Laparoscopic NerveSparing Radical Hysterectomy Prof Dr Metin apar
- Slides: 31
Laparoscopic Nerve-Sparing Radical Hysterectomy Prof. Dr. Metin Çapar Karatay University Faculty of Medicine OBS&GYNECOLOGY Konya /TURKEY
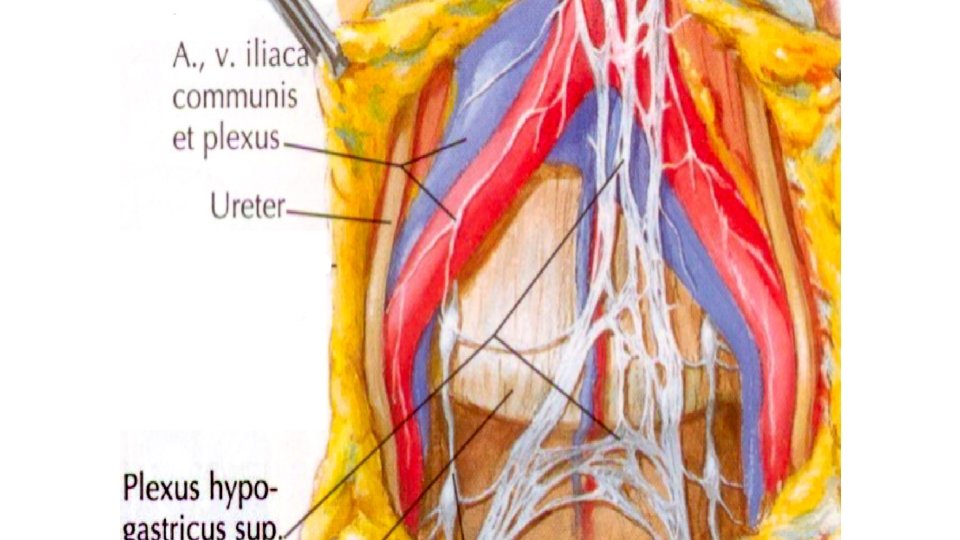
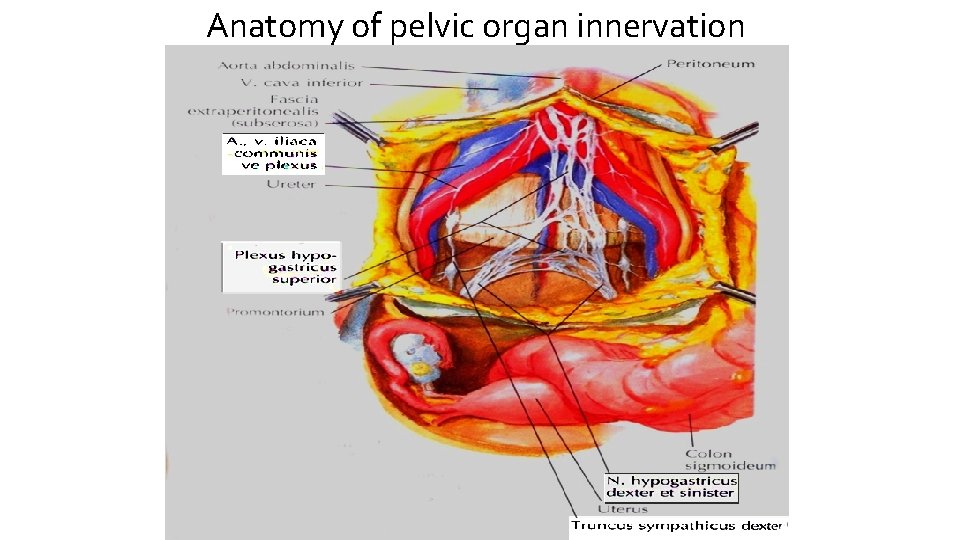
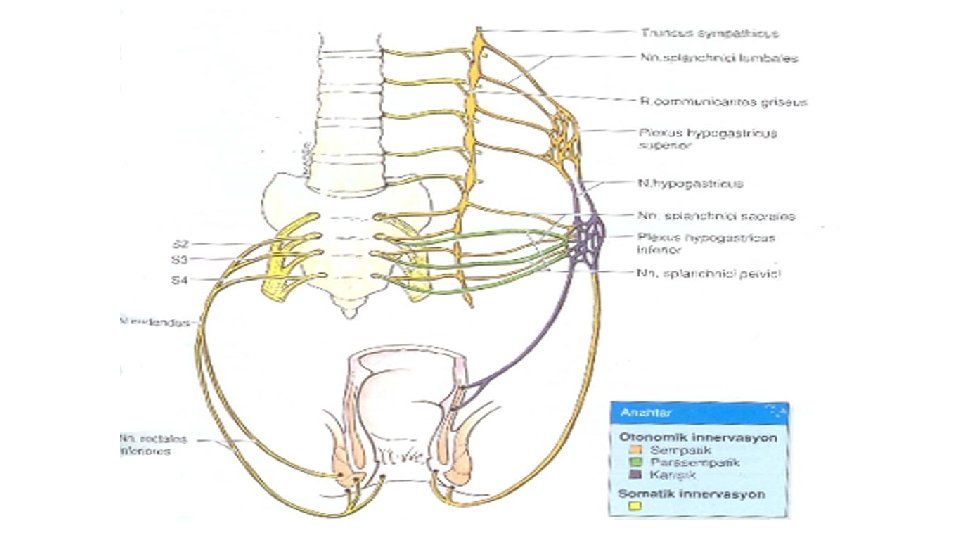
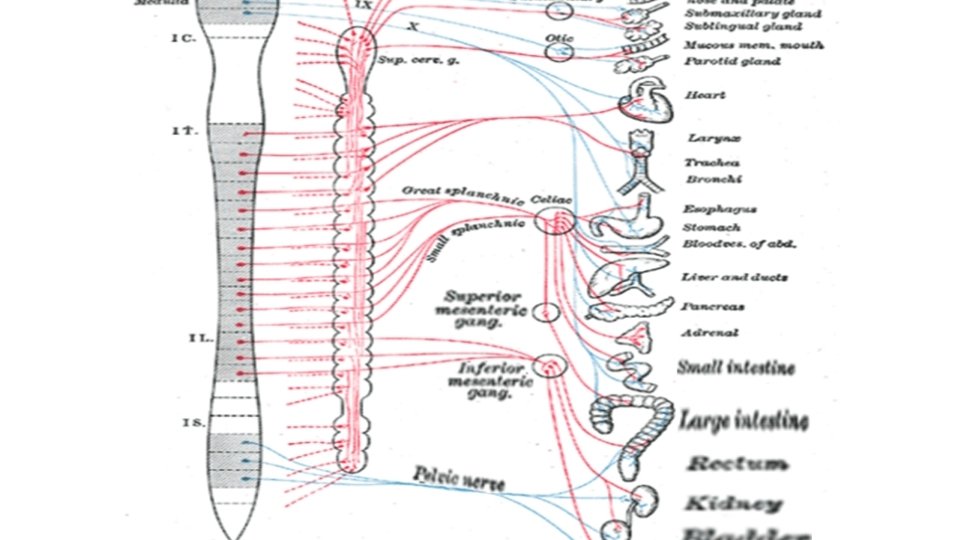
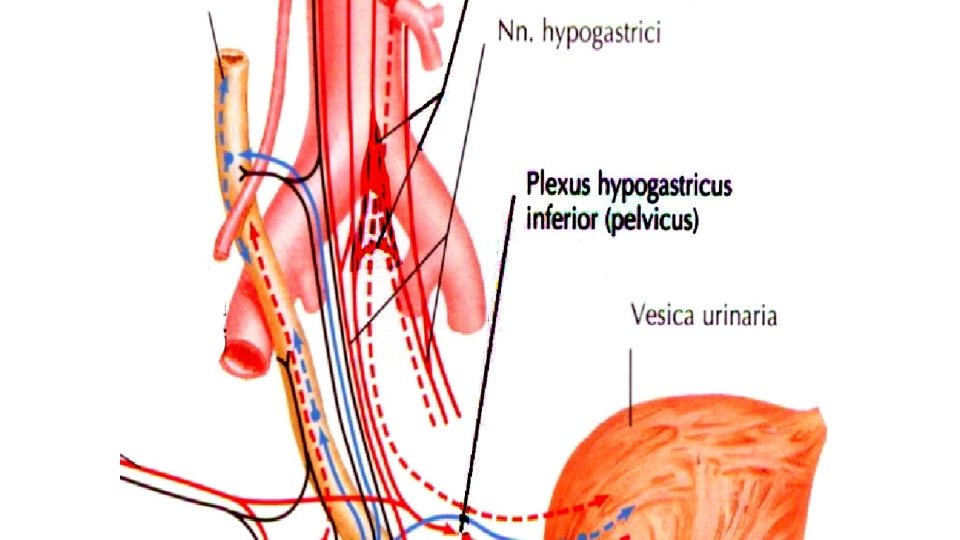
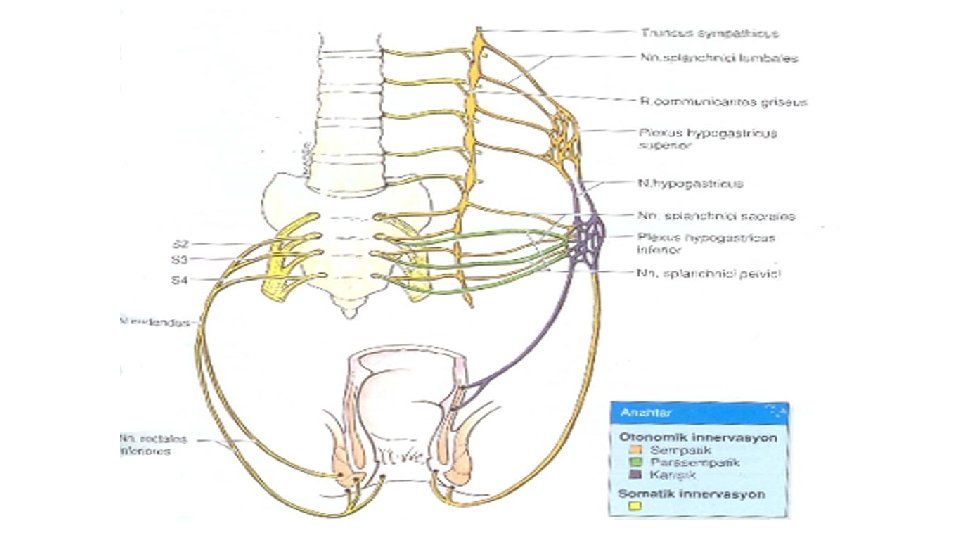
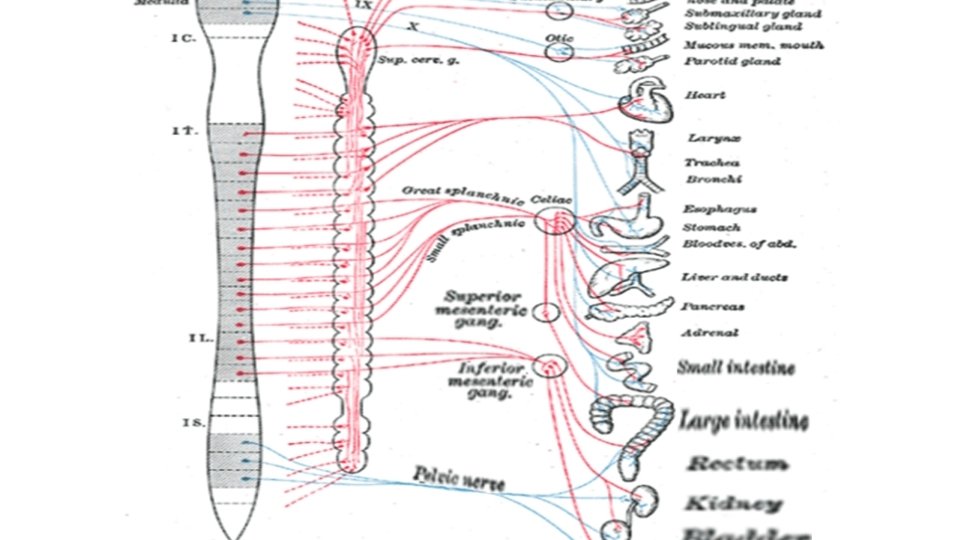
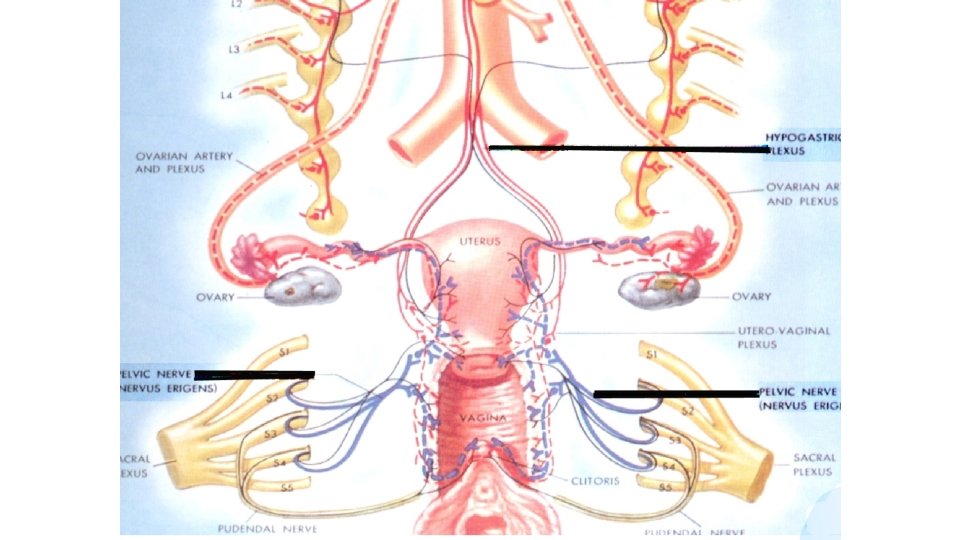
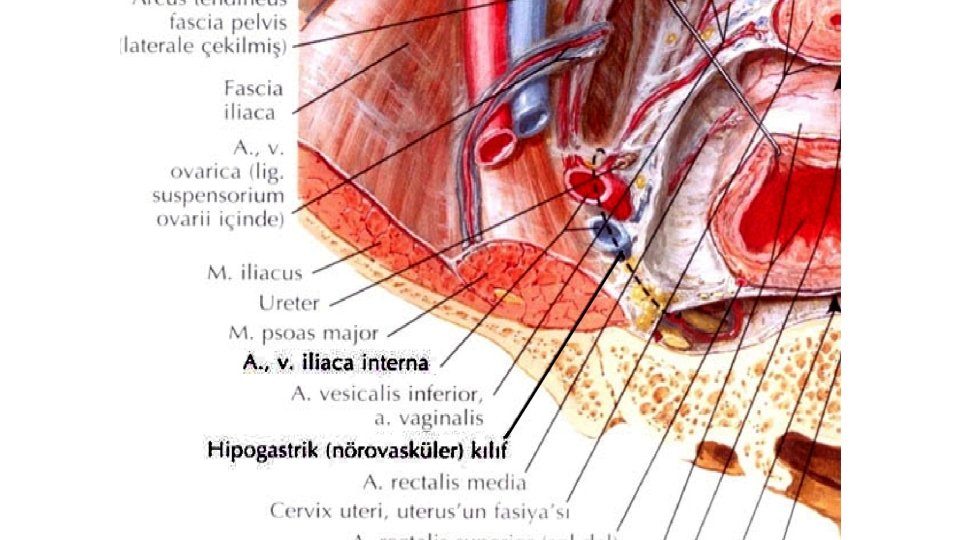
