ONCOLOGICAL DISORDERS TREATMENT MODALITIES PYRAMID POINTS Assessment of
- Slides: 48
ONCOLOGICAL DISORDERS TREATMENT MODALITIES
PYRAMID POINTS • Assessment of the client for pain • Interventions for the client in pain • Handling hazardous and infectious materials related to radiation or chemotherapy • Care of the client receiving external or internal radiation or chemotherapy • Monitoring for expected and unexpected effects of radiation and chemotherapy
PYRAMID POINTS • Interventions if an anaphylactic reaction occurs from the administration of chemotherapy • Safety related to caring for a client with an internal radiation implant • Interventions in the event of a dislodged radiation source • Monitoring for complications associated with bone marrow transplantation
PAIN CONTROL • CAUSES OF PAIN – Bone destruction – Obstruction of an organ – Compression of peripheral nerves – Infiltration or distention of tissue – Inflammation or necrosis – Psychological, such as fear or anxiety
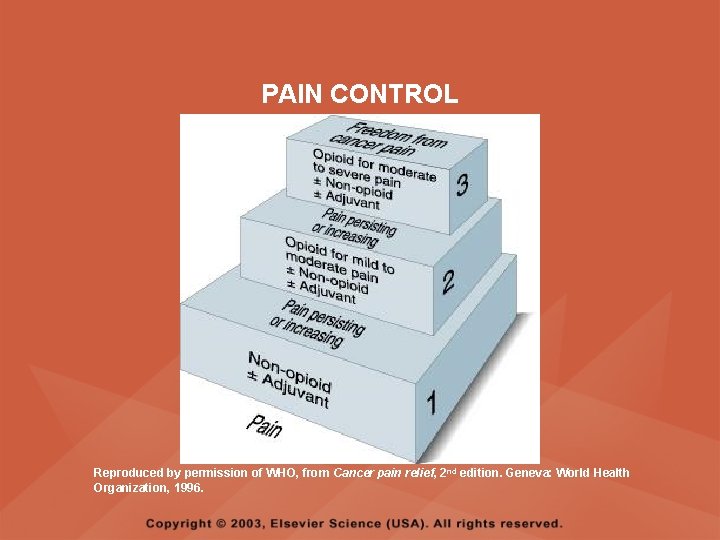
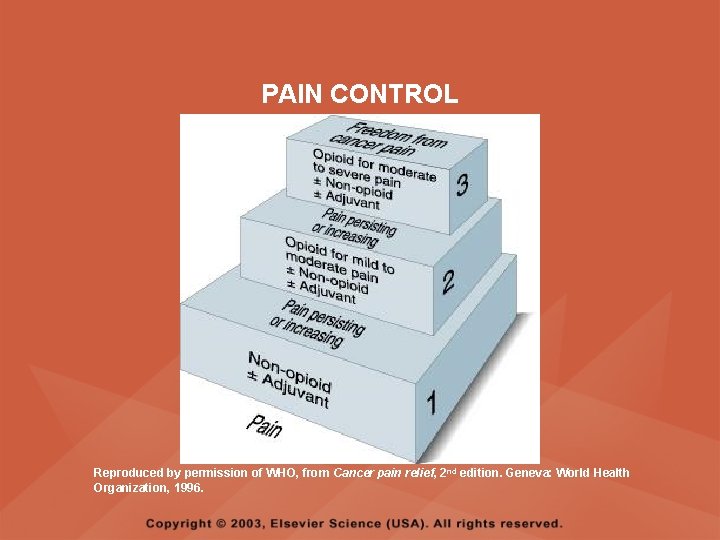
PAIN CONTROL Reproduced by permission of WHO, from Cancer pain relief, 2 nd edition. Geneva: World Health Organization, 1996.
