NHS GGC Rostering Masterclass Safe Effective Rostering QEUH





- Slides: 30
NHS GGC Rostering Masterclass: Safe & Effective Rostering QEUH Julie Tomlinson Professional Lead Nurse Bank + LN for area 1
Overview of the Day • • Background/ Policy context Financial governance/ monitoring/ FIP Predicted Absence Allowance (PAA) NHSGGC Policy/Monitoring & Escalating Guidance SCN Workforce Toolkit Rostering Rules HR Policies SSTS/ BOXI 2
Learning Outcomes • Application of NHSGGC Rostering Policy • Application of Predicted Absence Allowance (PAA) • Application of Rostering Rules • FIP awareness • Resource efficiency management • Identify rostering practice improvements • Identify further learning/ training required 3

Nursing Workforce Planning and Monitoring 4
National, Board & Professional Background • NHSGGC recognised the absence of a process to support effective rostering • Nationally, reports had highlighted the impact of insufficient staff on patient safety and quality of care • Current climate of heightened awareness and scrutiny of resources(FIP). The need to evidence value, includes review of ward Funded Establishment figures, Bank and agency use and NMWWPT results 5
National, Board & Professional Background Health Boards should ensure that …. . . ”where the clinical profile of a group or Ward/Clinical Area of patients changes, (due to acuity and/or dependency) an agreed review framework and process should be in place to ensure that the appropriate skills base and resource requirements are easily provided. ” (Vo. L Report: Recommendation 31) . . ”there is a straightforward and timely escalation process for nurses to report concerns about the staffing numbers/skill mix. ” (Vo. L Report: Recommendation 32) • Board Policy and Guidance • Links with Leading Better Care • NMC Code and Guidance 6
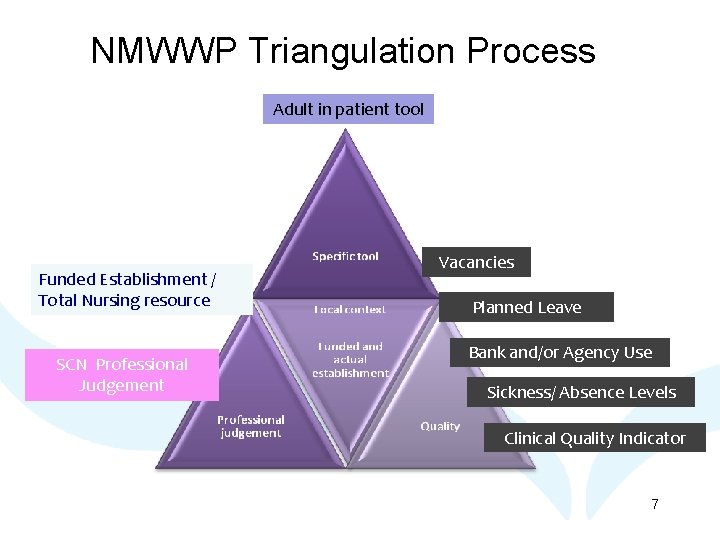
