Oncology Multidisciplinary Team Grf Lszl MD Multidisciplinary Team


- Slides: 24
Oncology Multidisciplinary Team Gráf László MD
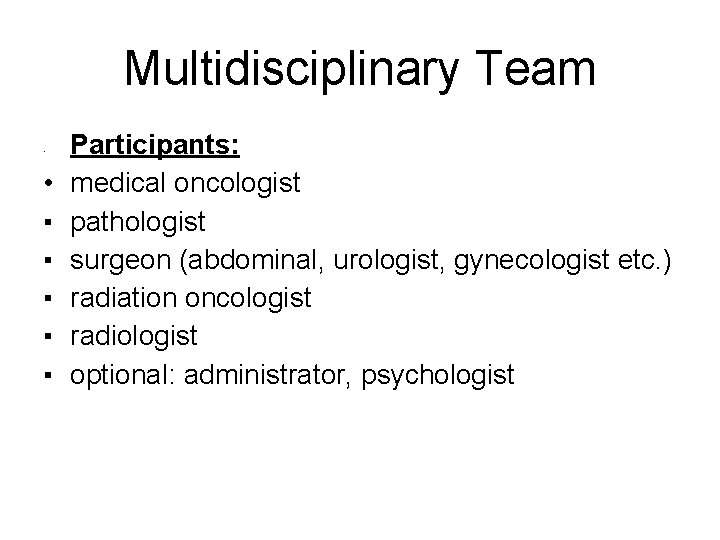
Multidisciplinary Team • • ▪ ▪ ▪ Participants: medical oncologist pathologist surgeon (abdominal, urologist, gynecologist etc. ) radiation oncologist radiologist optional: administrator, psychologist
Role of oncology team • Diagnostic algorhythm: – interpretation of results – indication of new examinations • Therapeutic algorhythm: – – Type Order Timing Location • Supervision of therapy: – change in treatment plan – palliation – rehabilitation
Role of oncology team • Oncology team should take place no later than 14 days after diagnosis: – Before surgery/resection because in some cases patient will benefit if neoadjuvant chemo or radiochemotherapy precedes surgery (localy advanced oesophagus/rectum/breast cancer • In case of oncology emergency (vena cava syndrome, hypercalcaemia etc. ) within 48 hours
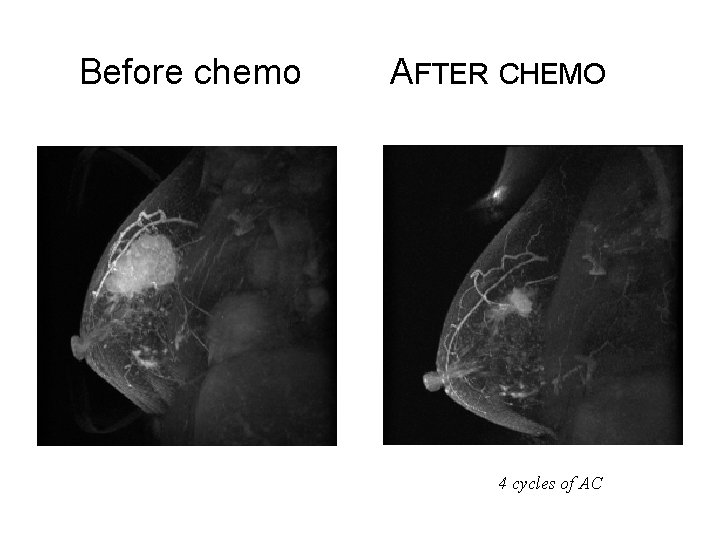
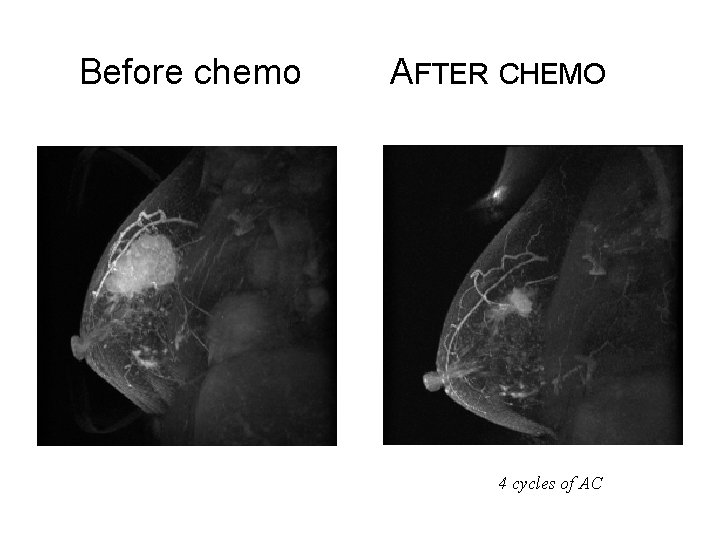
Before chemo AFTER CHEMO 4 cycles of AC
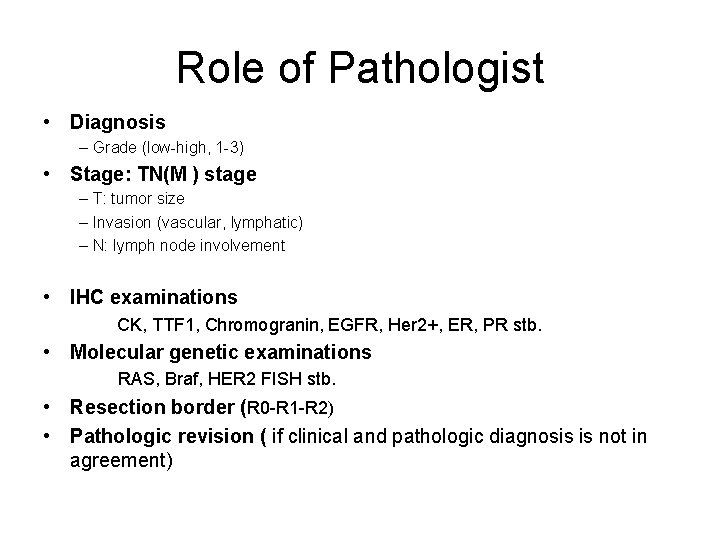
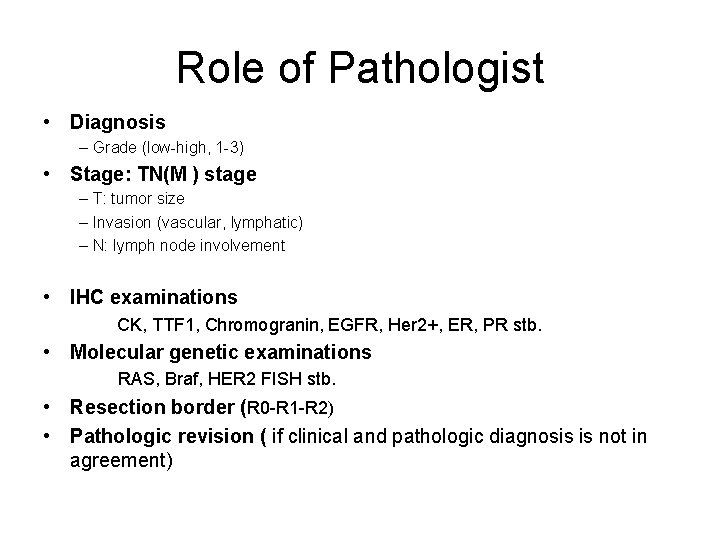
Role of Pathologist • Diagnosis – Grade (low-high, 1 -3) • Stage: TN(M ) stage – T: tumor size – Invasion (vascular, lymphatic) – N: lymph node involvement • IHC examinations CK, TTF 1, Chromogranin, EGFR, Her 2+, ER, PR stb. • Molecular genetic examinations RAS, Braf, HER 2 FISH stb. • Resection border (R 0 -R 1 -R 2) • Pathologic revision ( if clinical and pathologic diagnosis is not in agreement)