PAIN CONTROL • IMPLEMENTATION – Collaborate with other members of the health care team to develop a pain management program – Administer oral preparations if possible and if they provide adequate relief of pain – Mild and moderate pain may be treated with salicylates, acetaminophen (Tylenol), and nonsteroidal antiinflammatory drugs (NSAIDs)
PAIN CONTROL • IMPLEMENTATION – Severe pain is treated with narcotics such as codeine sulfate, meperidine (Demerol), morphine sulfate, and hydromorphone hydrochloride (Dilaudid) – Subcutaneous injections and continuous IV infusions of narcotics provide superior pain control
PAIN CONTROL • IMPLEMENTATION – Monitor for side effects of medications – Monitor for effectiveness of medications – Provide nonpharmacological techniques of pain control, such as relaxation, guided imagery, biofeedback, and diversion – Do not undermedicate the cancer client who is in pain
SURGERY • DESCRIPTION – Used to diagnose, stage, and treat cancer • TYPES – Prophylactic surgery – Curative surgery – Control (cytoreductive) surgery – Palliative surgery – Reconstructive or rehabilitative surgery
PROPHYLACTIC SURGERY • Performed in clients with an existing premalignant condition or a known family history that strongly predisposes the person to the development of cancer • An attempt is made to remove the tissue or organ at risk and thus prevent the development of cancer
CURATIVE SURGERY • All gross and microscopic tumor is either removed or destroyed
CONTROL (CYTOREDUCTIVE) SURGERY • A “debulking” procedure that consists of removing part of the tumor • It decreases the number of cancer cells and increases the chance that otherapies will be successful
PALLIATIVE SURGERY • Performed to improve quality of life during the survival time • Performed to reduce pain, relieve airway obstruction, relieve obstructions in the gastrointestinal (GI) and urinary tract, relieve pressure on the brain and spinal cord, prevent hemorrhage, remove infected and ulcerated tumors, and drain abscesses
RECONSTRUCTIVE OR REHABILITATIVE SURGERY • Performed to improve quality of life by restoring maximal function and appearance
SIDE EFFECTS OF SURGERY • • Loss or loss of function of a specific body part Reduced function as a result of organ loss Scarring or disfigurement Grieving about altered body image or imposed change in lifestyle
