Medical disengagement Christopher Dowrick Professor of Primary Medical



- Slides: 21

Medical disengagement Christopher Dowrick Professor of Primary Medical Care University of Liverpool, UK
Themes n n n Medically unexplained symptoms (MUS) in primary care Mismatch between help seeking and care received Medical disengagement
MUS are a problem n n Health care Doctors Patients Nosologists
Do doctors help, or hinder?
Research Team n n n Peter Salmon Chris Dowrick Adele Ring John Davies Gerry Humphris Larry Wissow n Liverpool n Dundee Johns Hopkins n
Principal Question n What strategies do patients with unexplained physical symptoms, and their doctors, use to influence treatment decisions? ¡ ¡ Somatic Psychosocial
Study summary n n 9 primary care sites on Merseyside, UK 42 general practitioners transcripts of 420 MUS consultations Liverpool Clinical Interaction Analysis Scheme n Ring et al, Soc Sci Med 2005
Key findings (1) n Patient presentations perceived as pressure ¡ n Normalisation by GPs common, but counterproductive ¡ n Ring et al, BMJ 2004 Dowrick et al, Br J Gen Pract 2004 Patients less dualistic than previously assumed ¡ Salmon et al, Br J Gen Pract 2004
Key findings (2) n Patients seek support > treatment ¡ n Salmon et al, J Psychosom Res 2005 Mismatch between help seeking and care n ‘Medical somatisation’ ¡ Ring et al, Soc Sci Med 2005
Psychosocial agendas voiced…. n 61% (of 420) referred to emotional or social problems ¡ ¡ n 41% by direct disclosure 41% by suggesting psychosocial explanations 70% requested explanations for their symptoms ¡ Only 9% did neither
