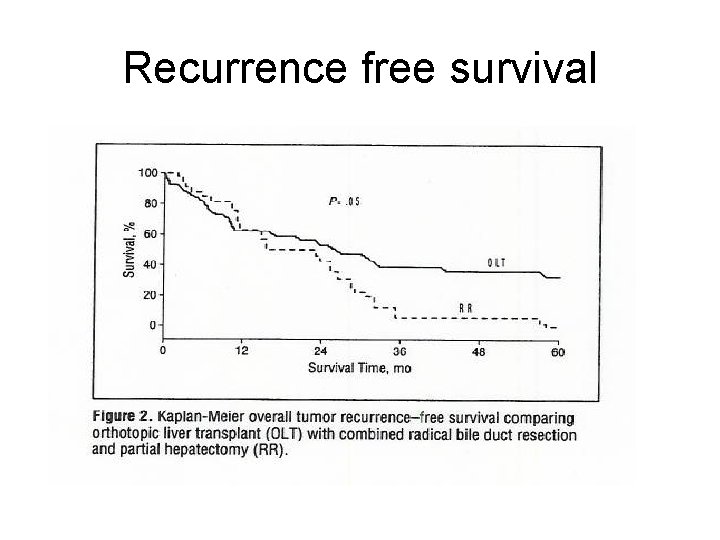
Recurrence free survival

• Accounts for 3% of biliary malignancies • Second most common primary hepatic malignancy (10 -25% worldwide) • Higher incidence in men – 1: 1. 2 -1. 5
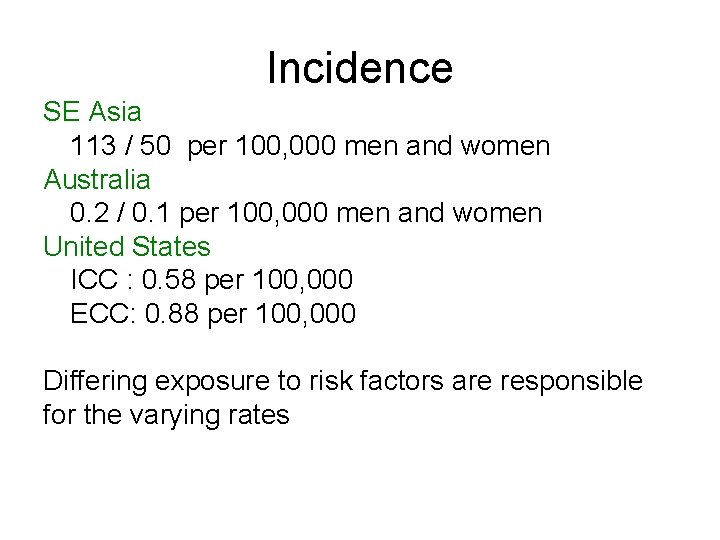
Incidence SE Asia 113 / 50 per 100, 000 men and women Australia 0. 2 / 0. 1 per 100, 000 men and women United States ICC : 0. 58 per 100, 000 ECC: 0. 88 per 100, 000 Differing exposure to risk factors are responsible for the varying rates
Possible Risk Factors • • • Inflammatory bowel disease Choledocholithiasis and cholangitis Chronic viral hepatitis and cirrhosis Alcohol Smoking Obesity and diabetes
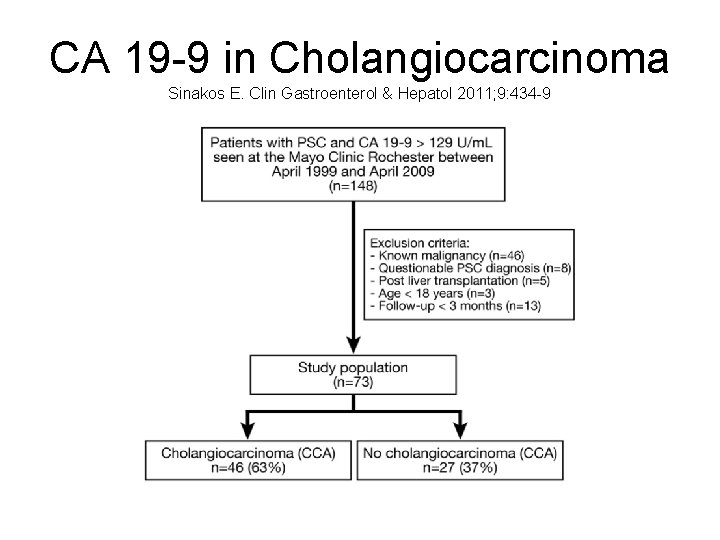
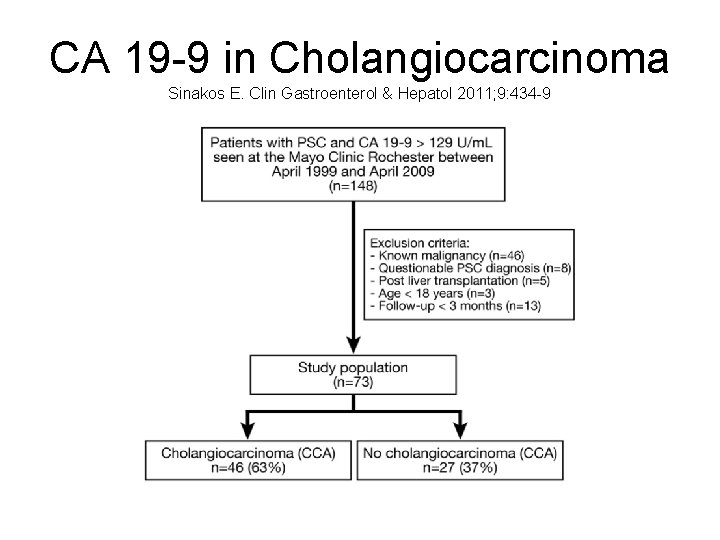
CA 19 -9 in Cholangiocarcinoma Sinakos E. Clin Gastroenterol & Hepatol 2011; 9: 434 -9


