Oneyear clinical outcome of interventionalistversus patient transfer strategies

- Slides: 16
One-year clinical outcome of interventionalistversus patient- transfer strategies for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction: Results from REVERSE-STEMI study Wei Feng Shen, MD, Ph. D Rui. Jin Hospital Shanghai Jiaotong University School of Medicine
One Year Outcome of Interventionalist Transfer for STEMI Background • Primary percutaneous coronary intervention (PPCI), when performed in a qualified center with a timely manner, has become the first treatment option for STEMI patients presenting to a hospital with PPCI capability. • Currently, almost half of hospitals equipped with angiographic facilities remain lack of interventionalists qualified for PPCI in China, where the volume of PCI increases dramatically in recent years. However, the strategy of transferring STEMI patients in large cities is still not consummate. • The RESVERSE-STEMI study investigated whether interventionalisttransfer strategy for PPCI could further shorten door-to-balloon (D 2 B) time and improve one-year clinical outcome in patients with acute STEMI.
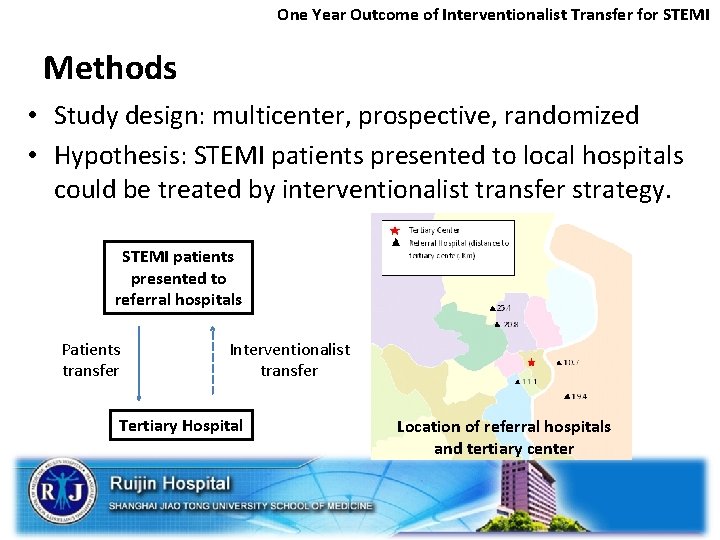
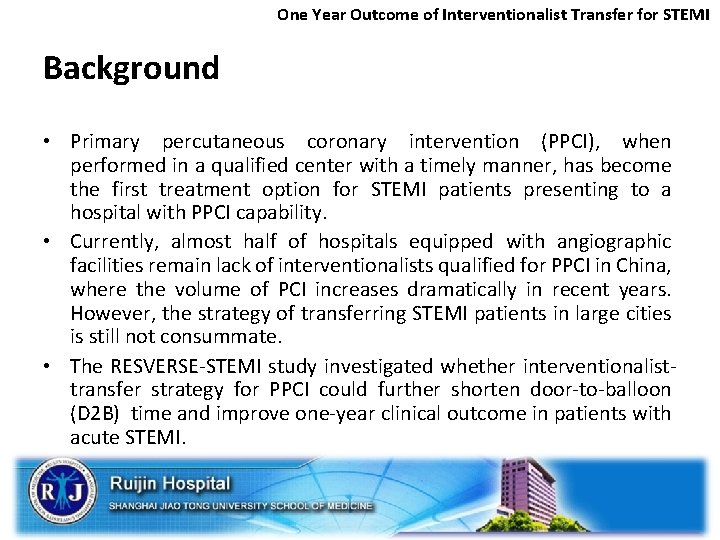
