Practical Management of Post Irradiation Haemorrhagic Cystitis JHL


- Slides: 29
Practical Management of Post. Irradiation Haemorrhagic Cystitis JHL Tsu Division of Urology Pamela Youde Nethersole Eastern Hospital JHSGR Sept 2006
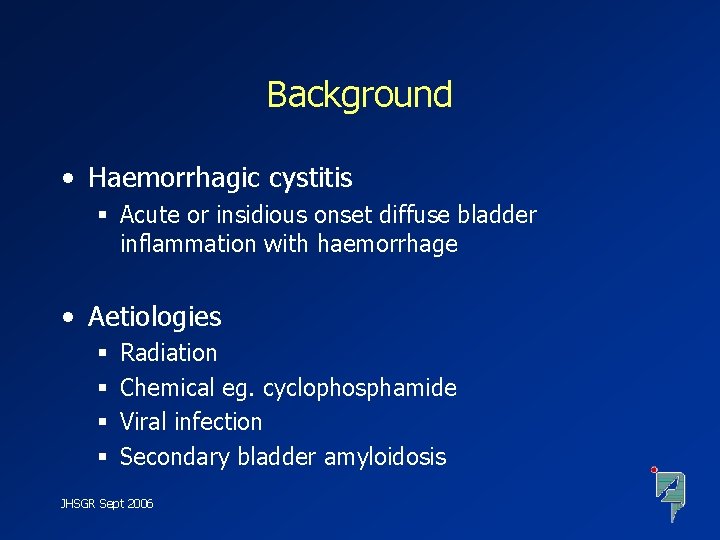
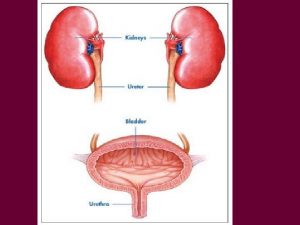
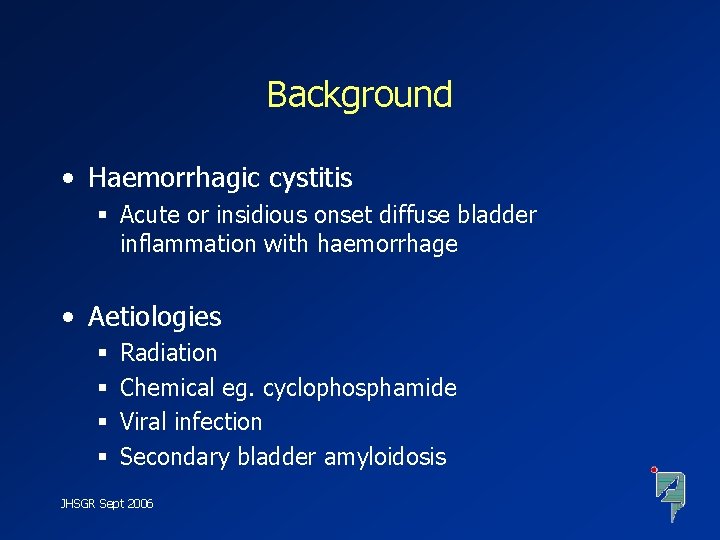
Background • Haemorrhagic cystitis § Acute or insidious onset diffuse bladder inflammation with haemorrhage • Aetiologies § § Radiation Chemical eg. cyclophosphamide Viral infection Secondary bladder amyloidosis JHSGR Sept 2006
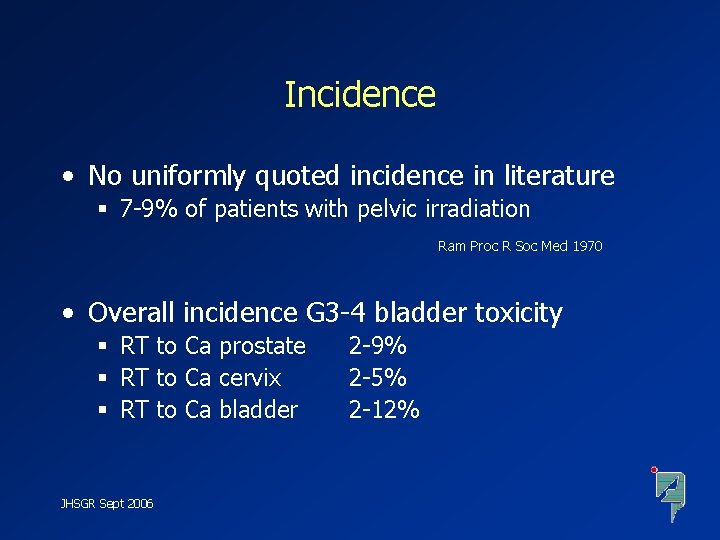
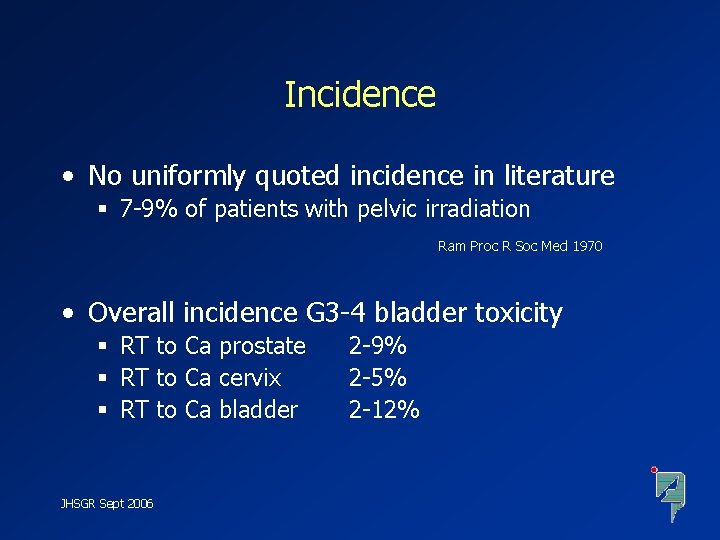
Incidence • No uniformly quoted incidence in literature § 7 -9% of patients with pelvic irradiation Ram Proc R Soc Med 1970 • Overall incidence G 3 -4 bladder toxicity § RT to Ca prostate § RT to Ca cervix § RT to Ca bladder JHSGR Sept 2006 2 -9% 2 -5% 2 -12%
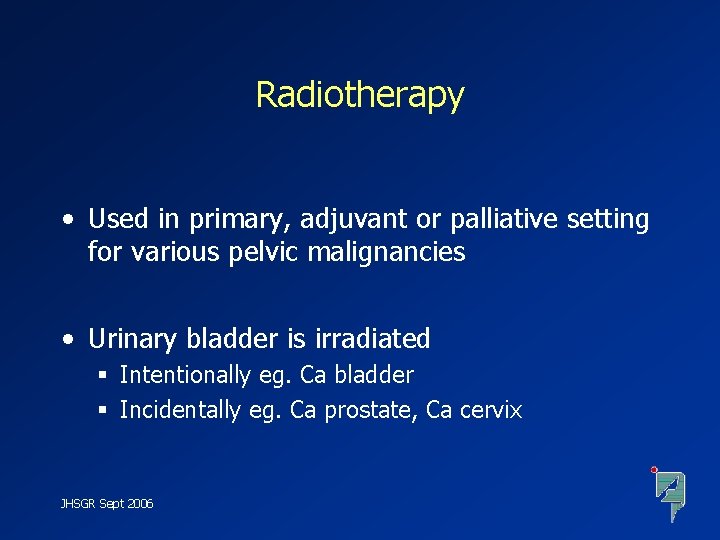
Radiotherapy • Used in primary, adjuvant or palliative setting for various pelvic malignancies • Urinary bladder is irradiated § Intentionally eg. Ca bladder § Incidentally eg. Ca prostate, Ca cervix JHSGR Sept 2006
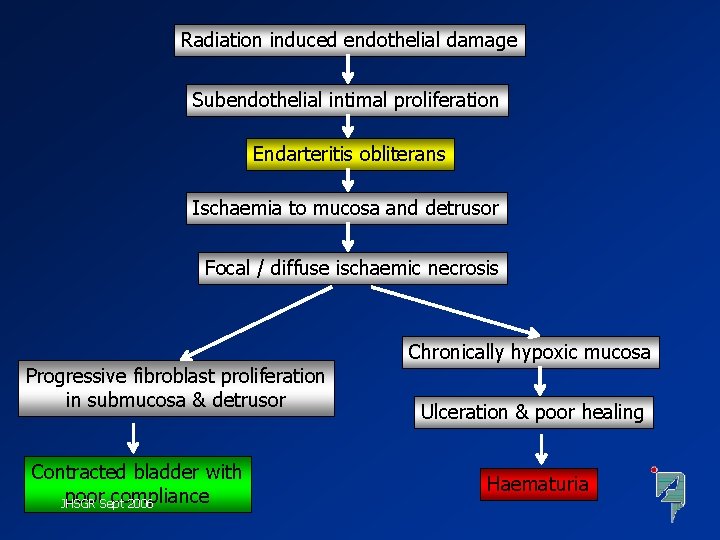
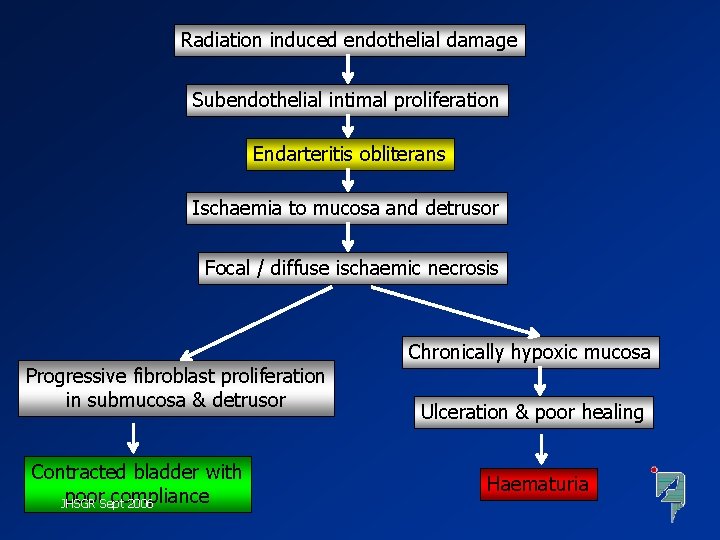
