Mainstreaming Traditional Medicine Potential Role for Universal Health

![Quality of Service [Stand alone/Co-located] Criteria for Grading Quality: • Infrastructure—Blding/space, cleanliness, signages, water&elec Quality of Service [Stand alone/Co-located] Criteria for Grading Quality: • Infrastructure—Blding/space, cleanliness, signages, water&elec](https://slidetodoc.com/presentation_image/4de6bd606794659a4cf27c233f812f83/image-28.jpg)
- Slides: 36
Mainstreaming Traditional Medicine: Potential Role for Universal Health Coverage in the Indian Context Ritu Priya 1 and Shweta A. S. 2 1 Ritu Priya (MBBS, Ph. D. ), Professor, Centre of Social Medicine & Community Health, Jawaharlal Nehru University, New Delhi Advisor (Public Health Planning), National Health Systems Resource Centre, NRHM, MOHFW, GOI. (ritu_priya_jnu@yahoo. com) 2 Shweta A. S. (BAMS, PGDEMS), Consultant (AYUSH-Public Health Planning), National Health Systems Resource Centre, New Delhi , NRHM, MOHFW, GOI. (drshweta. nhsrc@gmail. com) 1
Mainstreaming Traditional Medicine: Potential Role for Universal Health Coverage in the Indian Context Ritu Priya and Shweta A. S. XIII ASCON, ICDDR, BANGLADESH SCIENCE FOR ACCELERATING UNIVERSAL HEALTH COVERAGE DHAKA, 14 TH-17 TH MARCH, 2011 2
WHY TRADITIONAL MEDICINE? ? 3
A Health Systems Imperative TM is, in its various forms (Textual Systems, Folk Practitioners, Home Remedies, and CAM): § increasingly being used in high income countries, and § continues to be used by large proportion of the populations in the middle and low income countries. [estimated to be 70% of world by WHO Global Atlas on TM] The frontiers of medical research and practice today include a large section on herbal remedies, lifestyle determinants and therapies, body-mind therapies, interdisciplinary research such as psychoneuro-immunology. RCTs have provided evidence for efficacy of several herbal and other traditional therapies. However, in the emerging economies and other middle and low income countries, it is the better-off who are increasing their resort to TM and CAM while the poor are tending to lose their access to the natural resources required for them as well as the knowledge. 4
