Orthopedic Neurological Evaluation Dr Michael Gillespie Doctor of
- Slides: 40
Orthopedic & Neurological Evaluation Dr. Michael Gillespie Doctor of Chiropractic
Anatomic and Biomechanical Principles It is necessary to understand normal anatomy and healthy biomechanical relationships to accurately evaluate orthopedic and neurological conditions. Understand the relationship between structure and function. Anatomical and biomechanical variants can be present with a particular patient.
Clinical Assessment Protocol Patient History Inspection / observation Palpation Range of Motion Orthopedic and Neurologic Testing Diagnostic Imaging Functional Testing
Documentation Evaluate progress. Share information with other practitioners. Insurance records. Malpractice.
SOAP Notes Subjective – Patient History Objective – Observation and Testing Assessment – Based on compilation of findings Plan – Further testing and / or treatment
Patient History A thorough patient history can often lead to a proper diagnosis with no further testing. Emphasize the aspect of the patient history with the greatest clinical significance. Acquire all of the patient’s history whether or not something seems relevant at the time.
Patient History Keep the patient focused on the problem. Listen carefully. Do not lead the patient towards answers.
Closed-Ended History Question and Answer Format. Written Forms
Open-Ended History Dialogue between patient and examiner. Identify other problems that are either directly or indirectly related to the presenting complaint. Address the patient’s fears and concerns. Develop rapport. Keep the patient focused on the presenting problem.
OPQRST Mnemonic Onset of complaint Provoking or Palliative concerns Quality of pain Radiation to particular areas Site and Severity of complaint Time frame complaint
History – Other Factors Family History Occupational History Social History
Observation / Inspection General Appearance Functional Status Body Type Postural deviations Gait Muscle guarding Compensatory movements Assistant devices
Inspection – three layers Skin Subcutaneous tissue Bony structure
