Pheochromocytoma Dr Atallah AlRuhaily Pheochromocytoma 1 2 Catecholamine




- Slides: 48
Pheochromocytoma Dr. Atallah Al-Ruhaily
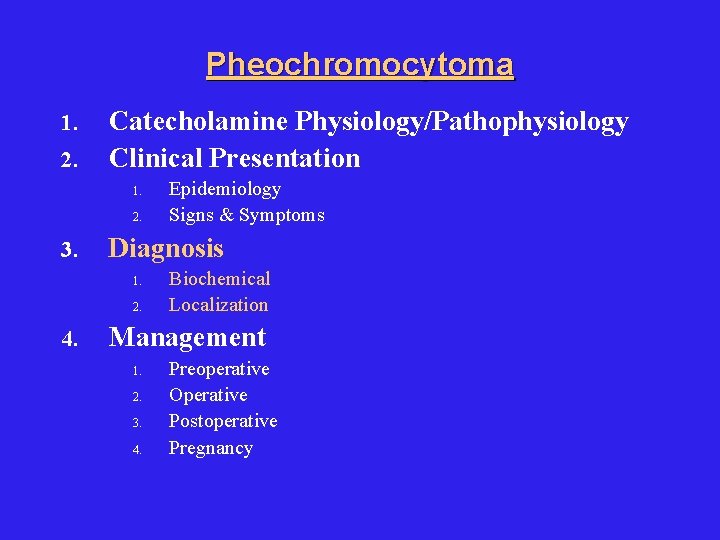
Pheochromocytoma 1. 2. Catecholamine Physiology/Pathophysiology Clinical Presentation 1. 2. 3. Diagnosis 1. 2. 4. Epidemiology Signs & Symptoms Biochemical Localization Management 1. 2. 3. 4. Preoperative Operative Postoperative Pregnancy
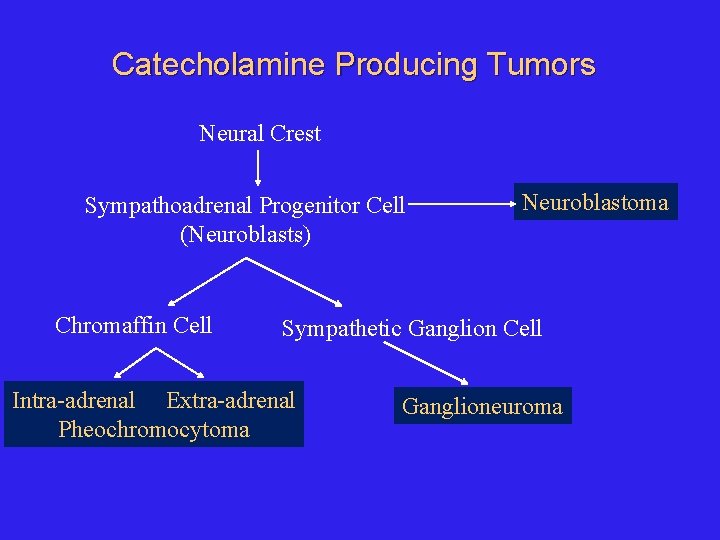
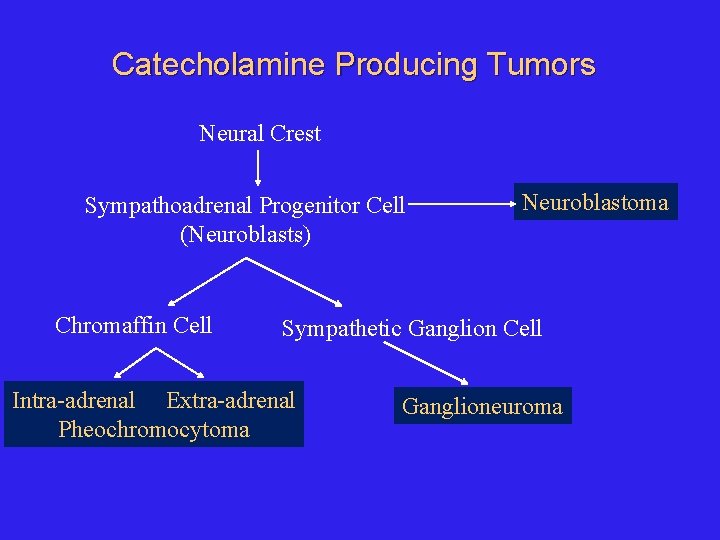
Catecholamine Producing Tumors Neural Crest Sympathoadrenal Progenitor Cell (Neuroblasts) Chromaffin Cell Neuroblastoma Sympathetic Ganglion Cell Intra-adrenal Extra-adrenal Pheochromocytoma Ganglioneuroma
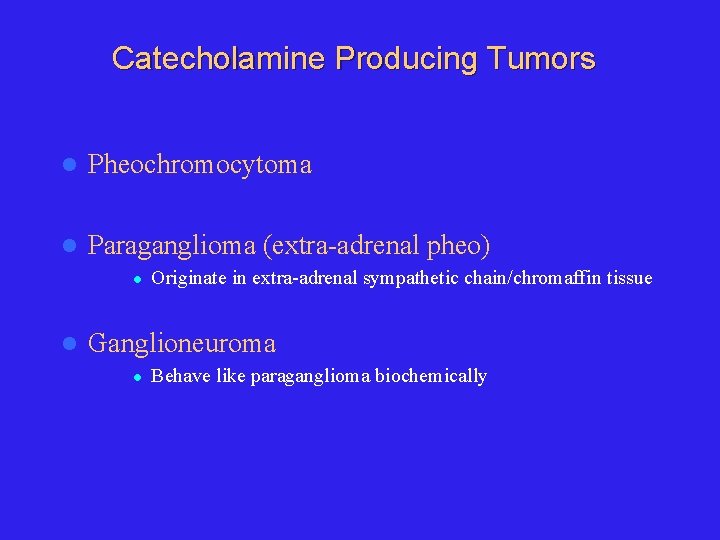
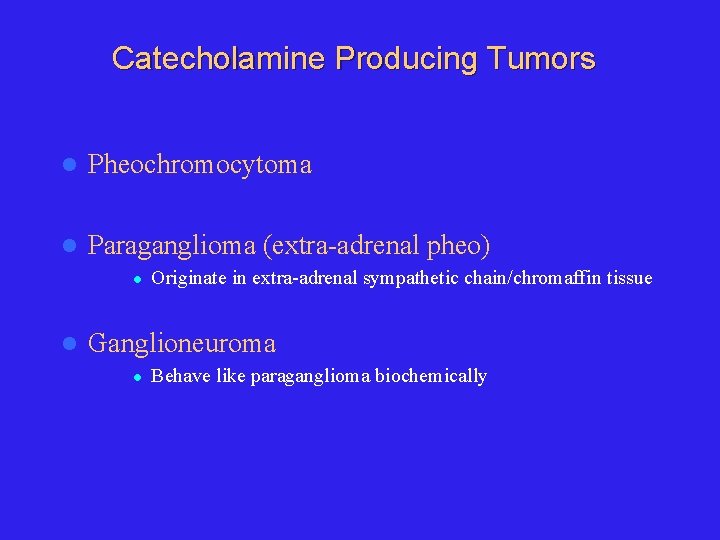
Catecholamine Producing Tumors l Pheochromocytoma l Paraganglioma (extra-adrenal pheo) l l Originate in extra-adrenal sympathetic chain/chromaffin tissue Ganglioneuroma l Behave like paraganglioma biochemically
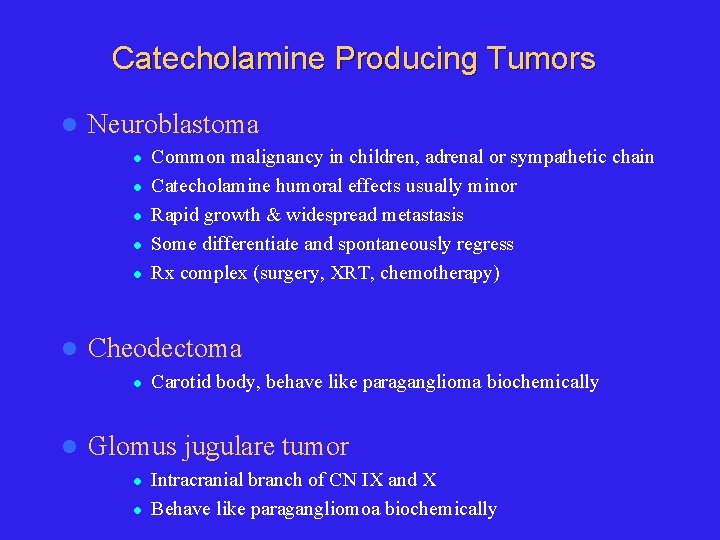
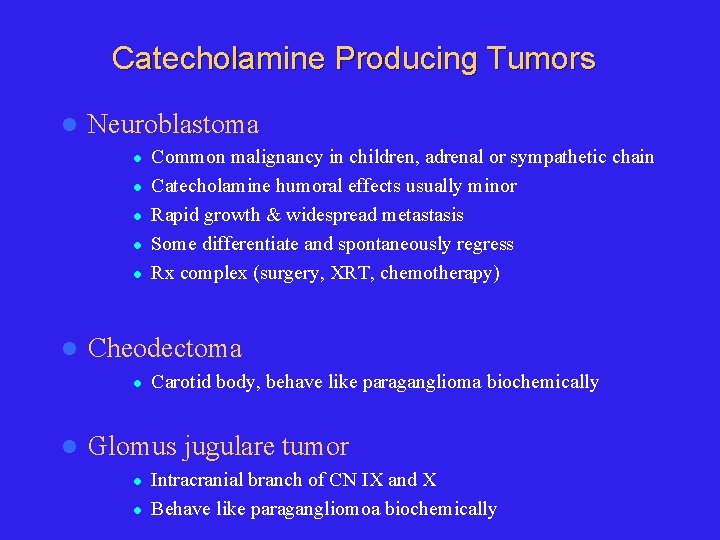
Catecholamine Producing Tumors l Neuroblastoma l l l Cheodectoma l l Common malignancy in children, adrenal or sympathetic chain Catecholamine humoral effects usually minor Rapid growth & widespread metastasis Some differentiate and spontaneously regress Rx complex (surgery, XRT, chemotherapy) Carotid body, behave like paraganglioma biochemically Glomus jugulare tumor l l Intracranial branch of CN IX and X Behave like paragangliomoa biochemically
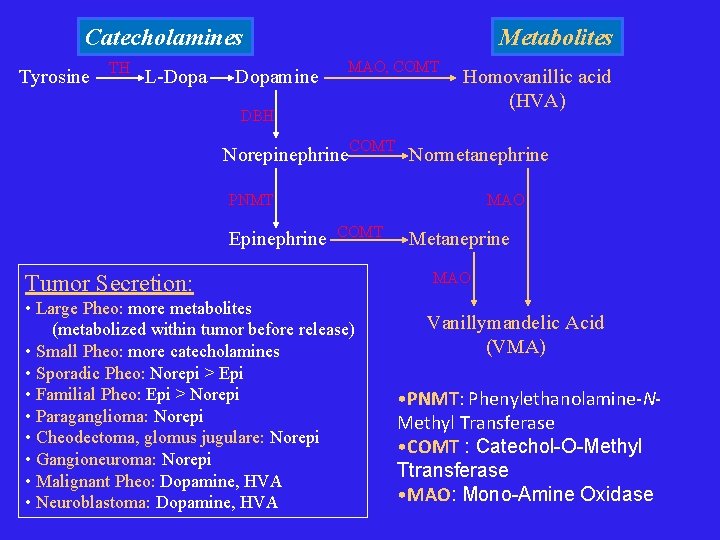
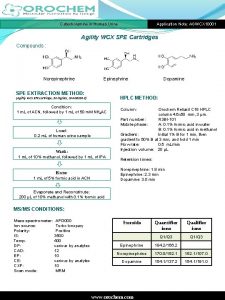
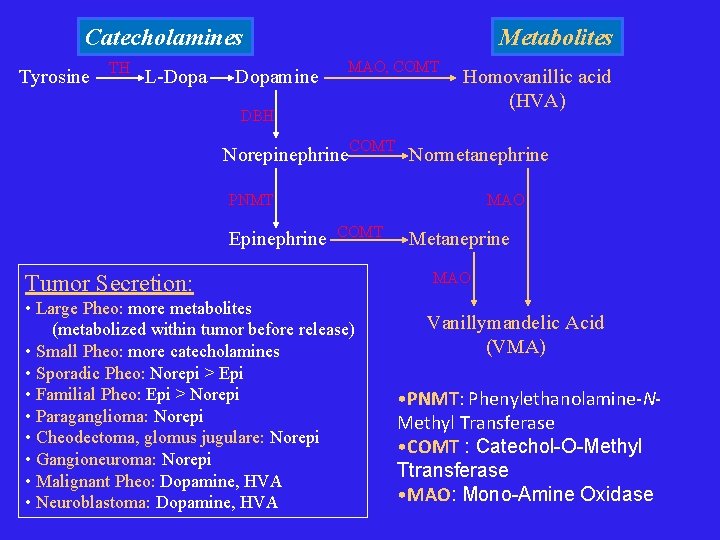
Catecholamines Tyrosine TH L-Dopamine Metabolites MAO, COMT DBH Homovanillic acid (HVA) Norepinephrine. COMT Normetanephrine PNMT Epinephrine MAO COMT Tumor Secretion: • Large Pheo: more metabolites (metabolized within tumor before release) • Small Pheo: more catecholamines • Sporadic Pheo: Norepi > Epi • Familial Pheo: Epi > Norepi • Paraganglioma: Norepi • Cheodectoma, glomus jugulare: Norepi • Gangioneuroma: Norepi • Malignant Pheo: Dopamine, HVA • Neuroblastoma: Dopamine, HVA Metaneprine MAO Vanillymandelic Acid (VMA) • PNMT: Phenylethanolamine-NMethyl Transferase • COMT : Catechol-O-Methyl Ttransferase • MAO: Mono-Amine Oxidase