CA 19 -9 concentration of 503 U/m. L at initial diagnosis sensitivity of 67%, specificity of 74%, PPV of 82%, NPV of 57% with an area under the curve (AUC) of 0. 77
Radiologic Diagnosis • Short dominant stricture on cholangiography • Polypoid masses • Rapid progression of stricturing • Hilar mass on imaging • PET scanning – may be more useful in nodular lesions and lymph node mets • EUS – hilar mass lesions / lymph nodes
Histological Diagnosis • Histopathology of tissue obtained by biopsy of tumors • Routine cytology of bile duct strictures • Advanced molecular techniques in cytology - FISH
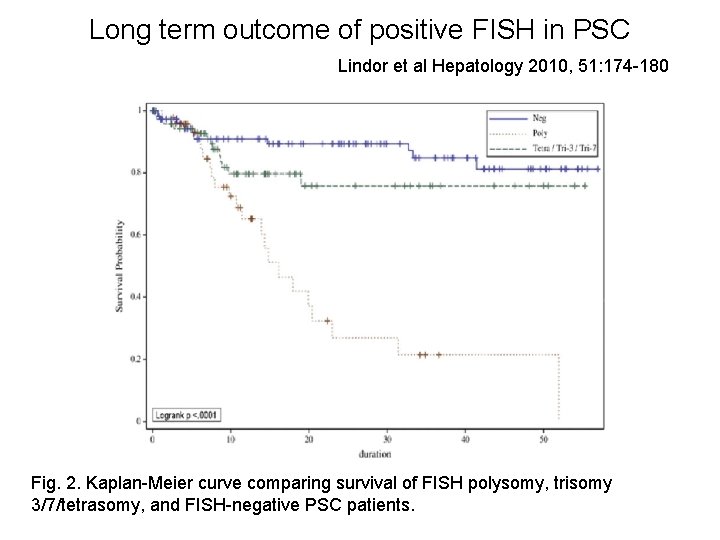
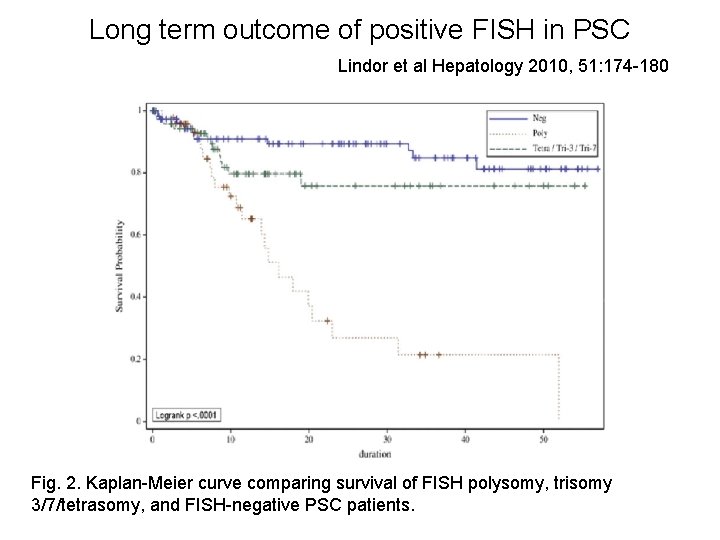
Long term outcome of positive FISH in PSC Lindor et al Hepatology 2010, 51: 174 -180 Fig. 2. Kaplan-Meier curve comparing survival of FISH polysomy, trisomy 3/7/tetrasomy, and FISH-negative PSC patients.