One Year Outcome of Interventionalist Transfer for STEMI Methods • Study design: multicenter, prospective, randomized • Hypothesis: STEMI patients presented to local hospitals could be treated by interventionalist transfer strategy. STEMI patients presented to referral hospitals Patients transfer Interventionalist transfer Tertiary Hospital Location of referral hospitals and tertiary center
One Year Outcome of Interventionalist Transfer for STEMI Methods • Tertiary hospital: Provided experienced interventionists to perform PCI in the referral hospitals, or received referral patients and then performed PPCI in the tertiary hospital. • Referral hospitals: (1) had coronary care unit (2) had cardiac catheterization laboratories (3) with cardiac interventional team, including operator, nurses and technicians, qualified for elective PCI (4) a formal training program of caring STEMI patients for technicians and nurses before starting the study
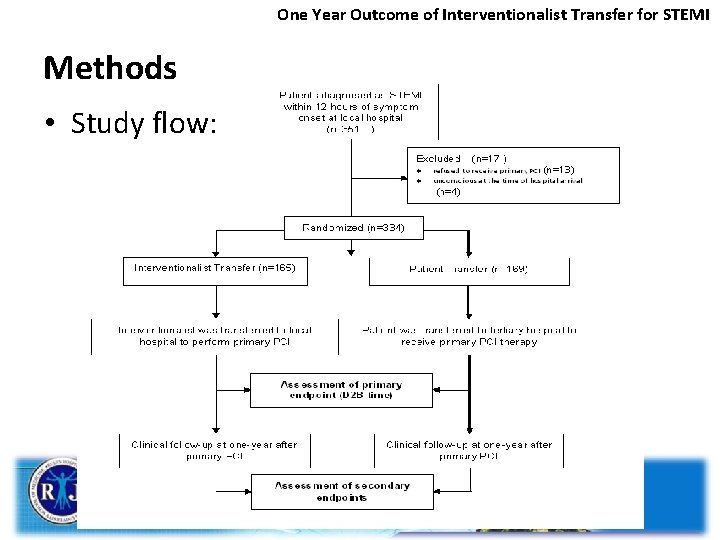
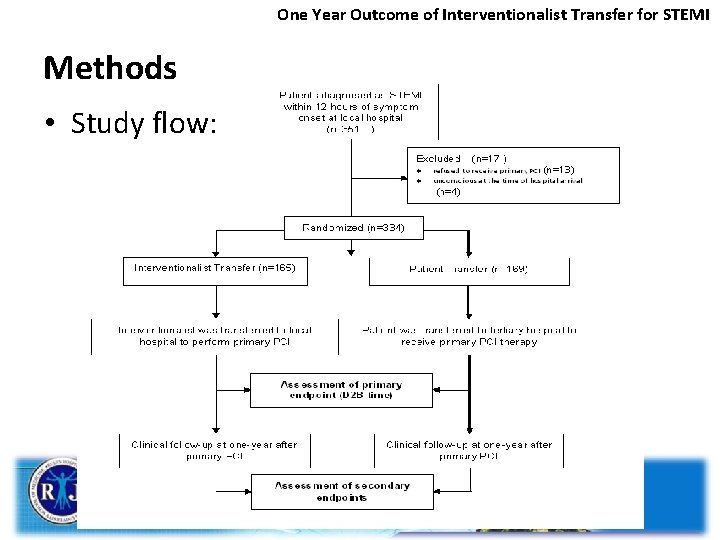
One Year Outcome of Interventionalist Transfer for STEMI Methods • Study flow:
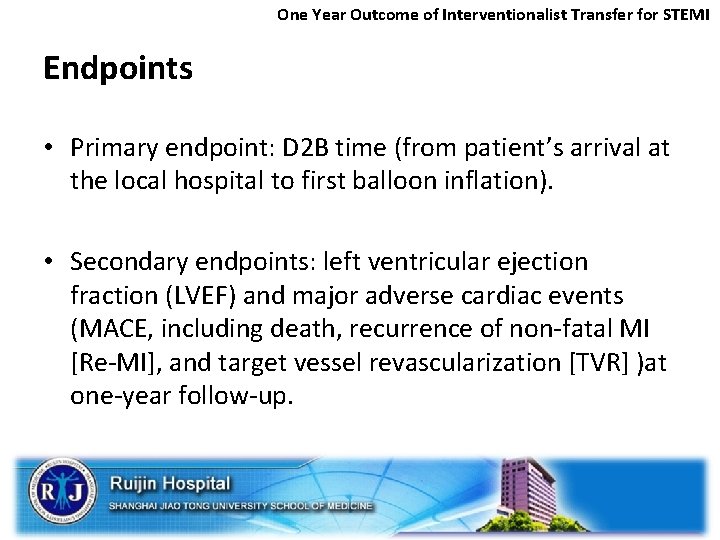
One Year Outcome of Interventionalist Transfer for STEMI Endpoints • Primary endpoint: D 2 B time (from patient’s arrival at the local hospital to first balloon inflation). • Secondary endpoints: left ventricular ejection fraction (LVEF) and major adverse cardiac events (MACE, including death, recurrence of non-fatal MI [Re-MI], and target vessel revascularization [TVR] )at one-year follow-up.