Surgical Oncology • Radical surgery • • • Minimal invasivity Reconstruction surgery Metastasectomy �Diagnostics, imaging: CT, MR, US �Histology: staging
Role of radiotherapy • Preoperative treatment: rectum-, cervix-, etc. Aim: down staging • Primary (definitive) treatment: inoperable, irresecable tumors • Intraoperative (perioperative) radiotherapy: soft tissue sarcomas, pancreas cancer, gynecological cacncers etc. • Radiochemotherapy: Advanced head and neck-, uribary bladder-, rectum-, oesophagus-, lung- cancers (synchronous or consecutive) • Postoperative treatment: breast cancer • Palliative irradiation: pain, compression, bleeding (mpx. cerebral met. , bone metastases)
Case presentations
Case I. • 50 y, female patient, negative family history. ECOG PS: 0 • Screening mammography detected 1 cm tumor on left side – core biopsy: tubular cc. (grade 1, IHC: ER 90%, PR: 100%, HER-2: +, Ki 67: 8 -10 %, p 53: 2 -3%) • Sectorectomy + SLNB – operative histology: tubular cc. (grade 1, IHC: ER 90%, PR: 100%, HER-2: +, Ki 67: 8 -10 %, p 53: 2 -3%). Tumor size : 9 mm. In situ component: low grade DCIS in less than 5%. Lymphovascular and perineural invasion: absent. The resection margins are negative. Sentinel node is negative (0/1). NPI: 2, 2 p. T 1 b p. N 0[sn, 0/1]. • Staging: chest Xray, abdominal US, bone isotope: neg. • Oncoteam Decision: adjuvant irradiation and endocrine therapy ( in case of postmenopause AI for 5 years).