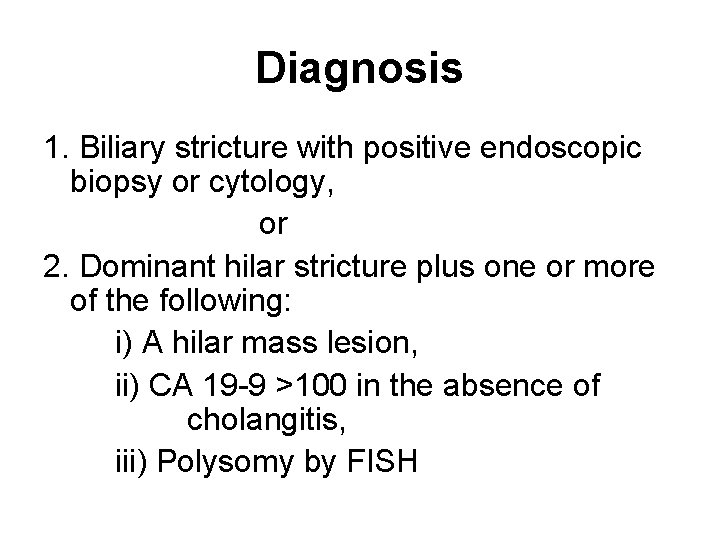
Diagnosis 1. Biliary stricture with positive endoscopic biopsy or cytology, or 2. Dominant hilar stricture plus one or more of the following: i) A hilar mass lesion, ii) CA 19 -9 >100 in the absence of cholangitis, iii) Polysomy by FISH
Treatment Surgical Resection Five year survival rates of 22 to 44% R 0 resection absence of lymph node metastases / vascular invasion
Inclusion Criteria 1. Lesion is located at the hilum with the stricture above the cystic duct 2. Patient must be suitable candidates for radiation therapy, chemotherapy and liver transplantation 3. No evidence of metastatic disease (intrahepatic or extra-hepatic)