---- Continued The costs of modern conventional medicine are becoming difficult for even the developed countries to bear, and TM tends to be less expensive. The iatrogenesis of modern medicine is increasingly being recognised (a high proportion of hospital admissions in the USA) There is a real threat of resistance levels to antibiotics increasing to such levels that other regimens have to be sought, and there are presently few lines of research for newer antibiotics. The doctors of modern medicine are reluctant to live and work in rural areas. Thus, multiple reasons for examining the potential role of TM -popular choice, a scientific need, a financial need, equity requirements -- and thereby a public health imperative. 5
The Assumptions That TM has inherent value and efficacy for health promotion, prevention and treatment; with areas of strength and limitations [based on growing evidence from bio-medical research as well as people’s experiential knowledge—NIH-USA studies, WHO-Global Atlas, ICMR and CCRAS] Thus it provides optional approaches to health care other than modern medicine, and measures for health problems that are sometimes complementary or supplementary to MM. Thereby ‘mainstreaming TM’ will be useful for all sections of the population—rural and urban, poor and rich, male and female. 6
Therefore , TM should be part of the ‘health coverage’ to be universalised Then What would ‘Health Coverage’ mean? Health Coverage=Access to Rational Health Care Need & Health Care = Self care, community level primary care, to secondary and tertiary institutional care of TM and MM 7
WHAT WOULD THIS REQUIRE OF HEALTH SYSTEMS AND HEALTH POLICY? q. Examining the situation of TM in the given country or region q. Analysing its Strengths and Weaknesses, Opportunities and Threats q. Developing a framework for the potential role of TM in health care in that country/region q. Identifying the gaps in performance of the potential role q. Planning to fill the gaps so as to optimise the benefits of all health knowledge q. Implementing the plans so that the coverage of TM reaches all 8

THE INDIAN CONTEXT 9
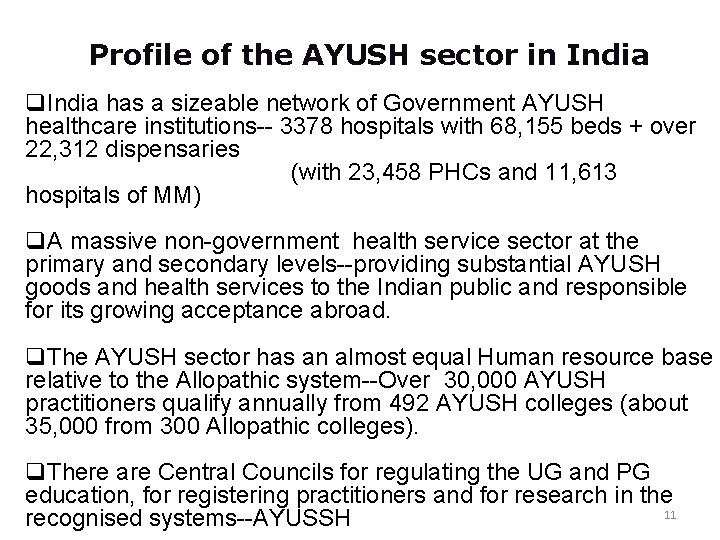
7 officially recognised systems of TM with their systematised knowledge, texts and live practice + orally transmitted Local Health Traditions 10
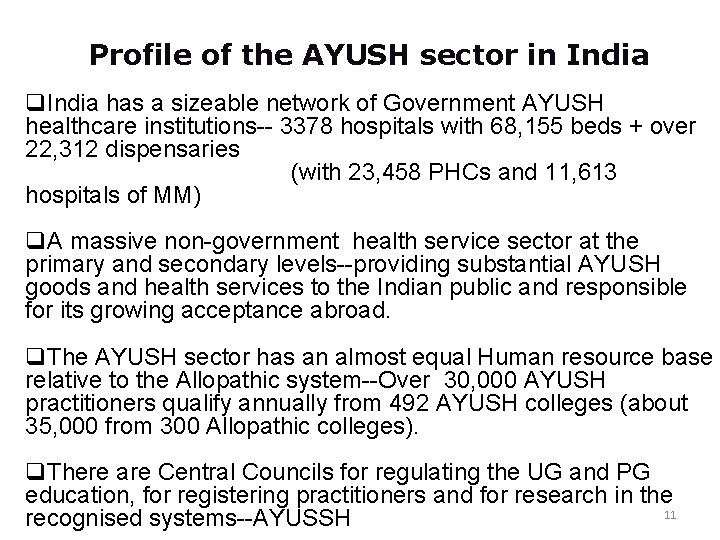