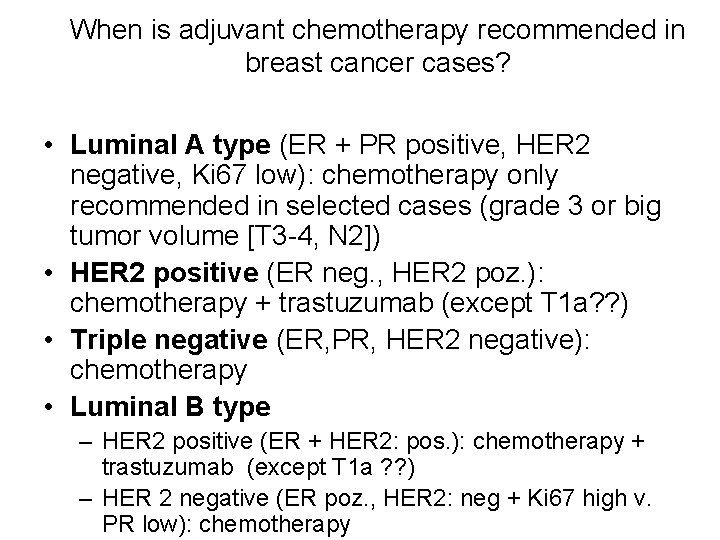
When is adjuvant chemotherapy recommended in breast cancer cases? • Luminal A type (ER + PR positive, HER 2 negative, Ki 67 low): chemotherapy only recommended in selected cases (grade 3 or big tumor volume [T 3 -4, N 2]) • HER 2 positive (ER neg. , HER 2 poz. ): chemotherapy + trastuzumab (except T 1 a? ? ) • Triple negative (ER, PR, HER 2 negative): chemotherapy • Luminal B type – HER 2 positive (ER + HER 2: pos. ): chemotherapy + trastuzumab (except T 1 a ? ? ) – HER 2 negative (ER poz. , HER 2: neg + Ki 67 high v. PR low): chemotherapy


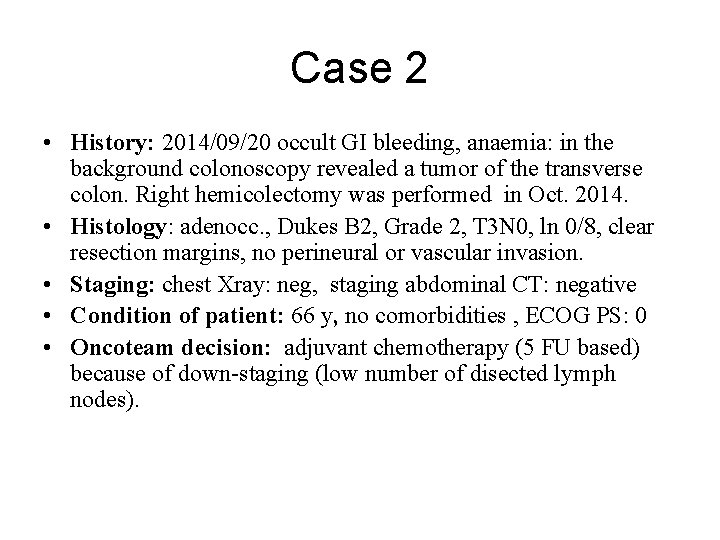
Case 2 • History: 2014/09/20 occult GI bleeding, anaemia: in the background colonoscopy revealed a tumor of the transverse colon. Right hemicolectomy was performed in Oct. 2014. • Histology: adenocc. , Dukes B 2, Grade 2, T 3 N 0, ln 0/8, clear resection margins, no perineural or vascular invasion. • Staging: chest Xray: neg, staging abdominal CT: negative • Condition of patient: 66 y, no comorbidities , ECOG PS: 0 • Oncoteam decision: adjuvant chemotherapy (5 FU based) because of down-staging (low number of disected lymph nodes).
