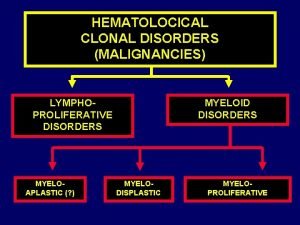
Myeloid Neoplasm and Hematopoietic Stem Cell Disorders Zartash

- Slides: 30
Myeloid Neoplasm and Hematopoietic Stem Cell Disorders Zartash Gul, MD Associate Professor of Medicine Division of Hematology & Oncology University of Cincinnati College of Medicine 2/4/2018
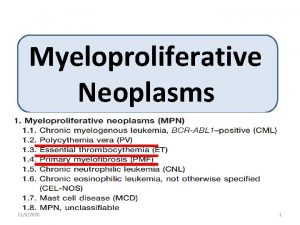
Overview • CML (BCR/ABL+ve) • Myeloproliferative neoplasms (JAK 2 +ve PV, ET, Myelofibrosis) • AML-APL • MDS • Hematopoietic stem cell transplant MPD
CML (Chronic Myeloid Leukemia) • Myeloproliferative disorder with overproduction of myeloid cells that differentiate. • Philadelphia chromosome positive t(9: 22) • Presentation – Chronic phase- <10% blasts asymptomatic, splenomegaly – accelerated phase-10 -20% blasts – Blast phase >20% blasts and/or extramedullary disease , s/s of acute leukemia (anemia, leukopenia, leukocytosis, thrombocytopenia)
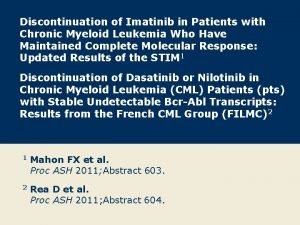
CML • Treatment: Imatinib, Dasatinib, Nilotinib– all inhibitors of BCR/ABL tyrosine kinase. • Most patients in chronic phase do not need upfront consideration for allogeneic transplant. • Patients who present in blast phase, accelerated phase or develop mutations on TKIs or are intolerant will need consideration for transplant.
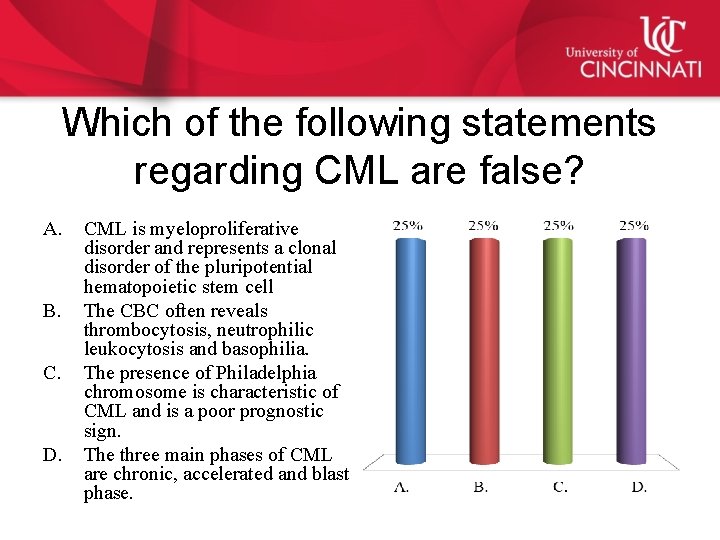
Which of the following statements regarding CML are false? A. B. C. D. CML is myeloproliferative disorder and represents a clonal disorder of the pluripotential hematopoietic stem cell The CBC often reveals thrombocytosis, neutrophilic leukocytosis and basophilia. The presence of Philadelphia chromosome is characteristic of CML and is a poor prognostic sign. The three main phases of CML are chronic, accelerated and blast phase.
Answer • C) Up to 95% of patients with CML express Philadelphia chromosome which results from a reciprocal translocation between long arms of chromosome 9 and 22. Patients with CML who do not have this translocation have a considerably worse prognosis than patients who do.