Profile of the AYUSH sector in India q. India has a sizeable network of Government AYUSH healthcare institutions-- 3378 hospitals with 68, 155 beds + over 22, 312 dispensaries (with 23, 458 PHCs and 11, 613 hospitals of MM) q. A massive non-government health service sector at the primary and secondary levels--providing substantial AYUSH goods and health services to the Indian public and responsible for its growing acceptance abroad. q. The AYUSH sector has an almost equal Human resource base relative to the Allopathic system--Over 30, 000 AYUSH practitioners qualify annually from 492 AYUSH colleges (about 35, 000 from 300 Allopathic colleges). q. There are Central Councils for regulating the UG and PG education, for registering practitioners and for research in the 11 recognised systems--AYUSSH
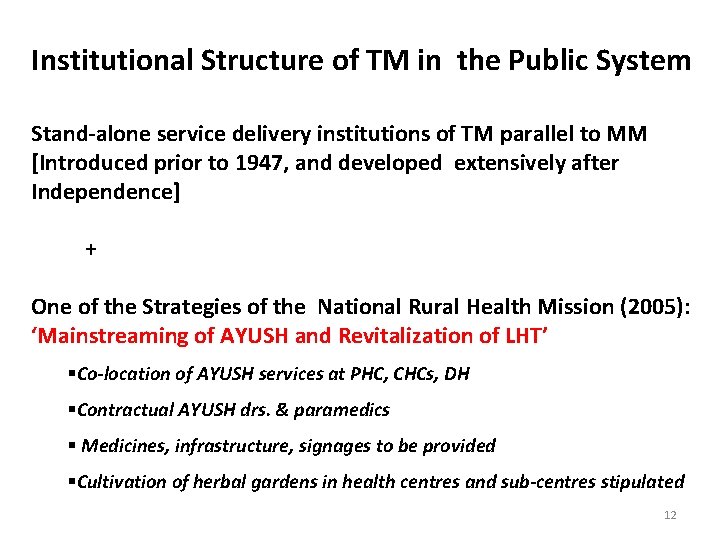
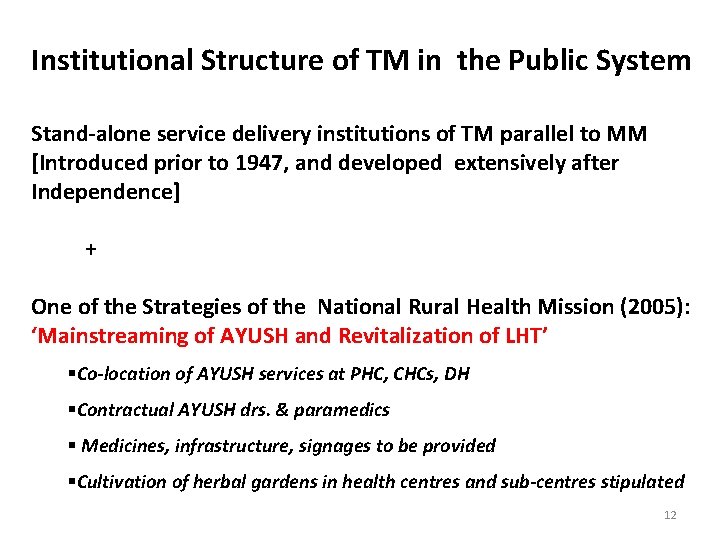
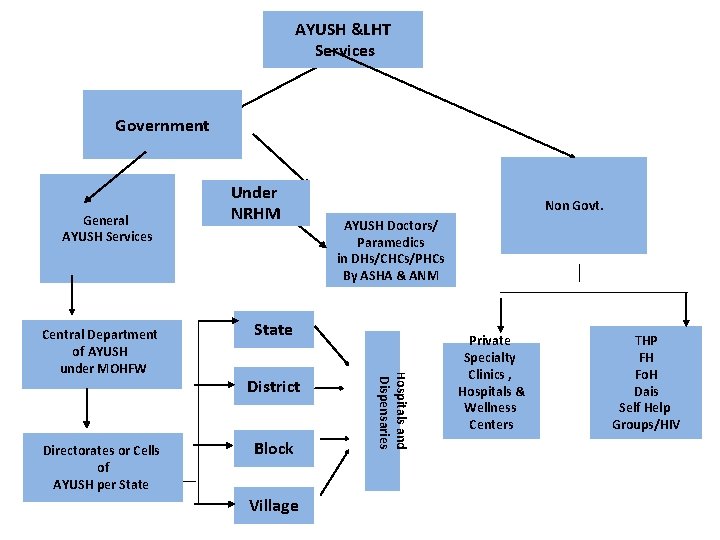
Institutional Structure of TM in the Public System Stand-alone service delivery institutions of TM parallel to MM [Introduced prior to 1947, and developed extensively after Independence] + One of the Strategies of the National Rural Health Mission (2005): ‘Mainstreaming of AYUSH and Revitalization of LHT’ §Co-location of AYUSH services at PHC, CHCs, DH §Contractual AYUSH drs. & paramedics § Medicines, infrastructure, signages to be provided §Cultivation of herbal gardens in health centres and sub-centres stipulated 12
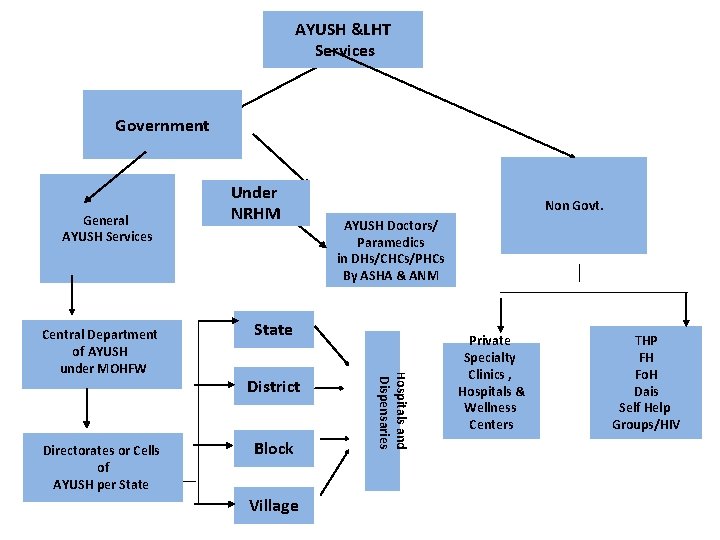
AYUSH &LHT Services Government General AYUSH Services Directorates or Cells of AYUSH per State Non Govt. AYUSH Doctors/ Paramedics in DHs/CHCs/PHCs By ASHA & ANM State District Block Village Hospitals and Dispensaries Central Department of AYUSH under MOHFW Under NRHM Private Specialty Clinics , Hospitals & Wellness Centers THP FH Fo. H Dais Self Help Groups/HIV
However: BUDGETRAY ALLOCATION ONLY 3% OF TOTAL CENTRAL HEALTH BUDGET NO CONCERN FOR QUALITY OF SERVICES 14
In 2008: q. No assessment of the quality or degree of utilisation of services found (only one assessment by Ferguson and Co. of Centrally Sponsored Schemes) q. Impression of most health administrators seemed to be that the AYUSH services are all defunct and ill-used. q. The role of ‘co-location’ was perceived by the central ministry and NRHM to be to provide substitutes for the missing MM doctors in rural areas. q. Argued by saying that now there is no demand for the services of these systems. q. But anthropological studies had demonstrated wide use, impressions of health system researchers with community experience tended to corroborate this, but nothing was known of the public services. 15