Skin Inspection Bruising Scarring Trauma or surgery Changes in color Vascular changes of inflammation Vascular deficiency – pallor or cyanosis Pigmented areas / Hairy areas Change in texture Open wounds – traumatic or insidious
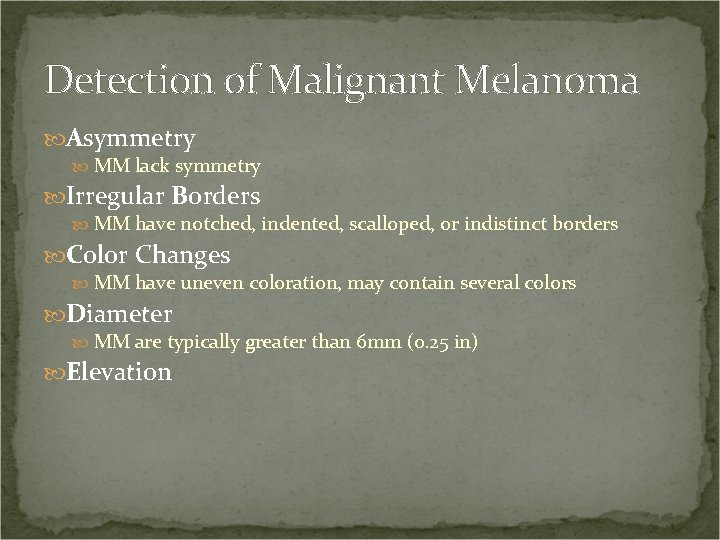
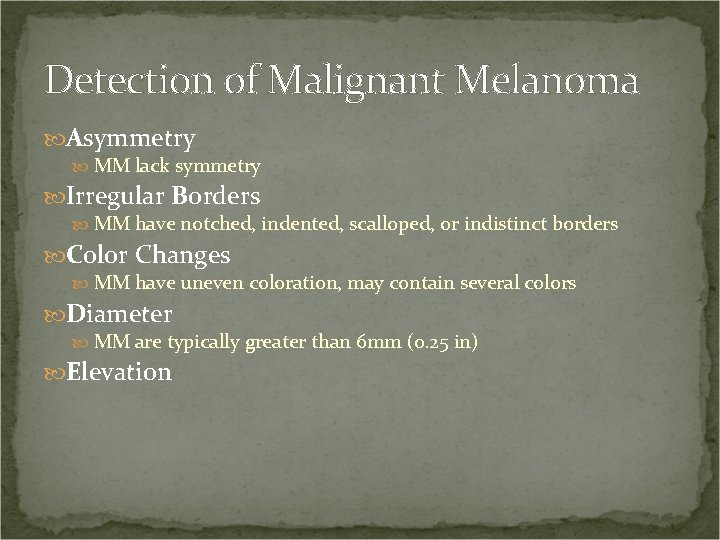
Detection of Malignant Melanoma Asymmetry MM lack symmetry Irregular Borders MM have notched, indented, scalloped, or indistinct borders Color Changes MM have uneven coloration, may contain several colors Diameter MM are typically greater than 6 mm (0. 25 in) Elevation
Subcutaneous Soft Tissue Inspection Evaluate for inflammation and swelling Atrophy Increase in size Edema, articular effusion, muscle hypertrophy Nodules, lymph nodes, or cysts Compare b/l symmetry, utilize circumferential measurements
Bony Structure Inspection Evaluate bony structure when gait or range of motion is altered. Evaluate the spine Scoliosis Kyphosis Lordosis Pelvic tilt Shoulder height Evaluate for congenital and traumatic bone deformities
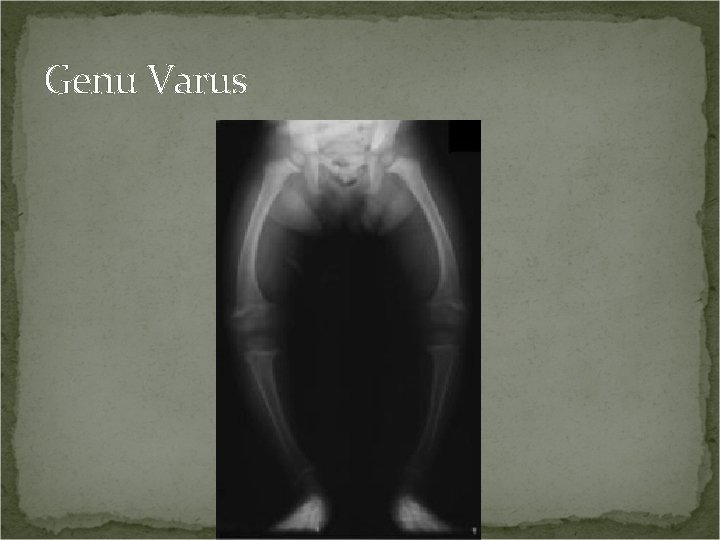
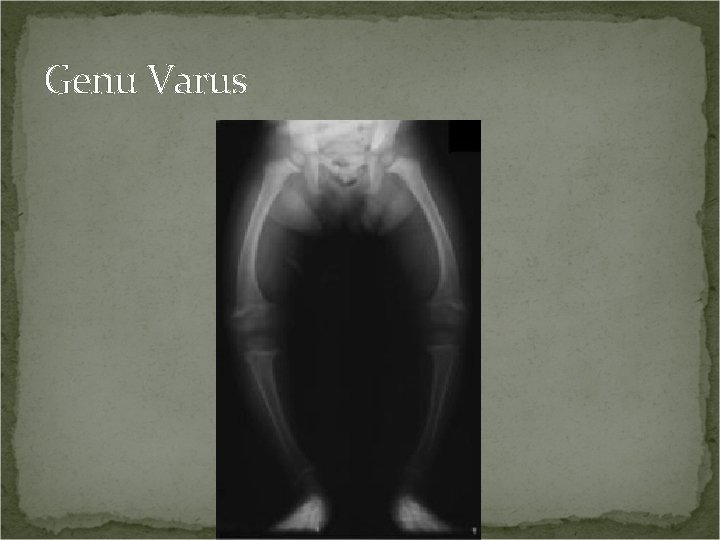
Genu Varus
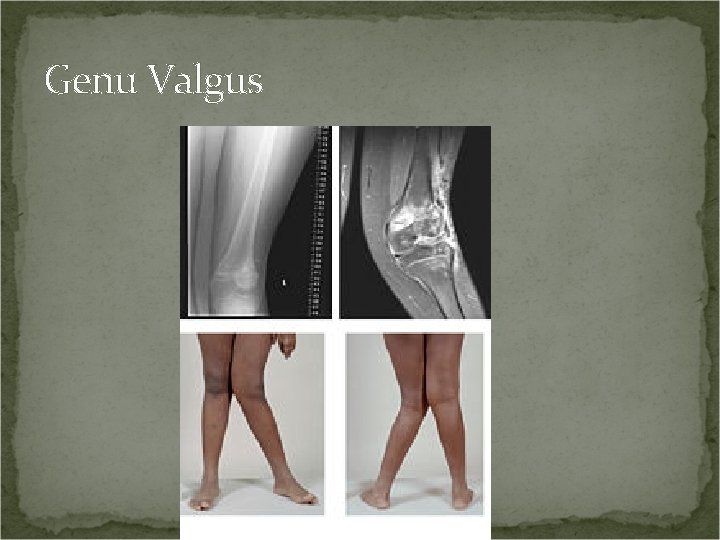
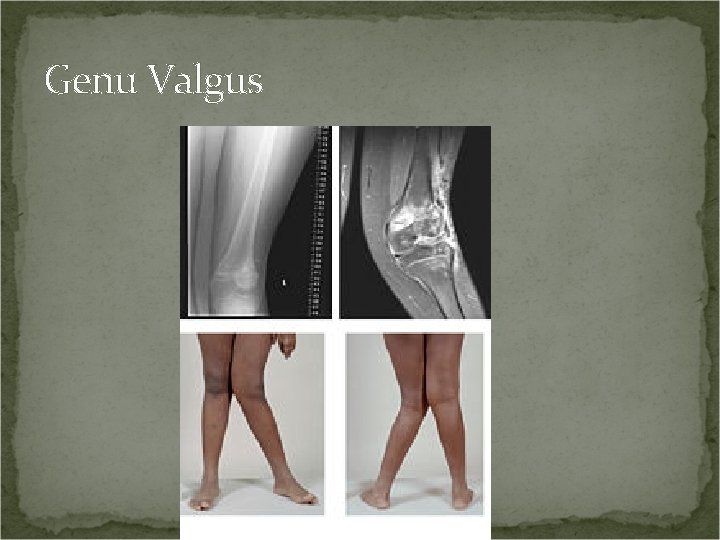
Genu Valgus
Palpation Palpate the patient in conjunction with inspection. Begin with a light touch. Dysesthesia. Hypoesthesia. Hyperesthesia. Anesthesia.
Skin Palpation Evaluate skin temperature High – inflammation Low – vascular insufficiency Adhesions
Subcutaneous Soft Tissue Palpation Subcutaneous soft tissue – fat, fascia, tendons, muscles, ligaments, joint capsules, nerves, blood vessels. Palpate with more pressure than with skin. Palpate for tenderness and swelling or edema.
Tenderness Grading Scale Grade I - Patient complains of pain Grade II - Patient complains of pain and winces Grade III - Patient winces and withdraws the joint Grade IV – Patient will not allow palpation of the joint
Types of Swelling Immediately after injury, hard and warm Contains blood 8 to 24 hours after an injury, boggy or spongy Contains synovial fluid Tough and dry Callus
