Introduction to AFP Surveillance Polio Eradication Strategies 1


- Slides: 22

Introduction to AFP Surveillance
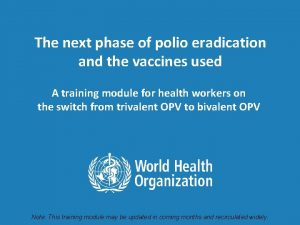
Polio Eradication Strategies 1. High routine immunization coverage 2. National Immunization Days (NIDs) 3. Acute Flaccid Paralysis (AFP) surveillance 4. ‘Mop-up’ campaigns Polio Eradication
Objectives and main strategy of AFP surveillance for Polio Eradication 1) Objectives: - detect polioviruses wherever they should still circulate -> to target immunization campaigns / mop-ups - show the absence of wild polioviruses - show that surveillance meets the level needed for certification. 2) Strategy: - report and investigate all cases of acute flaccid paralysis - collect and analyze stool specimens to identify polioviruses
How to 'prove' that polio is eradicated? How can we be certain that there is no wild poliovirus in a country that reports “ 0” cases of polio?
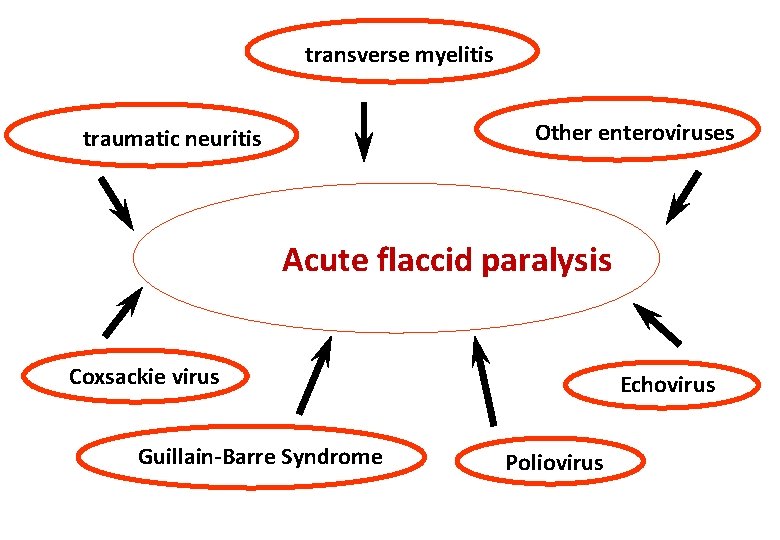
