MALNUTRITION MICRONUTRIENT DEFICIENCIES WHOS AT RISK FOR WHAT
- Slides: 33
MALNUTRITION & MICRONUTRIENT DEFICIENCIES: WHO’S AT RISK & FOR WHAT? Mary Litchford, Ph. D, RDN, LDN
Disclosures • The content of this program has met the continuing education criteria of being evidence-based, fair and balanced, and non-promotional. • Mary Litchford, Ph. D, RDN, LDN received an honorarium for this CE program. She is a consultant for Medline Industries, Prosynthesis Labs; Speaker’s Bureau - Abbott Nutrition, Nestle Nutrition; and Past President - National Pressure Ulcer Advisory Panel
Objectives • Review the prevalence of malnutrition and identification of adult malnutrition. • Examine the criteria used to define characteristics of malnutrition. • Discuss the prevalence of micronutrient deficiencies in different population groups. © CSB, 2019
How Do You Approach Assessment for Malnutrition? Photo taken on expedition to Antarctica © CSB, 2019
Think About Your Professional Education Program…. • What do you remember about malnutrition from college coursework? • What do you remember about the incidence of vitamin and mineral deficiencies from college coursework? Image from Dreamtime © CSB, 2019
What Do You Know about Nutrition? National Association of Clinical Nurse Specialists Malnutrition Task Force MALNUTRITION IN HOSPITALIZED ADULT PATIENTS (2017) • Nutrition knowledge survey on use of nutritional assessment & interventions: • 50% of NACNS members reported they received education on nutrition beyond an undergraduate course • 59% of NACNS members indicated they had basic or less than basic knowledge related to nutritional status or the nutritional needs of hospitalized adults. • No survey respondents identified that advanced practice registered nurses (APRNs) have primary responsibility for initiating nutritional intervention • 4. 