Measuring Health Systems Performance and NHA Agenda for
- Slides: 21
Measuring Health Systems Performance and NHA: Agenda for Health Services Research and Evaluation Akiko Maeda, Ph. D. Lead Health Specialist Europe and Central Asia Region The World Bank
Introduction NHA role in measuring health system performance n Challenges in measuring efficiency and quality of health care n Need for improved data collection and evaluation tools n Agenda for health services research & evaluation & NHA in developing countries n
Health Sector Resource Allocation & Utilization Questions n n How large is the sector? What are its constituent parts? What items currently dominates in resource allocation? Who pays for what, and what services do they get for their payment?
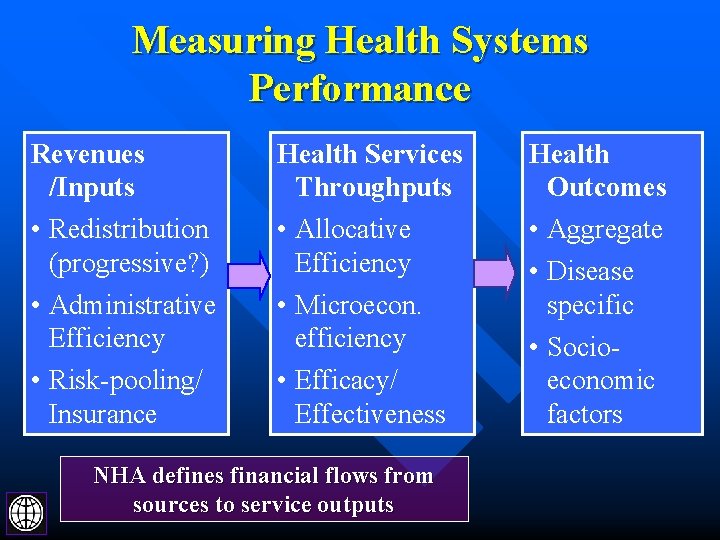
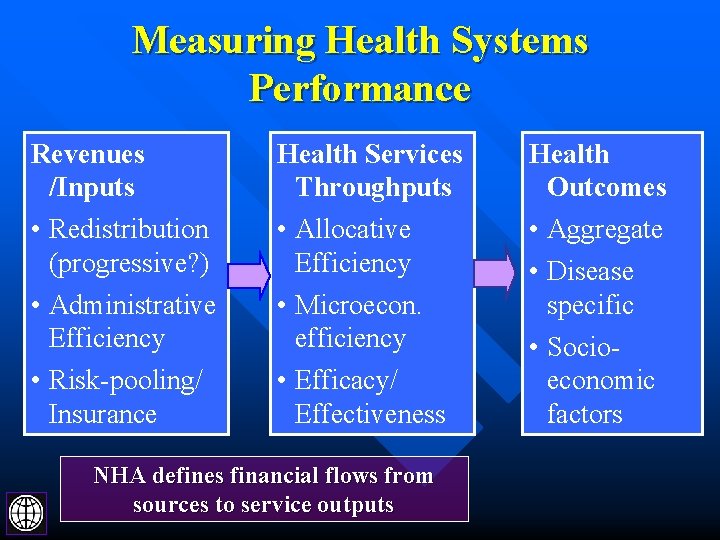
Measuring Health Systems Performance Revenues /Inputs Health Services Throughputs Health Outcomes • Redistribution (progressive? ) • Administrative Efficiency • Risk-pooling/ Insurance • Allocative Efficiency • Microecon. efficiency • Efficacy/ Effectiveness • Aggregate • Disease specific • Socioeconomic factors NHA defines financial flows from sources to service outputs
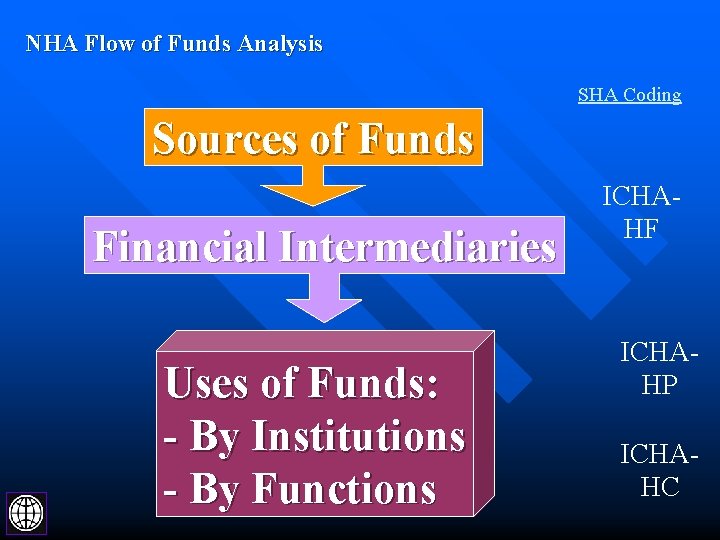