Why report 'AFP' and not 'Polio'? • Several other diseases look like clinical polio – true polio cases may be mis-diagnosed (Guillain-Barré Syndrome) – reporting of 'clinical polio' is not sensitive – likely to miss cases • Increase sensitivity to detect remaining polio by reporting a syndrome – Acute Flaccid Paralysis – which should include all polio cases – immediate reporting of all AFP in children < 15 yrs – separate true polio from non-polio AFP through testing of stool specimens for wild poliovirus
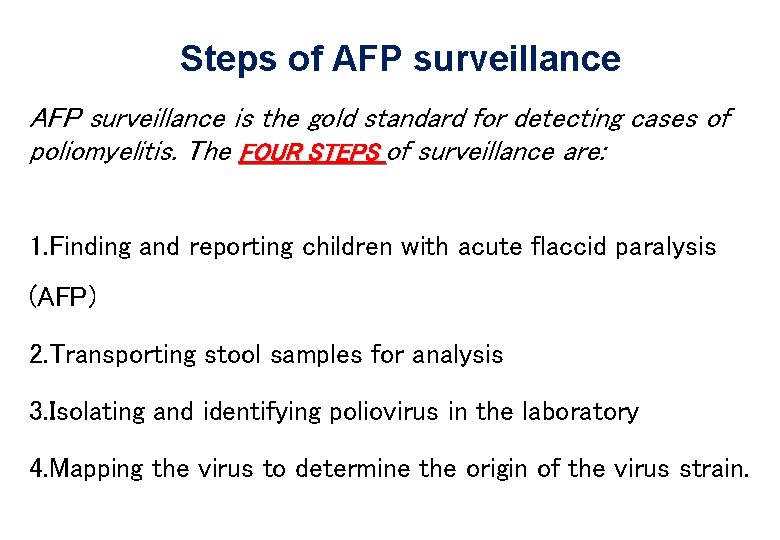
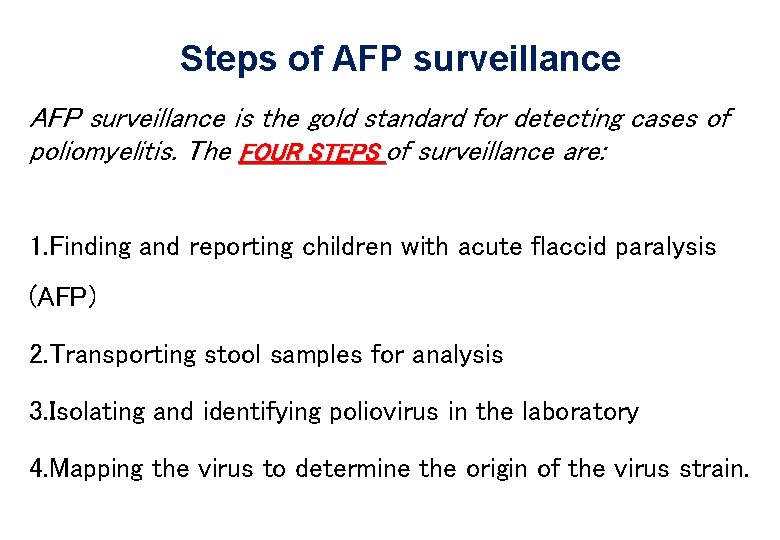
Steps of AFP surveillance is the gold standard for detecting cases of poliomyelitis. The FOUR STEPS of surveillance are: 1. Finding and reporting children with acute flaccid paralysis (AFP) 2. Transporting stool samples for analysis 3. Isolating and identifying poliovirus in the laboratory 4. Mapping the virus to determine the origin of the virus strain.
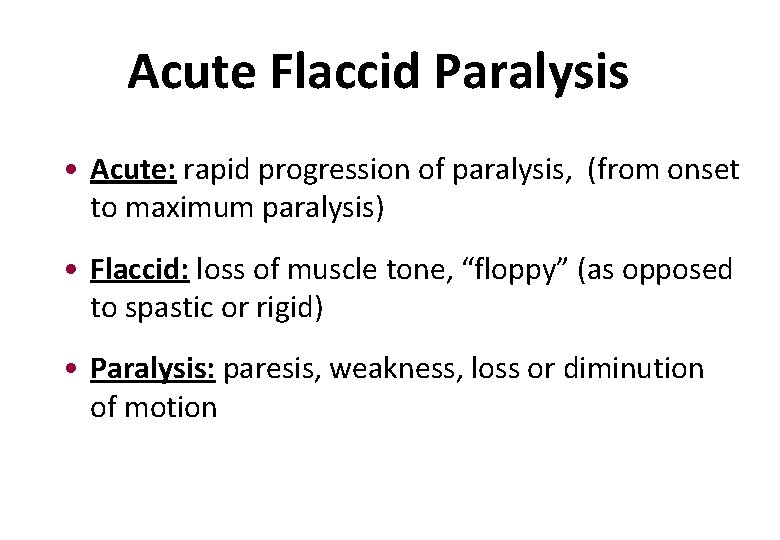
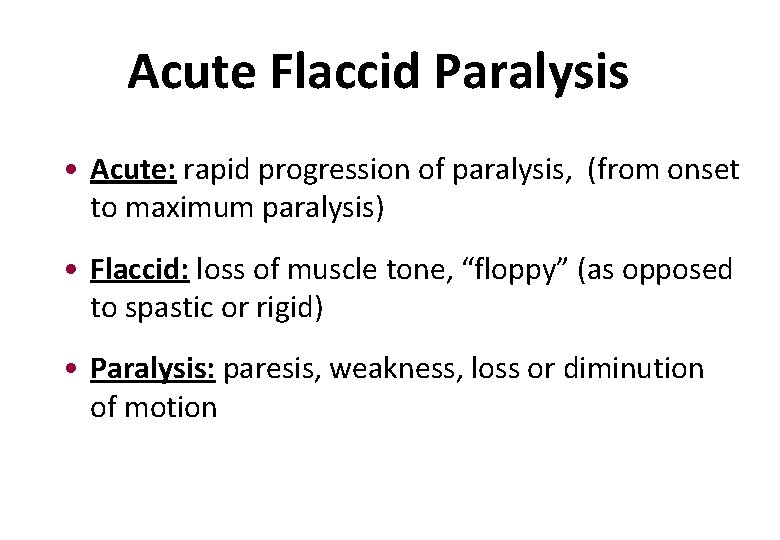
Acute Flaccid Paralysis • Acute: rapid progression of paralysis, (from onset to maximum paralysis) • Flaccid: loss of muscle tone, “floppy” (as opposed to spastic or rigid) • Paralysis: paresis, weakness, loss or diminution of motion