1% of respondents thought that APRNs have responsibility for maintaining nutritional interventions. NACNS. (2017). Malnutrition in hospitalized adult patients. The Role of the Clinical Nurse Specialist https: //nacns. org/professional-resources/toolkits-and-reports/malnutrition-in-hospitalized-adult-patients/ © CSB, 2019
Nutrition & Health Are Closely Related “About half of all American adults— 117 million individuals—have one or more preventable chronic diseases, many of which are related to poor eating and physical activity patterns. ” USDA Dietary. Guidelines. gov [website]. Dietary guidelines for Americans. 2015 -2020. 8 th ed. https: //health. gov/dietaryguidelines/2015/resources/2015 -2020_Dietary_Guidelines. pdf. © CSB, 2019
• Case report of nutritional optic neuropathy • Diet consisted of fried fish, chips, white bread & processed • • meat Age 14 yr- dx with B 12 deficiency Age 15 yr impaired hearing & vision (MRI was WNL) Age 17 yr legally blind, Copper & vitamin D deficiencies Conclusions: lack of awareness among healthcare professionals and the public about the links between a poor diet & permanently damage nervous system, particularly vision Harrison R, Warburton V, Lux A, Atan D. Blindness Caused by a Junk Food Diet. Ann Intern Med. [Epub ahead of print 3 September 2019] doi: 10. 7326/L 19 -0361 © CSB, 2019
Who is Malnourished? Images from Dreamtime & CDC PHIL © CSB, 2019
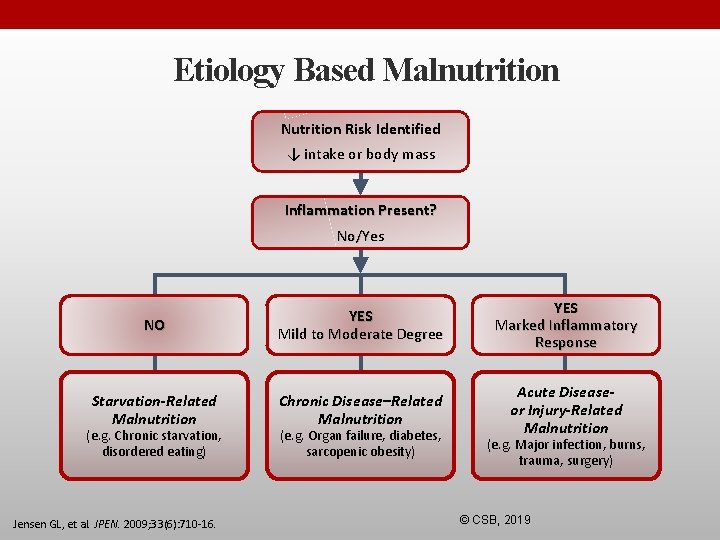
What is Malnutrition? Malnutrition is an acute, subacute or chronic state of nutrition, in which a combination of varying degrees of undernutrition with or without inflammatory activity have led to a change in body composition and diminished function. There are 3 etiology-based nutrition