Pharmacy Practice communication skills and influences on medicine












- Slides: 23

Pharmacy Practice – communication skills and influences on medicine taking Jane Portlock Professor of Pharmacy Education and CPPE tutor for Portsmouth
Learning outcomes for this lecture • - Distinguish the important features of effective communication from a theoretical perspective • - Have an appreciation of the need to develop effective communication skills in practice • - Distinguish the concepts of compliance, adherence and concordance • Therefore we are going to explore the basics of: – Communication skills for patient consultation – Influences on medicine taking • All of these will be explored in more detail and have workshops associated with them in Course E with me next academic year. 29/11/2020 2

An introduction to communication • In pairs answer the following questions: - – When will you communicate in pharmacy practice? – What are the barriers to good communication? – How can you overcome these barriers? 29/11/2020 3

Communication skills for pharmacists 29/11/2020 4

Put these statements in order of priority • • Putting the patient at the centre of healthcare Improved medicines adherence Job satisfaction and less work-related stress Being at your best in every patient consultation Fewer wasted medicines Patients understanding their medicines better Patient-centred approach to care Taking care of the patient like you would take care of your grandmother 29/11/2020 5
Patient – centred consultation • What do we mean by patient- centred consultation? • Which behaviours would a pharmacist demonstrate in a patient – centred consultation? • Which skills does a pharmacist need to be able to communicate with a patient? 29/11/2020 6
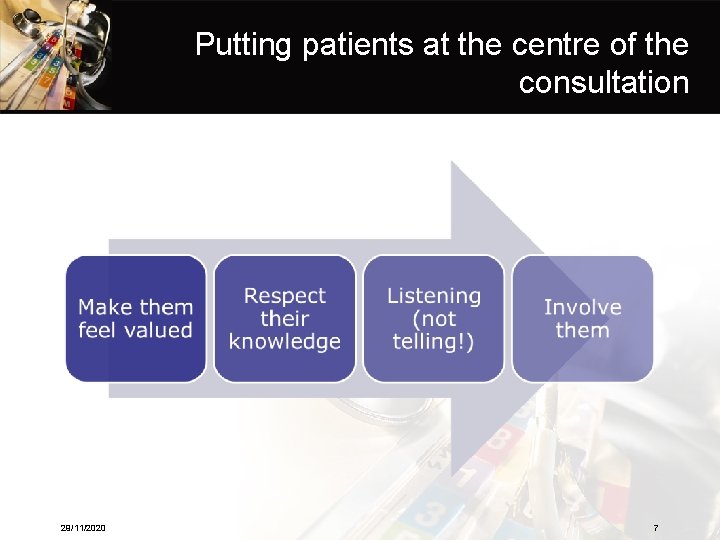
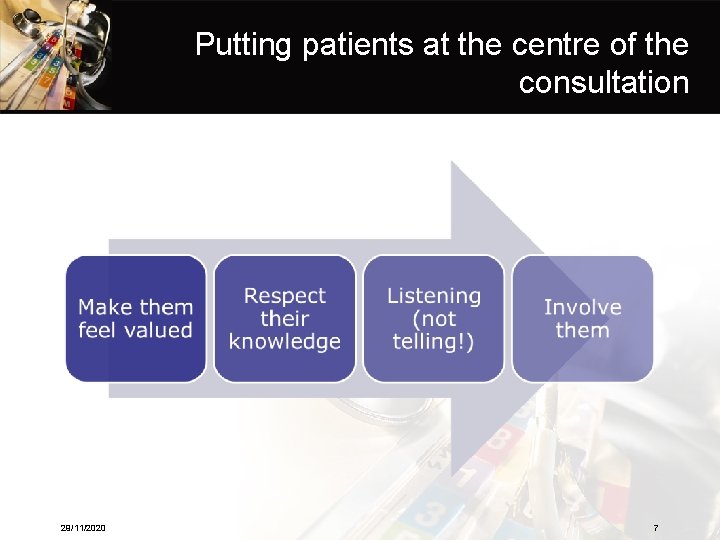
Putting patients at the centre of the consultation 29/11/2020 7
The beginning of the consultation • • Greet the patient (‘hello’) Introduce yourself Make sure you know the patient’s name Build rapport with appropriate body language and good eye contact • Smile but show empathy at appropriate times 29/11/2020 8
Asking questions • Let the patient tell their story • Open questions such as………………. • TED – ‘tell’, ‘explain’, ‘describe’ • Questions with options and leading questions • Beware! • Probing questions • ‘Can you describe that to me? ’ • Closed questions – ’yes’ or ‘no’ answers 29/11/2020 9

