Multivessel PCI Pearls of Wisdom for Success Jeffrey





- Slides: 39
Multivessel PCI: Pearls of Wisdom (? ) for Success Jeffrey W. Moses, MD Professor of Medicine Director, Interventional Cardiac Therapeutics Columbia University Medical Center Director Complex Coronary Interventions St. Francis Hospital, Roslyn, LI
Jeffrey Moses MD I have relevant financial relationships Consultant BSC Abiomed Abbott

MVD Pearls • Can PCI be done as safely as CABG?
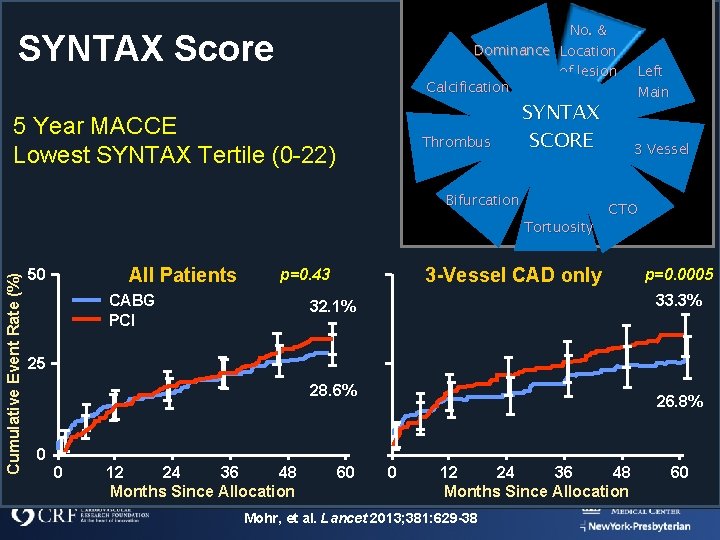
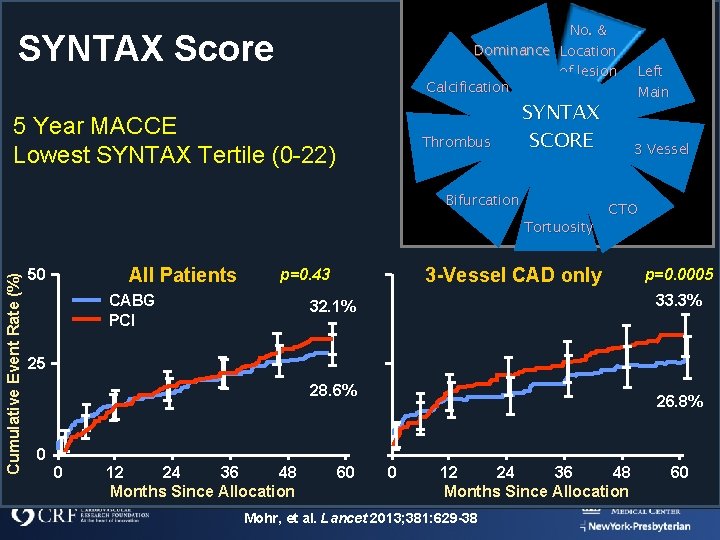
No. & Dominance Location of lesion Calcification SYNTAX Score 5 Year MACCE Lowest SYNTAX Tertile (0 -22) Thrombus SYNTAX SCORE Bifurcation Cumulative Event Rate (%) Tortuosity All Patients 50 CABG PCI 3 Vessel CTO 3 -Vessel CAD only p=0. 43 Left Main p=0. 0005 33. 3% 32. 1% 25 28. 6% 0 0 12 24 36 48 Months Since Allocation 60 26. 8% 0 12 24 36 48 Months Since Allocation Mohr, et al. Lancet 2013; 381: 629 -38 60
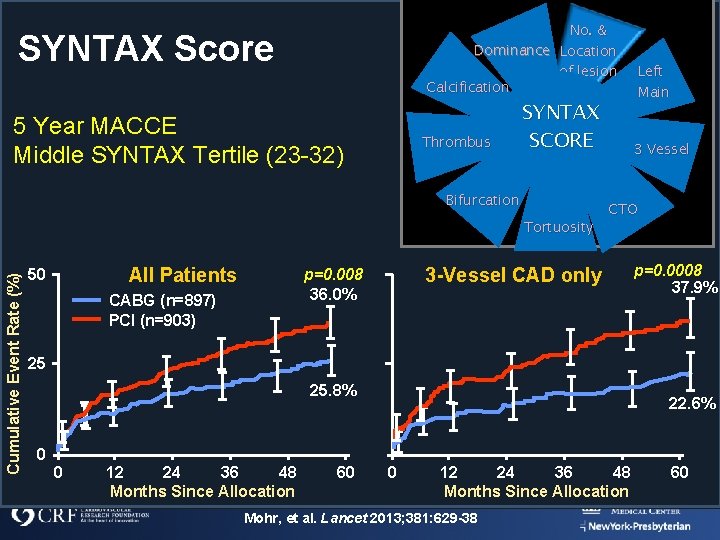
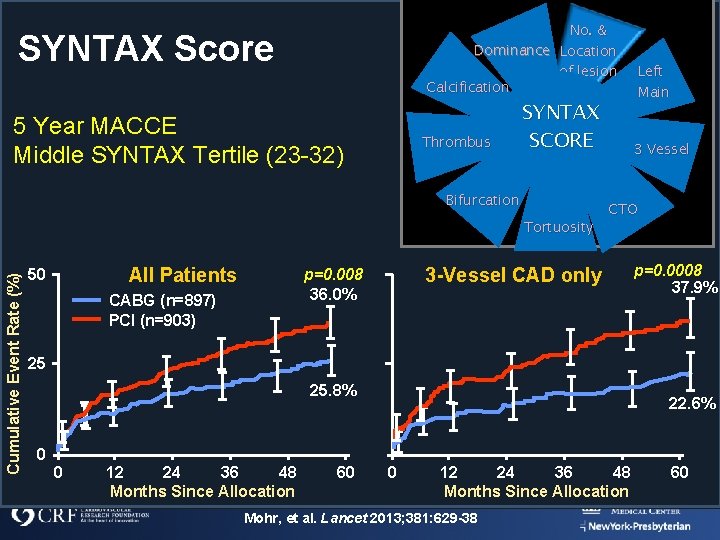
No. & Dominance Location of lesion Calcification SYNTAX Score 5 Year MACCE Middle SYNTAX Tertile (23 -32) Thrombus SYNTAX SCORE Bifurcation Cumulative Event Rate (%) Tortuosity All Patients 50 CABG (n=897) PCI (n=903) 3 Vessel CTO 3 -Vessel CAD only p=0. 008 36. 0% Left Main p=0. 0008 37. 9% 25 25. 8% 0 0 12 24 36 48 Months Since Allocation 60 22. 6% 0 12 24 36 48 Months Since Allocation Mohr, et al. Lancet 2013; 381: 629 -38 60
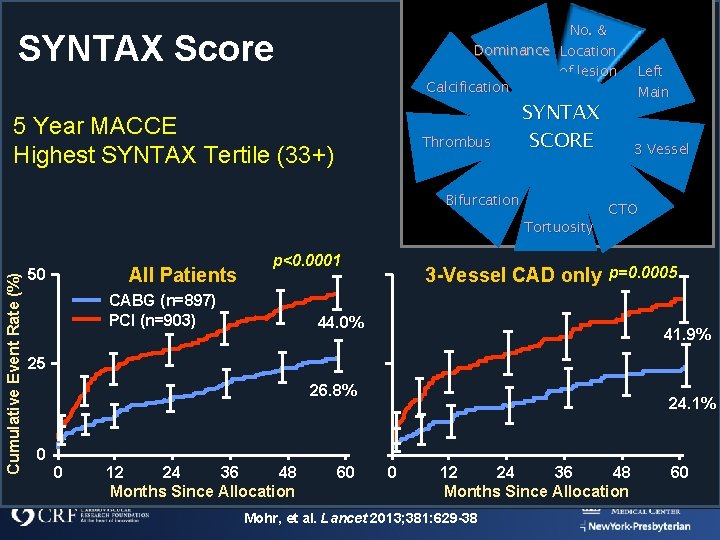
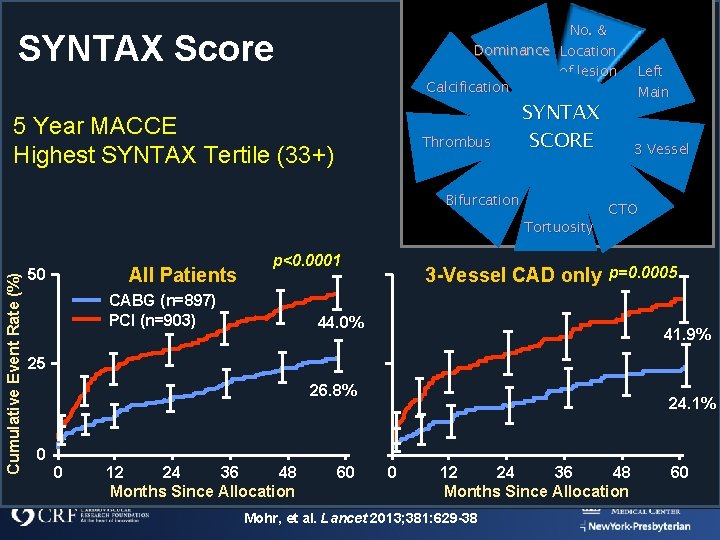
No. & Dominance Location of lesion Calcification SYNTAX Score 5 Year MACCE Highest SYNTAX Tertile (33+) Thrombus SYNTAX SCORE Bifurcation Cumulative Event Rate (%) Tortuosity All Patients 50 p<0. 0001 CABG (n=897) PCI (n=903) 3 -Vessel CAD only Left Main 3 Vessel CTO p=0. 0005 44. 0% 41. 9% 25 26. 8% 0 0 12 24 36 48 Months Since Allocation 60 24. 1% 0 12 24 36 48 Months Since Allocation Mohr, et al. Lancet 2013; 381: 629 -38 60
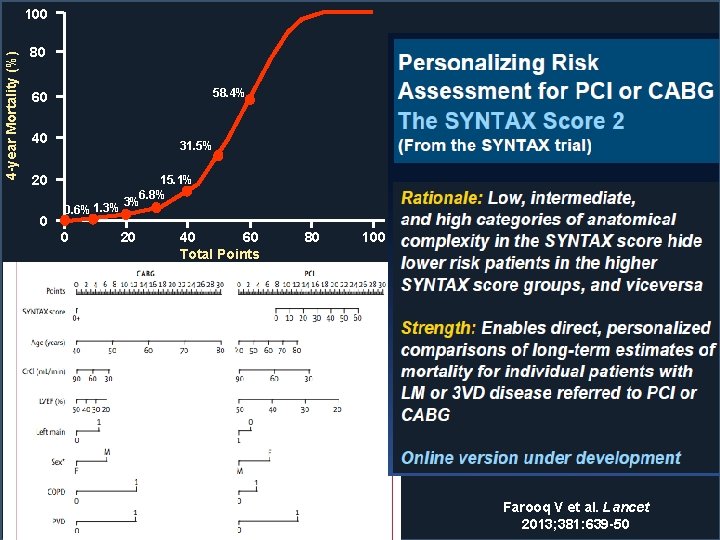