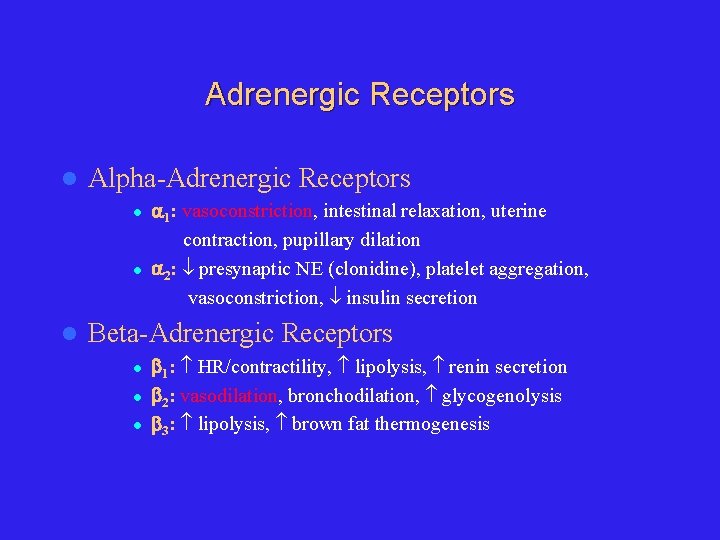
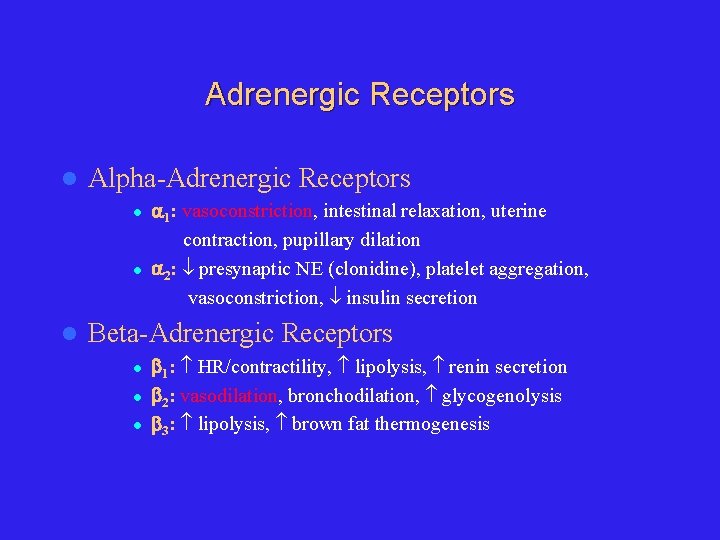
Adrenergic Receptors l Alpha-Adrenergic Receptors l l l 1: vasoconstriction, intestinal relaxation, uterine contraction, pupillary dilation 2: presynaptic NE (clonidine), platelet aggregation, vasoconstriction, insulin secretion Beta-Adrenergic Receptors l l l 1: HR/contractility, lipolysis, renin secretion 2: vasodilation, bronchodilation, glycogenolysis 3: lipolysis, brown fat thermogenesis
Pheochromocytoma 1. 2. Catecholamine Physiology/Pathophysiology Clinical Presentation 1. 2. 3. Diagnosis 1. 2. 4. Epidemiology Signs & Symptoms Biochemical Localization Management 1. 2. 3. 4. Preoperative Operative Postoperative Pregnancy
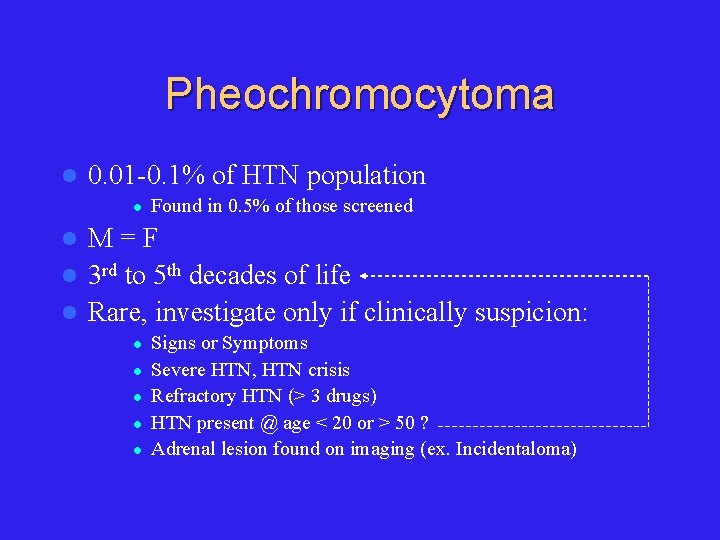
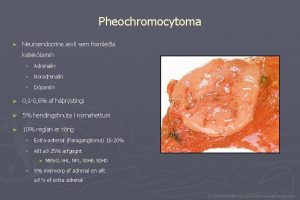
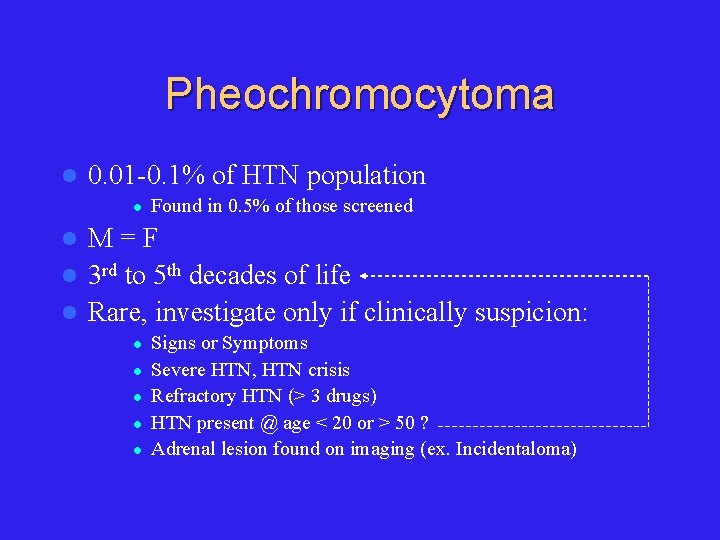
Pheochromocytoma l 0. 01 -0. 1% of HTN population l Found in 0. 5% of those screened M=F l 3 rd to 5 th decades of life l Rare, investigate only if clinically suspicion: l l l Signs or Symptoms Severe HTN, HTN crisis Refractory HTN (> 3 drugs) HTN present @ age < 20 or > 50 ? Adrenal lesion found on imaging (ex. Incidentaloma)
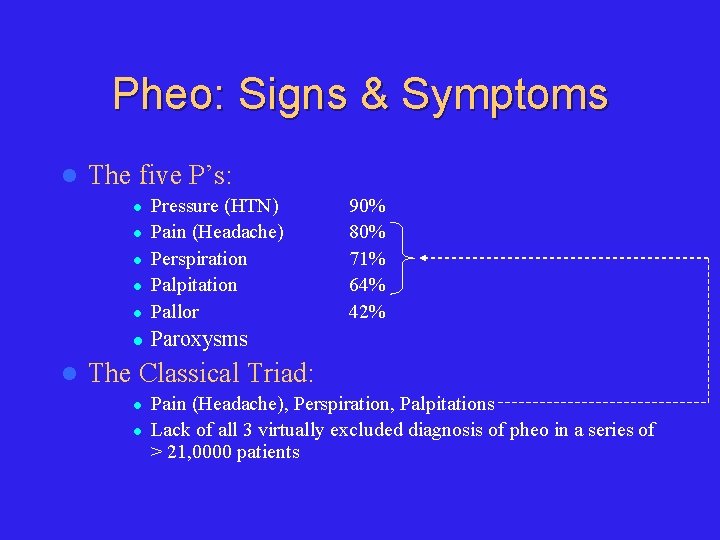
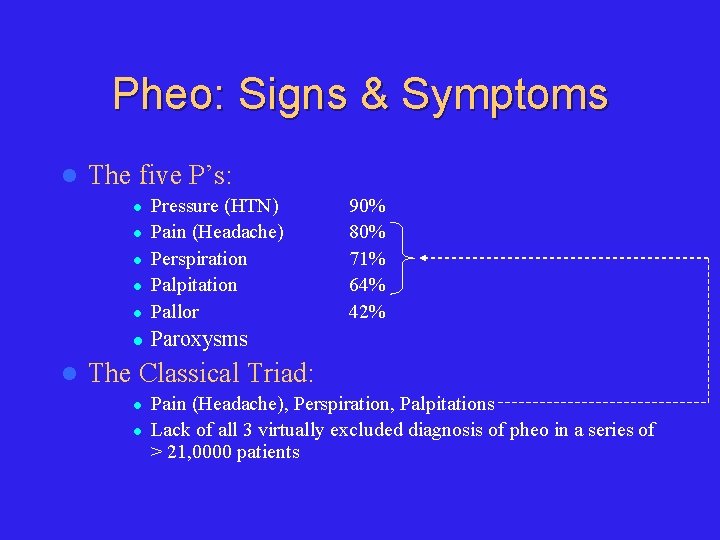
Pheo: Signs & Symptoms l The five P’s: l Pressure (HTN) Pain (Headache) Perspiration Palpitation Pallor l Paroxysms l l l 90% 80% 71% 64% 42% The Classical Triad: l l Pain (Headache), Perspiration, Palpitations Lack of all 3 virtually excluded diagnosis of pheo in a series of > 21, 0000 patients
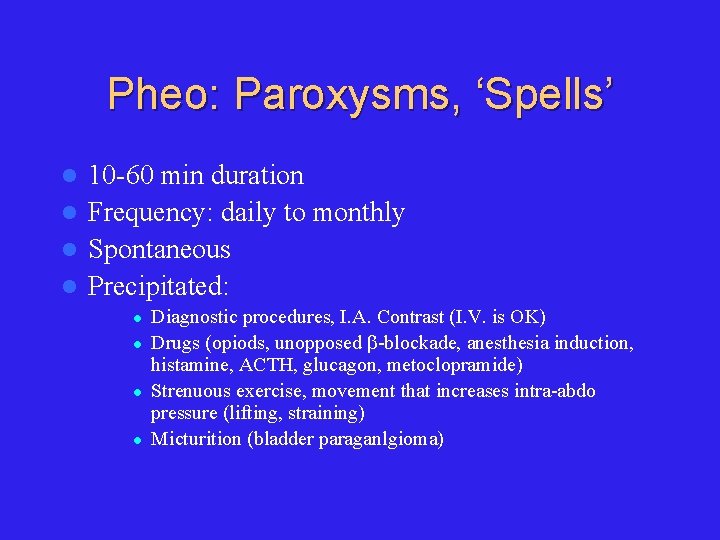
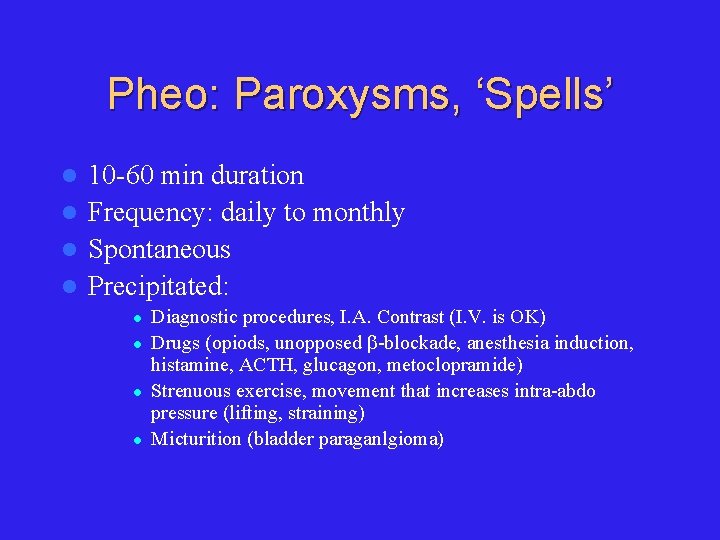