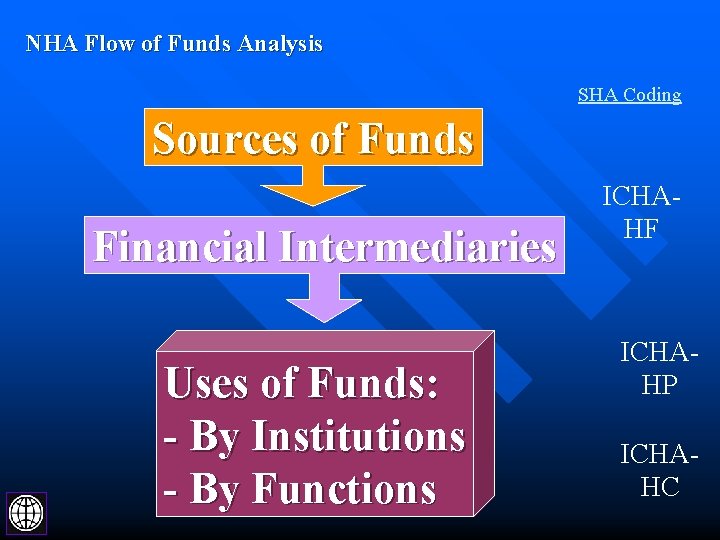
NHA Flow of Funds Analysis SHA Coding Sources of Funds Financial Intermediaries Uses of Funds: - By Institutions - By Functions ICHAHF ICHAHP ICHAHC
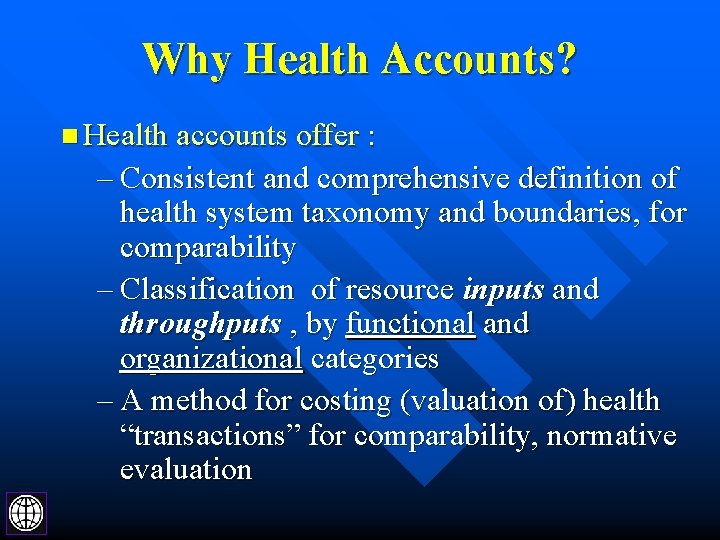
Why Health Accounts? n Health accounts offer : – Consistent and comprehensive definition of health system taxonomy and boundaries, for comparability – Classification of resource inputs and throughputs , by functional and organizational categories – A method for costing (valuation of) health “transactions” for comparability, normative evaluation
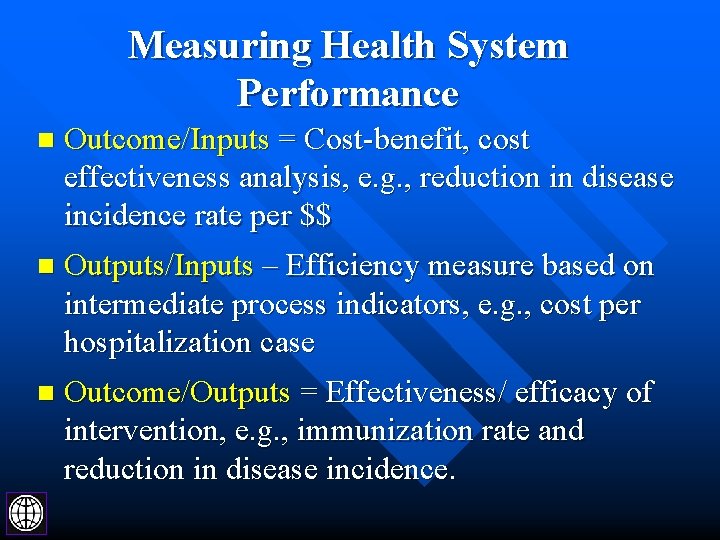
Measuring Health System Performance n Outcome/Inputs = Cost-benefit, cost effectiveness analysis, e. g. , reduction in disease incidence rate per $$ n Outputs/Inputs – Efficiency measure based on intermediate process indicators, e. g. , cost per hospitalization case n Outcome/Outputs = Effectiveness/ efficacy of intervention, e. g. , immunization rate and reduction in disease incidence.
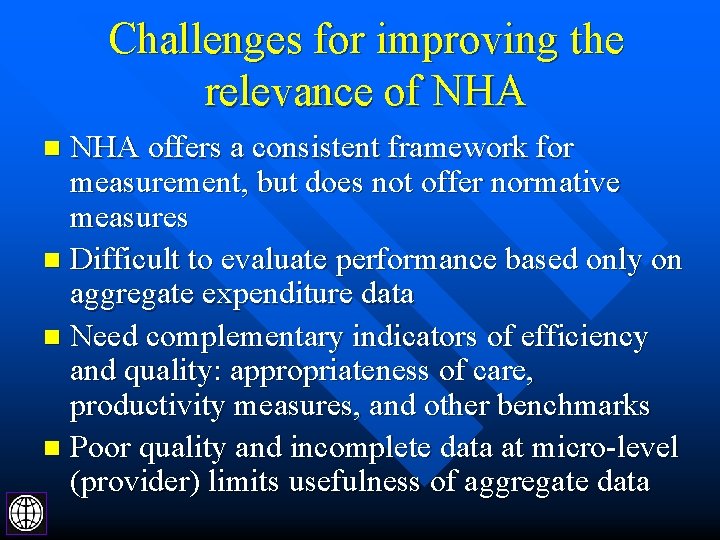
Challenges for improving the relevance of NHA offers a consistent framework for measurement, but does not offer normative measures n Difficult to evaluate performance based only on aggregate expenditure data n Need complementary indicators of efficiency and quality: appropriateness of care, productivity measures, and other benchmarks n Poor quality and incomplete data at micro-level (provider) limits usefulness of aggregate data n
Measuring “Efficiency” of Health System: Challenges Major gap between aggregate macro-level data GAP . . And microeconomic performance data at provider and population level
Challenges in Comparing Health System Performance Variability in the organization of health care delivery system n Dynamically evolving technology: e. g. , increasing use of day surgeries, decreasing acute care hospitalization days n Internal variability in performance among providers and outcome among population groups n Confounding factors: complex interactions between socio-economic factors and health outcomes n
Example: Using NHA to evaluate Estimating Allocative Efficiency n NHA functional categories: e. g. , public health programs, acute vs. chronic inpatient care provides common framework for defining products, but needs to be adjusted for: – Intensity, quality of care – Population – demographic profile – Evidence of clinical efficacy, costeffectiveness
What can we tell from these aggregate expenditure data. . . ?