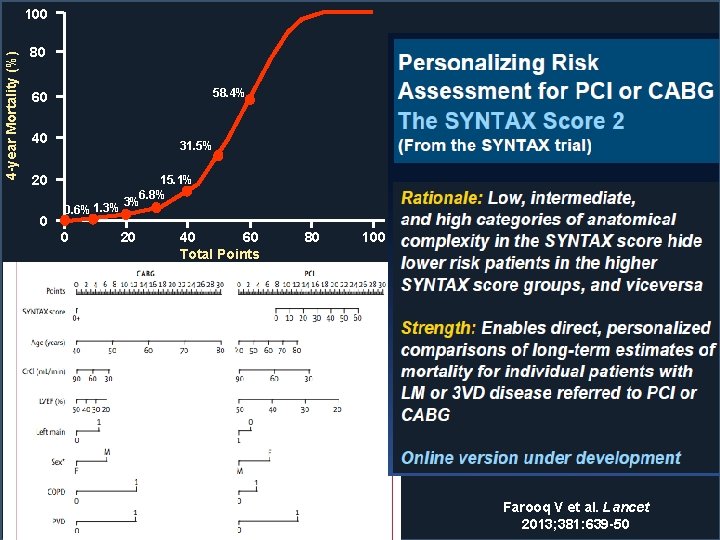
4 -year Mortality (%) 100 80 58. 4% 60 40 31. 5% 20 0 0. 6% 1. 3% 0 15. 1% 6. 8% 3% 20 40 60 Total Points 80 100 Farooq V et al. Lancet 2013; 381: 639 -50
MVD Pearls • Can I Completely Revascularize? (at least as well as the surgeon)
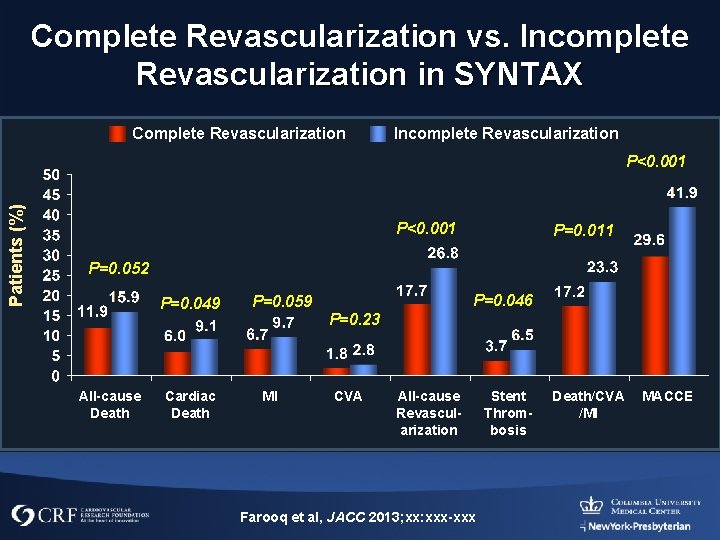
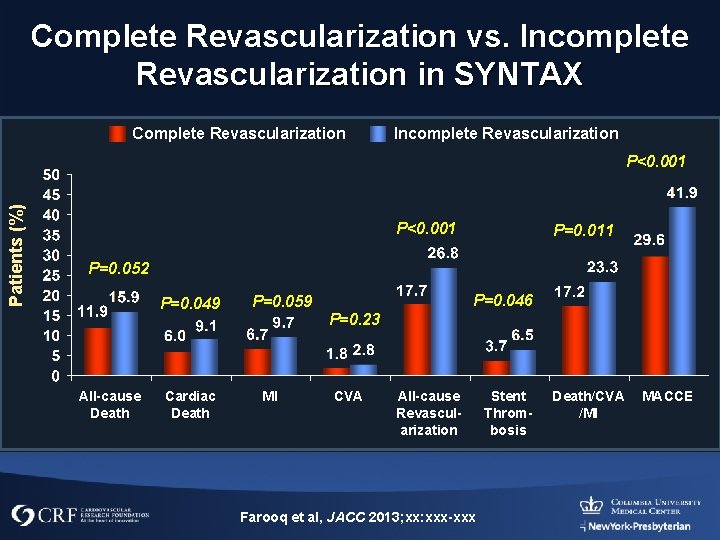
Complete Revascularization vs. Incomplete Revascularization in SYNTAX Complete Revascularization Incomplete Revascularization Patients (%) P<0. 001 P=0. 011 P=0. 052 P=0. 049 All-cause Death Cardiac Death P=0. 046 P=0. 059 P=0. 23 MI CVA All-cause Revascularization Farooq et al, JACC 2013; xx: xxx-xxx Stent Thrombosis Death/CVA /MI MACCE

Residual SS in SYNTAX Trial Low Baseline SYNTAX Score (0 -22) Estimated Event Rate 60% Residual SYNTAX Score 50% Log–rank P value. 022 Intermediate Baseline SYNTAX Score (23 -32) 60% 0 >0– 4 >4– 8 >8 50% Log–rank P value <. 001 60% Log–rank P value <. 001 50% 40% 30% 30% 20% 34. 1% High Baseline SYNTAX Score (≥ 33) 40% 39. 1% 23. 8% 20% 12. 9% 10. 1% 8. 2% 13. 8% 7. 7% 10% 6. 7% 0% 10% 0% 0 1 2 3 4 5 All-Cause Death (y) 11. 5% 10. 2% 9. 3% 10% 0% 0 1 2 3 4 5 All-Cause Death (y) Farooq Circ 2013; 128: 141 Kereiakes et al, Rev Cardiovasc Med. 2014; 15: 24 -30 0 1 2 3 4 5 All-Cause Death (y)
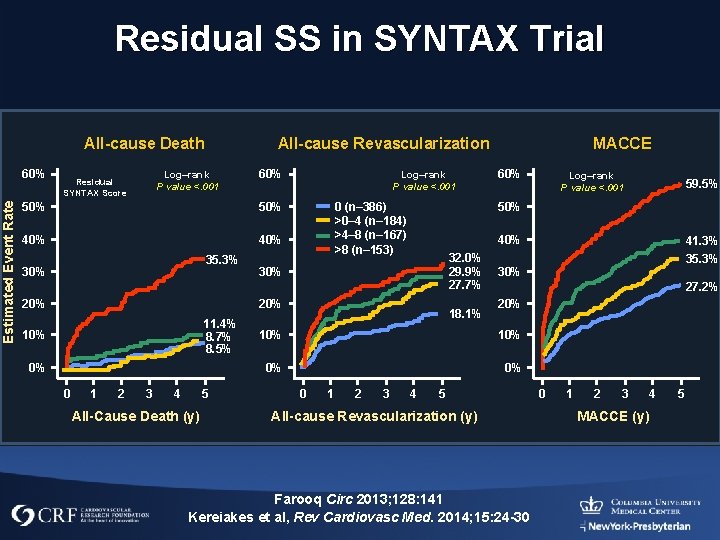
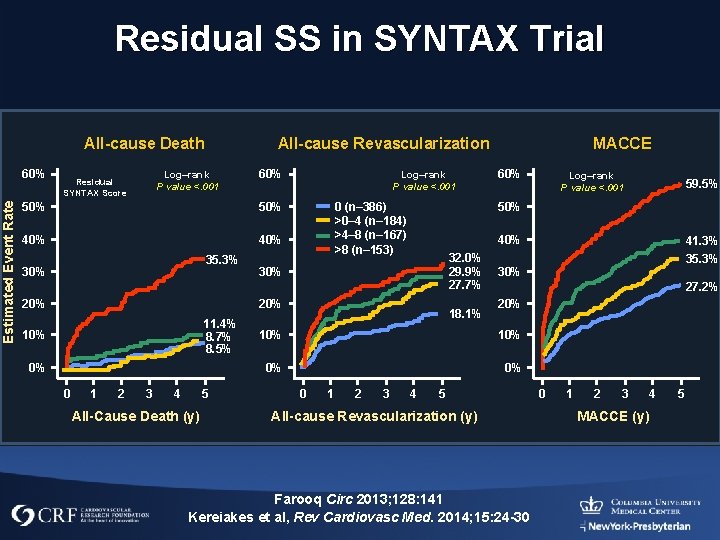
Residual SS in SYNTAX Trial All-cause Death Estimated Event Rate 60% All-cause Revascularization Log–rank P value <. 001 Residual SYNTAX Score 60% 50% 40% 35. 3% 30% 20% Log–rank P value <. 001 0 (n– 386) >0– 4 (n– 184) >4– 8 (n– 167) >8 (n– 153) 11. 4% 8. 7% 8. 5% 0% 0 1 2 3 4 5 All-Cause Death (y) 60% 32. 0% 29. 9% 27. 7% 18. 1% 20% 0% 0% 3 4 35. 3% 27. 2% 10% 2 41. 3% 30% 1 59. 5% 40% 30% 0 Log–rank P value <. 001 50% 20% 10% MACCE 5 All-cause Revascularization (y) Farooq Circ 2013; 128: 141 Kereiakes et al, Rev Cardiovasc Med. 2014; 15: 24 -30 0 1 2 3 MACCE (y) 4 5
MVD Pearls • Aggressively approach CTOs