Pheo: Paroxysms, ‘Spells’ 10 -60 min duration l Frequency: daily to monthly l Spontaneous l Precipitated: l l l Diagnostic procedures, I. A. Contrast (I. V. is OK) Drugs (opiods, unopposed -blockade, anesthesia induction, histamine, ACTH, glucagon, metoclopramide) Strenuous exercise, movement that increases intra-abdo pressure (lifting, straining) Micturition (bladder paraganlgioma)
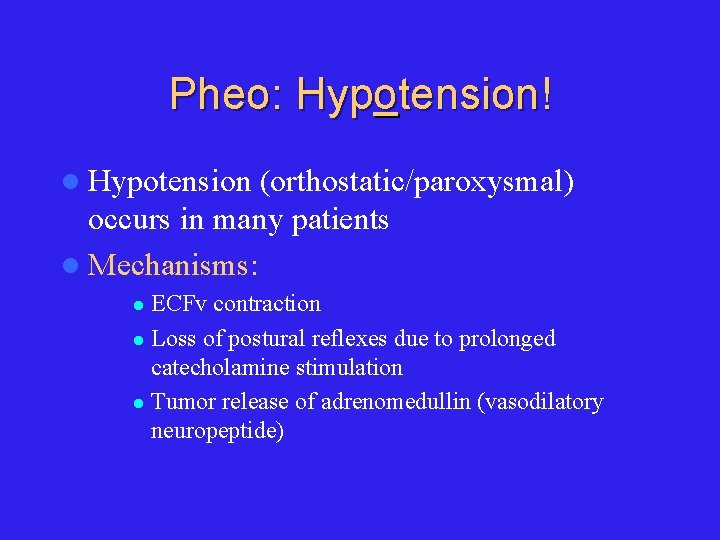
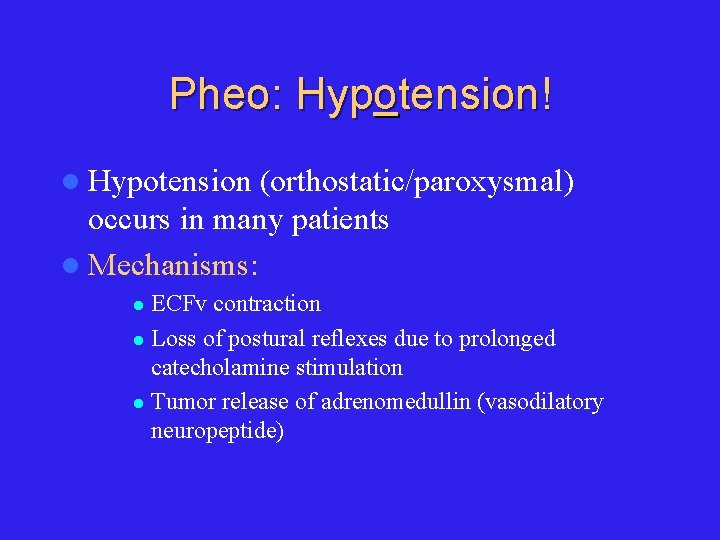
Pheo: Hypotension! l Hypotension (orthostatic/paroxysmal) occurs in many patients l Mechanisms: ECFv contraction l Loss of postural reflexes due to prolonged catecholamine stimulation l Tumor release of adrenomedullin (vasodilatory neuropeptide) l
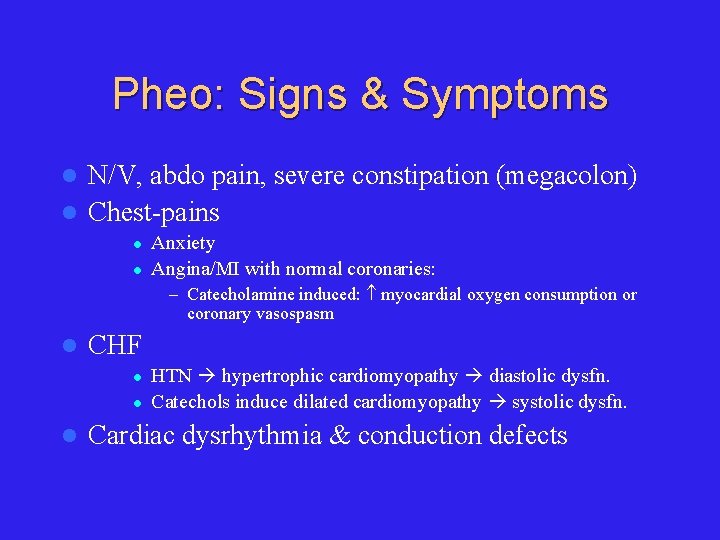
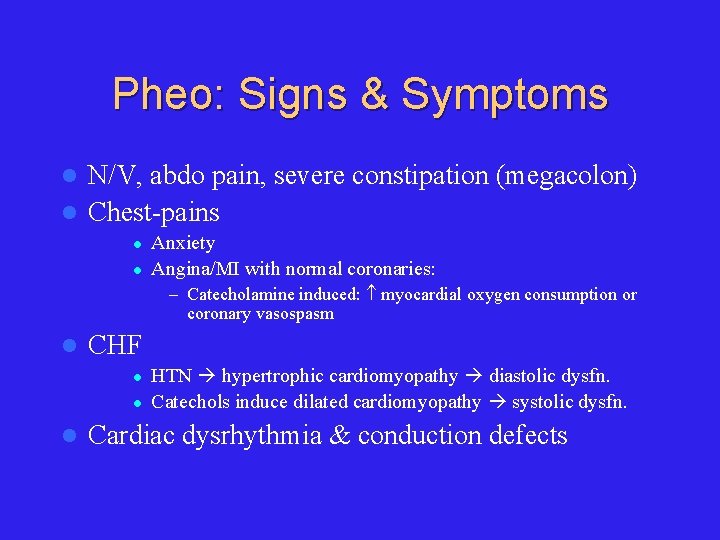
Pheo: Signs & Symptoms N/V, abdo pain, severe constipation (megacolon) l Chest-pains l l l Anxiety Angina/MI with normal coronaries: – Catecholamine induced: myocardial oxygen consumption or coronary vasospasm l CHF l l l HTN hypertrophic cardiomyopathy diastolic dysfn. Catechols induce dilated cardiomyopathy systolic dysfn. Cardiac dysrhythmia & conduction defects
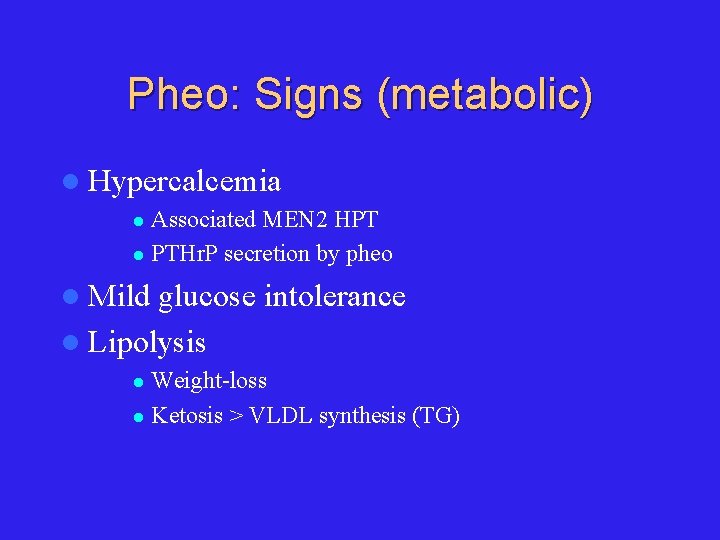
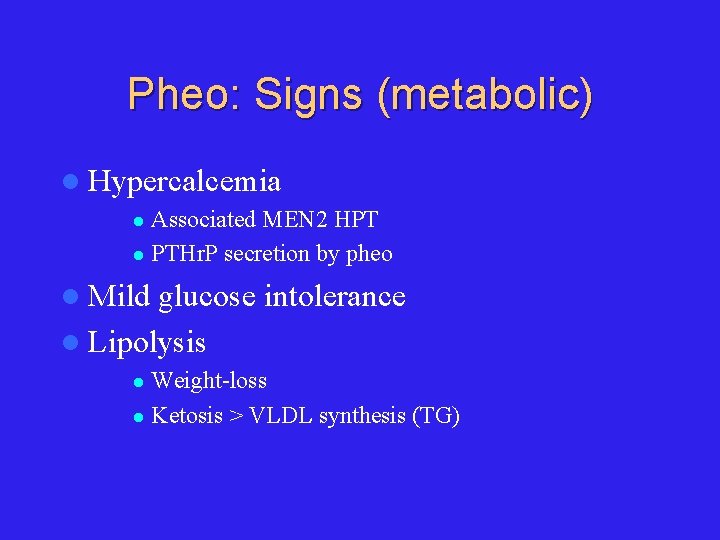
Pheo: Signs (metabolic) l Hypercalcemia Associated MEN 2 HPT l PTHr. P secretion by pheo l l Mild glucose intolerance l Lipolysis Weight-loss l Ketosis > VLDL synthesis (TG) l
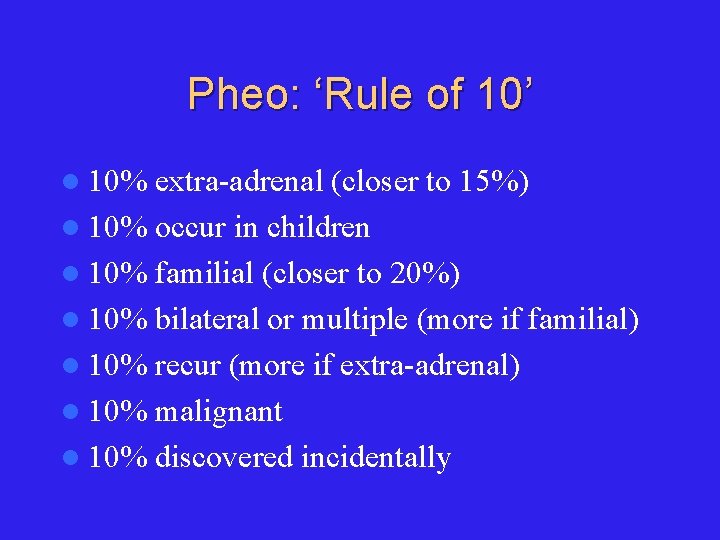
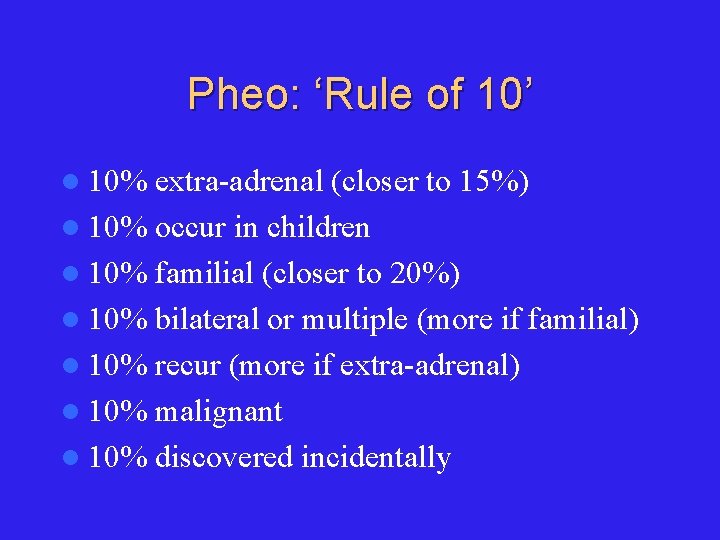
Pheo: ‘Rule of 10’ l 10% extra-adrenal (closer to 15%) l 10% occur in children l 10% familial (closer to 20%) l 10% bilateral or multiple (more if familial) l 10% recur (more if extra-adrenal) l 10% malignant l 10% discovered incidentally
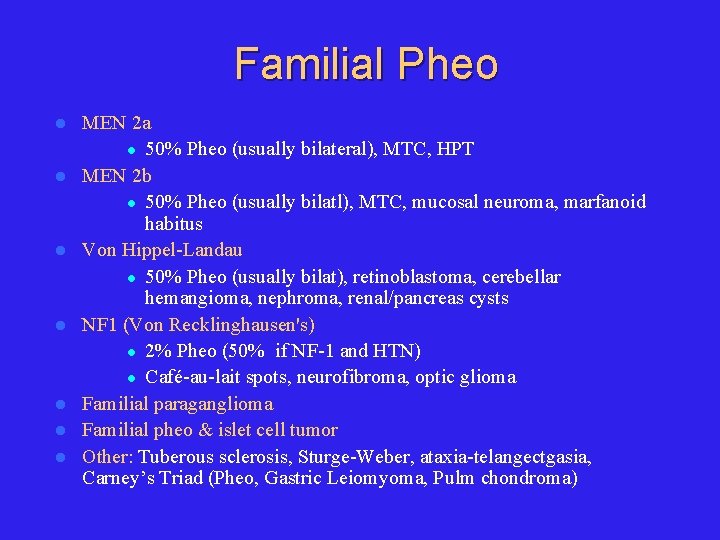
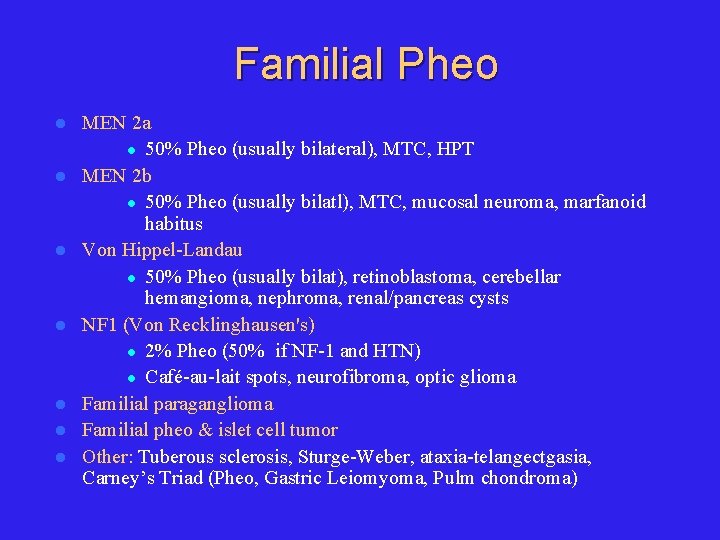
Familial Pheo l l l l MEN 2 a l 50% Pheo (usually bilateral), MTC, HPT MEN 2 b l 50% Pheo (usually bilatl), MTC, mucosal neuroma, marfanoid habitus Von Hippel-Landau l 50% Pheo (usually bilat), retinoblastoma, cerebellar hemangioma, nephroma, renal/pancreas cysts NF 1 (Von Recklinghausen's) l 2% Pheo (50% if NF-1 and HTN) l Café-au-lait spots, neurofibroma, optic glioma Familial paraganglioma Familial pheo & islet cell tumor Other: Tuberous sclerosis, Sturge-Weber, ataxia-telangectgasia, Carney’s Triad (Pheo, Gastric Leiomyoma, Pulm chondroma)
