NURSING On the Right Trach The Role of



- Slides: 24
NURSING On the Right Trach: The Role of the Tracheostomy Coordinator in Care Coordination of Medically-Complex, Tracheostomy-Dependent Children Erika Guillen, BSN, RN, CCRN Darlene Acorda, MSN, RN, CNE, CPNP-PC
NURSING MEDICALLY-COMPLEX CHILDREN BY THE NUMBERS • Defined as children with heterogenous medical conditions that often includes life-sustaining treatments. • Indications, complications, and epidemiological profile have changed over the past three decades. • >50% of children with tracheostomy are under 1 years old at the time of placement. • Average time the tracheostomy is present is 2 years. • Mortality associated with tracheostomy ranged from 0 to 5. 9% over the past three decades (Dal’Astra et al. , 2017).
NURSING PEDIATRIC TRACHEOSTOMIES AT TCH • Cohort of 426 patients between 2001 -2011 • Median patient age was 1. 5 years at time of tracheostomy • Age ranged between 3 days to 24 years • Most common indication: Congenital neurological disease (33%) • Median hospital LOS: 50 days • 53% had ventilator dependency at discharge • 38% underwent decannulation; median time of 5. 3 years • Mortality of 23% over a 10 year period (Mc. Pherson et al. , 2017)
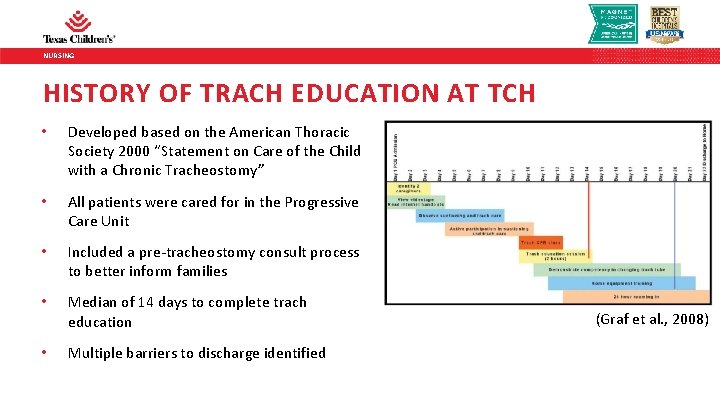
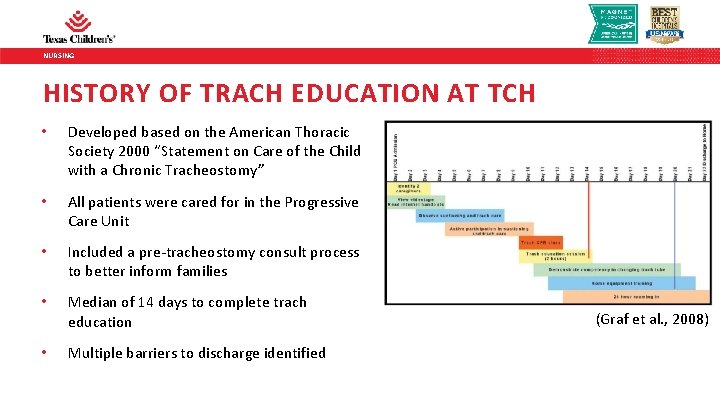
NURSING HISTORY OF TRACH EDUCATION AT TCH • Developed based on the American Thoracic Society 2000 “Statement on Care of the Child with a Chronic Tracheostomy” • All patients were cared for in the Progressive Care Unit • Included a pre-tracheostomy consult process to better inform families • Median of 14 days to complete trach education • Multiple barriers to discharge identified (Graf et al. , 2008)