diagnoses in adults: 1. Starvation-related malnutrition 2. Chronic disease-related malnutrition 3. Acute disease or injury-related malnutrition Soeters PB, Schols AM. Advances in understanding and assessing malnutrition. Curr Opin Clin Nutr Metab Care 2009; 12(5): 487– 494. © CSB, 2019
Why is identification important? 20 -50% of patients are at-risk for malnutrition upon hospital admission 1 -2 Yet only ~7% of hospitalized patients are diagnosed for malnutrition, leaving many others undiagnosed and untreated 3 Nutrition. Day study 4 on malnutrition (n = 10, 000) • 245 US hospitals • Found 33% of patients were at-risk for malnutrition • November 7, 2019 is the next Nutrition. Day 1. Barker LA, et al. Int J Environ Res Public Health. 2011; 8: 514 -27; 2 Pereira GF, et al. Ann Emerg Med. 2015; 65(1): 85 -91; 3 Barrett ML, et al. Non-maternal and non-neonatal inpatient stays in the United States involving malnutrition, 2016. Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project. August 2018; 4. Sauer AC, et al. JPEN. 2019. [Epub ahead of print] © CSB, 2019
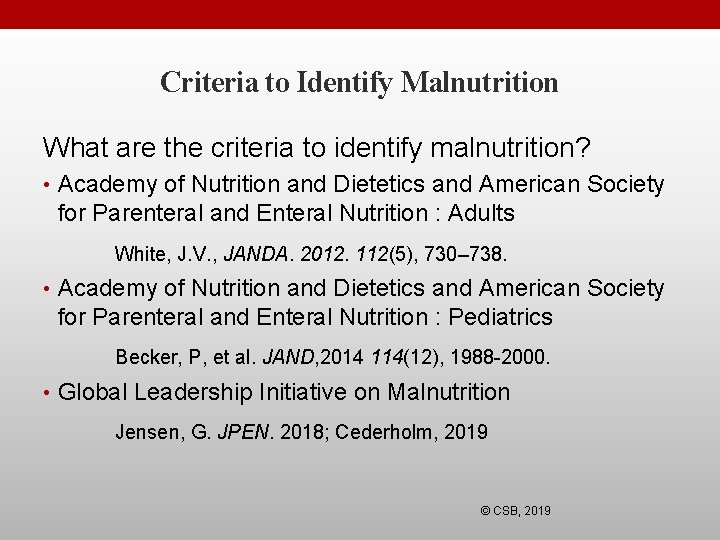
Criteria to Identify Malnutrition What are the criteria to identify malnutrition? • Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition : Adults White, J. V. , JANDA. 2012. 112(5), 730– 738. • Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition : Pediatrics Becker, P, et al. JAND, 2014 114(12), 1988 -2000. • Global Leadership Initiative on Malnutrition Jensen, G. JPEN. 2018; Cederholm, 2019 © CSB, 2019
Assessment for Malnutrition 2 Step Process: 1. Nutrition Screening • Completed by medical professionals other than RDN 2. Comprehensive Nutrition Assessment • Completed by the RDN © CSB, 2019
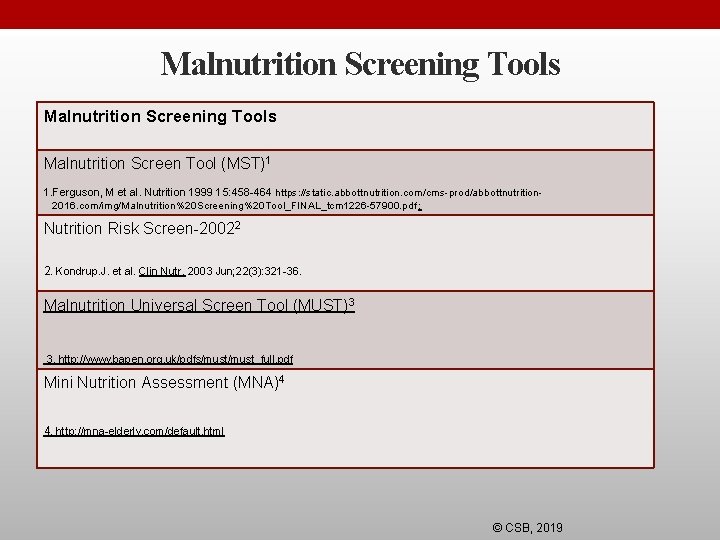