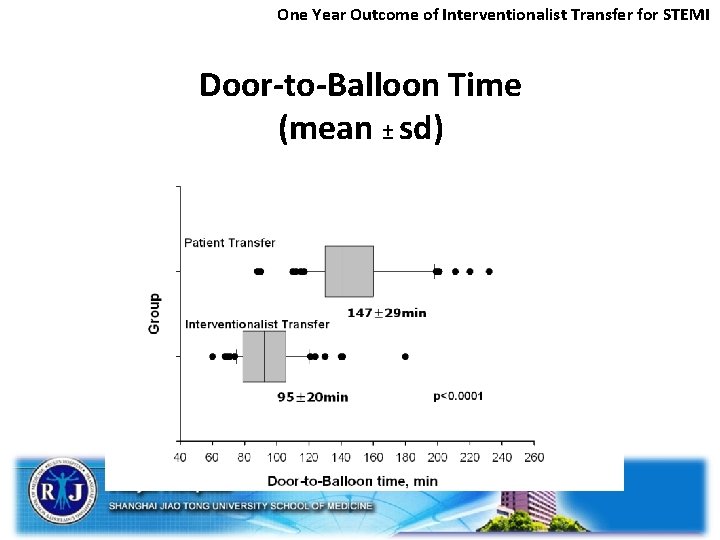
One Year Outcome of Interventionalist Transfer for STEMI Results • Baseline characteristics were not significantly different between the interventionalist- and patient-transfer groups, and medications at the end of one-year follow-up were similar. • Primary endpoint of D 2 B time was significantly reduced (median: 92 min vs. 141 min, p<0. 0001) with the interventionalist-transfer strategy, and more patients had first balloon angioplasty < 90 min (21. 2% vs. 7. 7%, p<0. 001).
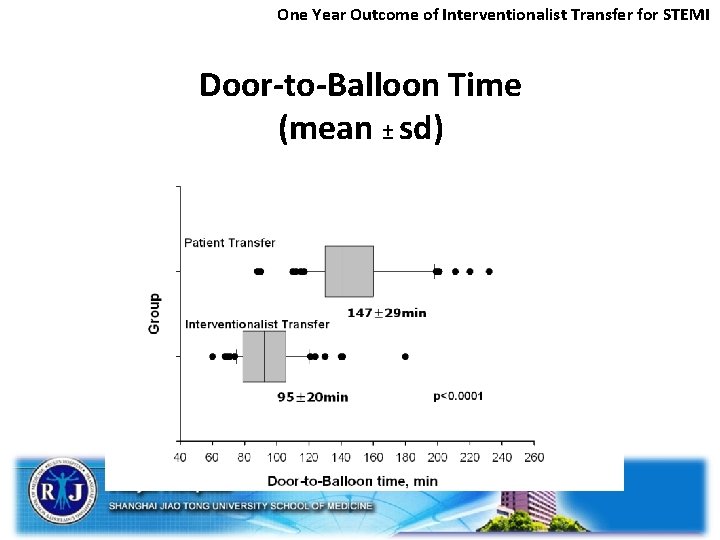
One Year Outcome of Interventionalist Transfer for STEMI Door-to-Balloon Time (mean ± sd)
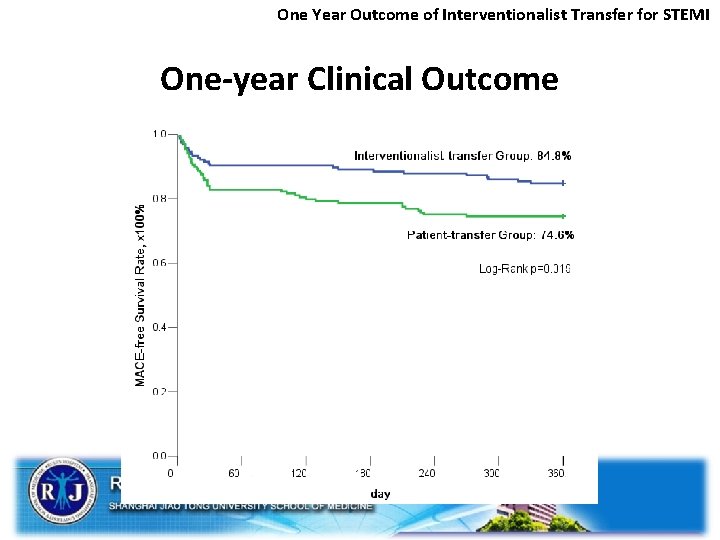
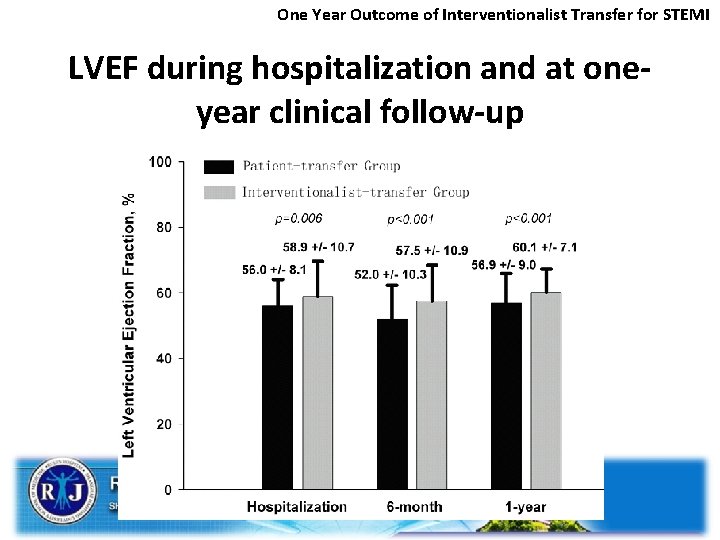
One Year Outcome of Interventionalist Transfer for STEMI Results • LVEF was significantly higher in the interventionalisttransfer group than in the patient-transfer group during hospitalization and at 6 -month and one-year follow-up. • The one-year MACE-free survival was significantly improved with interventionalist-transfer strategy (84. 8% vs. 74. 6%, p=0. 019).
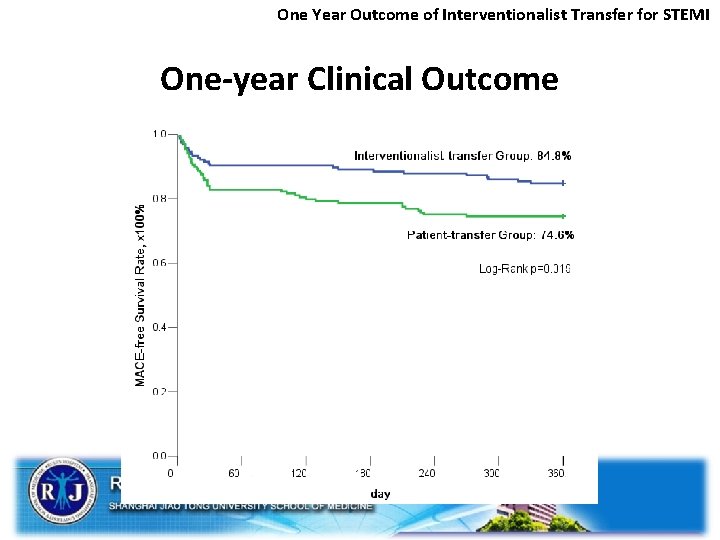
One Year Outcome of Interventionalist Transfer for STEMI One-year Clinical Outcome