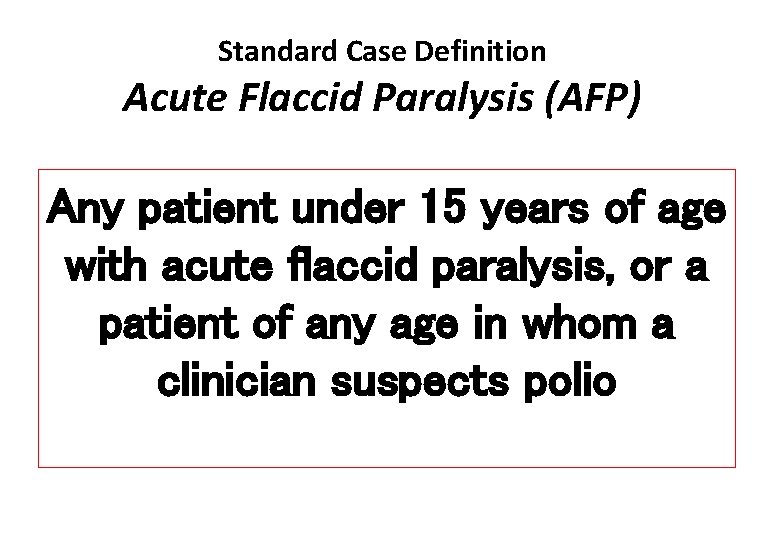
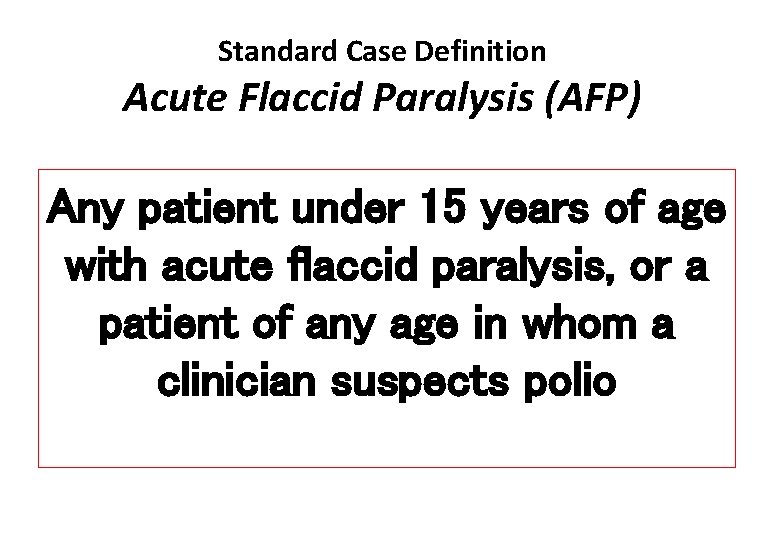
Standard Case Definition Acute Flaccid Paralysis (AFP) Any patient under 15 years of age with acute flaccid paralysis, or a patient of any age in whom a clinician suspects polio
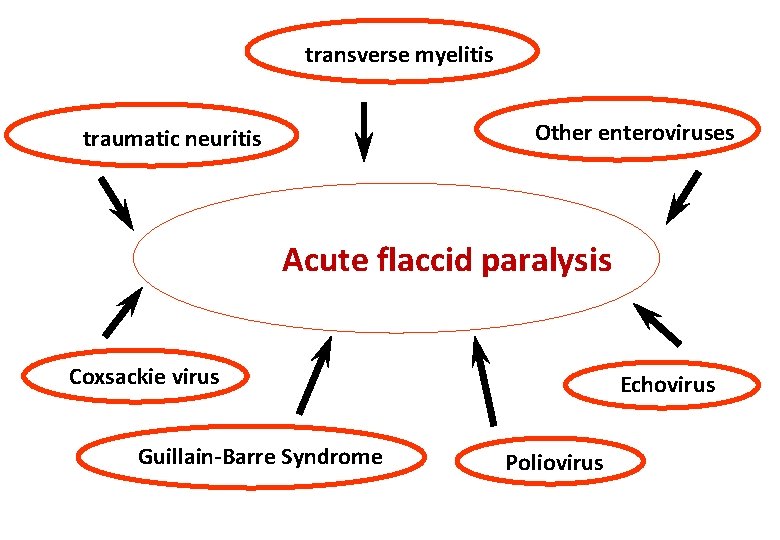
transverse myelitis Other enteroviruses traumatic neuritis Acute flaccid paralysis Coxsackie virus Guillain-Barre Syndrome Echovirus Poliovirus
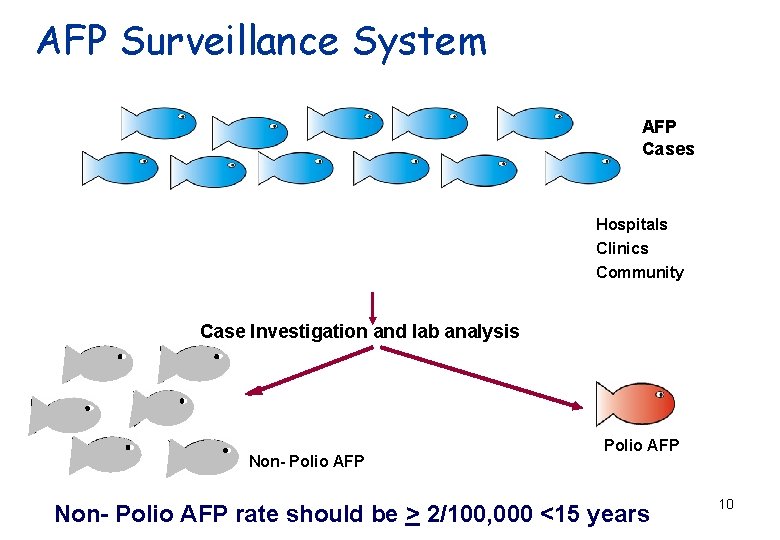
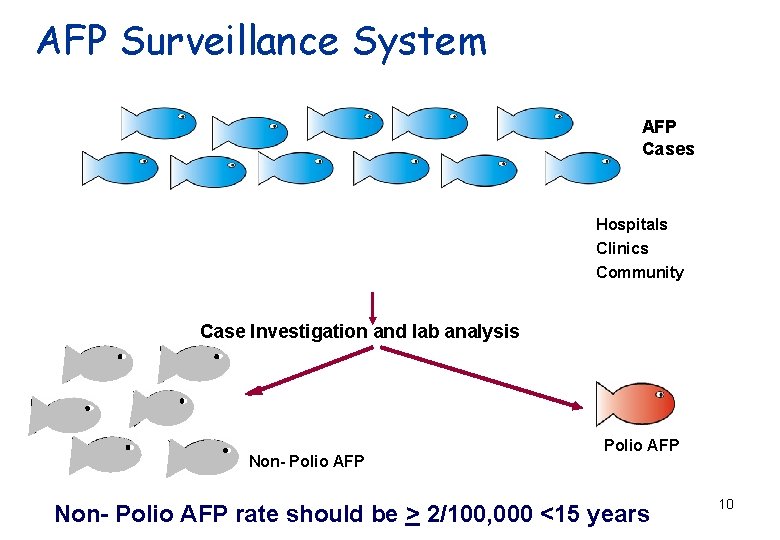
AFP Surveillance System AFP Cases Hospitals Clinics Community Case Investigation and lab analysis Non- Polio AFP rate should be > 2/100, 000 <15 years 10
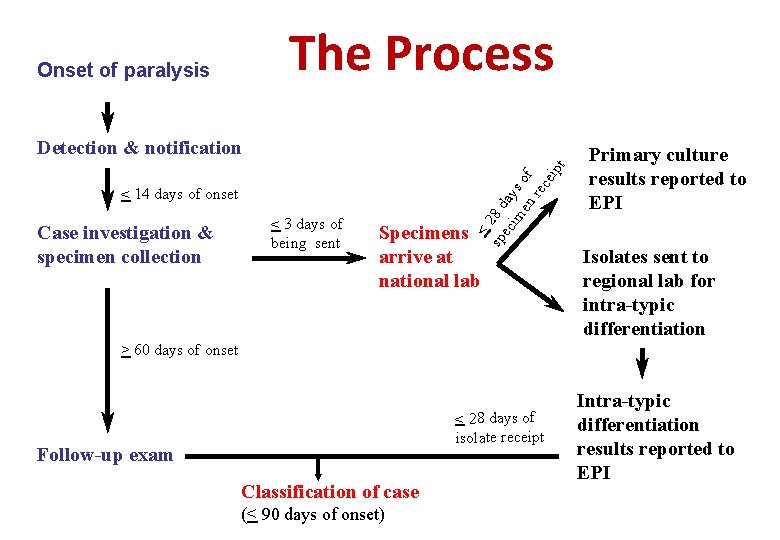
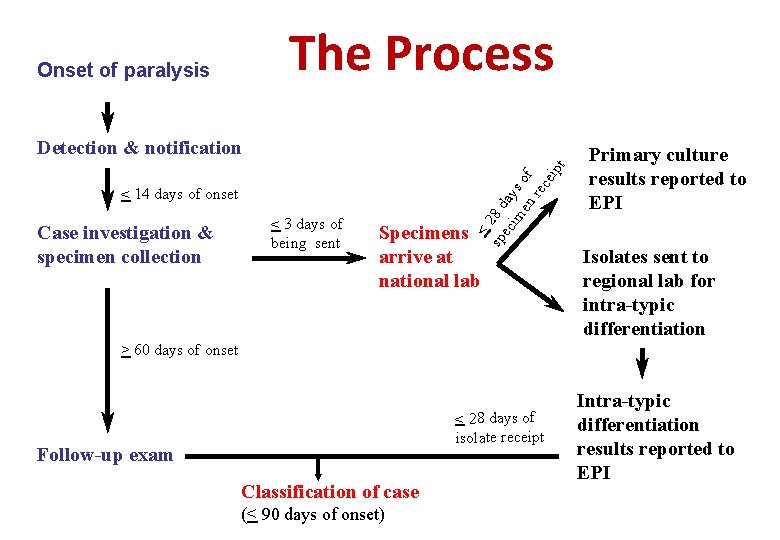
The Process Onset of paralysis < 14 days of onset Case investigation & specimen collection < 3 days of being sent < sp 28 d ec ay im s en of rec eip t Detection & notification