Myeloproliferative disorders (JAK 2 positive) • Polycythemia Vera –Increase in RBC mass , Increase in granulocytes and platelets. r/o gaisbock’s syndrome or other causes of erthrocytosis. • Presentation –hyper viscosity-headache, dizziness – Thrombosis – Bleeding – Pruritis (inc histamine form basophils) – Splenomegaly • Evaluation-Erythropoietin , inc WBC, basophils, , Vit B 12 LAP • Treatment: Phlebotomy (HCT men <45% and females<42%), Aspirin, Hydrea (if prior h/o thrombosis, age >60 or plt >1. 5 million)
Essential Thrombocytosis • Increase in platelets >600, 000/ul • r/o reactive thrombocytosis –inflammation, post splenectomy, iron deficiency etc. • Presentation: asymptomatic; thrombosis, erythromelalgia • Diagnosis: Peripheral smear-large hypogranular plts. • Bone marrow bx: megakaryocytic hyperplasia • Treatment: low risk –asprin, high risk add hydrea plt goal<400, 000
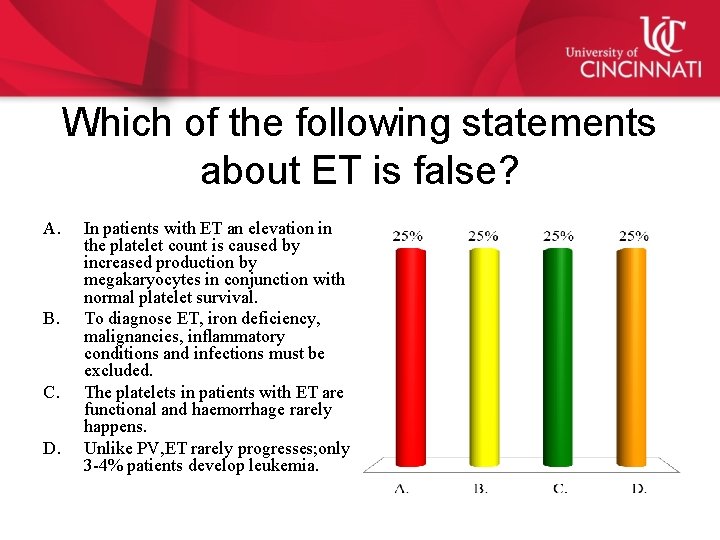
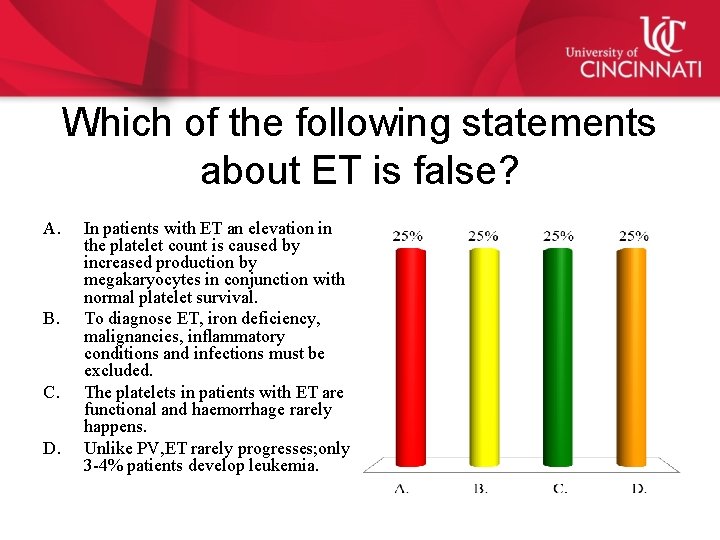
Which of the following statements about ET is false? A. B. C. D. In patients with ET an elevation in the platelet count is caused by increased production by megakaryocytes in conjunction with normal platelet survival. To diagnose ET, iron deficiency, malignancies, inflammatory conditions and infections must be excluded. The platelets in patients with ET are functional and haemorrhage rarely happens. Unlike PV, ET rarely progresses; only 3 -4% patients develop leukemia.