Inclusion Criteria (cont) 4. If a mass lesion is present, it should be less than or equal to approximately 3 cm in radial direction 5. The tumor is considered unresectable on the bass of technical considerations or underlying liver disease (eg. , primary sclerosing cholangitis) 6. Negative regional lymph nodes on endoscopic ultrasound and fine needle aspiration
Exclusion criteria 1. Patients with prior abdominal radiation 2. Patients who have undergone a transperitoneal biopsy of the tumor or open exploration with violation of the tumor plane. 3. Diagnosis of a previous malignancy within the prior 5 years (excluding superficial skin and cervical cancers)
Exclusion criteria (cont) 4. Presence of intrahepatic metastases and / or extrahepatic disease. 5. Presence of lymph node metastases 6. Patients younger than 18 and older than 70 years of age

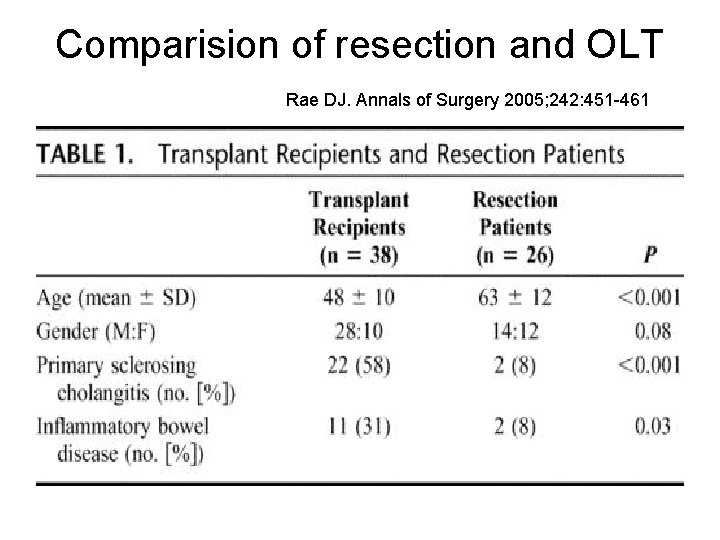
Comparision of resection and OLT Rae DJ. Annals of Surgery 2005; 242: 451 -461
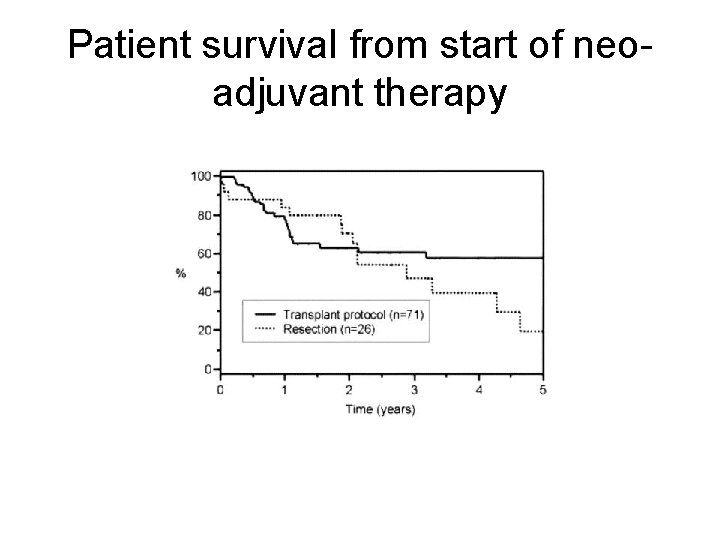
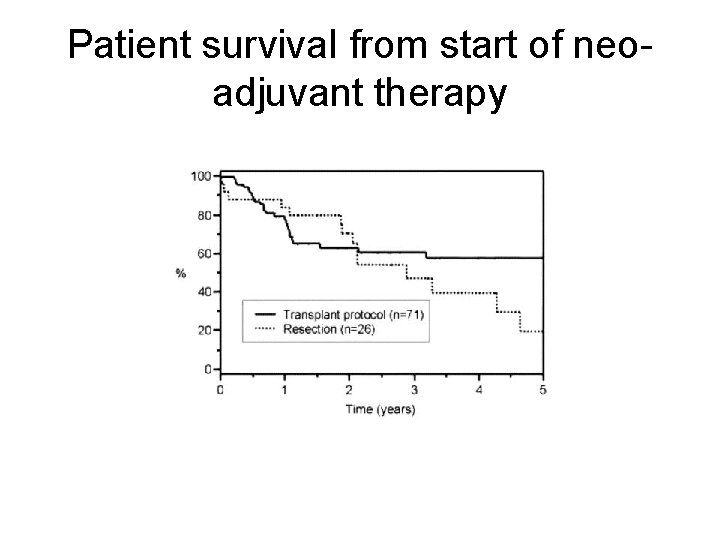
Patient survival from start of neoadjuvant therapy
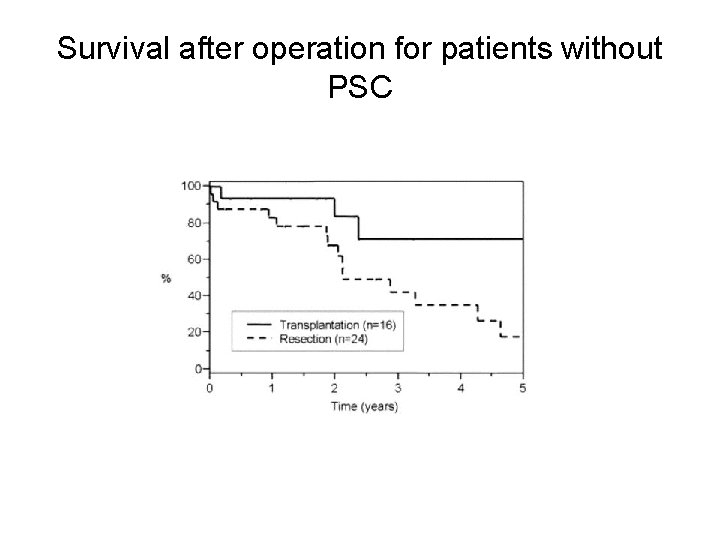
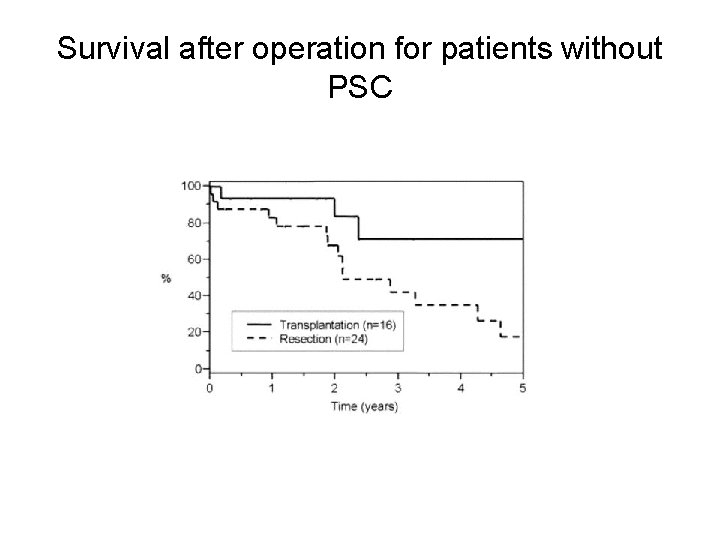
Survival after operation for patients without PSC
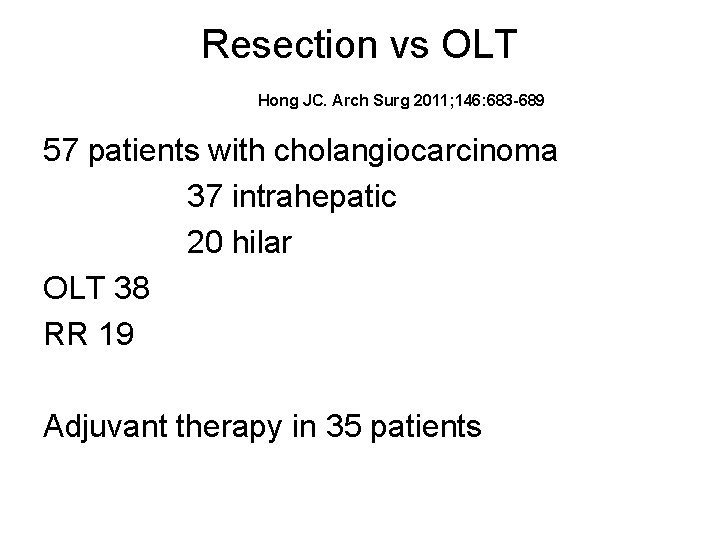
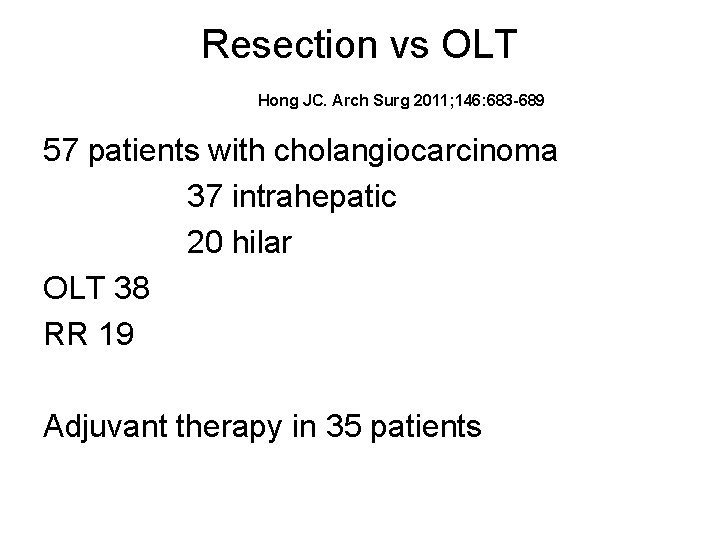