…. but often unheard n n n In 67% consultations, doctors indicated physical disease could be present In only 16% did doctors make empathic statements Doctors more likely than patients to propose symptomatic management
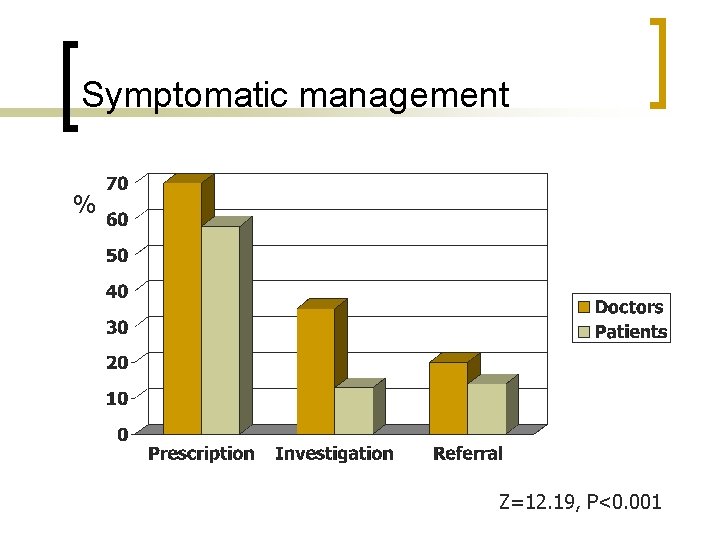
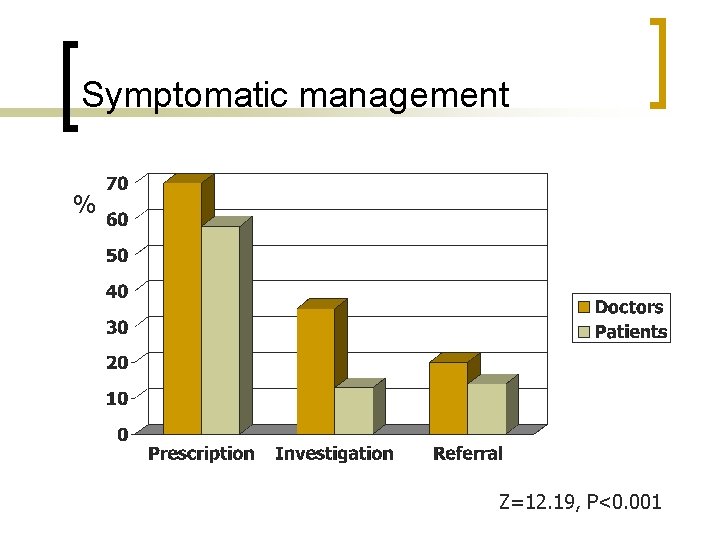
Symptomatic management % Z=12. 19, P<0. 001
Why this mismatch? Examining the role of doctors
Hypotheses n n Medical role Skill deficits Cognitive errors Disengagement
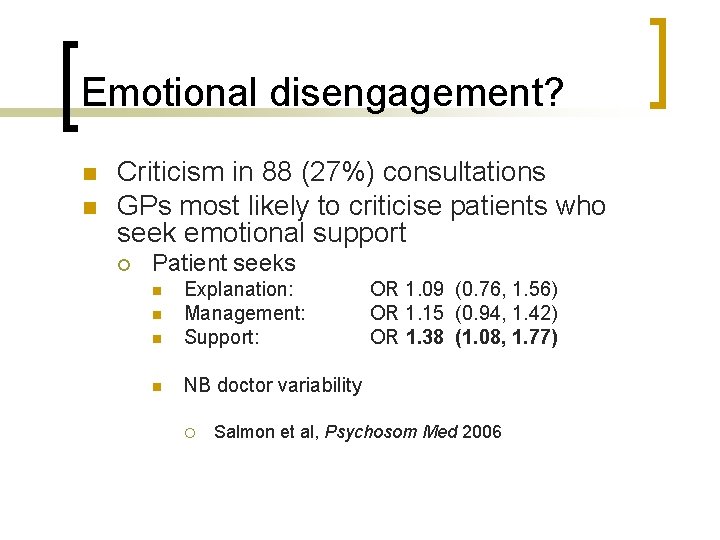
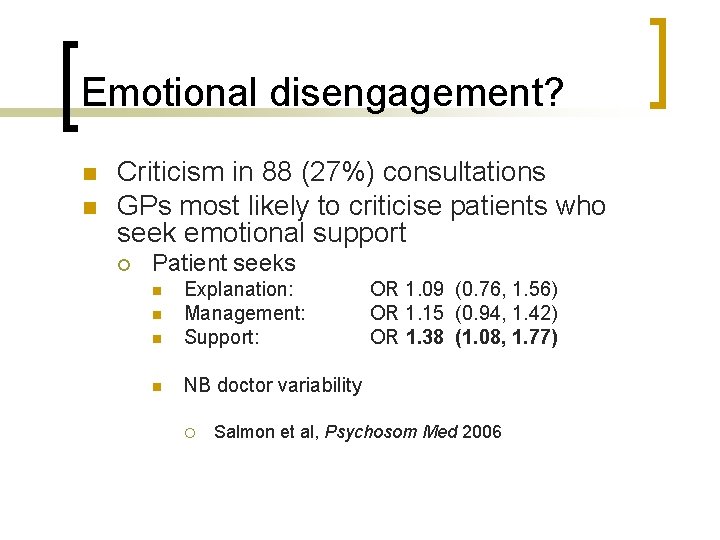
Emotional disengagement? n n Criticism in 88 (27%) consultations GPs most likely to criticise patients who seek emotional support ¡ Patient seeks n Explanation: Management: Support: n NB doctor variability n n ¡ OR 1. 09 (0. 76, 1. 56) OR 1. 15 (0. 94, 1. 42) OR 1. 38 (1. 08, 1. 77) Salmon et al, Psychosom Med 2006
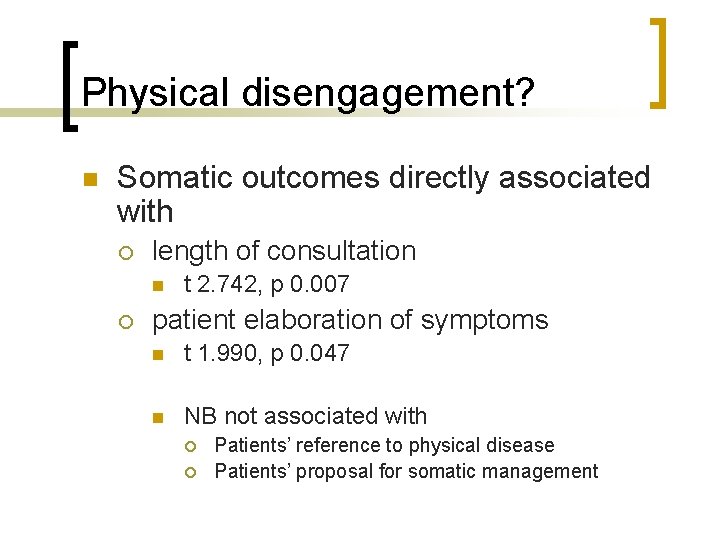
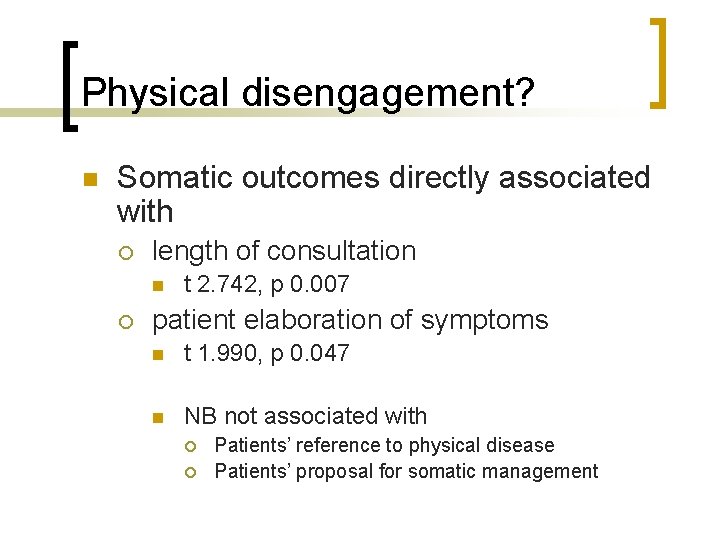
Physical disengagement? n Somatic outcomes directly associated with ¡ length of consultation n ¡ t 2. 742, p 0. 007 patient elaboration of symptoms n t 1. 990, p 0. 047 n NB not associated with ¡ ¡ Patients’ reference to physical disease Patients’ proposal for somatic management
Interpretation n Doctors’ strategies for disengagement contribute to somatic outcomes in consultations about MUS in primary care

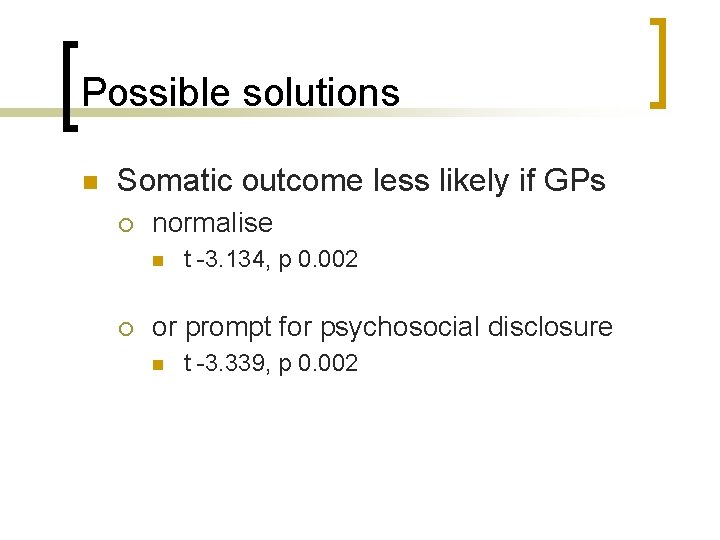