Superior hypogastric plexus(SHP) Ø It begins at the aortal bifurcation and continues through the presacral area to the pelvis. Ø It contains mostly sympathetic nerves from T 12 -L 2 segments of the spinal cord), Ø It also contains some fibres from L 1 -2 splanchnic nerves. Ø It caudally and laterally leads to the right and left hypogastric nerves.
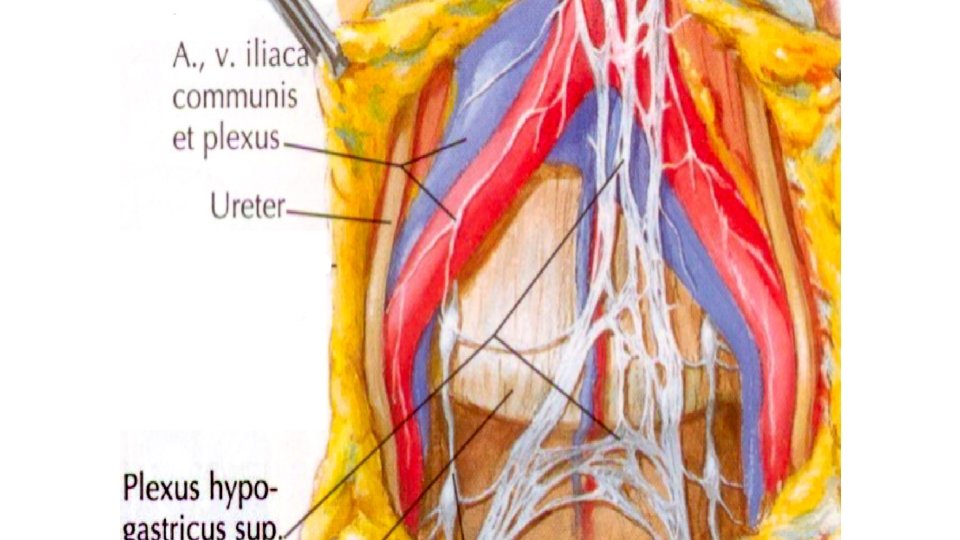
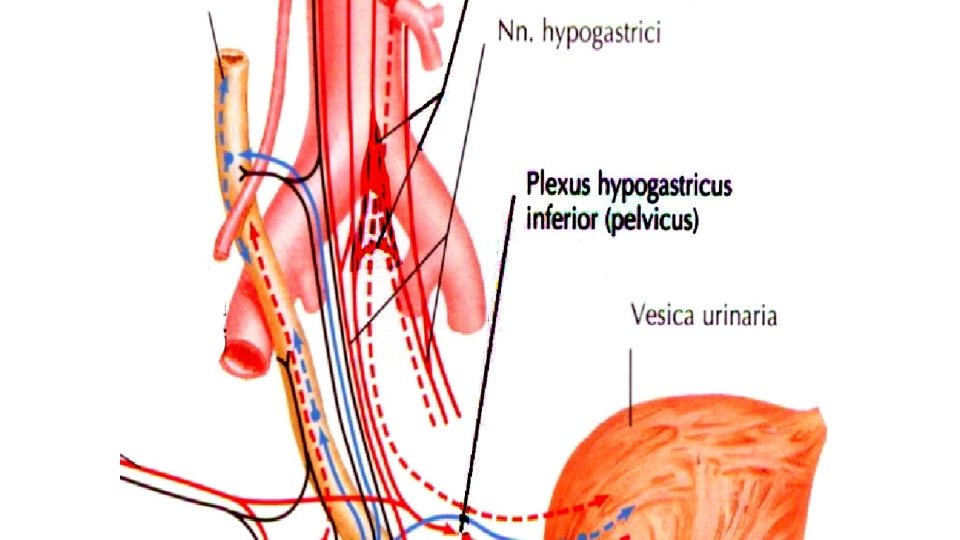
• hypogastric nerve is a term for the transition between the superior hypogastric plexus and the inferior hypogastric plexus. The hypogastric nerve enters the sympathetic chain at T 10 -L 2.