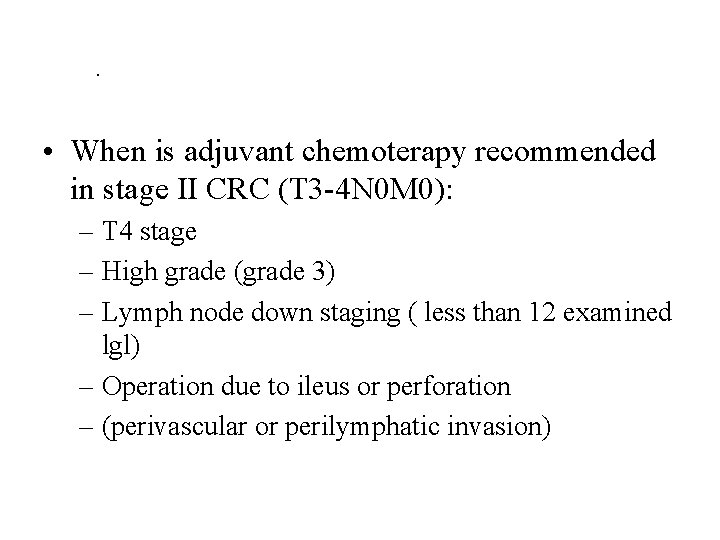
. • When is adjuvant chemoterapy recommended in stage II CRC (T 3 -4 N 0 M 0): – T 4 stage – High grade (grade 3) – Lymph node down staging ( less than 12 examined lgl) – Operation due to ileus or perforation – (perivascular or perilymphatic invasion)
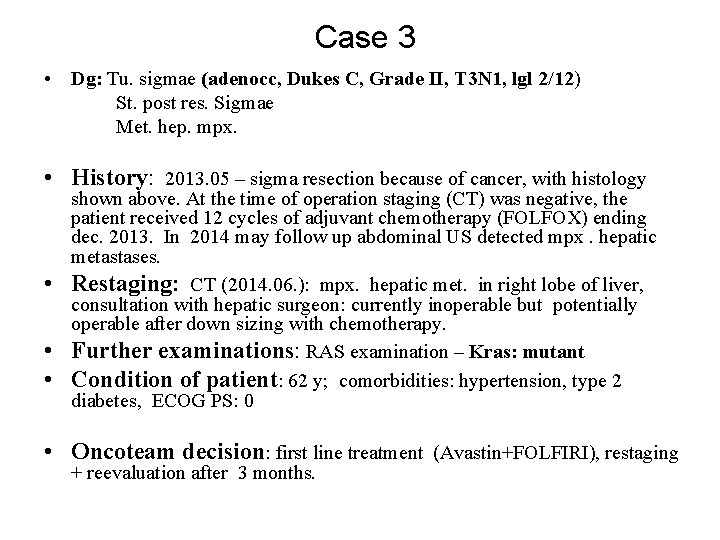
Case 3 • Dg: Tu. sigmae (adenocc, Dukes C, Grade II, T 3 N 1, lgl 2/12) St. post res. Sigmae Met. hep. mpx. • History: 2013. 05 – sigma resection because of cancer, with histology • • • shown above. At the time of operation staging (CT) was negative, the patient received 12 cycles of adjuvant chemotherapy (FOLFOX) ending dec. 2013. In 2014 may follow up abdominal US detected mpx. hepatic metastases. Restaging: CT (2014. 06. ): mpx. hepatic met. in right lobe of liver, consultation with hepatic surgeon: currently inoperable but potentially operable after down sizing with chemotherapy. Further examinations: RAS examination – Kras: mutant Condition of patient: 62 y; comorbidities: hypertension, type 2 diabetes, ECOG PS: 0 • Oncoteam decision: first line treatment (Avastin+FOLFIRI), restaging + reevaluation after 3 months.
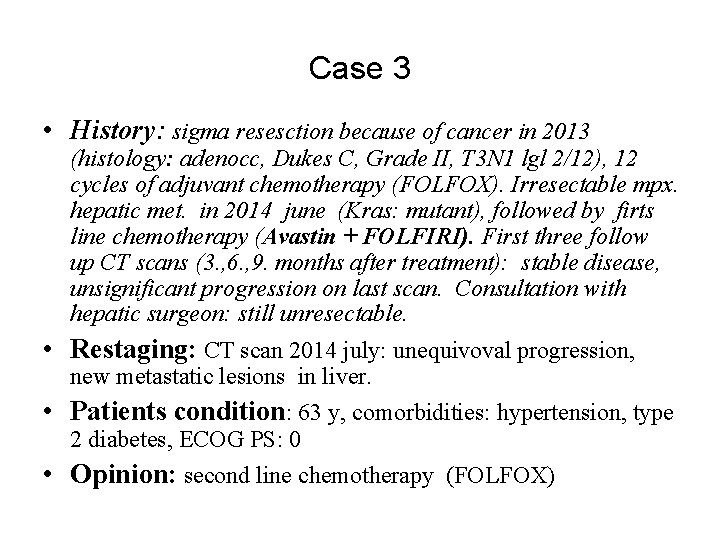
Case 3 • History: sigma resesction because of cancer in 2013 (histology: adenocc, Dukes C, Grade II, T 3 N 1 lgl 2/12), 12 cycles of adjuvant chemotherapy (FOLFOX). Irresectable mpx. hepatic met. in 2014 june (Kras: mutant), followed by firts line chemotherapy (Avastin + FOLFIRI). First three follow up CT scans (3. , 6. , 9. months after treatment): stable disease, unsignificant progression on last scan. Consultation with hepatic surgeon: still unresectable. • Restaging: CT scan 2014 july: unequivoval progression, new metastatic lesions in liver. • Patients condition: 63 y, comorbidities: hypertension, type 2 diabetes, ECOG PS: 0 • Opinion: second line chemotherapy (FOLFOX)