Answer • C) hemorrhagic events can occur in upto 40% patients with ET
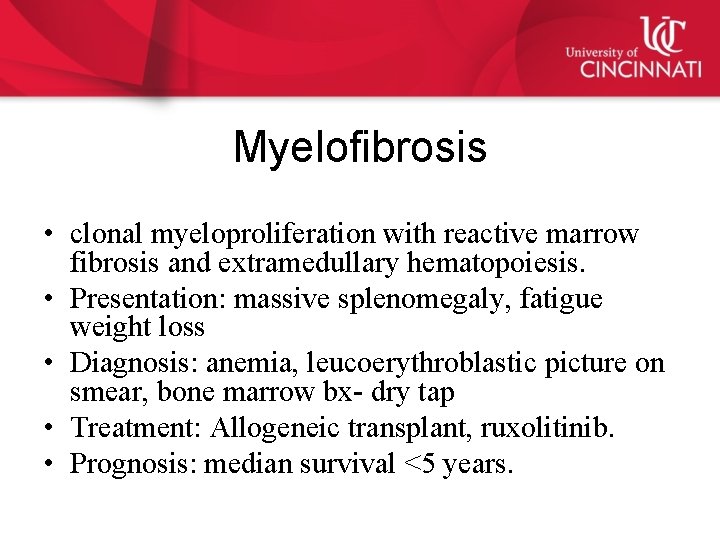
Myelofibrosis • clonal myeloproliferation with reactive marrow fibrosis and extramedullary hematopoiesis. • Presentation: massive splenomegaly, fatigue weight loss • Diagnosis: anemia, leucoerythroblastic picture on smear, bone marrow bx- dry tap • Treatment: Allogeneic transplant, ruxolitinib. • Prognosis: median survival <5 years.
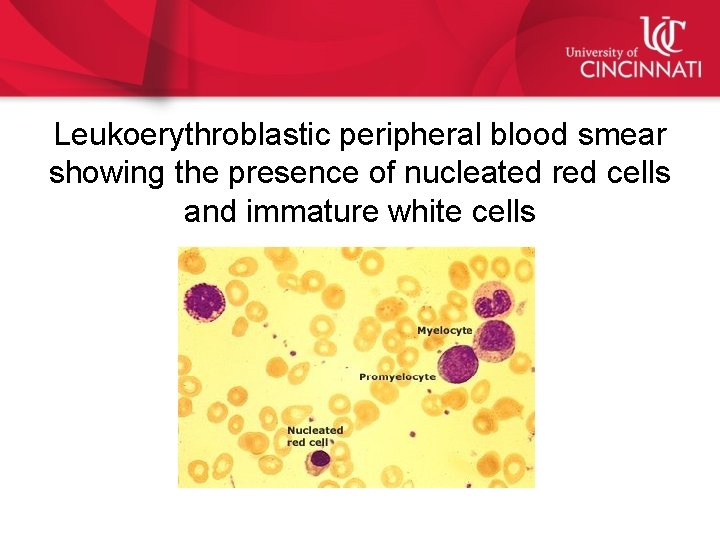
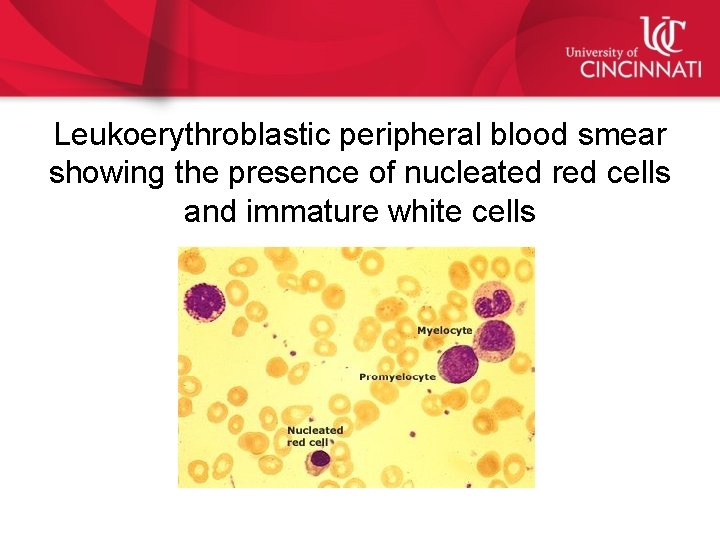
Leukoerythroblastic peripheral blood smear showing the presence of nucleated red cells and immature white cells

AML • Clonal proliferation of hematopoietic precursors with decreased ability to differentiate into mature cells. • Risk factors: prior radiation and chemotherapy. • Presentation: anemia, thrombocytopenia, leukostais, DIC, TLS. • Diagnosis: Peripheral smear, Bone marrow biopsy • Treatment: Induction with 7+3 (anthracycine and cytarabine) • Prognosis: age, cytogenetics.