CHEMOTHERAPY • DESCRIPTION – Kills or inhibits the reproduction of neoplastic cells – The effects are systemic and affect both healthy cells and cancerous cells – Normal cells most profoundly affected include the skin, hair, lining of the GI tract, spermatocytes, and hematopoietic cells
CHEMOTHERAPY • DESCRIPTION – Cell cycle phase-specific medications affect cells only during a certain phase of the reproductive cycle and cell cycle phasenonspecific medications affect cells in any phase of the reproductive cycle – Usually several medications are used in combination (combination therapy) to increase therapeutic response
CHEMOTHERAPY • DESCRIPTION – Combination chemotherapy is planned to avoid prescribing medications with nadirs (the time during which bone marrow activity and white blood cell counts are at their lowest) at or near the same time, to minimize immunosuppression – Antineoplastic therapy may be combined with other treatments such as surgery and radiation
CHEMOTHERAPY • DESCRIPTION – The preferred route of administration is by IV – Side effects include alopecia, nausea and vomiting, mucositis, skin changes, immunosuppression, anemia, and thrombocytopenia – Refer to the Module entitled Antineoplastic Medications for additional information related to chemotherapy
RADIATION THERAPY • DESCRIPTION – Destroys cancer cells with minimal exposure of normal cells to the damaging effects of radiation; the cells damaged either die or become unable to divide – Effective on tissues directly within the path of the radiation beam
RADIATION THERAPY • DESCRIPTION – Side effects include skin changes and irritation, alopecia, fatigue, and altered taste sensation; also, the effects vary according to the site of treatment – Teletherapy and brachytherapy are the most commonly used types of radiation therapy to treat cancer
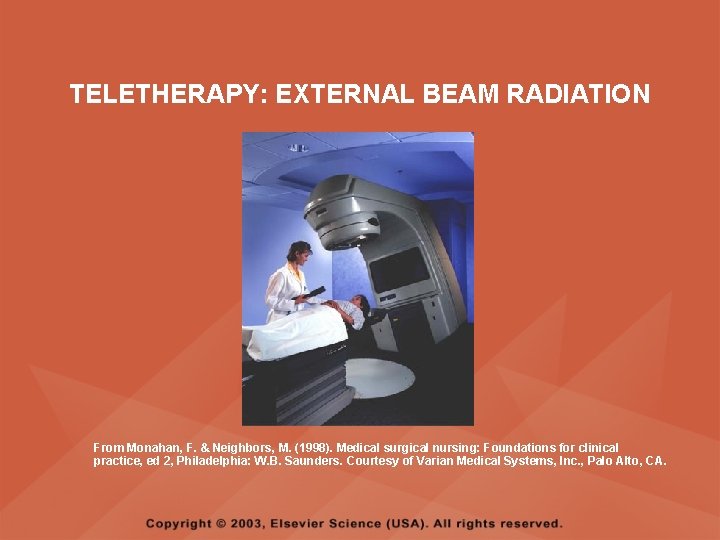
TELETHERAPY • DESCRIPTION – Also called beam radiation and the actual radiation source is external to the client – The client does not emit radiation and does not pose a hazard to anyone else
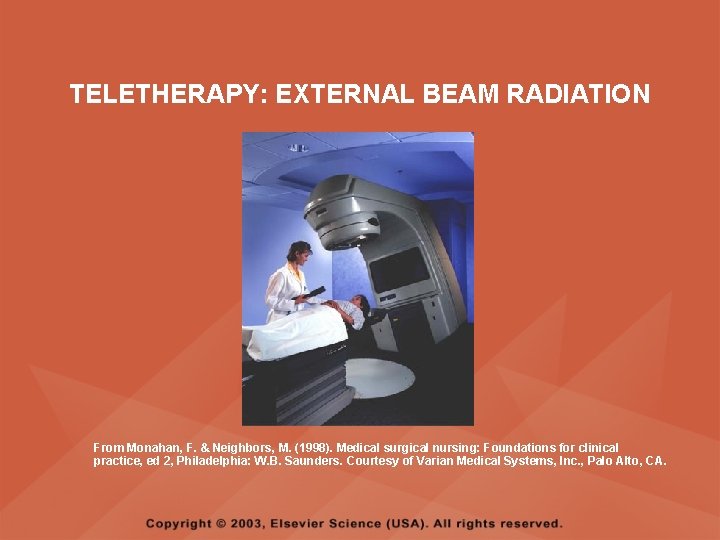
TELETHERAPY: EXTERNAL BEAM RADIATION From Monahan, F. & Neighbors, M. (1998). Medical surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders. Courtesy of Varian Medical Systems, Inc. , Palo Alto, CA.