NURSING BARRIERS TO EDUCATION COMPLETION AND DISCHARGE • Social factors such as lack of transportation, sibling childcare was the most common barrier to education completion (20%) • 10% related to language barrier • 43% of families experienced at least one barrier to education • 20% had multiple barriers to education completion • 89% of families had at least one barrier to discharge • Majority of children were discharged home due to lack of chronic care facilities in our region (Graf et al. , 2008)
NURSING

NURSING
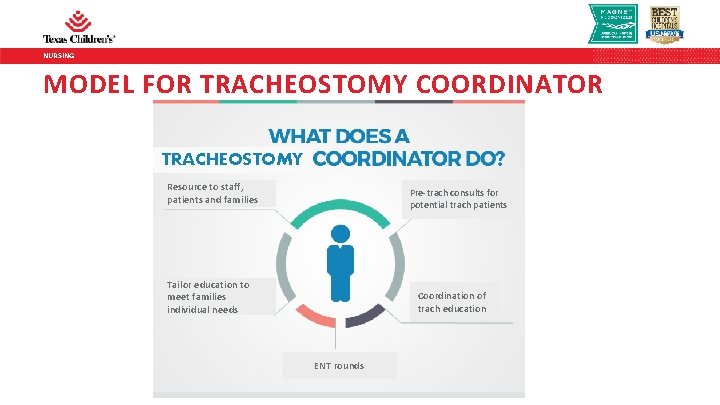
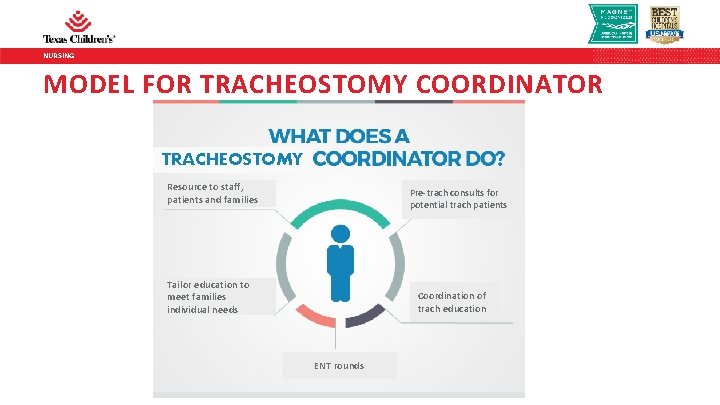
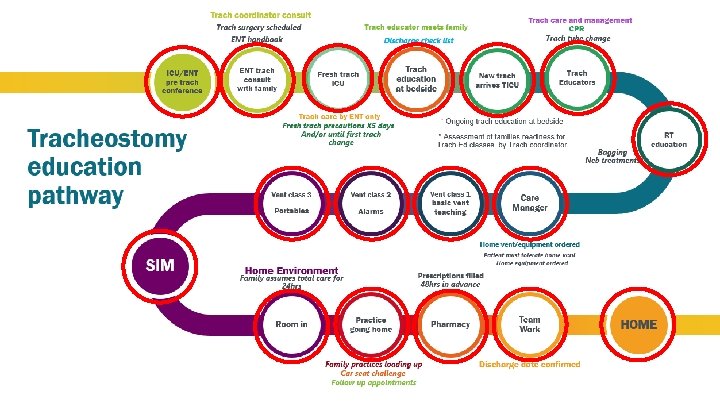
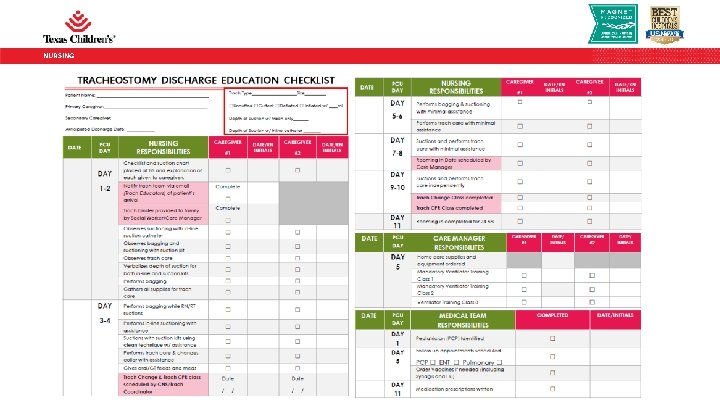
NURSING MODEL FOR TRACHEOSTOMY COORDINATOR TRACHEOSTOMY Resource to staff, patients and families Pre-trach consults for potential trach patients Tailor education to meet families individual needs Coordination of trach education ENT rounds
NURSING TRACH COORDINATOR ROLE • Serve on multiple house-wide trach-related committees • Implement QI initiatives to target education and outcomes • Facilitate simulation training of caregivers • Re-education of established patients readmitted to critical care
NURSING
NURSING

NURSING SIMULATION • Every family receives a 4 hour simulation training prior to rooming-in • Goal is to simulate trach emergencies in the home setting • Families are debriefed on their performance and discuss lessons learned • Highlight the 4 steps: Suction, Bag, Change the Trach, CPR • Involves Trach Coordinator, TICU Medical Director, Critical Care Attending, Clinical Specialist