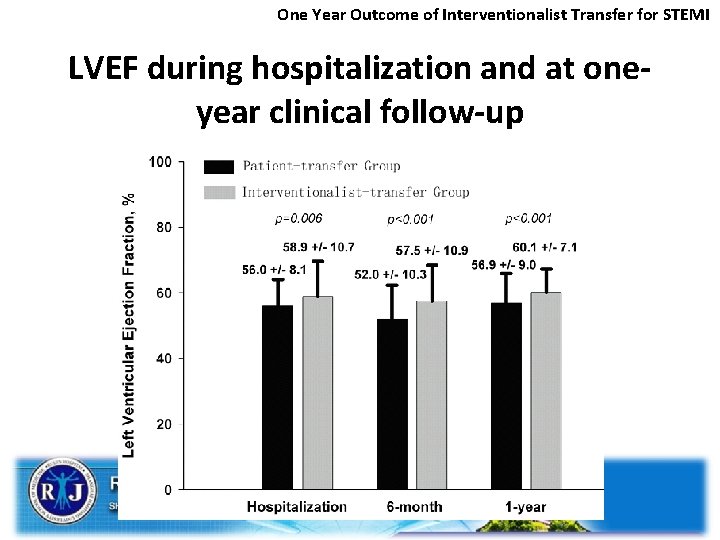
One Year Outcome of Interventionalist Transfer for STEMI LVEF during hospitalization and at oneyear clinical follow-up
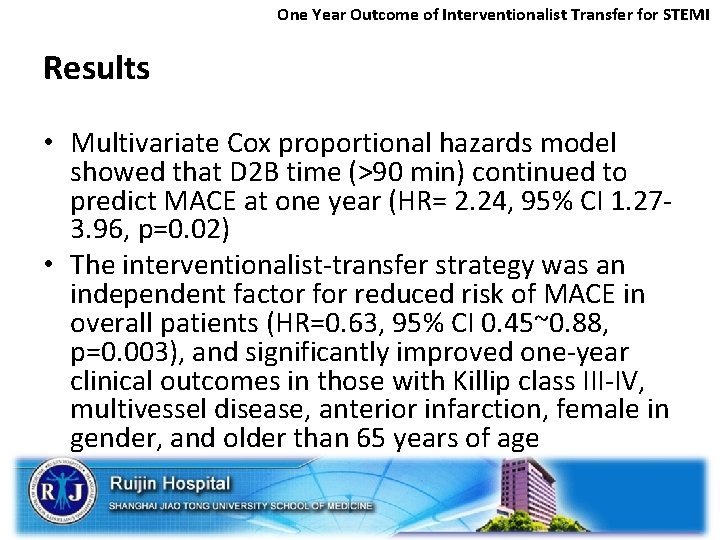
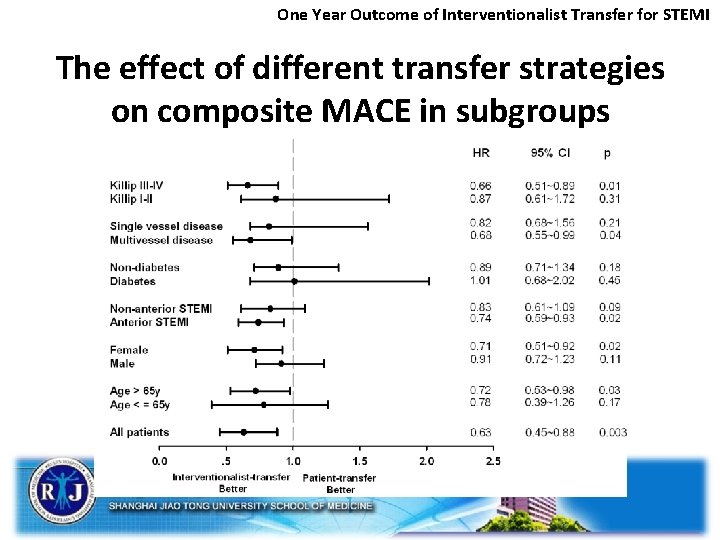
One Year Outcome of Interventionalist Transfer for STEMI Results • Multivariate Cox proportional hazards model showed that D 2 B time (>90 min) continued to predict MACE at one year (HR= 2. 24, 95% CI 1. 273. 96, p=0. 02) • The interventionalist-transfer strategy was an independent factor for reduced risk of MACE in overall patients (HR=0. 63, 95% CI 0. 45~0. 88, p=0. 003), and significantly improved one-year clinical outcomes in those with Killip class III-IV, multivessel disease, anterior infarction, female in gender, and older than 65 years of age
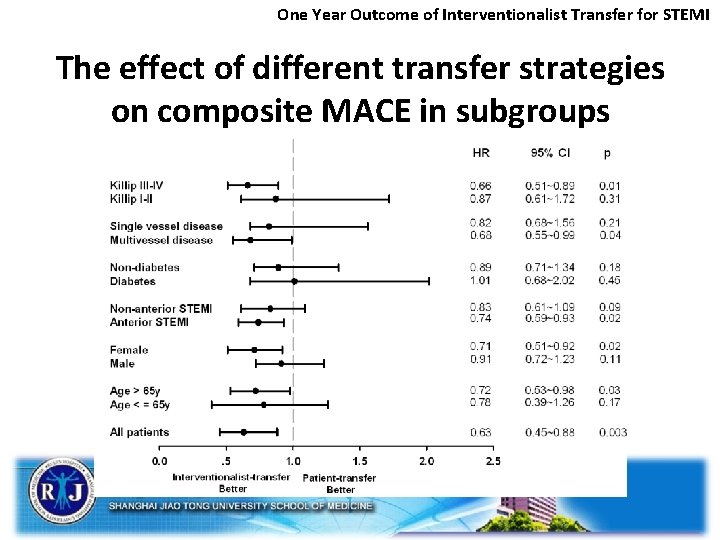
One Year Outcome of Interventionalist Transfer for STEMI The effect of different transfer strategies on composite MACE in subgroups
One Year Outcome of Interventionalist Transfer for STEMI Conclusions • The interventionalist-transfer strategy resulted in significantly reduced D 2 B time and subsequently improved one-year clinical outcome. • This novel transfer strategy for primary PCI may improve the care of STEMI patients presenting to a non-PPCI-capable hospital, particularly in a region where patient transfers could be prolonged by congestion.