TELETHERAPY: CLIENT EDUCATION • Wash area with water or mild soap and water using the hand rather than a washcloth; rinse the soap thoroughly, and pat dry using a soft towel or cloth • Do not remove the radiation markings from the skin • Use no powders, ointments, lotions, or creams on the area unless prescribed
TELETHERAPY: CLIENT EDUCATION • Wear soft clothing over the area avoiding belts, buckles, straps, or any clothing that binds or rubs the skin • Avoid sun and heat exposure • Monitor for moist desquamation (weeping of the skin) • If moist desquamation occurs, cleanse the area with warm water and pat dry, apply antibiotic ointment or corticosteroid cream as prescribed, and expose the site to air
BRACHYTHERAPY • DESCRIPTION – Radiation source comes into direct, continuous contact with tumor tissues for a specific time – The radiation source is within the client; for a period of time, the client emits radiation and can pose a hazard to others – Includes either an unsealed or sealed source of radiation
BRACHYTHERAPY • UNSEALED RADIATION SOURCES – Administered via the oral or IV routes, or as an instillation into body cavities – The source is not completely confined to one body area, and it enters body fluids and is eventually eliminated via various excreta, which is radioactive and harmful to others – Most of the source is eliminated from the body within 48 hours; then the client nor the excreta are radioactive or harmful
BRACHYTHERAPY • SEALED RADIATION SOURCES – A sealed, temporary or permanent radiation source (solid implant) placed within the tumor target tissues – The client emits radiation while the implant is in place, but the excreta is not radioactive
SEALED RADIATION SOURCE • NURSING CARE – Place the client in a private room with a private bath – Place a radiation caution sign on the client’s door – Organize nursing tasks to minimize exposure to the radiation source – Nursing assignments to a client with a radiation implant should be rotated
SEALED RADIATION SOURCE • NURSING CARE – Limit time to one-half hour per care provider per shift – Wear a dosimeter film badge to measure radiation exposure – Wear a lead shield to reduce the transmission of radiation – A nurse should never care for more than one client with a radiation implant at one time