Radiation induced endothelial damage Subendothelial intimal proliferation Endarteritis obliterans Ischaemia to mucosa and detrusor Focal / diffuse ischaemic necrosis Progressive fibroblast proliferation in submucosa & detrusor Contracted bladder with poor. Sept compliance JHSGR 2006 Chronically hypoxic mucosa Ulceration & poor healing Haematuria
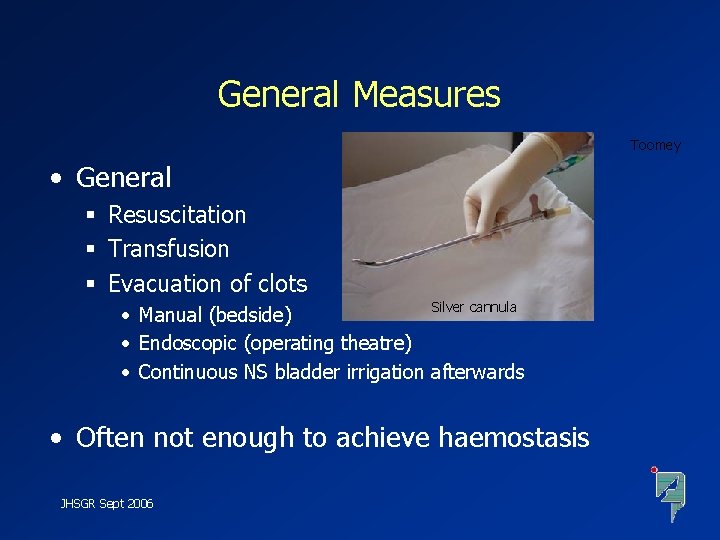
General Measures Toomey • General § Resuscitation § Transfusion § Evacuation of clots Silver cannula • Manual (bedside) • Endoscopic (operating theatre) • Continuous NS bladder irrigation afterwards • Often not enough to achieve haemostasis JHSGR Sept 2006
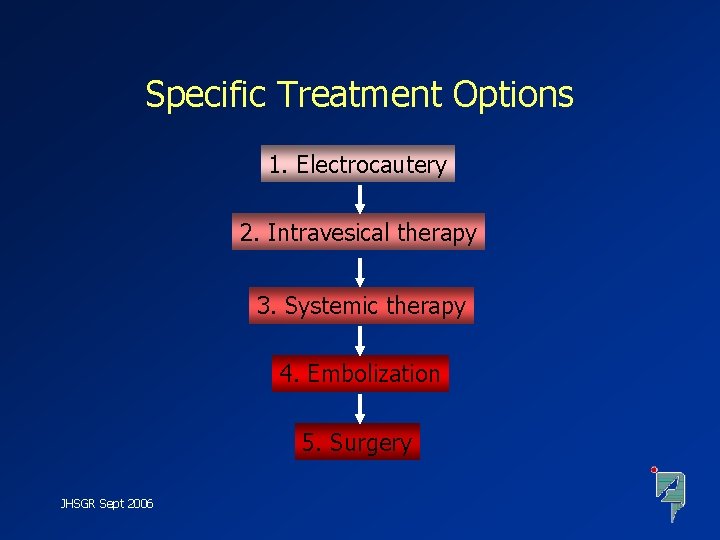
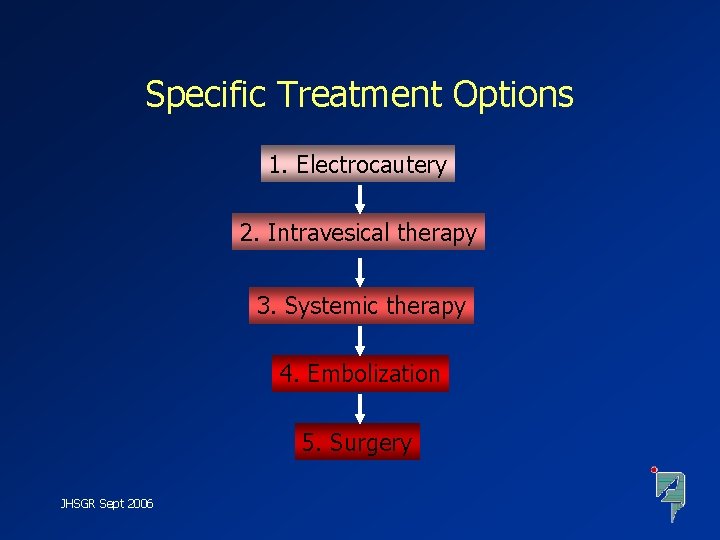
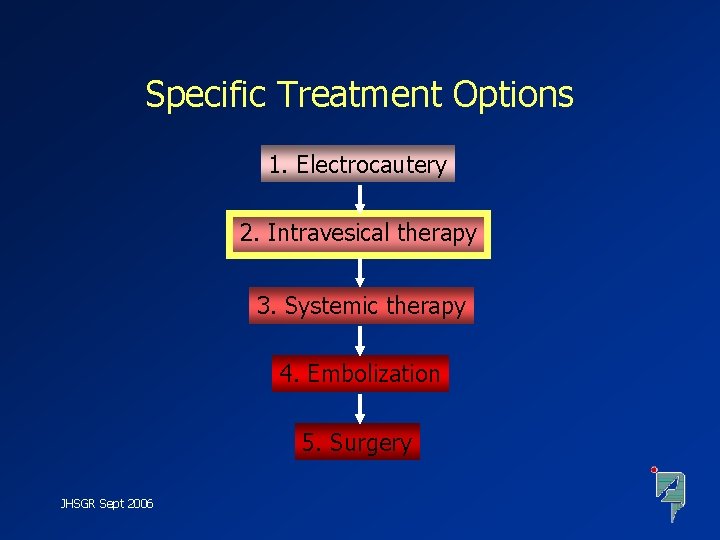
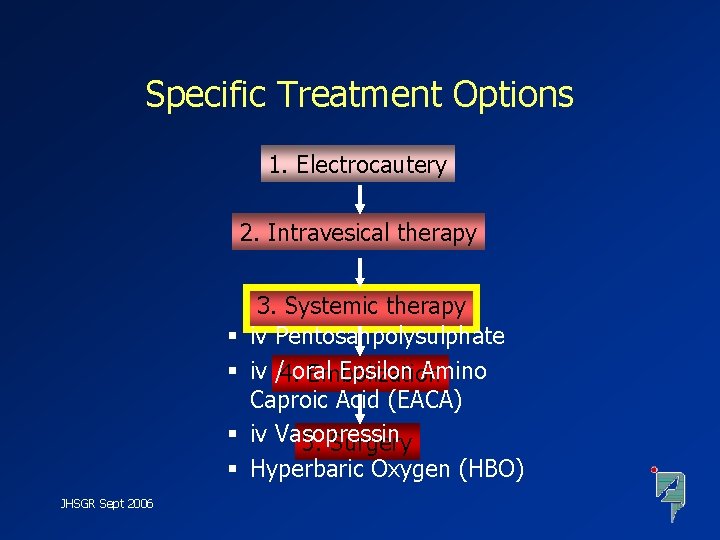
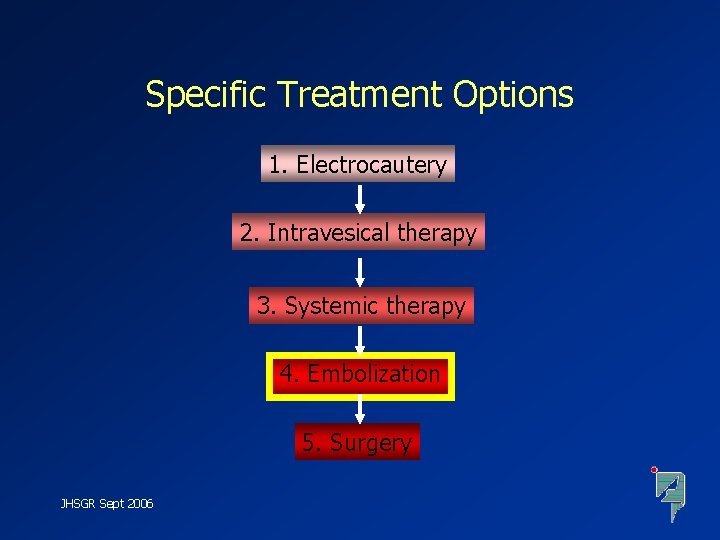
Specific Treatment Options 1. Electrocautery 2. Intravesical therapy 3. Systemic therapy 4. Embolization 5. Surgery JHSGR Sept 2006
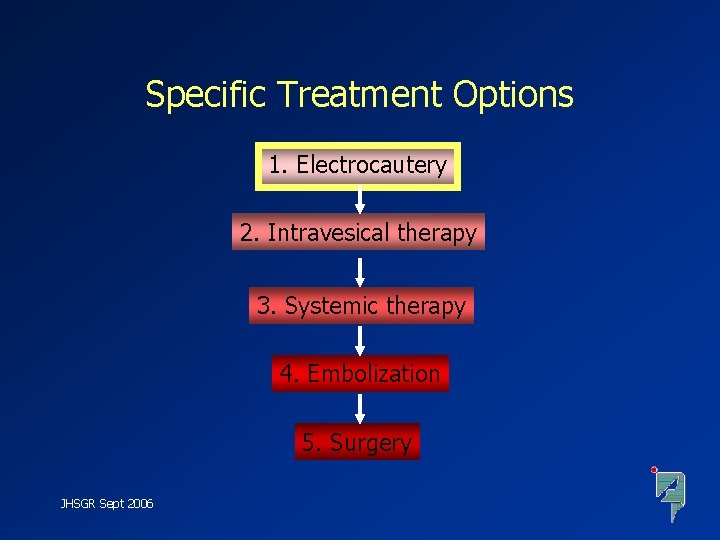
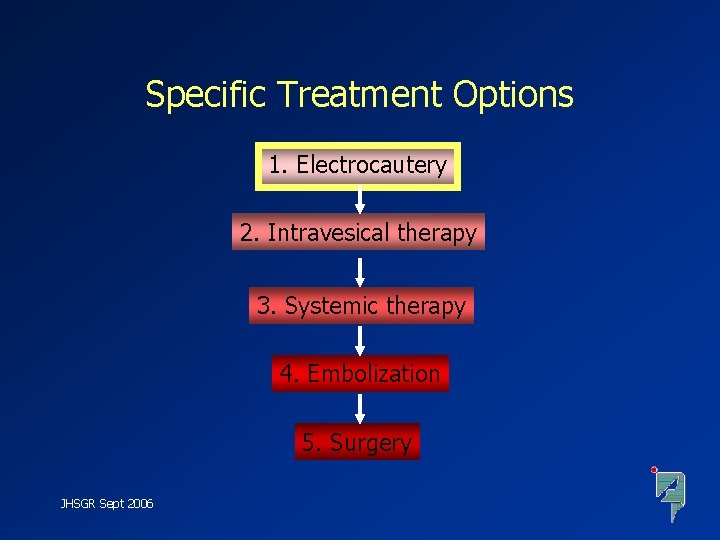
Specific Treatment Options 1. Electrocautery 2. Intravesical therapy 3. Systemic therapy 4. Embolization 5. Surgery JHSGR Sept 2006
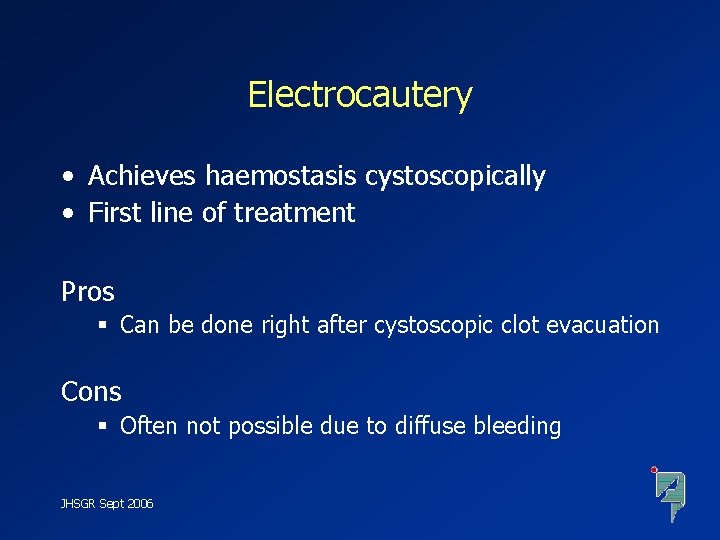
Electrocautery • Achieves haemostasis cystoscopically • First line of treatment Pros § Can be done right after cystoscopic clot evacuation Cons § Often not possible due to diffuse bleeding JHSGR Sept 2006
