CRT 2017 How to Increase Your Patient Volume



- Slides: 52
CRT 2017 How to Increase Your Patient Volume and Screening Efficiency Ramon Quesada, MD, FACP, FACC, FSCAI Medical Director, Structural Heart , Complex PCI & Cardiac Research Miami Cardiac & Vascular Institute, Miami, Florida Clinical Associate Professor of Medicine, Florida International University Herbert Wertheim School of Medicine
Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Consulting Fees/Honoraria Company Names ABBOTT, BSC, VOLCANO MERRIT
Patient Volume • • • Appropriate Selection Positive Outcomes Complex anatomy – Complex procedure Increase volume for comfort and familiarity Avoid complications (pericardial effusion, air embolism, device embolization, etc)
Screening Efficiencies v v Improved Communication It is an Elective Procedure Patient is asymptomatic until it’s too late Patient Experience
Screening Efficiencies v Improved Communication Why do patients screen out? – – – Something they heard Change of mind Transportation Labs Anatomy NO ONE CALLED TO TELL ME!! Patient Experience
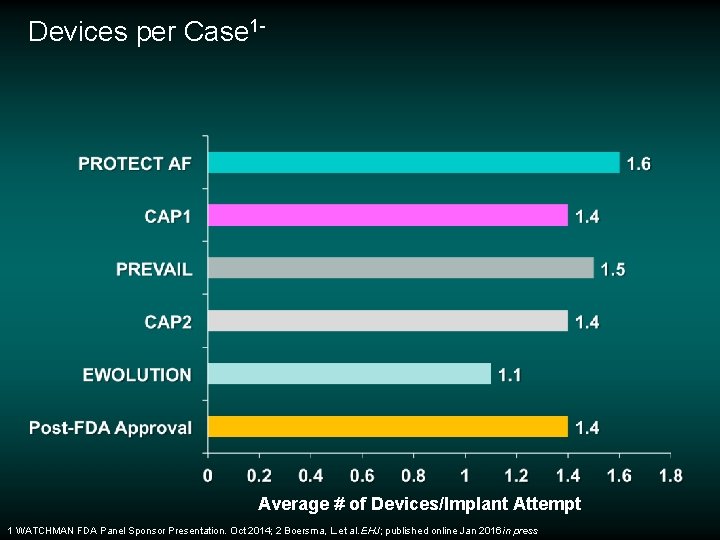
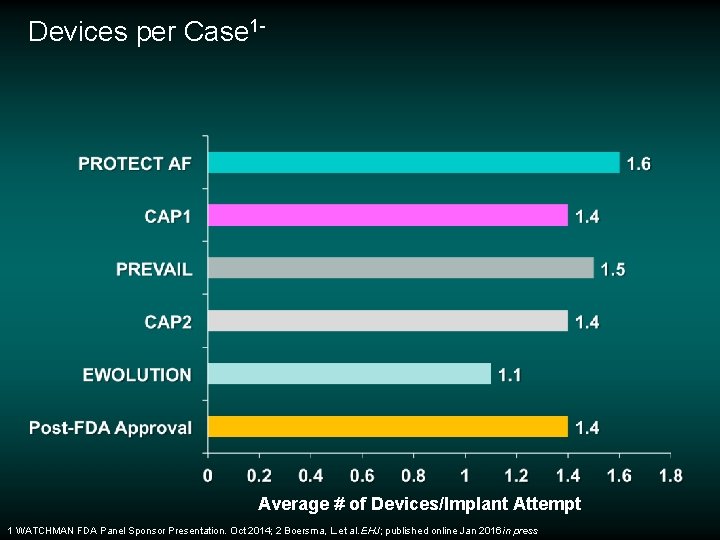
Devices per Case 1 - Average # of Devices/Implant Attempt 1 WATCHMAN FDA Panel Sponsor Presentation. Oct 2014; 2 Boersma, L. et al. EHJ; published online Jan 2016 in press
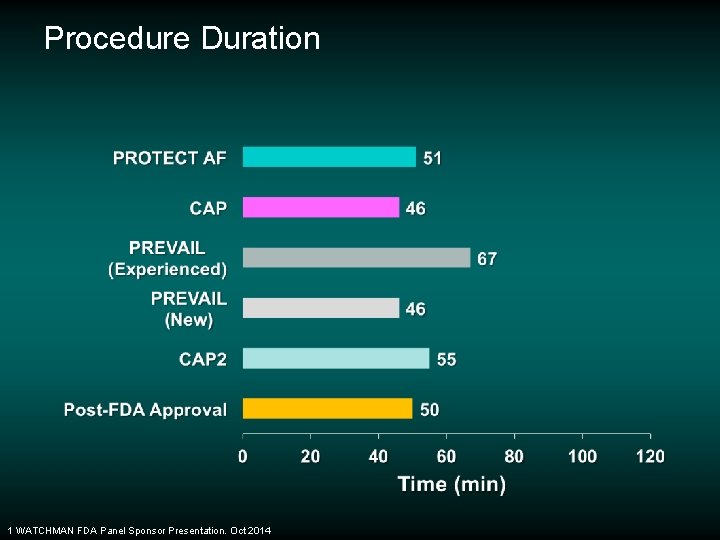
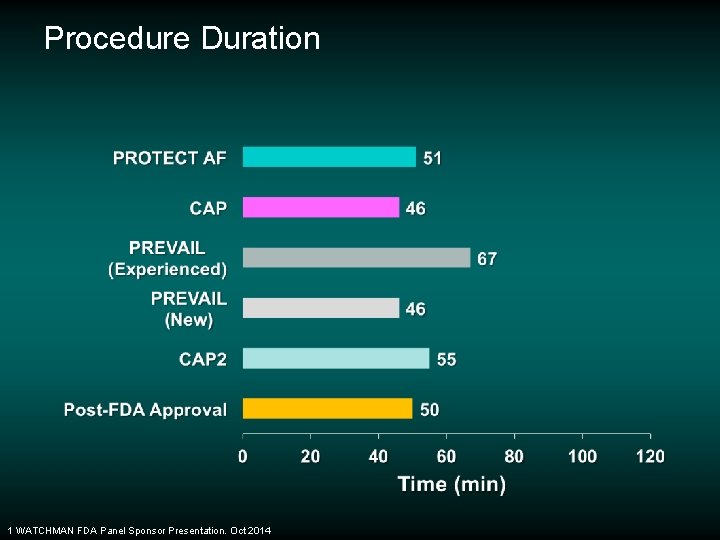
Procedure Duration 1 WATCHMAN FDA Panel Sponsor Presentation. Oct 2014
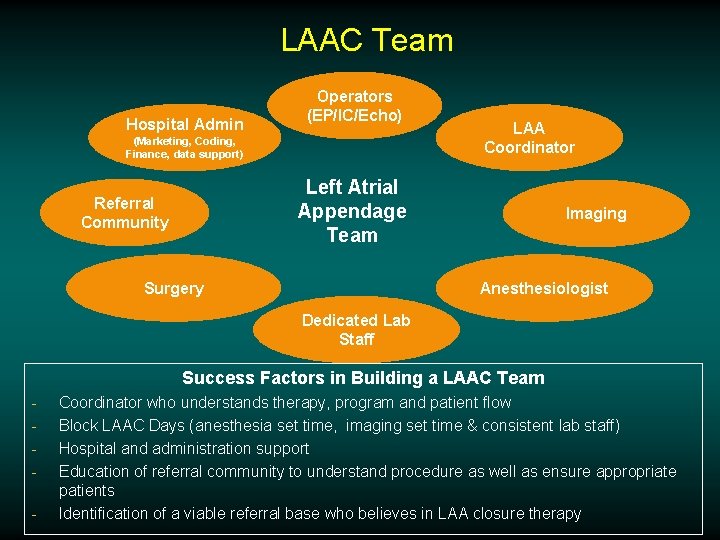
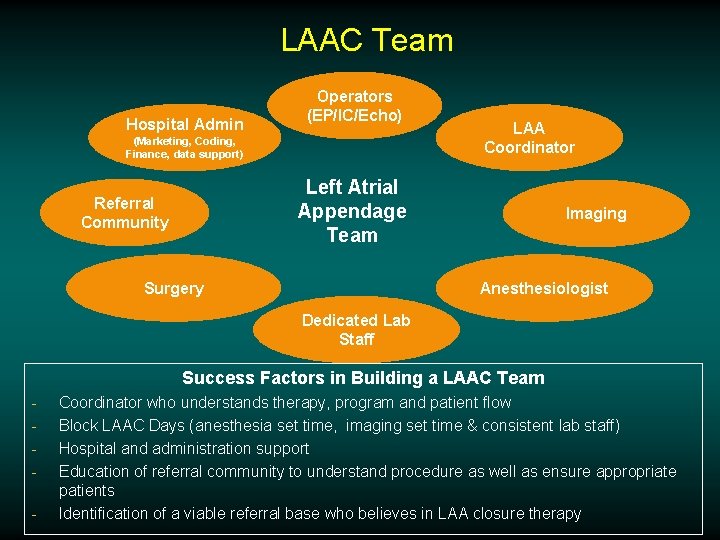
LAAC Team Hospital Admin Operators (EP/IC/Echo) (Marketing, Coding, Finance, data support) LAA Coordinator Left Atrial Appendage Team Referral Community Surgery Imaging Anesthesiologist Dedicated Lab Staff Success Factors in Building a LAAC Team - Coordinator who understands therapy, program and patient flow Block LAAC Days (anesthesia set time, imaging set time & consistent lab staff) Hospital and administration support Education of referral community to understand procedure as well as ensure appropriate patients Identification of a viable referral base who believes in LAA closure therapy
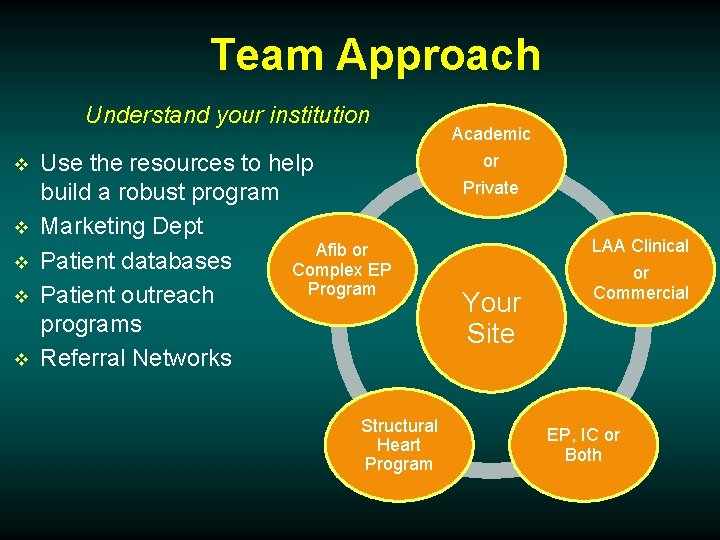
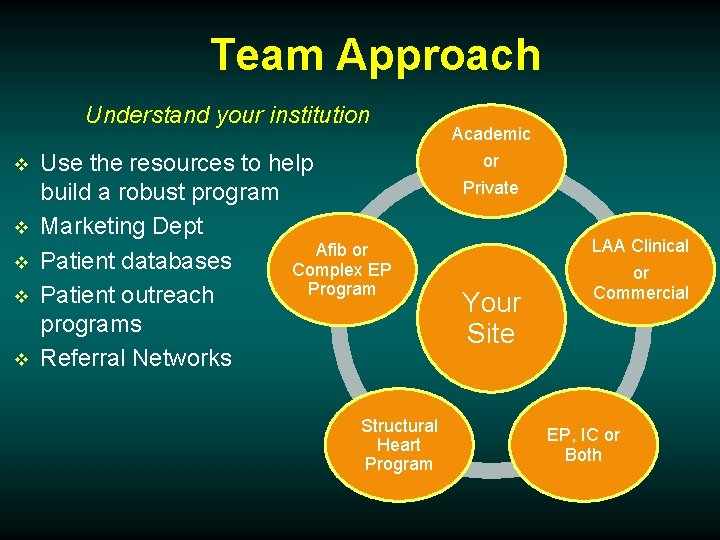
Team Approach Understand your institution v v v Use the resources to help build a robust program Marketing Dept Afib or Patient databases Complex EP Program Patient outreach programs Referral Networks Structural Heart Program Academic or Private LAA Clinical Your Site or Commercial EP, IC or Both
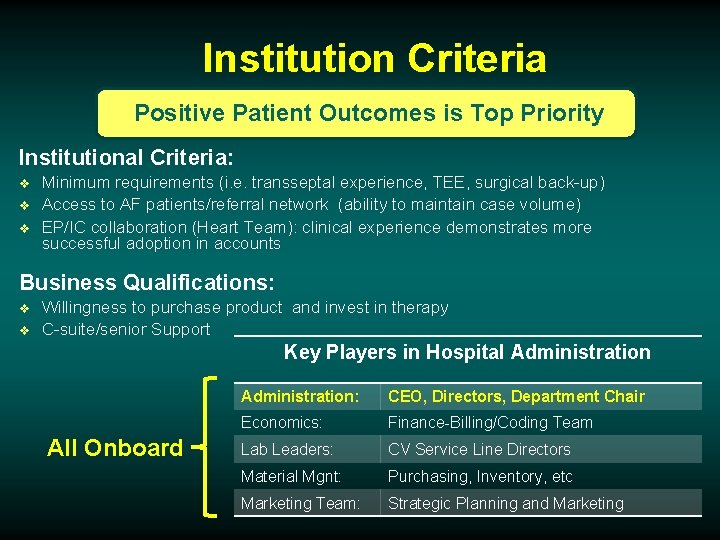
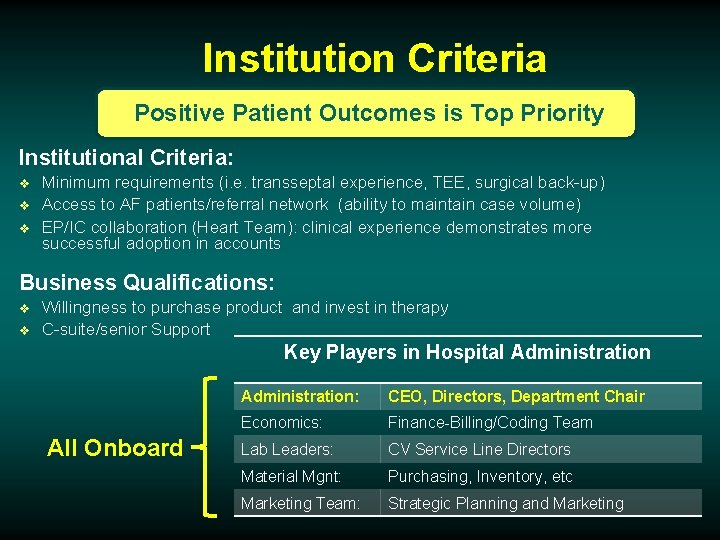
Institution Criteria Positive Patient Outcomes is Top Priority Institutional Criteria: v v v Minimum requirements (i. e. transseptal experience, TEE, surgical back-up) Access to AF patients/referral network (ability to maintain case volume) EP/IC collaboration (Heart Team): clinical experience demonstrates more successful adoption in accounts Business Qualifications: v v Willingness to purchase product and invest in therapy C-suite/senior Support Key Players in Hospital Administration All Onboard Administration: CEO, Directors, Department Chair Economics: Finance-Billing/Coding Team Lab Leaders: CV Service Line Directors Material Mgnt: Purchasing, Inventory, etc Marketing Team: Strategic Planning and Marketing
