Pharmacists role in a family medicine clinic a








- Slides: 24
Pharmacists’ role in a family medicine clinic: a focus on patients with diabetes Benjamin Chavez, Pharm. D, BCPP, BCACP Associate Professor Pacific University Oregon School of Pharmacy Previously: Clinical Associate Professor University of Hawaii John A Burns School of Medicine Department of Family Medicine and Community Health
Disclosures • No conflicts of interest to disclose
Objective • To describe the role of clinical pharmacist embedded in a family medicine clinic serving an underserved population
Practice Site – Physician Center at Mililani • Outpatient primary care, family-medicine, clinic • Main outpatient clinic for residency program for Department of Family Medicine and Community Health at University of Hawaii • 18 residents (6 each year) • 7 attending physicians • 6 -8 medical assistants • Front desk staff • 10 patient rooms

Patient Population • Serves mostly under-served lower socio-economic patient population – Mostly on Hawaii’s Medicaid or uninsured • “Rural” area • Large Pacific Islander patient population – – – Marshal Islands Federated States of Micronesia (Yap, Chuuk, Pohnpei, Kosrae) Guam Samoa Palau • Asian descent • As well as Hawaii locals
LET’S TALK GEOGRAPHY. . .




BACK TO OUR SERVICE
Pharmacy Services • Started in July 2010 • From electronic patient records, high-risk patients would be identified for intervention – Started with Hg. A 1 C > 10% – Telephone calls asking people to come in for appt with pharmacist – Success was moderate • Eventually, physicians and residents started referring more and more patients with different disease states • Specific protocols written for diabetes, hypertension, and hyperlipidemia • Other disease states seen as well • Pharmacy students were integrated in October 2010

Office Visits • Patient appointments were scheduled for 30 minutes • We did not bill for these services • Seen as an added benefit for our patients • ~2 -3 days per week of scheduled appointments – Also there to precept/support residents and students • ~1 -2 days per week of serving as preceptor for residents
Other Responsibilities • Communication with retail pharmacies • Phone calls from patients re: medication questions • Insurance companies prior authorizations • Provider education – Journal club – Topic discussions • Curbside consults
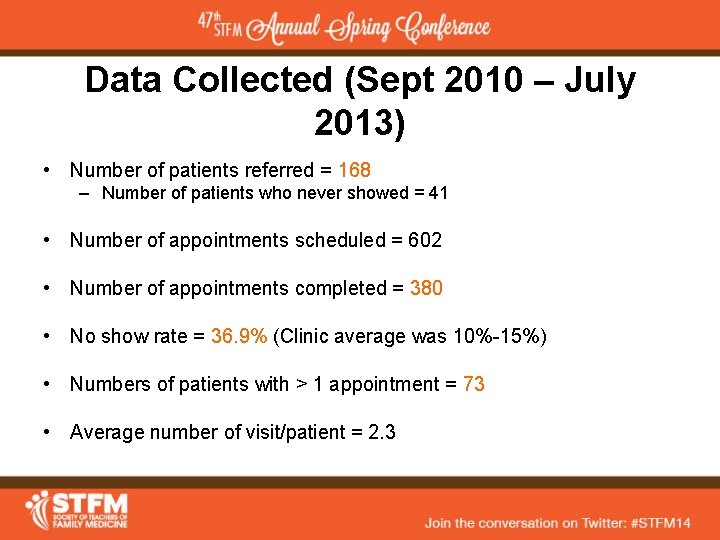
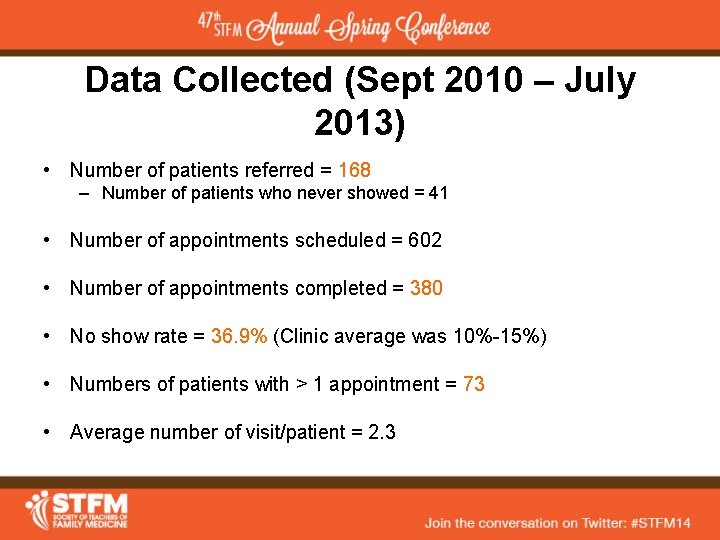
Data Collected (Sept 2010 – July 2013) • Number of patients referred = 168 – Number of patients who never showed = 41 • Number of appointments scheduled = 602 • Number of appointments completed = 380 • No show rate = 36. 9% (Clinic average was 10%-15%) • Numbers of patients with > 1 appointment = 73 • Average number of visit/patient = 2. 3