Therefore conducted an exploratory study across 18 states to answer the following questions: q. Present demand for AYUSH services and use of LHT q. Access to AYUSH services and LHT--Is co-location improving coverage? Is it ‘revitalising LHT’? q. Quality of services as assessed by public health management criteria, by AYUSH criteria, and by the demand for services. q. Potential Role of AYUSH and LHT in ‘Architectural correction’ of the health service system (with decentralization, context specific flexibility and communitisation as its principles) q What needs to be done to ensure AYUSH providers and LHT fulfil that potential? 16
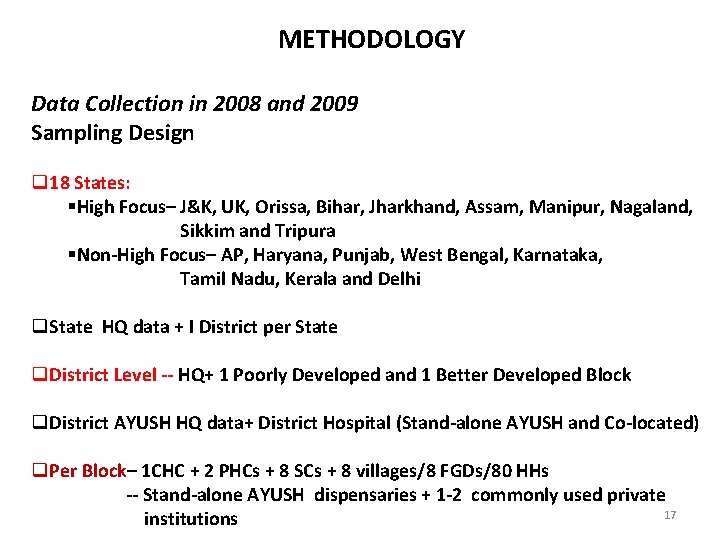
METHODOLOGY Data Collection in 2008 and 2009 Sampling Design q 18 States: §High Focus– J&K, UK, Orissa, Bihar, Jharkhand, Assam, Manipur, Nagaland, Sikkim and Tripura §Non-High Focus– AP, Haryana, Punjab, West Bengal, Karnataka, Tamil Nadu, Kerala and Delhi q. State HQ data + I District per State q. District Level -- HQ+ 1 Poorly Developed and 1 Better Developed Block q. District AYUSH HQ data+ District Hospital (Stand-alone AYUSH and Co-located) q. Per Block– 1 CHC + 2 PHCs + 8 SCs + 8 villages/8 FGDs/80 HHs -- Stand-alone AYUSH dispensaries + 1 -2 commonly used private 17 institutions
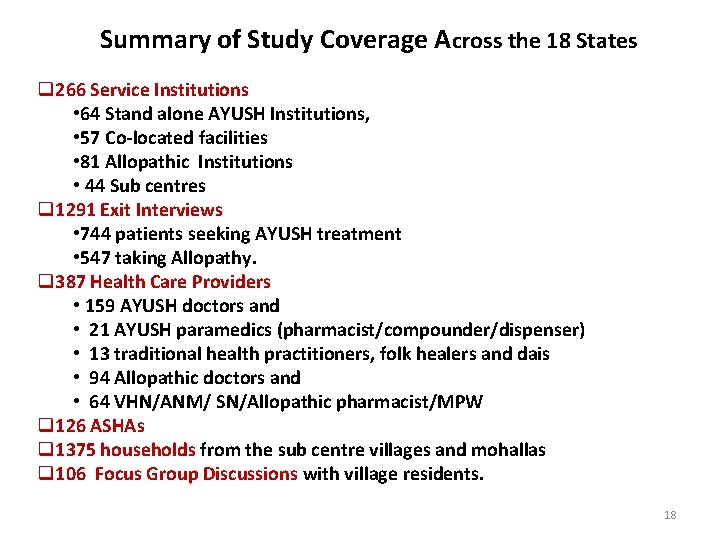
Summary of Study Coverage Across the 18 States q 266 Service Institutions • 64 Stand alone AYUSH Institutions, • 57 Co-located facilities • 81 Allopathic Institutions • 44 Sub centres q 1291 Exit Interviews • 744 patients seeking AYUSH treatment • 547 taking Allopathy. q 387 Health Care Providers • 159 AYUSH doctors and • 21 AYUSH paramedics (pharmacist/compounder/dispenser) • 13 traditional health practitioners, folk healers and dais • 94 Allopathic doctors and • 64 VHN/ANM/ SN/Allopathic pharmacist/MPW q 126 ASHAs q 1375 households from the sub centre villages and mohallas q 106 Focus Group Discussions with village residents. 18