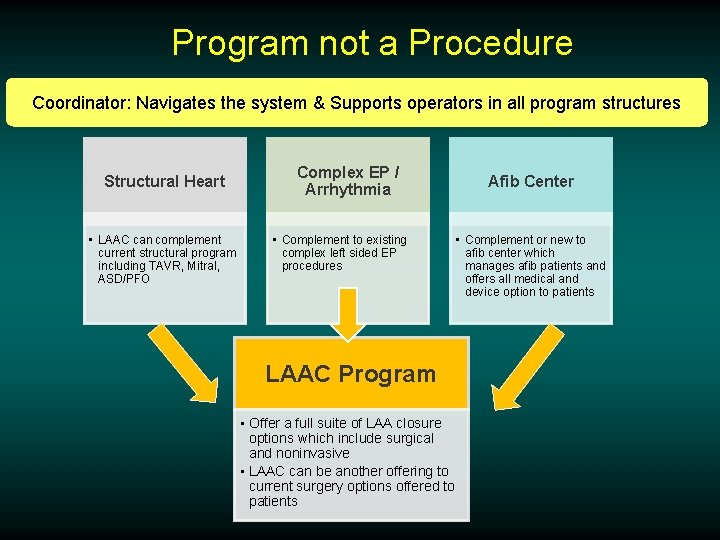
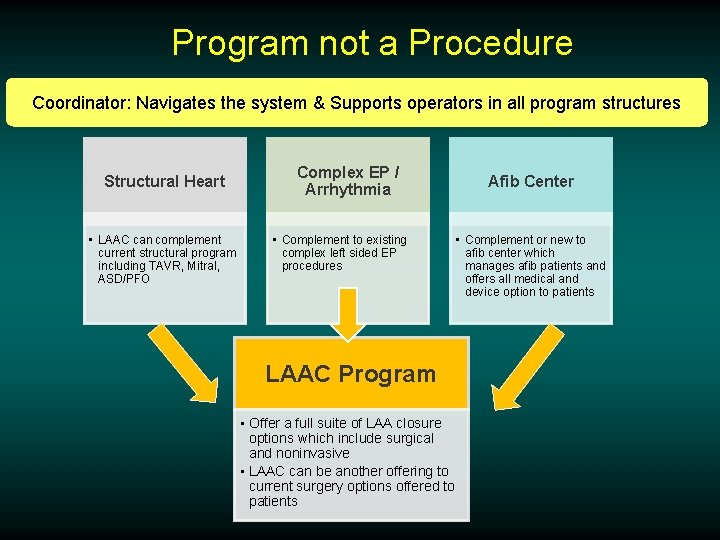
Program not a Procedure Coordinator: Navigates the system & Supports operators in all program structures Structural Heart • LAAC can complement current structural program including TAVR, Mitral, ASD/PFO Complex EP / Arrhythmia • Complement to existing complex left sided EP procedures LAAC Program • Offer a full suite of LAA closure options which include surgical and noninvasive • LAAC can be another offering to current surgery options offered to patients Afib Center • Complement or new to afib center which manages afib patients and offers all medical and device option to patients
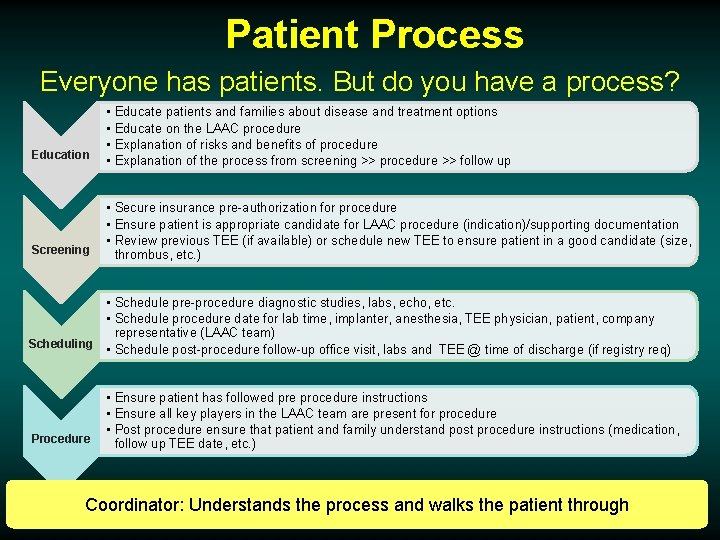
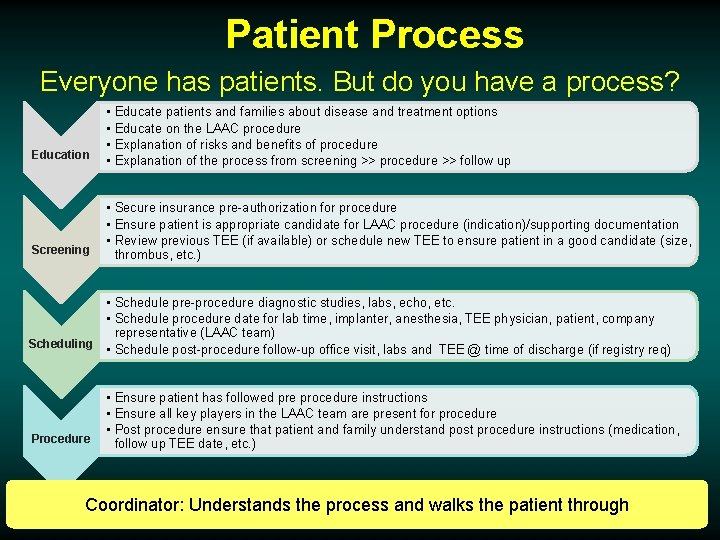
Patient Process Everyone has patients. But do you have a process? Education Screening • • Educate patients and families about disease and treatment options Educate on the LAAC procedure Explanation of risks and benefits of procedure Explanation of the process from screening >> procedure >> follow up • Secure insurance pre-authorization for procedure • Ensure patient is appropriate candidate for LAAC procedure (indication)/supporting documentation • Review previous TEE (if available) or schedule new TEE to ensure patient in a good candidate (size, thrombus, etc. ) • Schedule pre-procedure diagnostic studies, labs, echo, etc. • Schedule procedure date for lab time, implanter, anesthesia, TEE physician, patient, company representative (LAAC team) Scheduling • Schedule post-procedure follow-up office visit, labs and TEE @ time of discharge (if registry req) Procedure • Ensure patient has followed pre procedure instructions • Ensure all key players in the LAAC team are present for procedure • Post procedure ensure that patient and family understand post procedure instructions (medication, follow up TEE date, etc. ) Coordinator: Understands the process and walks the patient through
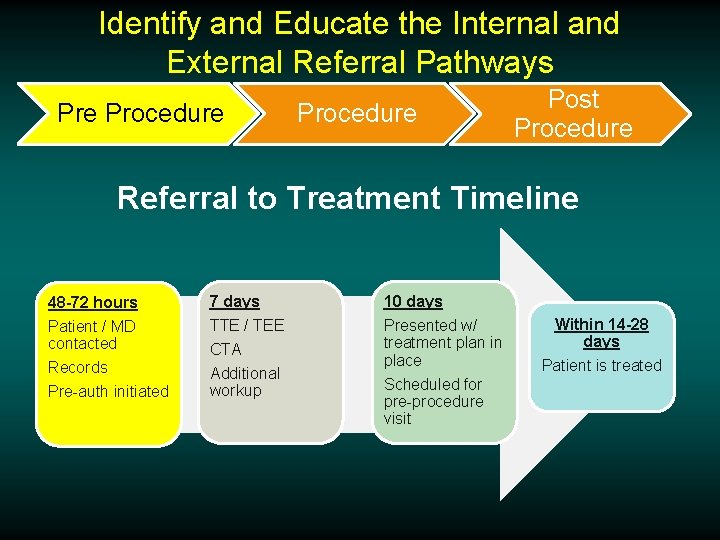
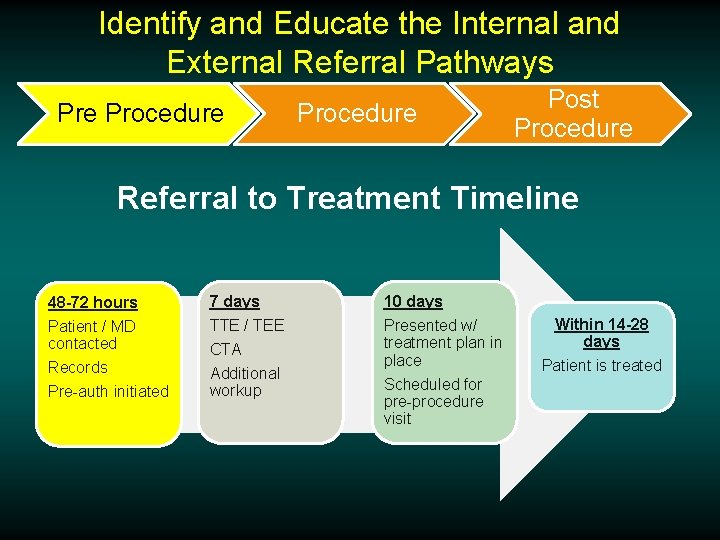
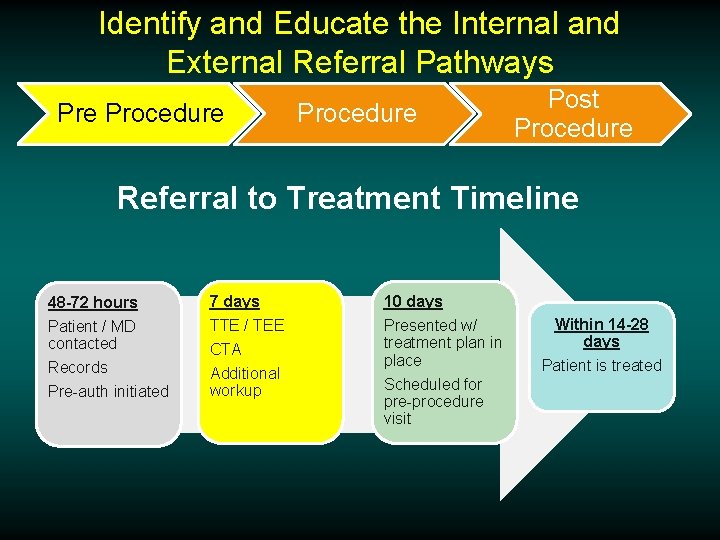
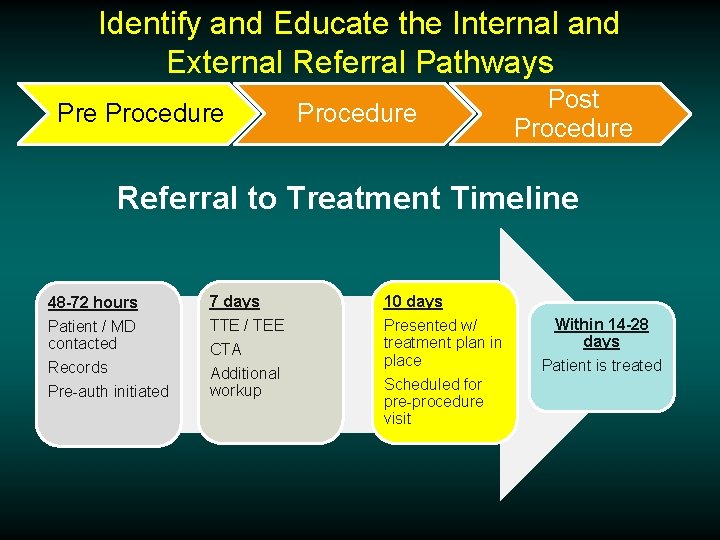
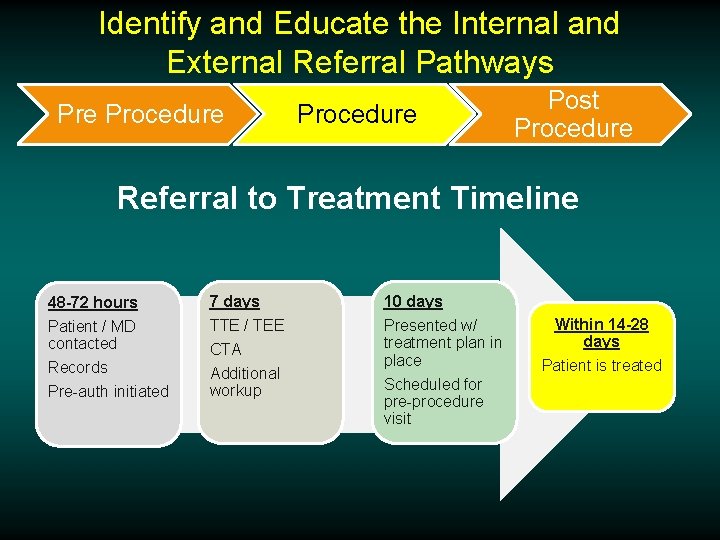
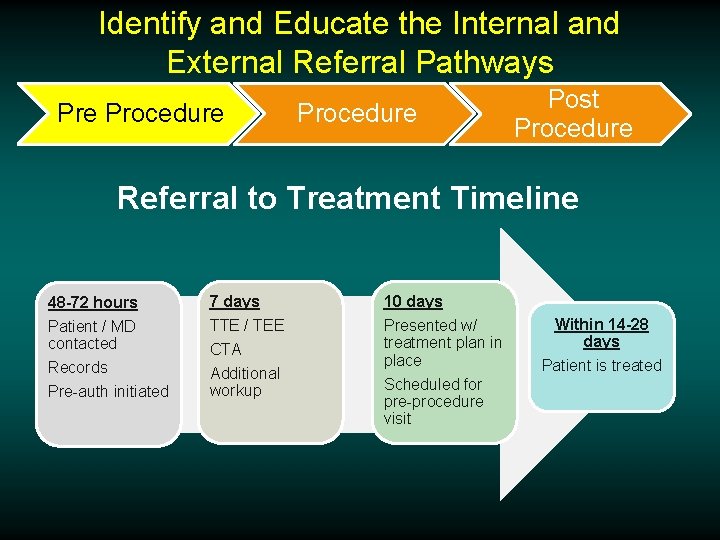
Identify and Educate the Internal and External Referral Pathways Pre Procedure Post Procedure Referral to Treatment Timeline 48 -72 hours 7 days 10 days Patient / MD contacted Records Pre-auth initiated TTE / TEE Presented w/ treatment plan in place Scheduled for pre-procedure visit CTA Additional workup Within 14 -28 days Patient is treated
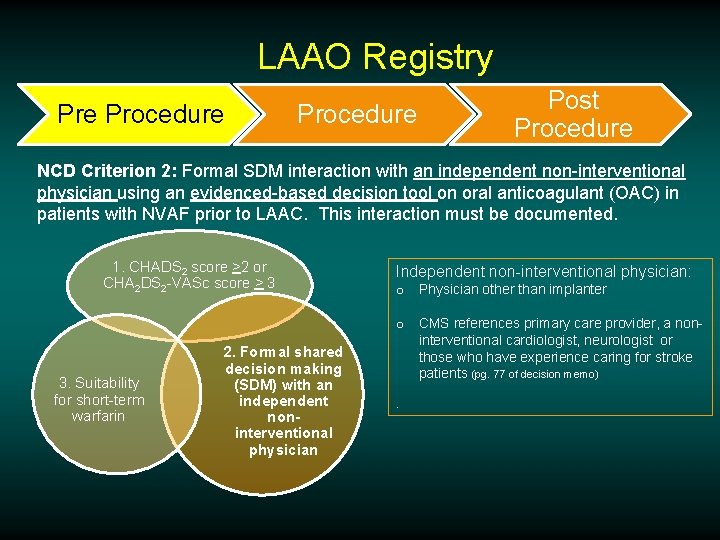
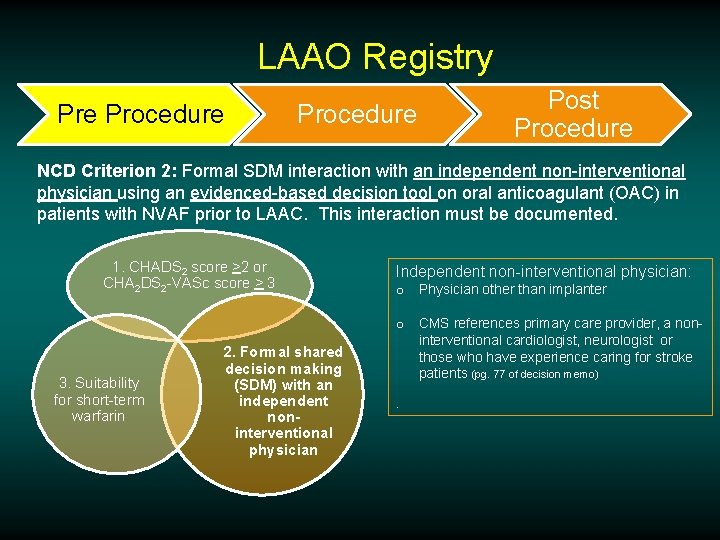
LAAO Registry Pre Procedure Post Procedure NCD Criterion 2: Formal SDM interaction with an independent non-interventional physician using an evidenced-based decision tool on oral anticoagulant (OAC) in patients with NVAF prior to LAAC. This interaction must be documented. 1. CHADS 2 score >2 or CHA 2 DS 2 -VASc score > 3 3. Suitability for short-term warfarin 2. Formal shared decision making (SDM) with an independent noninterventional physician Independent non-interventional physician: o Physician other than implanter o CMS references primary care provider, a noninterventional cardiologist, neurologist or those who have experience caring for stroke patients (pg. 77 of decision memo).