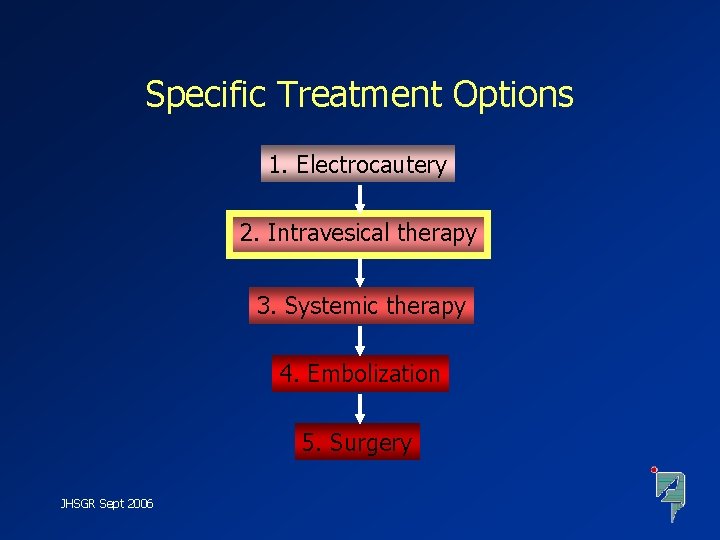
Specific Treatment Options 1. Electrocautery 2. Intravesical therapy 3. Systemic therapy 4. Embolization 5. Surgery JHSGR Sept 2006
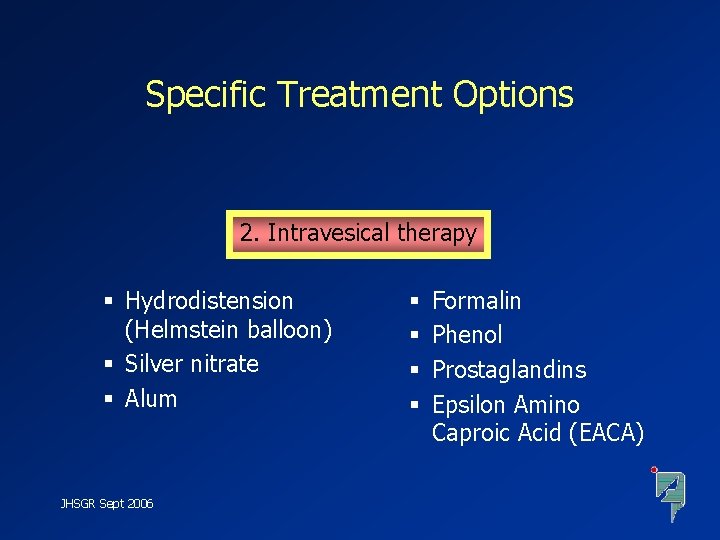
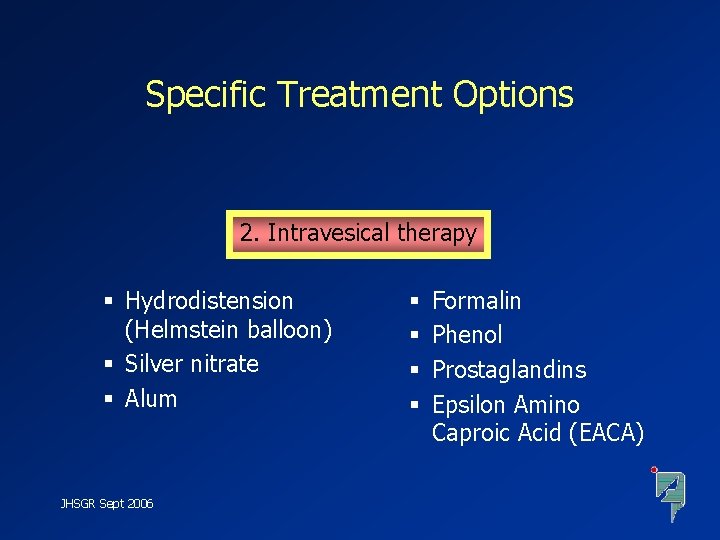
Specific Treatment Options 2. Intravesical therapy § Hydrodistension (Helmstein balloon) § Silver nitrate § Alum JHSGR Sept 2006 § § Formalin Phenol Prostaglandins Epsilon Amino Caproic Acid (EACA)
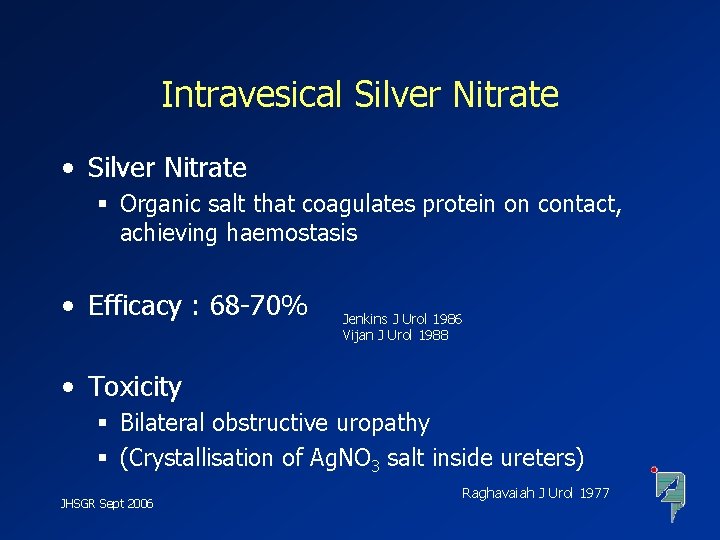
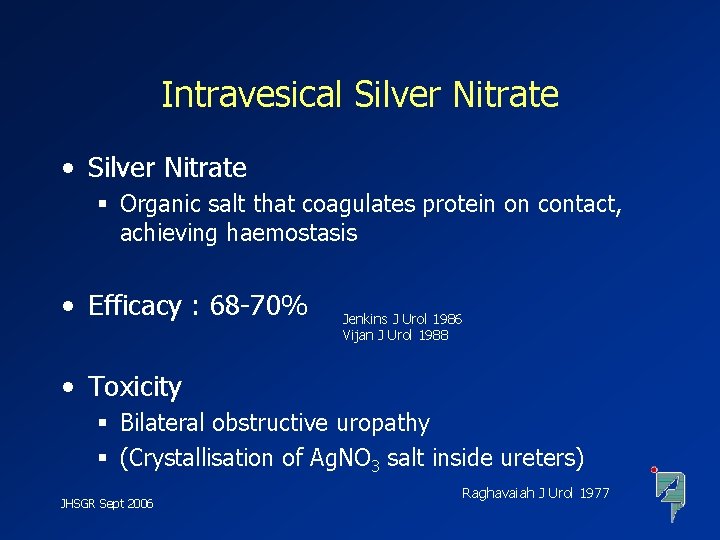
Intravesical Silver Nitrate • Silver Nitrate § Organic salt that coagulates protein on contact, achieving haemostasis • Efficacy : 68 -70% Jenkins J Urol 1986 Vijan J Urol 1988 • Toxicity § Bilateral obstructive uropathy § (Crystallisation of Ag. NO 3 salt inside ureters) JHSGR Sept 2006 Raghavaiah J Urol 1977
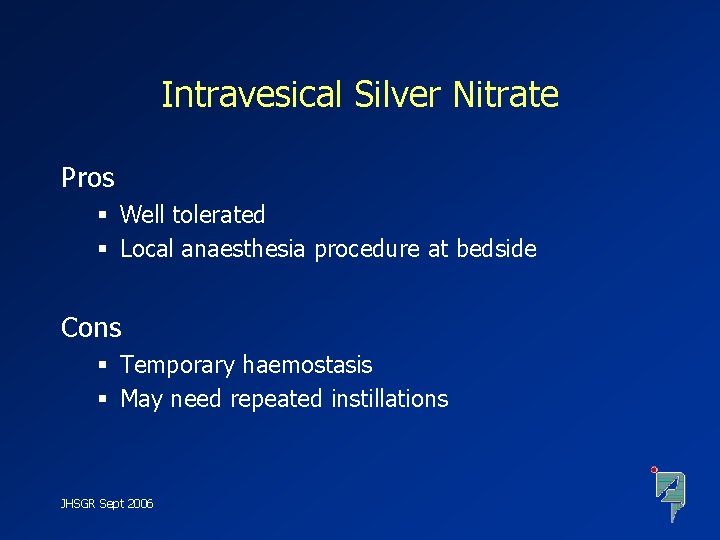
Intravesical Silver Nitrate Pros § Well tolerated § Local anaesthesia procedure at bedside Cons § Temporary haemostasis § May need repeated instillations JHSGR Sept 2006

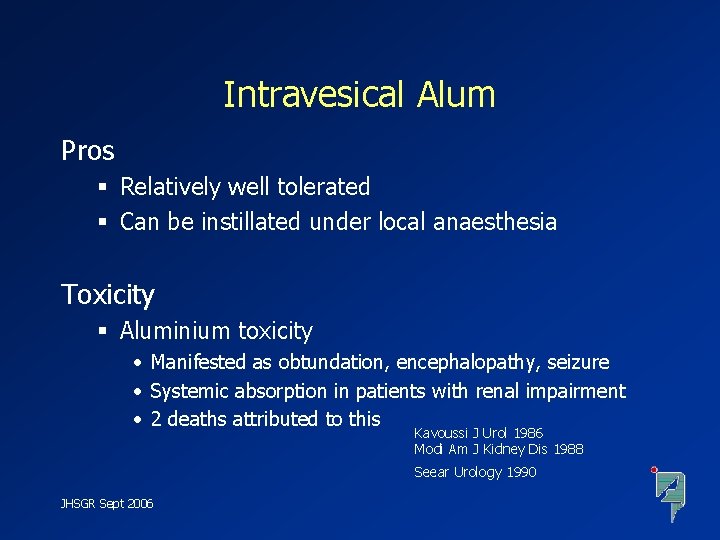
Intravesical Alum • Alum § Aluminium potassium sulfate § Industrial chemical to purify water • Reported efficacy : 67 -100% Kennedy BJU 1986 Arrizabalaga BJU 1987 Goel J Urol 1985 • Mechanism § Precipitates protein over bleeding vessels, causing vasoconstriction and haemostasis JHSGR Sept 2006