Malnutrition Screening Tools Malnutrition Screen Tool (MST)1 1. Ferguson, M et al. Nutrition 1999 15: 458 -464 https: //static. abbottnutrition. com/cms-prod/abbottnutrition 2016. com/img/Malnutrition%20 Screening%20 Tool_FINAL_tcm 1226 -57900. pdf ; Nutrition Risk Screen-20022 2. Kondrup. J. et al. Clin Nutr. 2003 Jun; 22(3): 321 -36. Malnutrition Universal Screen Tool (MUST)3 3. http: //www. bapen. org. uk/pdfs/must_full. pdf Mini Nutrition Assessment (MNA)4 4. http: //mna-elderly. com/default. html © CSB, 2019
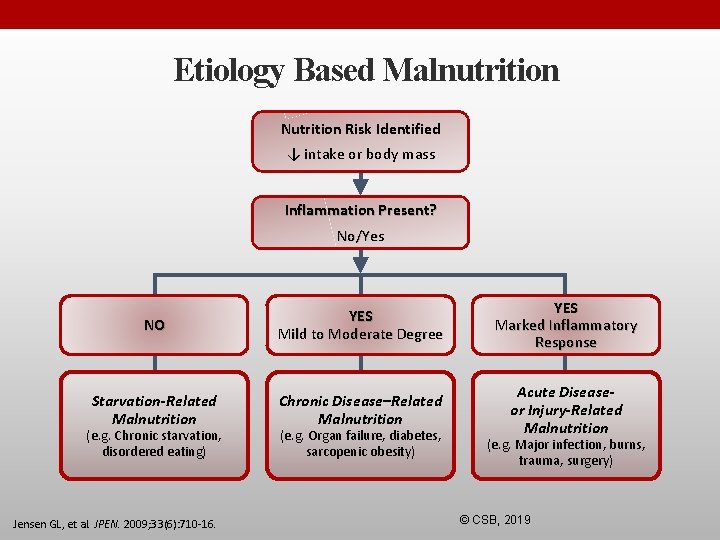
Etiology Based Malnutrition Nutrition Risk Identified ↓ intake or body mass Inflammation Present? No/Yes NO YES Mild to Moderate Degree YES Marked Inflammatory Response Starvation-Related Malnutrition Chronic Disease–Related Malnutrition Acute Diseaseor Injury-Related Malnutrition (e. g. Chronic starvation, disordered eating) Jensen GL, et al. JPEN. 2009; 33(6): 710 -16. (e. g. Organ failure, diabetes, sarcopenic obesity) (e. g. Major infection, burns, trauma, surgery) © CSB, 2019
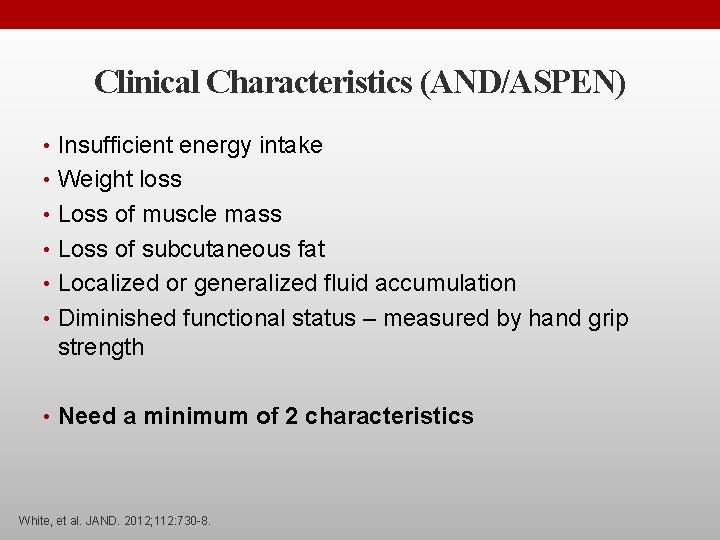
Clinical Characteristics (AND/ASPEN) • Insufficient energy intake • Weight loss • Loss of muscle mass • Loss of subcutaneous fat • Localized or generalized fluid accumulation • Diminished functional status – measured by hand grip strength • Need a minimum of 2 characteristics White, et al. JAND. 2012; 112: 730 -8.
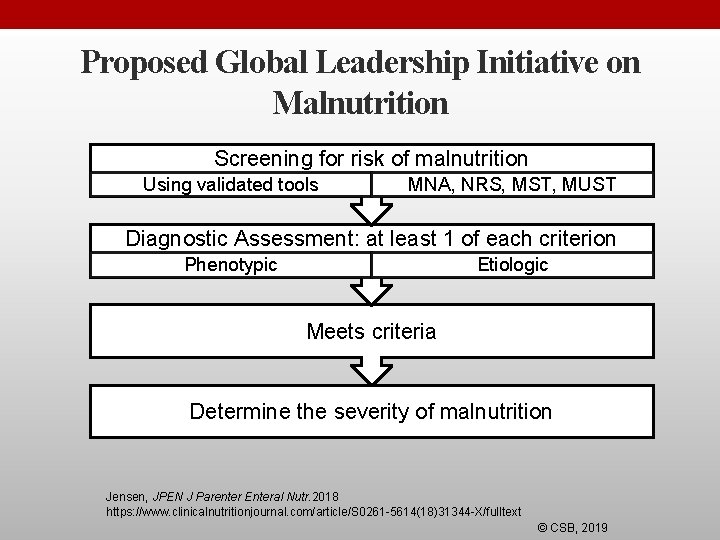
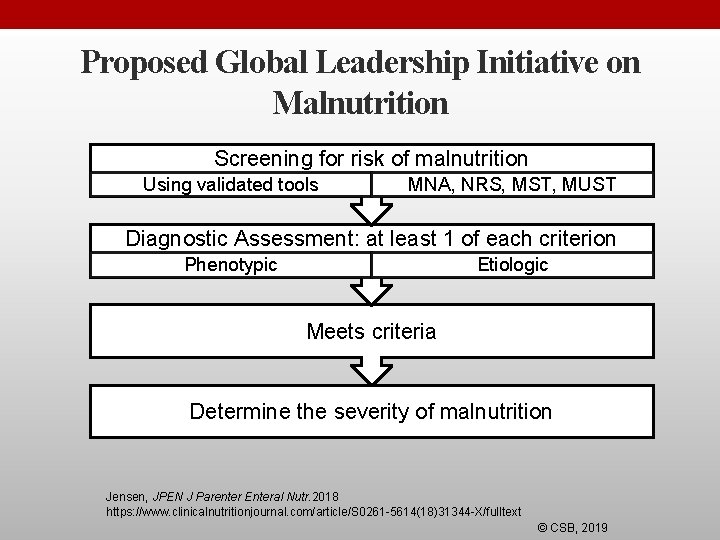
Proposed Global Leadership Initiative on Malnutrition Screening for risk of malnutrition Using validated tools MNA, NRS, MST, MUST Diagnostic Assessment: at least 1 of each criterion Phenotypic Etiologic Meets criteria Determine the severity of malnutrition Jensen, JPEN J Parenter Enteral Nutr. 2018 https: //www. clinicalnutritionjournal. com/article/S 0261 -5614(18)31344 -X/fulltext © CSB, 2019