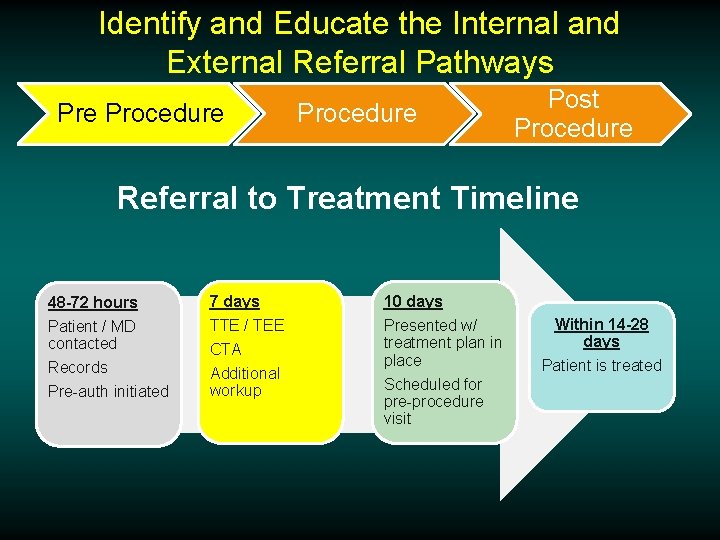
Identify and Educate the Internal and External Referral Pathways Pre Procedure Post Procedure Referral to Treatment Timeline 48 -72 hours 7 days 10 days Patient / MD contacted Records Pre-auth initiated TTE / TEE Presented w/ treatment plan in place Scheduled for pre-procedure visit CTA Additional workup Within 14 -28 days Patient is treated
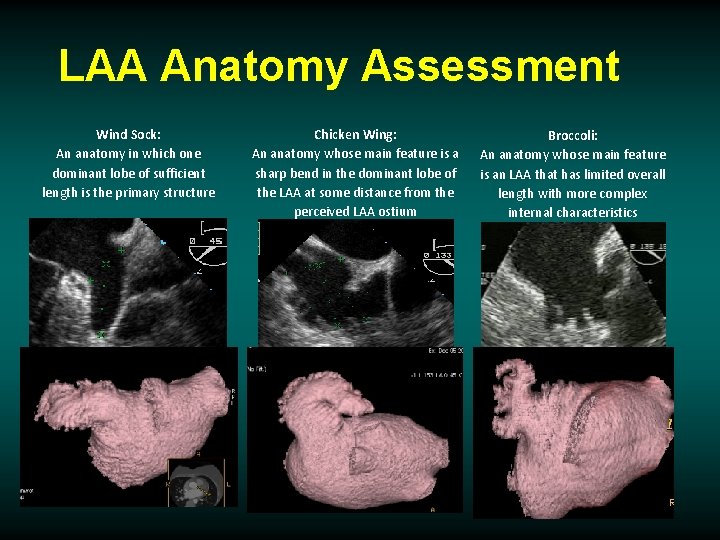
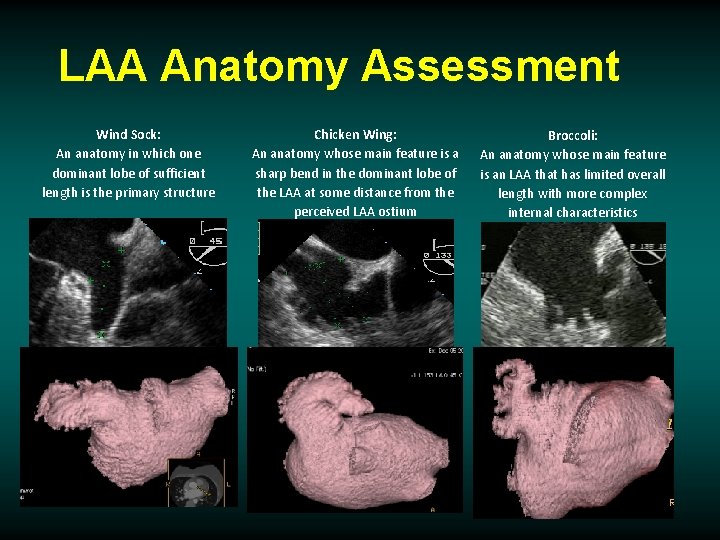
LAA Anatomy Assessment Wind Sock: An anatomy in which one dominant lobe of sufficient length is the primary structure Chicken Wing: An anatomy whose main feature is a sharp bend in the dominant lobe of the LAA at some distance from the perceived LAA ostium Broccoli: An anatomy whose main feature is an LAA that has limited overall length with more complex internal characteristics
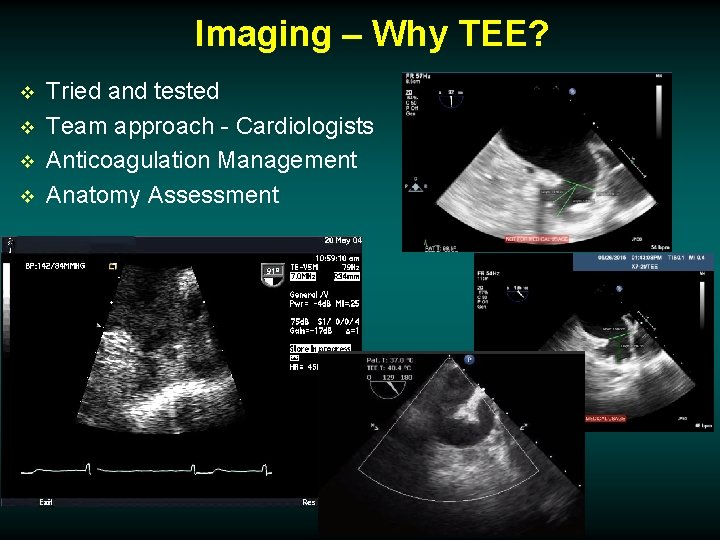
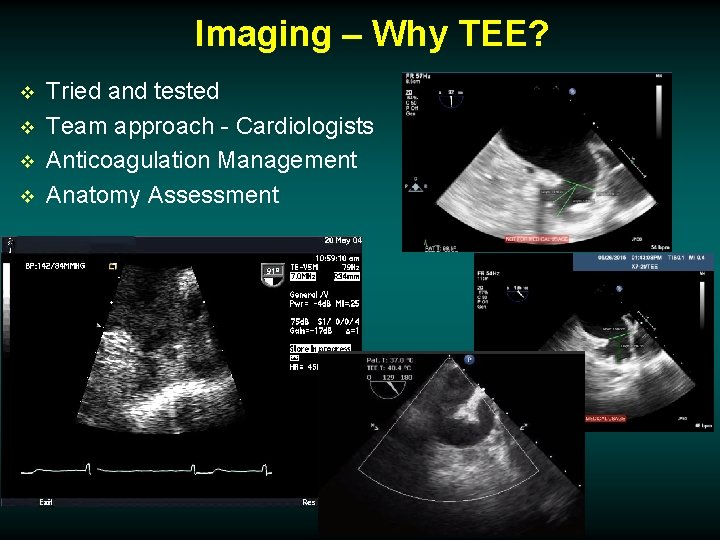
Imaging – Why TEE? v v Tried and tested Team approach - Cardiologists Anticoagulation Management Anatomy Assessment
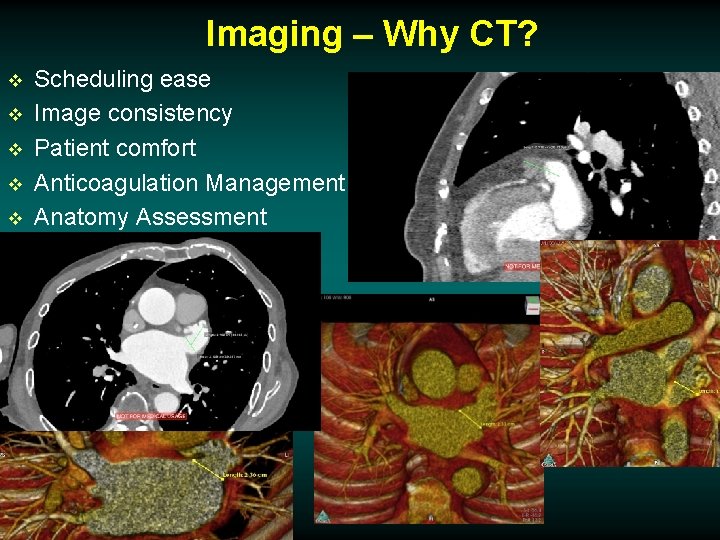
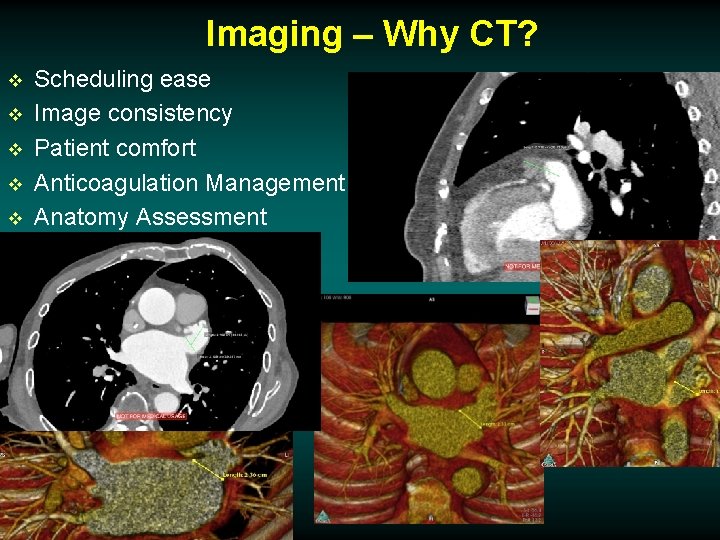
Imaging – Why CT? v v v Scheduling ease Image consistency Patient comfort Anticoagulation Management Anatomy Assessment
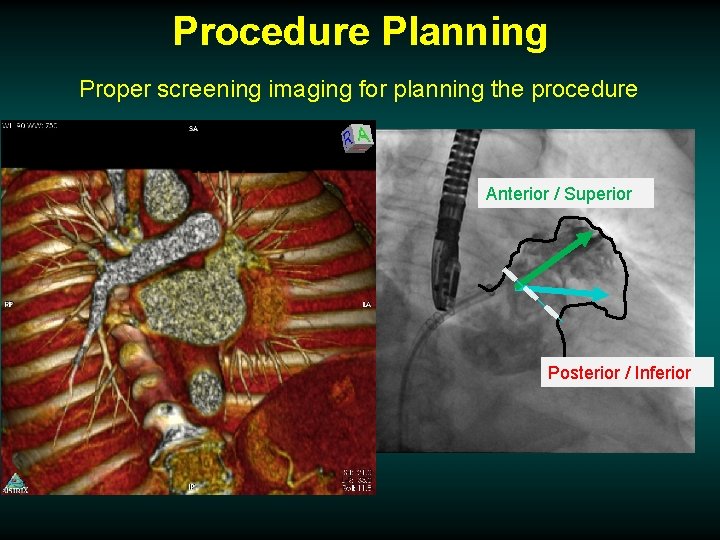
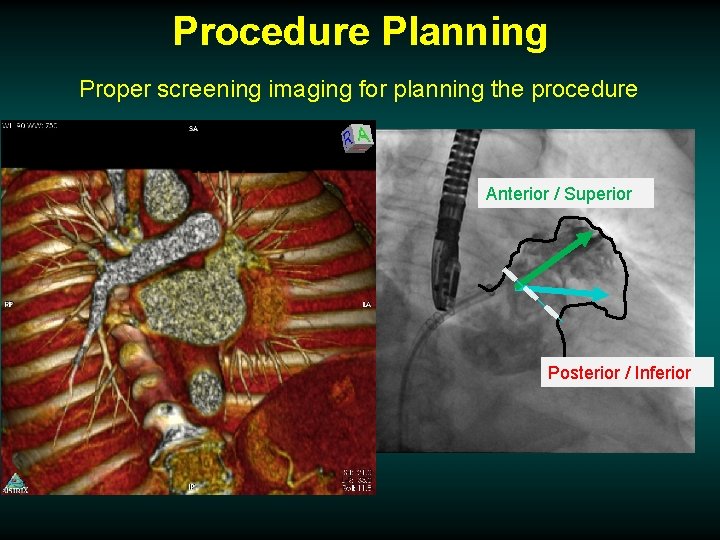
Procedure Planning Proper screening imaging for planning the procedure Anterior / Superior Posterior / Inferior
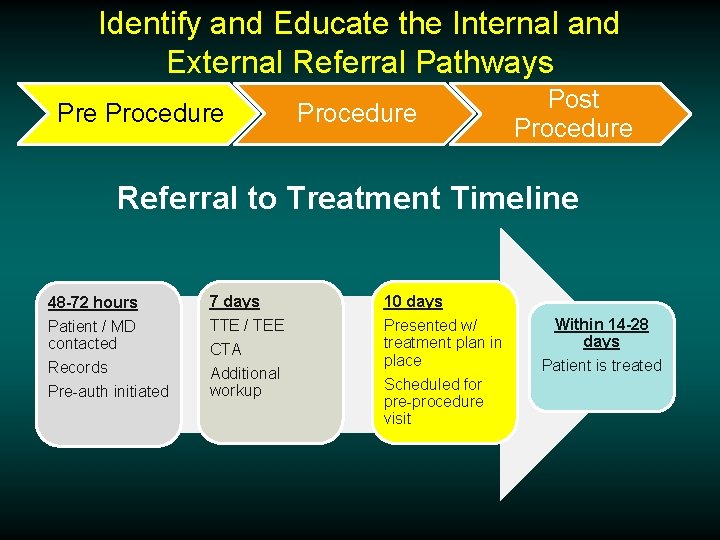
Identify and Educate the Internal and External Referral Pathways Pre Procedure Post Procedure Referral to Treatment Timeline 48 -72 hours 7 days 10 days Patient / MD contacted Records Pre-auth initiated TTE / TEE Presented w/ treatment plan in place Scheduled for pre-procedure visit CTA Additional workup Within 14 -28 days Patient is treated
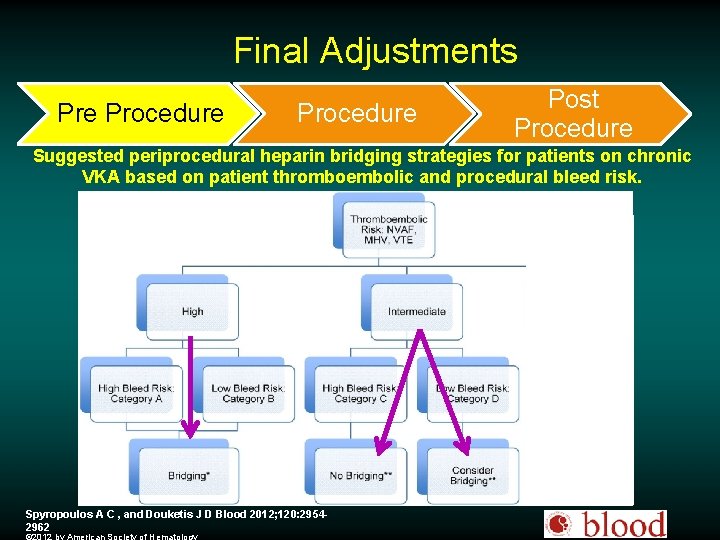
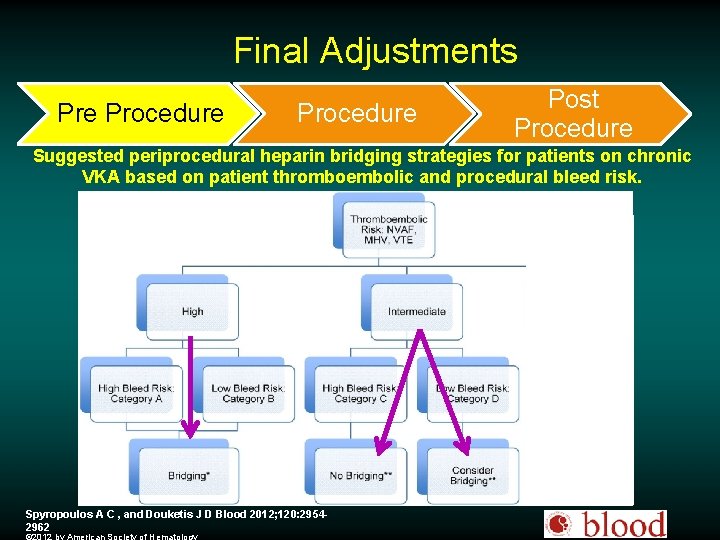