Intravesical Alum Pros § Relatively well tolerated § Can be instillated under local anaesthesia Toxicity § Aluminium toxicity • Manifested as obtundation, encephalopathy, seizure • Systemic absorption in patients with renal impairment • 2 deaths attributed to this Kavoussi J Urol 1986 Modi Am J Kidney Dis 1988 Seear Urology 1990 JHSGR Sept 2006

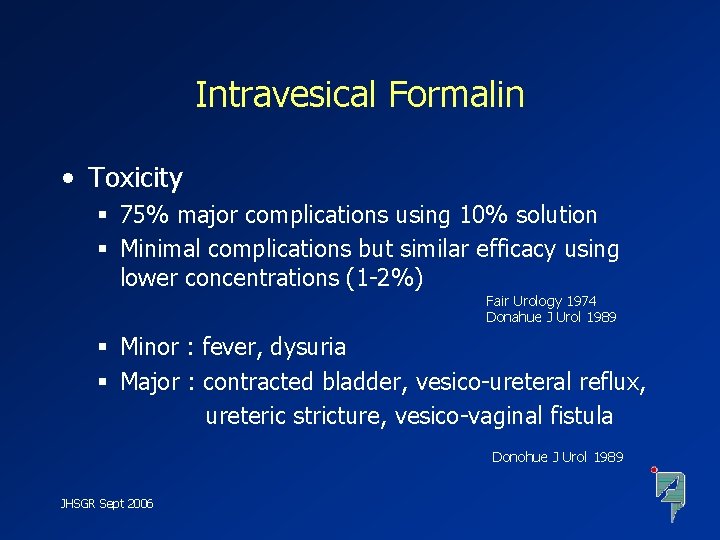
Intravesical Formalin • Formalin § Industrial chemical as tissue fixative and embalming agent • Efficacy : 80 -92% complete haemostasis Brown Med J Aust 1969 Kumar J Urol 1975 • Intravesical Formalin Shah J Urol 1973 § Cross-links proteins and precipitates it over mucosal surfaces, sealing off bleeding vessels JHSGR Sept 2006
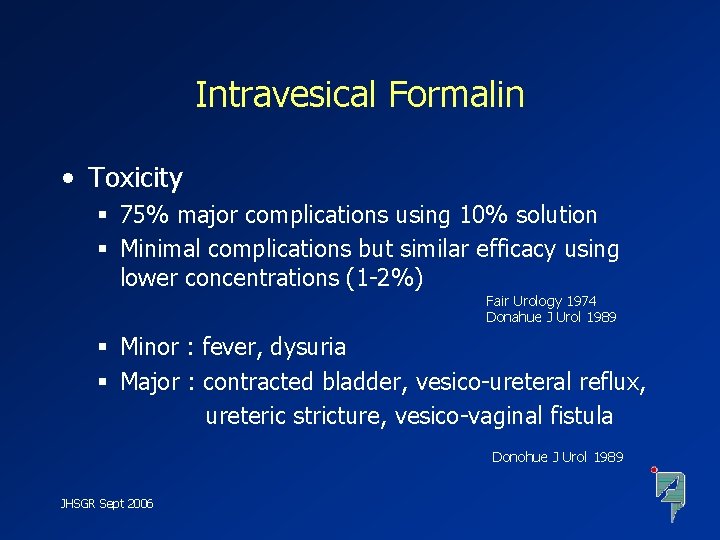
Intravesical Formalin • Toxicity § 75% major complications using 10% solution § Minimal complications but similar efficacy using lower concentrations (1 -2%) Fair Urology 1974 Donahue J Urol 1989 § Minor : fever, dysuria § Major : contracted bladder, vesico-ureteral reflux, ureteric stricture, vesico-vaginal fistula Donohue J Urol 1989 JHSGR Sept 2006
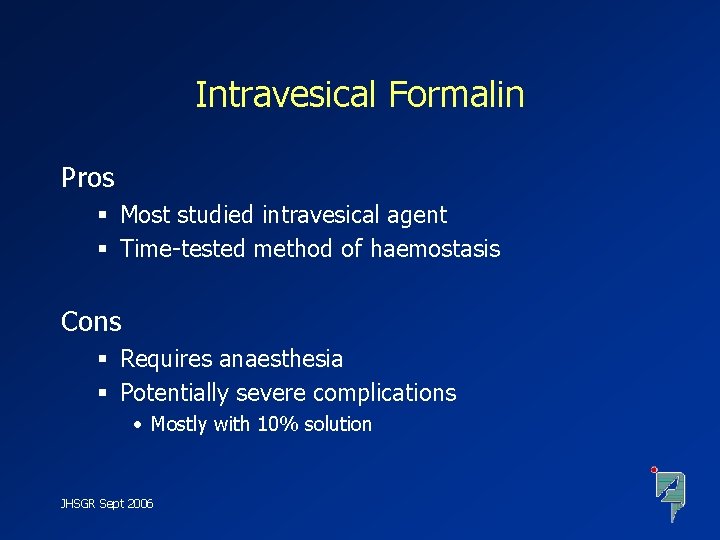
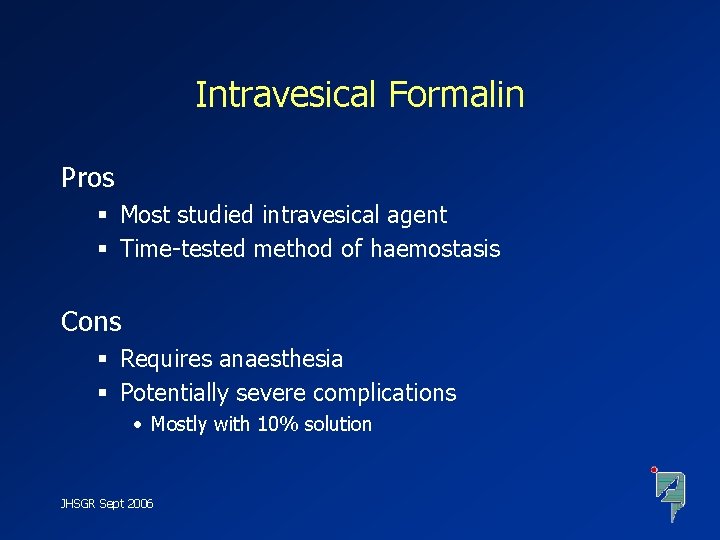