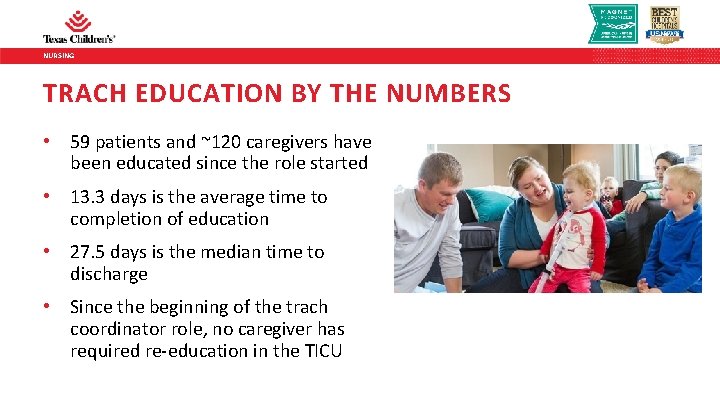
NURSING TRACH EDUCATION BY THE NUMBERS • 59 patients and ~120 caregivers have been educated since the role started • 13. 3 days is the average time to completion of education • 27. 5 days is the median time to discharge • Since the beginning of the trach coordinator role, no caregiver has required re-education in the TICU
NURSING BARRIERS TO EDUCATION • Lack of a second caregiver • Lack of caregiver presence at bedside • Living far from the hospital (e. g. Louisiana) • Childcare and time off from work
NURSING BARRIERS TO DISCHARGE • Patient status (e. g. PHTN, transplant) • Lack of housing • Custody issues • Multiple social issues
NURSING TRAINING STAFF • In FY 2018, over 600 staff trained in PICU/TICU and CPCU/CICU • ~50 Acute Care super users trained • Expansion of the trach program to the Heart Center including training of 7 new trach educators
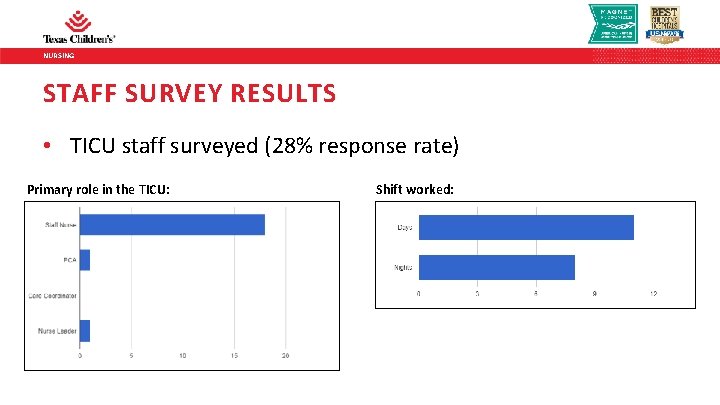
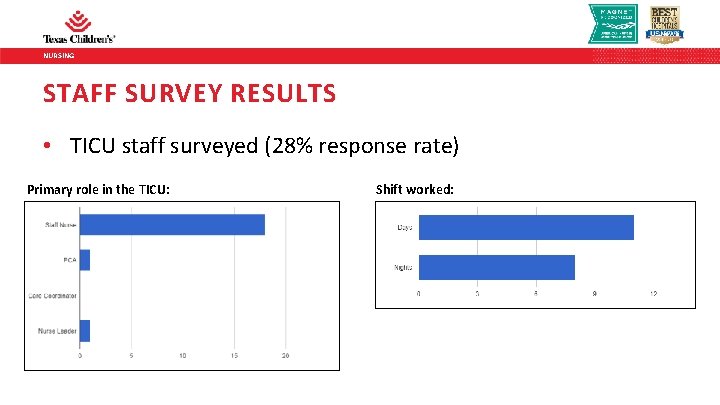
NURSING STAFF SURVEY RESULTS • TICU staff surveyed (28% response rate) Primary role in the TICU: Shift worked:
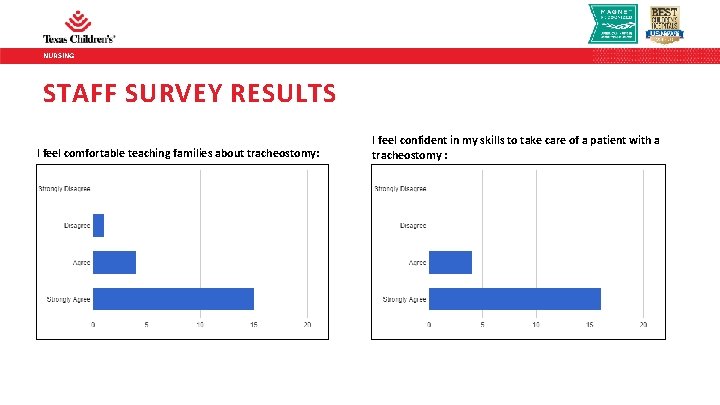
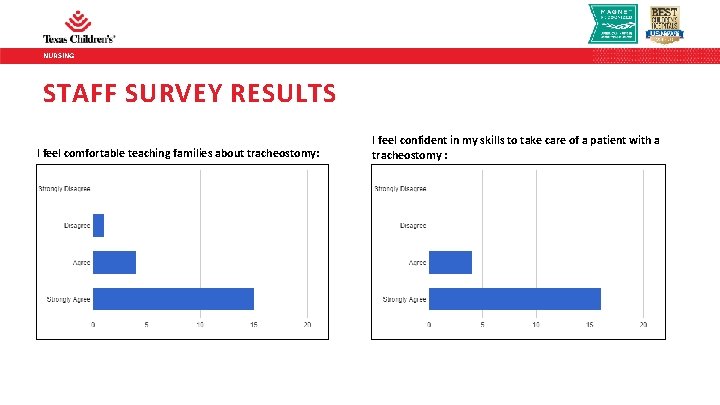
NURSING STAFF SURVEY RESULTS I feel comfortable teaching families about tracheostomy: I feel confident in my skills to take care of a patient with a tracheostomy :
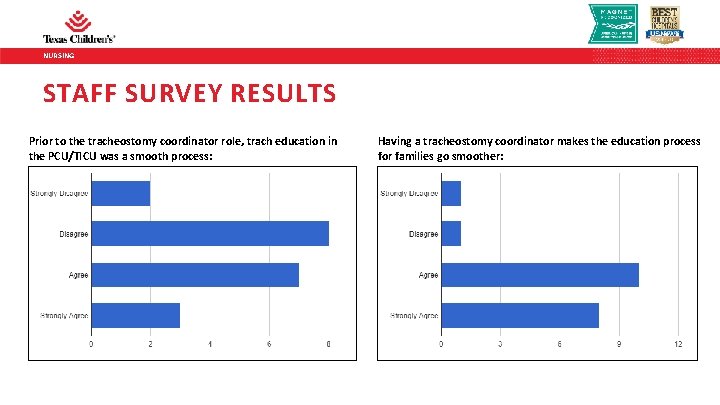
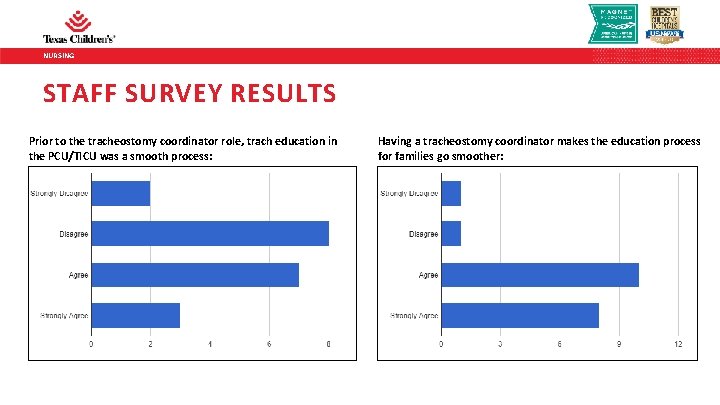