One Year Outcome of Interventionalist Transfer for STEMI Limitations • First, this study was powered on D 2 B time. Nevertheless, the results demonstrated significant difference in clinical outcomes at one-year follow-up between the two treatment strategies. • Second, the interventionalist-transfer strategy required PCI facilities or materials, and nurses or paramedics adequately trained to deal with STEMI patients and their acute problems in the local hospitals. • Third, compared with findings in contemporary studies, the proportion of patients with a D 2 B time <90 min was still relatively low in the interventionalist-transfer group. • Finally, the current interventionalist-transfer strategy may be a tentative option in shortening D 2 B time for STEMI patients and physician training in a single city with hospitals located close to each other. This model may not be applied to a rural geographic setting with long transfer distance.

One Year Outcome of Interventionalist Transfer for STEMI Funding Sources • This work was supported by the grants from Shanghai Science and Technology Foundation (05 DZ 19503), and National Nature Science Foundation of China (30900589)
 Patient intervention comparison outcome
Patient intervention comparison outcome Pico patient
Pico patient Decision making with probabilities example
Decision making with probabilities example Patient 2 patient
Patient 2 patient Increase patient volume
Increase patient volume The method used for transferring a patient depends on
The method used for transferring a patient depends on Disturbance that transfers energy
Disturbance that transfers energy Learning outcome generator
Learning outcome generator 5 w's of bacon's rebellion
5 w's of bacon's rebellion Myocardial infractio
Myocardial infractio What was the outcome of china's age of exploration?
What was the outcome of china's age of exploration? Outcome based massage
Outcome based massage Examples of educational goals and objectives
Examples of educational goals and objectives Arti outcome adalah
Arti outcome adalah The age of exploration outcome the atlantic slave trade
The age of exploration outcome the atlantic slave trade Rapid access clinic london ontario
Rapid access clinic london ontario Outcome of prisoner's dilemma
Outcome of prisoner's dilemma