Specimens arrive at national lab Primary culture results reported to EPI Isolates sent to regional lab for intra-typic differentiation > 60 days of onset < 28 days of isolate receipt Follow-up exam Classification of case (< 90 days of onset) Intra-typic differentiation results reported to EPI
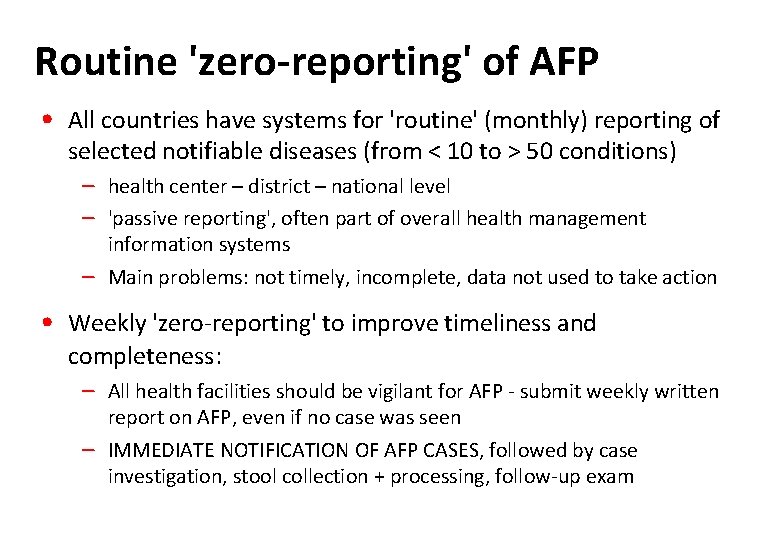
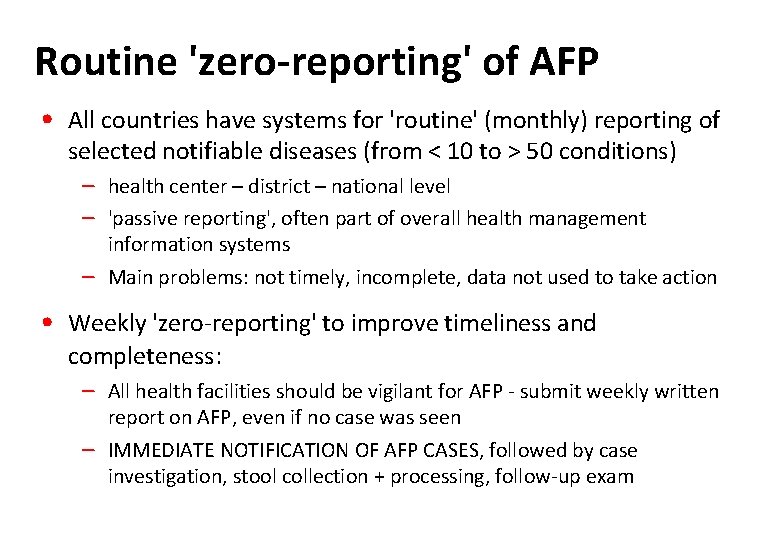
Routine 'zero-reporting' of AFP • All countries have systems for 'routine' (monthly) reporting of selected notifiable diseases (from < 10 to > 50 conditions) – health center – district – national level – 'passive reporting', often part of overall health management information systems – Main problems: not timely, incomplete, data not used to take action • Weekly 'zero-reporting' to improve timeliness and completeness: – All health facilities should be vigilant for AFP - submit weekly written report on AFP, even if no case was seen – IMMEDIATE NOTIFICATION OF AFP CASES, followed by case investigation, stool collection + processing, follow-up exam
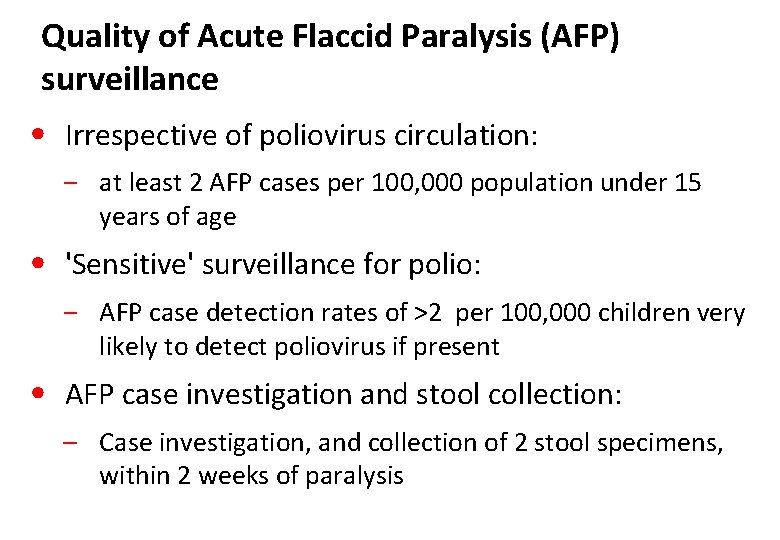