Aren’t Albumin & Prealbumin Markers of Malnutrition ? ? ? Image from Dreamtime © CSB, 2019
Who MOST Likely has a Serum Albumin within Normal Ranges? Images from CDC PHIL & Dreamtime © CSB, 2019
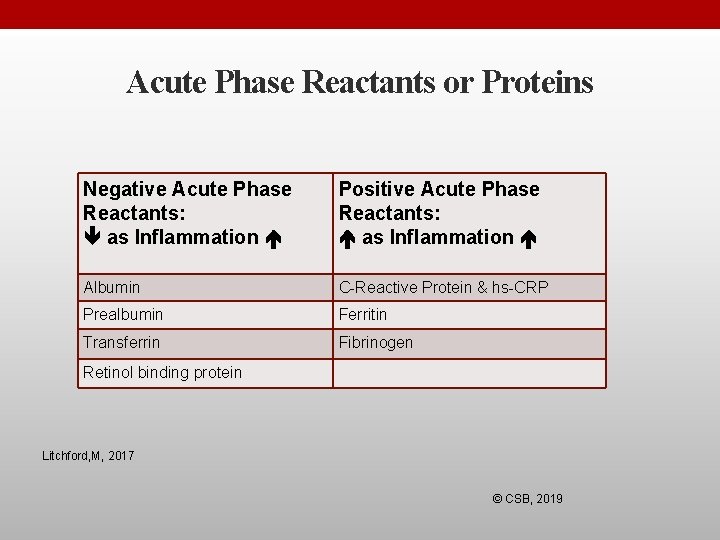
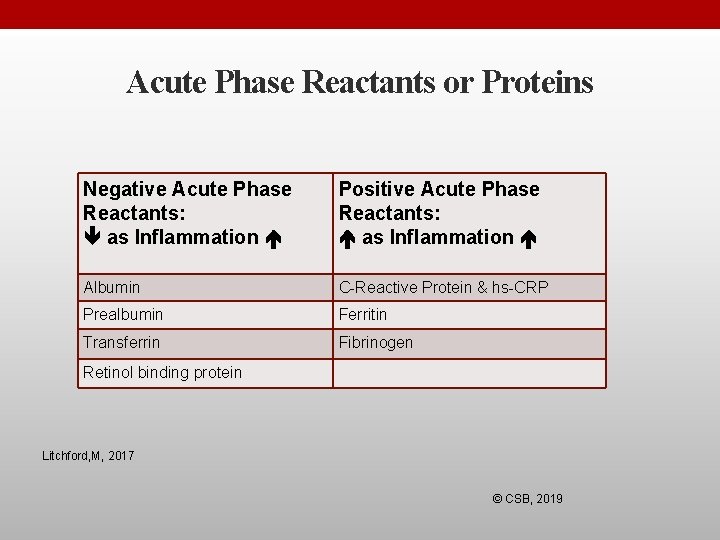
Acute Phase Reactants or Proteins Negative Acute Phase Reactants: as Inflammation Positive Acute Phase Reactants: as Inflammation Albumin C-Reactive Protein & hs-CRP Prealbumin Ferritin Transferrin Fibrinogen Retinol binding protein Litchford, M, 2017 © CSB, 2019
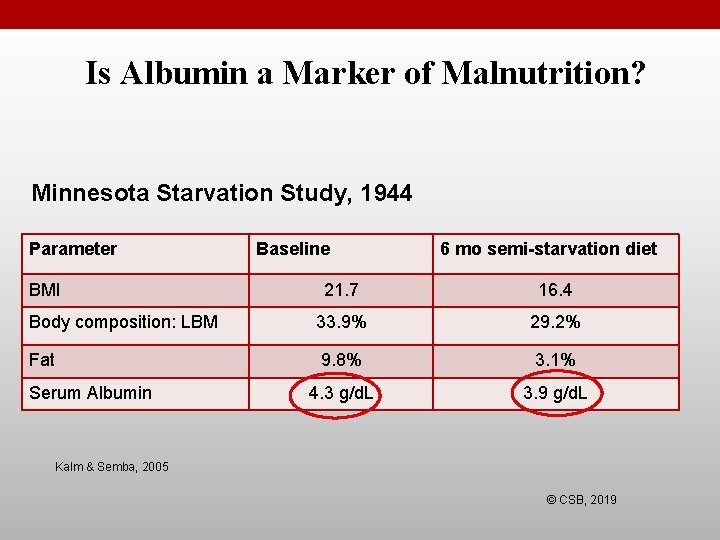
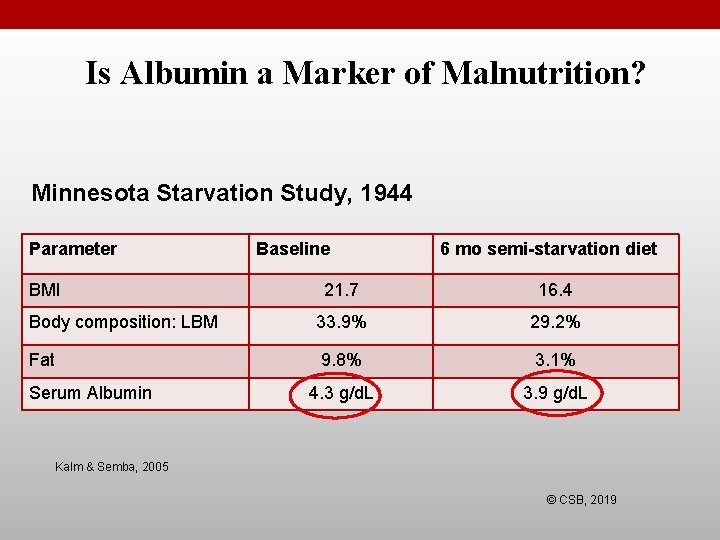
Is Albumin a Marker of Malnutrition? Minnesota Starvation Study, 1944 Parameter BMI Baseline 6 mo semi-starvation diet 21. 7 16. 4 Body composition: LBM 33. 9% 29. 2% Fat 9. 8% 3. 1% 4. 3 g/d. L 3. 9 g/d. L Serum Albumin Kalm & Semba, 2005 © CSB, 2019
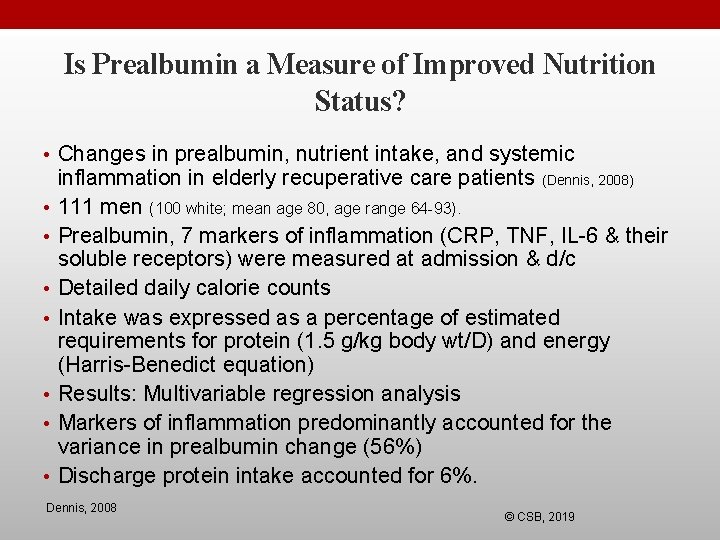
Is Prealbumin a Measure of Improved Nutrition Status? • Changes in prealbumin, nutrient intake, and systemic • • inflammation in elderly recuperative care patients (Dennis, 2008) 111 men (100 white; mean age 80, age range 64 -93). Prealbumin, 7 markers of inflammation (CRP, TNF, IL-6 & their soluble receptors) were measured at admission & d/c Detailed daily calorie counts Intake was expressed as a percentage of estimated requirements for protein (1. 5 g/kg body wt/D) and energy (Harris-Benedict equation) Results: Multivariable regression analysis Markers of inflammation predominantly accounted for the variance in prealbumin change (56%) Discharge protein intake accounted for 6%. Dennis, 2008 © CSB, 2019
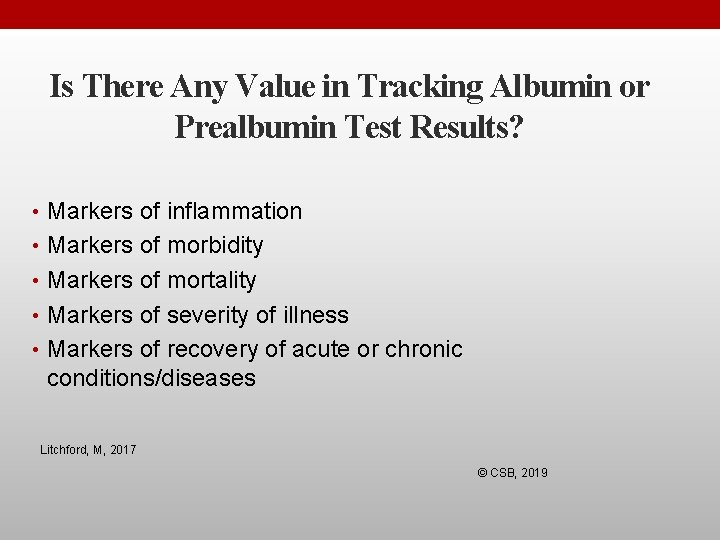