Listening • Reflecting back and responding to what a patient has told you will make them feel heard and understood. 29/11/2020 10

Explaining • Use an approach and language which is appropriate for each patient • Give a level of information relevant to the needs of the patient • Use pauses and check understanding • Make suggestions rather than directives • Repeat important points, write things down • Involve the patient in decisions and planning • Don’t be afraid of the patient’s questions ! 29/11/2020 11

Closing • Summarise • What are three most important things you want the patient to remember? • Allow the patient to tell you what they plan to do once they have left the consultation • Safety net – what if things don’t go to plan? • Use visual clues indicating the end of the discussion 29/11/2020 12
Overcoming the barriers • Common potential barriers in addition to those we identified at the beginning of the lecture: • Environment • Language, culture • Disability – sight, hearing, memory, learning disability, mental illness • How can the above be overcome? 29/11/2020 13

What does a medicines-related consultation look like? 29/11/2020 14
Let’s look at the Medication Related Consultation Framework • • • A – Introduction B – Data collection and problem identification C – Actions and solutions D – Closing the consultation E – Consultation behaviours • Developed by Professor Rob Horne and colleagues at the School of Pharmacy, University of Brighton. Professor Horne is now at UCL School of Pharmacy. 29/11/2020 15
Compliance, Concordance and Adherence • Terms which are commonly used in the pharmacy world • Compliance means………… • Concordance means…………………. • Adherence means…………. . • And are sometimes confused. 29/11/2020 16

Non- adherence • Unintentional non-adherence – Patient wants to follow the agreed treatment but is prevented from doing so by barriers beyond their control such as • Poor recall/forgetting to take the medicine • Difficulties in understanding the instructions • Problems using the treatment • Inability to pay for the treatment • Intentional non-adherence – Patient decides not to follow the treatment recommendations 29/11/2020 17
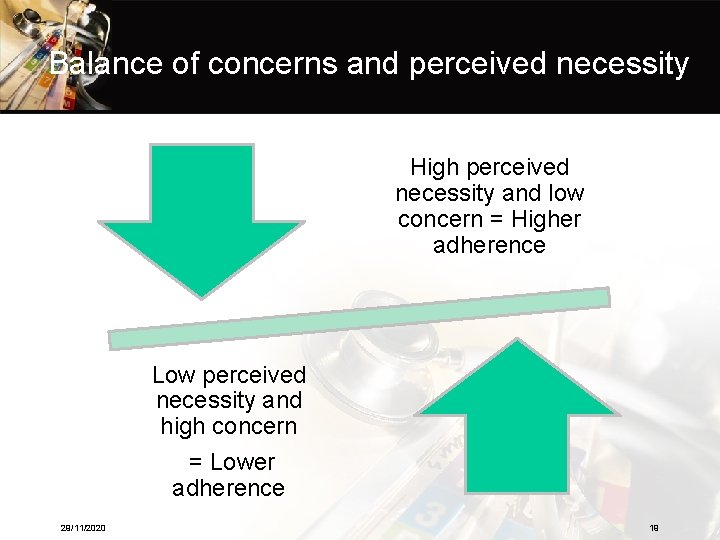
Intentional non-adherence • What causes intentional non-adherence? • Patients’ beliefs about medicines Perceived necessity of taking medicine versus Concerns about the consequences of taking the medicine 29/11/2020 18
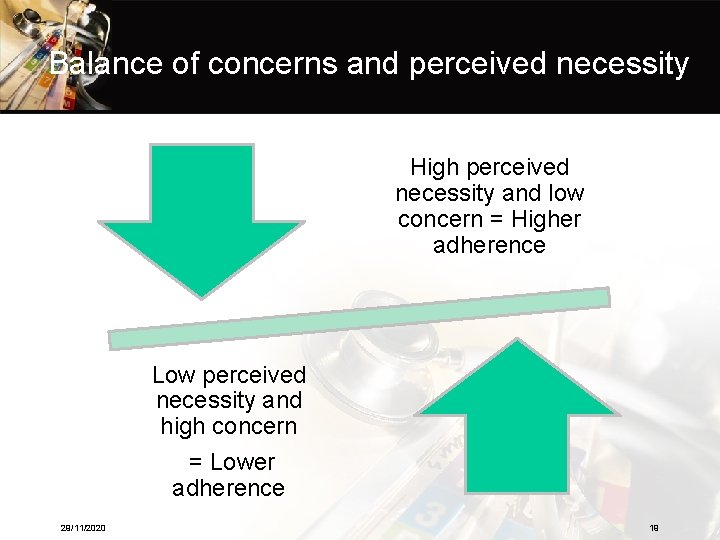
Balance of concerns and perceived necessity High perceived necessity and low concern = Higher adherence Low perceived necessity and high concern = Lower adherence 29/11/2020 19