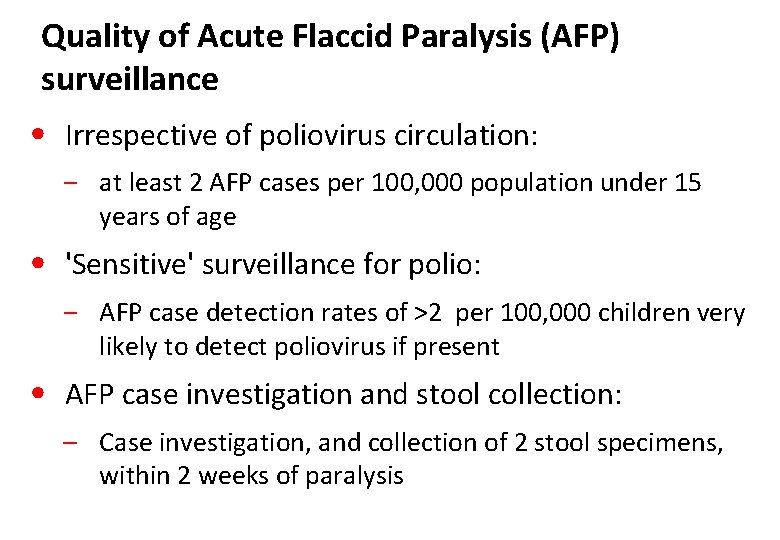
Quality of Acute Flaccid Paralysis (AFP) surveillance • Irrespective of poliovirus circulation: ‒ at least 2 AFP cases per 100, 000 population under 15 years of age • 'Sensitive' surveillance for polio: ‒ AFP case detection rates of >2 per 100, 000 children very likely to detect poliovirus if present • AFP case investigation and stool collection: – Case investigation, and collection of 2 stool specimens, within 2 weeks of paralysis
Two key indicators to measure performance of AFP surveillance Non-polio AFP rate (NPAFP) - Minimum 'operational' target: ≥ 2/100, 000 population <15 yrs • Indicator for 'sensitivity': if NPAFP is > 2/100, 000, likelihood of missing true polio cases is very low % AFP cases with 'adequate' specimens - Minimum target: ≥ 80% of all AFP with adequate stools • Reliable laboratory results are key for good surveillance • "Adequate": 2 specimens collected 24 hours apart within 14 days after onset of paralysis, arriving at the lab in good condition
Stool sample collection procedures for AFP case