Final Adjustments Pre Procedure Post Procedure Suggested periprocedural heparin bridging strategies for patients on chronic VKA based on patient thromboembolic and procedural bleed risk. Spyropoulos A C , and Douketis J D Blood 2012; 120: 29542962
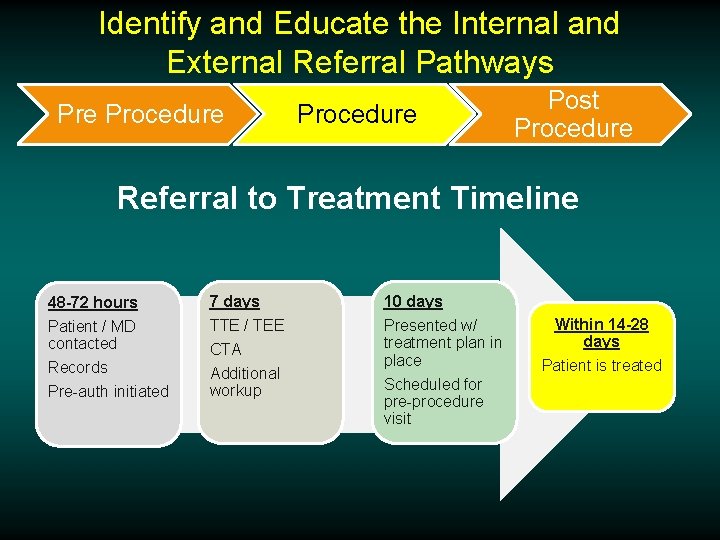
Identify and Educate the Internal and External Referral Pathways Pre Procedure Post Procedure Referral to Treatment Timeline 48 -72 hours 7 days 10 days Patient / MD contacted Records Pre-auth initiated TTE / TEE Presented w/ treatment plan in place Scheduled for pre-procedure visit CTA Additional workup Within 14 -28 days Patient is treated
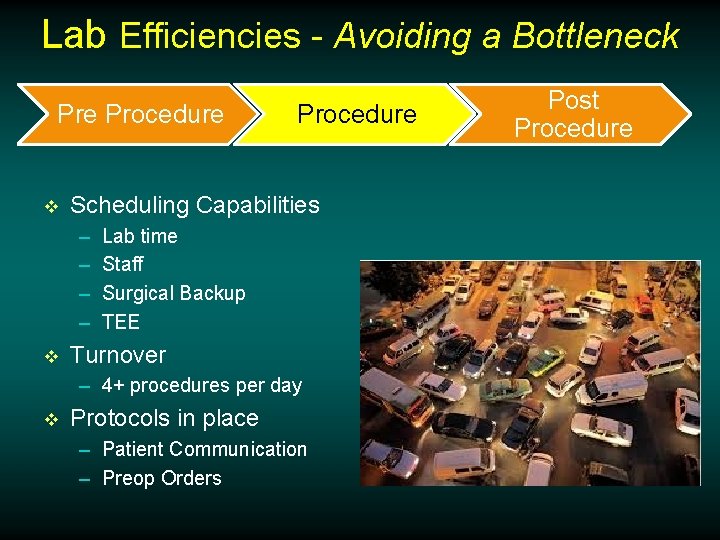
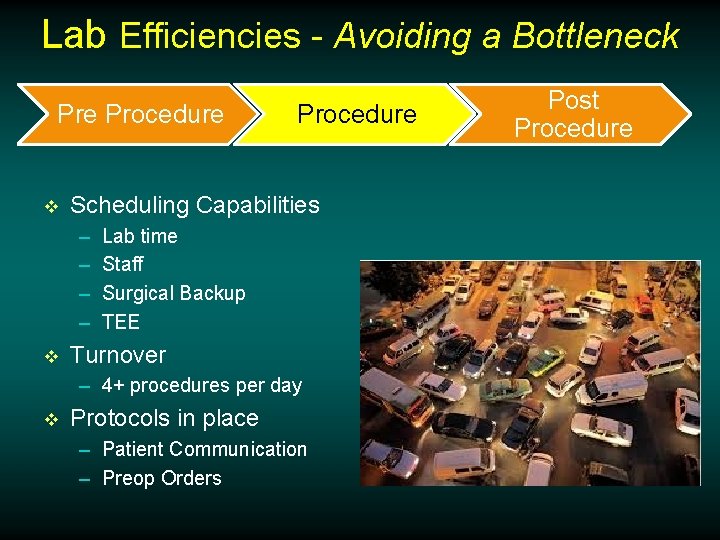
Lab Efficiencies - Avoiding a Bottleneck Pre Procedure v Scheduling Capabilities – – v Procedure Lab time Staff Surgical Backup TEE Turnover – 4+ procedures per day v Protocols in place – Patient Communication – Preop Orders Post Procedure

Post Procedure Care Procedure Post Procedure
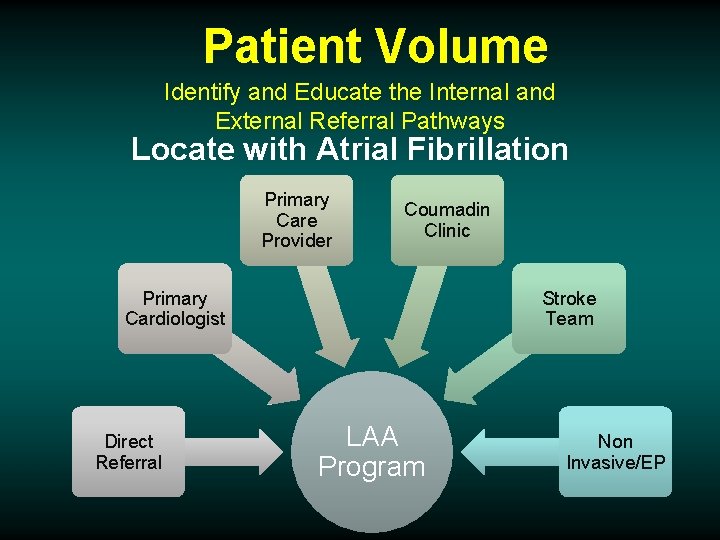
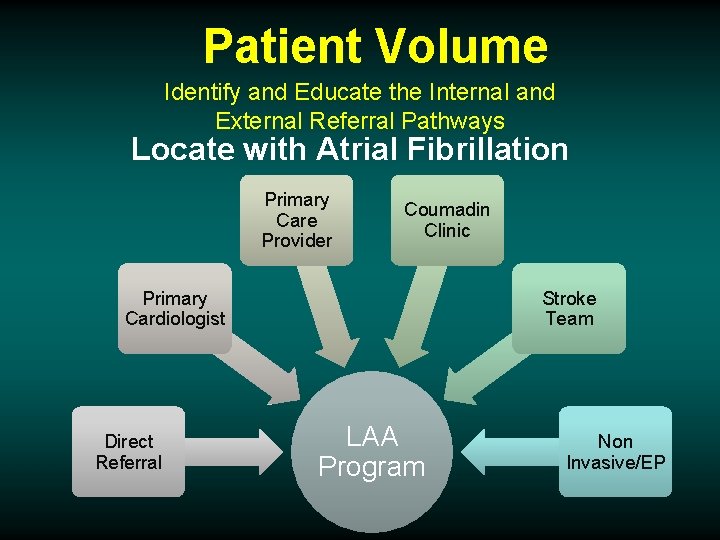
Patient Volume Identify and Educate the Internal and External Referral Pathways Locate with Atrial Fibrillation Primary Care Provider Coumadin Clinic Primary Cardiologist Direct Referral Stroke Team LAA Program Non Invasive/EP
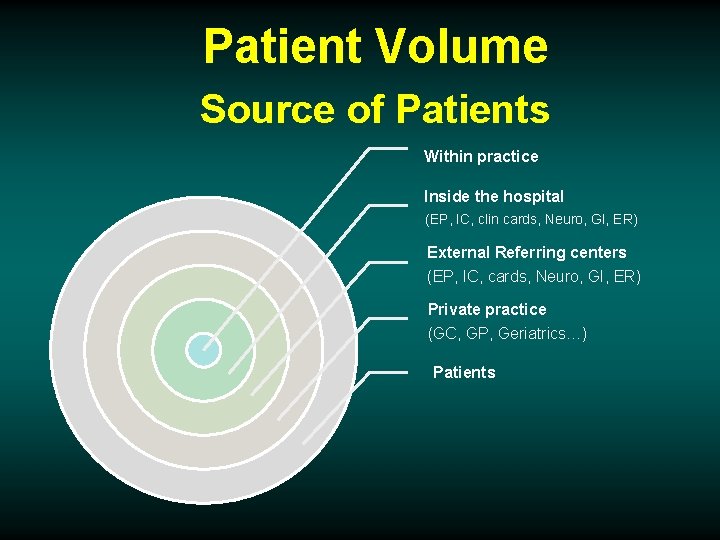
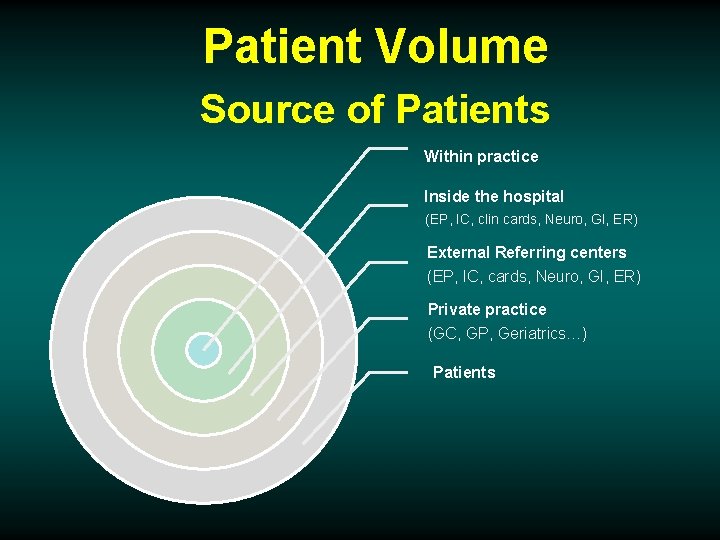
Patient Volume Source of Patients Within practice Inside the hospital (EP, IC, clin cards, Neuro, GI, ER) External Referring centers (EP, IC, cards, Neuro, GI, ER) Private practice (GC, GP, Geriatrics…) Patients
Patient Volume Hospital Marketing v v v v Hospital Press Release Template Product Messaging Guide Hospital Newsletter Template Product Images (. jpg files) Implant animation video Patient Testimonials Patient Education Brochure
A Simple Message For the Referring Community v. What is it? v. Does it work? v. Is it safe? v. Who is it for?