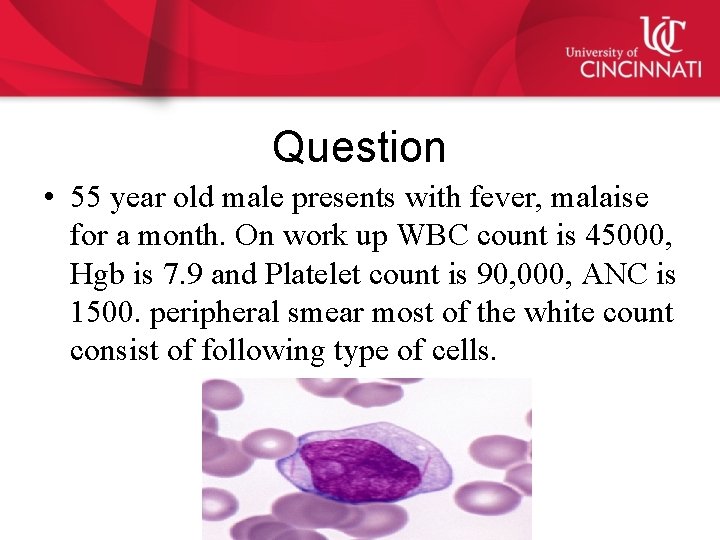
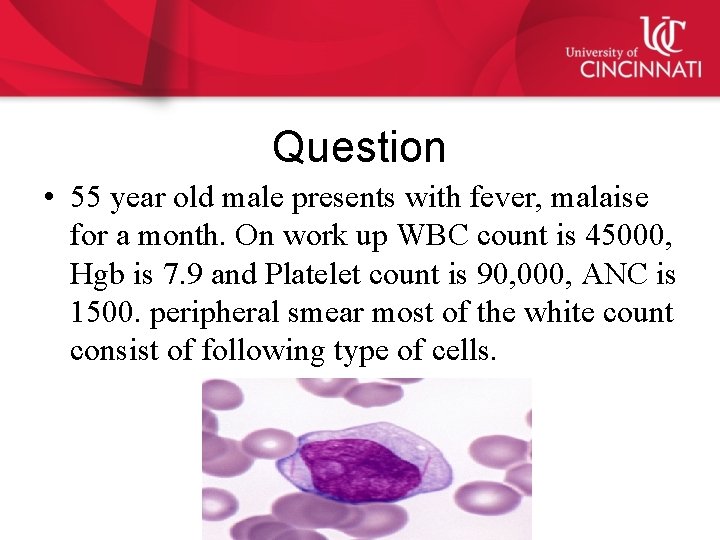
Question • 55 year old male presents with fever, malaise for a month. On work up WBC count is 45000, Hgb is 7. 9 and Platelet count is 90, 000, ANC is 1500. peripheral smear most of the white count consist of following type of cells.
What is your next step in management? A. Obtain blood cultures B. Start broad spectrum antibiotics. C. Start allopurinol D. Consult hematology/oncology
Answer C) start allopurinol • While obtaining blood cultures, starting antibiotics and consulting hematology/oncology are all important steps in managing the patient as an internist prevention of tumor lysis syndrome in a patient with acute leukemia is of utmost importance and therefore early institution of allopurinol.
APL • Biologically and clinically distinct variant of AML. APL -AML-M 3 -(FAB) classification system • Acute Promyelocytic Leukemia with t(15; 17); PML-RARA in the World Health Organization classification system. • Induction: All-Trans Retinoic Acid (ATRA) • Resulted in the highest cure rates. • High-risk patients: • Combination of ATRA and chemotherapy • Low-risk patients (WBC ≤ 10): • Combination of ATRA and Arsenic Trioxide for induction and consolidation therapy. • DIC well known complication-start therapy and supportive care.
33 year old male with APL started on ATRA. A few days later his WBC countis up from 4600/ul 36, 240/ul. He has low grade fever and a mild cough. Which of the following would be an appropriate next step in management of this patient? A. Discontinue ATRA B. Discontinue ATRA and start high dose dexamethasone. C. Continue current therapy. D. Start antibiotics.
Answer C) discontinue ATRA and start steroids. • Recognize ATRA syndrome. Fever, hyper leukocytosis, respiratory symptoms.
MDS • It is a heterogeneous group that shares 3 common featuresdysplastic looking marrow, peripheral blood cytopenia and a tendency to evolve into AML. • About 25% can progress to AML esp those with poor karyotype and >10% blasts. • Cause of death in most patients is infections. • In older patients we can use supportive care or hypomethylating agents. • Only curative therapy is allogeneic transplant. • Lenalidomide therapy is effective in patients with del 5 q.