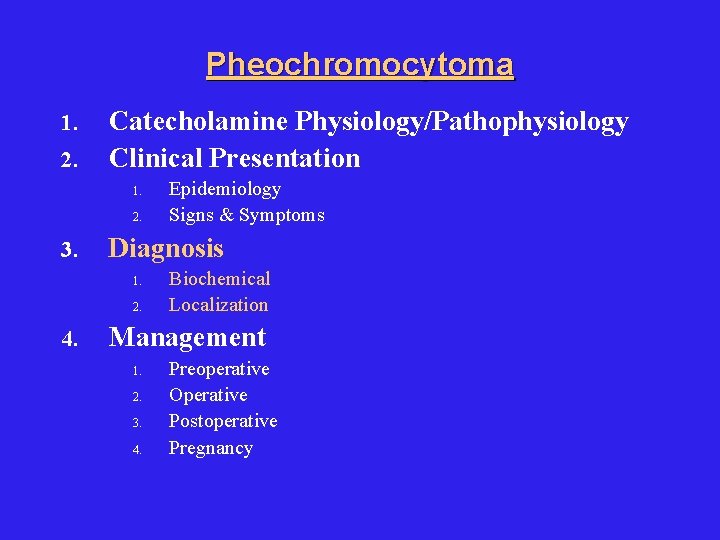
Pheochromocytoma 1. 2. Catecholamine Physiology/Pathophysiology Clinical Presentation 1. 2. 3. Diagnosis 1. 2. 4. Epidemiology Signs & Symptoms Biochemical Localization Management 1. 2. 3. 4. Preoperative Operative Postoperative Pregnancy
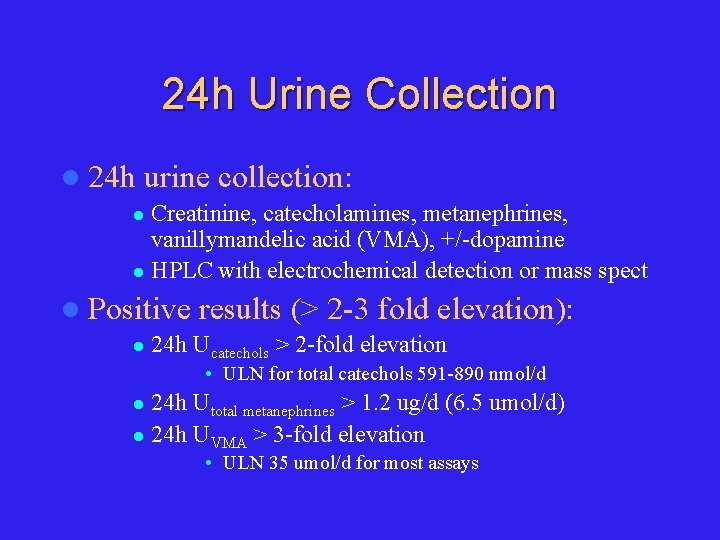
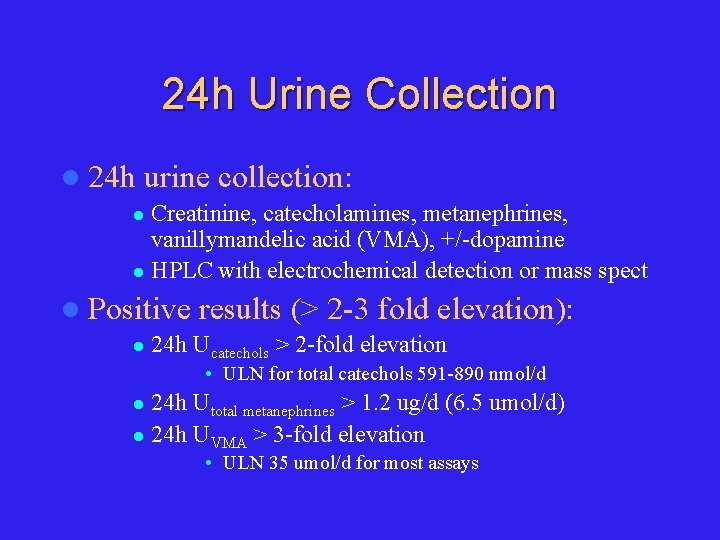
24 h Urine Collection l 24 h urine collection: Creatinine, catecholamines, metanephrines, vanillymandelic acid (VMA), +/-dopamine l HPLC with electrochemical detection or mass spect l l Positive l results (> 2 -3 fold elevation): 24 h Ucatechols > 2 -fold elevation • ULN for total catechols 591 -890 nmol/d 24 h Utotal metanephrines > 1. 2 ug/d (6. 5 umol/d) l 24 h UVMA > 3 -fold elevation l • ULN 35 umol/d for most assays
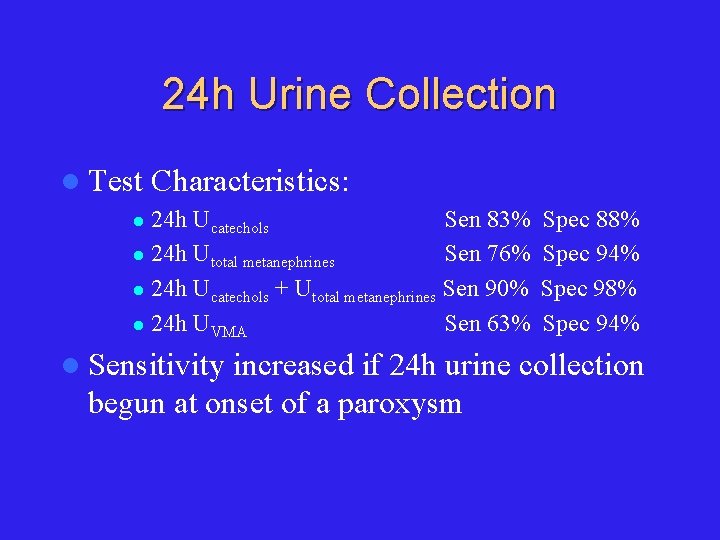
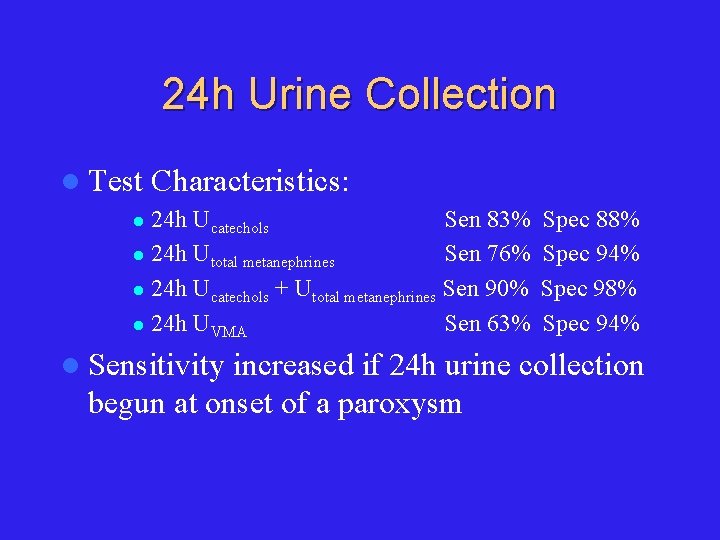
24 h Urine Collection l Test Characteristics: 24 h Ucatechols Sen 83% l 24 h Utotal metanephrines Sen 76% l 24 h Ucatechols + Utotal metanephrines Sen 90% l 24 h UVMA Sen 63% l l Sensitivity Spec 88% Spec 94% Spec 98% Spec 94% increased if 24 h urine collection begun at onset of a paroxysm

24 h Urine: False Positive Drugs: TCAs, MAO-i, levodopa, methyldopa, labetalol, propanolol, clonidine (withdrawal), ilicit drugs (opiods, amphetamines, cocaine), ethanol, sympathomimetics (cold remedies) l Hold these medications for 2 weeks! l Major physical stress (hypoglycemia, stroke, raised ICP, etc. ) l OSA l
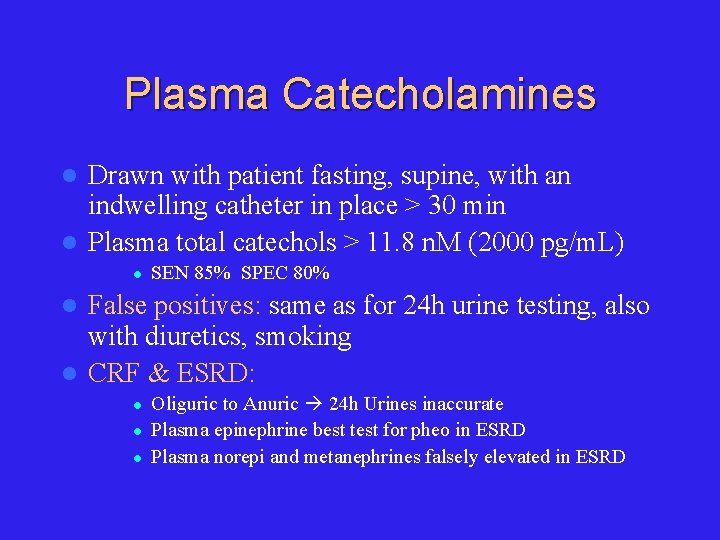
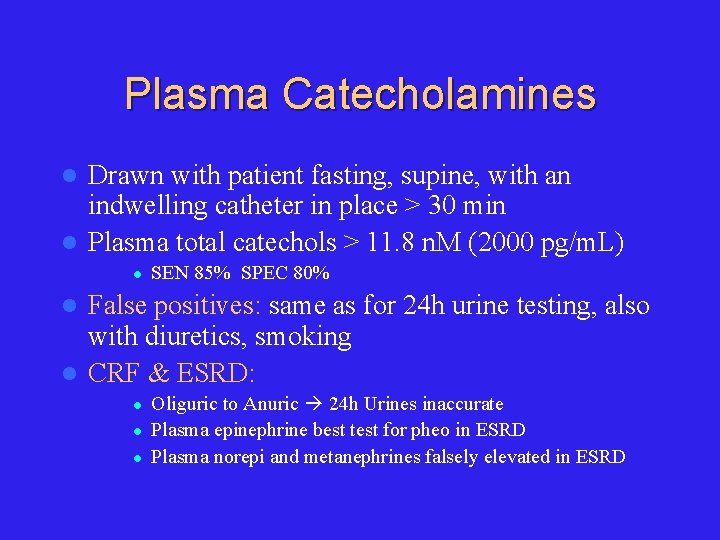
Plasma Catecholamines Drawn with patient fasting, supine, with an indwelling catheter in place > 30 min l Plasma total catechols > 11. 8 n. M (2000 pg/m. L) l l SEN 85% SPEC 80% False positives: same as for 24 h urine testing, also with diuretics, smoking l CRF & ESRD: l l Oliguric to Anuric 24 h Urines inaccurate Plasma epinephrine best test for pheo in ESRD Plasma norepi and metanephrines falsely elevated in ESRD
