Is interval appendicectomy justified after successful nonoperative treatment

















![Additional Researches � The role of routine interval appendectomy is questioned recently. [7] ◦ Additional Researches � The role of routine interval appendectomy is questioned recently. [7] ◦](https://slidetodoc.com/presentation_image_h2/a7e44444a020dc3655801fbd86503422/image-18.jpg)

- Slides: 19

Is interval appendicectomy justified after successful nonoperative treatment of an appendix mass in children? A systematic review [1] Clerk B 9602054 陳怡如 Clerk B 9602006 江柏興 Clerk B 9505009 李元超

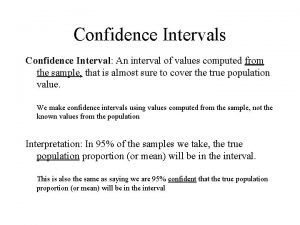
Background � Acute appendicitis enclosed by the omentum and adjacent loops of bowel an appendix mass (AM) � 9% of all children with acute appendicitis have an inflammatory mass (a recent meta-analysis) � Immediate appendectomy may be technically complicated. A high incidence of complications has been reported after that.

Background � Intravenous antibiotics and intestinal rest 8 -12 wks after successful nonoperative treatment, interval appendectomy (IA) � However, this practice has been questioned. The risk of recurrence may be low and there is a morbidity associated with IA.

Purpose � To evaluate the evidence for IA in children after successful nonoperative treatment of an AM

Methods of a Medline search: appendix mass, interval appendectomy, and children � January 1964 to July 2009, reports of successful nonoperative treatment of AM in children (<16 years) � Journal of Pediatric Surgery, Pediatric Surgery International, European Journal of Pediatric Surgery � Keywords

Methods � Inclusion criteria: nonoperative expectant management after successful nonoperative treatment of an AM in children, outcome after IA in children � Data: risk of recurrence, morbidity of IA, unexpected histopathologic findings after IA, and cost

Statistical Analysis � For each outcome measure binomial multilevel modeling technique, “one-sided” meta-analysis � Data relating to length of stay after IA were reported in an inconsistent fashion among individual studies descriptive form only

Recurrent acute appendicitis • 3 studies, total 127 children without IA • Recurrent range: 0%~42% • Overall incidence : 20. 5% (95% CI, 14. 3~28. 4)

Recurrent acute appendicitis • Time to recurrence of acute appendicitis was reported by both studies • One study reported : presence of faecolith, incidence

Morbidity of IA • Complications: wound infection, prolonged post-op ileus hematoma and intestinal obstruction • 23 studies (1247 children ) incidence complication: 3. 4%

Histologic findings • 15 studies (955 patients) findings: normal appendix with no inflammation, residual acute inflammation chronic inflammation • Incidence of carcinoid tumor in specimens removed at IA : 0. 9%

Discussion � Retrospective review studies limit the strength of the ◦ Unable to identify any data comparing IA & nonoperative management ◦ Inform current practice of obtaining prospective data

Discussion � Pros and cons of IA and “watchful waiting” Pros Cons IA Remove the risk of recurrence Risk of complication (3. 4%) Hospital cost (~3 day) Watchful waiting Avoid IA Risk of recurrence (20. 5%) Emergency operation Undetected carcinoid tumor (<1%)

Additional Researches � Frequency of morbidity a/w IA versus risk of recurrence in patients w/o IA [2] ◦ not substantially different (11% versus 7%) ◦ (morbidity: eg, postoperative infection, intestinal fistula, small bowel obstruction) ◦ Nonoperative treatment �Most recurrences developed within 6 months of hospital discharge. � 20% required percutaneous abscess drainage � 2 % delayed the diagnosis of Crohn's disease and cancer, more common in adult patients

Additional Researches � The rate of recurrence in children with an appendicolith was significantly higher than in those without an appendicolith (76% versus 26%) [3]

Additional Researches � For perforated appendicitis with a wellformed abscess ◦ NO difference in total length of hospitalization, recurrent abscess rates, or overall charges between initial LA & IA [4] ◦ Interval appendectomy is controversial

Additional Researches � Advanced appendicitis (perforation/ gangrene) without an appendiceal mass or phlegmon should usually be treated with early appendectomy [5] ◦ time to return to normal activities (mean number of days: 14 versus 19) ◦ reduced adverse events (eg, abscess, small bowel obstruction, or unplanned readmission) (30% versus 55 %) ◦ hospital charges ($17, 450 versus $22, 518)[6]
![Additional Researches The role of routine interval appendectomy is questioned recently 7 Additional Researches � The role of routine interval appendectomy is questioned recently. [7] ◦](https://slidetodoc.com/presentation_image_h2/a7e44444a020dc3655801fbd86503422/image-18.jpg)
Additional Researches � The role of routine interval appendectomy is questioned recently. [7] ◦ the risk of recurrence is low (5%-14%) ◦ recurrences usually exhibit a milder clinical course compared to the first episode of AA [8, 9]

References 1. 2. 3. 4. 5. 6. 7. 8. 9. Hall, N. J. , et al. , Is interval appendicectomy justified after successful nonoperative treatment of an appendix mass in children? A systematic review. J Pediatr Surg, 2011. 46(4): p. 767 -71. Andersson, R. E. and M. G. Petzold, Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg, 2007. 246(5): p. 741 -8. Ein, S. H. , J. C. Langer, and A. Daneman, Nonoperative management of pediatric ruptured appendix with inflammatory mass or abscess: presence of an appendicolith predicts recurrent appendicitis. J Pediatr Surg, 2005. 40(10): p. 1612 -5. St Peter, S. D. , et al. , Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg, 2010. 45(1): p. 236 -40. Blakely, M. L. , et al. , Early vs interval appendectomy for children with perforated appendicitis. Arch Surg, 2011. 146(6): p. 660 -5. Myers, A. L. , et al. , Hospital cost analysis of a prospective, randomized trial of early vs interval appendectomy for perforated appendicitis in children. J Am Coll Surg, 2012. 214(4): p. 42734; discussion 434 -5. Sakorafas, G. H. , et al. , Interval routine appendectomy following conservative treatment of acute appendicitis: Is it really needed. World J Gastrointest Surg, 2012. 4(4): p. 83 -6. Dixon, M. R. , et al. , An assessment of the severity of recurrent appendicitis. Am J Surg, 2003. 186(6): p. 718 -22; discussion 722. Kaminski, A. , et al. , Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg, 2005. 140(9): p. 897 -901.
 After me after me after me
After me after me after me John 14 1
John 14 1 Primary and secondary reinforcers
Primary and secondary reinforcers Variable interval
Variable interval Nada cg berjarak
Nada cg berjarak Julie woodside
Julie woodside The most dangerous game foreshadowing examples
The most dangerous game foreshadowing examples Discounted abnormal earnings model
Discounted abnormal earnings model Apa style justified
Apa style justified Ev/ebitda ratio
Ev/ebitda ratio Is romeo justified in killing tybalt
Is romeo justified in killing tybalt Is justified true belief knowledge
Is justified true belief knowledge 1. what condition threatens peeta's life?
1. what condition threatens peeta's life? Therefore since we have been justified by faith
Therefore since we have been justified by faith David matuszek
David matuszek Wisdom is proved right by her actions proverbs
Wisdom is proved right by her actions proverbs The reign of terror was it justified background essay
The reign of terror was it justified background essay How is the title of all my sons justified?
How is the title of all my sons justified? Reign of terror mini q document a answer key
Reign of terror mini q document a answer key Was the policy of appeasement justified
Was the policy of appeasement justified