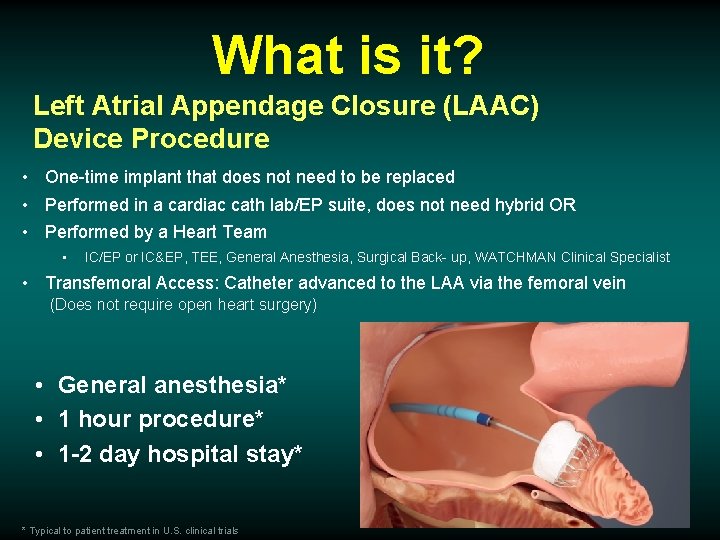
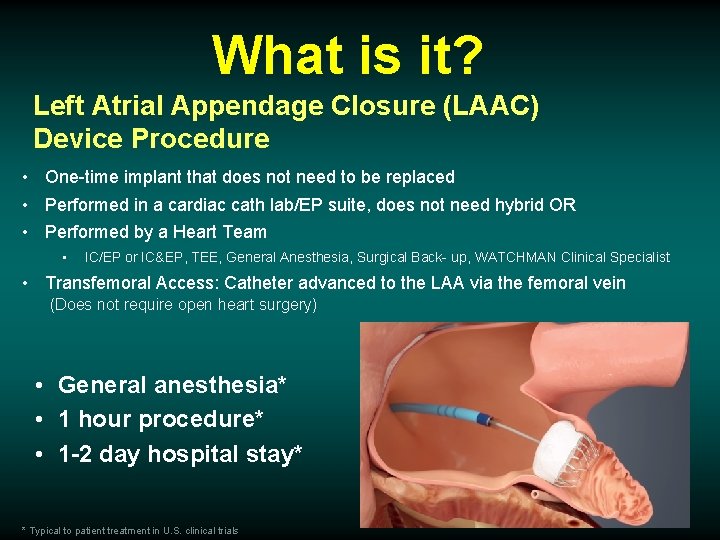
What is it? Left Atrial Appendage Closure (LAAC) Device Procedure • One-time implant that does not need to be replaced • Performed in a cardiac cath lab/EP suite, does not need hybrid OR • Performed by a Heart Team • IC/EP or IC&EP, TEE, General Anesthesia, Surgical Back- up, WATCHMAN Clinical Specialist • Transfemoral Access: Catheter advanced to the LAA via the femoral vein (Does not require open heart surgery) • General anesthesia* • 1 hour procedure* • 1 -2 day hospital stay* * Typical to patient treatment in U. S. clinical trials
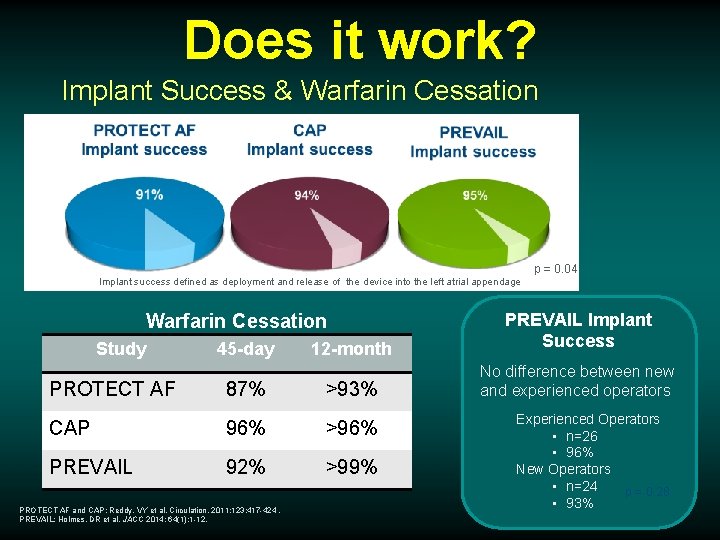
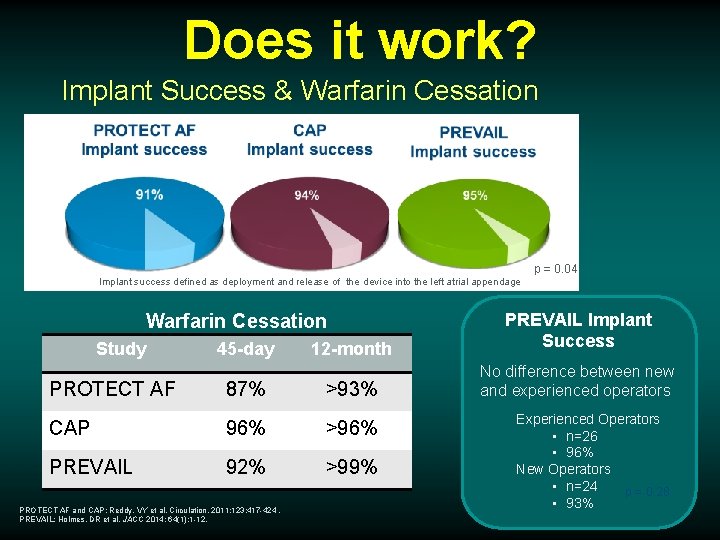
Does it work? Implant Success & Warfarin Cessation p = 0. 04 Implant success defined as deployment and release of the device into the left atrial appendage 12 -month PREVAIL Implant Success No difference between new and experienced operators Warfarin Cessation Study 45 -day PROTECT AF 87% >93% CAP 96% >96% PREVAIL 92% >99% PROTECT AF and CAP: Reddy, VY et al. Circulation. 2011; 123: 417 -424. PREVAIL: Holmes, DR et al. JACC 2014; 64(1): 1 -12. Experienced Operators • n=26 • 96% New Operators • n=24 p = 0. 28 • 93%
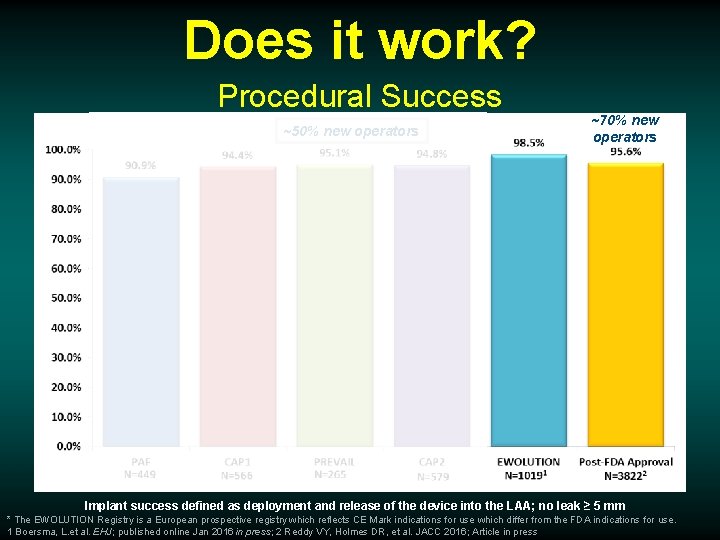
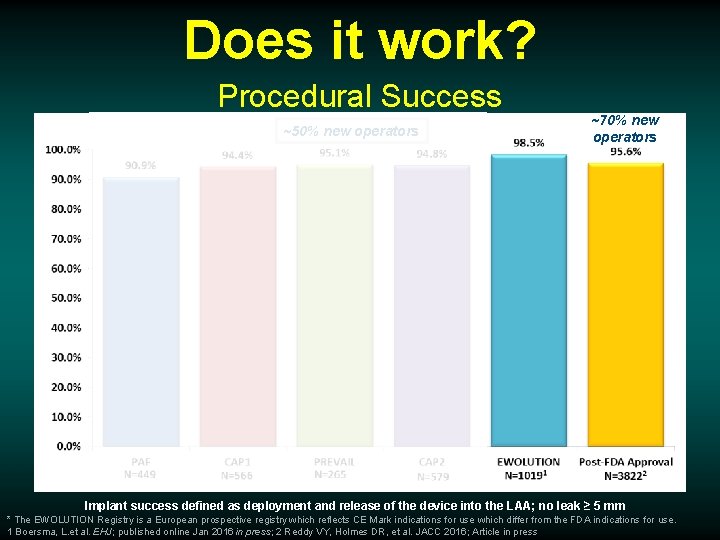
Does it work? Procedural Success ~50% new operators ~70% new operators Implant success defined as deployment and release of the device into the LAA; no leak ≥ 5 mm * The EWOLUTION Registry is a European prospective registry which reflects CE Mark indications for use which differ from the FDA indications for use. 1 Boersma, L. et al. EHJ; published online Jan 2016 in press; 2 Reddy VY, Holmes DR, et al. JACC 2016; Article in press
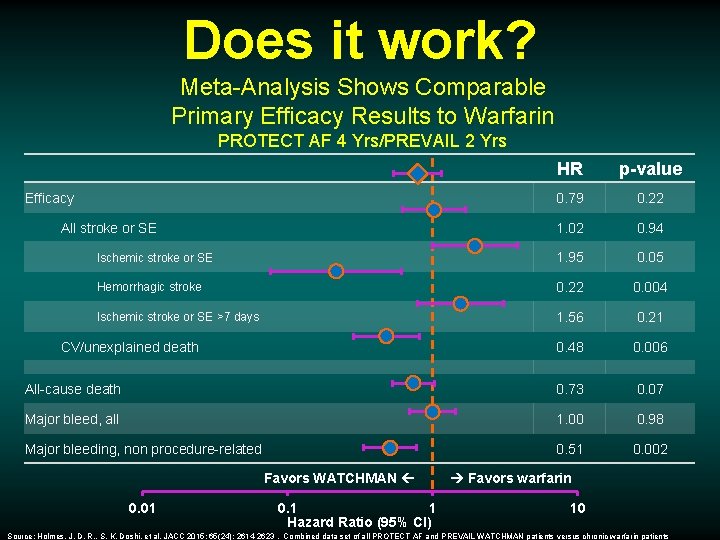
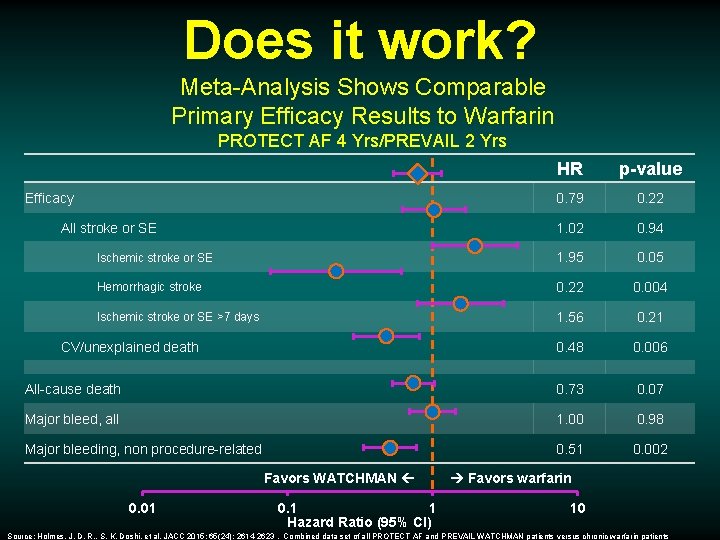
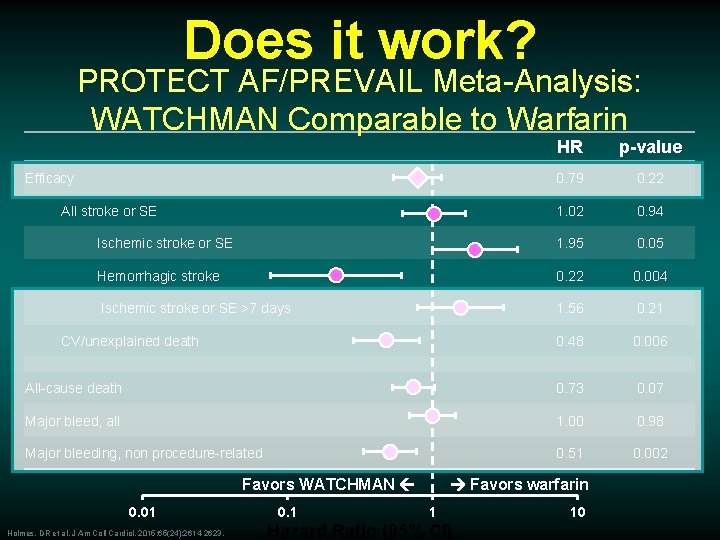
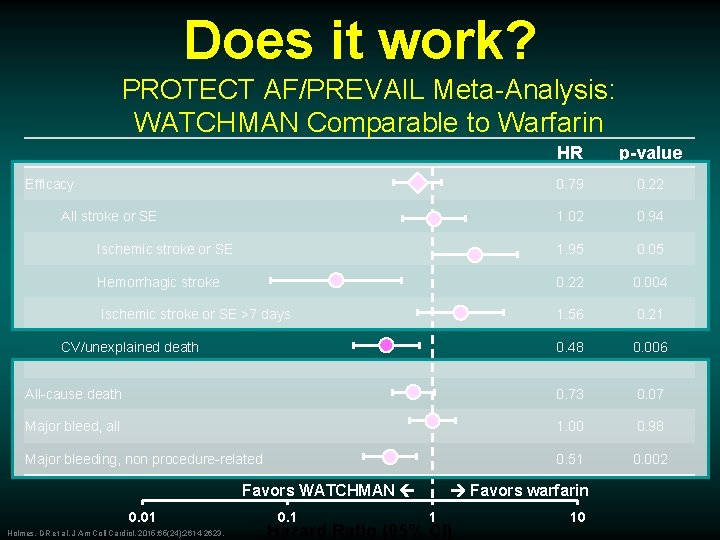
Does it work? Meta-Analysis Shows Comparable Primary Efficacy Results to Warfarin PROTECT AF 4 Yrs/PREVAIL 2 Yrs HR p-value 0. 79 0. 22 1. 02 0. 94 Ischemic stroke or SE 1. 95 0. 05 Hemorrhagic stroke 0. 22 0. 004 Ischemic stroke or SE >7 days 1. 56 0. 21 0. 48 0. 006 All-cause death 0. 73 0. 07 Major bleed, all 1. 00 0. 98 Major bleeding, non procedure-related 0. 51 0. 002 Efficacy All stroke or SE CV/unexplained death Favors WATCHMAN 0. 01 0. 1 1 Hazard Ratio (95% CI) Favors warfarin 10 Source: Holmes, J. D. R. , S. K. Doshi, et al. JACC 2015; 65(24): 2614 -2623. Combined data set of all PROTECT AF and PREVAIL WATCHMAN patients versus chronic warfarin patients
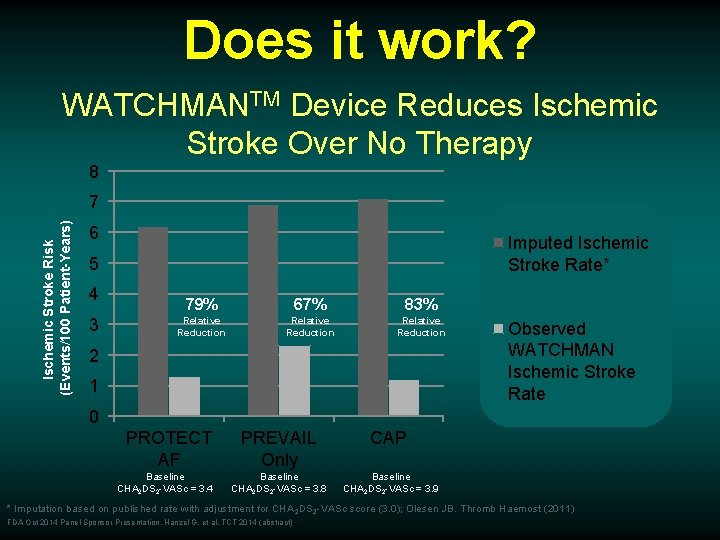
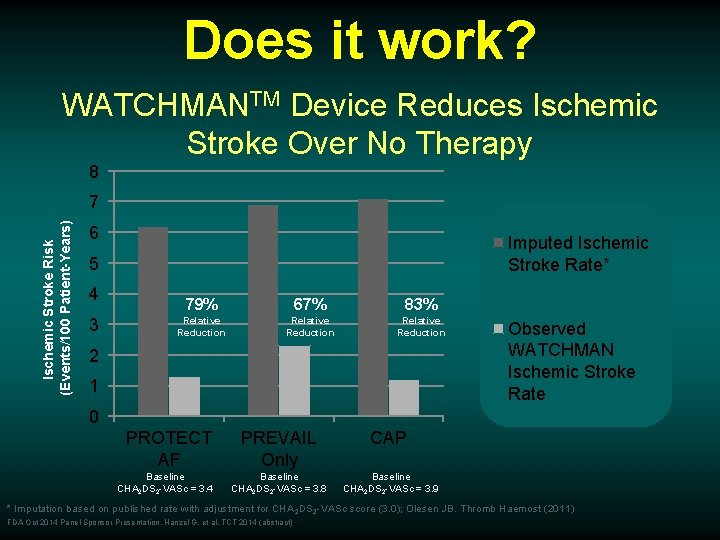
Does it work? WATCHMANTM Device Reduces Ischemic Stroke Over No Therapy 8 Ischemic Stroke Risk (Events/100 Patient-Years) 7 6 Imputed Ischemic Stroke Rate* 5 4 3 79% 67% 83% Relative Reduction 2 1 Observed WATCHMAN Ischemic Stroke Rate 0 PROTECT AF Baseline CHA 2 DS 2 -VASc = 3. 4 PREVAIL Only CAP Baseline CHA 2 DS 2 -VASc = 3. 8 Baseline CHA 2 DS 2 -VASc = 3. 9 * Imputation based on published rate with adjustment for CHA 2 DS 2 -VASc score (3. 0); Olesen JB. Thromb Haemost (2011) FDA Oct 2014 Panel Sponsor Presentation. Hanzel G, et al. TCT 2014 (abstract)