Intravesical Formalin Pros § Most studied intravesical agent § Time-tested method of haemostasis Cons § Requires anaesthesia § Potentially severe complications • Mostly with 10% solution JHSGR Sept 2006
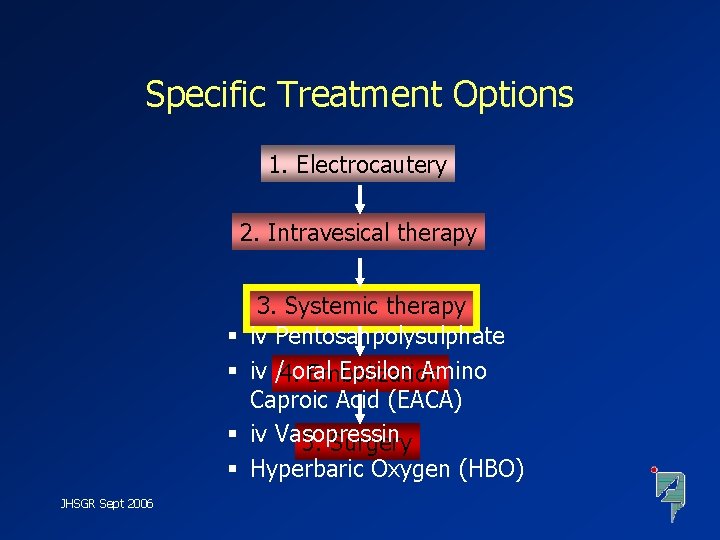
Specific Treatment Options 1. Electrocautery 2. Intravesical therapy § § JHSGR Sept 2006 3. Systemic therapy iv Pentosanpolysulphate iv /4. oral Epsilon Amino Embolization Caproic Acid (EACA) iv Vasopressin 5. Surgery Hyperbaric Oxygen (HBO)
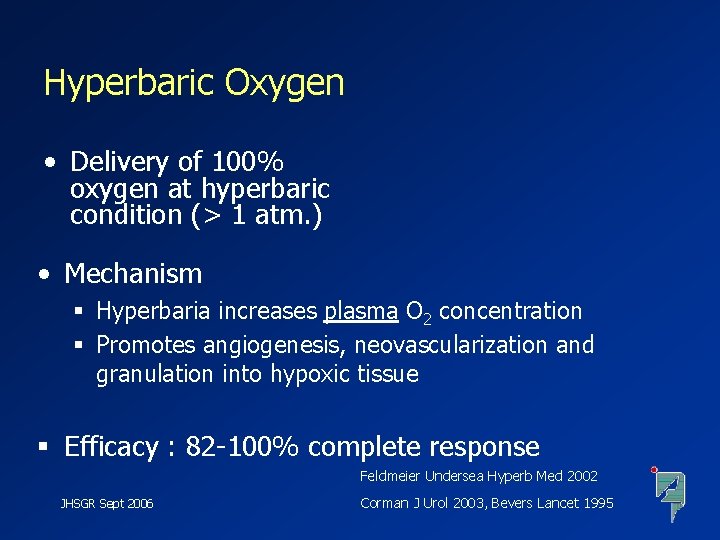
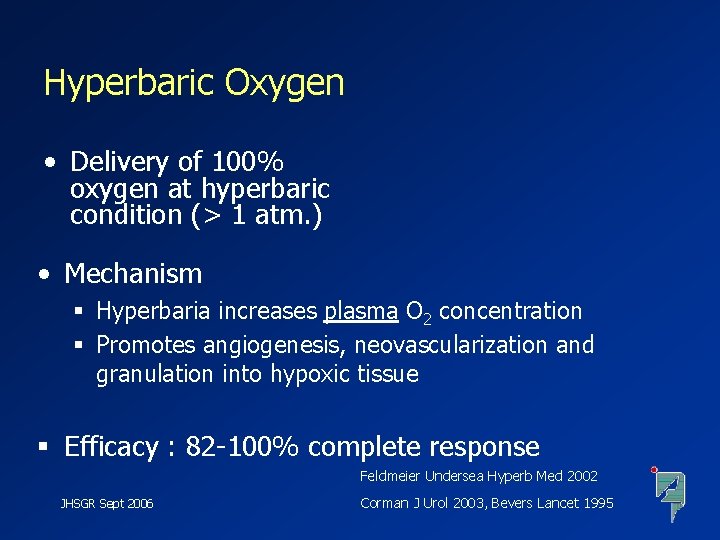
Hyperbaric Oxygen • Delivery of 100% oxygen at hyperbaric condition (> 1 atm. ) • Mechanism § Hyperbaria increases plasma O 2 concentration § Promotes angiogenesis, neovascularization and granulation into hypoxic tissue § Efficacy : 82 -100% complete response Feldmeier Undersea Hyperb Med 2002 JHSGR Sept 2006 Corman J Urol 2003, Bevers Lancet 1995
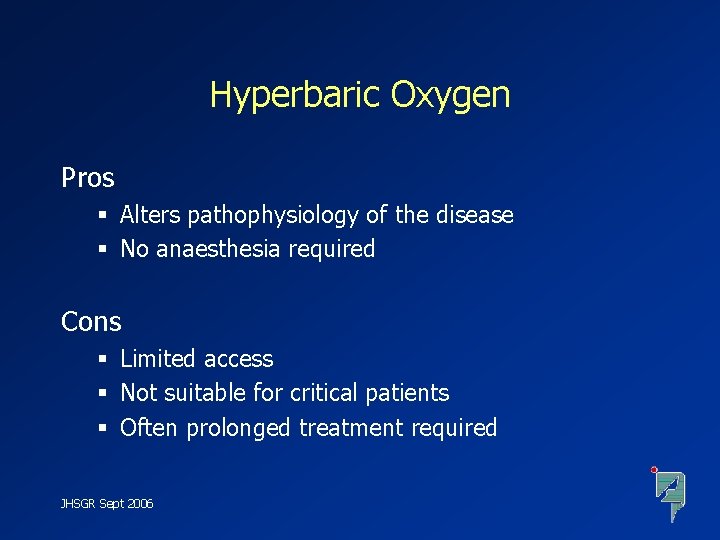
Hyperbaric Oxygen Pros § Alters pathophysiology of the disease § No anaesthesia required Cons § Limited access § Not suitable for critical patients § Often prolonged treatment required JHSGR Sept 2006
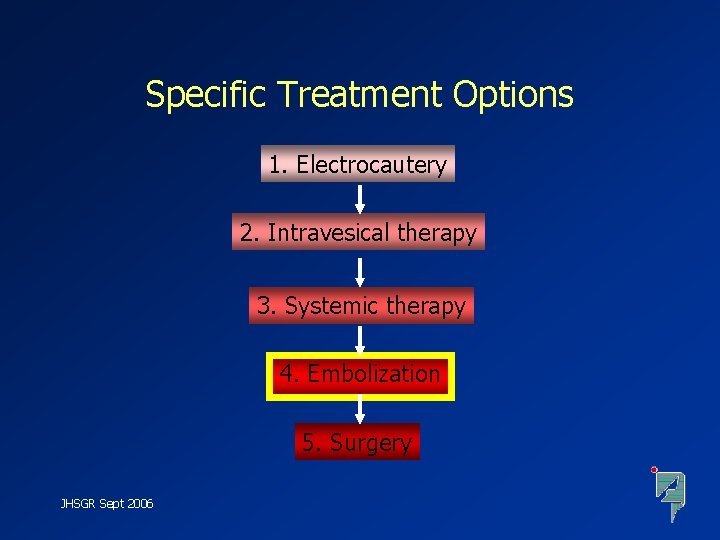
Specific Treatment Options 1. Electrocautery 2. Intravesical therapy 3. Systemic therapy 4. Embolization 5. Surgery JHSGR Sept 2006