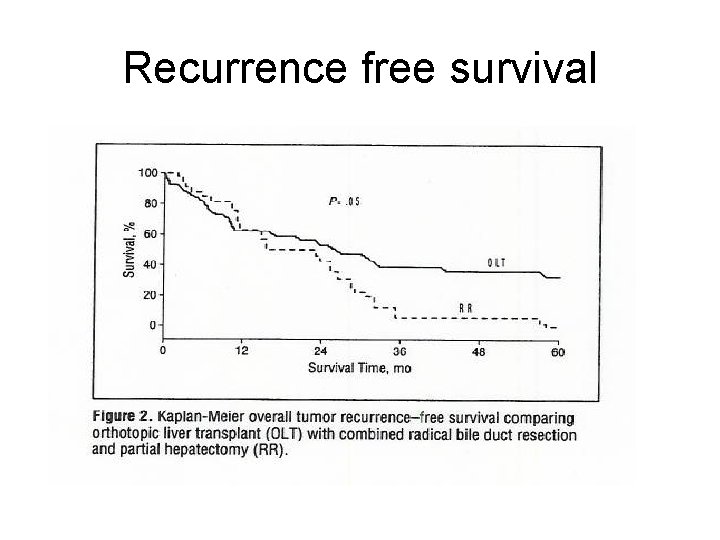
Resection vs OLT Hong JC. Arch Surg 2011; 146: 683 -689 57 patients with cholangiocarcinoma 37 intrahepatic 20 hilar OLT 38 RR 19 Adjuvant therapy in 35 patients
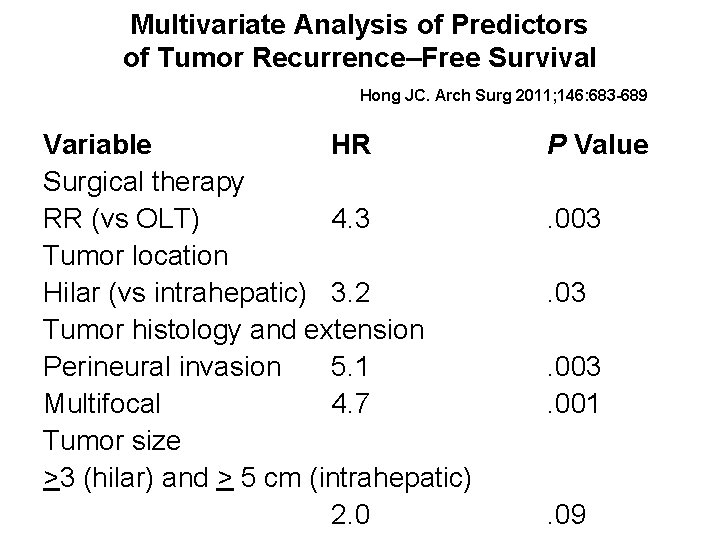
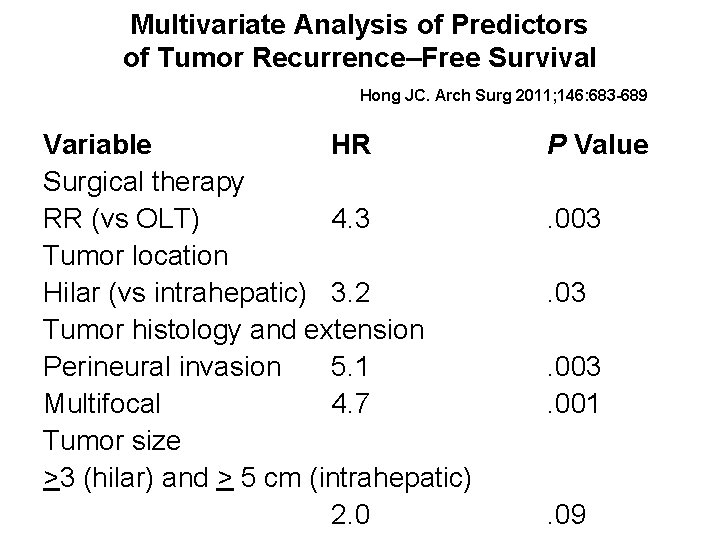
Multivariate Analysis of Predictors of Tumor Recurrence–Free Survival Hong JC. Arch Surg 2011; 146: 683 -689 Variable HR Surgical therapy RR (vs OLT) 4. 3 Tumor location Hilar (vs intrahepatic) 3. 2 Tumor histology and extension Perineural invasion 5. 1 Multifocal 4. 7 Tumor size >3 (hilar) and > 5 cm (intrahepatic) 2. 0 P Value. 003. 001 . 09
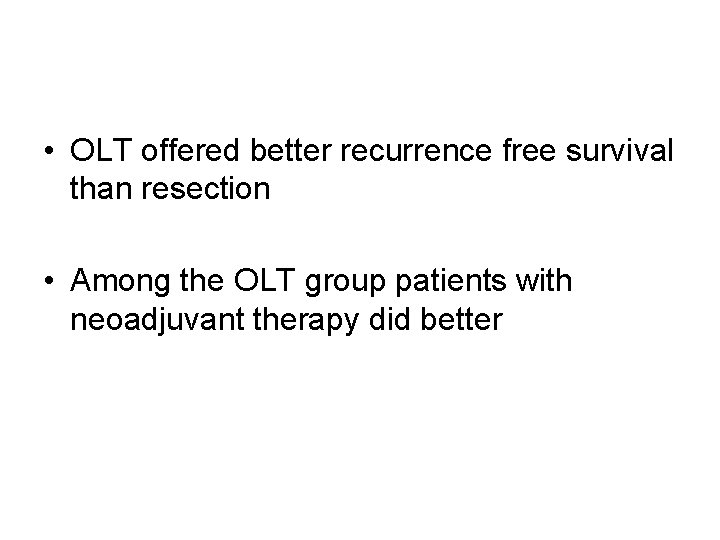