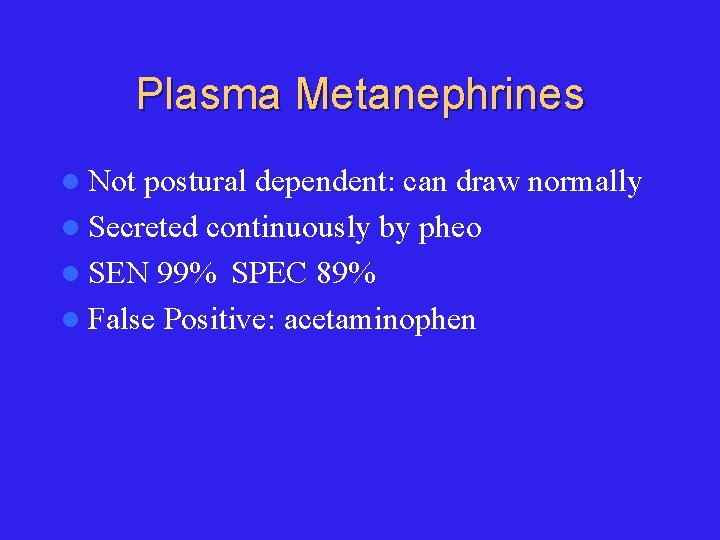
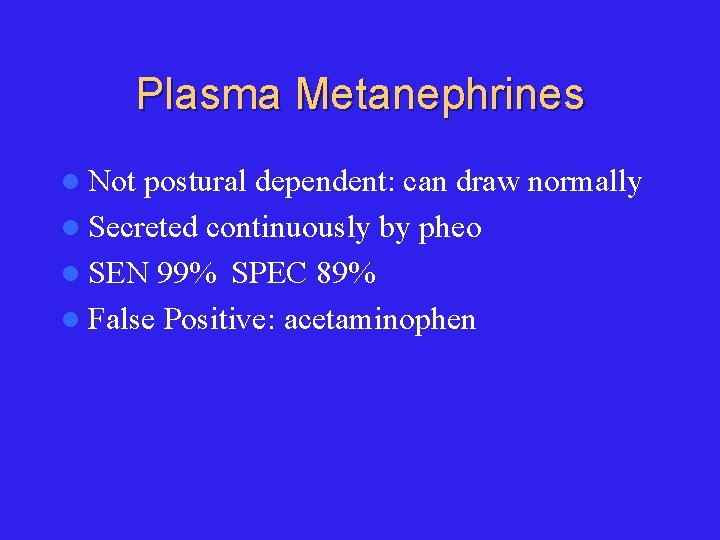
Plasma Metanephrines l Not postural dependent: can draw normally l Secreted continuously by pheo l SEN 99% SPEC 89% l False Positive: acetaminophen
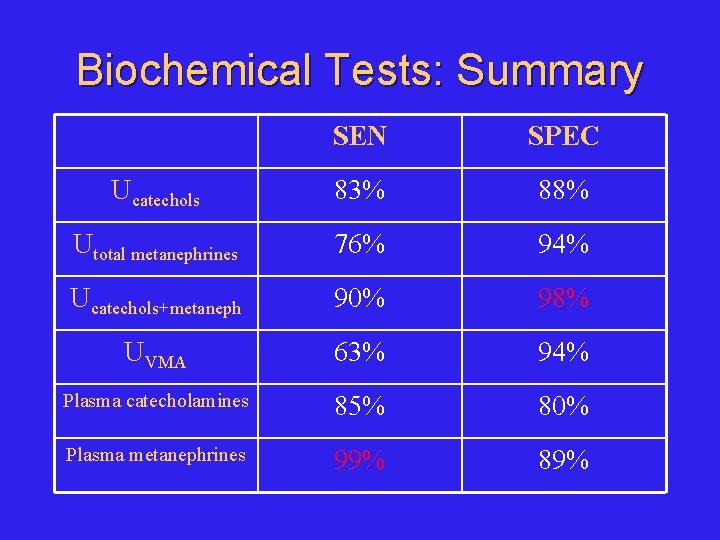
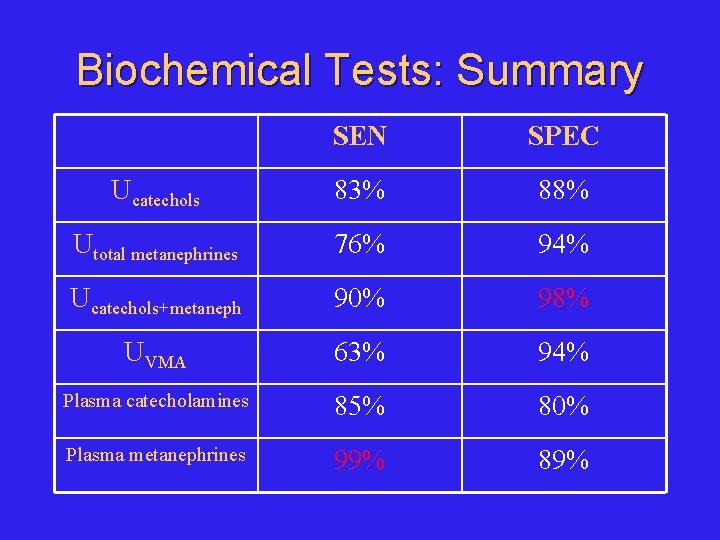
Biochemical Tests: Summary SEN SPEC Ucatechols 83% 88% Utotal metanephrines 76% 94% Ucatechols+metaneph 90% 98% UVMA 63% 94% Plasma catecholamines 85% 80% Plasma metanephrines 99% 89%
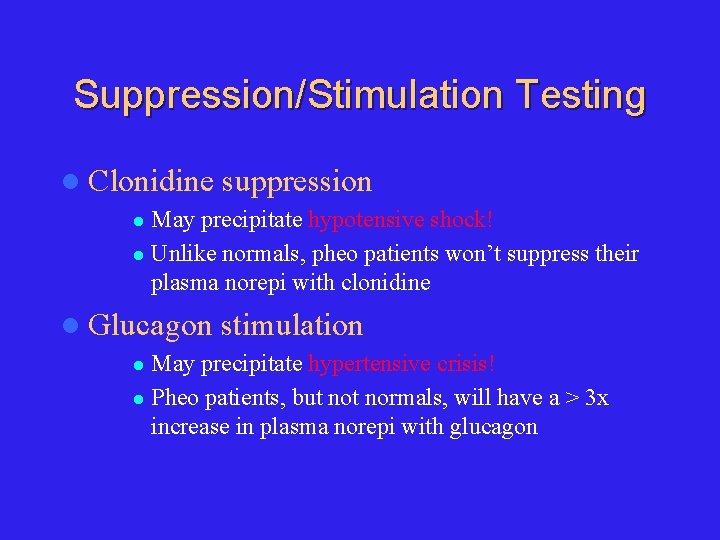
Suppression/Stimulation Testing l Clonidine suppression May precipitate hypotensive shock! l Unlike normals, pheo patients won’t suppress their plasma norepi with clonidine l l Glucagon stimulation May precipitate hypertensive crisis! l Pheo patients, but normals, will have a > 3 x increase in plasma norepi with glucagon l
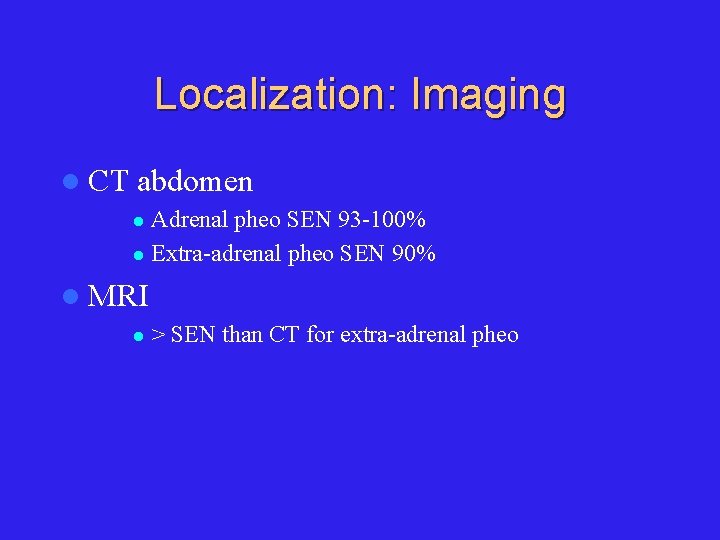
Localization: Imaging l CT abdomen Adrenal pheo SEN 93 -100% l Extra-adrenal pheo SEN 90% l l MRI l > SEN than CT for extra-adrenal pheo

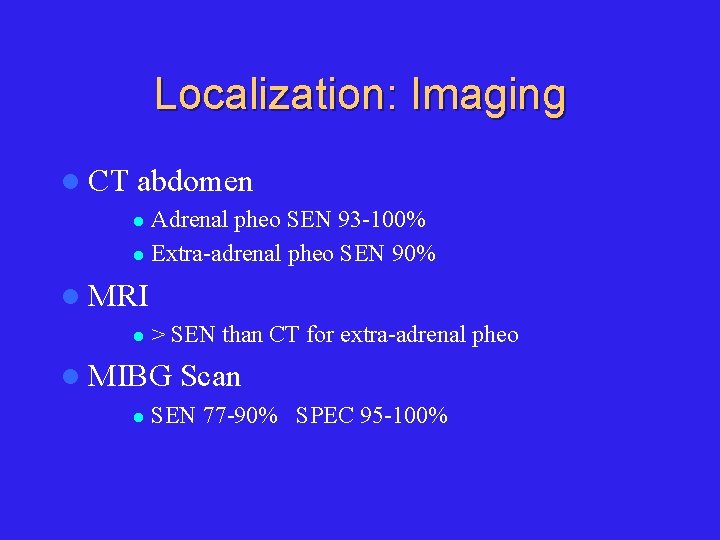
Localization: Imaging l CT abdomen Adrenal pheo SEN 93 -100% l Extra-adrenal pheo SEN 90% l l MRI l > SEN than CT for extra-adrenal pheo l MIBG l Scan SEN 77 -90% SPEC 95 -100%
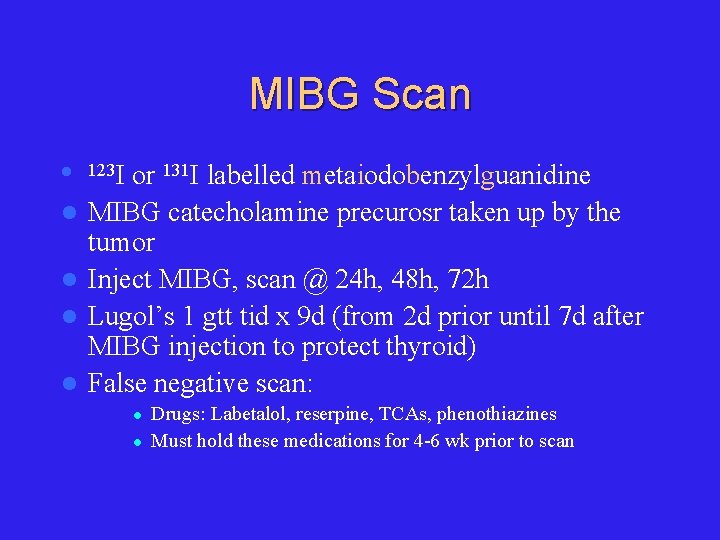
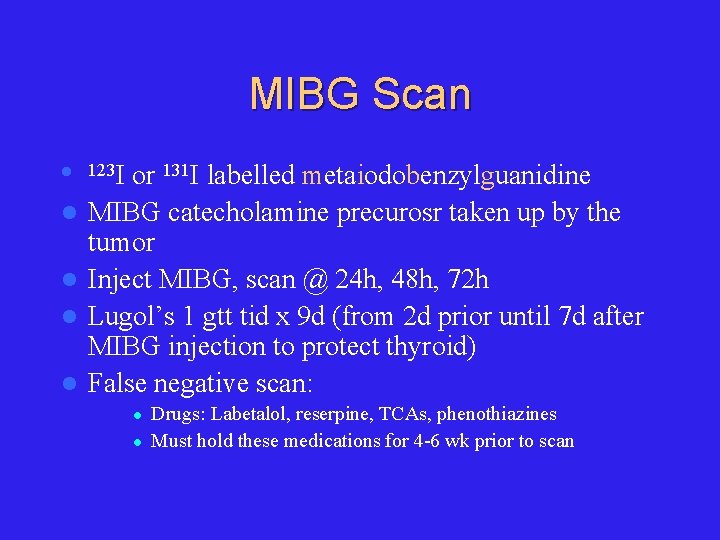
MIBG Scan l l l 123 I or 131 I labelled metaiodobenzylguanidine MIBG catecholamine precurosr taken up by the tumor Inject MIBG, scan @ 24 h, 48 h, 72 h Lugol’s 1 gtt tid x 9 d (from 2 d prior until 7 d after MIBG injection to protect thyroid) False negative scan: l l Drugs: Labetalol, reserpine, TCAs, phenothiazines Must hold these medications for 4 -6 wk prior to scan

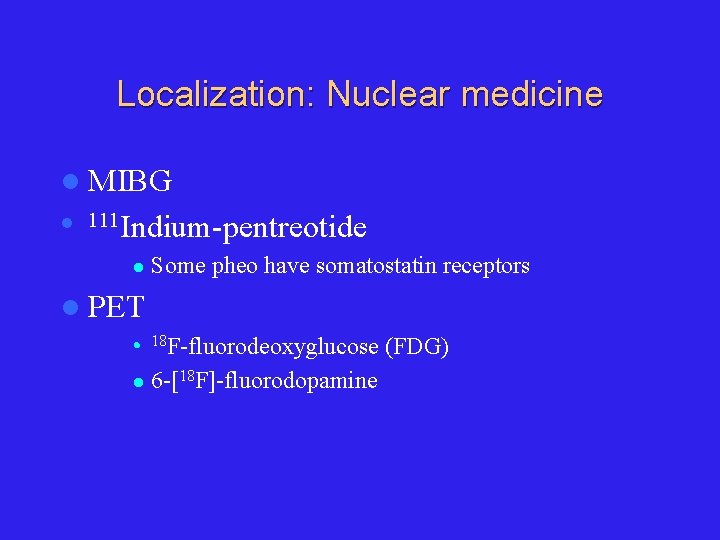
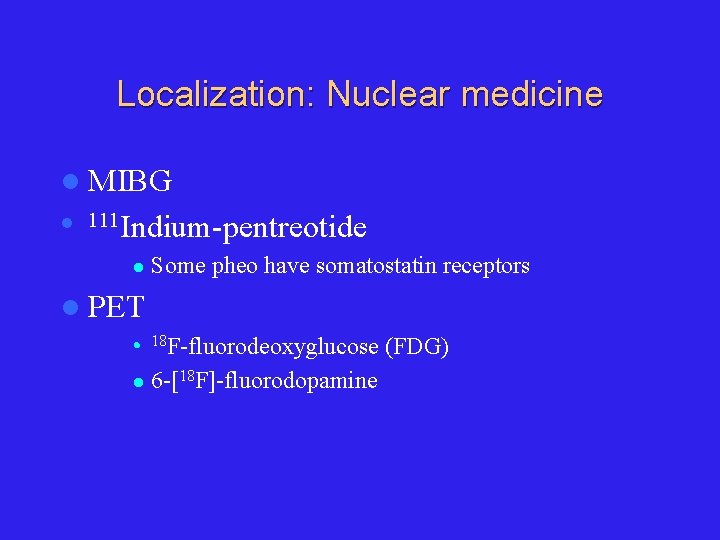
Localization: Nuclear medicine l MIBG l 111 Indium-pentreotide l Some pheo have somatostatin receptors l PET l 18 F-fluorodeoxyglucose l 6 -[18 F]-fluorodopamine (FDG)