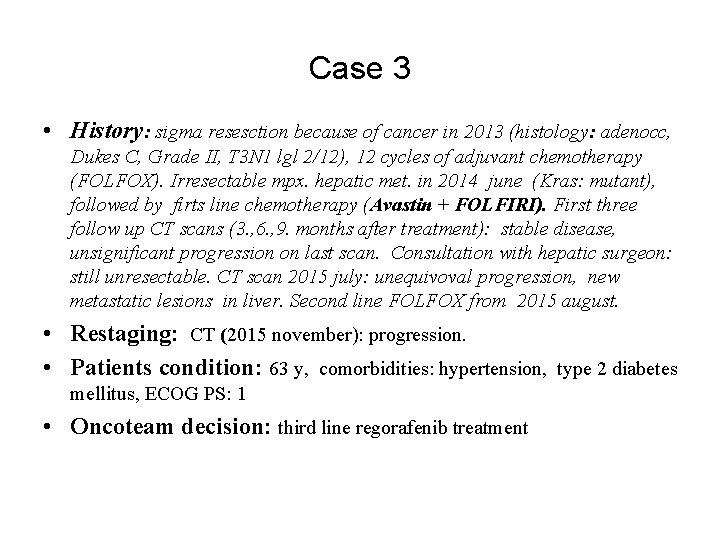
Case 3 • History: sigma resesction because of cancer in 2013 (histology: adenocc, Dukes C, Grade II, T 3 N 1 lgl 2/12), 12 cycles of adjuvant chemotherapy (FOLFOX). Irresectable mpx. hepatic met. in 2014 june (Kras: mutant), followed by firts line chemotherapy (Avastin + FOLFIRI). First three follow up CT scans (3. , 6. , 9. months after treatment): stable disease, unsignificant progression on last scan. Consultation with hepatic surgeon: still unresectable. CT scan 2015 july: unequivoval progression, new metastatic lesions in liver. Second line FOLFOX from 2015 august. • Restaging: CT (2015 november): progression. • Patients condition: 63 y, comorbidities: hypertension, type 2 diabetes mellitus, ECOG PS: 1 • Oncoteam decision: third line regorafenib treatment
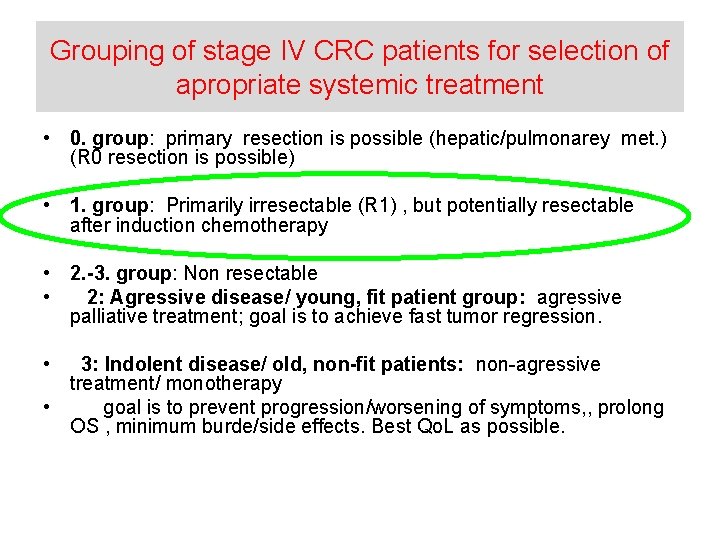
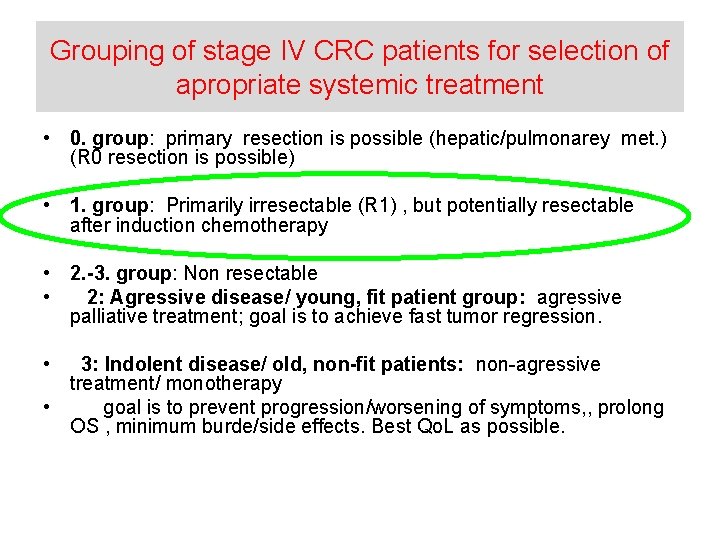
Grouping of stage IV CRC patients for selection of apropriate systemic treatment • 0. group: primary resection is possible (hepatic/pulmonarey met. ) (R 0 resection is possible) • 1. group: Primarily irresectable (R 1) , but potentially resectable after induction chemotherapy • 2. -3. group: Non resectable • 2: Agressive disease/ young, fit patient group: agressive palliative treatment; goal is to achieve fast tumor regression. • 3: Indolent disease/ old, non-fit patients: non-agressive treatment/ monotherapy • goal is to prevent progression/worsening of symptoms, , prolong OS , minimum burde/side effects. Best Qo. L as possible.