• OLT offered better recurrence free survival than resection • Among the OLT group patients with neoadjuvant therapy did better
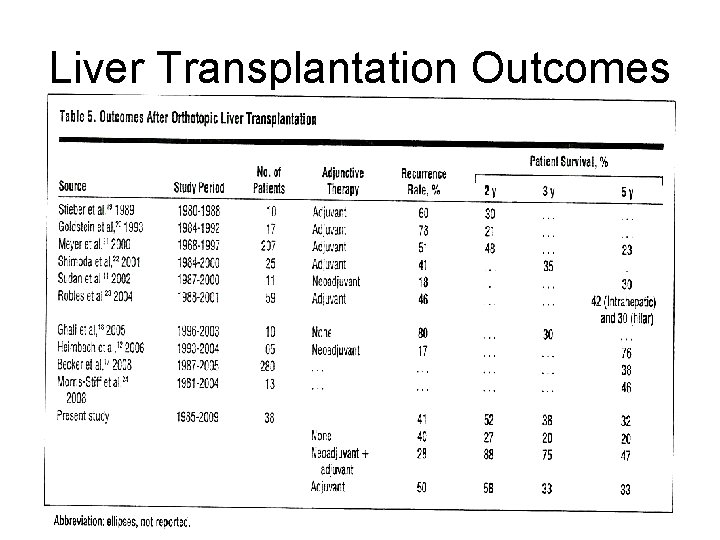
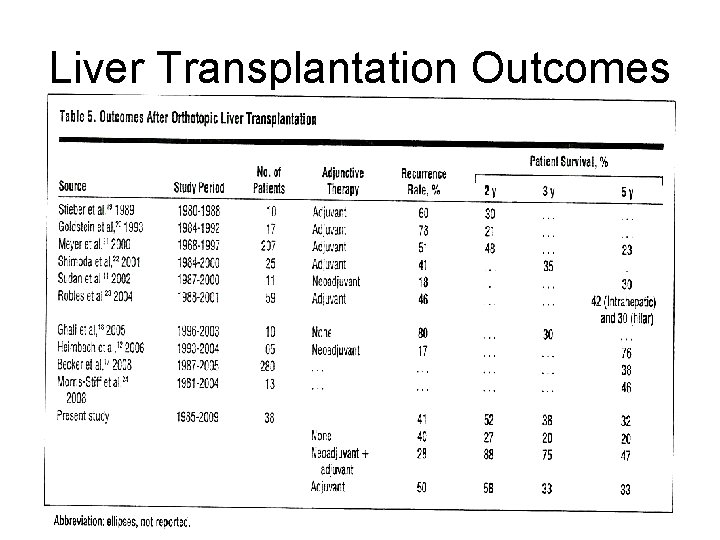
Liver Transplantation Outcomes
 What is biliary cirrhosis
What is biliary cirrhosis Small duct psc
Small duct psc Primary biliary cholangitis labs
Primary biliary cholangitis labs Primary biliary cholangitis skin
Primary biliary cholangitis skin Primary biliary cholangitis skin
Primary biliary cholangitis skin Mrcp galdesten
Mrcp galdesten Cholangitis prognosis
Cholangitis prognosis Standards of the disciplines organized around a theme.