Types of Swelling Thickened and leathery Chronic swelling Soft and fluctuating Acute Hard Bone Thick and slow moving Pitting edema
Pulse Palpate for pulse rate, rhythm, and amplitude Normal healthy resting pulse rate for an adult is 60 – 100 bpm
Palpating Bony Structures Detection of alignment problems Dislocations, luxations, subluxations, fractures Identify ligaments and tendons that attach to the bones Detect bony enlargements
Range of Motion Passive Active Resisted
Passive Range of Motion The examiner moves the body part without the patient’s help. Note normal, increased, or decreased movement. Note pain. Capsular or ligamentous lesion on side of movement and / or muscular lesion on side opposite of movement.
Six Range of Motion Pain Variations 1. Normal mobility with no pain. No lesion – normal joint. 2. Normal mobility with pain. Minor ligament sprain or capsular lesion. 3. Hypomobility with no pain. Adhesion.
Six Range of Motion Pain Variations 4. Hypomobility with pain. Acute ligament sprain or capsular lesion. Guarding from muscle spasm. 5. Hypermobility with no pain. Complete tear with no fibers intact where pain can be elcited. 6. Hypermobility with pain. Partial tear with some fibers still intact.
Sprain Vs. Strain Sprain - A sprain is an injury involving the stretching or tearing of a ligament (tissue that connects bone to bone) or a joint capsule, which help provide joint stability. Strain - Strains are injuries that involve the stretching or tearing of a musculo-tendinous (muscle and tendon) structure.
End Feel Evaluate for end feel after determining the degree of passive range of motion. Passively move the joint to the end of its range of motion and then apply slight overpressure to the joint.
End Feel Evaluation Table 1 -1 Page 6
Active Range of Motion Yields information regarding the patient’s general ability and willingness to use a body part. Assessment value is limited. Note the degree of motion as well as pain elicited. Crepitus should be noted. Inclinometers and goniometers are used to measure range of motion.