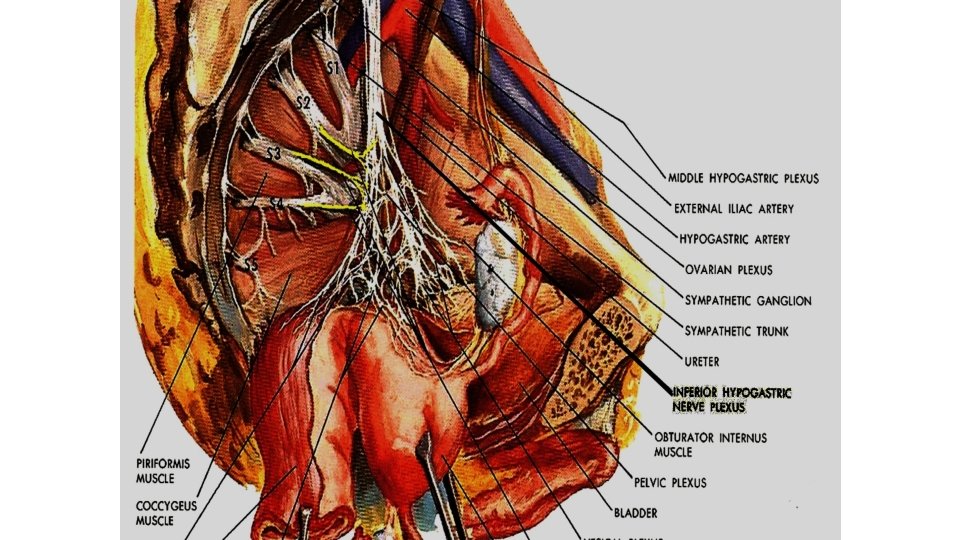
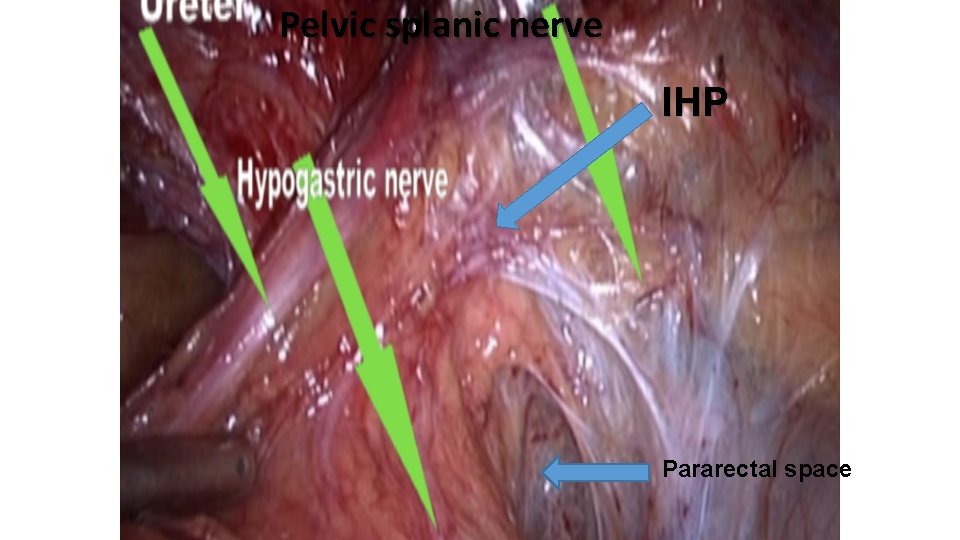
Inferior hypogastric(IHP) The inferior hypogastric plexus(IHP) is a condensation of nerve elements, fibres, and ganglia. It is composed of sympathetic fibres from hypogastric nerve and parasympathetic nerves from pelvic splanchnic nerve
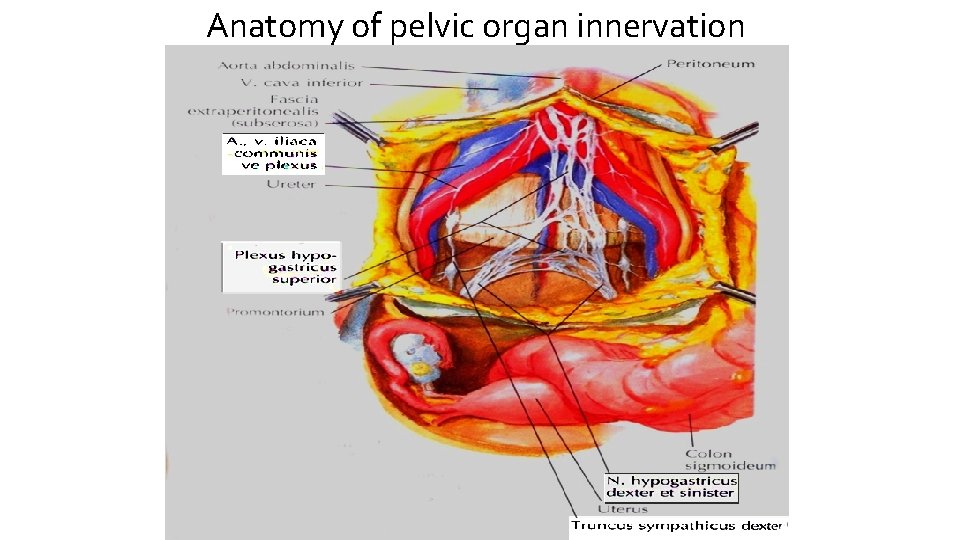
Anatomy of pelvic organ innervation
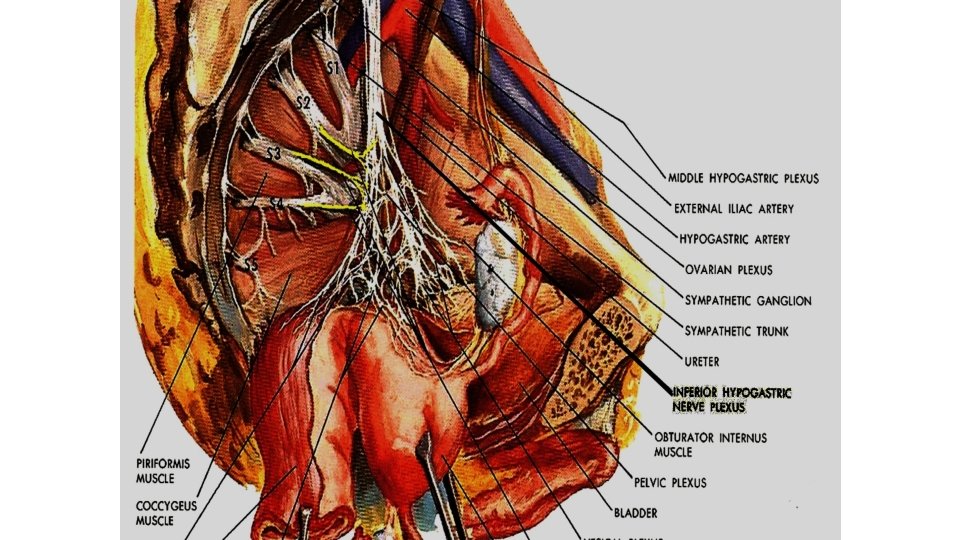
• The inferior hypogastric plexus is a paired structure, with each situated on the side of the rectum in the male, and at the sides of the rectum and vagina in the female.