Standards of the disciplines organized around a theme. Multisectoral and multidisciplinary
Multisectoral and multidisciplinary Multidisciplinary team pros and cons
Multidisciplinary team pros and cons Uksn almora
Uksn almora Temasek laboratories
Temasek laboratories Multidisciplinary vs interdisciplinary
Multidisciplinary vs interdisciplinary Multidisciplinary nature of environmental studies ppt
Multidisciplinary nature of environmental studies ppt Multidisciplinary engineering definition
Multidisciplinary engineering definition Conflict in multidisciplinary teams
Conflict in multidisciplinary teams Interdisciplinary multidisciplinary transdisciplinary
Interdisciplinary multidisciplinary transdisciplinary Epcc degree plans
Epcc degree plans Datagram switching and virtual circuit switching
Datagram switching and virtual circuit switching Tony wagner's seven survival skills
Tony wagner's seven survival skills Theoretical models of counseling
Theoretical models of counseling Waterfall approach in international marketing
Waterfall approach in international marketing Multiple approach avoidance conflict
Multiple approach avoidance conflict Bandura's reciprocal determinism
Bandura's reciprocal determinism What is research approach definition
What is research approach definition Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Direct approach in primary language classroom
Direct approach in primary language classroom Comprehensive primary health care definition
Comprehensive primary health care definition Primary care a collaborative approach
Primary care a collaborative approach Yellow magenta and cyan are the ___
Yellow magenta and cyan are the ___ Women and development wad
Women and development wad Top down and bottom up approach
Top down and bottom up approach Essay cognitive psychology
Essay cognitive psychology Examples of approach, method and technique
Examples of approach, method and technique Advantages and disadvantages of the golden rule
Advantages and disadvantages of the golden rule Top down vs bottom up psychology
Top down vs bottom up psychology Psychodynamic approach to schizophrenia evaluation
Psychodynamic approach to schizophrenia evaluation Persuasive communication definition
Persuasive communication definition Method and approach difference
Method and approach difference Heroes and holidays approach
Heroes and holidays approach Ethnocentric orientation example company
Ethnocentric orientation example company A formal approach to game design and game research
A formal approach to game design and game research Method and technique
Method and technique Formalist
Formalist Formalism and structuralism
Formalism and structuralism 3 approaches to measuring performance
3 approaches to measuring performance Costs and risks of database approach
Costs and risks of database approach Cognitive approach strengths
Cognitive approach strengths Defining performance and choosing a measurement approach
Defining performance and choosing a measurement approach Stephen splevins
Stephen splevins Gandhian approach in management
Gandhian approach in management Difference between code first and database first approach
Difference between code first and database first approach Top down strategy in reading
Top down strategy in reading Female deficit model example
Female deficit model example Formalism and new criticism example
Formalism and new criticism example Direct or expository approach
Direct or expository approach Dynamic approach language and gender
Dynamic approach language and gender One's viewpoint towards teaching
One's viewpoint towards teaching Multistage graph forward and backward approach
Multistage graph forward and backward approach Tpr procedure
Tpr procedure