Agenda for Research n Developing data collection and research capacity in the following areas: – Household consumption and expenditure surveys, with improved designs on medical services purchased directly or through insurance – Health care provider utilization surveys – Improved quality of expenditure data at provider level (case-mix, medical procedures)
Agenda for NHA in Developing Countries n Review of classification of services – Need to review, adapt OECD SHA functional and provider classifications to suit developing country health systems n Health services research agenda: – Developing affordable instruments for collecting data at provider (private & public) and population groups
Examples of Priority Topics for Health System Research Rational Use of Drugs n Hospitalization – tracking changes in acute and chronic care admission rates, length of stay n Administrative efficiency n Public health programs – allocation on prevention and population-based programs versus personal/ clinical interventions n
Agenda for Health System Research n Recommendations: – Focus greater attention on capacity building on health services research and evaluation – Introduce National Health Accounts within the context of health services evaluation, not as a stand-alone instrument – With improved quality of data, it should become more feasible to undertake meaningful national and international comparisons
Agenda for Health System Research World Bank’s standard economic and sector work focuses on Public Expenditure Reviews (PER) and Household Surveys (e. g. , Living Standards Measurement Surveys) n Complementary capacity building should focus on supporting provider surveys, operational research on services n
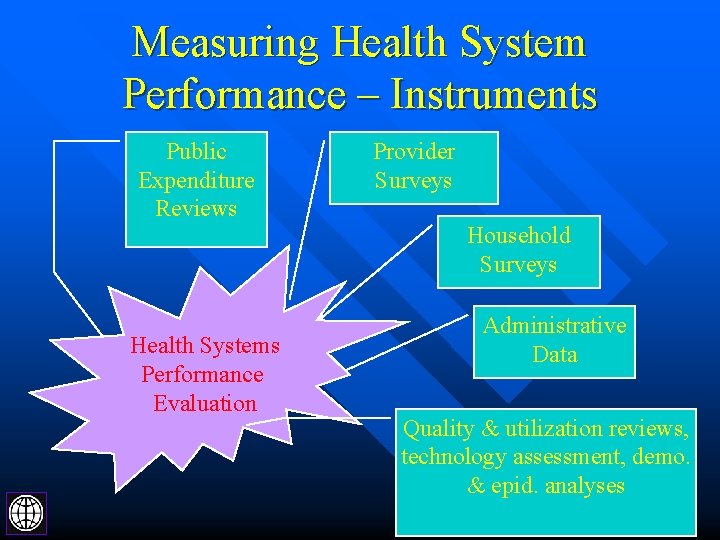
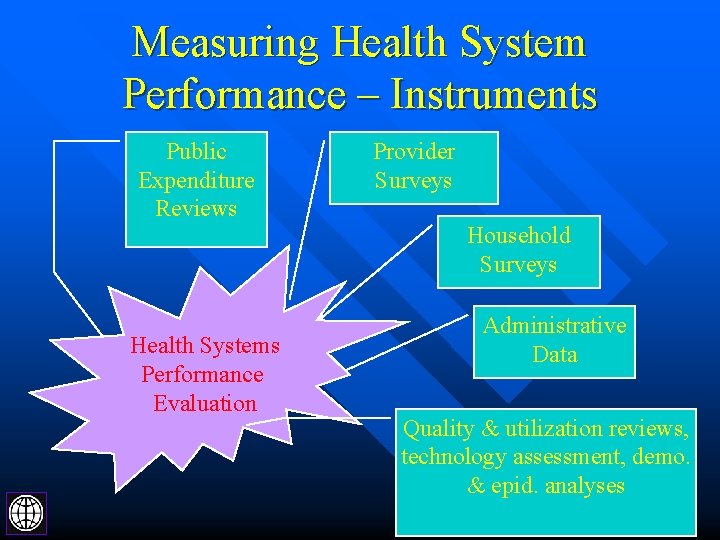
Measuring Health System Performance – Instruments Public Expenditure Reviews Health Systems Performance Evaluation Provider Surveys Household Surveys Administrative Data Quality & utilization reviews, technology assessment, demo. & epid. analyses
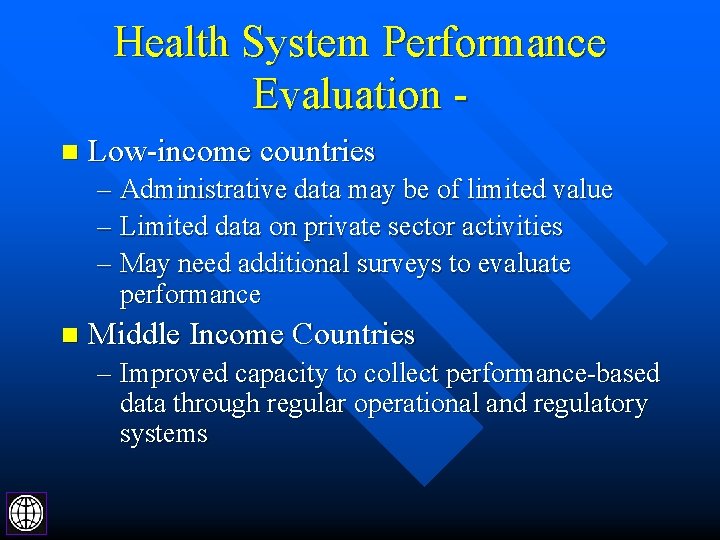
Health System Performance Evaluation n Low-income countries – Administrative data may be of limited value – Limited data on private sector activities – May need additional surveys to evaluate performance n Middle Income Countries – Improved capacity to collect performance-based data through regular operational and regulatory systems
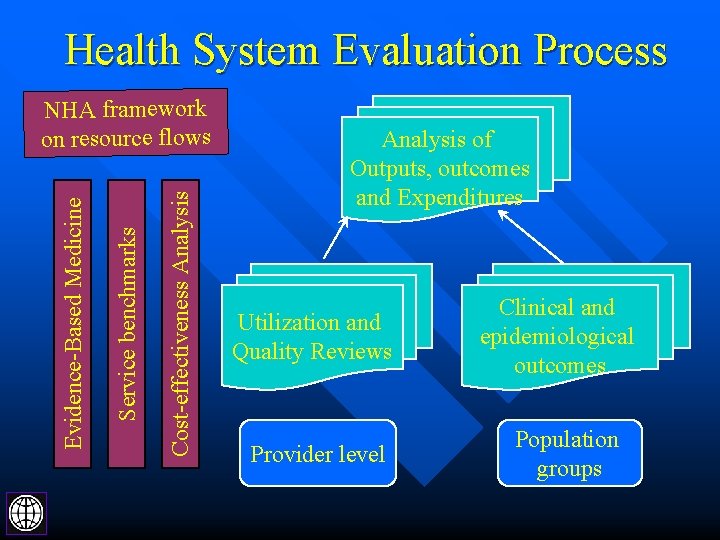
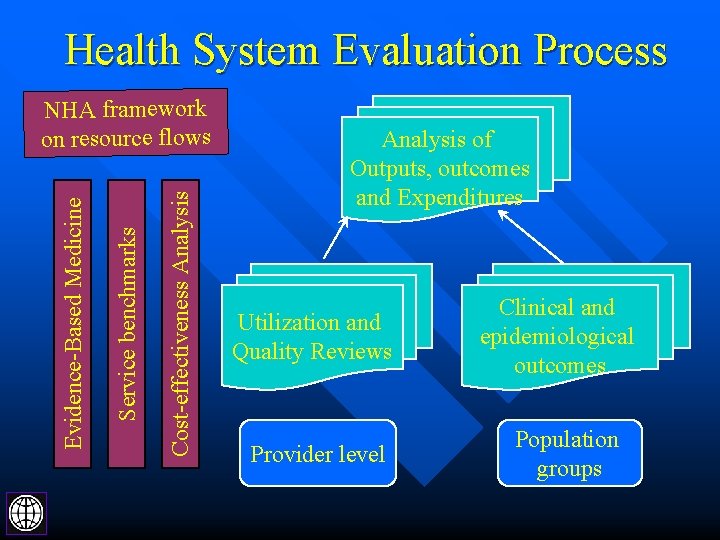
Health System Evaluation Process Cost-effectiveness Analysis Service benchmarks Evidence-Based Medicine NHA framework on resource flows Analysis of Outputs, outcomes and Expenditures Utilization and Quality Reviews Provider level Clinical and epidemiological outcomes Population groups
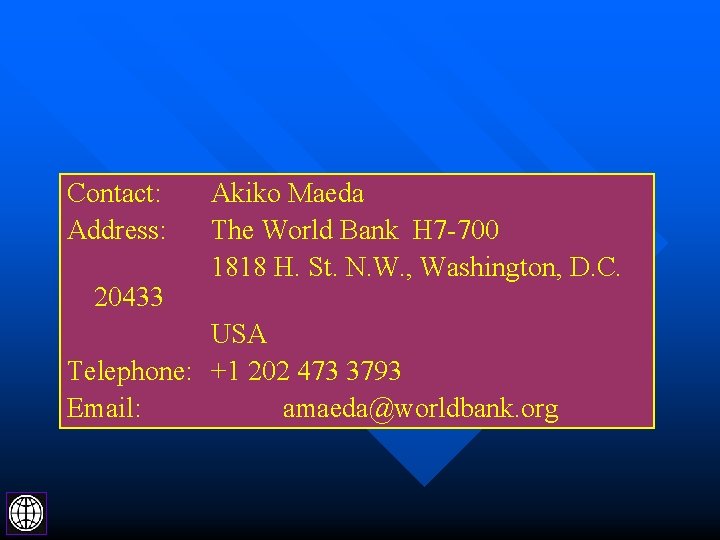
Contact: Address: 20433 Akiko Maeda The World Bank H 7 -700 1818 H. St. N. W. , Washington, D. C. USA Telephone: +1 202 473 3793 Email: amaeda@worldbank. org
