Mental Health Issues of Veterans Returning from Iraq


- Slides: 26
Mental Health Issues of Veterans Returning from Iraq & Afghanistan Heather Brown, Ph. D Louis A Johnson VA Medical Ctr Clarksburg, WV Heather. Brown 4@va. gov
Following this presentation, the learner will: ¬identify specific combat issues impacting service members in Afghanistan and Iraq ¬state the mental health needs of Veterans and their families ¬understand the role of community providers in the readjustment process
Problems of returning service members seeking VA care: ¬ 1) Musculoskeletal diseases (joint and back), 43% ¬ 2) Mental health problems (higher in Guard/Reserves, non-officers), 36% ¬ 3) Signs and symptoms of ill-defined diseases, 33%
Mental Health problems of returning service members seeking VA care: ¬ 1) Adjustment Reactions (includes Post Traumatic Stress Disorder) ¬ 2) Drug abuse (includes nicotine) ¬ 3) Depression
Hidden Wounds: ¬Traumatic Brain Injuries (TBI) ¬Post-Traumatic Stress Disorder (PTSD)
Traumatic Brain Injuries (TBI): ¬ 80% of TBI cases are mild and involve no loss of consciousness ¬Primarily due to blast injuries ¬ 29% of battle evacuees had TBI
TBI (cont’d) ¬TBI and PTSD symptoms often overlap (sleep/memory problems, decreased concentration, mood disturbance) ¬Unrecognized TBI leads to poor psychosocial functioning ¬Have high suicide rates
TBI medical considerations ¬Use caution when sending TBI patients for MRI because of metal fragments (do CT scans first) ¬Wellbutrin and TBI may not mix (due to increased seizure risk) ¬If have genetic markers for Alzheimer’s disease, will develop sooner in TBI pts.
PTSD: ¬ 17% of the OEF/OIF population currently treated at VA are diagnosed with PTSD ¬Among new patients, PTSD rates are progressively higher than in previous years
Symptoms of PTSD (DSM V) 1. 2. 3. 4. 5. Exposure to actual or threatened death, serious injury, or sexual violence [i. e. , traumatic stressor] Presence of one (or more) intrusion symptoms associated with the traumatic event(s) [formerly, re-experiencing] Persistent avoidance of stimuli associated with the traumatic event(s) Negative alterations in cognitions and mood associated with the traumatic event(s) [new; formerly emotional numbing only] Marked alterations in arousal and reactivity associated with the traumatic event(s)
Substance Abuse ¬ 11 percent of OEF and OIF veterans have been diagnosed with a substance use disorder (SUD)— an alcohol use disorder, a drug use disorder, or both ¬ Almost 22 percent of OEF and OIF veterans with post-traumatic stress disorder (PTSD) also have an SUD ¬ SUD may co-occur with a mental health issue for “self-medication”
Facts about Veteran suicide • From the total noted deaths by suicide, 22 each day are Veterans (VA Suicide Data Report, 2012) • Veterans are more likely than the general population to use firearms as a means for suicide (National Violent Death Reporting System 2013) • 35 percent of recent Veteran suicides have a history of previous attempts (VA National Suicide Prevention Coordinator reports, 2012) • West Virginia’s total population is 1, 854, 304 (2013 approx. Census data) West Virginia has a total Veteran population of 170, 783 (Census 2010) West Virginia has a higher population of service members who serve or have served in the National Guard or Reserves
Operation S. A. V. E. will help you act with care and compassion if you encounter a Veteran who is in in distress or might be experiencing a suicidal crisis. The acronym “S. A. V. E. ” helps one remember the important steps involved in suicide prevention: Signs of suicidal thinking should be recognized Ask the most important question of all Validate the Veteran’s experience Encourage treatment and Expedite getting help
Signs of a person of concern Learn to recognize these warning signs: *Remember, it is commonly a combination of signs/symptoms rather than just one thing • Hopelessness, feeling like there’s no way out or no reason to live • Anxiety, agitation, sleeplessness or mood swings • Rage or anger • Engaging in risky activities without thinking
Signs of a person of concern (cont’d) • Increasing alcohol or drug abuse • Withdrawing from family and friends • Talking about death, dying or suicide • Over-focusing on giving valued belongings away and preparing for ones death (Not mindful preparation/planning of a person’s preference of arrangements following a natural death) • Overachieving, perfectionism (newer signs that clinicians are identifying)
Ask the Question & Validate the experience ¬ Are you thinking of suicide? ¬ Have you had thoughts about taking your own life? ¬ Are you thinking about killing yourself? ¬ Are you thinking of hurting yourself? ¬ Talk openly about suicide. Be willing to listen and allow the Veteran to express his or her feelings. ¬ Recognize that the situation is serious ¬ Do not pass judgment ¬ Reassure that help is available
Encourage treatment and Expedite getting help • Gently escort them to the closest professional person--let the person know that you would like to walk with them to find a professional that can help. (Complete a warm hand off to the next professional, explaining why you are there with the Veteran). • Alert the nearest staff person to assist you with the Veteran-you may wish to stay with the Veteran while the other staff person gets more help or next necessary level of care
Special issues of returning female service members: ¬Sexual Harassment ¬Sexual Assault ¬May not self-identify as “combat vets”
Family reintegration issues (after the “Honeymoon”): ¬Role changes (parenting, household responsibilities, etc. ) ¬Employment issues ¬Financial issues ¬Safety concerns