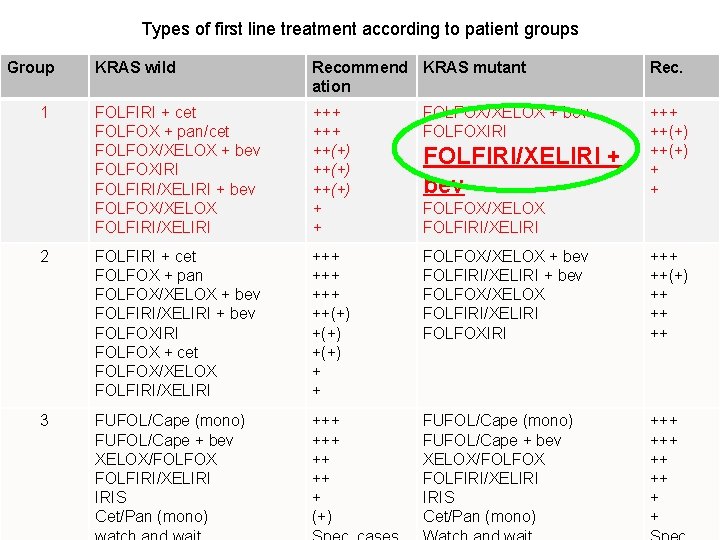
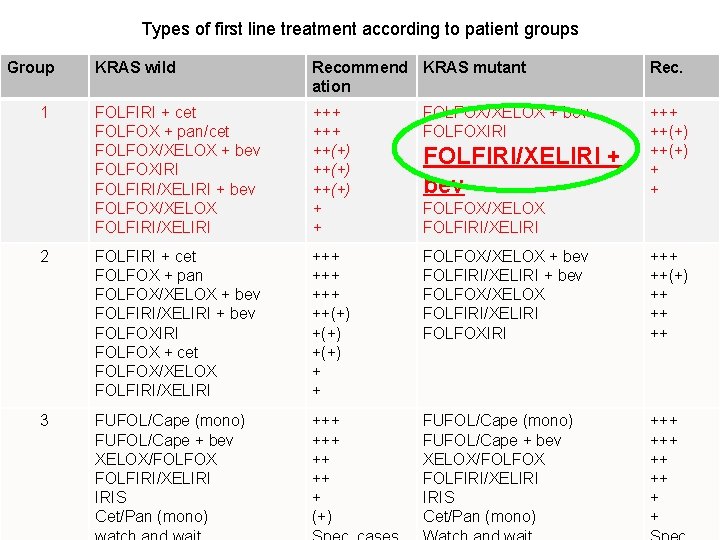
Types of first line treatment according to patient groups Group KRAS wild Recommend KRAS mutant ation Rec. FOLFIRI + cet FOLFOX + pan/cet FOLFOX/XELOX + bev FOLFOXIRI FOLFIRI/XELIRI + bev FOLFOX/XELOX FOLFIRI/XELIRI +++ ++(+) + + FOLFOX/XELOX + bev FOLFOXIRI +++ ++(+) + + 2 FOLFIRI + cet FOLFOX + pan FOLFOX/XELOX + bev FOLFIRI/XELIRI + bev FOLFOXIRI FOLFOX + cet FOLFOX/XELOX FOLFIRI/XELIRI +++ +++ ++(+) + + FOLFOX/XELOX + bev FOLFIRI/XELIRI + bev FOLFOX/XELOX FOLFIRI/XELIRI FOLFOXIRI +++ ++(+) ++ ++ ++ 3 FUFOL/Cape (mono) FUFOL/Cape + bev XELOX/FOLFOX FOLFIRI/XELIRI IRIS Cet/Pan (mono) +++ ++ ++ + (+) FUFOL/Cape (mono) FUFOL/Cape + bev XELOX/FOLFOX FOLFIRI/XELIRI IRIS Cet/Pan (mono) +++ ++ ++ + + 1 FOLFIRI/XELIRI + bev FOLFOX/XELOX FOLFIRI/XELIRI