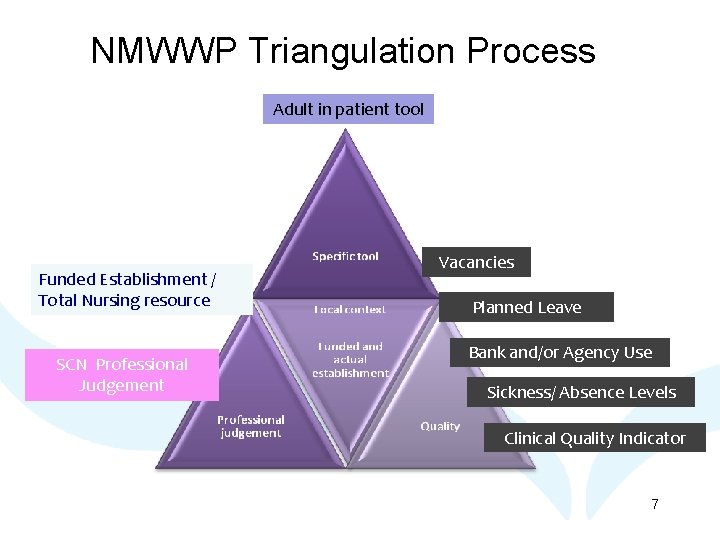
NMWWP Triangulation Process Adult in patient tool Funded Establishment / Total Nursing resource SCN Professional Judgement Vacancies Planned Leave Bank and/or Agency Use Sickness/ Absence Levels Clinical Quality Indicator 7
FIP & Financial Governance Ensuring effective and efficient use of the workforce resource to meet safe, effective person centred care • Why do we need financial governance? • What is it? • Who does it? • How is it monitored locally? • Responsibility and accountability for public spend • Overview of SCN/ service manager role in financial governance. • FIP nursing work streams 8
Evidence of Rostering Problems • External rostering reviews (Deloitte/PWC) • Daily huddles • NMWWPT returns • Increases in supplementary staffing usage • Weekly Bank Use/Agency Reports • Finance reports • Ward visits – corporate visit, inspection • Staff reports – unable to attend meetings due to unexpected shortages, cancelled activities, unable to honour supervisory days, etc. 9
Group Discussion Split into small groups and consider. . . • Problems you have encountered with rostering • Discuss how you have solved these problems • Identify what would have helped you solve problems 10
Comfort Break 11
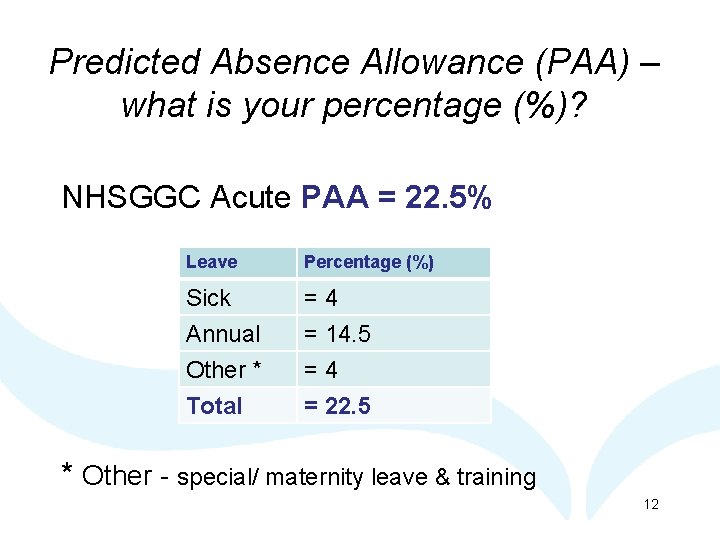
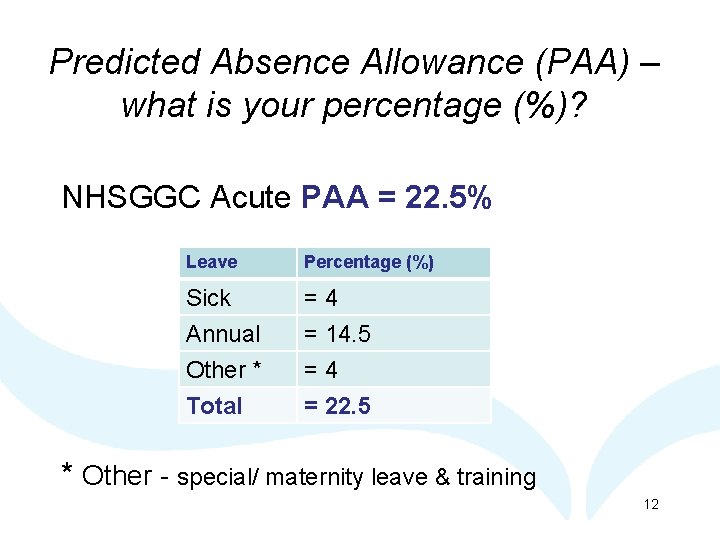
Predicted Absence Allowance (PAA) – what is your percentage (%)? NHSGGC Acute PAA = 22. 5% Leave Percentage (%) Sick Annual Other * =4 = 14. 5 =4 Total = 22. 5 * Other - special/ maternity leave & training 12

13

14

15
Reasons Rostering within the PAA % can be a problem • Roster creators and approvers unfamiliar with PAA • Unexpected mass absences (flu, norovirus, etc) • Staff moving from other areas with pre-agreed leave • Multiple maternity leave • Conflicting standards set in HR policies • Conflicting advice from HR advisors • Achieving the core standard for SCN supervisory days • SCNs only working core hours, counted in numbers • Breaks required on long-day shift systems. 16