Family reintegration (cont’d) ¬Driving ¬Relationship w/spouse, children ¬Communication difficulties ¬Changes in support system
Seeking treatment (or not): ¬Stigma (military, cultural) ¬ 68% of OEF/OIF vets eligible for VA services have NOT sought treatment ¬Where are they? In the community!
Role of community providers: ¬Awareness of Veterans needing assistance in the community ¬Awareness of VA and Vet Centers as referral sources ¬Understanding of why service members may not seek treatment (i. e. , consequences) ¬Partner with local clergy
Role of health providers: ¬Primary care may be service members’ only contact with treatment ¬Screen for common mental health problems (e. g. , depression) ¬Ask about exposure to blast injuries, screen for TBI

VA Medical Centers in West Virginia ¬Clarksburg VAMC, 304 -623 -3461 ¬Martinsburg VAMC, 304 -263 -0811 ¬Beckley VAMC, 304 -255 -2121 ¬Huntington VAMC, 304 -429 -6741
Other VA treatment locations in WV ¬Community Based Outpatient Clinics (CBOC) [Multiple locations, including some rural counties] ¬Vet Centers [Beckley, Charleston, Huntington, Martinsburg, Morgantown, Princeton, Wheeling and outreach sites]
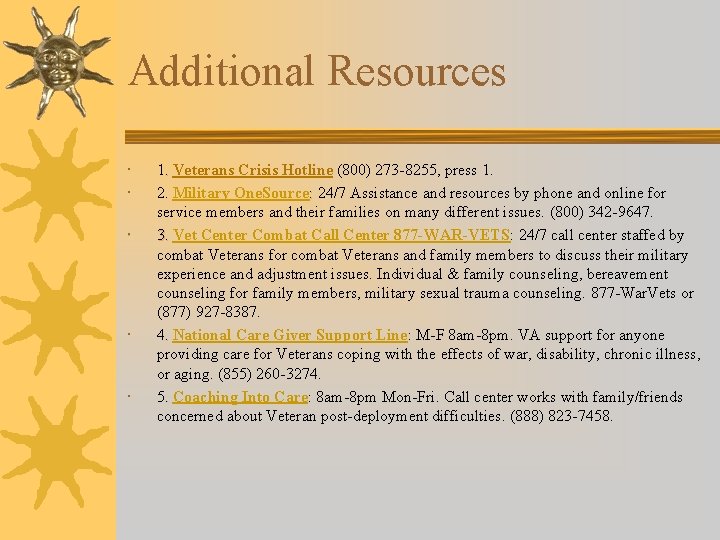
Additional Resources 1. Veterans Crisis Hotline (800) 273 -8255, press 1. 2. Military One. Source: 24/7 Assistance and resources by phone and online for service members and their families on many different issues. (800) 342 -9647. 3. Vet Center Combat Call Center 877 -WAR-VETS: 24/7 call center staffed by combat Veterans for combat Veterans and family members to discuss their military experience and adjustment issues. Individual & family counseling, bereavement counseling for family members, military sexual trauma counseling. 877 -War. Vets or (877) 927 -8387. 4. National Care Giver Support Line: M-F 8 am-8 pm. VA support for anyone providing care for Veterans coping with the effects of war, disability, chronic illness, or aging. (855) 260 -3274. 5. Coaching Into Care: 8 am-8 pm Mon-Fri. Call center works with family/friends concerned about Veteran post-deployment difficulties. (888) 823 -7458.
 Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy questions
Mental health jeopardy questions Veterans health administration organizational chart
Veterans health administration organizational chart Uccs health circle
Uccs health circle Bayang magiliw lyrics
Bayang magiliw lyrics A value-returning function is
A value-returning function is University of texas at tyler scholarships
University of texas at tyler scholarships Returning back to god
Returning back to god Powerschool huntsville
Powerschool huntsville Leaving returning it
Leaving returning it I conclude then returning to being feared and loved
I conclude then returning to being feared and loved Returning warrior workshop
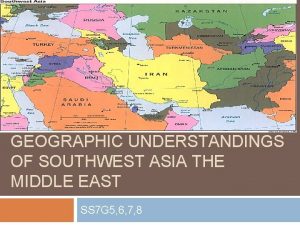
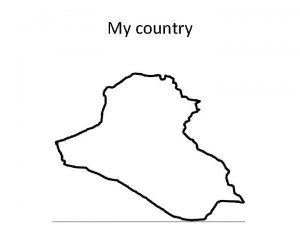
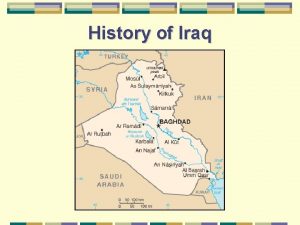
Returning warrior workshop Is iraq a landlocked country
Is iraq a landlocked country Iraq
Iraq What rivers run through iraq
What rivers run through iraq Iraq
Iraq Giz iraq
Giz iraq Iraq catering company
Iraq catering company Iraq
Iraq Iraq
Iraq Economic conditions
Economic conditions Muhammad ibn ya'qub al-kulayni
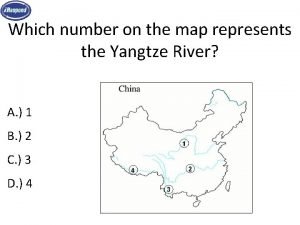
Muhammad ibn ya'qub al-kulayni Which number on the map shows the yangtze river?
Which number on the map shows the yangtze river? World map label
World map label Parade
Parade Iraq
Iraq Coalition definition
Coalition definition