Is There Any Value in Tracking Albumin or Prealbumin Test Results? • Markers of inflammation • Markers of morbidity • Markers of mortality • Markers of severity of illness • Markers of recovery of acute or chronic conditions/diseases Litchford, M, 2017 © CSB, 2019
Who is at Risk for Malnutrition & Nutrient Deficiencies? © CSB, 2019 Images from Dreamtime
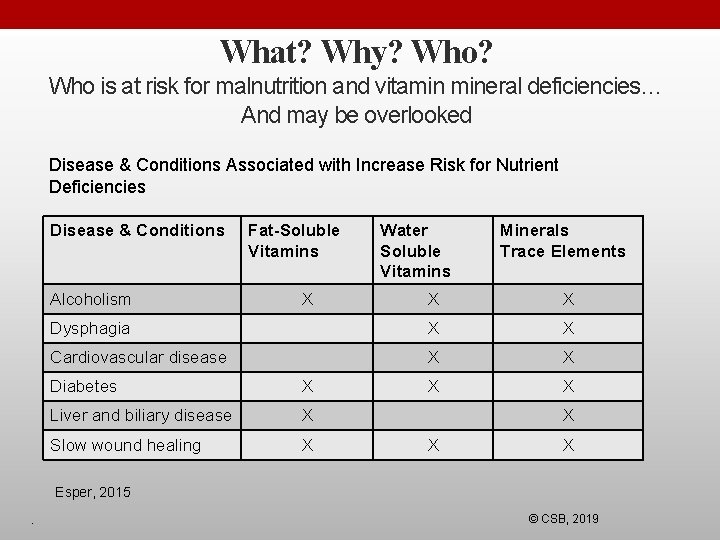
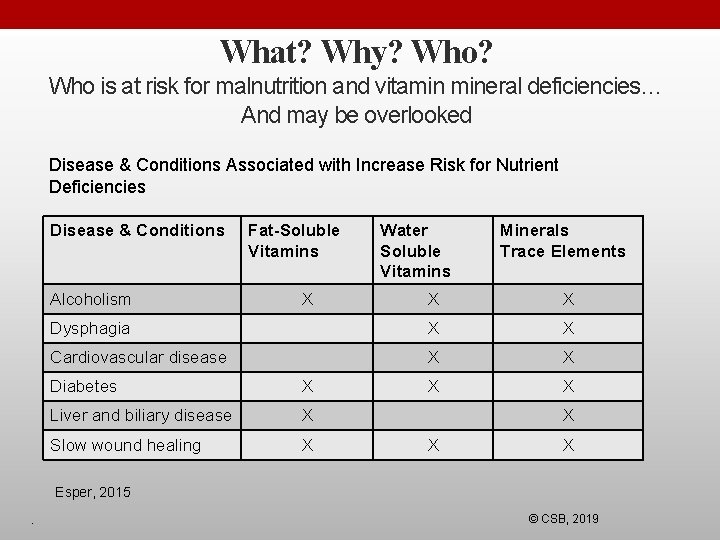
What? Why? Who is at risk for malnutrition and vitamin mineral deficiencies… And may be overlooked Disease & Conditions Associated with Increase Risk for Nutrient Deficiencies Disease & Conditions Alcoholism Fat-Soluble Vitamins X Water Soluble Vitamins Minerals Trace Elements X X Dysphagia X X Cardiovascular disease X X Diabetes X Liver and biliary disease X Slow wound healing X X Esper, 2015. © CSB, 2019
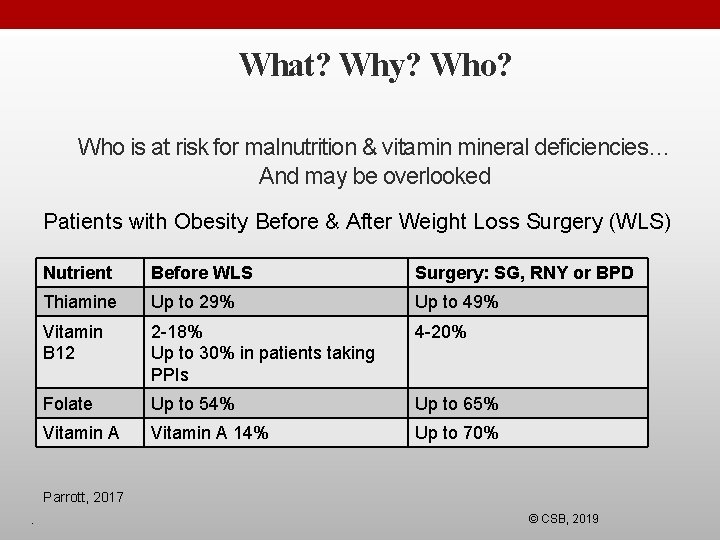
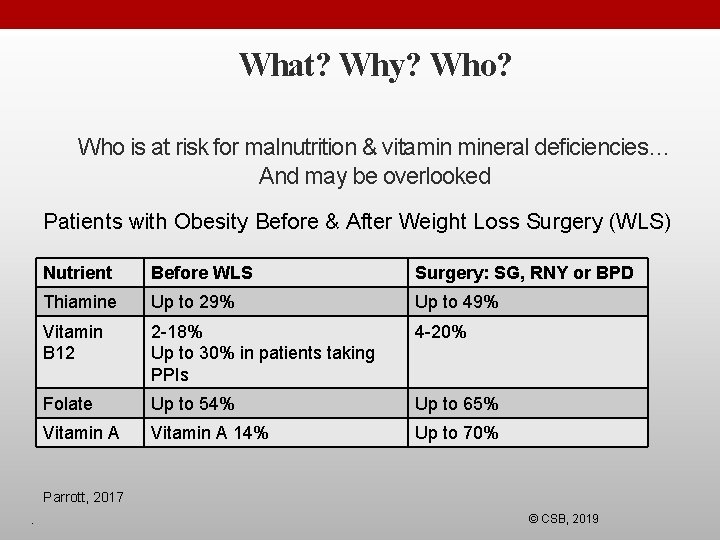
What? Why? Who is at risk for malnutrition & vitamin mineral deficiencies… And may be overlooked Patients with Obesity Before & After Weight Loss Surgery (WLS) Nutrient Before WLS Surgery: SG, RNY or BPD Thiamine Up to 29% Up to 49% Vitamin B 12 2 -18% Up to 30% in patients taking PPIs 4 -20% Folate Up to 54% Up to 65% Vitamin A 14% Up to 70% Parrott, 2017. © CSB, 2019
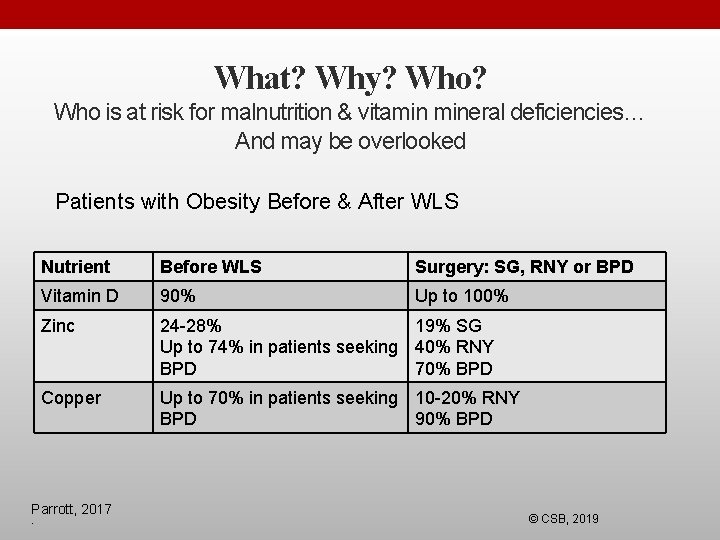
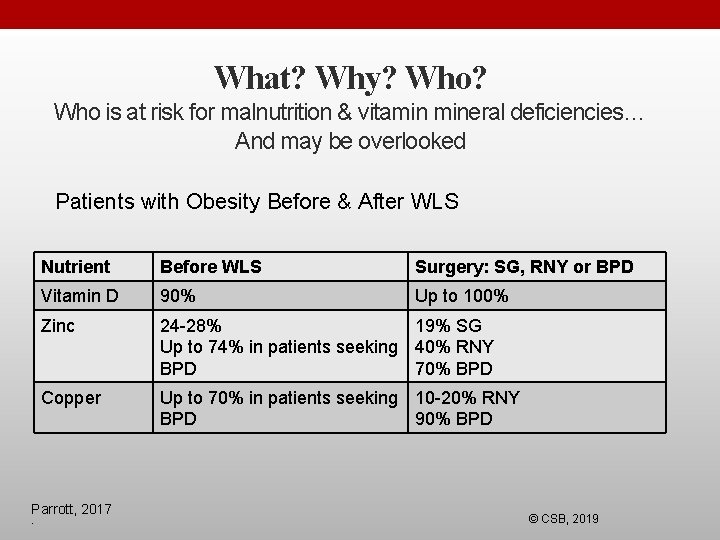
What? Why? Who is at risk for malnutrition & vitamin mineral deficiencies… And may be overlooked Patients with Obesity Before & After WLS Nutrient Before WLS Surgery: SG, RNY or BPD Vitamin D 90% Up to 100% Zinc 24 -28% 19% SG Up to 74% in patients seeking 40% RNY BPD 70% BPD Copper Up to 70% in patients seeking 10 -20% RNY BPD 90% BPD Parrott, 2017. © CSB, 2019
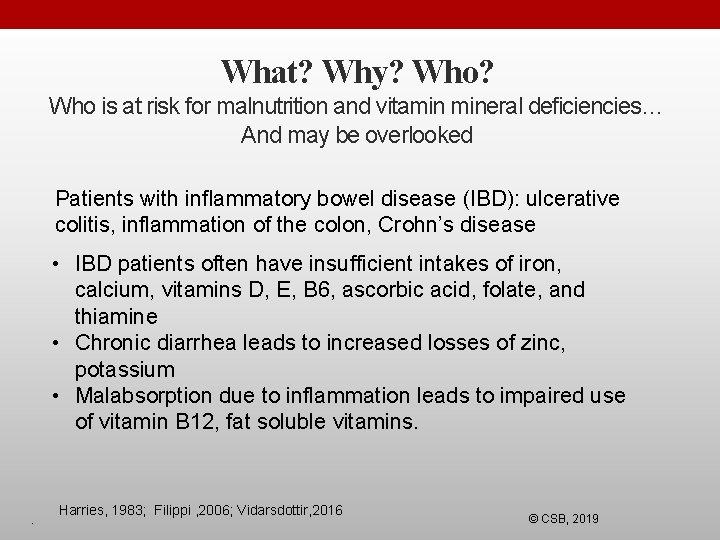