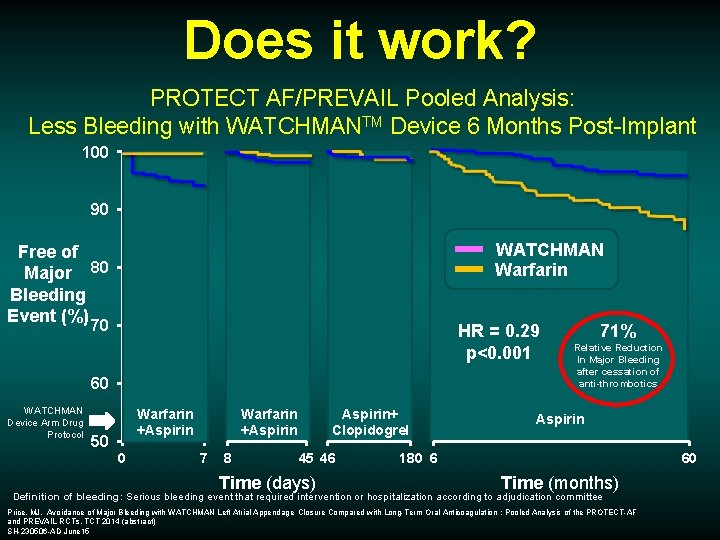
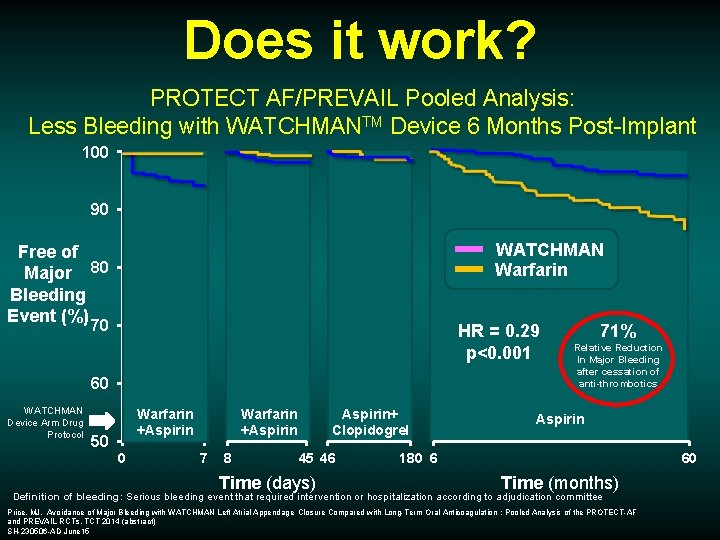
Does it work? PROTECT AF/PREVAIL Pooled Analysis: Less Bleeding with WATCHMANTM Device 6 Months Post-Implant 100 90 WATCHMAN Warfarin Free of Major 80 Bleeding Event (%) 70 HR = 0. 29 p<0. 001 60 WATCHMAN Device Arm Drug Protocol Warfarin +Aspirin 50 0 Warfarin +Aspirin 7 8 Aspirin+ Clopidogrel 45 46 Time (days) 71% Relative Reduction In Major Bleeding after cessation of anti-thrombotics Aspirin 180 6 60 Time (months) Definition of bleeding: Serious bleeding event that required intervention or hospitalization according to adjudication committee Price, MJ. Avoidance of Major Bleeding with WATCHMAN Left Atrial Appendage Closure Compared with Long-Term Oral Anticoagulation : Pooled Analysis of the PROTECT-AF and PREVAIL RCTs. TCT 2014 (abstract) SH-230506 -AD June 15
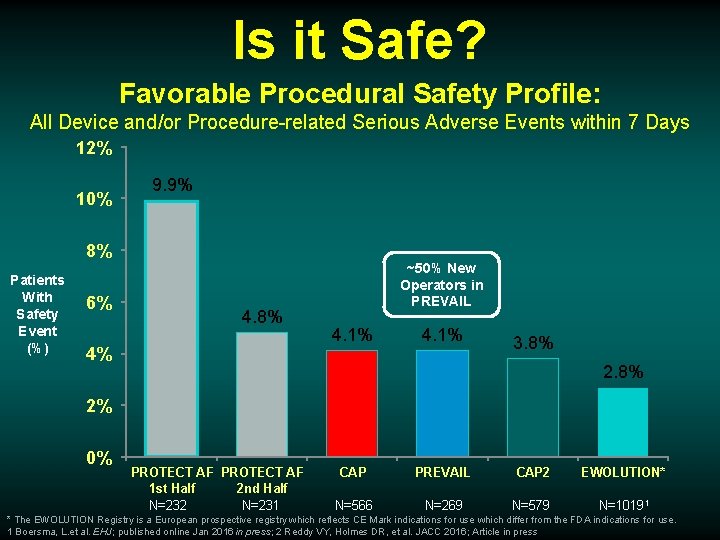
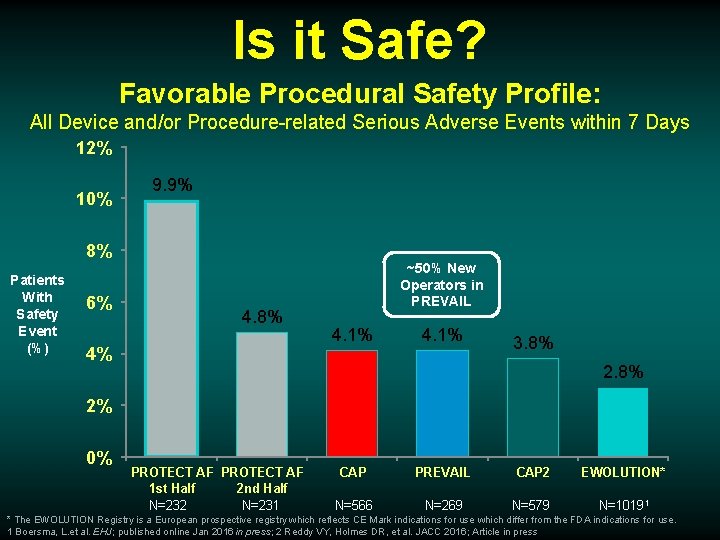
Is it Safe? Favorable Procedural Safety Profile: All Device and/or Procedure-related Serious Adverse Events within 7 Days 12% 10% 9. 9% 8% Patients With Safety Event (%) 6% 4. 8% 4% ~50% New Operators in PREVAIL 4. 1% 3. 8% 2% 0% PROTECT AF 1 st Half 2 nd Half N=232 N=231 CAP PREVAIL CAP 2 EWOLUTION* N=566 N=269 N=579 N=10191 * The EWOLUTION Registry is a European prospective registry which reflects CE Mark indications for use which differ from the FDA indications for use. 1 Boersma, L. et al. EHJ; published online Jan 2016 in press; 2 Reddy VY, Holmes DR, et al. JACC 2016; Article in press
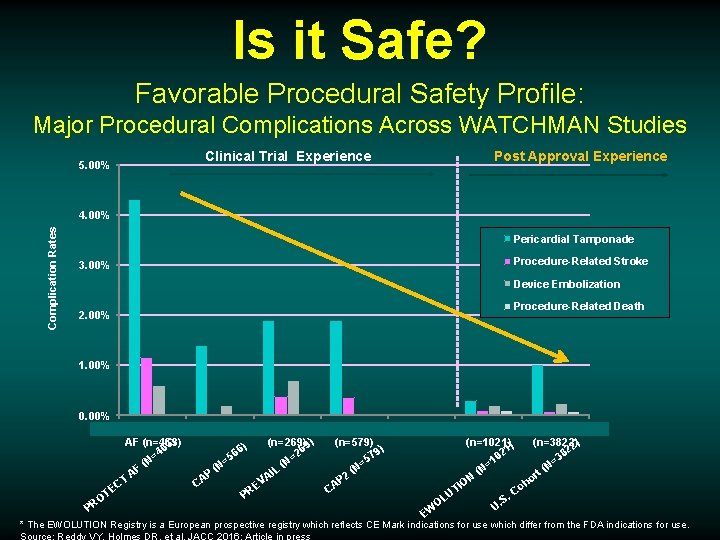
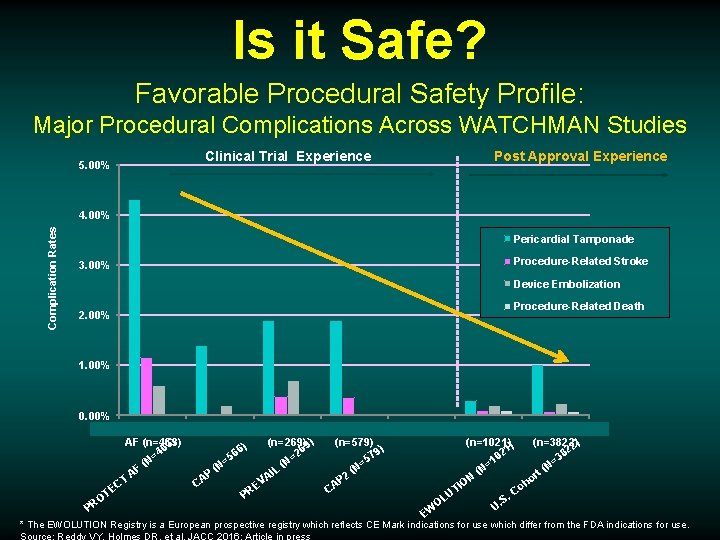
Is it Safe? Favorable Procedural Safety Profile: Major Procedural Complications Across WATCHMAN Studies 5. 00% Clinical Trial Experience Post Approval Experience Complication Rates 4. 00% Pericardial Tamponade Procedure-Related Stroke 3. 00% Device Embolization Procedure-Related Death 2. 00% 1. 00% 0. 00% PROTECT CAP (n=566) PREVAIL AF (n=463) (n=269) 9) 3) 6 6) 46 6 = =2 5 = N (N ( (N L AF P AI A T V C C E TE PR O PR CAP 2 (n=579) ) 79 5 = (N 2 P CA EWOLUTION US Cohort (n=1021) ) (n=3822)2) 2 21 0 38 1 = = (N (N rt N o O h TI Co U. S OL U. W E * The EWOLUTION Registry is a European prospective registry which reflects CE Mark indications for use which differ from the FDA indications for use. Source: Reddy VY, Holmes DR, et al. JACC 2016; Article in press
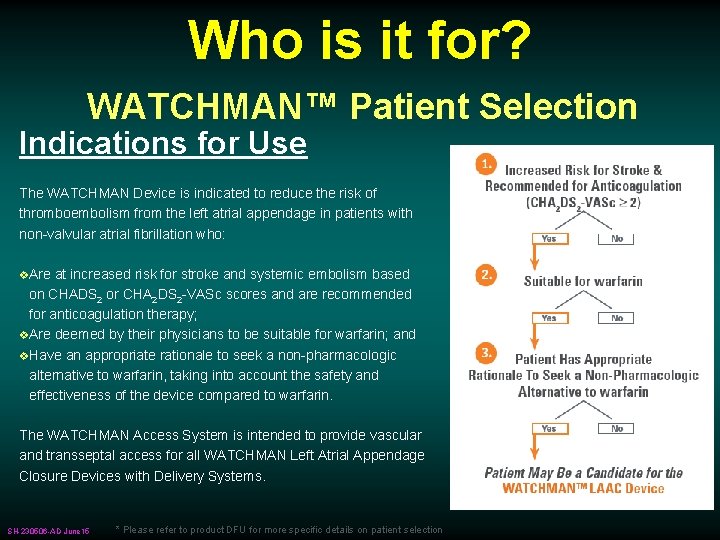
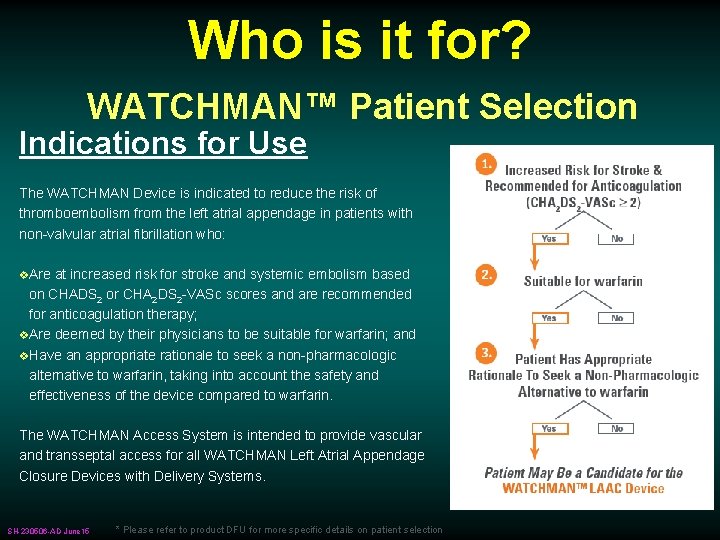
Who is it for? WATCHMAN™ Patient Selection Indications for Use The WATCHMAN Device is indicated to reduce the risk of thromboembolism from the left atrial appendage in patients with non-valvular atrial fibrillation who: v. Are at increased risk for stroke and systemic embolism based on CHADS 2 or CHA 2 DS 2 -VASc scores and are recommended for anticoagulation therapy; v. Are deemed by their physicians to be suitable for warfarin; and v. Have an appropriate rationale to seek a non-pharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device compared to warfarin. The WATCHMAN Access System is intended to provide vascular and transseptal access for all WATCHMAN Left Atrial Appendage Closure Devices with Delivery Systems. SH-230506 -AD June 15 * Please refer to product DFU for more specific details on patient selection