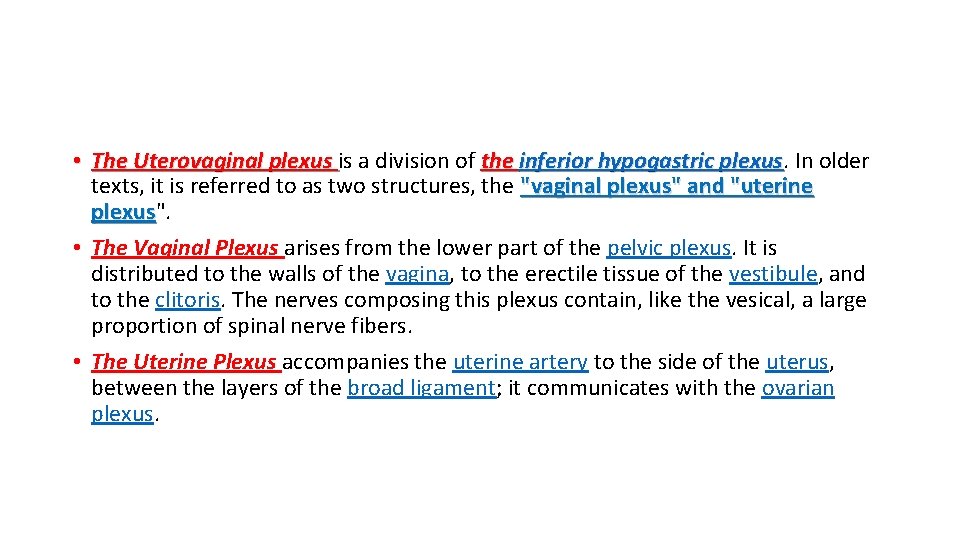
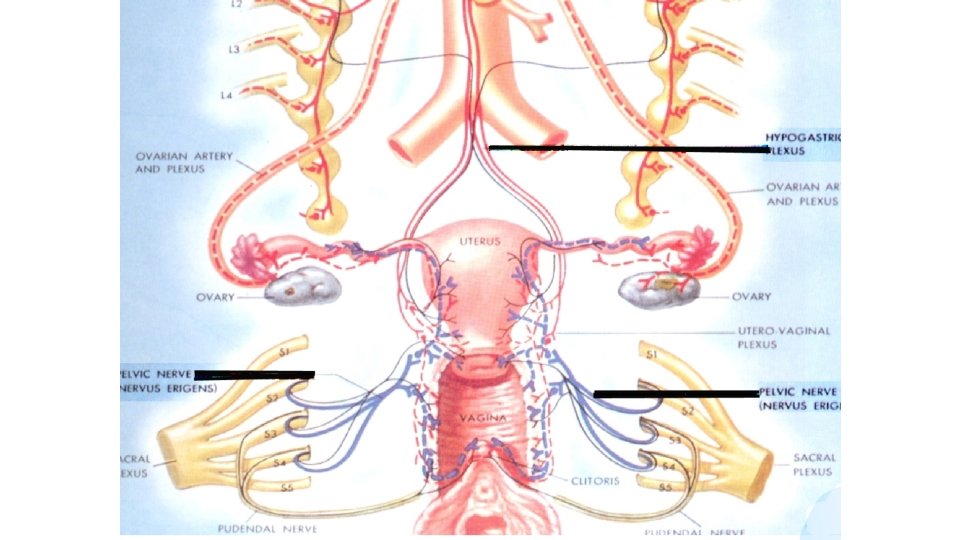
• The Uterovaginal plexus is a division of the inferior hypogastric plexus In older texts, it is referred to as two structures, the "vaginal plexus" and "uterine plexus". plexus • The Vaginal Plexus arises from the lower part of the pelvic plexus. It is distributed to the walls of the vagina, to the erectile tissue of the vestibule, and to the clitoris. The nerves composing this plexus contain, like the vesical, a large proportion of spinal nerve fibers. • The Uterine Plexus accompanies the uterine artery to the side of the uterus, between the layers of the broad ligament; it communicates with the ovarian plexus.
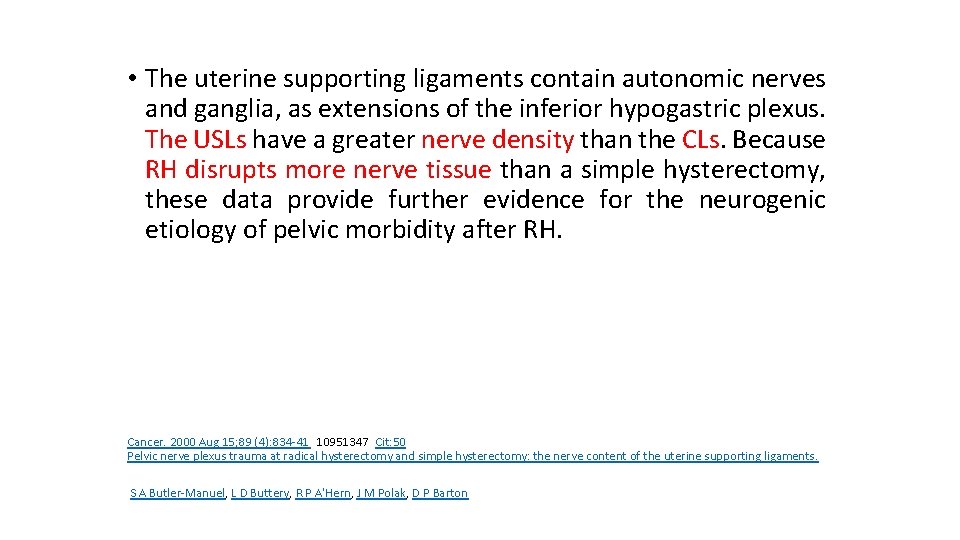
• The uterine supporting ligaments contain autonomic nerves and ganglia, as extensions of the inferior hypogastric plexus. The USLs have a greater nerve density than the CLs. Because RH disrupts more nerve tissue than a simple hysterectomy, these data provide further evidence for the neurogenic etiology of pelvic morbidity after RH. Cancer. 2000 Aug 15; 89 (4): 834 -41 10951347 Cit: 50 Pelvic nerve plexus trauma at radical hysterectomy and simple hysterectomy: the nerve content of the uterine supporting ligaments. S A Butler-Manuel, L D Buttery, R P A'Hern, J M Polak, D P Barton
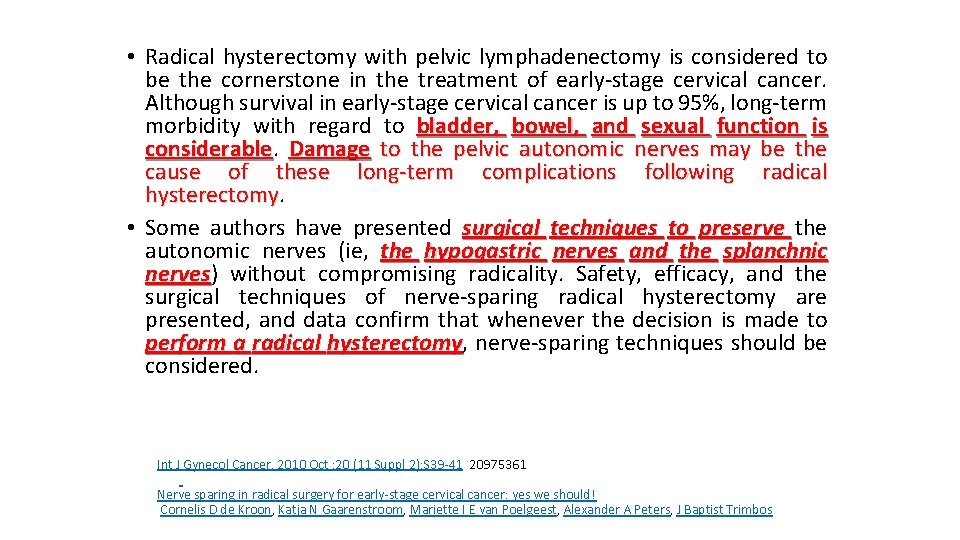