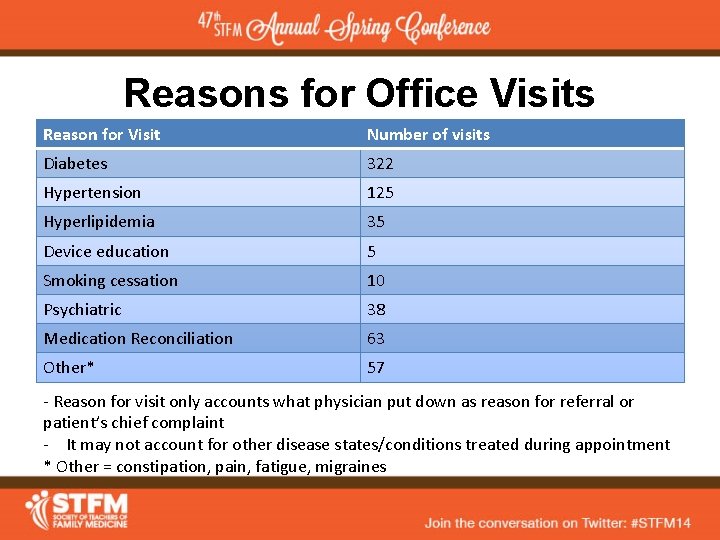
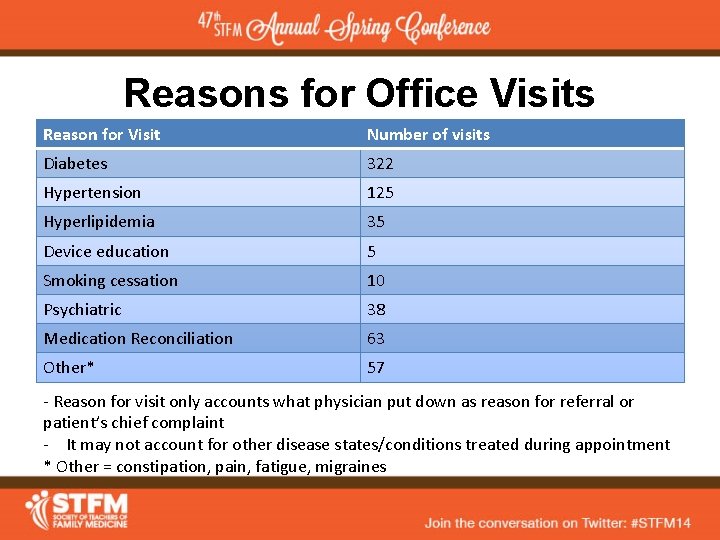
Reasons for Office Visits Reason for Visit Number of visits Diabetes 322 Hypertension 125 Hyperlipidemia 35 Device education 5 Smoking cessation 10 Psychiatric 38 Medication Reconciliation 63 Other* 57 - Reason for visit only accounts what physician put down as reason for referral or patient’s chief complaint - It may not account for other disease states/conditions treated during appointment * Other = constipation, pain, fatigue, migraines
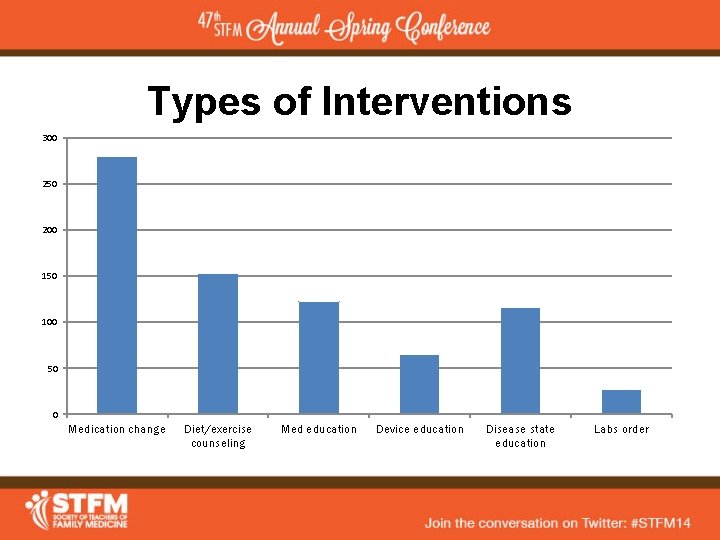
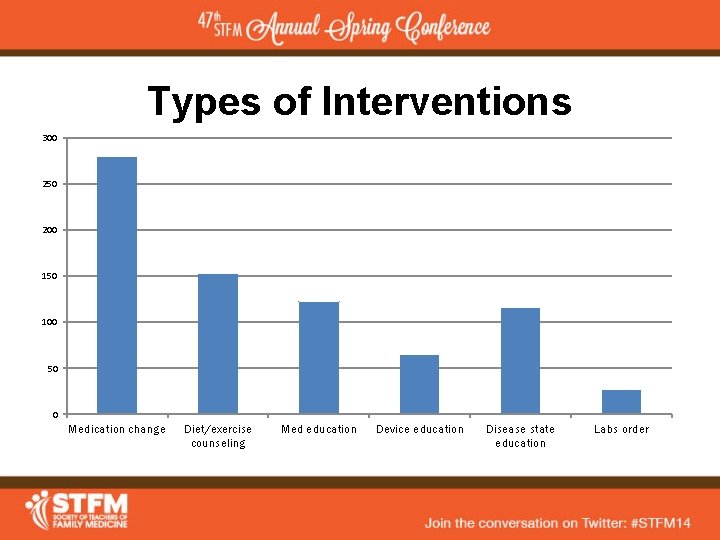
Types of Interventions 300 250 200 150 100 50 0 Medication change Diet/exercise counseling Med education Device education Disease state education Labs order
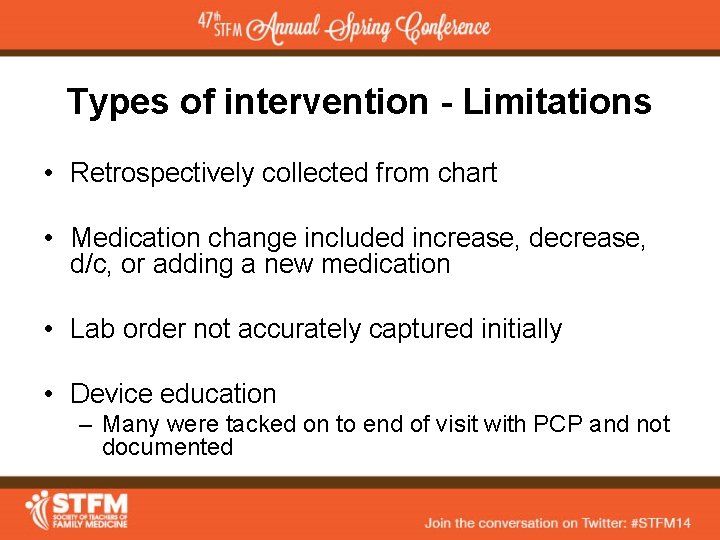
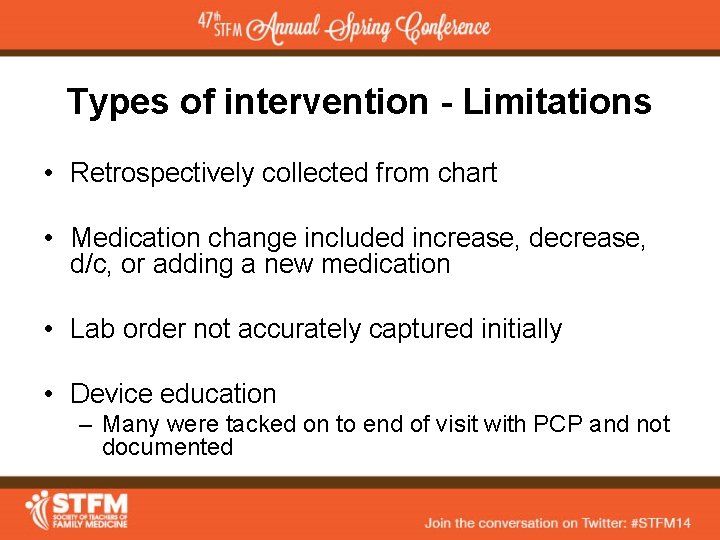
Types of intervention - Limitations • Retrospectively collected from chart • Medication change included increase, decrease, d/c, or adding a new medication • Lab order not accurately captured initially • Device education – Many were tacked on to end of visit with PCP and not documented
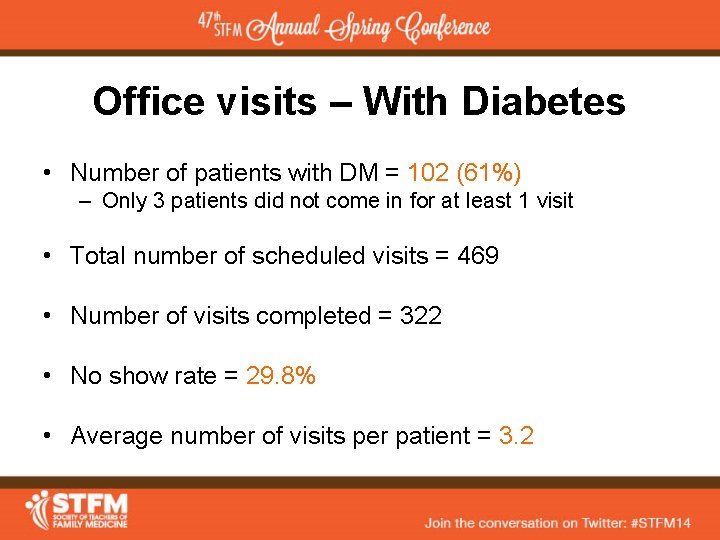
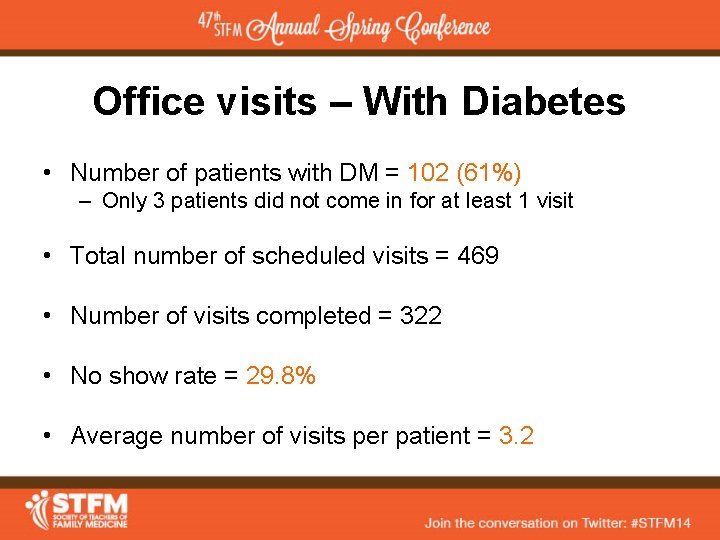
Office visits – With Diabetes • Number of patients with DM = 102 (61%) – Only 3 patients did not come in for at least 1 visit • Total number of scheduled visits = 469 • Number of visits completed = 322 • No show rate = 29. 8% • Average number of visits per patient = 3. 2