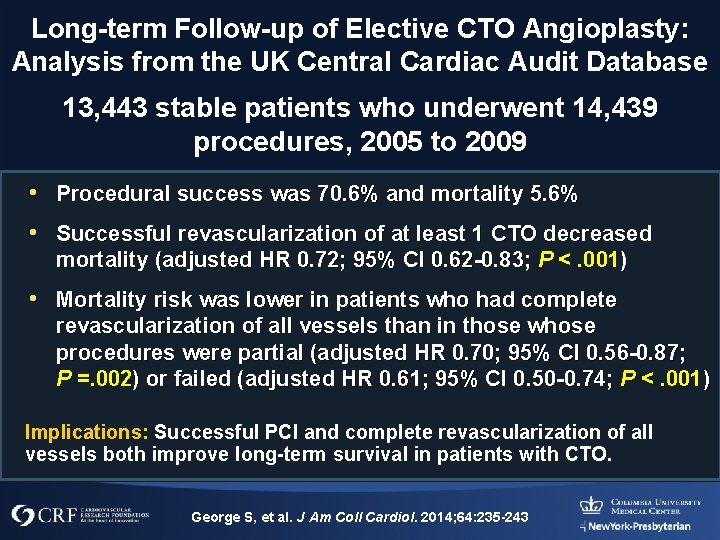
Long-term Follow-up of Elective CTO Angioplasty: Analysis from the UK Central Cardiac Audit Database 13, 443 stable patients who underwent 14, 439 procedures, 2005 to 2009 • Procedural success was 70. 6% and mortality 5. 6% • Successful revascularization of at least 1 CTO decreased mortality (adjusted HR 0. 72; 95% CI 0. 62 -0. 83; P <. 001) • Mortality risk was lower in patients who had complete revascularization of all vessels than in those whose procedures were partial (adjusted HR 0. 70; 95% CI 0. 56 -0. 87; P =. 002) or failed (adjusted HR 0. 61; 95% CI 0. 50 -0. 74; P <. 001) Implications: Successful PCI and complete revascularization of all vessels both improve long-term survival in patients with CTO. George S, et al. J Am Coll Cardiol. 2014; 64: 235 -243
MVD Pearls • SYNTAX score is not an absolute indicator of MACE especially with newer generation stents

SIRTAX: SYNTAX Score Is Not a Measure of Absolute Risk: Different Stent, Different Outcomes MACE 1 Y 50 SES P=0. 46 P=0. 98 P=0. 001 40 30 23. 9 20 10 0 6. 6 60 9. 0 7. 3 7. 5 8. 6 CSSLOW CSSMID CSSHIGH n=283 n=282 n=283 50 DEATH 1 Y % 60 SES P=0. 95 P=0. 35 P=0. 21 1. 5 1. 4 0. 70. 0 4. 9 2. 1 40 30 20 10 0 CSSLOW CSSMID CSSHIGH n=283 n=282 n=283 Girasis et al, Euro Heart J 2011; “in press”
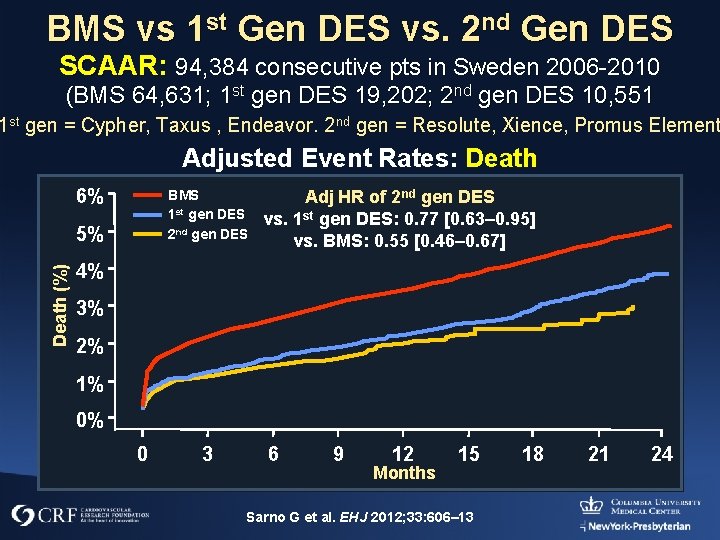
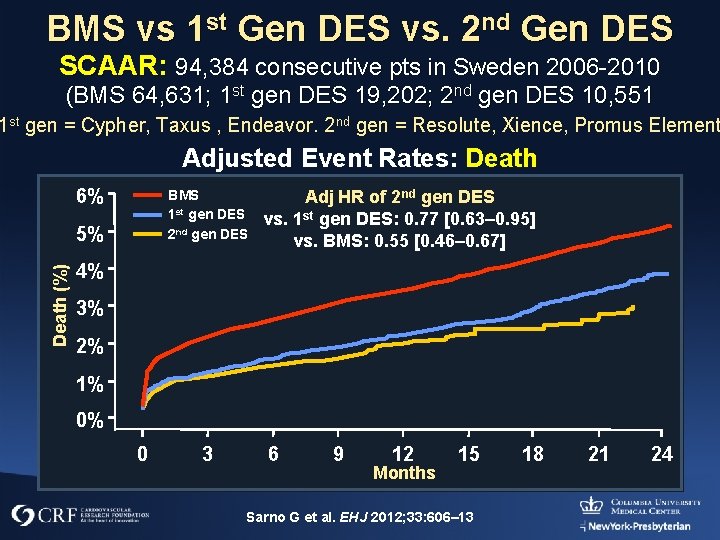
BMS vs 1 st Gen DES vs. 2 nd Gen DES SCAAR: 94, 384 consecutive pts in Sweden 2006 -2010 (BMS 64, 631; 1 st gen DES 19, 202; 2 nd gen DES 10, 551 1 st gen = Cypher, Taxus , Endeavor. 2 nd gen = Resolute, Xience, Promus Element Adjusted Event Rates: Death 6% BMS 1 st gen DES 2 nd gen DES Death (%) 5% Adj HR of 2 nd gen DES vs. 1 st gen DES: 0. 77 [0. 63– 0. 95] vs. BMS: 0. 55 [0. 46– 0. 67] 4% 3% 2% 1% 0% 0 3 6 9 12 Months 15 Sarno G et al. EHJ 2012; 33: 606– 13 18 21 24
MVD Pearls • Evaluate Diabetes in the overall context of the patient and anatomy
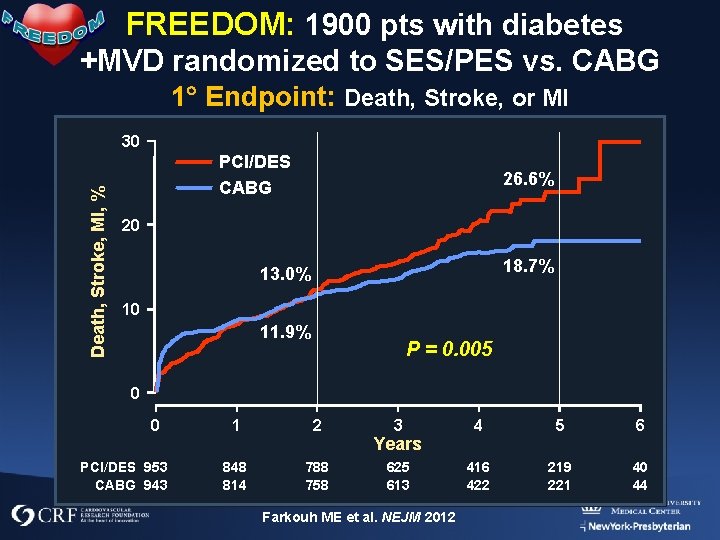
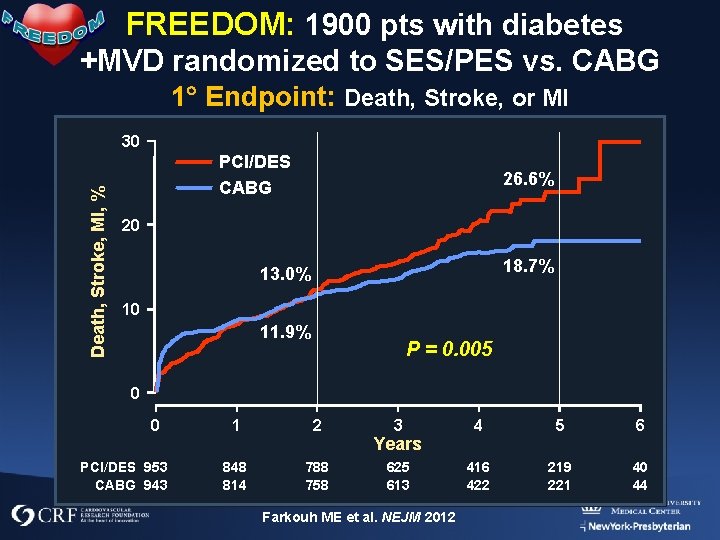
FREEDOM: 1900 pts with diabetes +MVD randomized to SES/PES vs. CABG 1 Endpoint: Death, Stroke, or MI Death, Stroke, MI, % 30 PCI/DES CABG 26. 6% 20 18. 7% 13. 0% 10 11. 9% P = 0. 005 0 0 PCI/DES 953 CABG 943 1 2 848 814 788 758 3 4 5 6 625 613 416 422 219 221 40 44 Years Farkouh ME et al. NEJM 2012
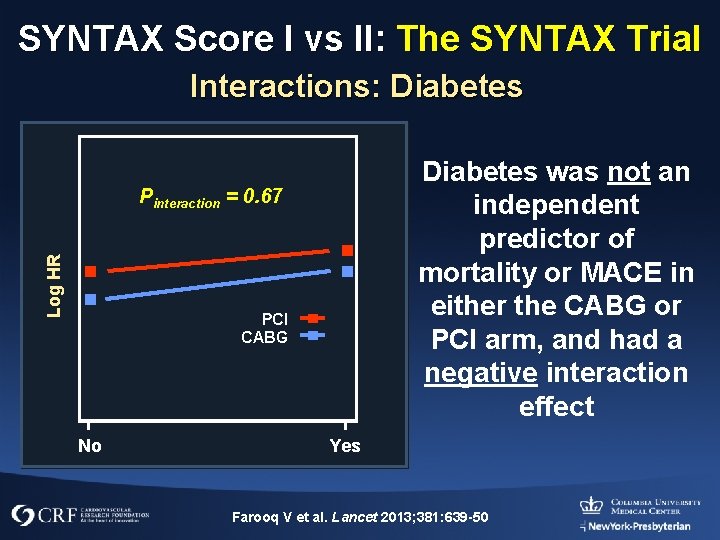
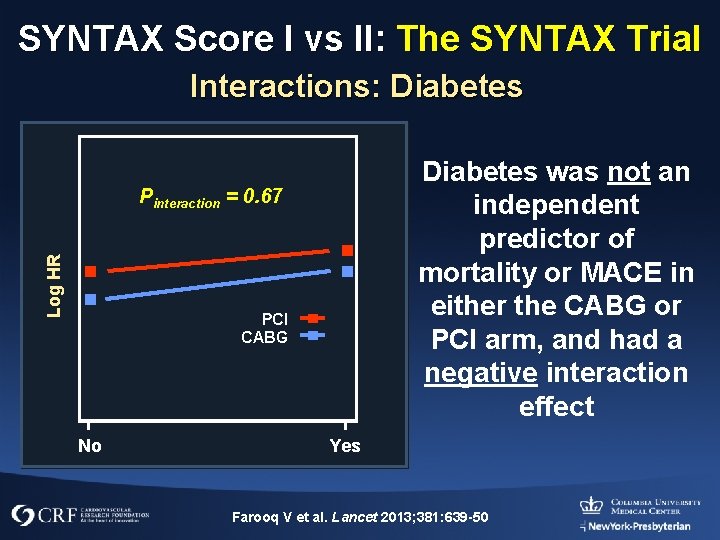
SYNTAX Score I vs II: The SYNTAX Trial Interactions: Diabetes was not an independent predictor of mortality or MACE in either the CABG or PCI arm, and had a negative interaction effect Log HR Pinteraction = 0. 67 PCI CABG No Yes Farooq V et al. Lancet 2013; 381: 639 -50
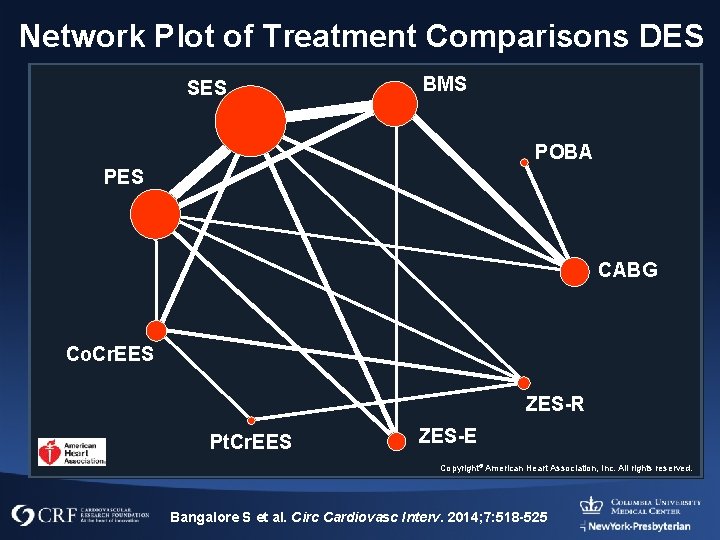
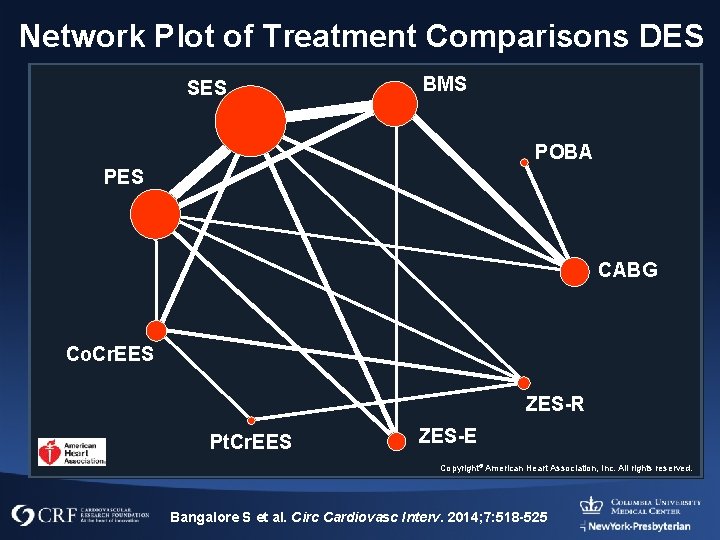
Network Plot of Treatment Comparisons DES SES BMS POBA PES CABG Co. Cr. EES ZES-R Pt. Cr. EES ZES-E Copyright© American Heart Association, Inc. All rights reserved. Bangalore S et al. Circ Cardiovasc Interv. 2014; 7: 518 -525
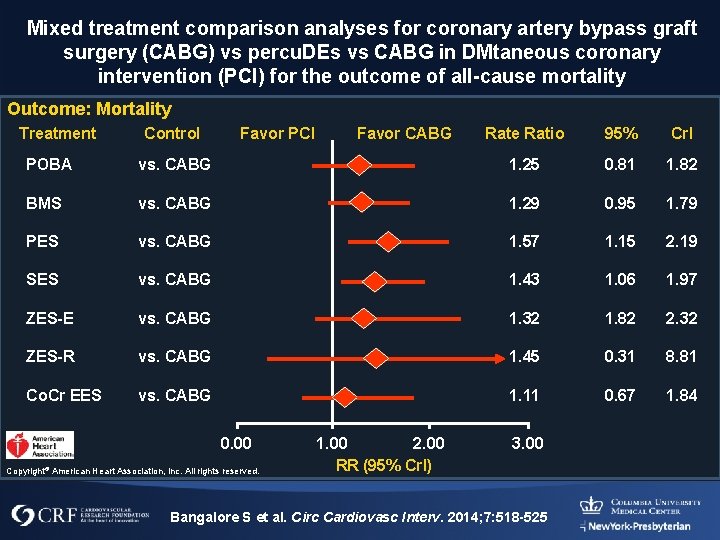
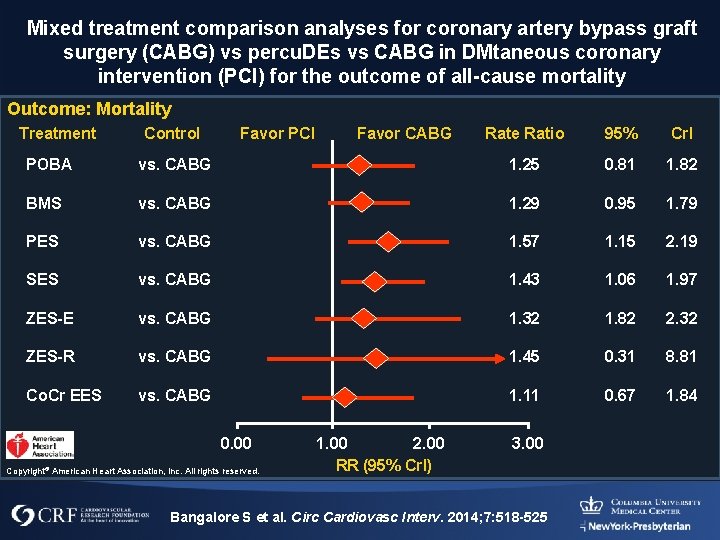
Mixed treatment comparison analyses for coronary artery bypass graft surgery (CABG) vs percu. DEs vs CABG in DMtaneous coronary intervention (PCI) for the outcome of all-cause mortality Outcome: Mortality Treatment Control Favor PCI Favor CABG Rate Ratio 95% Crl POBA vs. CABG 1. 25 0. 81 1. 82 BMS vs. CABG 1. 29 0. 95 1. 79 PES vs. CABG 1. 57 1. 15 2. 19 SES vs. CABG 1. 43 1. 06 1. 97 ZES-E vs. CABG 1. 32 1. 82 2. 32 ZES-R vs. CABG 1. 45 0. 31 8. 81 Co. Cr EES vs. CABG 1. 11 0. 67 1. 84 0. 00 Copyright© American Heart Association, Inc. All rights reserved. 1. 00 2. 00 RR (95% Crl) 3. 00 Bangalore S et al. Circ Cardiovasc Interv. 2014; 7: 518 -525
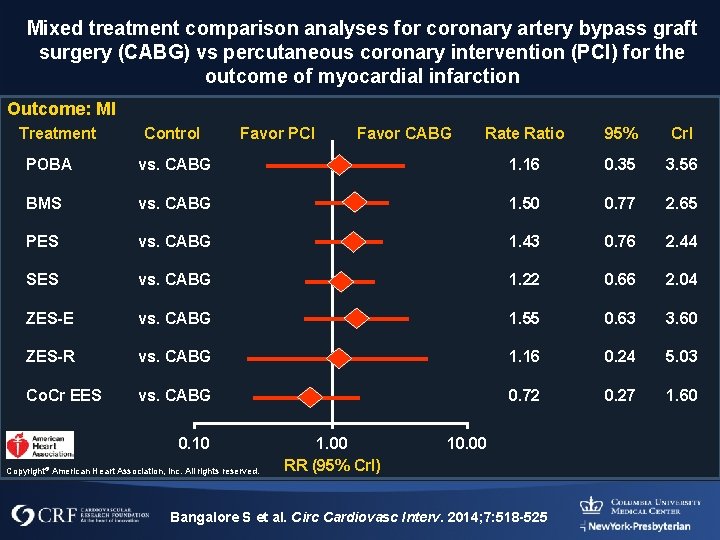
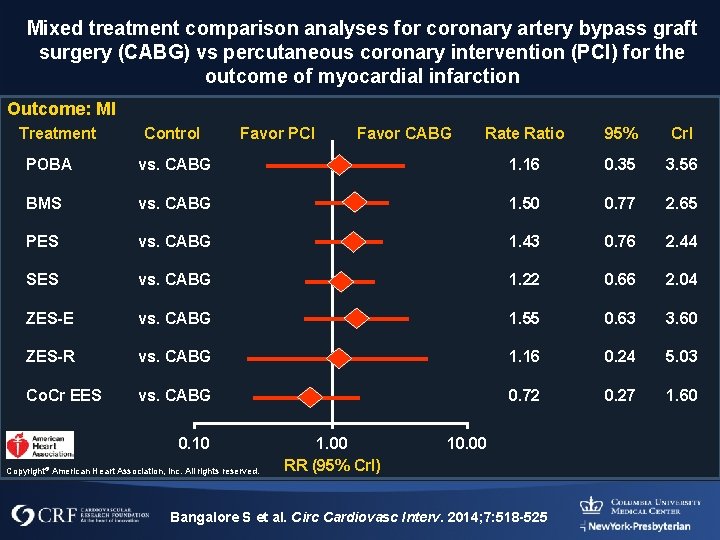
Mixed treatment comparison analyses for coronary artery bypass graft surgery (CABG) vs percutaneous coronary intervention (PCI) for the outcome of myocardial infarction Outcome: MI Treatment Control Favor PCI Favor CABG Rate Ratio 95% Crl POBA vs. CABG 1. 16 0. 35 3. 56 BMS vs. CABG 1. 50 0. 77 2. 65 PES vs. CABG 1. 43 0. 76 2. 44 SES vs. CABG 1. 22 0. 66 2. 04 ZES-E vs. CABG 1. 55 0. 63 3. 60 ZES-R vs. CABG 1. 16 0. 24 5. 03 Co. Cr EES vs. CABG 0. 72 0. 27 1. 60 0. 10 Copyright© American Heart Association, Inc. All rights reserved. 1. 00 RR (95% Crl) 10. 00 Bangalore S et al. Circ Cardiovasc Interv. 2014; 7: 518 -525
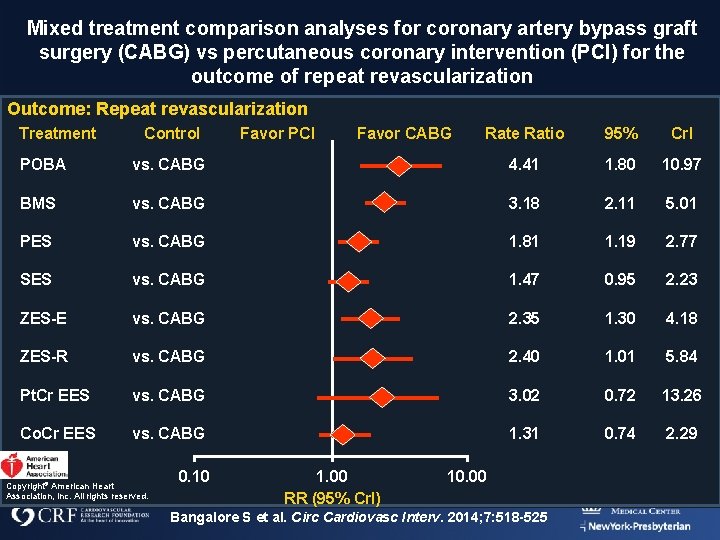
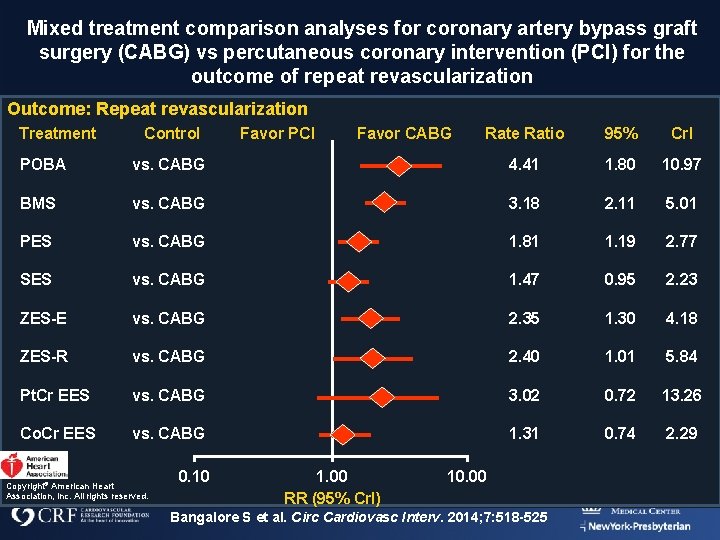
Mixed treatment comparison analyses for coronary artery bypass graft surgery (CABG) vs percutaneous coronary intervention (PCI) for the outcome of repeat revascularization Outcome: Repeat revascularization Treatment Control Favor PCI Favor CABG Rate Ratio 95% Crl POBA vs. CABG 4. 41 1. 80 10. 97 BMS vs. CABG 3. 18 2. 11 5. 01 PES vs. CABG 1. 81 1. 19 2. 77 SES vs. CABG 1. 47 0. 95 2. 23 ZES-E vs. CABG 2. 35 1. 30 4. 18 ZES-R vs. CABG 2. 40 1. 01 5. 84 Pt. Cr EES vs. CABG 3. 02 0. 72 13. 26 Co. Cr EES vs. CABG 1. 31 0. 74 2. 29 Copyright© American Heart Association, Inc. All rights reserved. 0. 10 1. 00 RR (95% Crl) 10. 00 Bangalore S et al. Circ Cardiovasc Interv. 2014; 7: 518 -525
MVD Pearls • Carefully decide on treatment order • If staging make sure to treat the “culprit” in the first session in symptomatic patients • Try to bootstrap for complex lesions to minimize risk of an ultracomplex vessel • For CTO consider treating donor vessel to allow for retrograde option
MVD Pearls • Optimize lesion preparation ¡ MVD has a higher propensity for calcification ¡ Think • Angiosculpt, CB • Roto, Orbital
MVD Pearls • Rational use of hemodynamic support

When Do I Consider Support? • Last Remaining Vessel • Severe LV dysfunction: support for ischemic stress and contrast load • LV dysfunction with prospect of uncontrolled interruption of coronary flow ¡ Difficult wiring ¡ Difficult stent delivery ¡ High risk of no reflow (i. e. , SVGs, Roto, thrombus)
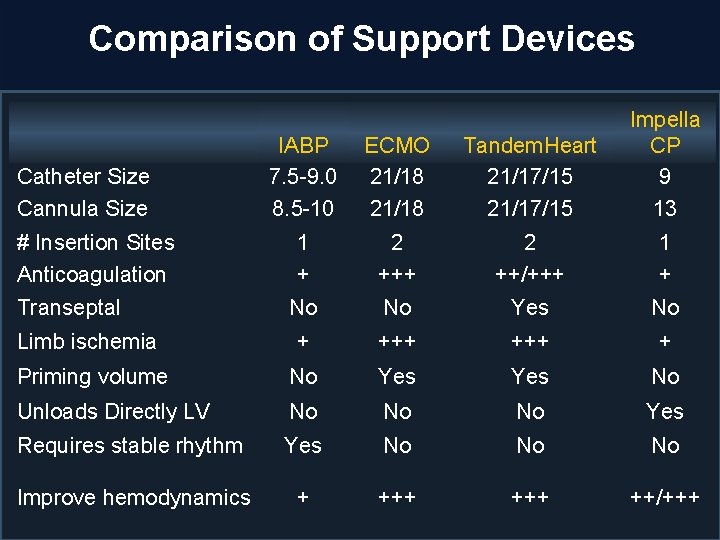
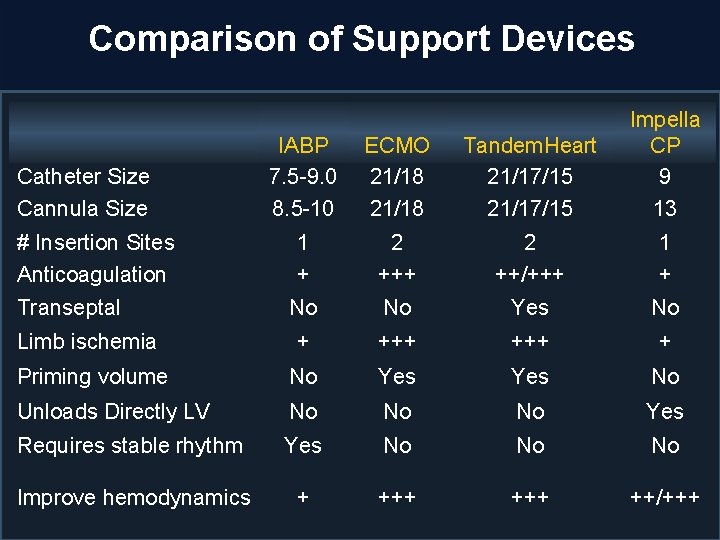
Comparison of Support Devices IABP 7. 5 -9. 0 8. 5 -10 ECMO 21/18 Tandem. Heart 21/17/15 Impella CP 9 13 1 + 2 ++/+++ 1 + No No Yes No Limb ischemia + +++ + Priming volume No Yes No Unloads Directly LV No No No Yes Requires stable rhythm Yes No No No Improve hemodynamics + +++ ++/+++ Catheter Size Cannula Size # Insertion Sites Anticoagulation Transeptal
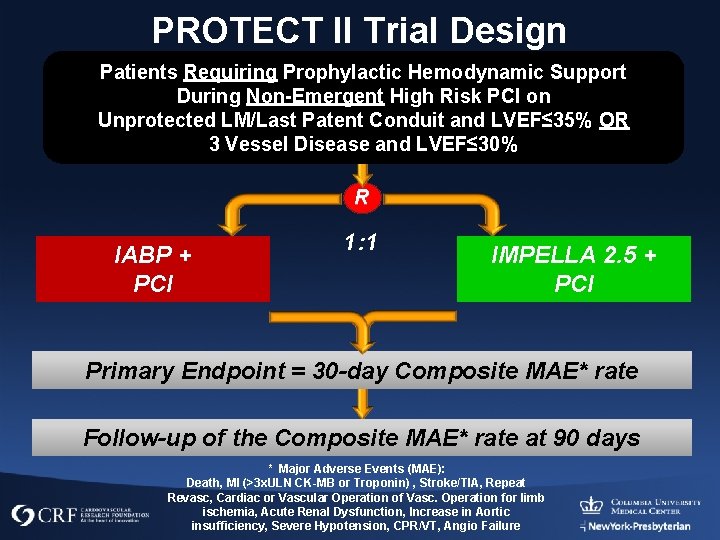
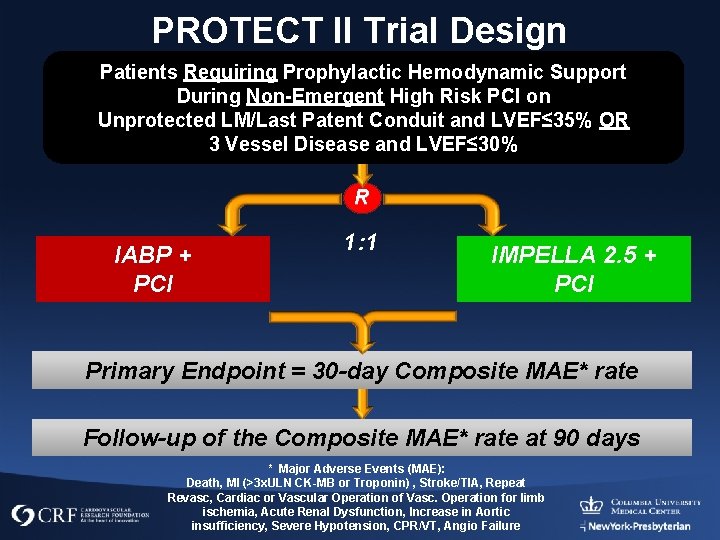
PROTECT II Trial Design Patients Requiring Prophylactic Hemodynamic Support During Non-Emergent High Risk PCI on Unprotected LM/Last Patent Conduit and LVEF≤ 35% OR 3 Vessel Disease and LVEF≤ 30% R IABP + PCI 1: 1 IMPELLA 2. 5 + PCI Primary Endpoint = 30 -day Composite MAE* rate Follow-up of the Composite MAE* rate at 90 days * Major Adverse Events (MAE): Death, MI (>3 x. ULN CK-MB or Troponin) , Stroke/TIA, Repeat Revasc, Cardiac or Vascular Operation of Vasc. Operation for limb ischemia, Acute Renal Dysfunction, Increase in Aortic insufficiency, Severe Hypotension, CPR/VT, Angio Failure
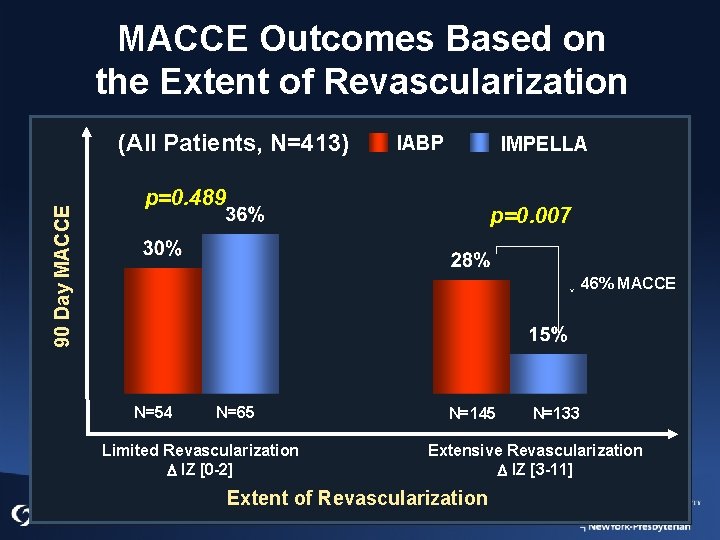
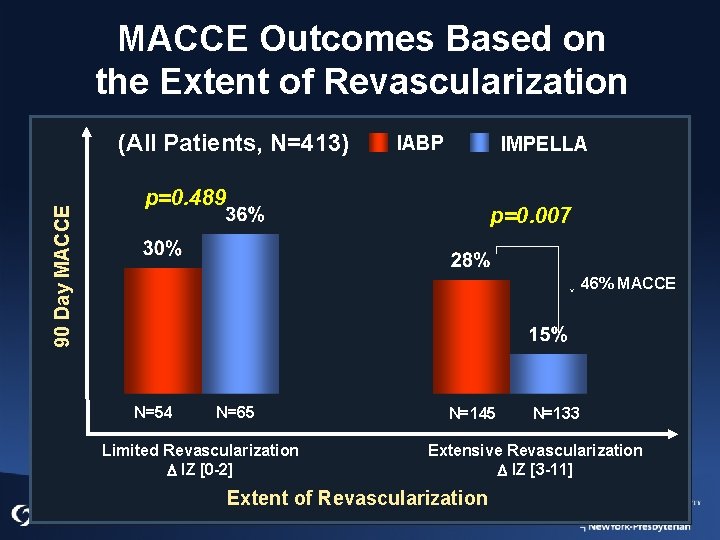
MACCE Outcomes Based on the Extent of Revascularization 90 Day MACCE (All Patients, N=413) IABP IMPELLA p=0. 489 p=0. 007 ↓ 46% MACCE N=54 N=65 Limited Revascularization D IZ [0 -2] N=145 N=133 Extensive Revascularization D IZ [3 -11] Extent of Revascularization
Be Prepared to Consider Certain Cases for PCI after Heart Team Evaluation • High CABG risk ¡ Low EF ¡ Severe COPD ¡ CKD ¡ Unusual comorbidities
MVD Pearls • Consider the patient’s point of view • While “Death and MI” may be key to clinical trialists the patient may believe otherwise
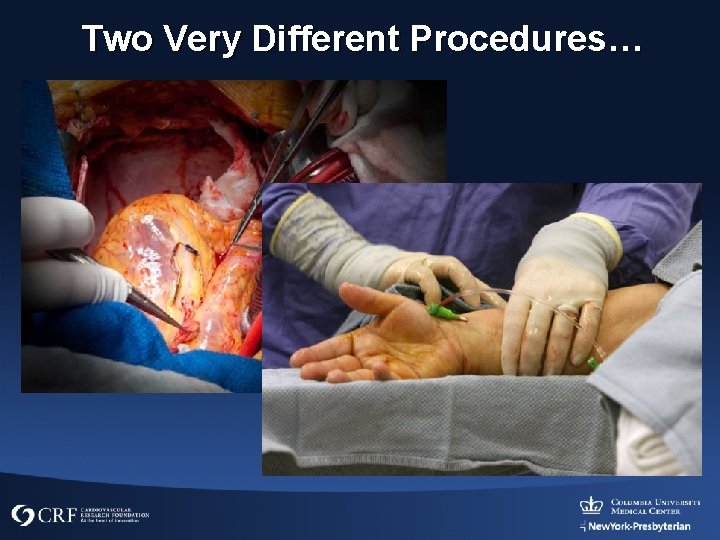
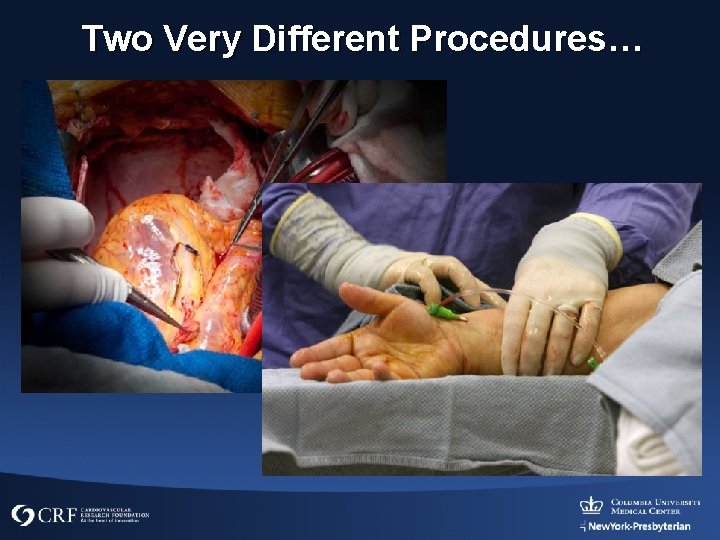
Two Very Different Procedures…
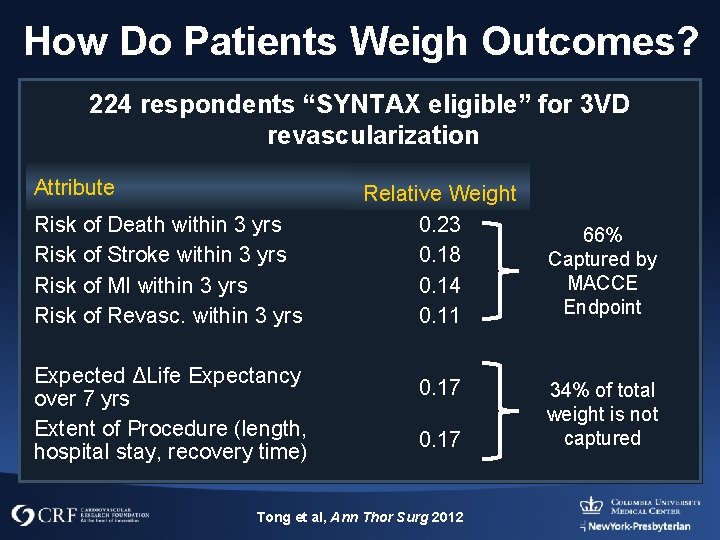
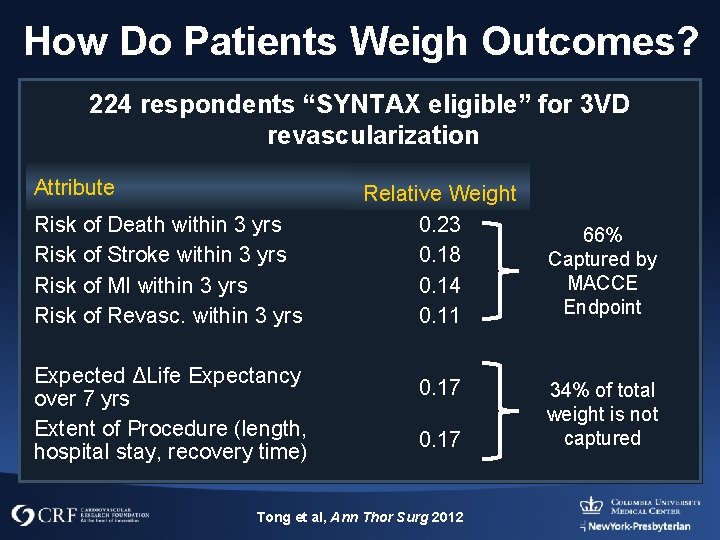
How Do Patients Weigh Outcomes? 224 respondents “SYNTAX eligible” for 3 VD revascularization Attribute Risk of Death within 3 yrs Risk of Stroke within 3 yrs Risk of MI within 3 yrs Risk of Revasc. within 3 yrs Expected ΔLife Expectancy over 7 yrs Extent of Procedure (length, hospital stay, recovery time) Relative Weight 0. 23 0. 18 0. 14 0. 11 0. 17 Tong et al, Ann Thor Surg 2012 66% Captured by MACCE Endpoint 34% of total weight is not captured

Scenario Presented PCI CABG 2 day 4 day 1 week 6 weeks Death 6% 3% MI 7% 3% CVA 3% 2% Revasc 20% 10% Hospital stay Recovery Life expectancy 0 1 year? Blinded – 83% CABG Open – 73% CABG PCI Choice: more familiarity with PCI, High socioeconomic status Tong et al, Ann Thor Surgery 2012; 94: 1908
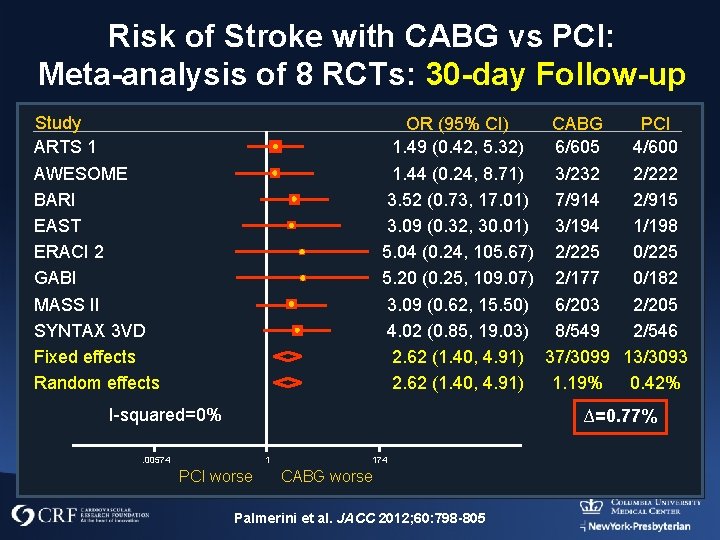
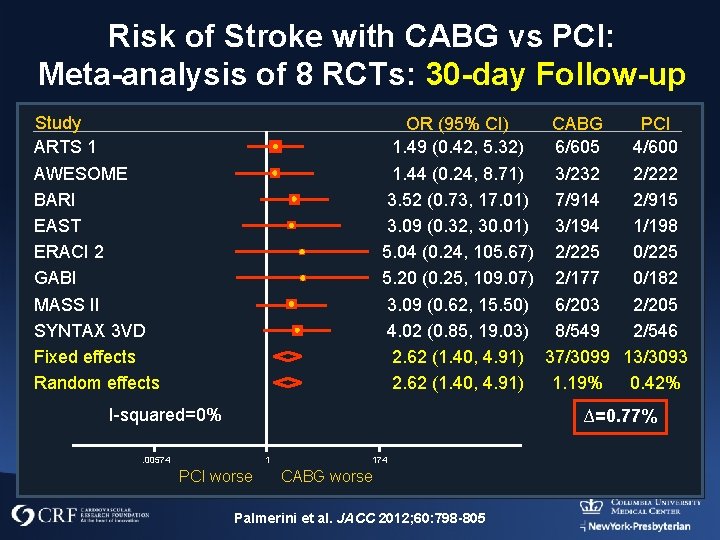
Risk of Stroke with CABG vs PCI: Meta-analysis of 8 RCTs: 30 -day Follow-up Study ARTS 1 AWESOME BARI EAST ERACI 2 GABI MASS II SYNTAX 3 VD Fixed effects Random effects OR (95% CI) CABG PCI 1. 49 (0. 42, 5. 32) 6/605 4/600 1. 44 (0. 24, 8. 71) 3/232 2/222 3. 52 (0. 73, 17. 01) 7/914 2/915 3. 09 (0. 32, 30. 01) 3/194 1/198 5. 04 (0. 24, 105. 67) 2/225 0/225 5. 20 (0. 25, 109. 07) 2/177 0/182 3. 09 (0. 62, 15. 50) 6/203 2/205 4. 02 (0. 85, 19. 03) 8/549 2/546 2. 62 (1. 40, 4. 91) 37/3099 13/3093 2. 62 (1. 40, 4. 91) 1. 19% 0. 42% I-squared=0% ∆=0. 77% 1 . 00574 PCI worse 174 CABG worse Palmerini et al. JACC 2012; 60: 798 -805
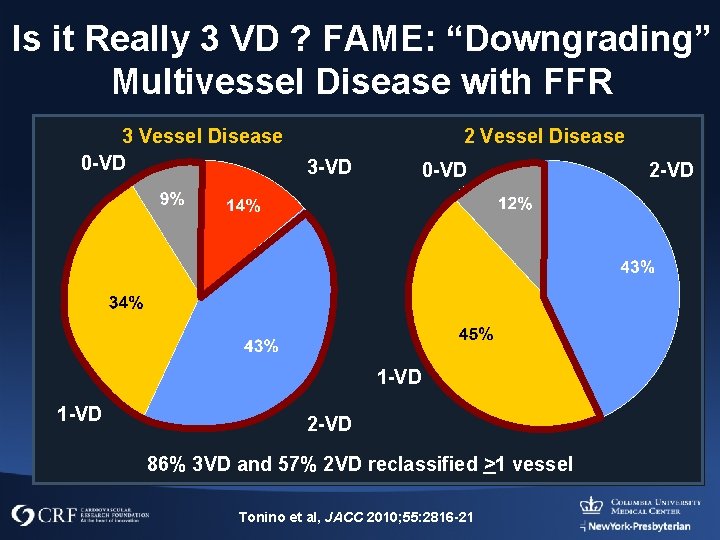
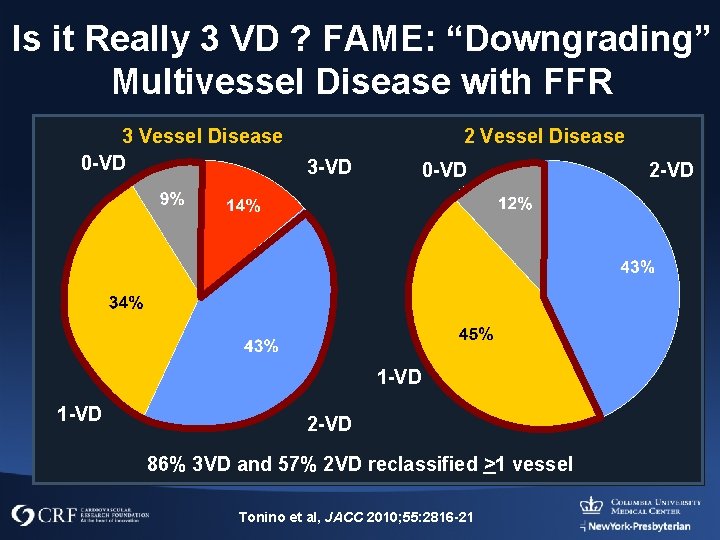
Is it Really 3 VD ? FAME: “Downgrading” Multivessel Disease with FFR 3 Vessel Disease 0 -VD 2 Vessel Disease 3 -VD 0 -VD 1 -VD 2 -VD 86% 3 VD and 57% 2 VD reclassified >1 vessel Tonino et al, JACC 2010; 55: 2816 -21 2 -VD
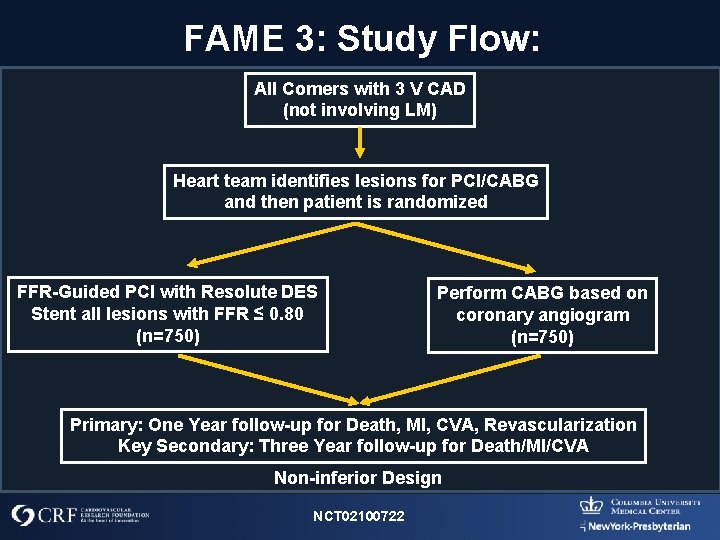
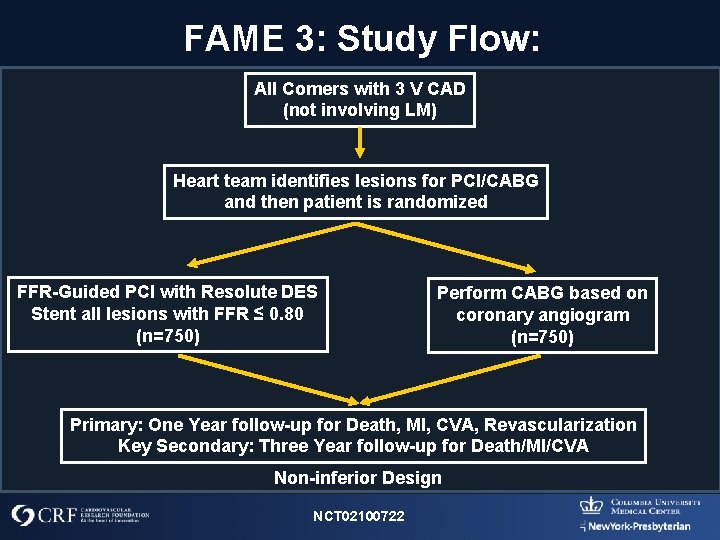
FAME 3: Study Flow: All Comers with 3 V CAD (not involving LM) Heart team identifies lesions for PCI/CABG and then patient is randomized FFR-Guided PCI with Resolute DES Stent all lesions with FFR ≤ 0. 80 (n=750) Perform CABG based on coronary angiogram (n=750) Primary: One Year follow-up for Death, MI, CVA, Revascularization Key Secondary: Three Year follow-up for Death/MI/CVA Non-inferior Design NCT 02100722
Conclusions • Multivessel PCI is appropriate for a large group of patients • Reflexive CABG referral is unwarranted • Careful assessment of patient, anatomy and treatment plan are essential for optimal results
 Godly wisdom vs worldly wisdom
Godly wisdom vs worldly wisdom Heavenly wisdom
Heavenly wisdom James 3 15 16
James 3 15 16 Your child's success or lack of success
Your child's success or lack of success Your child's success or lack of success
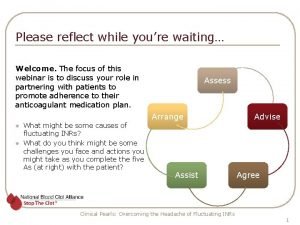
Your child's success or lack of success Clinical pearls
Clinical pearls Pearls kommunikation
Pearls kommunikation Stat pearls impact factor
Stat pearls impact factor Analisis pearls
Analisis pearls Pearl symbolism meaning
Pearl symbolism meaning Pharmacy clinical pearls
Pharmacy clinical pearls Is small skinny and black or brown in colour
Is small skinny and black or brown in colour Natural pearls are found in which creature
Natural pearls are found in which creature Twilight heucherella
Twilight heucherella Obgyn pearls
Obgyn pearls Pearls adalah
Pearls adalah Plastic packing pearls
Plastic packing pearls Pearls of sicily lido di noto
Pearls of sicily lido di noto Lsct np
Lsct np Rabindranath tagore taj mahal
Rabindranath tagore taj mahal Jill miller pci
Jill miller pci Pci magistrala
Pci magistrala Pci dss tutorial
Pci dss tutorial Datakiosk
Datakiosk Pci en salud
Pci en salud Pci-8330
Pci-8330 Pci tutorial
Pci tutorial Ranura agp
Ranura agp Jan jeventiin
Jan jeventiin Pci uex
Pci uex Redual pci
Redual pci Barramento pci
Barramento pci Pci en salud
Pci en salud Modle
Modle Pci class code
Pci class code What is concrete edge breakout
What is concrete edge breakout Gangorra geometria molecular
Gangorra geometria molecular Pci en salud
Pci en salud Microsoft from back doors patch gov
Microsoft from back doors patch gov Pci
Pci