• Radical hysterectomy with pelvic lymphadenectomy is considered to be the cornerstone in the treatment of early-stage cervical cancer. Although survival in early-stage cervical cancer is up to 95%, long-term morbidity with regard to bladder, bowel, and sexual function is considerable Damage to the pelvic autonomic nerves may be the cause of these long-term complications following radical hysterectomy • Some authors have presented surgical techniques to preserve the autonomic nerves (ie, the hypogastric nerves and the splanchnic nerves) nerves without compromising radicality. Safety, efficacy, and the surgical techniques of nerve-sparing radical hysterectomy are presented, and data confirm that whenever the decision is made to perform a radical hysterectomy, hysterectomy nerve-sparing techniques should be considered. Int J Gynecol Cancer. 2010 Oct ; 20 (11 Suppl 2): S 39 -41 20975361 Nerve sparing in radical surgery for early-stage cervical cancer: yes we should! Cornelis D de Kroon, Katja N Gaarenstroom, Mariette I E van Poelgeest, Alexander A Peters, J Baptist Trimbos
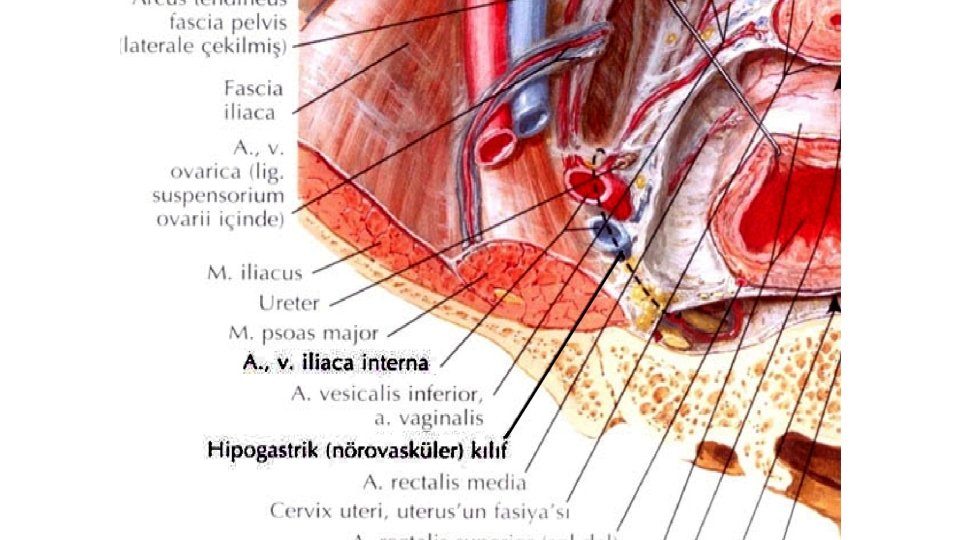
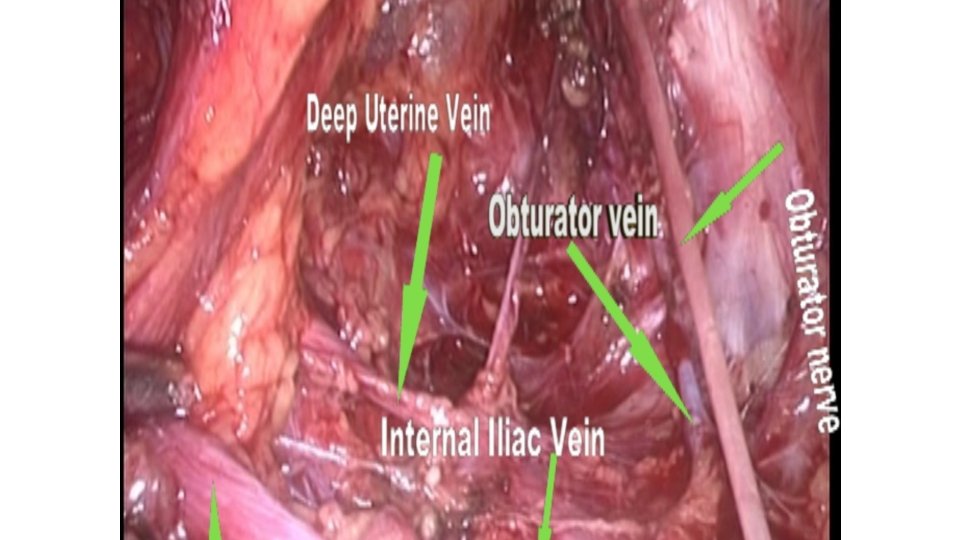
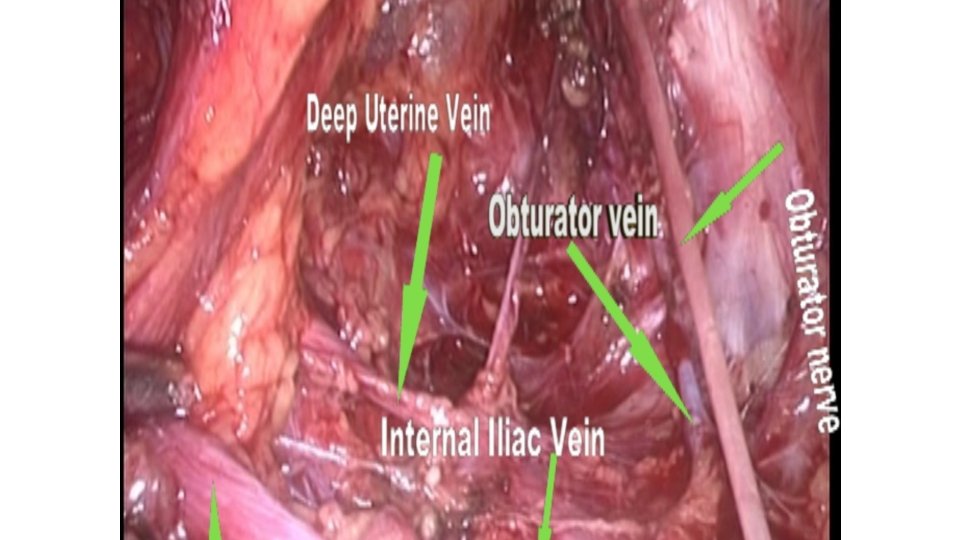
Deep uterine vein(DUV) It collect blood from uterine and bladder and connect to internal iliac vein, Just beyond the PSN
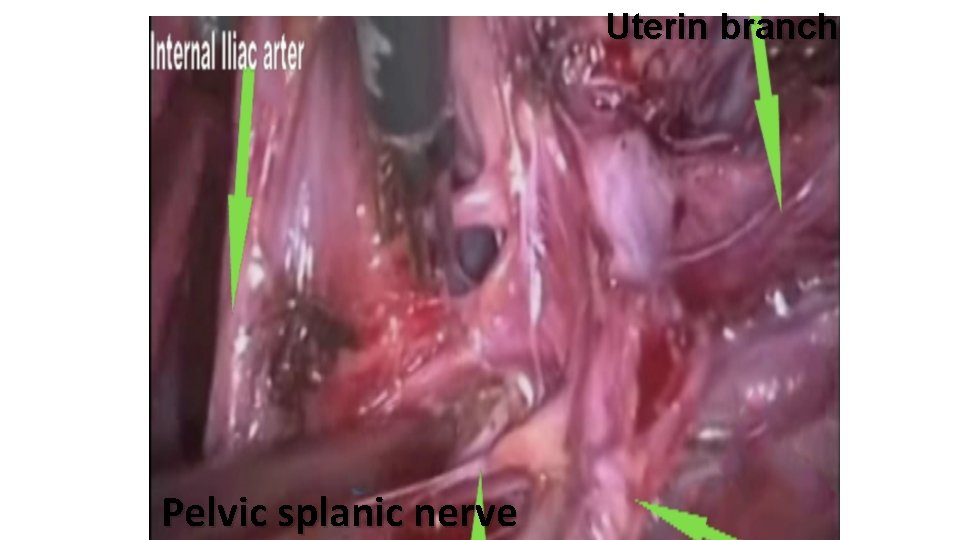
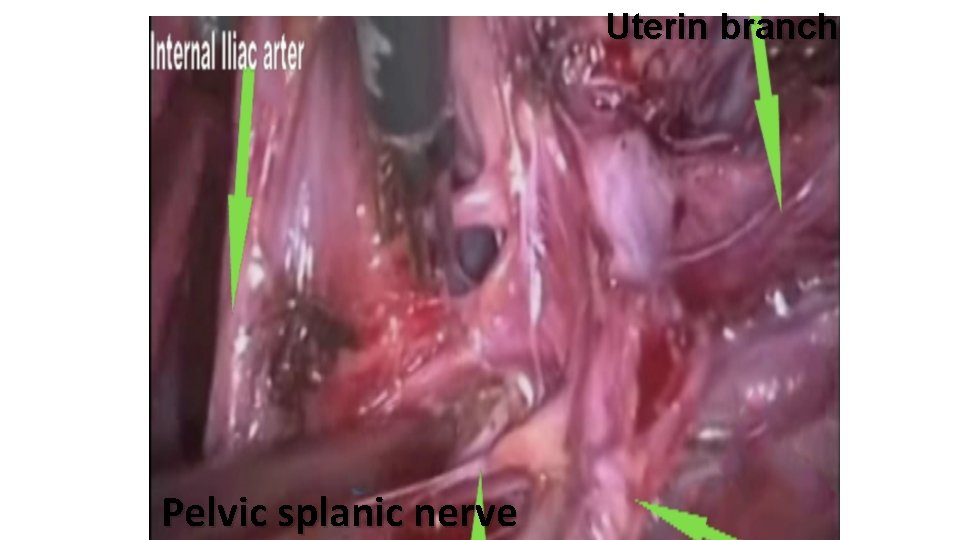
Uterin branch Pelvic splanic nerve
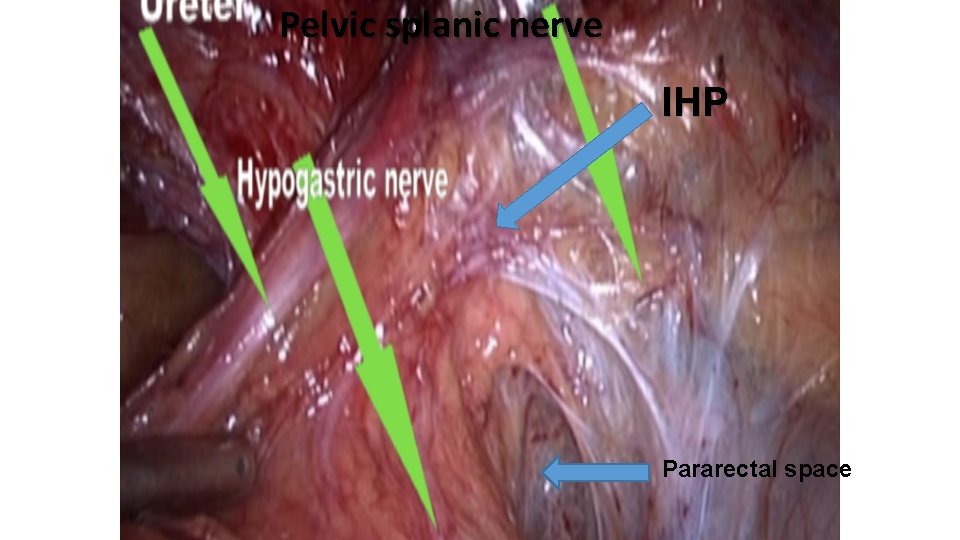
Pelvic splanic nerve IHP Pararectal space
IHP and parametrium is in the middle of the three space
Paravaginal space The paravaginal space is locate in the angle formed by bladder branch and uterine branch of nerve. This space also locate between bladder and vagina.