SEALED RADIATION SOURCE • NURSING CARE – Do not allow a pregnant nurse to care for the client – Do not allow children under the age of 16 or a pregnant woman to visit the client – Limit visitors to one-half hour per day; visitors should be at least six feet from the source – Save bed linens and dressings until the source is removed, then dispose in the usual manner – Other equipment can be removed from the room at any time
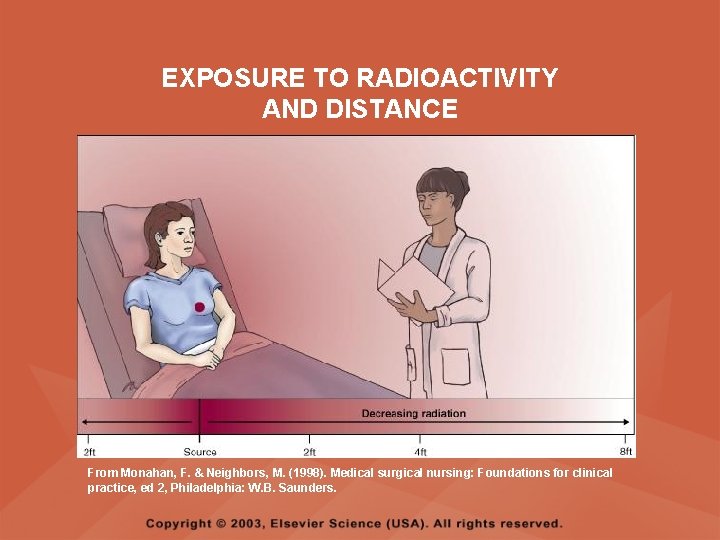
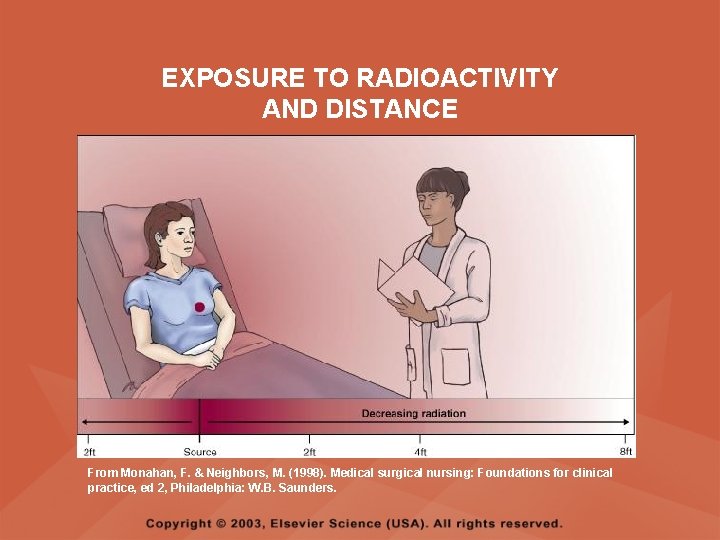
EXPOSURE TO RADIOACTIVITY AND DISTANCE From Monahan, F. & Neighbors, M. (1998). Medical surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
A DISLODGED RADIATION SOURCE • Do not touch a dislodged radiation source with bare hands • If the radiation source dislodges, use a longhandled forcep and place in the lead container kept in the client’s room, and call the physician • If unable to locate the radiation source, bar visitors and notify the physician
REMOVAL OF SEALED RADIATION SOURCES • The client is no longer radioactive • Inform the client that sexual partners cannot “catch” cancer • Inform the female client that she may resume sexual intercourse after 7 to 10 days, if the implant was cervical or vaginal • Provide a betadine douche if prescribed, if the implant was placed in the cervix • Administer a Fleets enema if prescribed
REMOVAL OF SEALED RADIATION SOURCES • Advise the client who had a cervical or vaginal implant to notify the physician if nausea, vomiting, diarrhea, frequent urination, vaginal or rectal bleeding, hematuria, foul-smelling vaginal discharge, abdominal pain or distention, or a fever occurs
BONE MARROW TRANSPLANTATION • Used in the treatment of leukemia for clients who have closely matched donors and who are experiencing temporary remission with chemotherapy • The goal of treatment is to rid the client of all leukemic or other malignant cells through treatment with high doses of chemotherapy and whole body irradiation • Since these treatments are lethal to bone marrow, without the replacement of bone marrow function through transplantation, the client would die of infection or hemorrhage
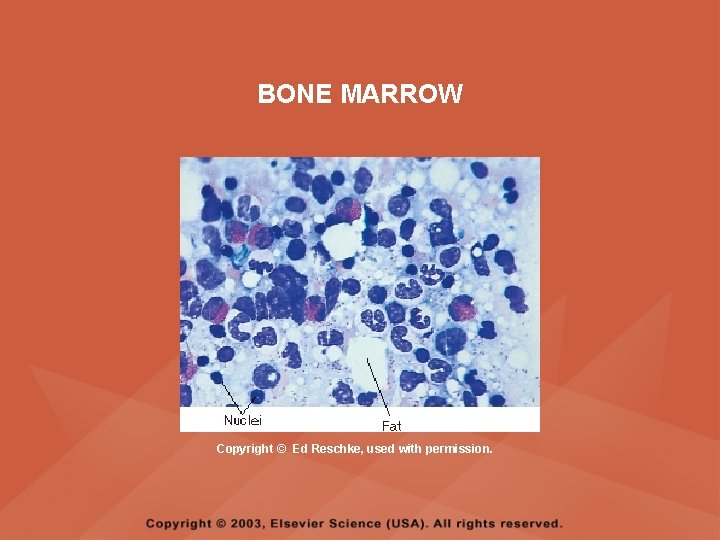
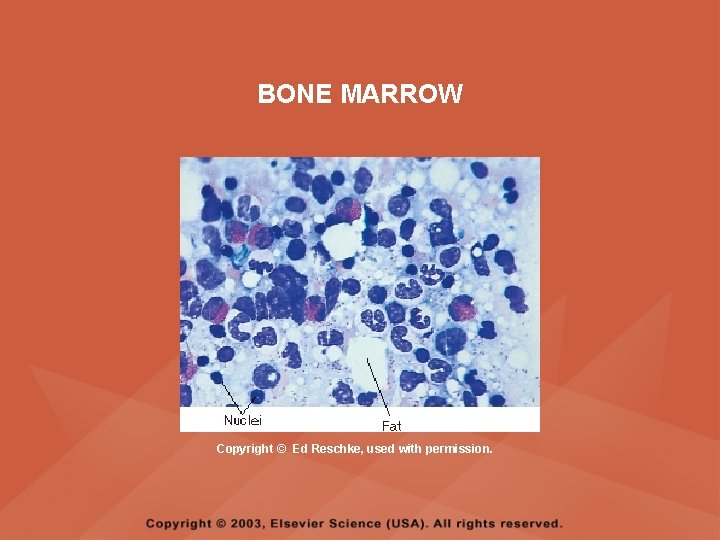
BONE MARROW Copyright © Ed Reschke, used with permission.