Pheochromocytoma 1. 2. Catecholamine Physiology/Pathophysiology Clinical Presentation 1. 2. 3. Diagnosis 1. 2. 4. Epidemiology Signs & Symptoms Biochemical Localization Management 1. 2. 3. 4. Preoperative Operative Postoperative Pregnancy
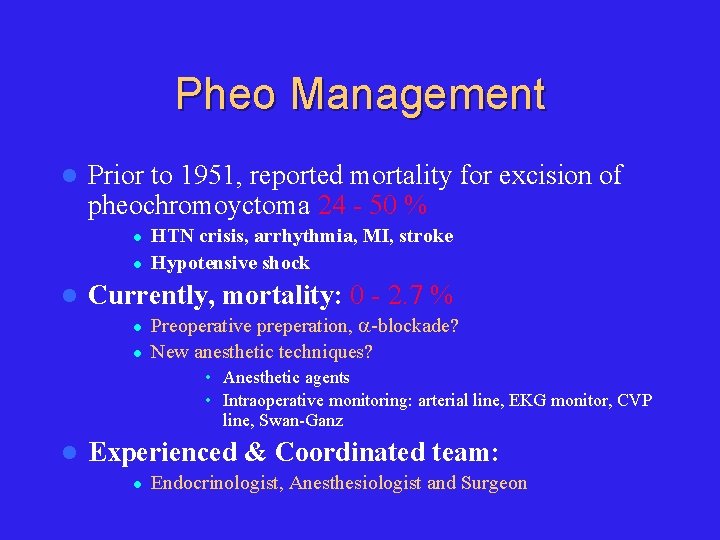
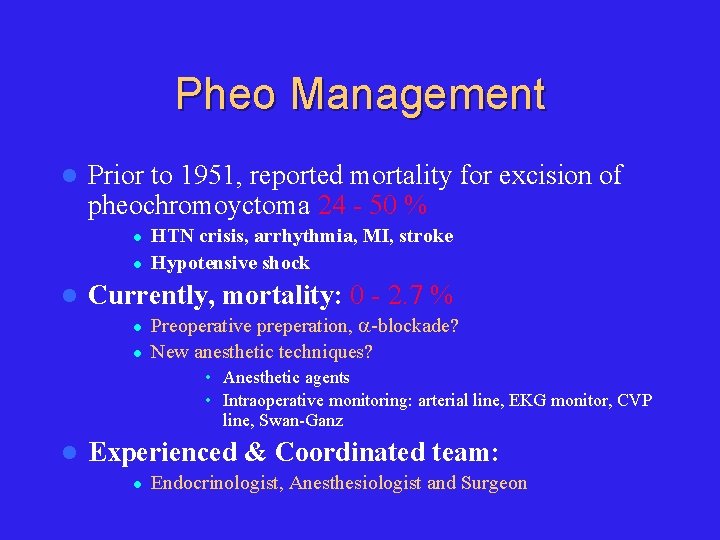
Pheo Management l Prior to 1951, reported mortality for excision of pheochromoyctoma 24 - 50 % l l l HTN crisis, arrhythmia, MI, stroke Hypotensive shock Currently, mortality: 0 - 2. 7 % l l Preoperative preperation, -blockade? New anesthetic techniques? • Anesthetic agents • Intraoperative monitoring: arterial line, EKG monitor, CVP line, Swan-Ganz l Experienced & Coordinated team: l Endocrinologist, Anesthesiologist and Surgeon
Preop W/up l CBC, lytes, creatinine, INR/PTT l CXR l EKG l Echo (r/o dilated CMY 2º catechols)
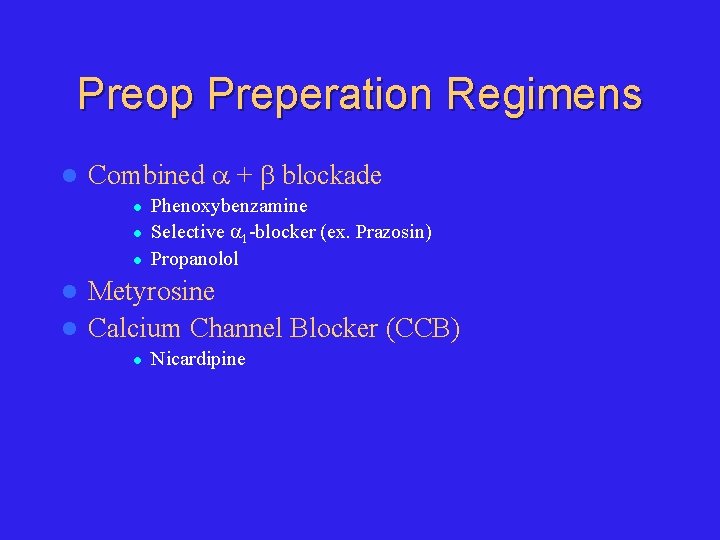
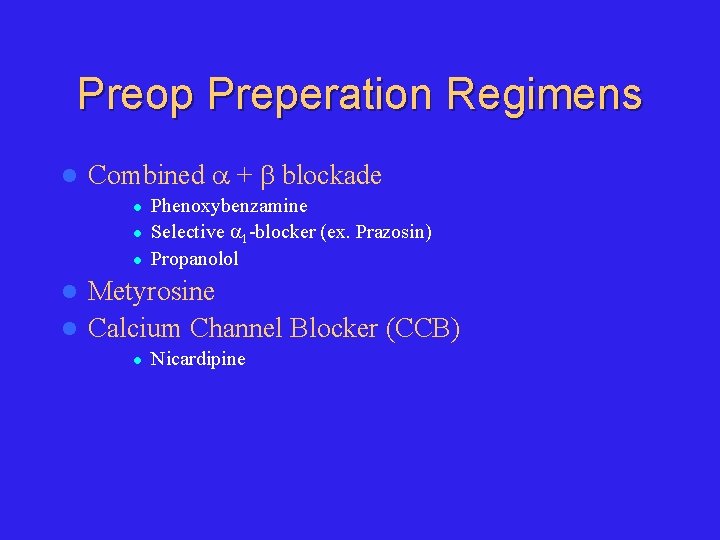
Preop Preperation Regimens l Combined + blockade l l l Phenoxybenzamine Selective 1 -blocker (ex. Prazosin) Propanolol Metyrosine l Calcium Channel Blocker (CCB) l l Nicardipine
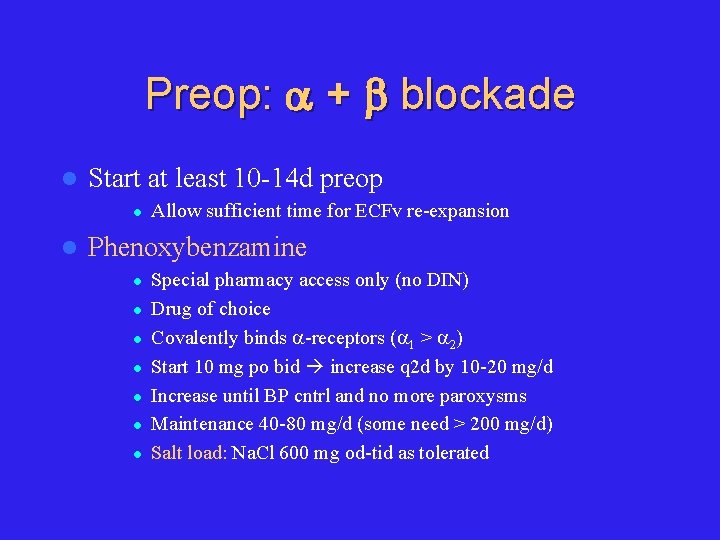
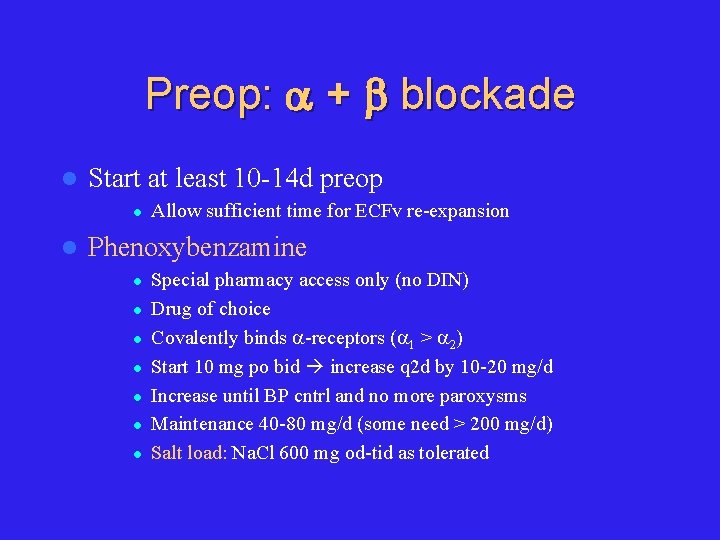
Preop: + blockade l Start at least 10 -14 d preop l l Allow sufficient time for ECFv re-expansion Phenoxybenzamine l l l l Special pharmacy access only (no DIN) Drug of choice Covalently binds -receptors ( 1 > 2) Start 10 mg po bid increase q 2 d by 10 -20 mg/d Increase until BP cntrl and no more paroxysms Maintenance 40 -80 mg/d (some need > 200 mg/d) Salt load: Na. Cl 600 mg od-tid as tolerated
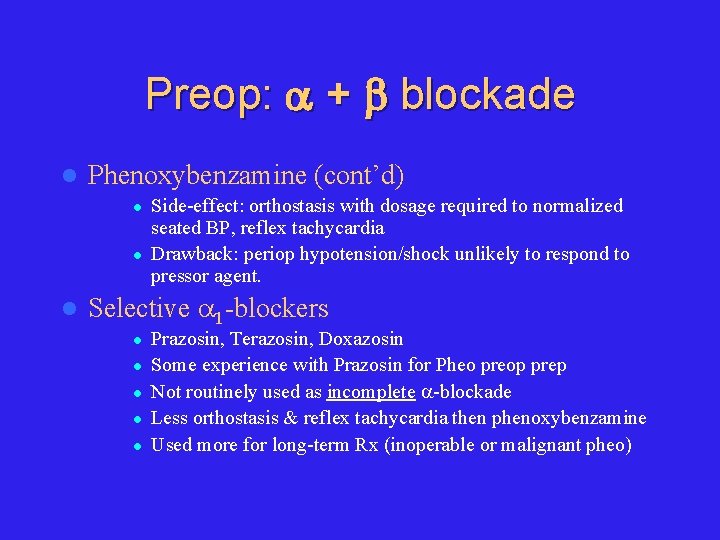
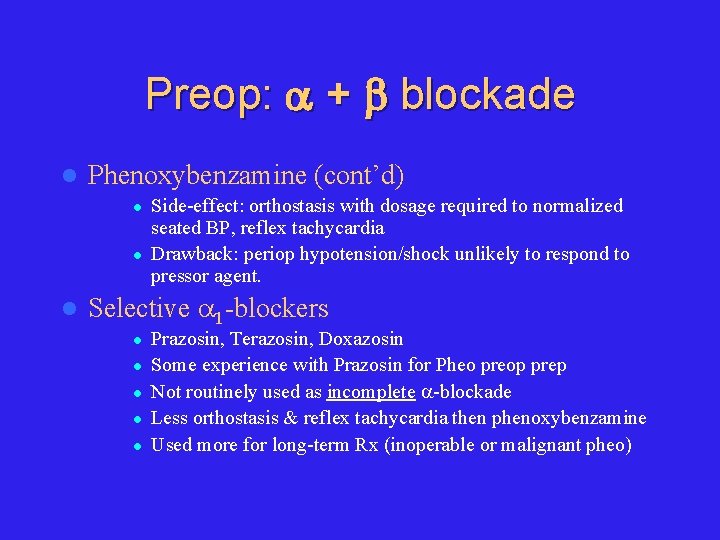
Preop: + blockade l Phenoxybenzamine (cont’d) l l l Side-effect: orthostasis with dosage required to normalized seated BP, reflex tachycardia Drawback: periop hypotension/shock unlikely to respond to pressor agent. Selective 1 -blockers l l l Prazosin, Terazosin, Doxazosin Some experience with Prazosin for Pheo preop prep Not routinely used as incomplete -blockade Less orthostasis & reflex tachycardia then phenoxybenzamine Used more for long-term Rx (inoperable or malignant pheo)