Possible solutions n Somatic outcome less likely if GPs ¡ normalise n ¡ t -3. 134, p 0. 002 or prompt for psychosocial disclosure n t -3. 339, p 0. 002
Next steps n Doctor variability ¡ ¡ n attachment style patient-centredness Direct hypothesis testing ¡ TAR interviews with doctors and patients

Watch this space… n cfd@liv. ac. uk
 Theories of ageing
Theories of ageing Disengagement theory
Disengagement theory Disengagment theory
Disengagment theory Disengagement theory
Disengagement theory Betty when did you come betty wanted to know
Betty when did you come betty wanted to know Promotion from assistant to associate professor
Promotion from assistant to associate professor St christopher primary school coventry
St christopher primary school coventry St christopher primary school
St christopher primary school The primary pigments are _____ the primary colors.
The primary pigments are _____ the primary colors. Primary, secondary, tertiary care
Primary, secondary, tertiary care Leiomyosarcoma
Leiomyosarcoma Unstructured lumigraph rendering
Unstructured lumigraph rendering Christopher hirata
Christopher hirata Cma cgm christopher columbus
Cma cgm christopher columbus Notorious big thomas
Notorious big thomas Atkins ford winder
Atkins ford winder Devion christopher brooks
Devion christopher brooks Christopher p cannon
Christopher p cannon When did christopher columbus discover america
When did christopher columbus discover america Christopher dalley
Christopher dalley Macbeth connections
Macbeth connections Finally, it has arrived
Finally, it has arrived