TYPES OF DONOR MARROW • ALLOGENEIC – Marrow donor is usually a sibling or parent with a similar tissue type • SYNGENEIC – Uses bone marrow from an identical twin • AUTOLOGOUS – Most common type – The marrow donor is also the recipient – Marrow is harvested during disease remission and is stored frozen to be reinfused later
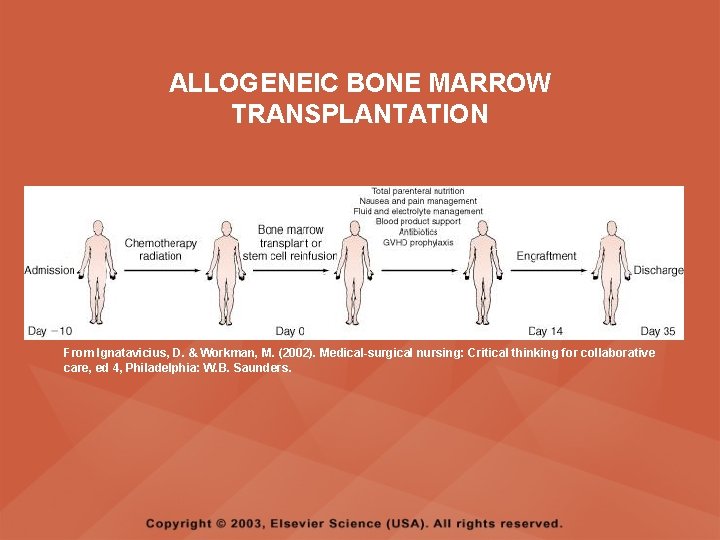
BONE MARROW TRANSPLANTATION HARVEST • Marrow is harvested through multiple aspirations from the iliac crest to retrieve sufficient bone marrow for the transplant • Approximately 500 to 1000 ml of marrow is aspirated • Marrow is filtered for any residual cancer cells and to deplete cells that may cause graft versus host disease • Allogeneic marrow is transfused immediately; autologous marrow is frozen for later use • Harvest is obtained before the initiation of the conditioning regimen
BONE MARROW TRANSPLANTATION CONDITIONING • Refers to an immunosuppression therapy regimen used to eradicate all malignant cells, provide a state of immunosuppression, and create space in the bone marrow for the engraftment of the new marrow
BONE MARROW TRANSPLANTATION TRANSPLANT • Bone marrow is administered through the client’s central line in a manner similar to a blood transfusion • Marrow is infused over a 30 -minute period or may be administered by IV push directly into the central line
BONE MARROW TRANSPLANTATION ENGRAFTMENT • The transfused bone marrow cells move to the marrow-forming sites of the recipient’s bones • Engraftment occurs when the white blood cells, erythrocyte, and platelet counts begin to rise • When successful, the engraftment process takes 2 to 5 weeks
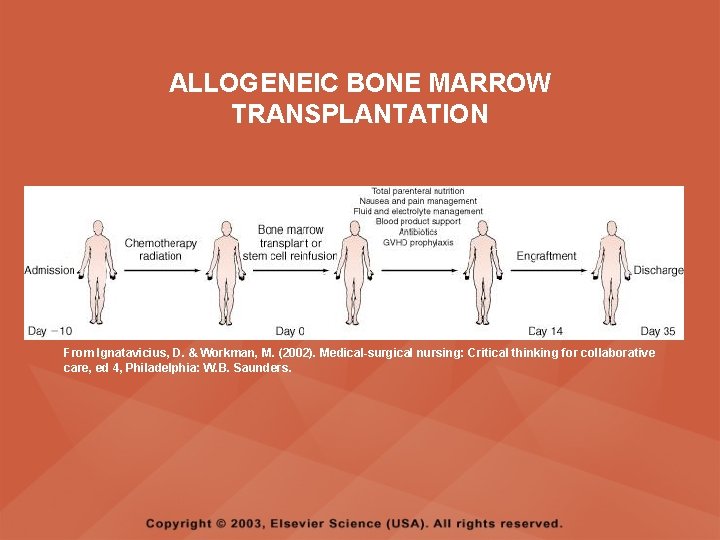
ALLOGENEIC BONE MARROW TRANSPLANTATION From Ignatavicius, D. & Workman, M. (2002). Medical-surgical nursing: Critical thinking for collaborative care, ed 4, Philadelphia: W. B. Saunders.