MAJOR FINDINGS Highly variable results across the Indian states Demand Generally High: 20 -98% households had used AYUSH services in last 3 months Home remedies used by 5 -70% of exit interview respondents for presenting complaint Utilisation of public services range: • Stand-alone= 8 - 78 OP attendance /facility/day • Co-located = 1 - 75 OP attendance /facility/day • Relative to Allopathic = 20% - 60% Utilisation directly related with quality of AYUSH services Not directly related to quality or coverage of public services of MM 19
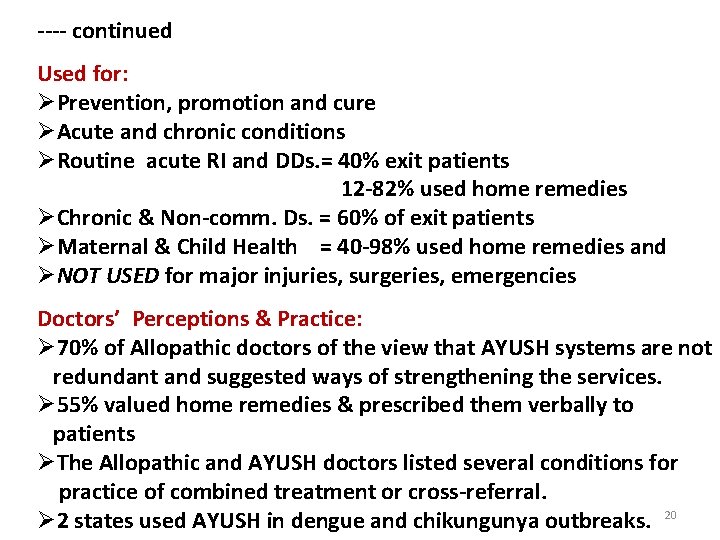
---- continued Used for: ØPrevention, promotion and cure ØAcute and chronic conditions ØRoutine acute RI and DDs. = 40% exit patients 12 -82% used home remedies ØChronic & Non-comm. Ds. = 60% of exit patients ØMaternal & Child Health = 40 -98% used home remedies and ØNOT USED for major injuries, surgeries, emergencies Doctors’ Perceptions & Practice: Ø 70% of Allopathic doctors of the view that AYUSH systems are not redundant and suggested ways of strengthening the services. Ø 55% valued home remedies & prescribed them verbally to patients ØThe Allopathic and AYUSH doctors listed several conditions for practice of combined treatment or cross-referral. Ø 2 states used AYUSH in dengue and chikungunya outbreaks. 20
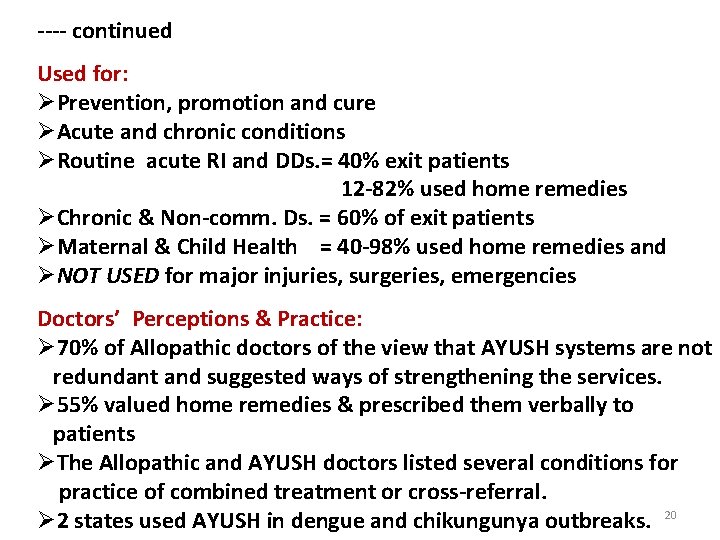
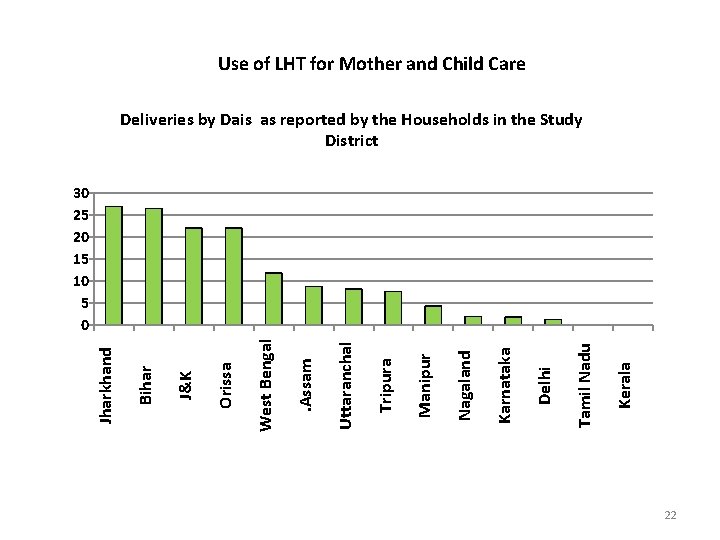
0 Karnataka J&K Haryana Delhi Tamil Nadu Punjab Jharkhand West Bengal Assam Sikkim Orissa Uttarakhand Andhra Pradesh Kerala Nagaland Bihar Tripura Manipur %response Use of LHT for Mother and Child Care Use of Home remedies for Baby's health by the Households in the study District 120 100 80 60 40 20 21
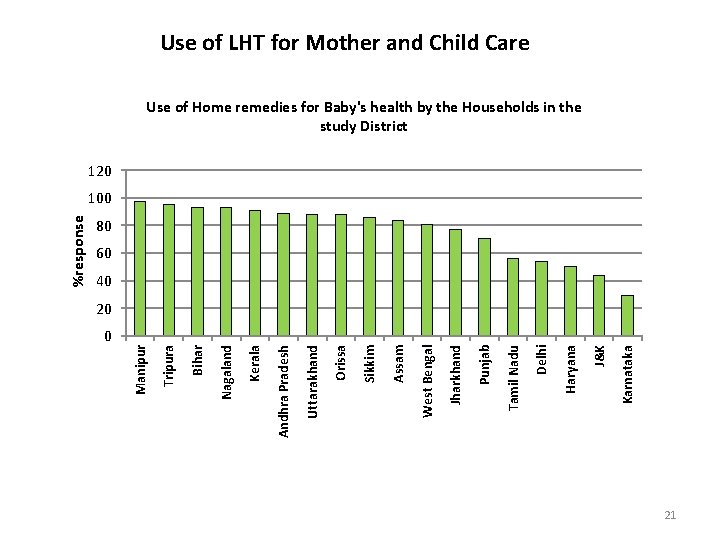
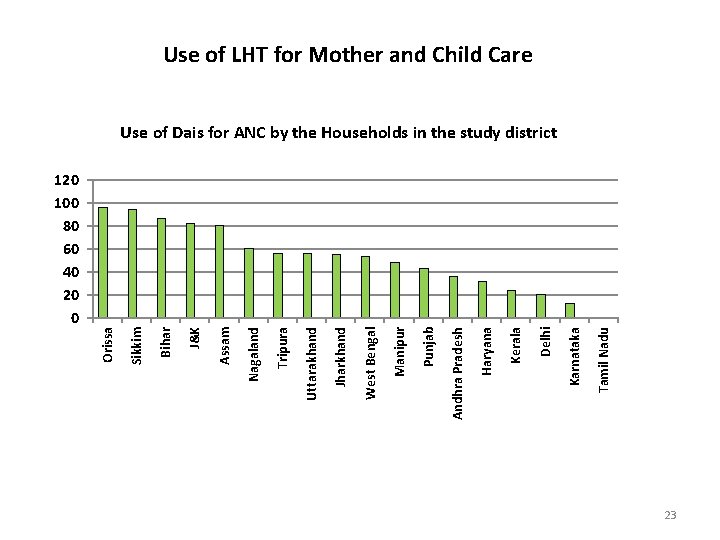
Use of LHT for Mother and Child Care Deliveries by Dais as reported by the Households in the Study District Kerala Tamil Nadu Delhi Karnataka Nagaland Manipur Tripura Uttaranchal . Assam West Bengal Orissa J&K Bihar Jharkhand 30 25 20 15 10 5 0 22
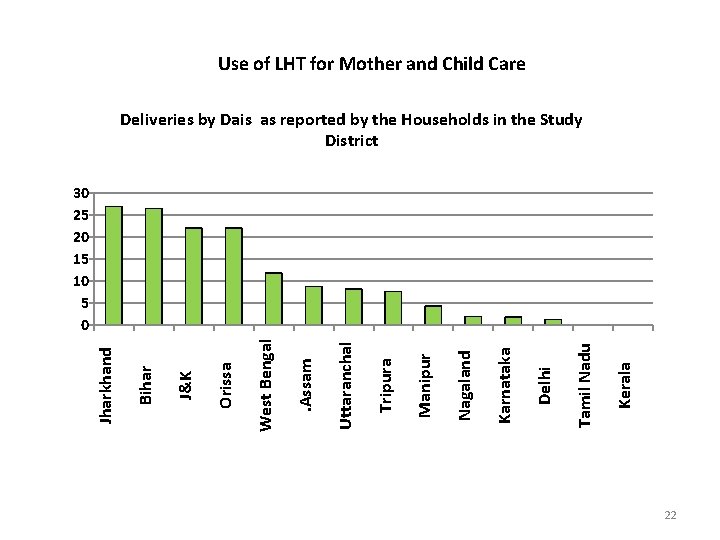
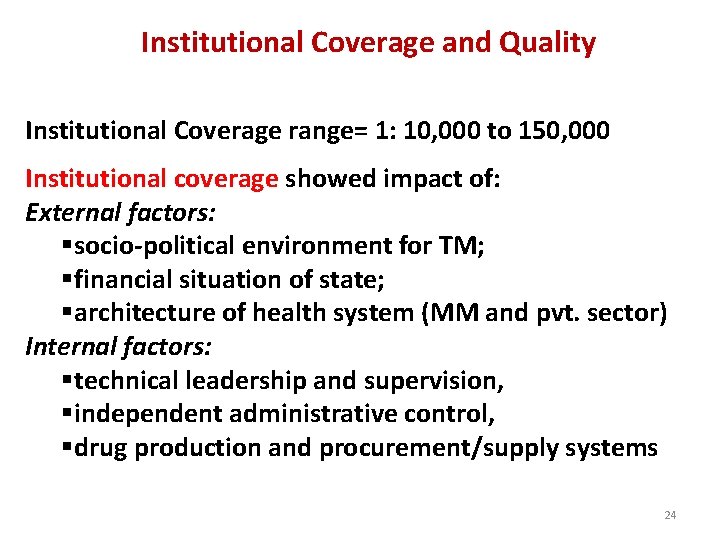
120 100 80 60 40 20 0 Tamil Nadu Karnataka Delhi Kerala Haryana Andhra Pradesh Punjab Manipur West Bengal Jharkhand Uttarakhand Tripura Nagaland Assam J&K Bihar Sikkim Orissa Use of LHT for Mother and Child Care Use of Dais for ANC by the Households in the study district 23