Group Discussion In small groups and explore…. . • How you apply PAA when rostering • How you currently calculate PAA • Who monitors PAA for your ward/ service • Views on SCN Workforce Planning Toolkit • If there any changes that you need to make to your rostering practice. 17

What is in place to support you? • • NHS GGC Rostering Policy NHS GGC Monitoring and Escalation Guidance Roster Rules Local Champions SSTS and BOXI Supplementary staff locally available Manpower co-ordinator / nurse pageholder (or equivalent) • Nurse Bank Operational Policy • H. R. Connect – Support and Advice Unit. • NMWWP Tools. 18
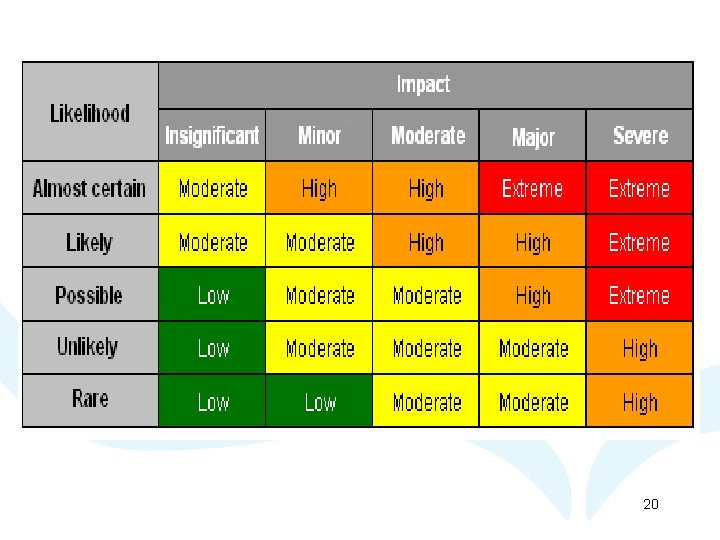
Monitoring and Escalation • Purpose • Categories of Risk • Nurse in Charge responsibility & accountability • Senior Charge Nurse responsibility & accountability • Lead Nurse/Service Manager responsibility and accountability 19
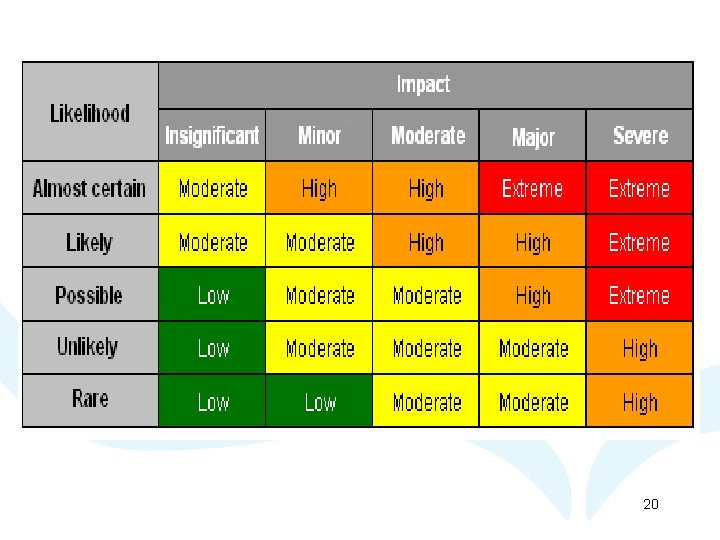
20
HR Session • FAQ • HRConnect 21
Lunch 22
Board Policy & Guidance Nursing & Midwifery Rostering Policy Monitoring & Escalation Guidance • Ensuring right mix of nursing skills, experience & competency within all of our clinical areas at all times is a complex matrix of interdependent systems and processes both clinical and operational. • Policy and Guidance aim to support the decision making of staff who have responsibility for safe and effective staff decision making on a day to day, shift by shift basis. 23
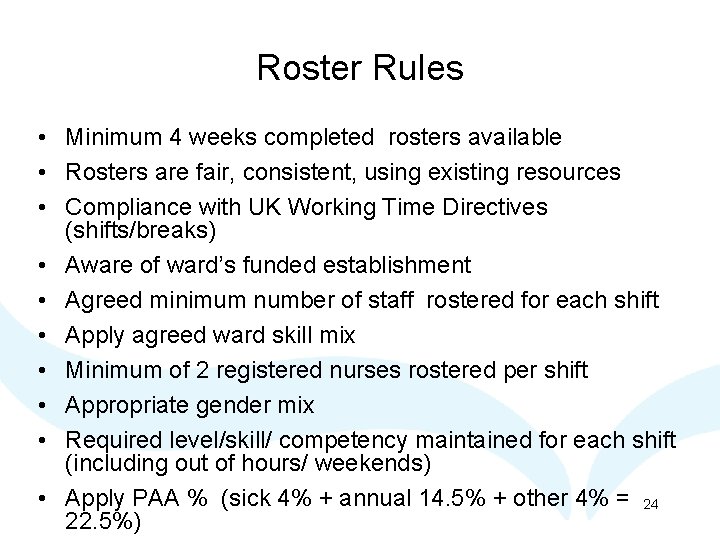