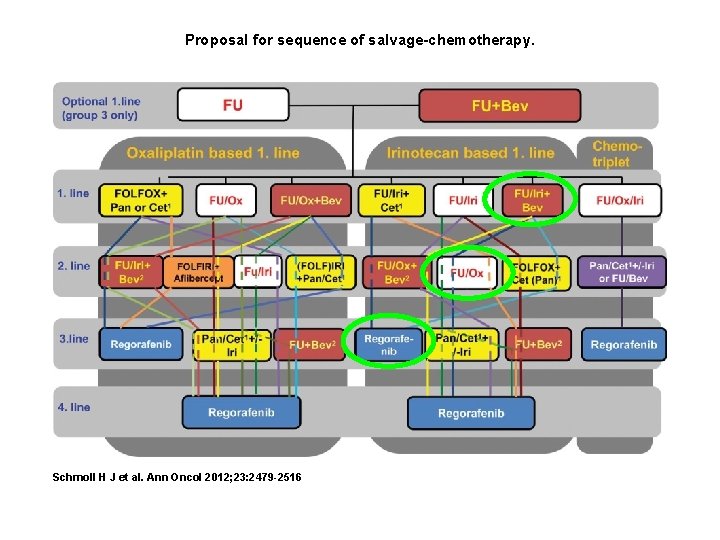
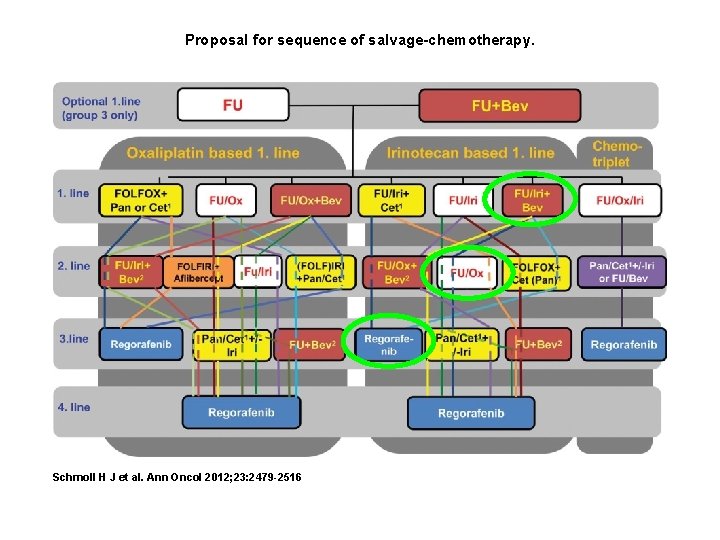
Proposal for sequence of salvage-chemotherapy. Schmoll H J et al. Ann Oncol 2012; 23: 2479 -2516
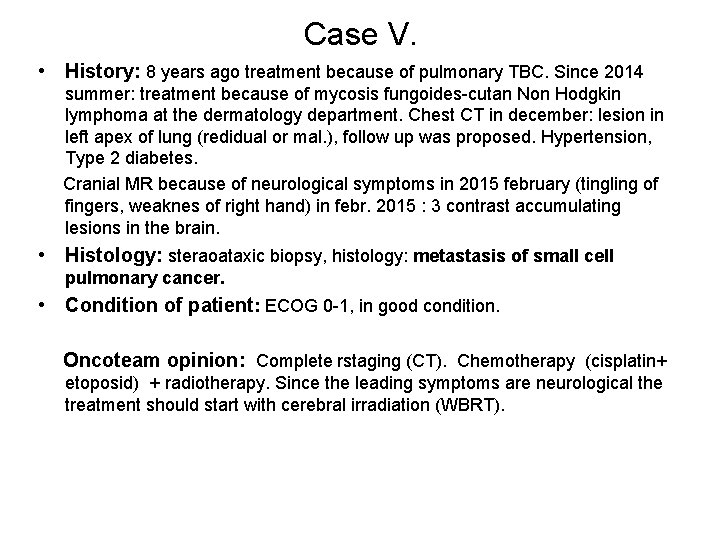
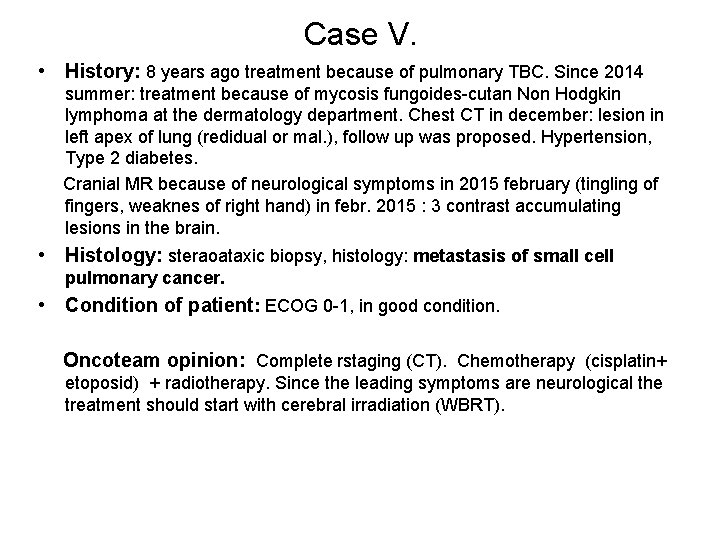
Case V. • History: 8 years ago treatment because of pulmonary TBC. Since 2014 summer: treatment because of mycosis fungoides-cutan Non Hodgkin lymphoma at the dermatology department. Chest CT in december: lesion in left apex of lung (redidual or mal. ), follow up was proposed. Hypertension, Type 2 diabetes. Cranial MR because of neurological symptoms in 2015 february (tingling of fingers, weaknes of right hand) in febr. 2015 : 3 contrast accumulating lesions in the brain. • Histology: steraoataxic biopsy, histology: metastasis of small cell pulmonary cancer. • Condition of patient: ECOG 0 -1, in good condition. Oncoteam opinion: Complete rstaging (CT). Chemotherapy (cisplatin+ etoposid) + radiotherapy. Since the leading symptoms are neurological the treatment should start with cerebral irradiation (WBRT).
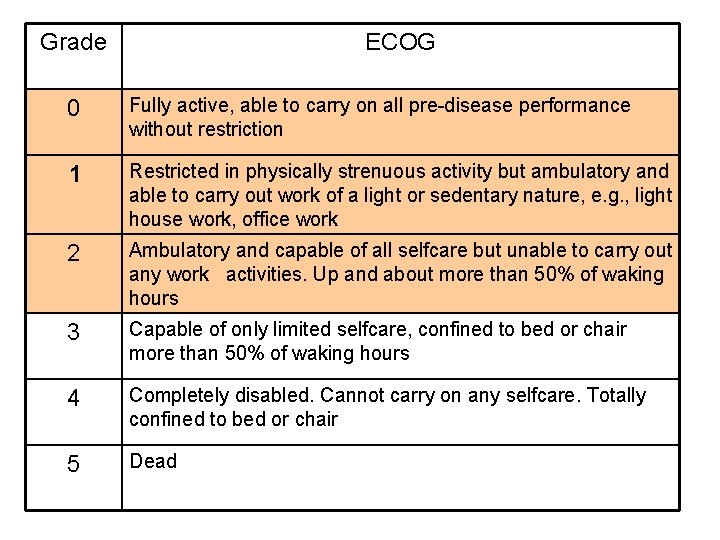
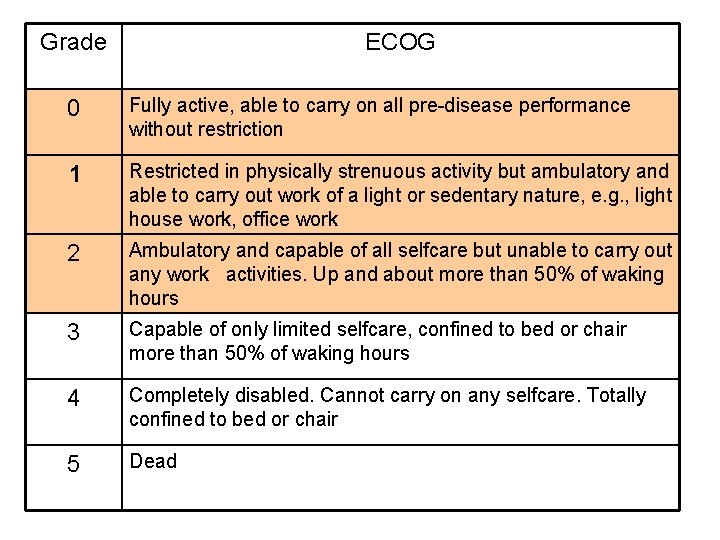
Grade ECOG 0 Fully active, able to carry on all pre-disease performance without restriction 1 Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e. g. , light house work, office work 2 Ambulatory and capable of all selfcare but unable to carry out any work activities. Up and about more than 50% of waking hours 3 Capable of only limited selfcare, confined to bed or chair more than 50% of waking hours 4 Completely disabled. Cannot carry on any selfcare. Totally confined to bed or chair 5 Dead
Thank you