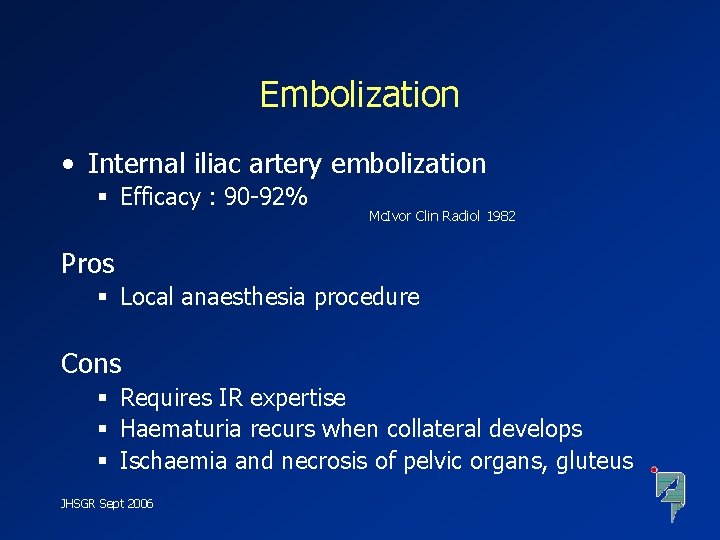
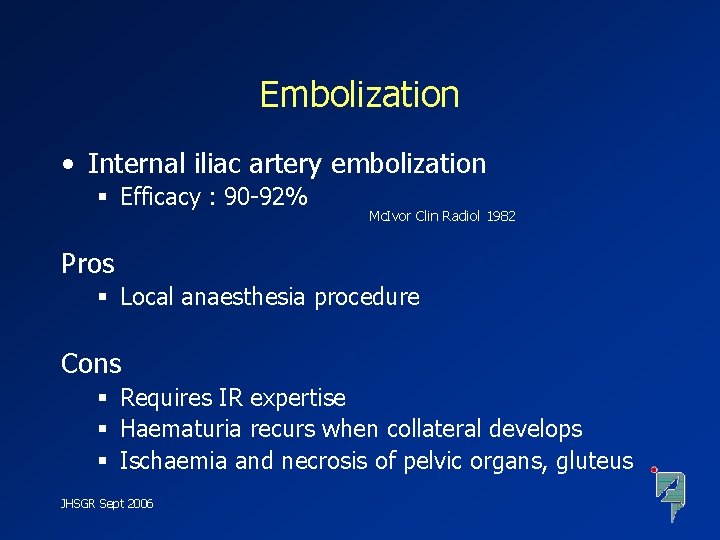
Embolization • Internal iliac artery embolization § Efficacy : 90 -92% Mc. Ivor Clin Radiol 1982 Pros § Local anaesthesia procedure Cons § Requires IR expertise § Haematuria recurs when collateral develops § Ischaemia and necrosis of pelvic organs, gluteus JHSGR Sept 2006
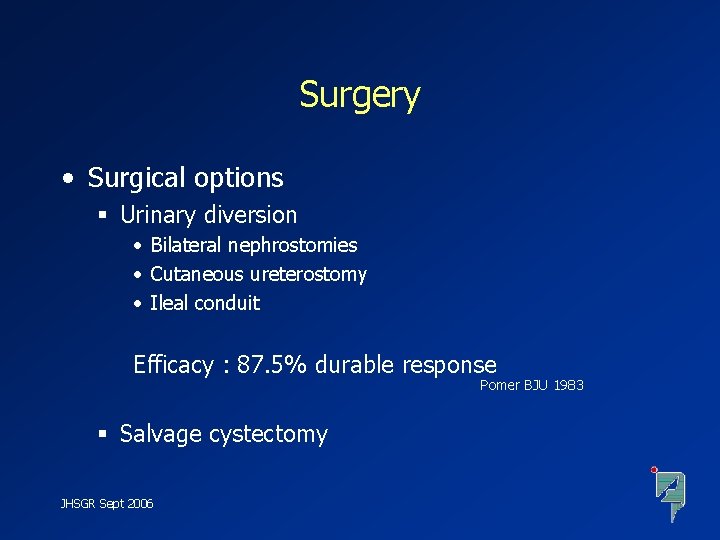
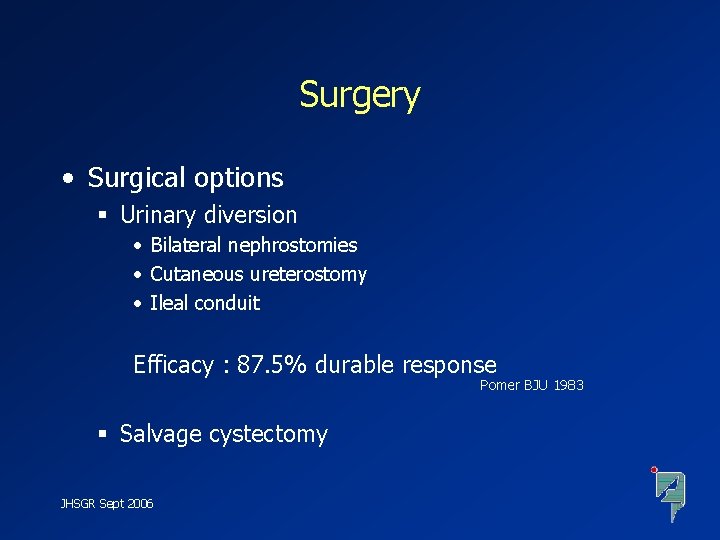
Surgery • Surgical options § Urinary diversion • Bilateral nephrostomies • Cutaneous ureterostomy • Ileal conduit Efficacy : 87. 5% durable response Pomer BJU 1983 § Salvage cystectomy JHSGR Sept 2006
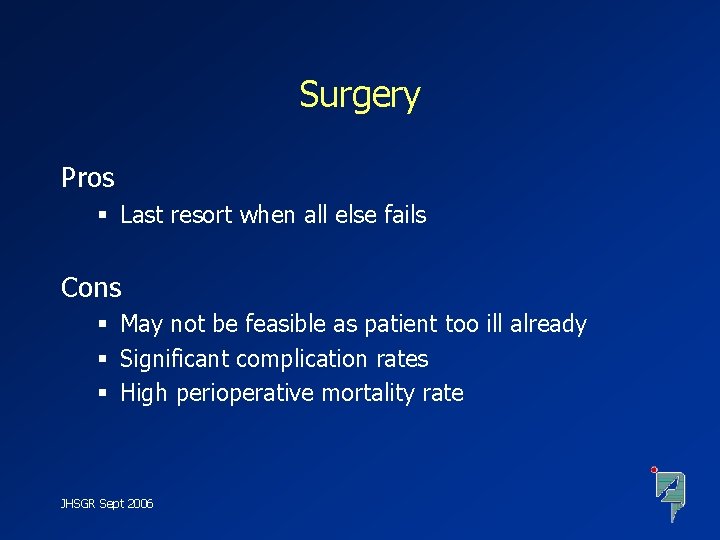
Surgery Pros § Last resort when all else fails Cons § May not be feasible as patient too ill already § Significant complication rates § High perioperative mortality rate JHSGR Sept 2006
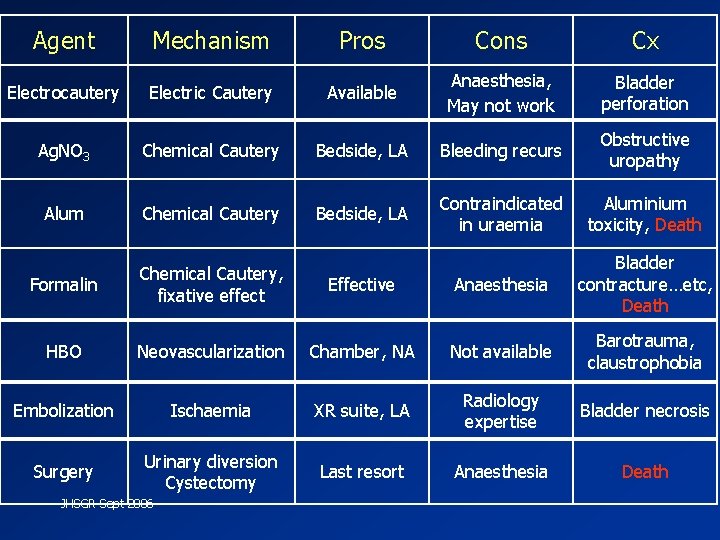
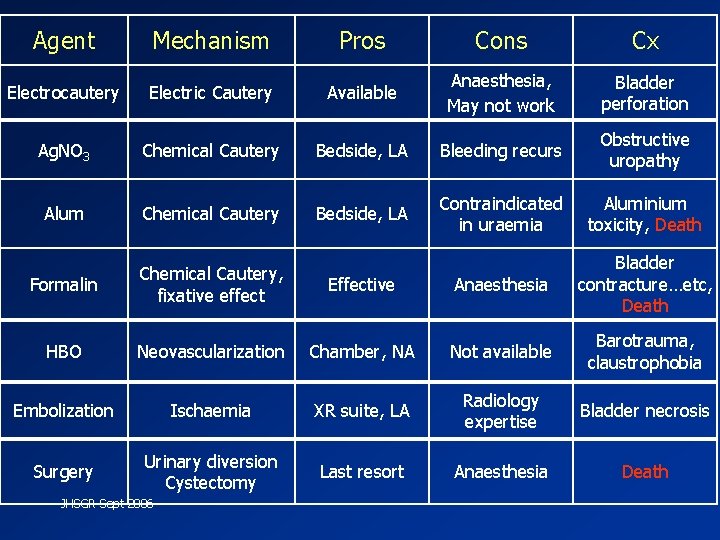
Agent Mechanism Pros Cons Cx Electrocautery Electric Cautery Available Anaesthesia, May not work Bladder perforation Ag. NO 3 Chemical Cautery Bedside, LA Bleeding recurs Obstructive uropathy Alum Chemical Cautery Bedside, LA Contraindicated in uraemia Aluminium toxicity, Death Formalin Chemical Cautery, fixative effect Effective Anaesthesia Bladder contracture…etc, Death