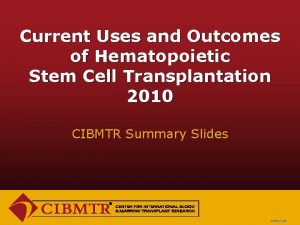
Hematopoietic stem cell transplant • Autologous stem cell transplant – Patient is his own donor – No risk of GVHD – Used mostly in Multiple myeloma, lymphoma and immune mediated disorders • Allogeneic stem cell transplant – Patient needs a donor related, unrelated, fully HLA matched, mismatched donor, Haploidentical donor or cord blood transplant. – Risk of GVHD, VOD, infections – Mostly done for leukemias or lymphomas that relapse after autologous transplant
Complications of allogeneic transplant. • Early<30 days: – – Mucositis, GI toxicity, VOD, Infection, Agvhd • >30 days and long term – – acute and chronic GVHD infertility, second malignancy, cardiovascular disease.
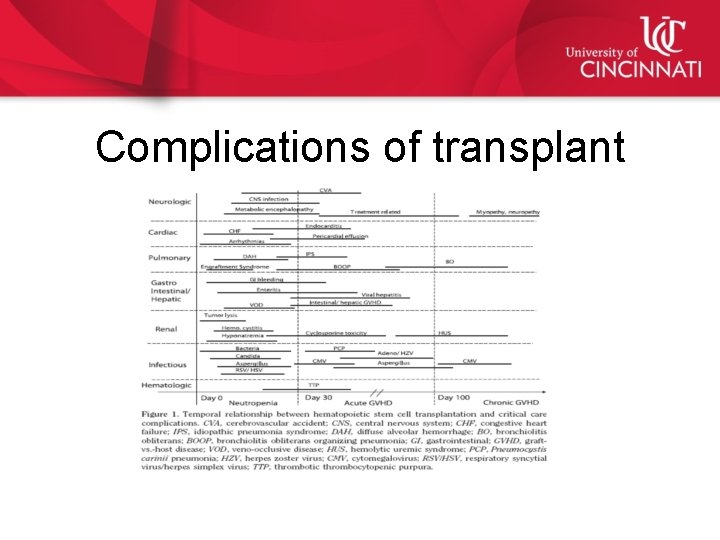