What? Why? Who is at risk for malnutrition and vitamin mineral deficiencies… And may be overlooked Patients with inflammatory bowel disease (IBD): ulcerative colitis, inflammation of the colon, Crohn’s disease • IBD patients often have insufficient intakes of iron, calcium, vitamins D, E, B 6, ascorbic acid, folate, and thiamine • Chronic diarrhea leads to increased losses of zinc, potassium • Malabsorption due to inflammation leads to impaired use of vitamin B 12, fat soluble vitamins. . Harries, 1983; Filippi , 2006; Vidarsdottir, 2016 © CSB, 2019
What? Why? Who is at risk for malnutrition and vitamin mineral deficiencies… And may be overlooked Poor diets with limited food choices and processed foods • Nutritional optic neuropathy resulting in blindness due to multiple vitamin and mineral deficiencies including copper deficiency . Harries, 1983; Filippi , 2006; Vidarsdottir, 2016 © CSB, 2019
What? Why? Who is at risk for malnutrition and vitamin mineral deficiencies… And may be overlooked Medications interfere with nutrient utilization • Examples: sulfasalazine- folate antagonist • cholestyramine impairs absorption of fat soluble vitamins • glucocorticoids might impair absorption of calcium, phosphorus and zinc and alter metabolism of calcium and Vitamin D . Harries, 1983; Filippi , 2006; Vidarsdottir, 2016 © CSB, 2019
NFPE Identifies Abnormal Findings • Loss of muscle mass • Loss of subcutaneous fat wasting • Physical changes that impair eating • Physical changes that impair breathing ability • Changes in appetite • Evidence of abnormal affect • Physical changes associated with malnutrition, disease or treatment for disease • Impaired functional status • Poor wound healing AND, 2013; Litchford, 2016 © CSB, 2019
Questions? ? ? Image from Dreamtime © CSB, 2019