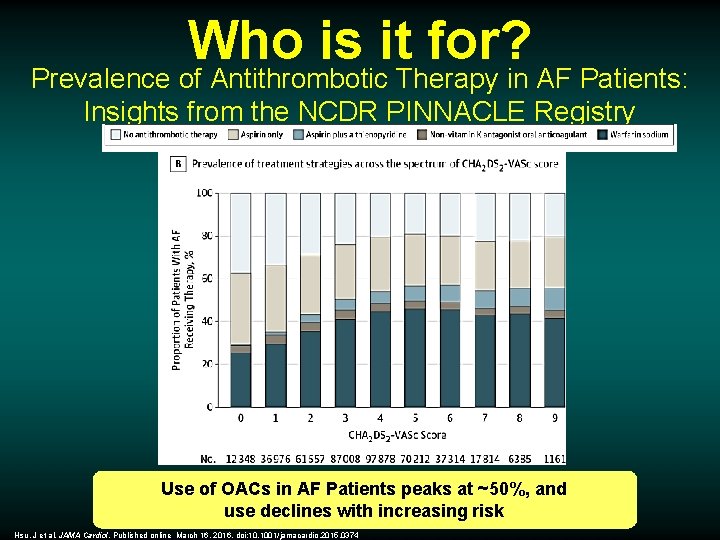
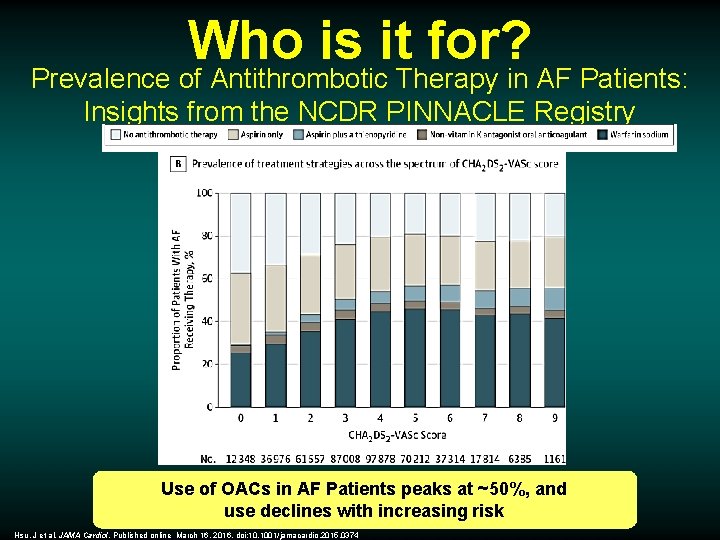
Who is it for? Prevalence of Antithrombotic Therapy in AF Patients: Insights from the NCDR PINNACLE Registry Use of OACs in AF Patients peaks at ~50%, and use declines with increasing risk Hsu, J et al. JAMA Cardiol. Published online March 16, 2016. doi: 10. 1001/jamacardio. 2015. 0374
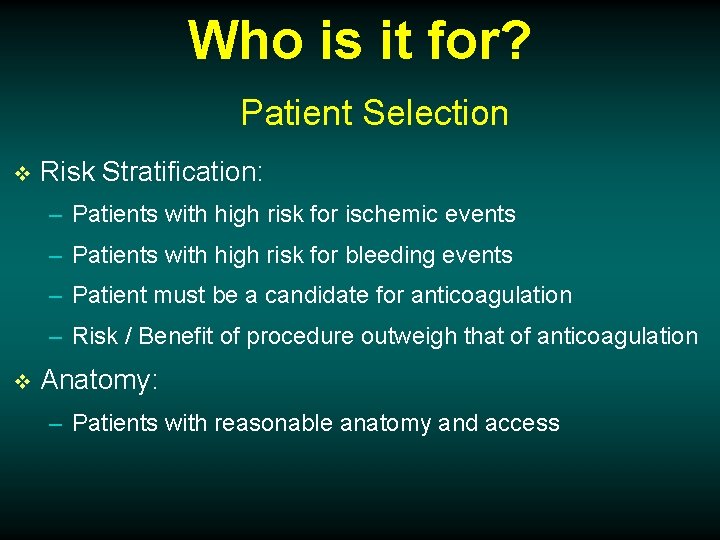
Who is it for? Patient Selection v Risk Stratification: – Patients with high risk for ischemic events – Patients with high risk for bleeding events – Patient must be a candidate for anticoagulation – Risk / Benefit of procedure outweigh that of anticoagulation v Anatomy: – Patients with reasonable anatomy and access
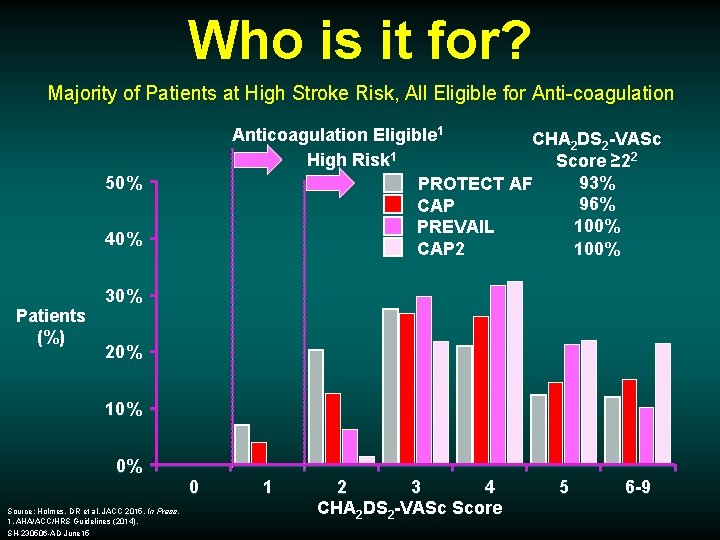
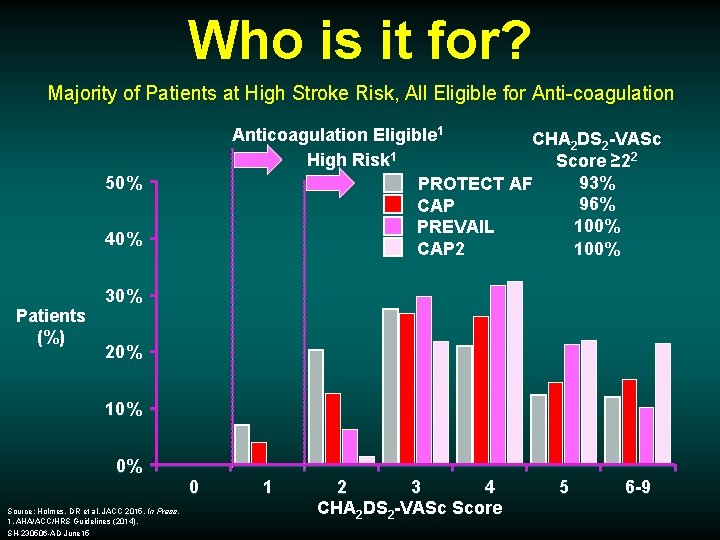
Who is it for? Majority of Patients at High Stroke Risk, All Eligible for Anti-coagulation Anticoagulation Eligible 1 CHA 2 DS 2 -VASc High Risk 1 Score ≥ 22 93% PROTECT AF 96% CAP 100% PREVAIL 100% CAP 2 50% 40% Patients (%) 30% 20% 10% 0% 0 Source: Holmes, DR et al. JACC 2015. In Press. 1. AHA/ACC/HRS Guidelines (2014). SH-230506 -AD June 15 1 2 3 4 CHA 2 DS 2 -VASc Score 5 6 -9
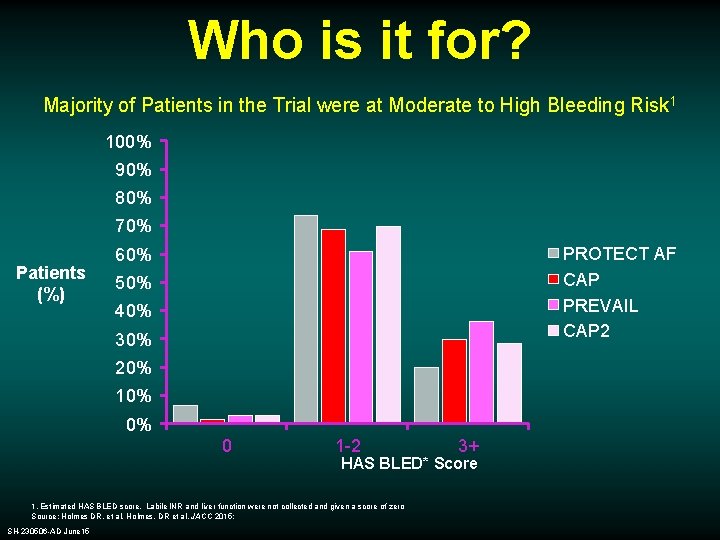
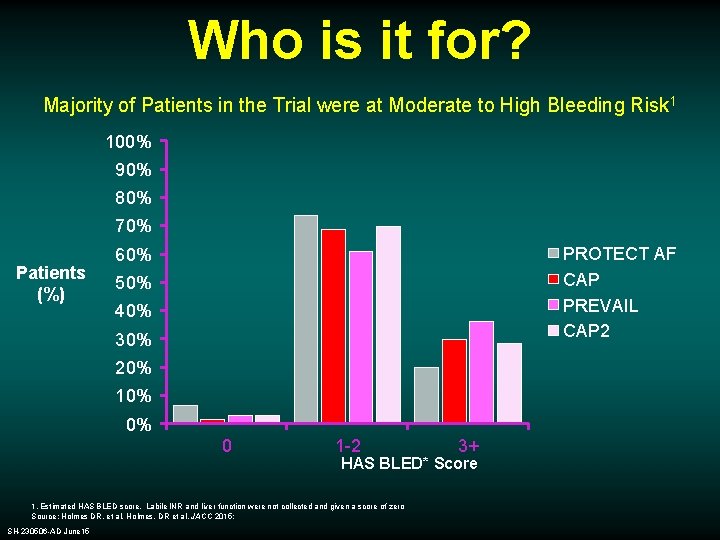
Who is it for? Majority of Patients in the Trial were at Moderate to High Bleeding Risk 1 100% 90% 80% 70% Patients (%) PROTECT AF CAP PREVAIL CAP 2 60% 50% 40% 30% 20% 10% 0% 0 1 -2 HAS BLED* Score 1. Estimated HAS BLED score. Labile INR and liver function were not collected and given a score of zero Source: Holmes DR, et al. Holmes, DR et al. JACC 2015; SH-230506 -AD June 15 3+
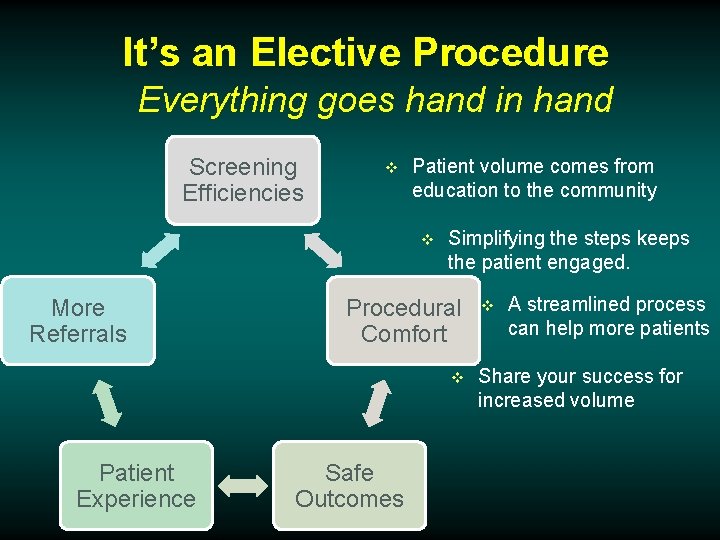
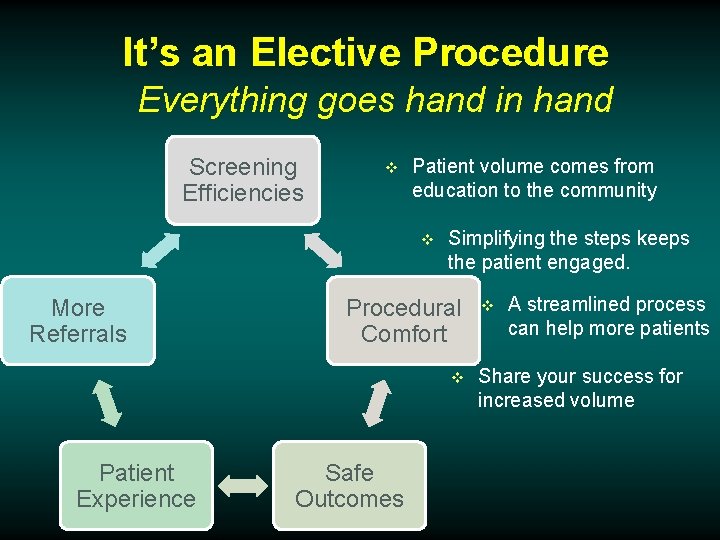
It’s an Elective Procedure Everything goes hand in hand Screening Efficiencies v Patient volume comes from education to the community v More Referrals Simplifying the steps keeps the patient engaged. Procedural Comfort v Patient Experience Safe Outcomes v A streamlined process can help more patients Share your success for increased volume
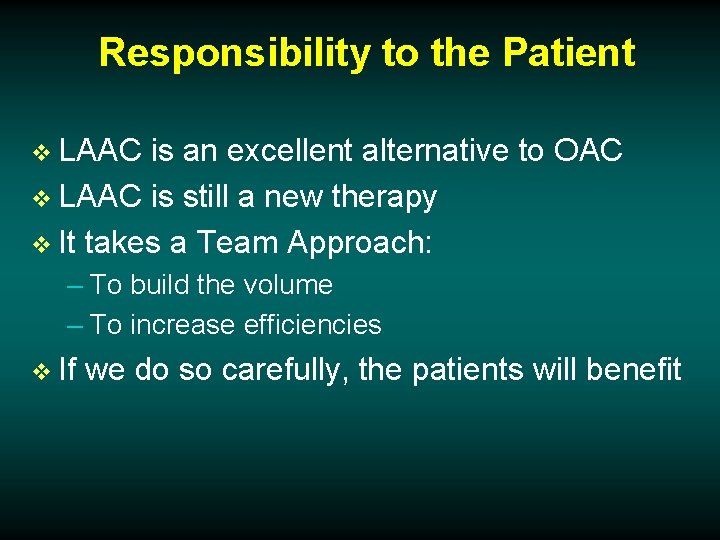
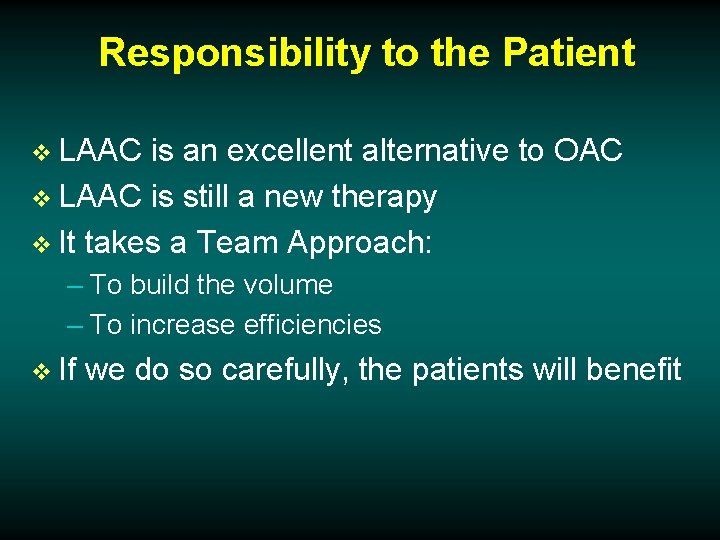
Responsibility to the Patient v LAAC is an excellent alternative to OAC v LAAC is still a new therapy v It takes a Team Approach: – To build the volume – To increase efficiencies v If we do so carefully, the patients will benefit


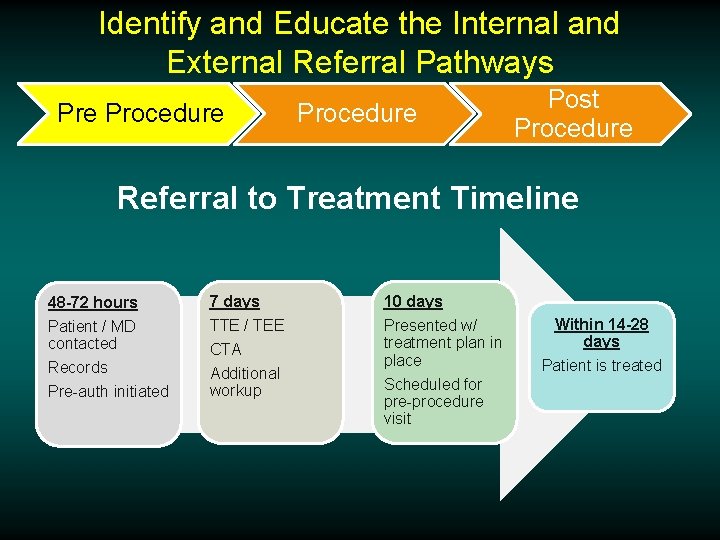
Identify and Educate the Internal and External Referral Pathways Pre Procedure Post Procedure Referral to Treatment Timeline 48 -72 hours 7 days 10 days Patient / MD contacted Records Pre-auth initiated TTE / TEE Presented w/ treatment plan in place Scheduled for pre-procedure visit CTA Additional workup Within 14 -28 days Patient is treated