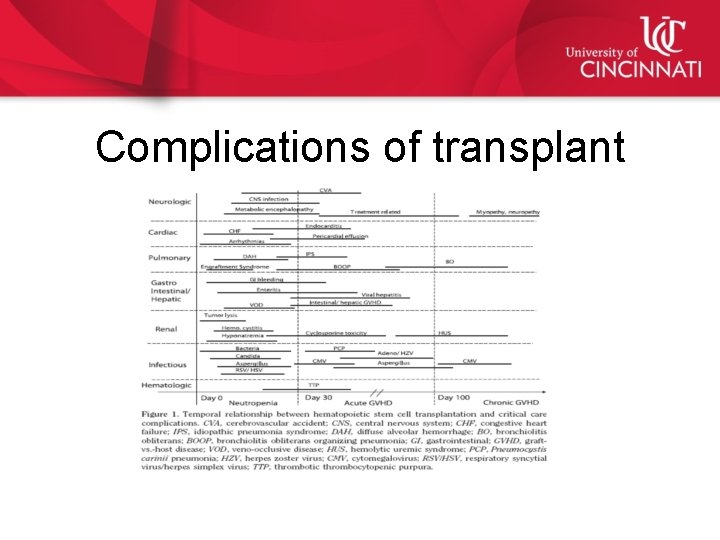
Complications of transplant
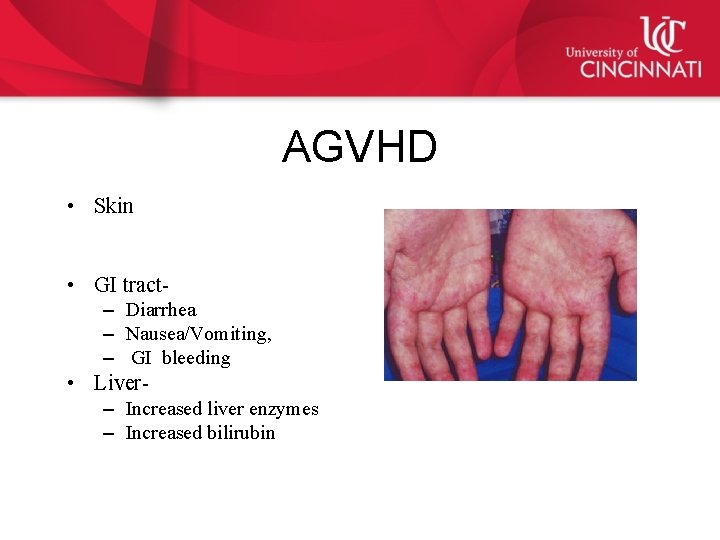
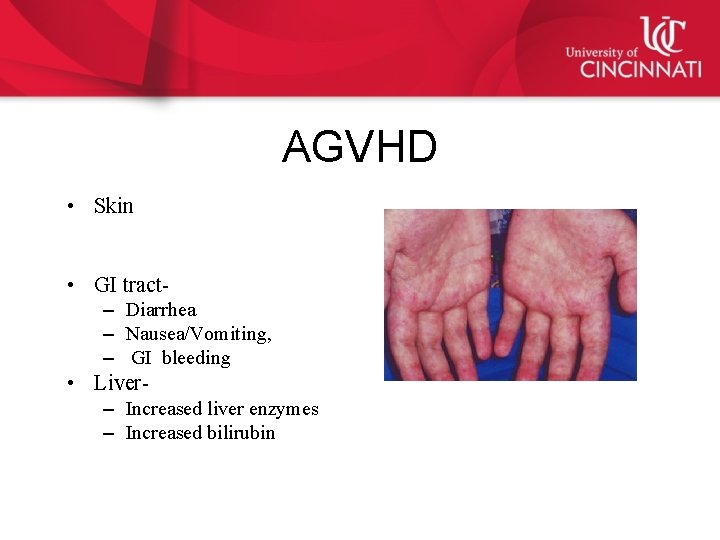
AGVHD • Skin • GI tract– Diarrhea – Nausea/Vomiting, – GI bleeding • Liver– Increased liver enzymes – Increased bilirubin
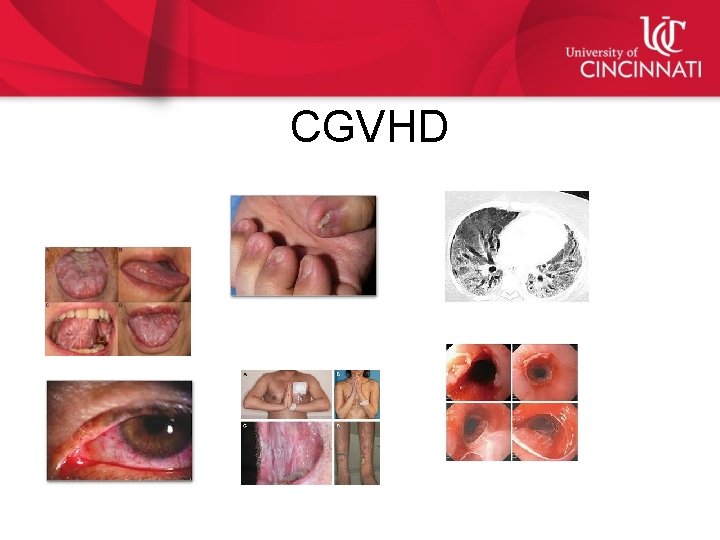
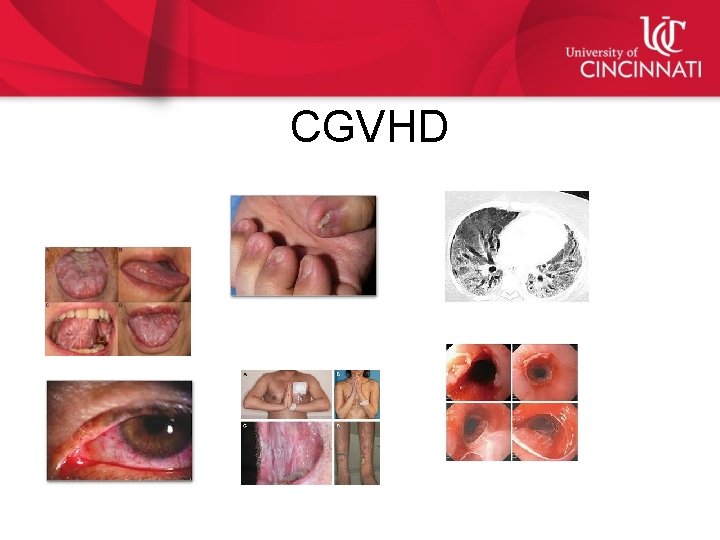
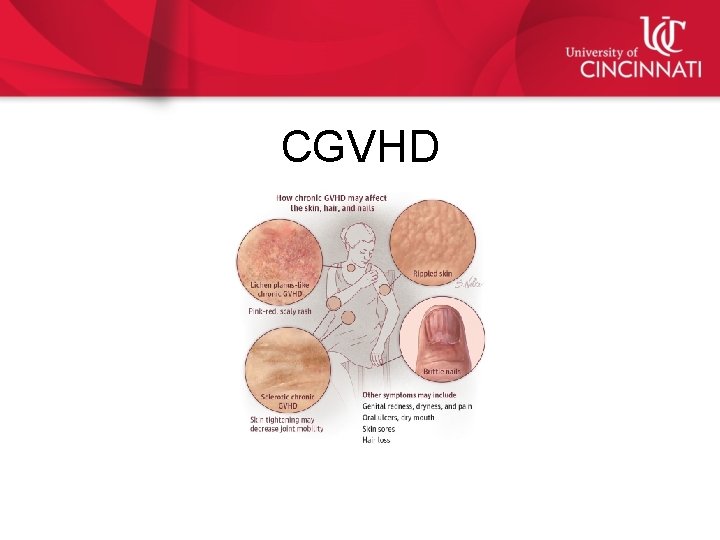
CGVHD
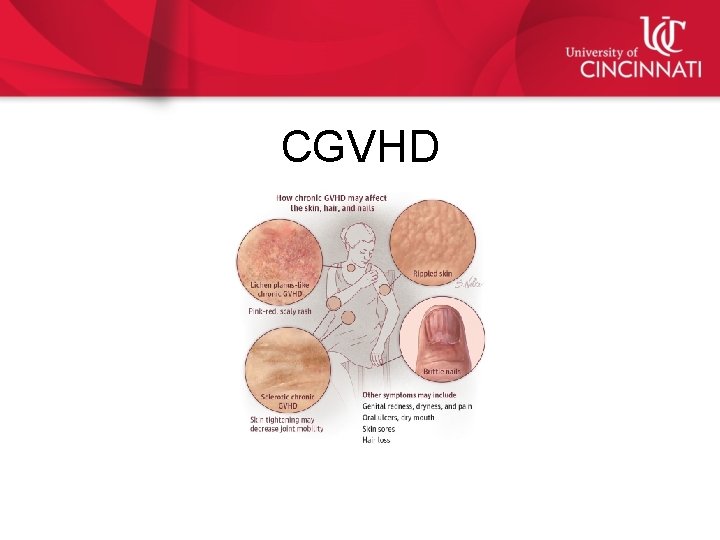
CGVHD
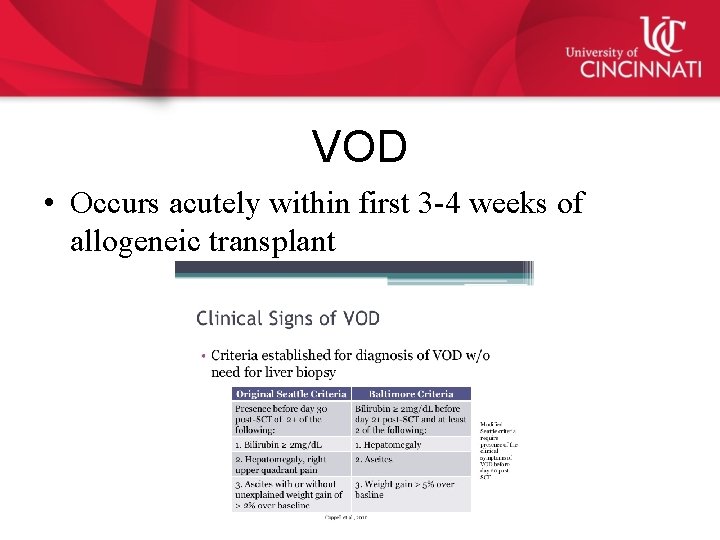
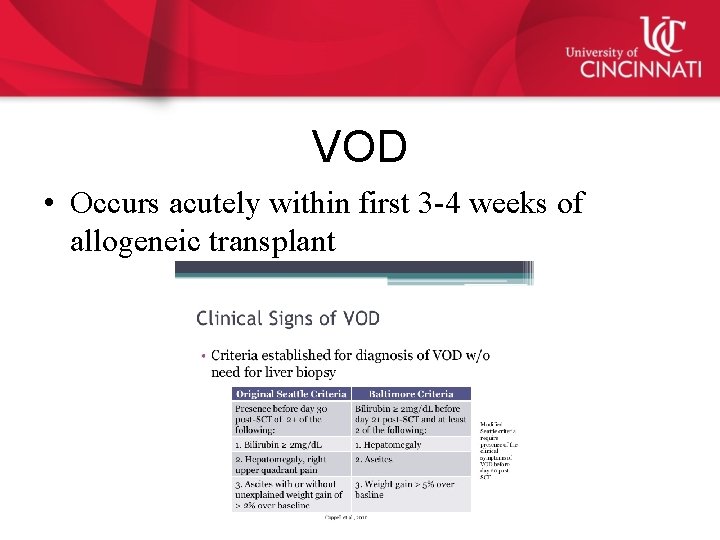
VOD • Occurs acutely within first 3 -4 weeks of allogeneic transplant
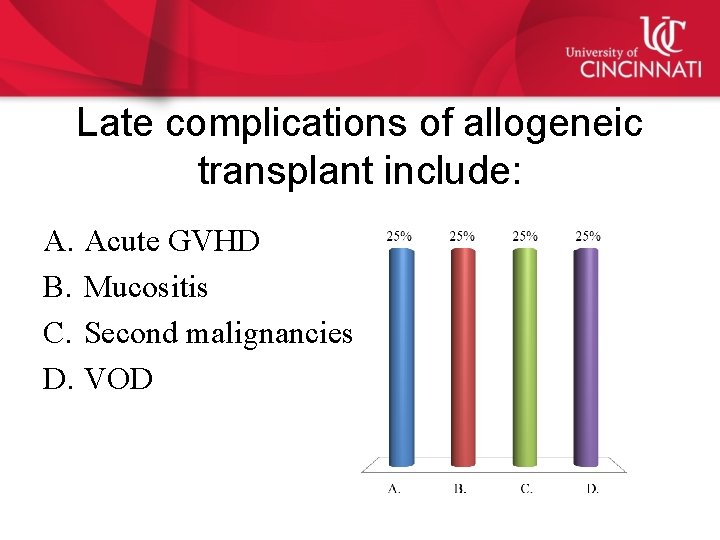
Late complications of allogeneic transplant include: A. Acute GVHD B. Mucositis C. Second malignancies D. VOD
Answer • Second malignancies.
Thank you