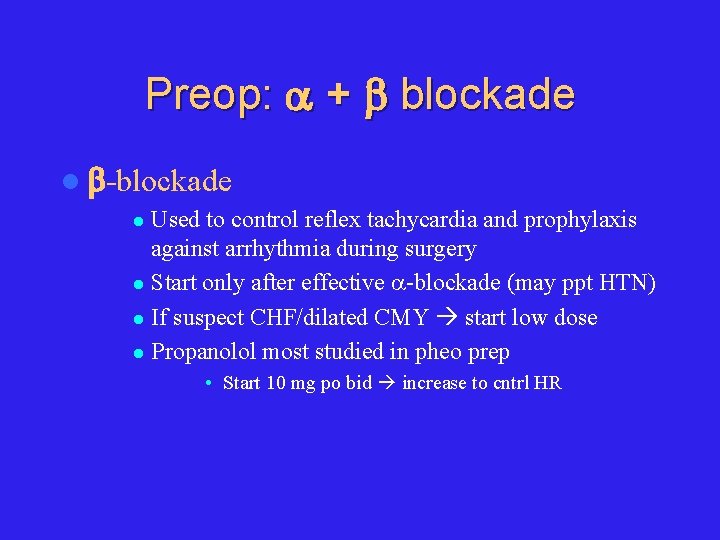
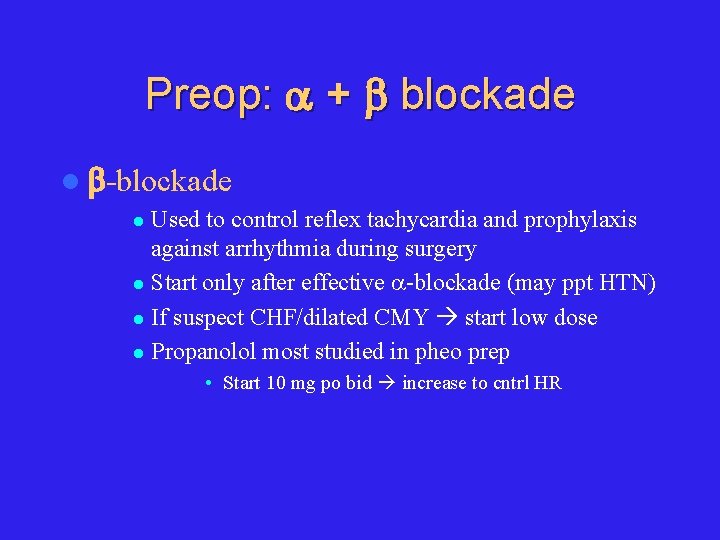
Preop: + blockade l -blockade Used to control reflex tachycardia and prophylaxis against arrhythmia during surgery l Start only after effective -blockade (may ppt HTN) l If suspect CHF/dilated CMY start low dose l Propanolol most studied in pheo prep l • Start 10 mg po bid increase to cntrl HR
Preop: + blockade l If BP still not cntrl despite + blockade Add Prazosin to Phenoxybenzamine l Add CCB, ACE-I l Avoid diuretics as already ECFv contracted l Metyrosine l
Preop: + blockade Meds given on AM of surgery l Periop HTN: l l IV phentolamine – Short acting non-selective -blocker – Test dose 1 mg, then 2 -5 mg IV q 1 -2 h PRN or as continuous infusion (100 mg in 500 cc D 5 W, titrate to BP) l IV Nitroprusside (NTP) Periop arrhythmia: IV esmolol l Periop Hypothension: IV crystalloid +/- colloid l
Pheo: Rx of HTN Crisis l IV phentolamine l IV NTP l IV esmolol l IV labetalol – combined + blocker
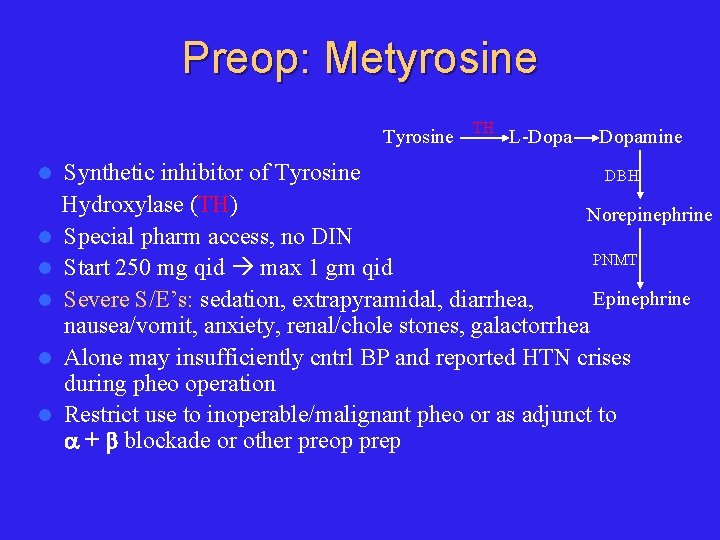
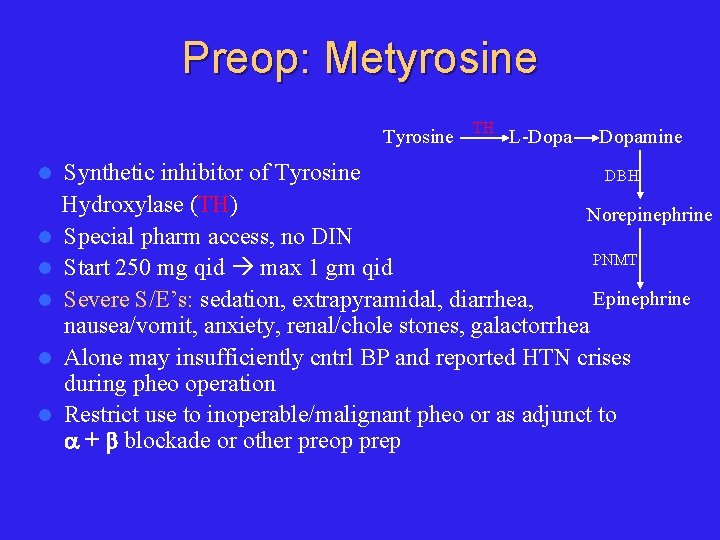
Preop: Metyrosine Tyrosine l l l TH L-Dopamine Synthetic inhibitor of Tyrosine DBH Hydroxylase (TH) Norepinephrine Special pharm access, no DIN PNMT Start 250 mg qid max 1 gm qid Epinephrine Severe S/E’s: sedation, extrapyramidal, diarrhea, nausea/vomit, anxiety, renal/chole stones, galactorrhea Alone may insufficiently cntrl BP and reported HTN crises during pheo operation Restrict use to inoperable/malignant pheo or as adjunct to + blockade or other preop prep
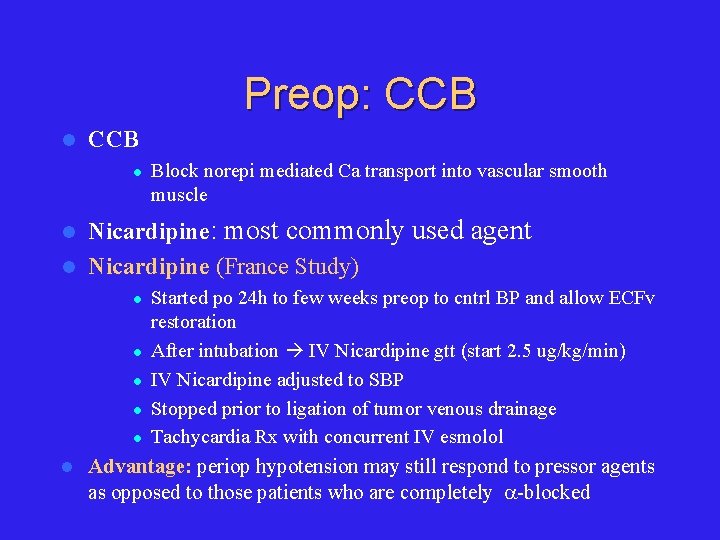
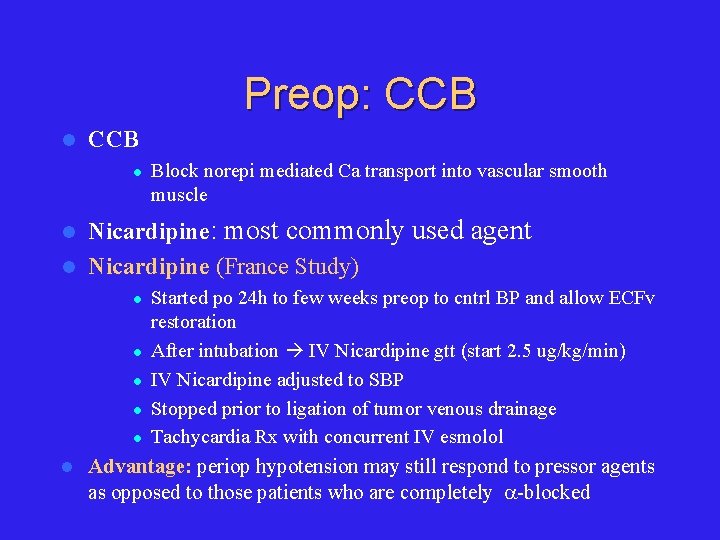
Preop: CCB l Block norepi mediated Ca transport into vascular smooth muscle Nicardipine: most commonly used agent l Nicardipine (France Study) l l l l Started po 24 h to few weeks preop to cntrl BP and allow ECFv restoration After intubation IV Nicardipine gtt (start 2. 5 ug/kg/min) IV Nicardipine adjusted to SBP Stopped prior to ligation of tumor venous drainage Tachycardia Rx with concurrent IV esmolol Advantage: periop hypotension may still respond to pressor agents as opposed to those patients who are completely -blocked