Want to Know More? Join us Saturday September 14 12 -3 PM Practicums Nutrition & Wound Healing, Nutrition Focused Physical Exam, Lab Assessment Intervention & Nutrition-Related Litigation Mary Litchford, Ph. D, RDN, LDN © CSB, 2019
 Exaggerated physical deficiencies
Exaggerated physical deficiencies Abnormal development adler
Abnormal development adler Market risk assessment
Market risk assessment +winter +wheat +micronutrient
+winter +wheat +micronutrient Conjunctivitius
Conjunctivitius +winter +wheat +micronutrient
+winter +wheat +micronutrient Matlab command window clear
Matlab command window clear Whos nemos dad
Whos nemos dad Whose child is this
Whose child is this Whos line is it anyway
Whos line is it anyway Omniscient narrator
Omniscient narrator The story of achilles heel
The story of achilles heel Animal farm chapter 1
Animal farm chapter 1 Who is taylor swift anyway
Who is taylor swift anyway Hamlet character constellation
Hamlet character constellation Macbeth discussion questions
Macbeth discussion questions Mapp public health
Mapp public health Whos entitled to 30 hours free childcare
Whos entitled to 30 hours free childcare Whos this
Whos this Justine in frankenstein
Justine in frankenstein Who are the thanes in macbeth
Who are the thanes in macbeth Whos sitting bull
Whos sitting bull Ku leuven whos who
Ku leuven whos who Whos for the game jessie pope
Whos for the game jessie pope Adjectives for romeo and juliet characters
Adjectives for romeo and juliet characters Whos job is it
Whos job is it Whos job is it
Whos job is it Whos boxer in animal farm
Whos boxer in animal farm Site:slidetodoc.com
Site:slidetodoc.com Whos ghost does macbeth see
Whos ghost does macbeth see Bombardier beetle darwin
Bombardier beetle darwin Whos darwin
Whos darwin Whos jane addams
Whos jane addams Whos a famous painter
Whos a famous painter