• The exact incidence of lower urinary tract dysfunction is not known • its pathogenesis is not completely understood. Advances in urodynamic assessment and widespread availability of a standardized technique have facilitated its exploration prior to and subsequent to the surgical management of patients with gynecologic pelvic cancer. Aoun F 1, Peltier A 1, van Velthoven R 1. Adv Urol. 2014; 2014: 303958. doi: 10. 1155/2014/303958. Epub 2014 Nov 23
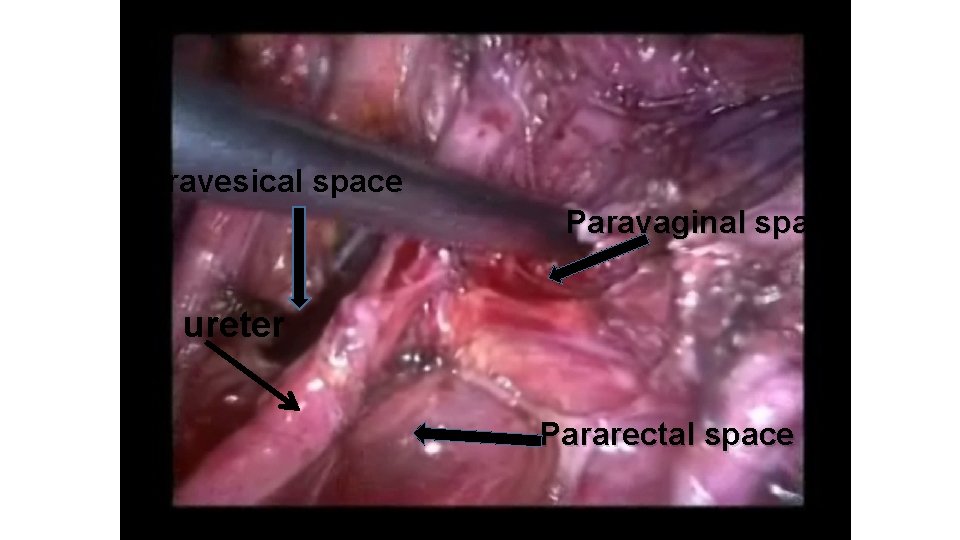
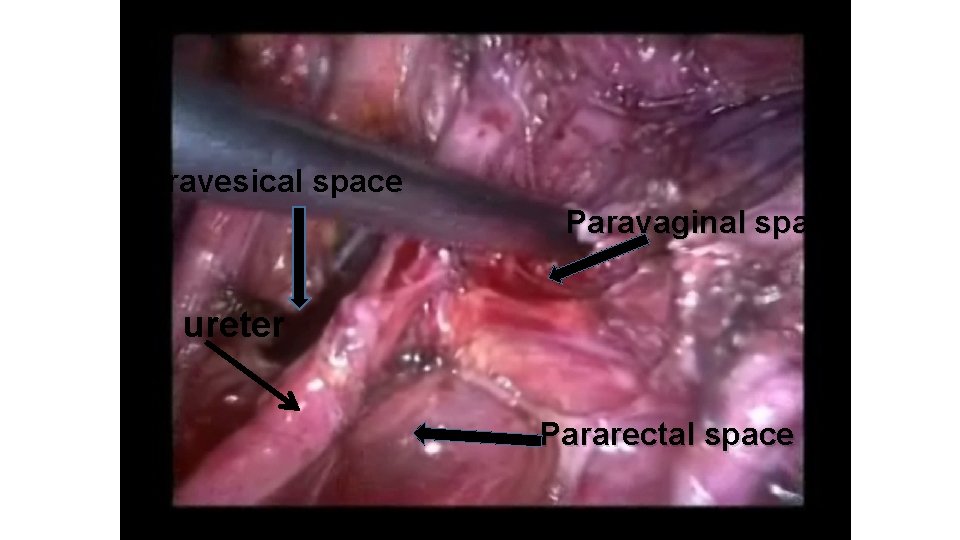
Paravesical space Paravaginal space ureter Pararectal space
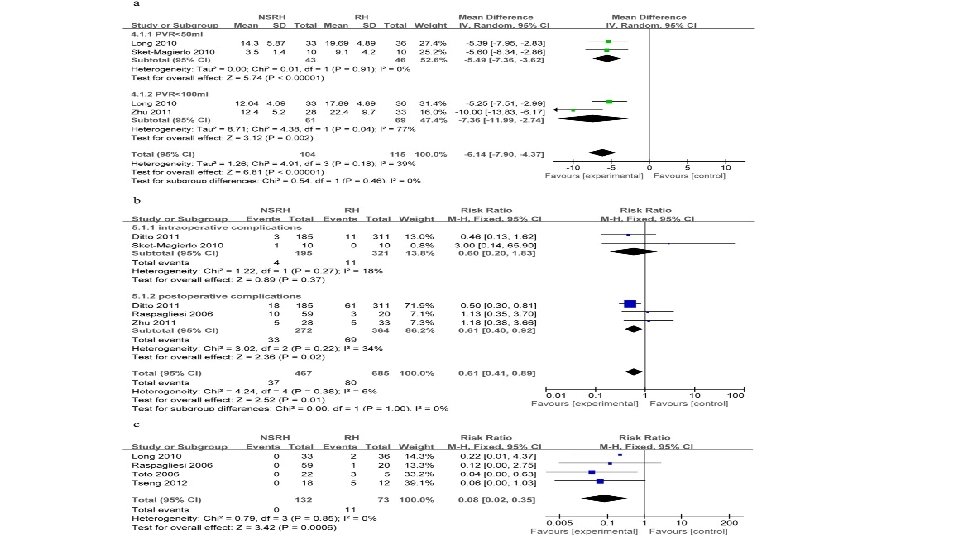
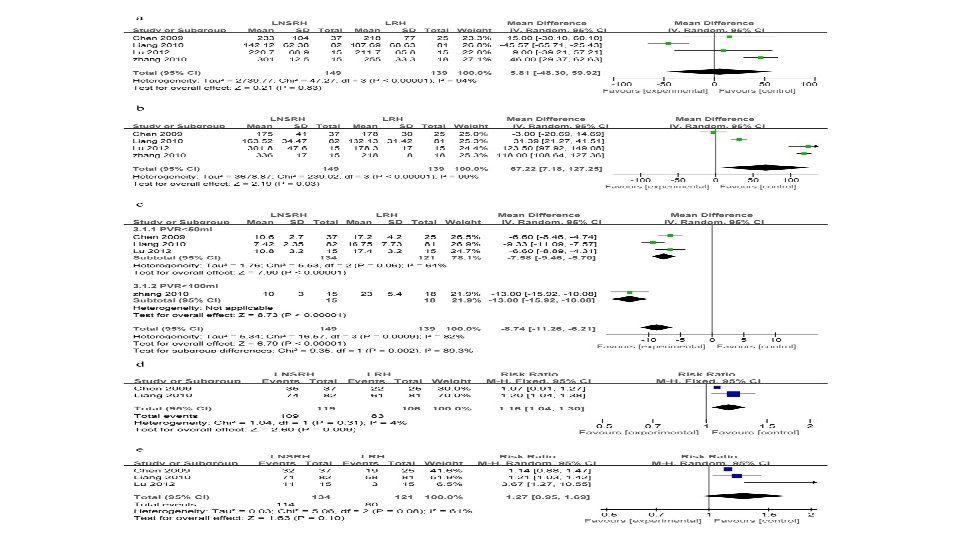
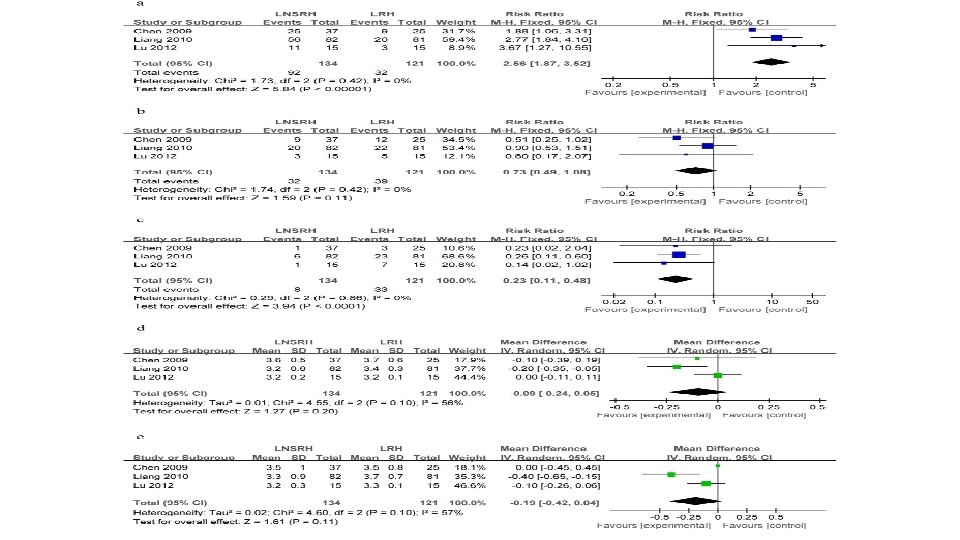
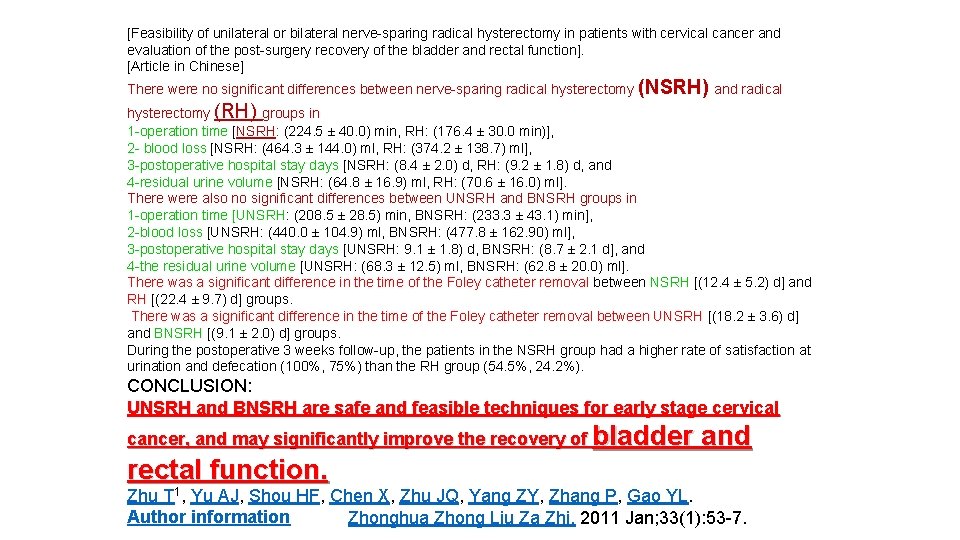
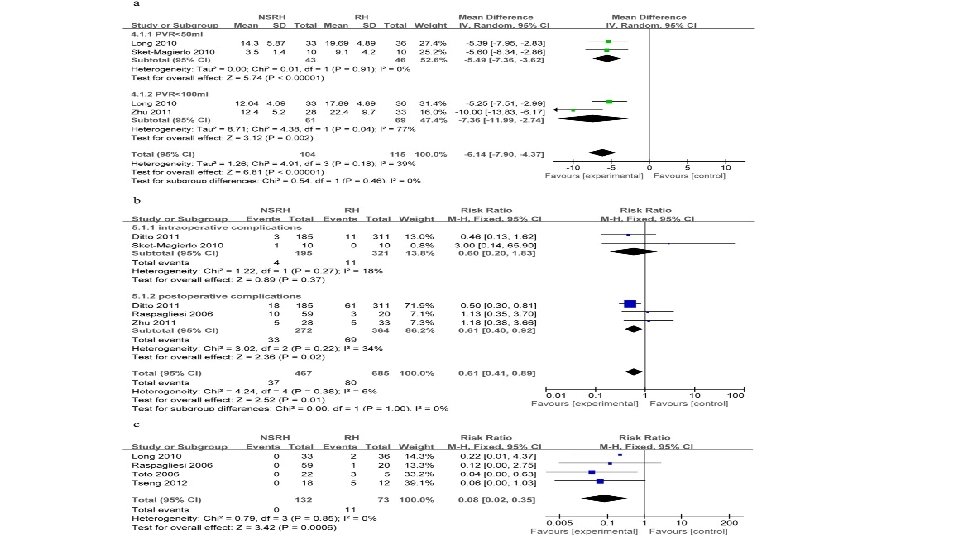
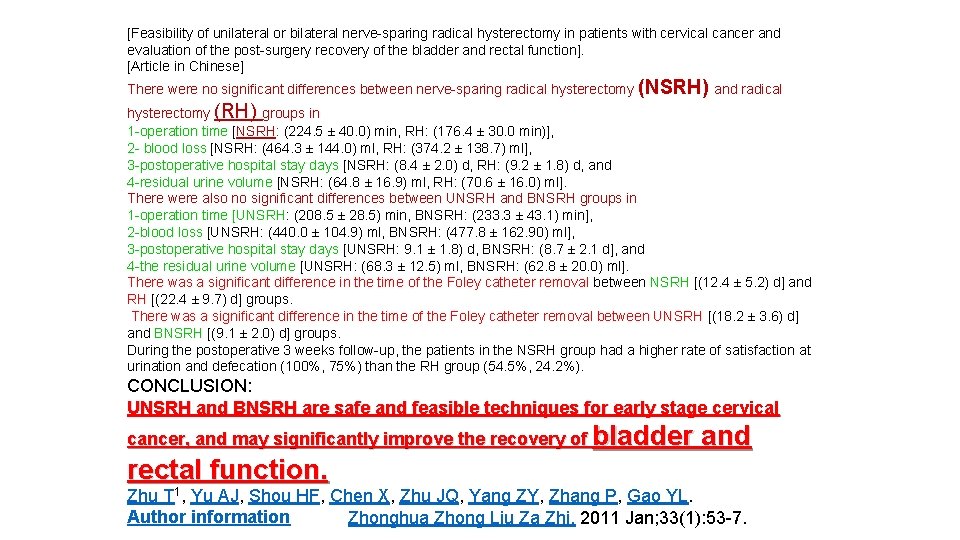
[Feasibility of unilateral or bilateral nerve sparing radical hysterectomy in patients with cervical cancer and evaluation of the post surgery recovery of the bladder and rectal function]. [Article in Chinese] There were no significant differences between nerve sparing radical hysterectomy (NSRH) and radical hysterectomy (RH) groups in 1 operation time [NSRH: (224. 5 ± 40. 0) min, RH: (176. 4 ± 30. 0 min)], 2 blood loss [NSRH: (464. 3 ± 144. 0) ml, RH: (374. 2 ± 138. 