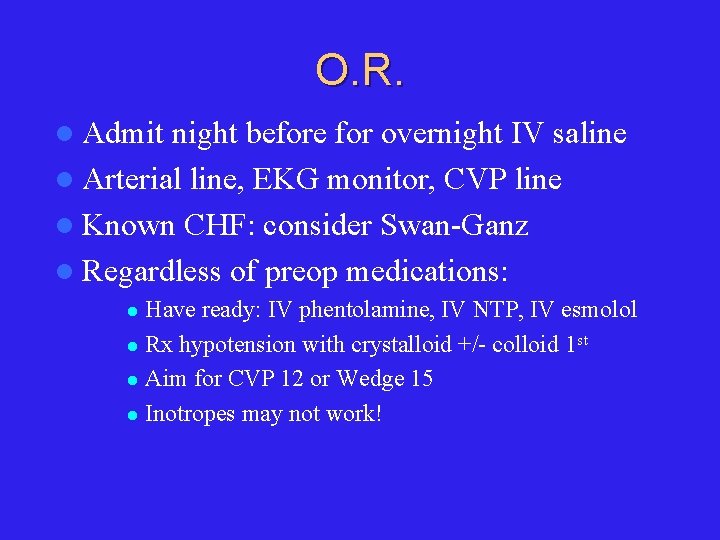
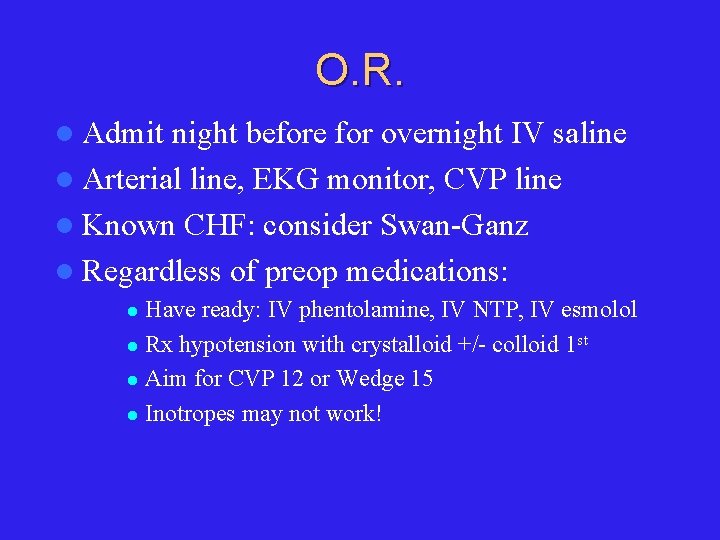
O. R. l Admit night before for overnight IV saline l Arterial line, EKG monitor, CVP line l Known CHF: consider Swan-Ganz l Regardless of preop medications: Have ready: IV phentolamine, IV NTP, IV esmolol l Rx hypotension with crystalloid +/- colloid 1 st l Aim for CVP 12 or Wedge 15 l Inotropes may not work! l
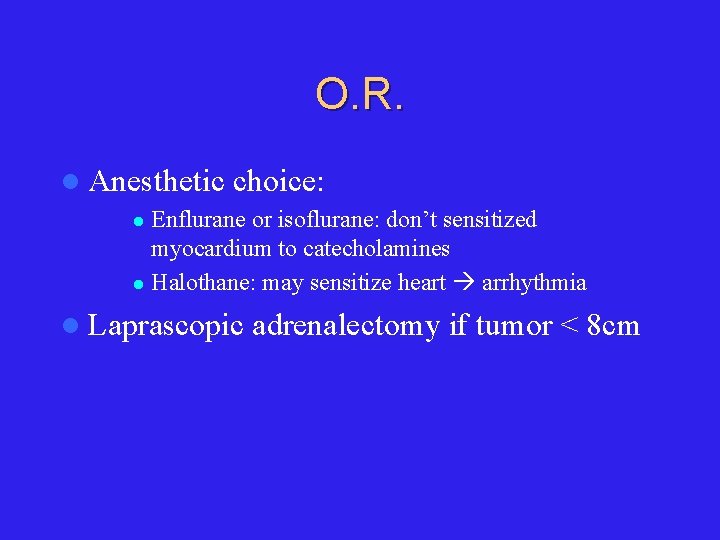
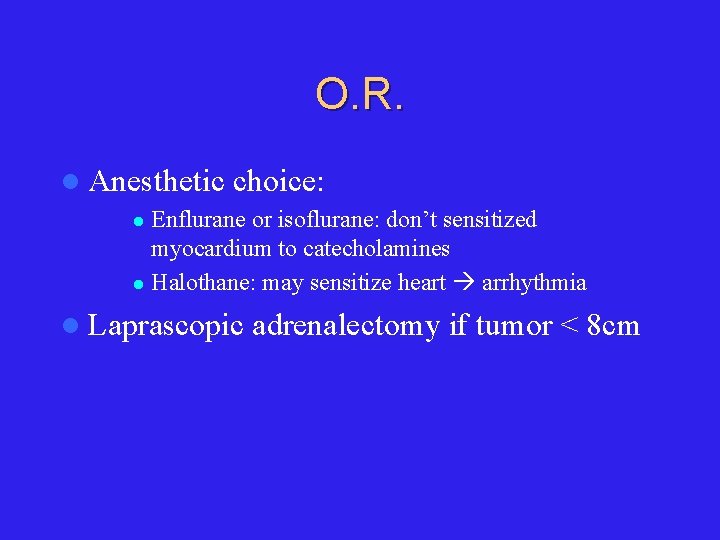
O. R. l Anesthetic choice: Enflurane or isoflurane: don’t sensitized myocardium to catecholamines l Halothane: may sensitize heart arrhythmia l l Laprascopic adrenalectomy if tumor < 8 cm
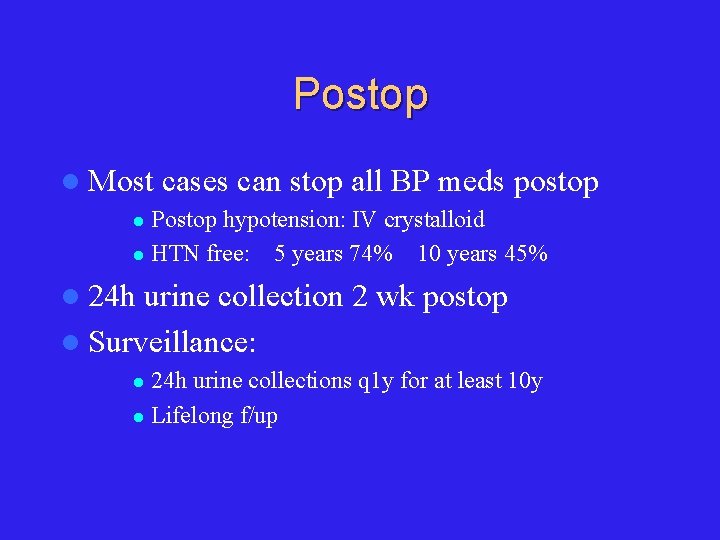
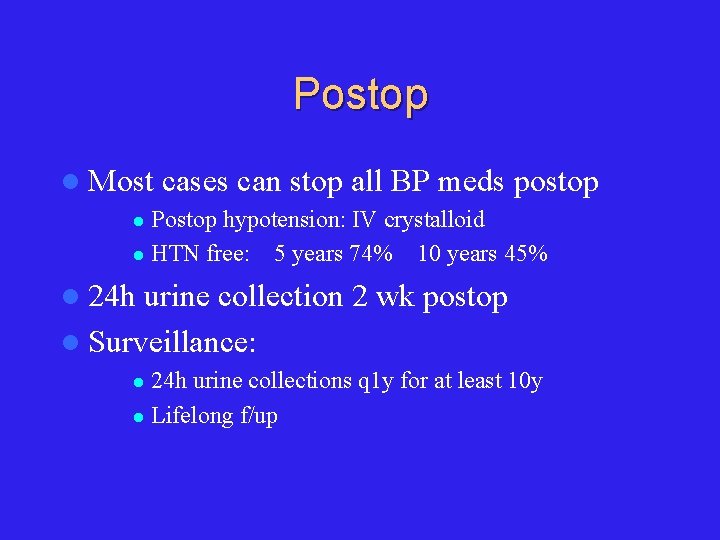
Postop l Most cases can stop all BP meds postop Postop hypotension: IV crystalloid l HTN free: 5 years 74% 10 years 45% l l 24 h urine collection 2 wk postop l Surveillance: 24 h urine collections q 1 y for at least 10 y l Lifelong f/up l
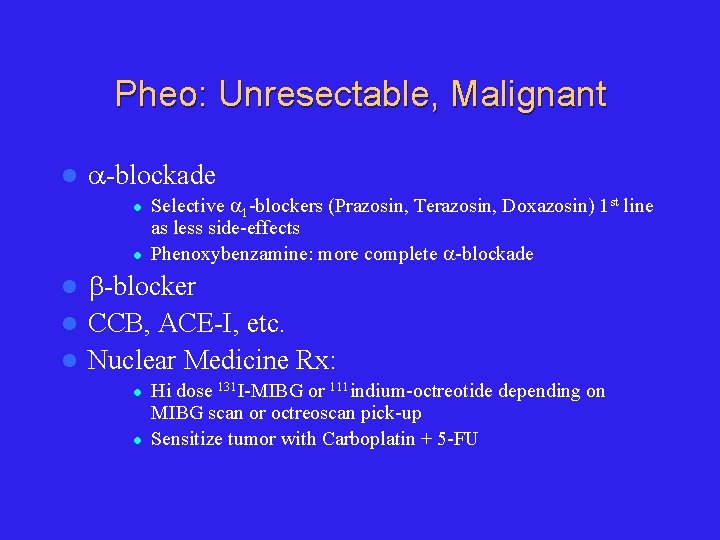
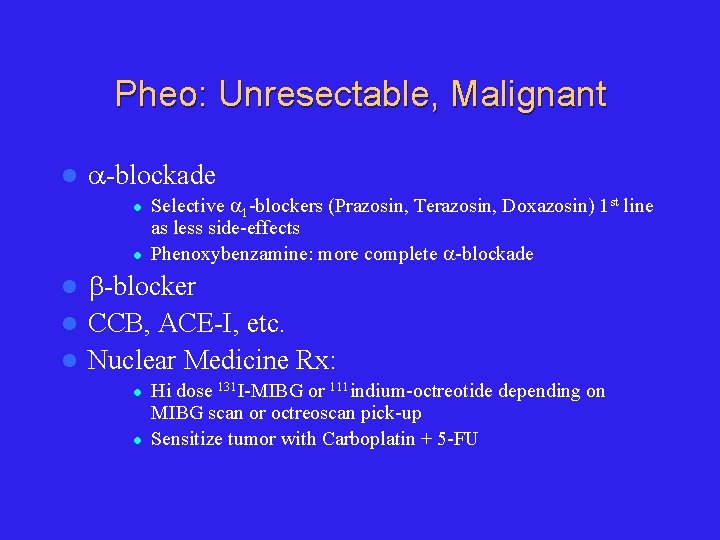
Pheo: Unresectable, Malignant l -blockade l l Selective 1 -blockers (Prazosin, Terazosin, Doxazosin) 1 st line as less side-effects Phenoxybenzamine: more complete -blockade -blocker l CCB, ACE-I, etc. l Nuclear Medicine Rx: l l l Hi dose 131 I-MIBG or 111 indium-octreotide depending on MIBG scan or octreoscan pick-up Sensitize tumor with Carboplatin + 5 -FU
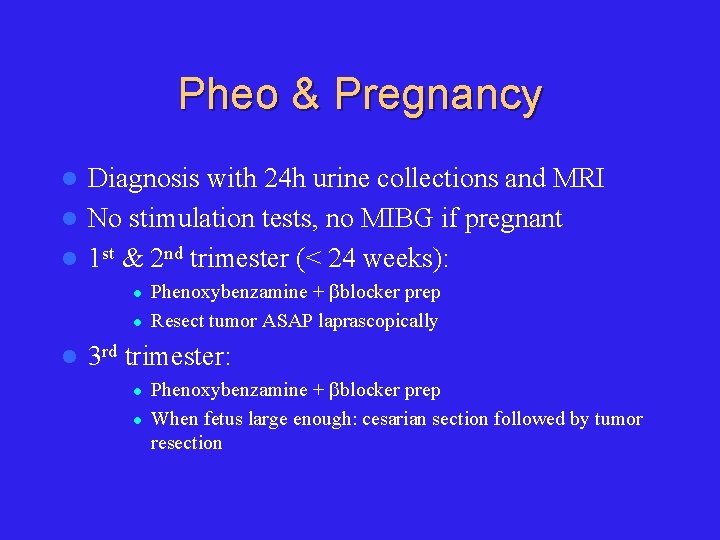
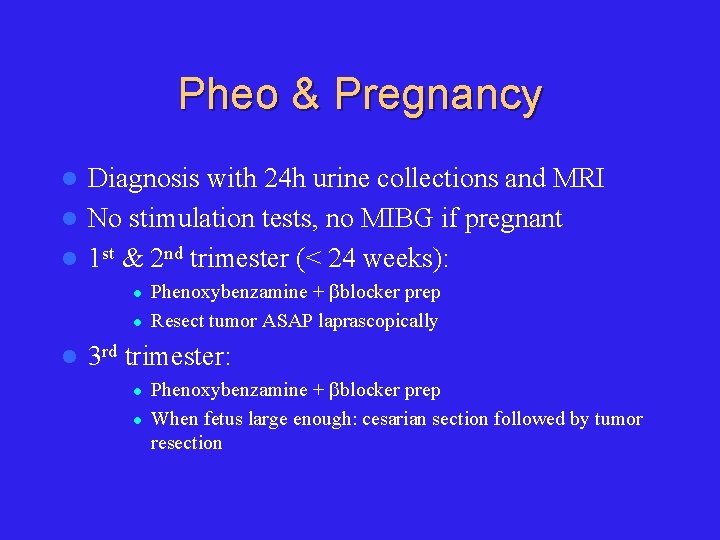
Pheo & Pregnancy Diagnosis with 24 h urine collections and MRI l No stimulation tests, no MIBG if pregnant l 1 st & 2 nd trimester (< 24 weeks): l l Phenoxybenzamine + blocker prep Resect tumor ASAP laprascopically 3 rd trimester: l l Phenoxybenzamine + blocker prep When fetus large enough: cesarian section followed by tumor resection