 Agenda sistemica y agenda institucional
Agenda sistemica y agenda institucional Evaluating bank performance
Evaluating bank performance Measuring hotel performance
Measuring hotel performance Measuring computer performance
Measuring computer performance 3 approaches to measuring performance
3 approaches to measuring performance Defining performance and choosing a measurement approach
Defining performance and choosing a measurement approach Measuring the actual performance
Measuring the actual performance Measuring the actual performance
Measuring the actual performance Measuring the actual performance
Measuring the actual performance John r. schermerhorn
John r. schermerhorn Agenda management systems
Agenda management systems Agenda open systems
Agenda open systems Bớt đầu thì bé nhất nhà
Bớt đầu thì bé nhất nhà Các cơ quan trong bộ máy nhà nước
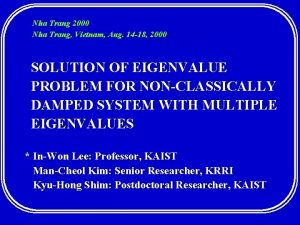
Các cơ quan trong bộ máy nhà nước Dừng chân nghỉ lại nha trang
Dừng chân nghỉ lại nha trang Design thking
Design thking Thời gian hình thành nhà nước văn lang
Thời gian hình thành nhà nước văn lang Nhà tôi ở hà nội cách hồ gươm không xa
Nhà tôi ở hà nội cách hồ gươm không xa đi nhà trẻ các bạn ơi cùng vui chơi
đi nhà trẻ các bạn ơi cùng vui chơi Bài tập về nhà
Bài tập về nhà Tiêu luận chuỗi cung ứng của th true milk
Tiêu luận chuỗi cung ứng của th true milk O.hen-ri
O.hen-ri