7) ml], 3 postoperative hospital stay days [NSRH: (8. 4 ± 2. 0) d, RH: (9. 2 ± 1. 8) d, and 4 residual urine volume [NSRH: (64. 8 ± 16. 9) ml, RH: (70. 6 ± 16. 0) ml]. There were also no significant differences between UNSRH and BNSRH groups in 1 operation time [UNSRH: (208. 5 ± 28. 5) min, BNSRH: (233. 3 ± 43. 1) min], 2 blood loss [UNSRH: (440. 0 ± 104. 9) ml, BNSRH: (477. 8 ± 162. 90) ml], 3 postoperative hospital stay days [UNSRH: 9. 1 ± 1. 8) d, BNSRH: (8. 7 ± 2. 1 d], and 4 the residual urine volume [UNSRH: (68. 3 ± 12. 5) ml, BNSRH: (62. 8 ± 20. 0) ml]. There was a significant difference in the time of the Foley catheter removal between NSRH [(12. 4 ± 5. 2) d] and RH [(22. 4 ± 9. 7) d] groups. There was a significant difference in the time of the Foley catheter removal between UNSRH [(18. 2 ± 3. 6) d] and BNSRH [(9. 1 ± 2. 0) d] groups. During the postoperative 3 weeks follow up, the patients in the NSRH group had a higher rate of satisfaction at urination and defecation (100%, 75%) than the RH group (54. 5%, 24. 2%). CONCLUSION: UNSRH and BNSRH are safe and feasible techniques for early stage cervical cancer, and may significantly improve the recovery of bladder and rectal function. Zhu T 1, Yu AJ, Shou HF, Chen X, Zhu JQ, Yang ZY, Zhang P, Gao YL. Author information Zhonghua Zhong Liu Za Zhi. 2011 Jan; 33(1): 53 7.