Roster Rules • Minimum 4 weeks completed rosters available • Rosters are fair, consistent, using existing resources • Compliance with UK Working Time Directives (shifts/breaks) • Aware of ward’s funded establishment • Agreed minimum number of staff rostered for each shift • Apply agreed ward skill mix • Minimum of 2 registered nurses rostered per shift • Appropriate gender mix • Required level/skill/ competency maintained for each shift (including out of hours/ weekends) • Apply PAA % (sick 4% + annual 14. 5% + other 4% = 24 22. 5%)
Roster Rules continued. . . • Allocate planned annual leave over the calendar year (ensure PAA= 14. 5%) • Planned leave prioritised over unplanned leave e. g. Statutory/Mandatory training is prioritised over other study/parental leave • Calculate PAA% prior to applying maximum planned leave allocations • Unplanned leave i. e. Sickness (4%) & Special/Maternity (4%) of the PAA is monitored and taken into consideration when allocating planned leave so that overall 22. 5% PAA is applied • Mentors rostered to supervise nursing students • Plan statutory/ mandatory training over calendar year 25
Scenarios In small groups …. . • Discuss the scenarios (review rosters) • Consider the Roster Rules • Identify issues impacting on effective rostering • Consider roster creator/ approver roles • Identify resource efficiency improvements (if any) that can be made. 26
SSTS / BOXI Practical demonstration SSTS & BOXI functionality facilitated by SSTS team 27
Questions Any “lightbulb” moments? What will be your challenges? Anything you know you didn’t know at the beginning of the day? Discussion 28
Next Steps ü Identify one action to take forward from today ü Identify additional learning needs/ further training required ü Let us know what you think of this programme! 29
Evaluation • Rate today’s sessions • What immediate follow-up is required? • Complete follow-up questionnaire to be sent in 3 months • NWWPT baseline measures • Impact evaluation Thank you The End 30