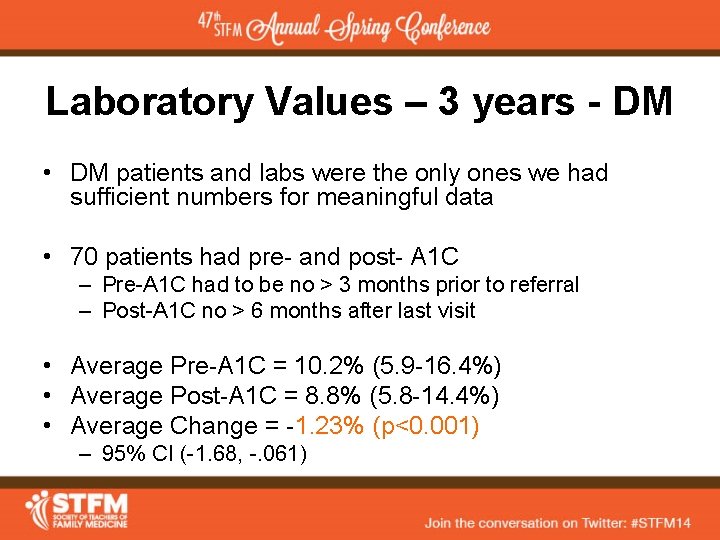
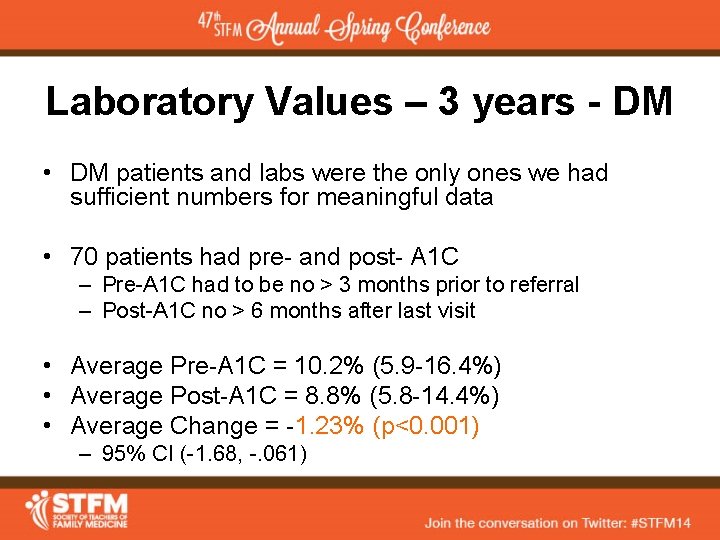
Laboratory Values – 3 years - DM • DM patients and labs were the only ones we had sufficient numbers for meaningful data • 70 patients had pre- and post- A 1 C – Pre-A 1 C had to be no > 3 months prior to referral – Post-A 1 C no > 6 months after last visit • Average Pre-A 1 C = 10. 2% (5. 9 -16. 4%) • Average Post-A 1 C = 8. 8% (5. 8 -14. 4%) • Average Change = -1. 23% (p<0. 001) – 95% CI (-1. 68, -. 061)

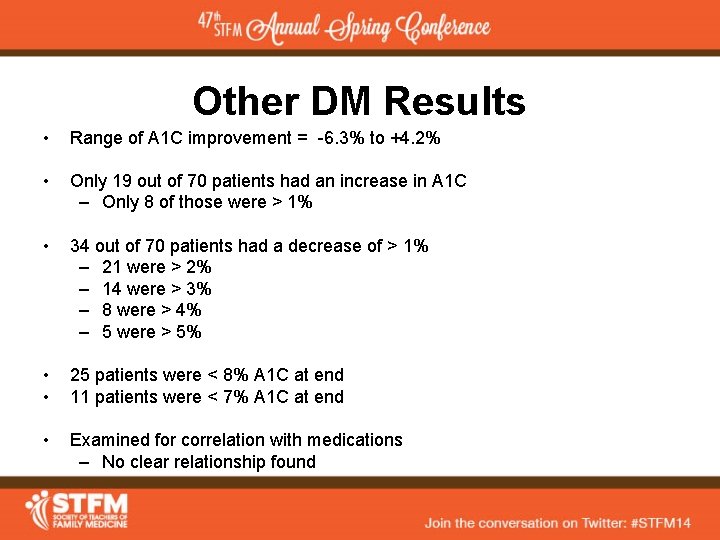
Other DM Results • Range of A 1 C improvement = -6. 3% to +4. 2% • Only 19 out of 70 patients had an increase in A 1 C – Only 8 of those were > 1% • 34 out of 70 patients had a decrease of > 1% – 21 were > 2% – 14 were > 3% – 8 were > 4% – 5 were > 5% • • 25 patients were < 8% A 1 C at end 11 patients were < 7% A 1 C at end • Examined for correlation with medications – No clear relationship found
Challenges / Limitations • Recruitment of patients • High no-show rate • Retrospective collection method • Multiple factors involved in improvement • Not everything pharmacy did was documented

QUESTIONS? COMMENTS?
 Paul cornelison
Paul cornelison Emory dermatology clinic
Emory dermatology clinic Cogdell family clinic
Cogdell family clinic Role of pharmacognosy in traditional system of medicine
Role of pharmacognosy in traditional system of medicine What is web role and worker role in azure
What is web role and worker role in azure Role making role taking beispiele
Role making role taking beispiele Statuses and their related roles determine
Statuses and their related roles determine Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus medical center family medicine residency
Meritus medical center family medicine residency Family physician facts
Family physician facts Milestones family medicine
Milestones family medicine Janalynn beste md
Janalynn beste md Principles of primary health care
Principles of primary health care Wonca definition of family medicine
Wonca definition of family medicine Pediatrics shelf percentiles
Pediatrics shelf percentiles Family ecomap example
Family ecomap example Unfunded residency positions
Unfunded residency positions Af williams family medicine center
Af williams family medicine center Kaiser permanente san diego family medicine residency
Kaiser permanente san diego family medicine residency Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord nc
Cabarrus family medicine concord nc Uthscsa internal medicine residents
Uthscsa internal medicine residents St louis university family medicine residency
St louis university family medicine residency