BONE MARROW TRANSPLANTATION • POST-TRANSPLANTATION PERIOD – The client remains without any natural immunity until the donor marrow begins to proliferate and engraftment occurs – Infection and severe thrombocytopenia are major concerns until engraftment occurs
BONE MARROW TRANSPLANTATION COMPLICATIONS • FAILURE TO ENGRAFT – If the transplanted bone marrow fails to engraft, the client will die unless another transplantation is attempted and is successful
BONE MARROW TRANSPLANTATION COMPLICATIONS • GRAFT VERSUS HOST DISEASE (GVHD) – Although the recipient cannot recognize the donated bone marrow cells as foreign or nonself because of the total immunosuppression, the immune-competent cells of the donated marrow recognize the client’s cells as foreign and mount an immune offense against them – The graft is actually trying to attack the host
BONE MARROW TRANSPLANTATION COMPLICATIONS • GRAFT VERSUS HOST DISEASE (GVHD) – GVHD is managed with immunosuppressive agents, with caution to avoid suppressing the new immune system to the extent that the client becomes more susceptible to infection, or the transplanted cells stop engrafting
BONE MARROW TRANSPLANTATION COMPLICATIONS • VENO-OCCLUSIVE DISEASE – Involves occlusion of the hepatic venules by thrombosis or phlebitis – Signs include right upper quadrant abdominal pain, jaundice, ascites, weight gain, and hepatomegaly – Early detection is critical because there is no known way to open the hepatic vessels – The client will be treated with fluids and supportive therapy
 Schistocytes
Schistocytes Chapter 41 musculoskeletal care modalities
Chapter 41 musculoskeletal care modalities Superficial thermal agents
Superficial thermal agents Therapuetic modalities
Therapuetic modalities Physical modalities
Physical modalities Thermal modalities
Thermal modalities Mechanical modalities
Mechanical modalities Brand frame of reference
Brand frame of reference Point of difference and point of parity
Point of difference and point of parity Assessment and treatment alternatives
Assessment and treatment alternatives Coroneal reflex
Coroneal reflex Reconfigured assessment pyramid
Reconfigured assessment pyramid Features and principles of portfolio assessment
Features and principles of portfolio assessment Define dynamic assessment
Define dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Health and social care level 3 unit 14
Health and social care level 3 unit 14 Unit 14 assignment 2 health and social care
Unit 14 assignment 2 health and social care Neurocognitive disorders
Neurocognitive disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Flinders model of chronic care self-management limitations
Flinders model of chronic care self-management limitations Emotional disturbance assistive technology
Emotional disturbance assistive technology Somatic symptom disorder
Somatic symptom disorder Ego dystonic
Ego dystonic Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Medical model psychology
Medical model psychology Diathesis stress model
Diathesis stress model Cluster c
Cluster c Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Avoidant personality traits
Avoidant personality traits Personality disorders dsm 5
Personality disorders dsm 5 Group c personality disorders
Group c personality disorders Cluster b
Cluster b Cluster b personality disorder traits
Cluster b personality disorder traits Personality disorder definition
Personality disorder definition Yorkshire centre for eating disorders
Yorkshire centre for eating disorders Neurosis disorder
Neurosis disorder Mild neurocognitive disorder
Mild neurocognitive disorder Immunoproliferative disorders examples
Immunoproliferative disorders examples Mood disorders
Mood disorders Purine disorders
Purine disorders Purine disorders
Purine disorders Down turner and klinefelter syndrome
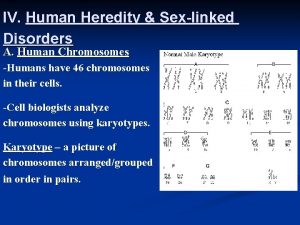
Down turner and klinefelter syndrome Sex linked disorders
Sex linked disorders Unit 14 physiological disorders assignment 1
Unit 14 physiological disorders assignment 1 Autism authorization online program
Autism authorization online program