HBO Neovascularization Chamber, NA Not available Barotrauma, claustrophobia Embolization Ischaemia XR suite, LA Radiology expertise Bladder necrosis Surgery Urinary diversion Cystectomy Last resort Anaesthesia Death JHSGR Sept 2006
To bring home • Post-irradiation haemorrhagic cystitis…. § A particularly difficult clinical problem of haemostasis for urologist § …. the practical management of which involves…. . JHSGR Sept 2006
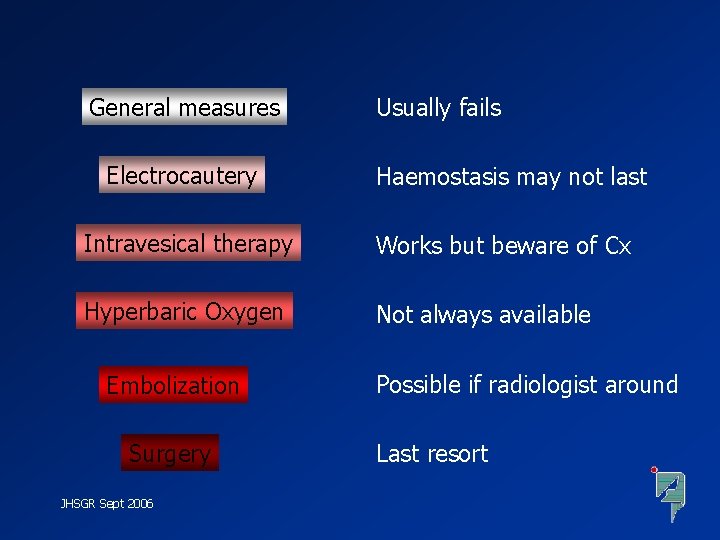
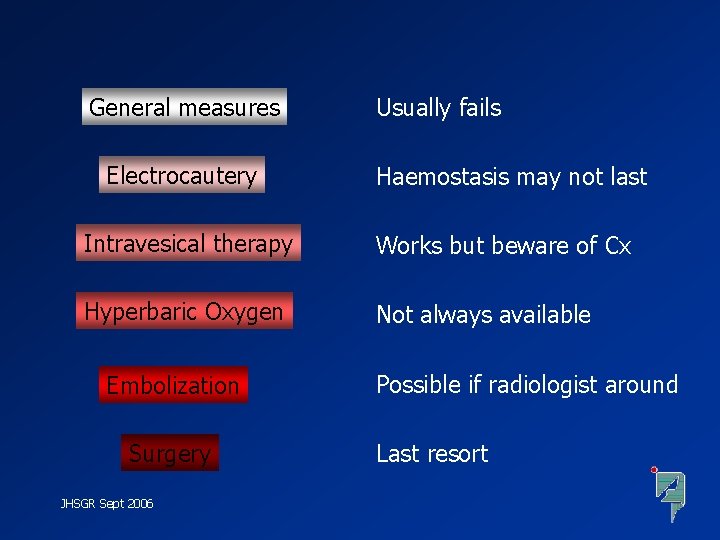
General measures Electrocautery Usually fails Haemostasis may not last Intravesical therapy Works but beware of Cx Hyperbaric Oxygen Not always available Embolization Surgery JHSGR Sept 2006 Possible if radiologist around Last resort
Thank you JHSGR Sept 2006
 Nitrofurantonin
Nitrofurantonin Thorium
Thorium Irradiation vs contamination
Irradiation vs contamination Cystitis physical exam findings
Cystitis physical exam findings Gamma irradiation sterilization process
Gamma irradiation sterilization process Cystitis cystica
Cystitis cystica Solar energy syllabus
Solar energy syllabus Ultra violet germicidal irradiation
Ultra violet germicidal irradiation Epidydmis
Epidydmis Sabulous cystitis
Sabulous cystitis Practical operations
Practical operations Practical investment management
Practical investment management Angelo kinicki management: a practical introduction
Angelo kinicki management: a practical introduction Read management: a practical introduction online
Read management: a practical introduction online Practical financial management
Practical financial management Management a practical introduction
Management a practical introduction Management a practical introduction 3e
Management a practical introduction 3e Kinicki: management: a practical introduction 3rd edition
Kinicki: management: a practical introduction 3rd edition Post fall management
Post fall management Post stocking management
Post stocking management Nursing intervention of cataract
Nursing intervention of cataract Four fish nursery management practices
Four fish nursery management practices Post award contract management
Post award contract management Post harvest management definition
Post harvest management definition Post harvest management of sugarcane
Post harvest management of sugarcane Post operative nursing care
Post operative nursing care Preoperative checklist definition
Preoperative checklist definition Obsessive compulsive disorder nursing interventions
Obsessive compulsive disorder nursing interventions Top management and middle management
Top management and middle management Management pyramid
Management pyramid