NURSING STAFF SURVEY RESULTS Prior to the tracheostomy coordinator role, trach education in the PCU/TICU was a smooth process: Having a tracheostomy coordinator makes the education process for families go smoother:
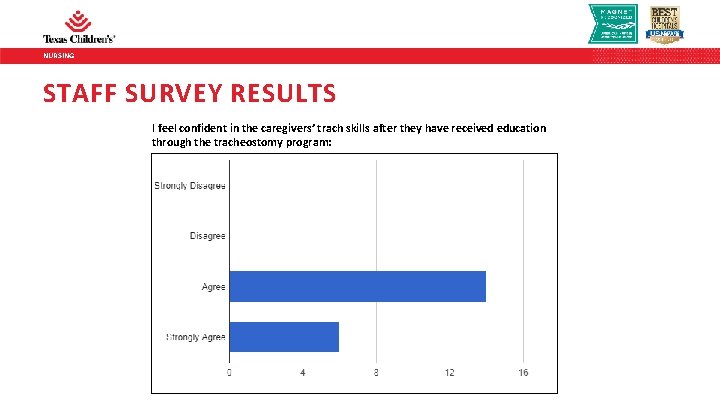
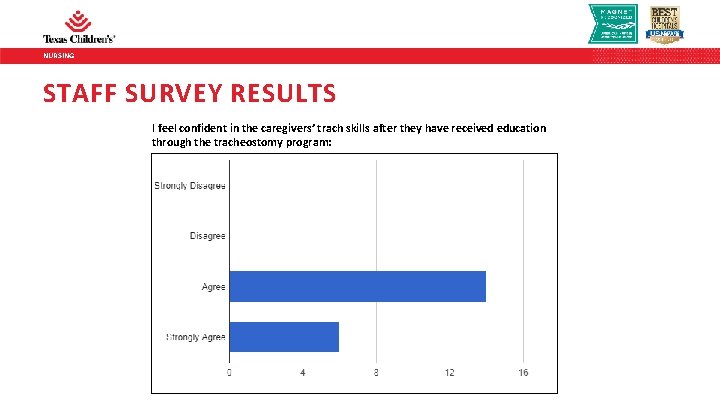
NURSING STAFF SURVEY RESULTS I feel confident in the caregivers’ trach skills after they have received education through the tracheostomy program:
NURSING STAFF SURVEY RESULTS “I like how there is a coordinator who oversees the process/progress of parents in regards to trach education; and is able to help schedule and coordinate classes in a way that is beneficial to the families. ” “I like that there is one person (trach coordinator) we can direct our answers to. ” “The Trach Coordinator is knowledgeable and approachable and friendly with staff. I love the weekly emails. ” “I like that the parents are given all the resources to become competent and confident caregivers. ”
NURSING FUTURE IMPROVEMENT AND RESEARCH • Accidental Decannulation – Lean Project • Qualitative research on the experience of families learning to manage children with tracheostomies • Experience of parents undergoing trach simulation – area ripe for research • Evaluation of overall outcomes of trach education • Innovative ways of teaching families
NURSING REFERENCES • Dal’Astra A. , Quirino, A. V. , de Sousa Caixeta, J. A. , & Avelino, M. (2017). Tracheostomy in childhood: review of the lliterature on complications and mortality over the last three decades. Brazilian Journal of Otorhinolaryngology, 83(2), 207 -214. • Mc. Pherson, M. L. , Shekerdemian, L. , Goldsworthy, M. , Minard, C. G. , Nelson, C. S. , Stein, F. , & Graf, J. M. (2017). A decade of pediatric tracheostomies: Indications, outcomes, and longterm prognosis. Pediatric Pulmonology, 52(7), 946 -953. • Graf, J. M. , Montagnino, B. A. , Hueckel, R. , Mc. Pherson, M. L. (2008). Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatric Pulmonology, 43(8), 788 -794.

NURSING COMMENTS/QUESTIONS?
 Right product right place right time right price
Right product right place right time right price Family time
Family time The right man on the right place at the right time
The right man on the right place at the right time Single vs double lumen tracheostomy tube
Single vs double lumen tracheostomy tube Tracheostomy decannulation
Tracheostomy decannulation Trach collar oxygen flow rates
Trach collar oxygen flow rates Simple mask
Simple mask Resuscitate
Resuscitate Worker role azure
Worker role azure Role making krappmann
Role making krappmann Role conflict occurs when fulfilling the role expectations
Role conflict occurs when fulfilling the role expectations Left left right right go go go
Left left right right go go go Put your right foot in put your right foot out
Put your right foot in put your right foot out Left left right right go go go
Left left right right go go go List of community roles
List of community roles Functional nursing care model
Functional nursing care model Nursing intervention for ocd
Nursing intervention for ocd Preoperative nursing care for eye surgery
Preoperative nursing care for eye surgery Psychiatric nursing process
Psychiatric nursing process Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào