Minimally Invasive Cardiac Surgery in Children Seoul National


- Slides: 18

Minimally Invasive Cardiac Surgery in Children Seoul National University Hospital Department of Thoracic & Cardiovascular Surgery

Minimally Invasive Cardiac Surgery in Children Seoul National University Hospital Department of Thoracic & Cardiovascular Surgery
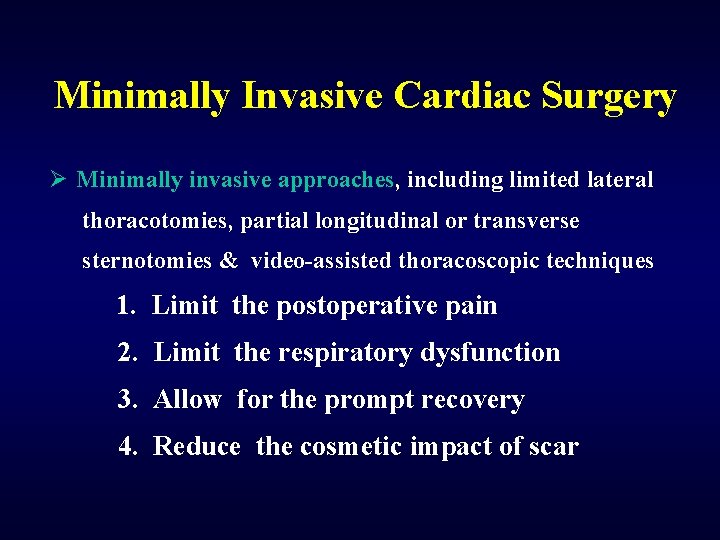
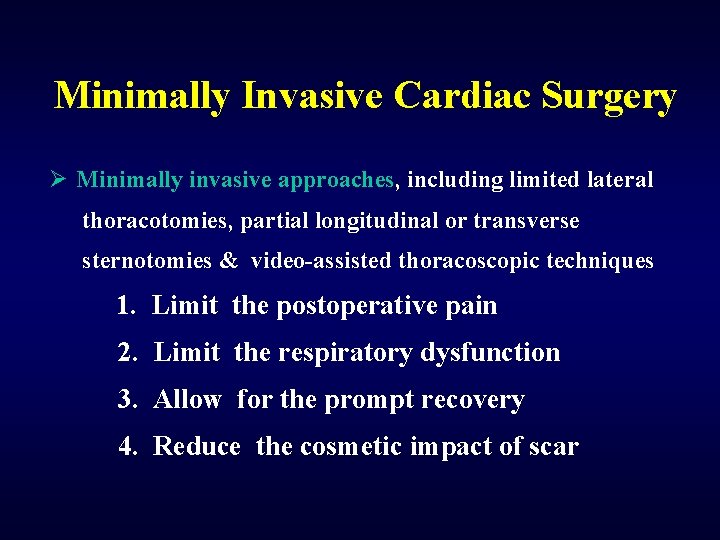
Minimally Invasive Cardiac Surgery Ø Minimally invasive approaches, including limited lateral thoracotomies, partial longitudinal or transverse sternotomies & video-assisted thoracoscopic techniques 1. Limit the postoperative pain 2. Limit the respiratory dysfunction 3. Allow for the prompt recovery 4. Reduce the cosmetic impact of scar
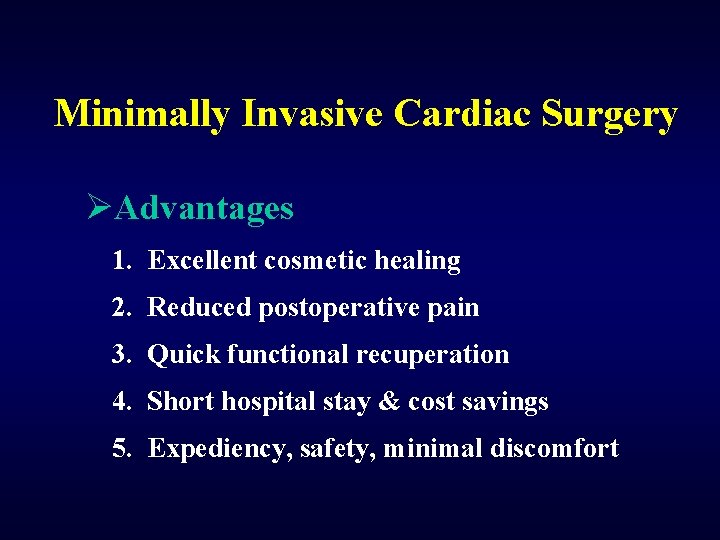
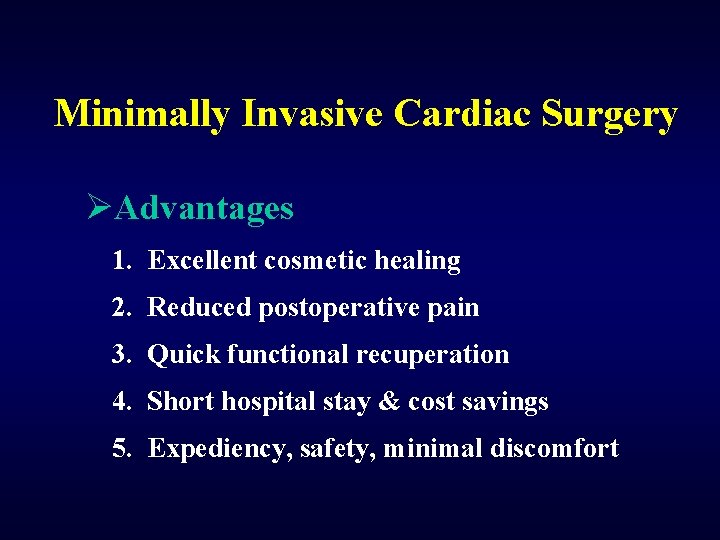
Minimally Invasive Cardiac Surgery ØAdvantages 1. Excellent cosmetic healing 2. Reduced postoperative pain 3. Quick functional recuperation 4. Short hospital stay & cost savings 5. Expediency, safety, minimal discomfort
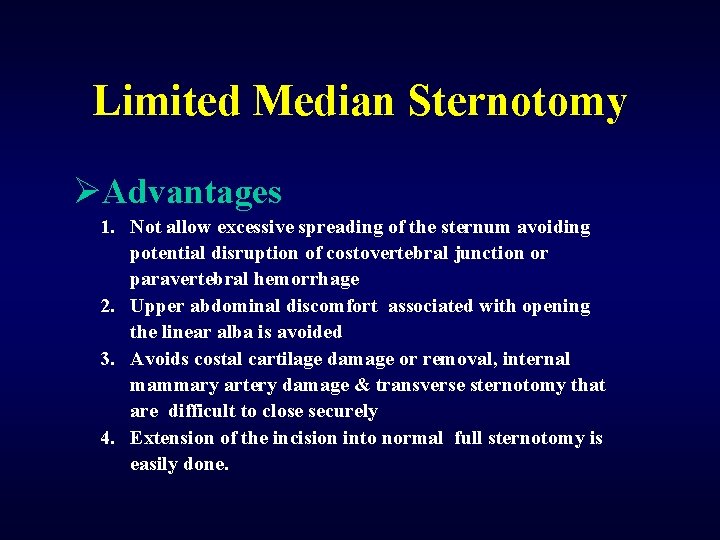
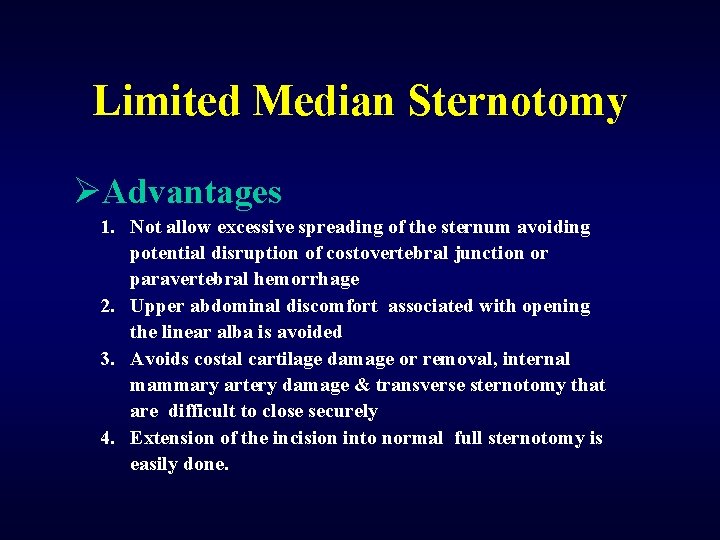
Limited Median Sternotomy ØAdvantages 1. Not allow excessive spreading of the sternum avoiding potential disruption of costovertebral junction or paravertebral hemorrhage 2. Upper abdominal discomfort associated with opening the linear alba is avoided 3. Avoids costal cartilage damage or removal, internal mammary artery damage & transverse sternotomy that are difficult to close securely 4. Extension of the incision into normal full sternotomy is easily done.
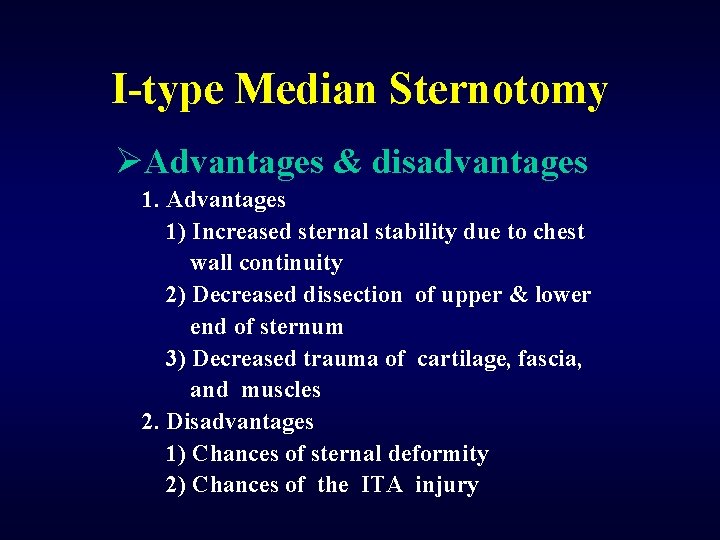
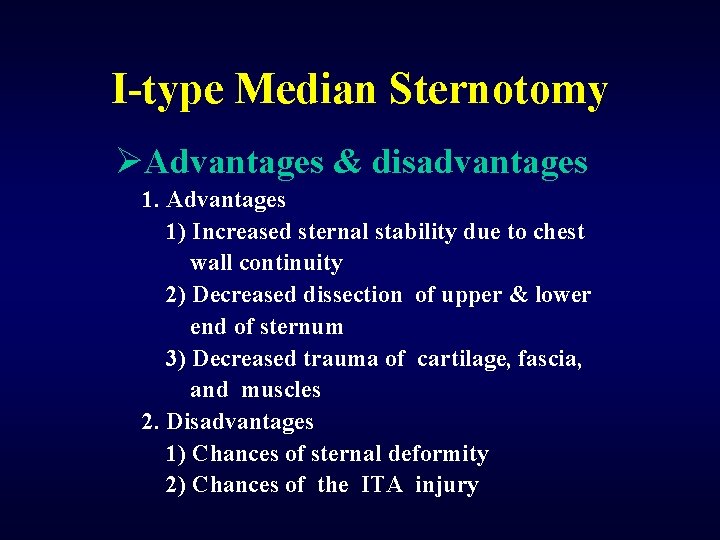
I-type Median Sternotomy ØAdvantages & disadvantages 1. Advantages 1) Increased sternal stability due to chest wall continuity 2) Decreased dissection of upper & lower end of sternum 3) Decreased trauma of cartilage, fascia, and muscles 2. Disadvantages 1) Chances of sternal deformity 2) Chances of the ITA injury
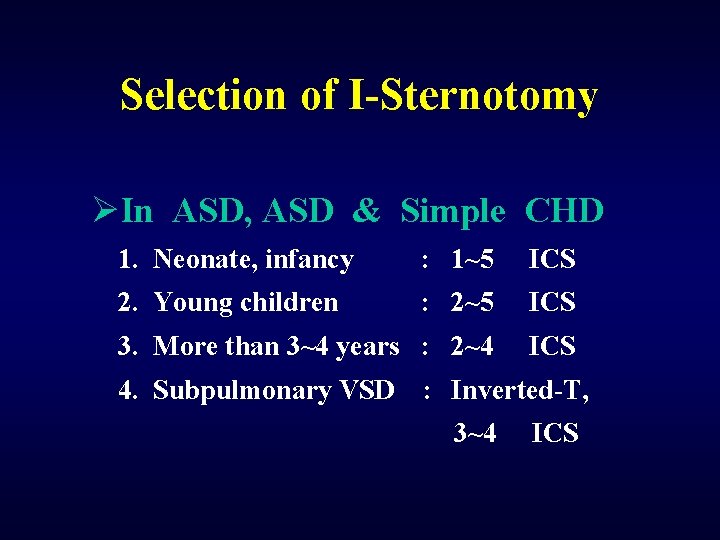
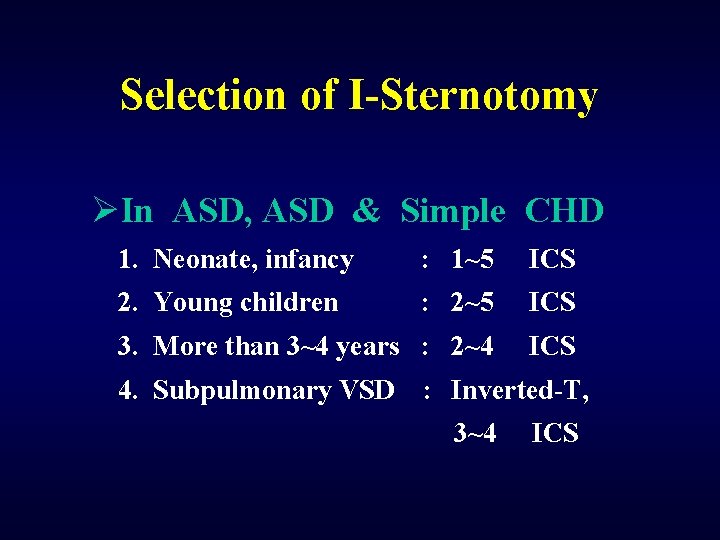
Selection of I-Sternotomy ØIn ASD, ASD & Simple CHD 1. Neonate, infancy : 1~5 ICS 2. Young children : 2~5 ICS 3. More than 3~4 years : 2~4 ICS 4. Subpulmonary VSD : Inverted-T, 3~4 ICS
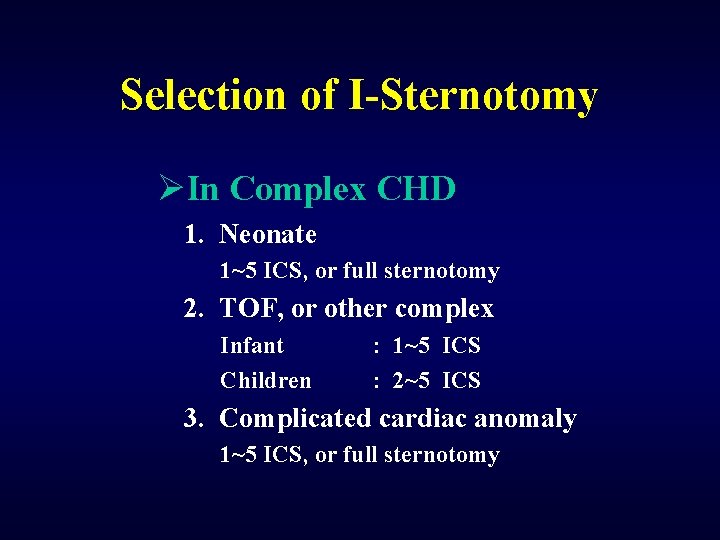
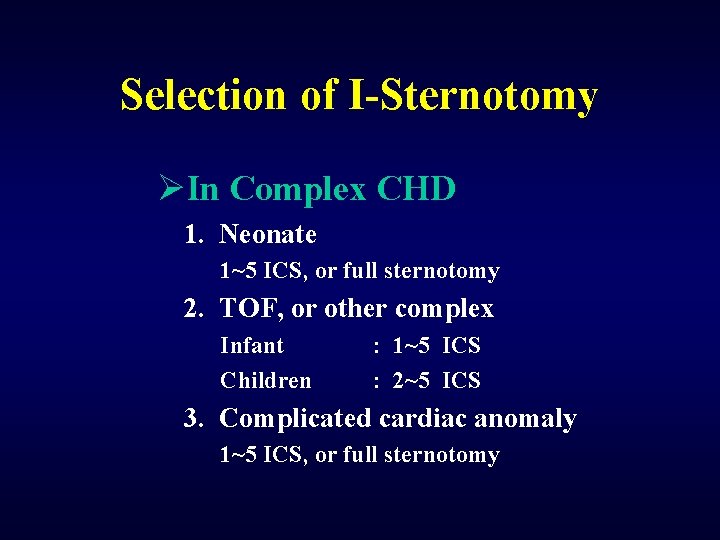
Selection of I-Sternotomy ØIn Complex CHD 1. Neonate 1~5 ICS, or full sternotomy 2. TOF, or other complex Infant Children : 1~5 ICS : 2~5 ICS 3. Complicated cardiac anomaly 1~5 ICS, or full sternotomy
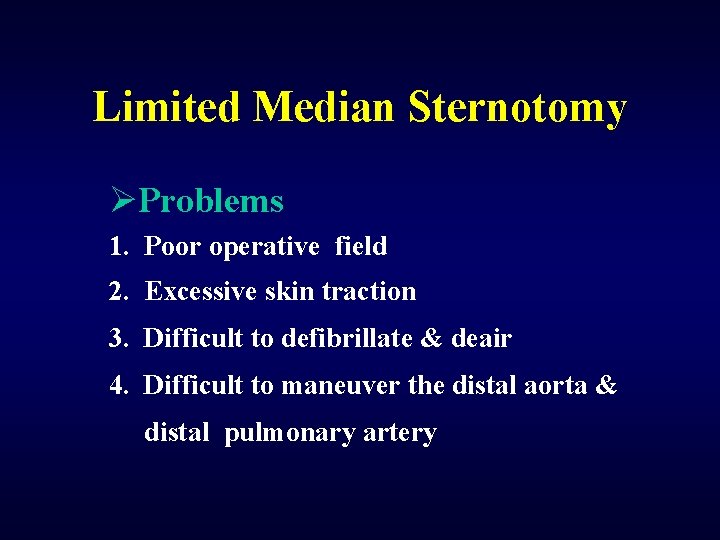
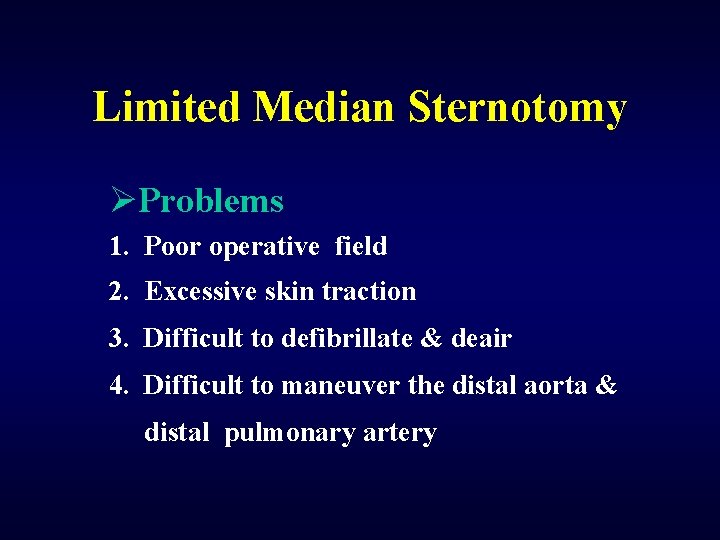
Limited Median Sternotomy ØProblems 1. Poor operative field 2. Excessive skin traction 3. Difficult to defibrillate & deair 4. Difficult to maneuver the distal aorta & distal pulmonary artery
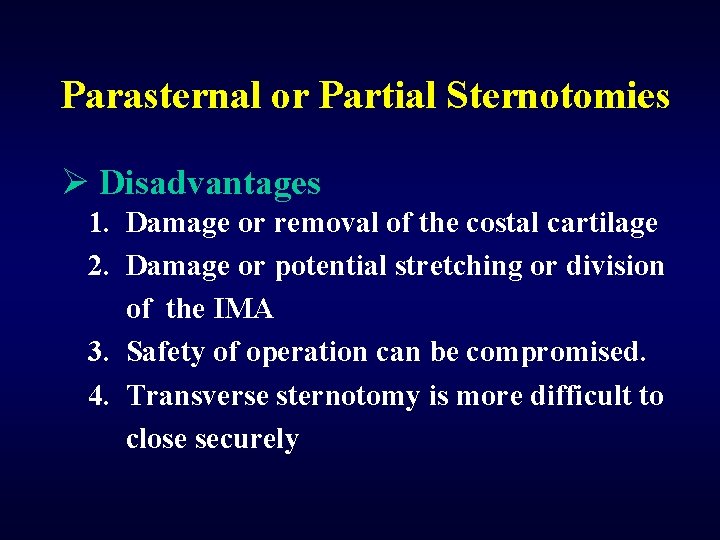
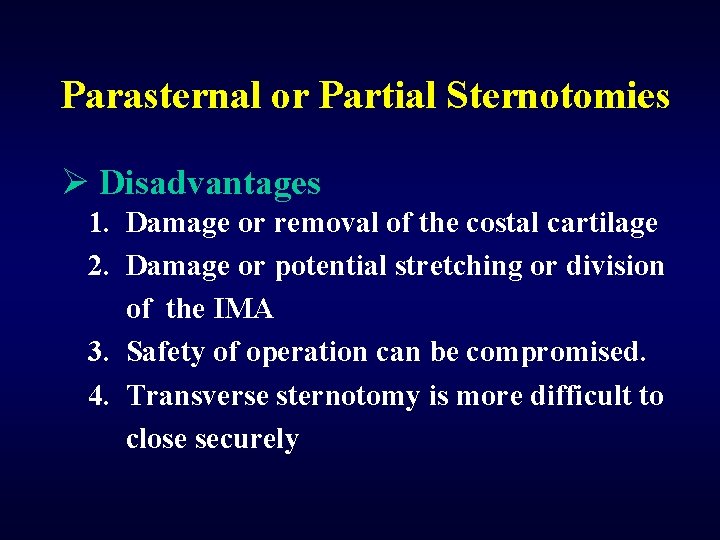
Parasternal or Partial Sternotomies Ø Disadvantages 1. Damage or removal of the costal cartilage 2. Damage or potential stretching or division of the IMA 3. Safety of operation can be compromised. 4. Transverse sternotomy is more difficult to close securely
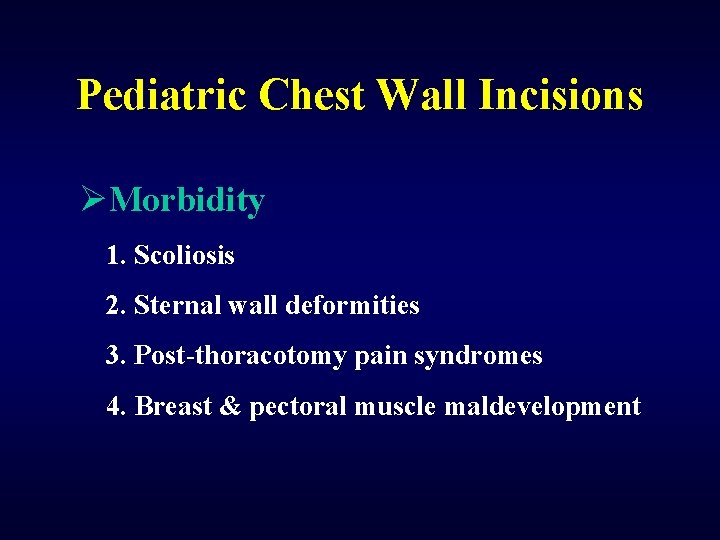
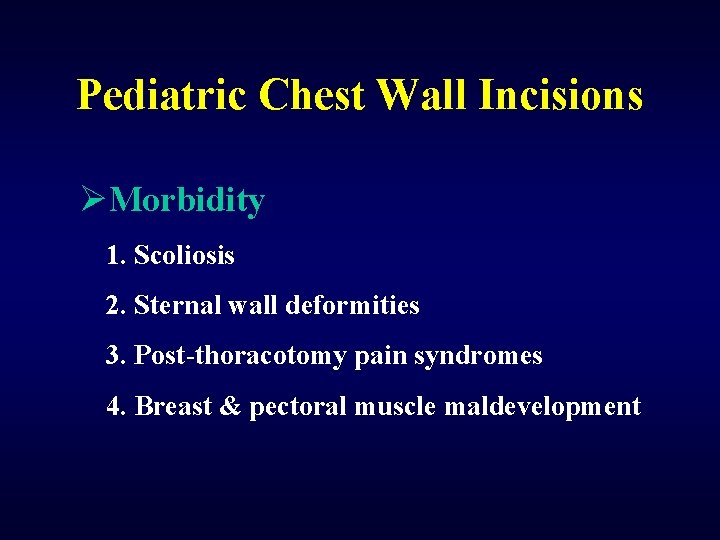
Pediatric Chest Wall Incisions ØMorbidity 1. Scoliosis 2. Sternal wall deformities 3. Post-thoracotomy pain syndromes 4. Breast & pectoral muscle maldevelopment
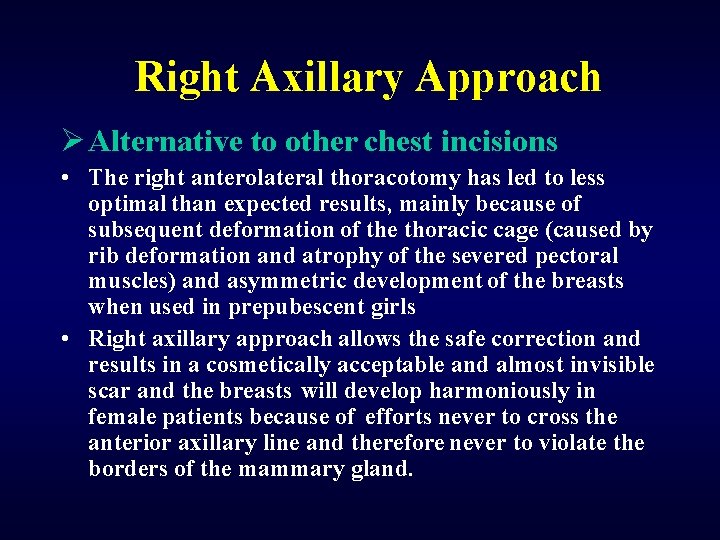
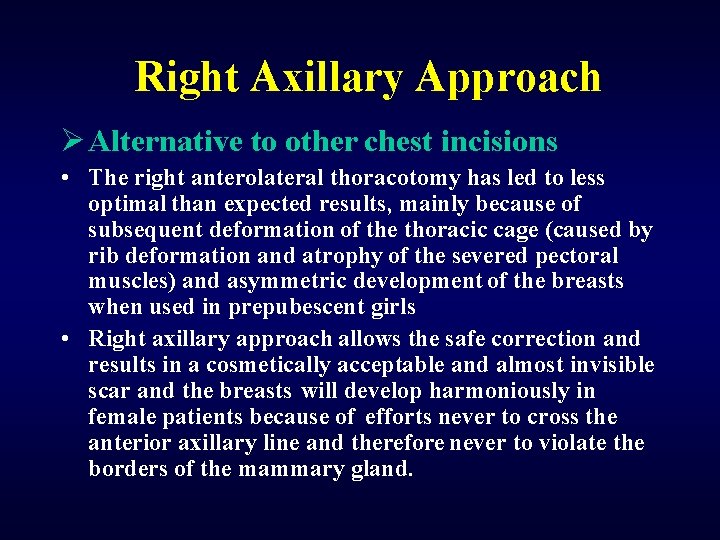
Right Axillary Approach Ø Alternative to other chest incisions • The right anterolateral thoracotomy has led to less optimal than expected results, mainly because of subsequent deformation of the thoracic cage (caused by rib deformation and atrophy of the severed pectoral muscles) and asymmetric development of the breasts when used in prepubescent girls • Right axillary approach allows the safe correction and results in a cosmetically acceptable and almost invisible scar and the breasts will develop harmoniously in female patients because of efforts never to cross the anterior axillary line and therefore never to violate the borders of the mammary gland.
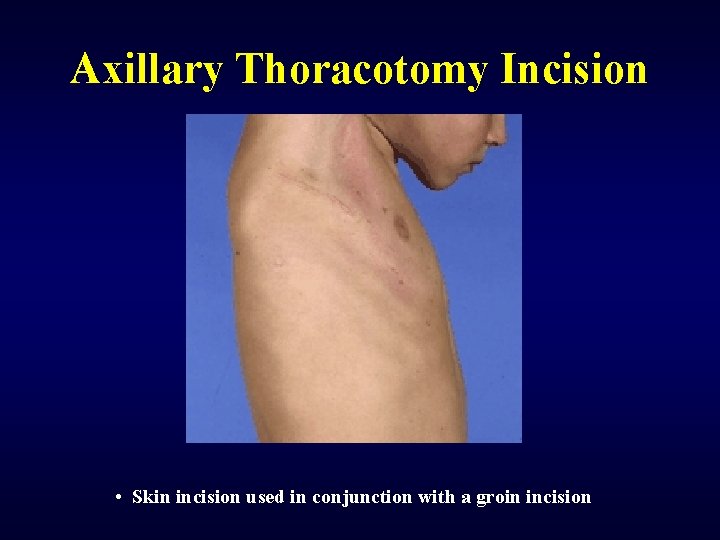
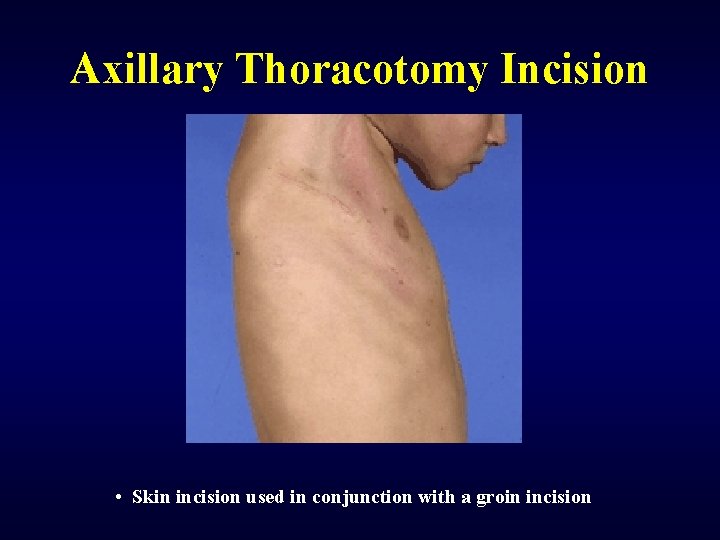
Axillary Thoracotomy Incision • Skin incision used in conjunction with a groin incision
Submammary Incision ØProblems 1. Sensory & sympathetic denervation 2. Hypesthesia of the anterior chest wall (38. 8%) 3 Decreased sensation & erection of nipples (12. 5%) 4. Risks of infection and ischemic or necrotic damage to the skin flaps 5. Clinical complications such as hematoma, seroma, hypertrophic scar or keloid formation, galactorrhea, mastodynia, & hypoesthesia
Right Thoracotomy Incision ØContraindications in CHD 1. 2. 3. 4. Pulmonary stenosis Severe pulmonary hypertension Age less than 2 years Patent ductus arteriosus & Lt SVC
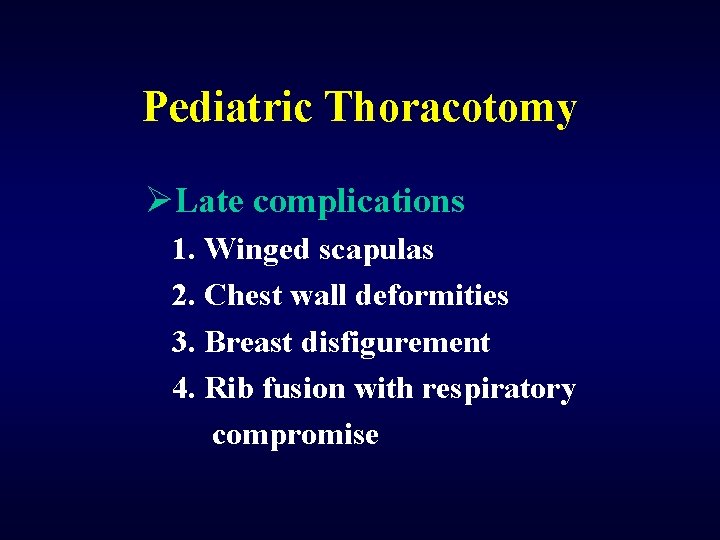
Pediatric Thoracotomy ØLate complications 1. Winged scapulas 2. Chest wall deformities 3. Breast disfigurement 4. Rib fusion with respiratory compromise
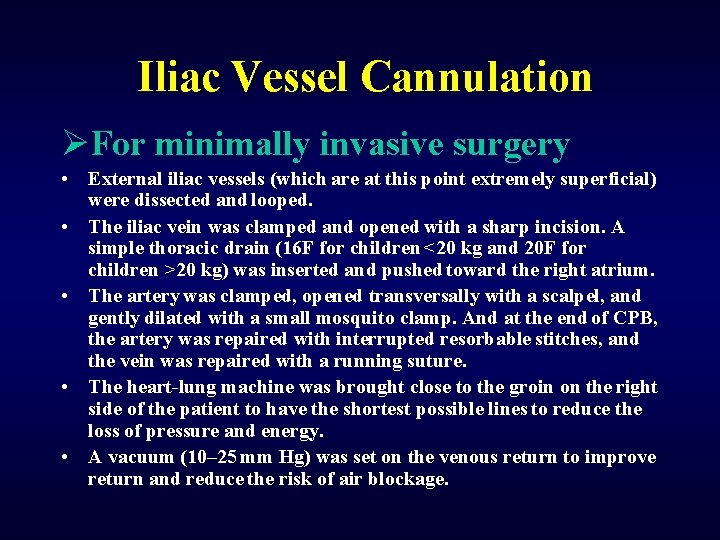
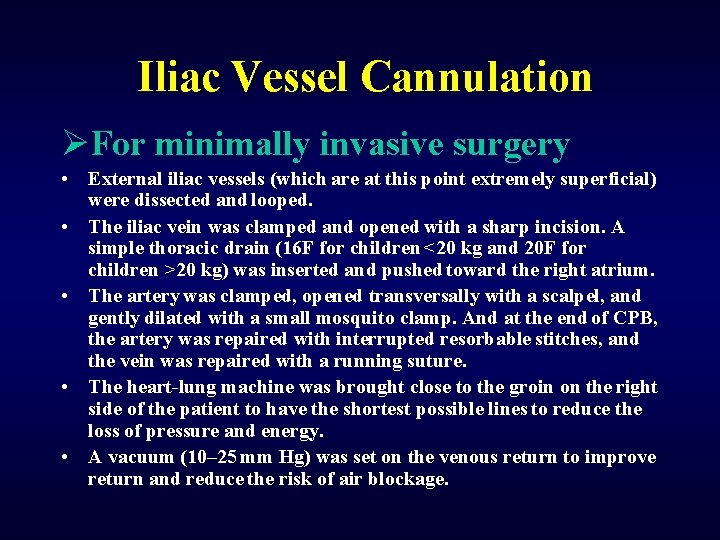
Iliac Vessel Cannulation ØFor minimally invasive surgery • External iliac vessels (which are at this point extremely superficial) were dissected and looped. • The iliac vein was clamped and opened with a sharp incision. A simple thoracic drain (16 F for children <20 kg and 20 F for children >20 kg) was inserted and pushed toward the right atrium. • The artery was clamped, opened transversally with a scalpel, and gently dilated with a small mosquito clamp. And at the end of CPB, the artery was repaired with interrupted resorbable stitches, and the vein was repaired with a running suture. • The heart-lung machine was brought close to the groin on the right side of the patient to have the shortest possible lines to reduce the loss of pressure and energy. • A vacuum (10– 25 mm Hg) was set on the venous return to improve return and reduce the risk of air blockage.
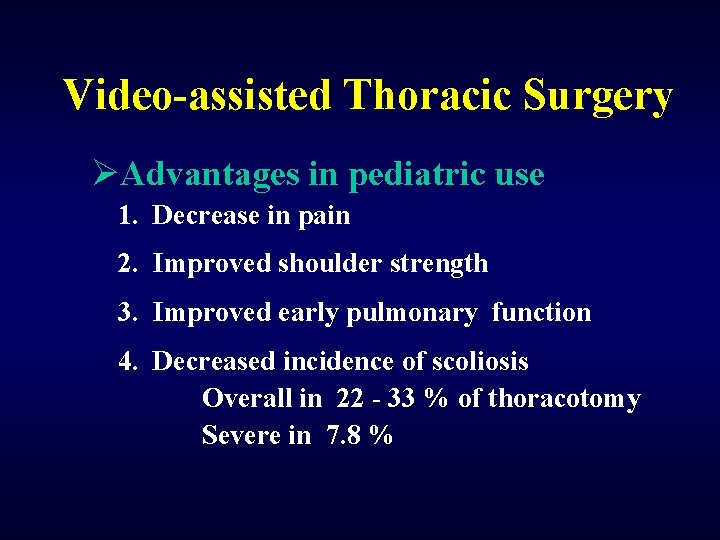
Video-assisted Thoracic Surgery ØAdvantages in pediatric use 1. Decrease in pain 2. Improved shoulder strength 3. Improved early pulmonary function 4. Decreased incidence of scoliosis Overall in 22 - 33 % of thoracotomy Severe in 7. 8 %
 Minimally invasive surgery
Minimally invasive surgery Minimally conscious state
Minimally conscious state Secondary action
Secondary action Seoul national university computer science
Seoul national university computer science Seoul national university medical school
Seoul national university medical school Exceptional control flow
Exceptional control flow Ebevlet
Ebevlet Seoul metro map
Seoul metro map Seoul semiconductor vina
Seoul semiconductor vina Undergraduate graduate postgraduate
Undergraduate graduate postgraduate Sunsangnim
Sunsangnim Seoul
Seoul Seoul metal vietnam
Seoul metal vietnam Công ty seoul semiconductor vina
Công ty seoul semiconductor vina Seoul idrc
Seoul idrc Seoul accord
Seoul accord Seoul
Seoul Exotic species definition
Exotic species definition Ontario invasive fish
Ontario invasive fish