A randomised phase III trial comparing radical hysterectomy
- Slides: 1
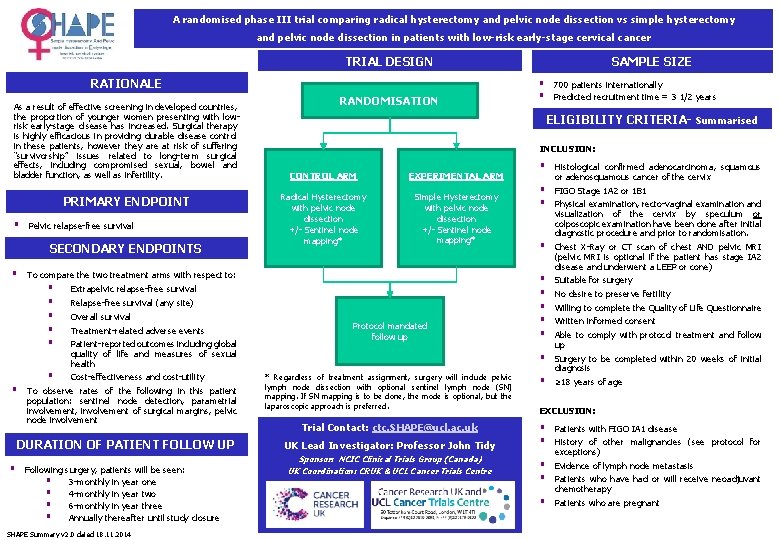
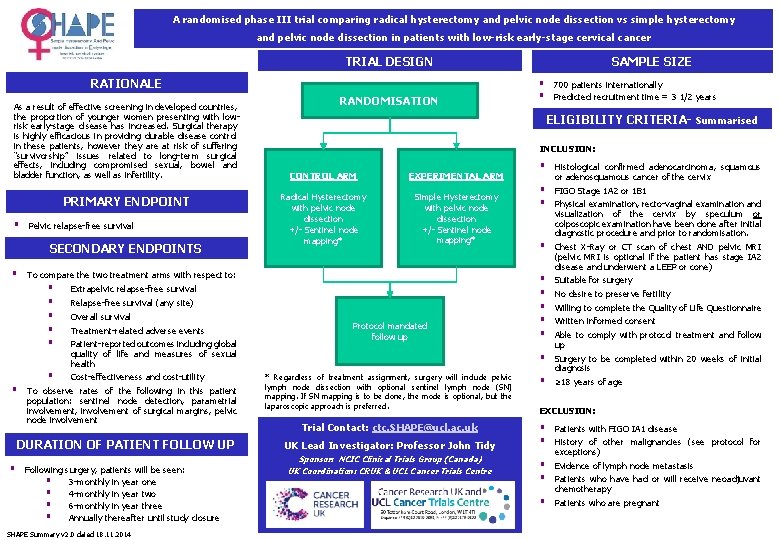
A randomised phase III trial comparing radical hysterectomy and pelvic node dissection vs simple hysterectomy and pelvic node dissection in patients with low-risk early-stage cervical cancer TRIAL DESIGN RATIONALE As a result of effective screening in developed countries, the proportion of younger women presenting with lowrisk early-stage disease has increased. Surgical therapy is highly efficacious in providing durable disease control in these patients, however they are at risk of suffering “survivorship” issues related to long-term surgical effects, including compromised sexual, bowel and bladder function, as well as infertility. PRIMARY ENDPOINT § Pelvic relapse-free survival SECONDARY ENDPOINTS § § Patient-reported outcomes including global quality of life and measures of sexual health Cost-effectiveness and cost-utility To observe rates of the following in this patient population: sentinel node detection, parametrial involvement, involvement of surgical margins, pelvic node involvement DURATION OF PATIENT FOLLOW UP § § Histological confirmed adenocarcinoma, squamous or adenosquamous cancer of the cervix § § FIGO Stage 1 A 2 or 1 B 1 § Chest X-Ray or CT scan of chest AND pelvic MRI (pelvic MRI is optional if the patient has stage IA 2 disease and underwent a LEEP or cone) § § § Suitable for surgery § * Regardless of treatment assignment, surgery will include pelvic lymph node dissection with optional sentinel lymph node (SN) mapping. If SN mapping is to be done, the mode is optional, but the laparoscopic approach is preferred. Surgery to be completed within 20 weeks of initial diagnosis § ≥ 18 years of age Trial Contact: ctc. SHAPE@ucl. ac. uk § § Patients with FIGO IA 1 disease § § Evidence of lymph node metastasis § Patients who are pregnant CONTROL ARM EXPERIMENTAL ARM Radical Hysterectomy with pelvic node dissection +/- Sentinel node mapping* Simple Hysterectomy with pelvic node dissection +/- Sentinel node mapping* Relapse-free survival (any site) Treatment-related adverse events Following surgery, patients will be seen: § 3 -monthly in year one § 4 -monthly in year two § 6 -monthly in year three § Annually thereafter until study closure SHAPE Summary v 2. 0 dated 18. 11. 2014 700 patients internationally Predicted recruitment time = 3 1/2 years INCLUSION: Extrapelvic relapse-free survival Overall survival § § ELIGIBILITY CRITERIA- Summarised To compare the two treatment arms with respect to: § § § RANDOMISATION SAMPLE SIZE Protocol mandated follow up UK Lead Investigator: Professor John Tidy Sponsor: NCIC Clinical Trials Group (Canada) UK Coordination: CRUK & UCL Cancer Trials Centre Physical examination, recto-vaginal examination and visualization of the cervix by speculum or colposcopic examination have been done after initial diagnostic procedure and prior to randomisation. No desire to preserve fertility Willing to complete the Quality of Life Questionnaire Written informed consent Able to comply with protocol treatment and follow up EXCLUSION: History of other malignancies (see protocol for exceptions) Patients who have had or will receive neoadjuvant chemotherapy