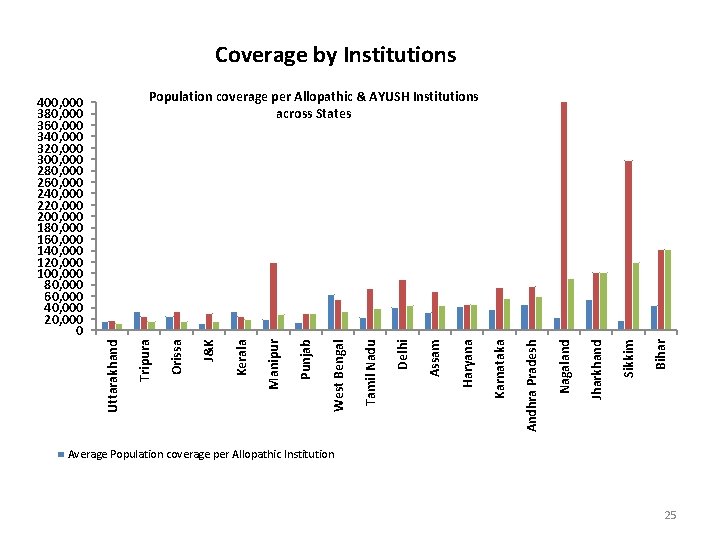
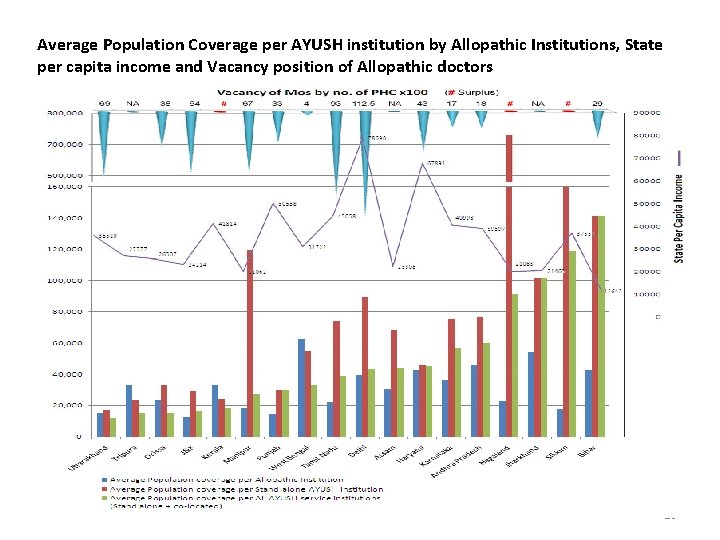
Institutional Coverage and Quality Institutional Coverage range= 1: 10, 000 to 150, 000 Institutional coverage showed impact of: External factors: §socio-political environment for TM; §financial situation of state; §architecture of health system (MM and pvt. sector) Internal factors: §technical leadership and supervision, §independent administrative control, §drug production and procurement/supply systems 24
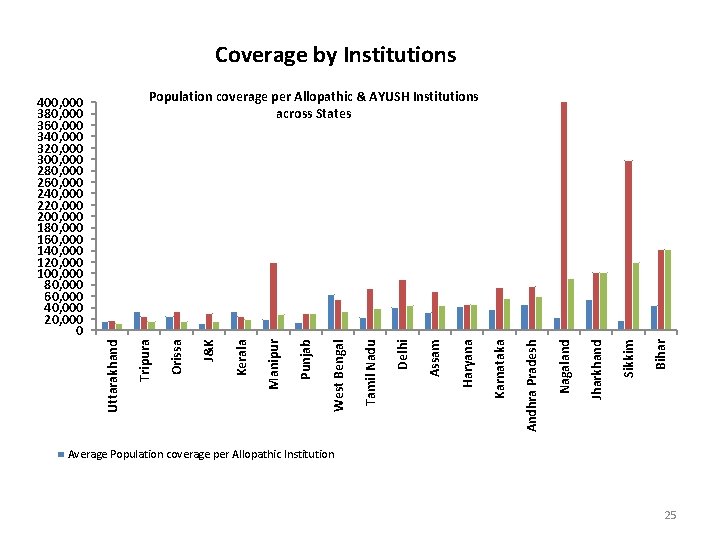
Coverage by Institutions Bihar Sikkim Jharkhand Nagaland Andhra Pradesh Karnataka Haryana Assam Delhi Tamil Nadu West Bengal Punjab Manipur Kerala J&K Orissa Uttarakhand Tripura Population coverage per Allopathic & AYUSH Institutions across States 400, 000 380, 000 360, 000 340, 000 320, 000 300, 000 280, 000 260, 000 240, 000 220, 000 200, 000 180, 000 160, 000 140, 000 120, 000 100, 000 80, 000 60, 000 40, 000 20, 000 0 Average Population coverage per Allopathic Institution 25
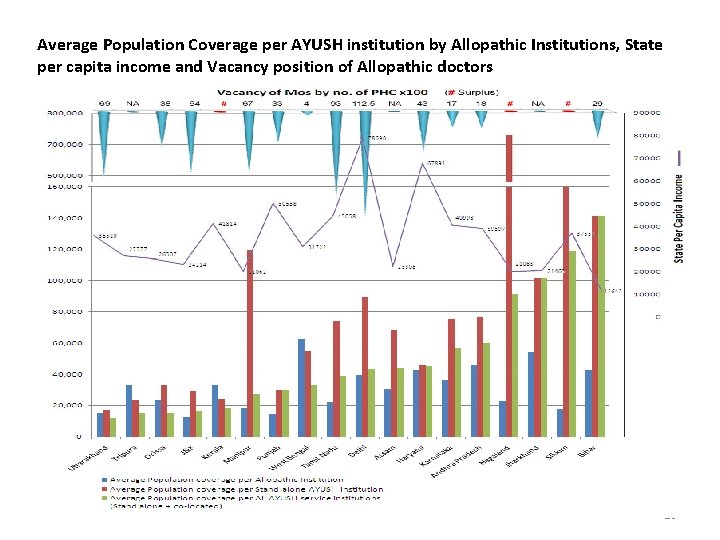
Average Population Coverage per AYUSH institution by Allopathic Institutions, State per capita income and Vacancy position of Allopathic doctors 26
Quality Determinants: Generally good in the states with good quality of Allopathic services—indicating the political/policy environment Financial situation of the State Technical leadership & supervision Stand-alone of better quality than co-located, except in states with earlier co-location 27
![Quality of Service Stand aloneColocated Criteria for Grading Quality InfrastructureBldingspace cleanliness signages waterelec Quality of Service [Stand alone/Co-located] Criteria for Grading Quality: • Infrastructure—Blding/space, cleanliness, signages, water&elec](https://slidetodoc.com/presentation_image/4de6bd606794659a4cf27c233f812f83/image-28.jpg)
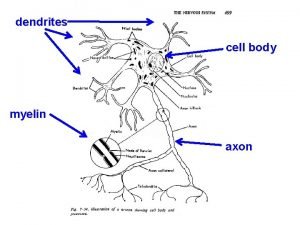
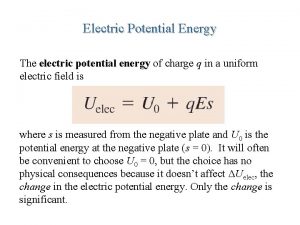
Quality of Service [Stand alone/Co-located] Criteria for Grading Quality: • Infrastructure—Blding/space, cleanliness, signages, water&elec • AYUSH Drug Supply– Present; Inadequate/ Adequate • Human Resources– Doctor / Paramedic • Record Keeping– Regular OPD & Indoor patient records • Additional inputs—herbal gardens, staff residence Findings: ØStand-alone grading better in all states, except 2 where it is same. ØGood for Co-located where they have stabilised over time. ØBetter in the Non-High focus states compared to the High focus. ØNo initiatives for ‘revitaising LHT’ in most states, except ASHAs 28 taught about medicinal plants; no herbal garden cultivation in hcs.
Validation of AYUSH Prescriptions at Exit Interview üAcross the 9 states, in general over 75% of the prescriptions used AYUSH medicines and approximately 25% of the prescriptions were outside. üHomeopathic prescriptions were found valid in 11 States and doctors used Modern terms and methods of diagnosis. üIn 3 States, they exclusively used Ayurveda terminology for diagnosis whereas in 4 they used a mix of Ayurvedic and modern terms. In 2 States they used only modern terms for diagnosis. üRaw herbs were rarely used by the doctors in the public system and they relied entirely on packaged medicine 29
Validation of Community Knowledge by AYUSH Texts and Principles üThe validation of community knowledge about medicinal value of foods was largely verified by the texts, from 75 -100% items were validated across states. üHowever there was also a substantial component of modern knowledge about nutritional value of food items, from 3 -25%, eg. About ‘green leafy vegetables’, or ‘a balanced diet’ ü Apart from plant based items, many food items with animal, mineral or sea origin were also part of the food items mentioned by the households. üFood items mentioned showed community specificity in terms of their geographical and cultural background. 30
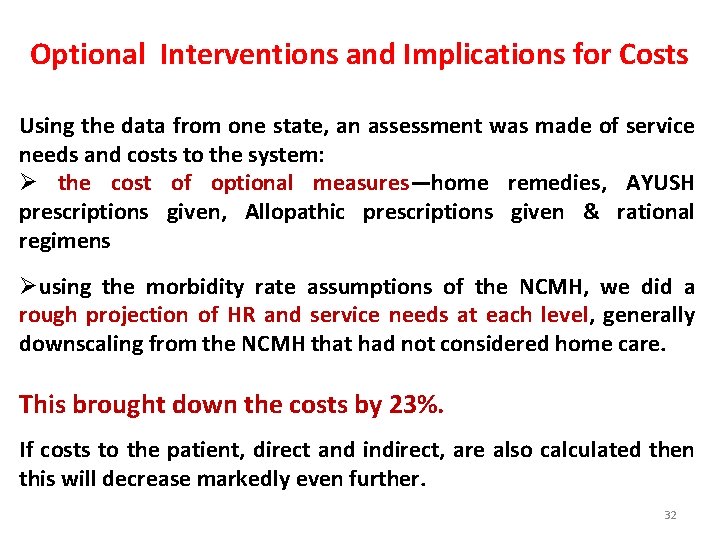
Findings related to Governance Issues q Diversity of AYUSH service development and LHT presence across states q Multiple determinants of Coverage and Quality across states-- encompassing issues of governance, management and the hierarchy of knowledge q No linkage of LHT with AYUSH in the public system— related Indian Public Health Standards not met q Co-located AYUSH falling between two stools; poor coordination between NRHM and Dept. of AYUSH q The present initiatives may lead to either “mainstreaming of AYUSH systems or merely mainstreaming of the AYUSH providers” depending on roles assigned to them—thereby 31 architectural correction may or may not happen.
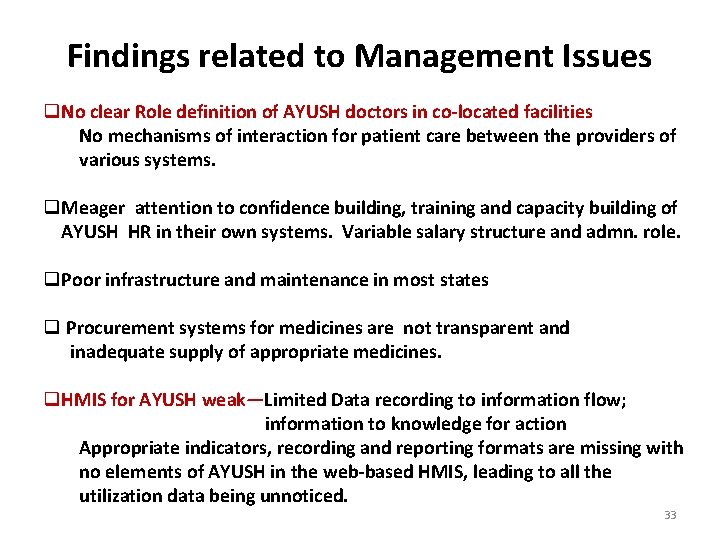
Optional Interventions and Implications for Costs Using the data from one state, an assessment was made of service needs and costs to the system: Ø the cost of optional measures—home remedies, AYUSH prescriptions given, Allopathic prescriptions given & rational regimens Øusing the morbidity rate assumptions of the NCMH, we did a rough projection of HR and service needs at each level, generally downscaling from the NCMH that had not considered home care. This brought down the costs by 23%. If costs to the patient, direct and indirect, are also calculated then this will decrease markedly even further. 32
Findings related to Management Issues q. No clear Role definition of AYUSH doctors in co-located facilities No mechanisms of interaction for patient care between the providers of various systems. q. Meager attention to confidence building, training and capacity building of AYUSH HR in their own systems. Variable salary structure and admn. role. q. Poor infrastructure and maintenance in most states q Procurement systems for medicines are not transparent and inadequate supply of appropriate medicines. q. HMIS for AYUSH weak—Limited Data recording to information flow; information to knowledge for action Appropriate indicators, recording and reporting formats are missing with no elements of AYUSH in the web-based HMIS, leading to all the utilization data being unnoticed. 33
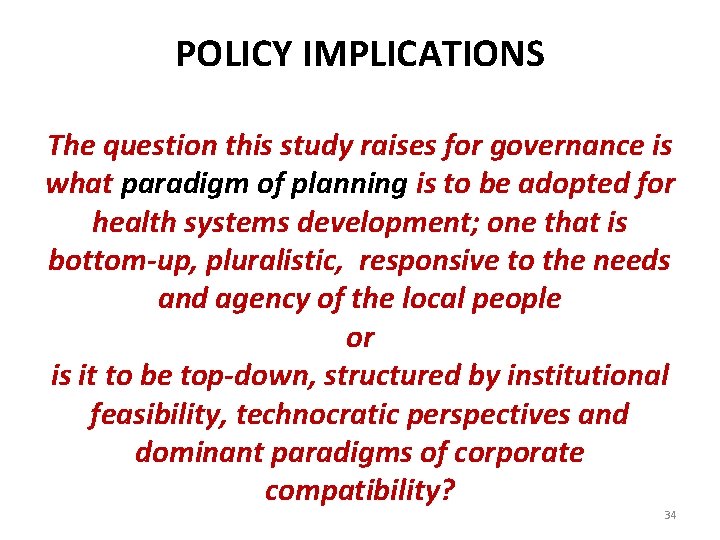
POLICY IMPLICATIONS The question this study raises for governance is what paradigm of planning is to be adopted for health systems development; one that is bottom-up, pluralistic, responsive to the needs and agency of the local people or is it to be top-down, structured by institutional feasibility, technocratic perspectives and dominant paradigms of corporate compatibility? 34
In the Indian context it seems to be expedient that we: §Define the role of the services of TM, and §Address the gaps in quality of TM services §Develop systems to document, validate and promote LHT §Among all sections of the population, promote use of TM as validated §Develop mechanisms for integrated use of the strengths of each system and promote their use §Develop institutional capacity to undertake these tasks Detailed exercises have been done that can be examined This would be the most cost effective, non-iatrogenic and 35 sustainable way to develop universal coverage.
IF UNIVERSAL HEALTH COVERAGE IS ABOUT DEMOCRATIC HEALTH SERVICE SYSTEMS, THEN WE WILLL HAVE TO THINK INNOVATIVELY TOWARDS A PLURALISTIC APPROACH TO HEALTH KNOWLEDGE, PEOPLE CENTRE-STAGE AND AS ACTORS WITH THEIR OWN AGENCY THANK YOU!! The National Health Systems Resource Centre, NRHM, GOI & The Centre of Social Medicine & Community Health, Jawaharlal Nehru University (ritu_priya_jnu@yahoo. com) (drshweta. nhsrc@gmail. com) 36
 Madar kabab chini tagar are the example of
Madar kabab chini tagar are the example of Protection mainstreaming principles
Protection mainstreaming principles What is gender mainstreaming?
What is gender mainstreaming? What is gender mainstreaming?
What is gender mainstreaming? Environmental mainstreaming tools
Environmental mainstreaming tools Sex videao
Sex videao Gender mainstreaming
Gender mainstreaming Mainstreaming in swahili
Mainstreaming in swahili Role of occupational health nurse
Role of occupational health nurse Who traditional medicine strategy: 2014-2023
Who traditional medicine strategy: 2014-2023 New york college of traditional chinese medicine
New york college of traditional chinese medicine Medicine wheel colors in order
Medicine wheel colors in order The acquisition of a traditional masculine or feminine role
The acquisition of a traditional masculine or feminine role Flaccid cell
Flaccid cell Flaccid turgid and plasmolysis
Flaccid turgid and plasmolysis Calculating solute potential
Calculating solute potential Graded potential vs action potential
Graded potential vs action potential Graded potential
Graded potential Graded potentials
Graded potentials Difference between action and graded potential
Difference between action and graded potential Graded potential
Graded potential Water potential
Water potential Source of bioelectric potential is dash in nature
Source of bioelectric potential is dash in nature Transmission across a synapse
Transmission across a synapse Suggmadex
Suggmadex Action potential resting potential
Action potential resting potential Action potential resting potential
Action potential resting potential Market potential and forecasting
Market potential and forecasting Define electric potential and potential difference.
Define electric potential and potential difference. Volts to ev
Volts to ev Electric potential and potential difference
Electric potential and potential difference Potential due to a dipole
Potential due to a dipole Electrical potential energy
Electrical potential energy Peelectric
Peelectric Electric potential
Electric potential Web role in azure
Web role in azure Interaktionistisches rollenmodell
Interaktionistisches rollenmodell