 Zartash uzmi
Zartash uzmi Hematopoietic drugs wikipedia
Hematopoietic drugs wikipedia Plasma cell neoplasm
Plasma cell neoplasm Bronchogenic neoplasm
Bronchogenic neoplasm Excessive and frequent menstruation with irregular cycle
Excessive and frequent menstruation with irregular cycle Icd 10 ca nasofaring
Icd 10 ca nasofaring Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Perdida de polaridad celular
Perdida de polaridad celular Classification of polycythemia
Classification of polycythemia Carcinoma in situ
Carcinoma in situ Exocrine tumors of pancreas
Exocrine tumors of pancreas Lumpy jaw meaning
Lumpy jaw meaning Myeloid tissue is a type of
Myeloid tissue is a type of Liters to gallon
Liters to gallon Treatment of cml
Treatment of cml Sites of bone marrow
Sites of bone marrow Chronic myeloid leukemia
Chronic myeloid leukemia Chronic myeloid leukemia
Chronic myeloid leukemia Mark juckett md
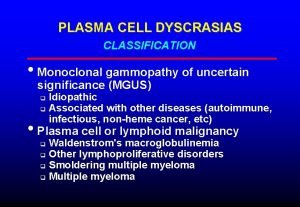
Mark juckett md Plasma cell dyscrasias classification
Plasma cell dyscrasias classification In figure 10-4 what role does structure a play in mitosis
In figure 10-4 what role does structure a play in mitosis Keva triple stem cell benefits
Keva triple stem cell benefits Stem cell politics
Stem cell politics Stem cell
Stem cell Stem cell culture
Stem cell culture Stem cell therapy rhode island
Stem cell therapy rhode island Oncogens
Oncogens Stem cell markers slideshare
Stem cell markers slideshare Stem cell classification chart
Stem cell classification chart Papaemmanuil
Papaemmanuil Lll leukemia
Lll leukemia