UNSRH and BNSRH are safe and feasible techniques for early stage cervical cancer, and may significantly improve the recovery of bladder and rectal function.
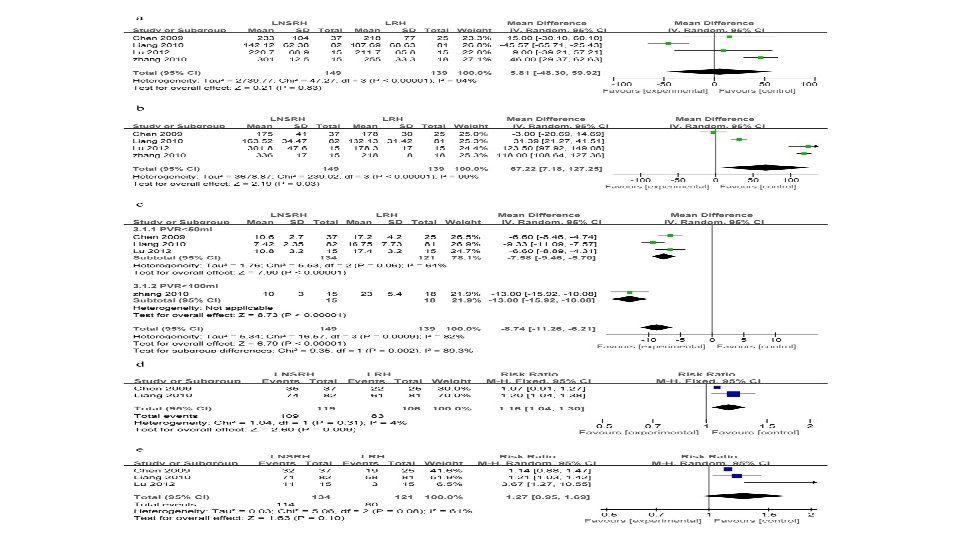
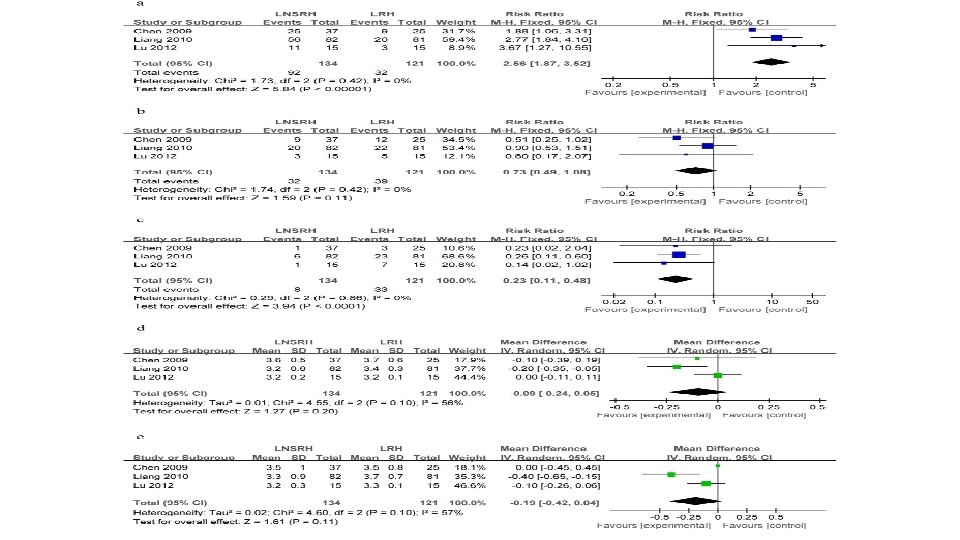
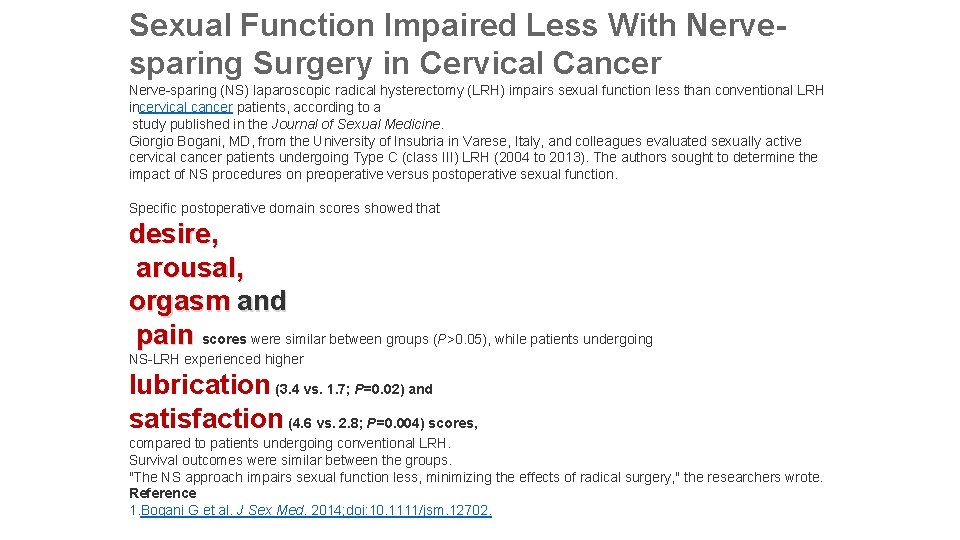
Sexual Function Impaired Less With Nervesparing Surgery in Cervical Cancer Nerve sparing (NS) laparoscopic radical hysterectomy (LRH) impairs sexual function less than conventional LRH incervical cancer patients, according to a study published in the Journal of Sexual Medicine. Giorgio Bogani, MD, from the University of Insubria in Varese, Italy, and colleagues evaluated sexually active cervical cancer patients undergoing Type C (class III) LRH (2004 to 2013). The authors sought to determine the impact of NS procedures on preoperative versus postoperative sexual function. Specific postoperative domain scores showed that desire, arousal, orgasm and pain scores were similar between groups (P>0. 05), while patients undergoing NS LRH experienced higher lubrication (3. 4 vs. 1. 7; P=0. 02) and satisfaction (4. 6 vs. 2. 8; P=0. 004) scores, compared to patients undergoing conventional LRH. Survival outcomes were similar between the groups. "The NS approach impairs sexual function less, minimizing the effects of radical surgery, " the researchers wrote. Reference 1. Bogani G et al. J Sex Med. 2014; doi: 10. 1111/jsm. 12702.
1 -Vaka takdimi ve konsultasyon grubu (FACEBOOK) 2 -Kadın Hastalıkları ve Doğum Hukuk Bürosu (FACEBOOK)
 Myotectomy
Myotectomy Dalam menggunakan apar selalu berpedoman pada istilah
Dalam menggunakan apar selalu berpedoman pada istilah Alege varianta corecta personajele care apar
Alege varianta corecta personajele care apar Atat?rk ?niversitesi
Atat?rk ?niversitesi Vajnal
Vajnal Prof dr metin ingeç
Prof dr metin ingeç Metin ercan
Metin ercan Prof. dr. ali metin kafadar kimdir
Prof. dr. ali metin kafadar kimdir Cpt code for laparoscopic pyloroplasty
Cpt code for laparoscopic pyloroplasty Hysterectomy
Hysterectomy Most common site of ureteric injury during hysterectomy
Most common site of ureteric injury during hysterectomy Indications of hysterectomy
Indications of hysterectomy Cesarean hysterectomy steps
Cesarean hysterectomy steps Entire radical form
Entire radical form Entire radical form
Entire radical form Unit 6 radical functions homework 8
Unit 6 radical functions homework 8 Metin tulgar
Metin tulgar Metin tabanlı programlama nedir
Metin tabanlı programlama nedir Metin ingeç klinik
Metin ingeç klinik Metin olgun
Metin olgun Karagöz ve mehtap ta yazılı bir metin yoktur
Karagöz ve mehtap ta yazılı bir metin yoktur Atıldı bir mehmetçik büyüyü bozdu
Atıldı bir mehmetçik büyüyü bozdu Metin olgun
Metin olgun Metin aktulga
Metin aktulga Lineer salpingostomi
Lineer salpingostomi Lig rectouterinum
Lig rectouterinum Metinle öğrenme nedir
Metinle öğrenme nedir Dosya ve klasörlerin saklanabileceği fiziksel aygıt
Dosya ve klasörlerin saklanabileceği fiziksel aygıt Metin olgun
Metin olgun Iltizam nedir tarih
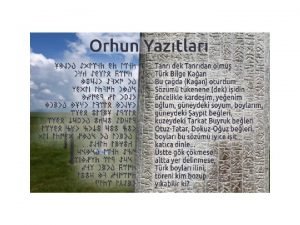
Iltizam nedir tarih Orhun yazıtları anlamı
Orhun yazıtları anlamı üleştirme sayıların yazımı
üleştirme sayıların yazımı