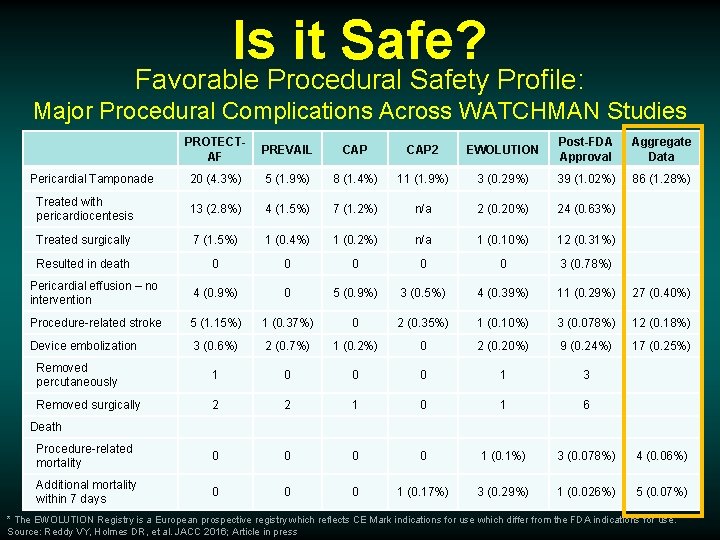
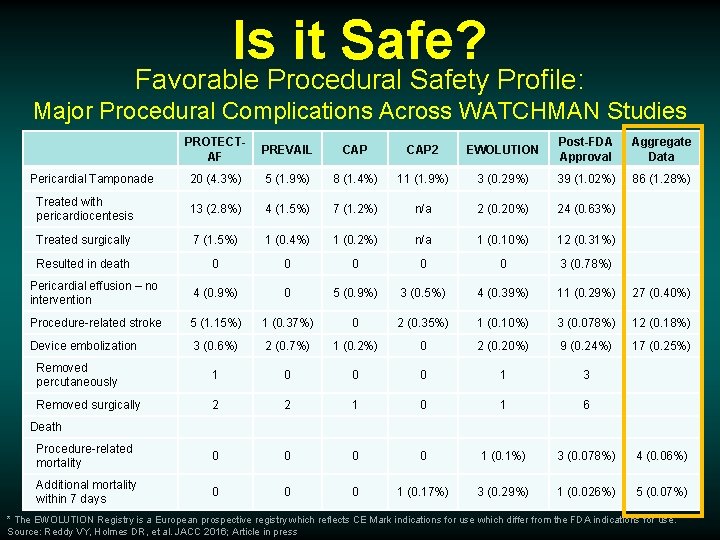
Is it Safe? Favorable Procedural Safety Profile: Major Procedural Complications Across WATCHMAN Studies PROTECTAF PREVAIL CAP 2 EWOLUTION Post-FDA Approval Aggregate Data 20 (4. 3%) 5 (1. 9%) 8 (1. 4%) 11 (1. 9%) 3 (0. 29%) 39 (1. 02%) 86 (1. 28%) Treated with pericardiocentesis 13 (2. 8%) 4 (1. 5%) 7 (1. 2%) n/a 2 (0. 20%) 24 (0. 63%) Treated surgically 7 (1. 5%) 1 (0. 4%) 1 (0. 2%) n/a 1 (0. 10%) 12 (0. 31%) Resulted in death 0 0 0 3 (0. 78%) Pericardial effusion – no intervention 4 (0. 9%) 0 5 (0. 9%) 3 (0. 5%) 4 (0. 39%) 11 (0. 29%) 27 (0. 40%) Procedure-related stroke 5 (1. 15%) 1 (0. 37%) 0 2 (0. 35%) 1 (0. 10%) 3 (0. 078%) 12 (0. 18%) Device embolization 3 (0. 6%) 2 (0. 7%) 1 (0. 2%) 0 2 (0. 20%) 9 (0. 24%) 17 (0. 25%) Removed percutaneously 1 0 0 0 1 3 Removed surgically 2 2 1 0 1 6 Procedure-related mortality 0 0 1 (0. 1%) 3 (0. 078%) 4 (0. 06%) Additional mortality within 7 days 0 0 0 1 (0. 17%) 3 (0. 29%) 1 (0. 026%) 5 (0. 07%) Pericardial Tamponade Death * The EWOLUTION Registry is a European prospective registry which reflects CE Mark indications for use which differ from the FDA indications for use. Source: Reddy VY, Holmes DR, et al. JACC 2016; Article in press
Pre Procedure Post Procedure
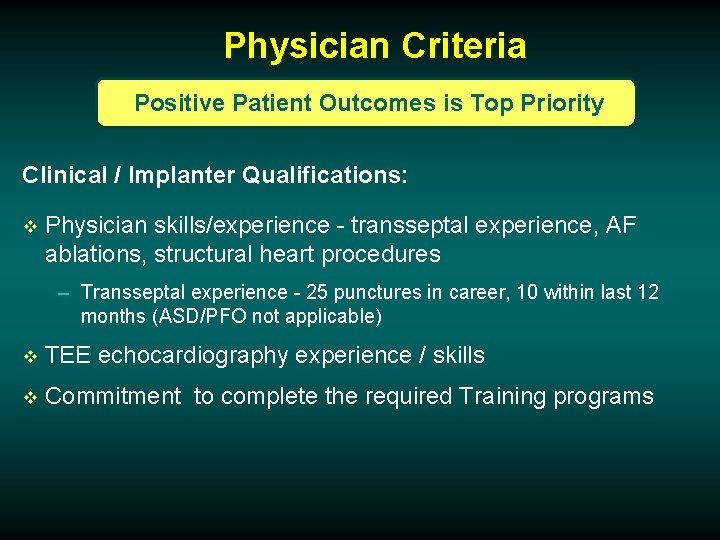
Physician Criteria Positive Patient Outcomes is Top Priority Clinical / Implanter Qualifications: v Physician skills/experience - transseptal experience, AF ablations, structural heart procedures – Transseptal experience - 25 punctures in career, 10 within last 12 months (ASD/PFO not applicable) v TEE echocardiography experience / skills v Commitment to complete the required Training programs
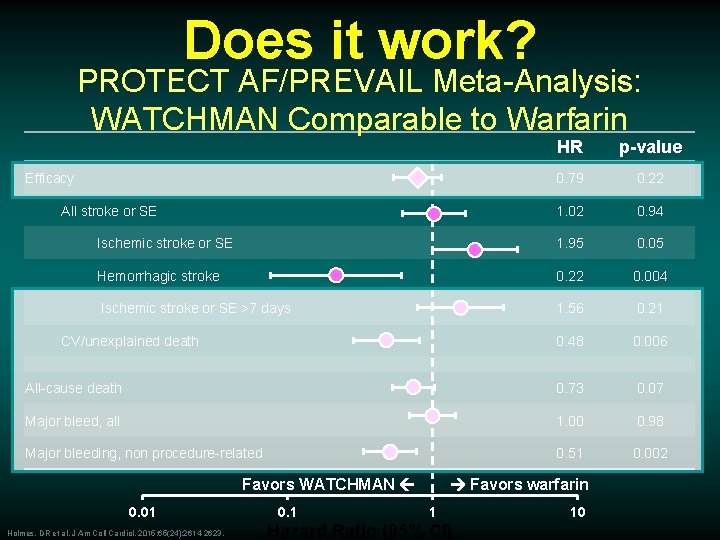
Does it work? PROTECT AF/PREVAIL Meta-Analysis: WATCHMAN Comparable to Warfarin HR p-value 0. 79 0. 22 1. 02 0. 94 Ischemic stroke or SE 1. 95 0. 05 Hemorrhagic stroke 0. 22 0. 004 Ischemic stroke or SE >7 days 1. 56 0. 21 0. 48 0. 006 All-cause death 0. 73 0. 07 Major bleed, all 1. 00 0. 98 Major bleeding, non procedure-related 0. 51 0. 002 Efficacy All stroke or SE CV/unexplained death Favors WATCHMAN 0. 01 Holmes, DR et al. J Am Coll Cardiol. 2015; 65(24): 2614 -2623. 0. 1 Favors warfarin 1 Hazard Ratio (95% CI) 10
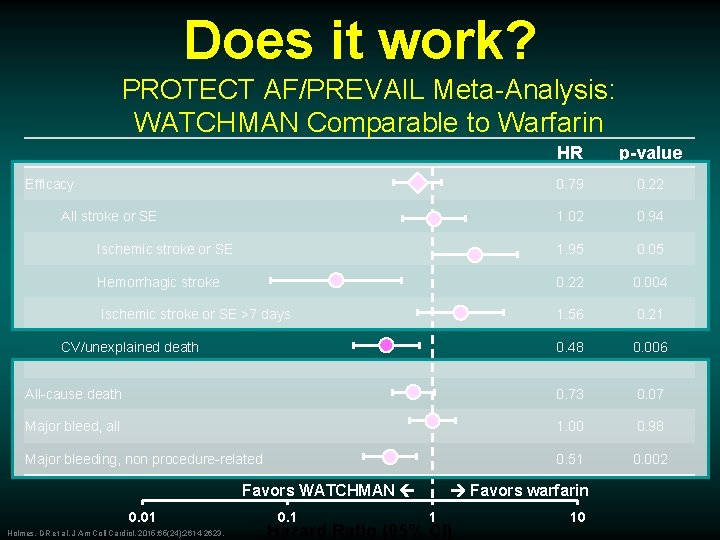
Does it work? PROTECT AF/PREVAIL Meta-Analysis: WATCHMAN Comparable to Warfarin HR p-value 0. 79 0. 22 1. 02 0. 94 Ischemic stroke or SE 1. 95 0. 05 Hemorrhagic stroke 0. 22 0. 004 Ischemic stroke or SE >7 days 1. 56 0. 21 0. 48 0. 006 All-cause death 0. 73 0. 07 Major bleed, all 1. 00 0. 98 Major bleeding, non procedure-related 0. 51 0. 002 Efficacy All stroke or SE CV/unexplained death Favors WATCHMAN 0. 01 Holmes, DR et al. J Am Coll Cardiol. 2015; 65(24): 2614 -2623. 0. 1 Favors warfarin 1 Hazard Ratio (95% CI) 10
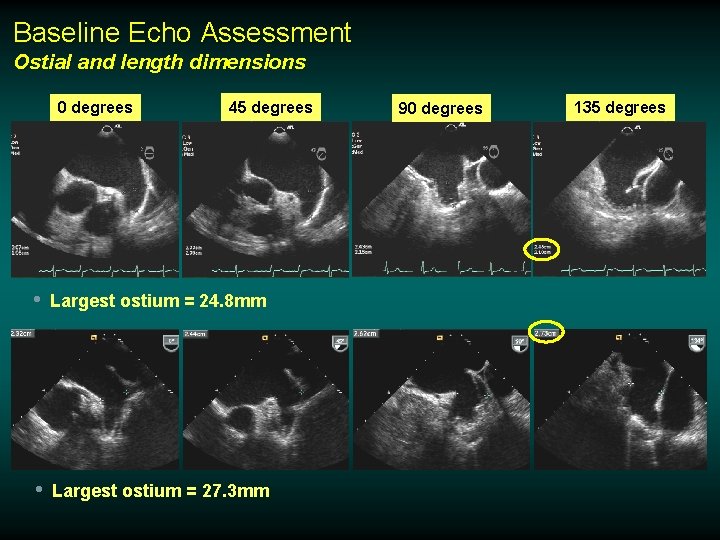
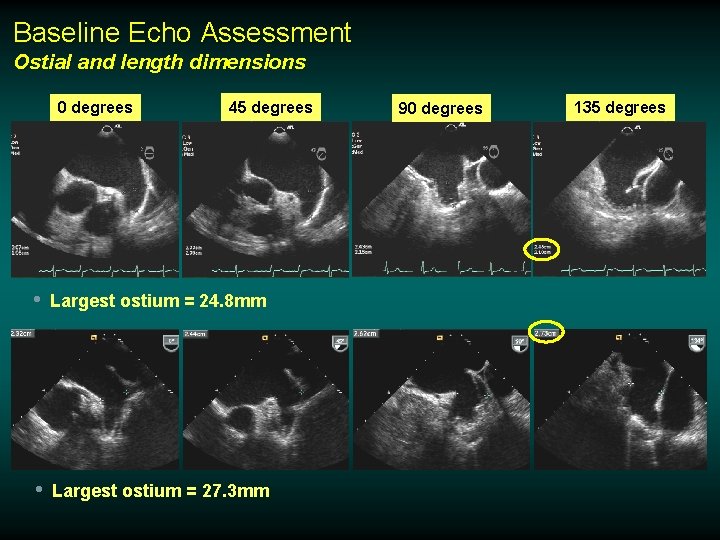
Baseline Echo Assessment Ostial and length dimensions 0 degrees 45 degrees • Largest ostium = 24. 8 mm • Largest ostium = 27. 3 mm 90 degrees 135 degrees