Inclinometer
Goniometer
Resisted Range of Motion Resisted range of motion assesses musculotendinous and neurologic structures. Musculotendinous injuries tend to be more painful than they are weak. Neurologic injuries tend to be more weak than they are painful.
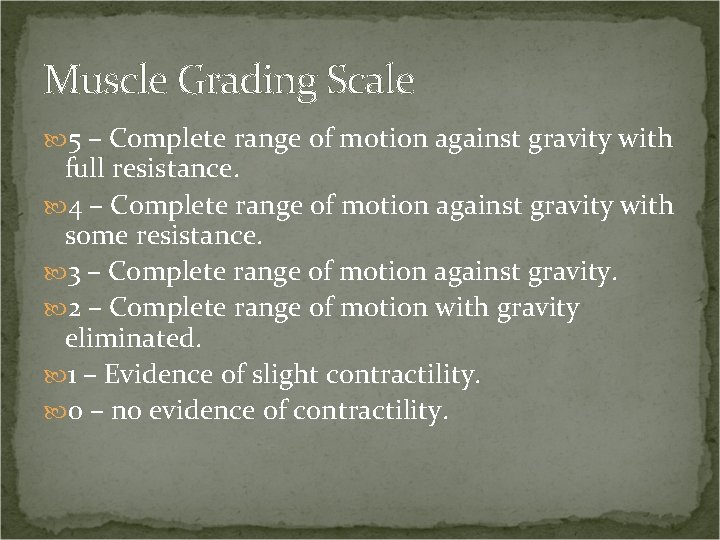
Muscle Grading Scale 5 – Complete range of motion against gravity with full resistance. 4 – Complete range of motion against gravity with some resistance. 3 – Complete range of motion against gravity. 2 – Complete range of motion with gravity eliminated. 1 – Evidence of slight contractility. 0 – no evidence of contractility.
Resistant Range of Motion Reactions Strong with no pain – Normal. Strong with pain – lesion of muscle or tendon. Weak and painless – neurological lesion or complete rupture of a tendon or muscle. Weak and painful – partial tear of muscle or tendon. Fracture, neoplasm, and acute inflammation are possibilities.
 Doctor who google drive
Doctor who google drive Vickie gillespie
Vickie gillespie Ann gillespie ira
Ann gillespie ira Duncan gillespie pilot
Duncan gillespie pilot Chuck gillespie
Chuck gillespie Site:slidetodoc.com
Site:slidetodoc.com Gillespie fracture
Gillespie fracture Dr laurie gillespie
Dr laurie gillespie Uw neurological surgery
Uw neurological surgery Muscle power neurological examination
Muscle power neurological examination Motor function neurological assessment
Motor function neurological assessment Solent physiotherapy
Solent physiotherapy Haapsalu neurological rehabilitation centre
Haapsalu neurological rehabilitation centre Power of limbs
Power of limbs Wessex neurological centre
Wessex neurological centre Ao classification system
Ao classification system What is focal neurological signs
What is focal neurological signs Fudoscopy
Fudoscopy Neurological based behavior
Neurological based behavior Glasgow coma scale video
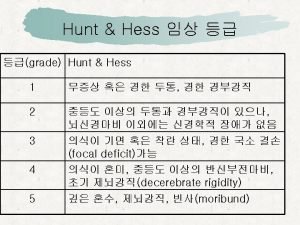
Glasgow coma scale video Wfns grading system
Wfns grading system Psychomotor considerations language acquisition
Psychomotor considerations language acquisition Noxious stimuli
Noxious stimuli Neurological disease
Neurological disease Neurological examination
Neurological examination Neurological assessment chart
Neurological assessment chart Trait theory criminology
Trait theory criminology Is adhd a neurological disorder
Is adhd a neurological disorder Orthopedic case presentation
Orthopedic case presentation Search engine optimization for orthopedic practices
Search engine optimization for orthopedic practices Nachlas test
Nachlas test Todd wilcox md
Todd wilcox md Orthopedic icats
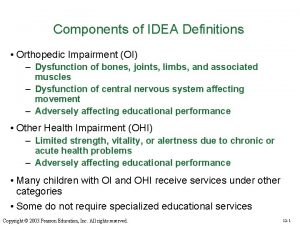
Orthopedic icats Idea orthopedic impairment
Idea orthopedic impairment Orthopedic history
Orthopedic history Causes of orthopedic impairment
Causes of orthopedic impairment Uva powerpoint
Uva powerpoint Lokmanya hospitals private limited
Lokmanya hospitals private limited O'donoghue maneuver
O'donoghue maneuver Orthopedic case presentation
Orthopedic case presentation Concussion
Concussion