NICE National Institute for Health and Clinical Excellence • Medicines Adherence • Clinical Guideline 76 – Involving patients in decisions about prescribed medicines and supporting adherence • Key principles – Adapt consultation style to the needs of the patient – Establish the most effective way of communicating with each patient – Offer all patients the opportunity to be involved in making decisions about prescribed medicines 29/11/2020 20

NICE Medicines Adherence • Key principles – Be aware that increasing patient involvement may mean that the patient decides not the take the medicine – Be aware of the patients’ concerns and whether they believe they need them affect how and whether they will take their prescribed medicines – Offer patients information that is relevant to their condition, possible treatments and personal circumstances, and that is easy to understand free from jargon – Recognise that non-adherence is common and that most patients are non-adherent sometimes – Routinely assess adherence in a non-judgemental way whenever you dispense, review or prescribe medicines 29/11/2020 21
Professional activities • • • Medicines Use Review New Medicines Service Clinical Medication Review Medicines Optimisation Health promotion – stop smoking, EHC, alcohol, weight management, healthy eating • Healthy Living Pharmacies • More on all of these in Courses E and G 29/11/2020 22

Medicines Optimisation • Some areas of current focus: • Laxatives - review and, where appropriate, revise prescribing of laxatives for adults to ensure that they are only prescribed routinely for the short-term treatment of constipation, where dietary and lifestyle measures have proven unsuccessful or where there is an immediate clinical need. • ACE inhibitors - review and, where appropriate, revise prescribing to ensure it is in line with NICE guidance. • Antidepressants - review and, where appropriate, revise prescribing of antidepressants in adults to ensure that it is in line with NICE guidance. • Other medicines – include antibiotics, hypnotics, antidiabetic agents, corticosteroids in asthma – 15 current areas in total 29/11/2020 23
 Consultation skills for pharmacy practice
Consultation skills for pharmacy practice Consultation skills for pharmacy practice
Consultation skills for pharmacy practice Universitatea de medicina si farmacie victor babes
Universitatea de medicina si farmacie victor babes Victor babeş university of medicine and pharmacy
Victor babeş university of medicine and pharmacy Victor babes university of medicine
Victor babes university of medicine Pharmacotritae
Pharmacotritae Les facteurs qui influencent la communication
Les facteurs qui influencent la communication Dilution pharmacy calculations
Dilution pharmacy calculations Interpersonal and intrapersonal skills examples
Interpersonal and intrapersonal skills examples Hard skill vs soft skill
Hard skill vs soft skill Pharmacy practice
Pharmacy practice Pharmacy clinical pearls
Pharmacy clinical pearls Sop gpp
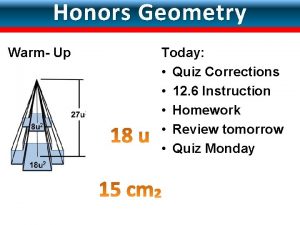
Sop gpp Unit 6 lesson 6 surface areas and volumes of spheres
Unit 6 lesson 6 surface areas and volumes of spheres Secure assess evolve
Secure assess evolve What proof uses figures
What proof uses figures Practice 5-3 concurrent lines medians and altitudes answers
Practice 5-3 concurrent lines medians and altitudes answers Helping students practice skills, strategies, and processes
Helping students practice skills, strategies, and processes Triangles and coordinate proof
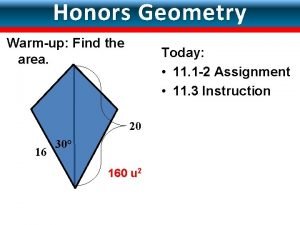
Triangles and coordinate proof 11-3 volume of pyramids and cones
11-3 volume of pyramids and cones Segments and distance
Segments and distance Lesson 3: surface areas of pyramids and cones
Lesson 3: surface areas of pyramids and cones 11-3 area of circles and sectors
11-3 area of circles and sectors Constant rate of change example
Constant rate of change example