Indication for stool collection To identify presence or absence of Polio virus in the stool specimens
Outline ü Stool collection ü Materials for collection ü Procedure of stool collection ü Storage, transportation and reversed cold chain ü Challenges
AFP Stool collection ü Issues to consider for stool collection üEnsure the child fulfil the criteria of true AFP case üAge: <15 years or clinician suspect polio üParalysis: FLACCID/FLOPPY, not spastic üOnset of paralysis: should be < 60 days (If >60 days, Just complete CIF and follow-up exam)
Procedure of stool collection ü 2 Stool specimens ü Two specimens should be collected at least 24 -48 hours apart ü Best time to collect samples within 14 days of onset of paralysis but sample can collect up to 60 days of onset of paralysis ü Each sample should be adequate (8 gm) in amount
Condition of Stool Specimen Upon arrival at laboratory, stool specimen should show: – No desiccation (not dried-out) – No leakage – Adequate documentation – Evidence that the cold chain was maintained 20
Further Instructions: § § § If the patient cannot produce stool, leave the collection kit, specimen carrier box and frozen ice packs in the health facility or with the family Explain in simple language the specimen collection procedure. Return at a later time to collect the specimen container box Transportation arrangements should have been made in advance to transport the stool specimens as soon as possible to the laboratory (this is the reverse cold chain system).

Thank you!
 H pylori eradication therapy
H pylori eradication therapy Weed definition in agriculture
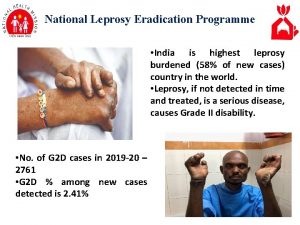
Weed definition in agriculture National leprosy eradication programme ppt
National leprosy eradication programme ppt Containment eradication
Containment eradication Post-polio syndrome
Post-polio syndrome Introduction of immunization
Introduction of immunization Poliomyelitis
Poliomyelitis Kernig bulgusu
Kernig bulgusu Ipv merieux fachinformation
Ipv merieux fachinformation Cell response
Cell response Opv medical abbreviation
Opv medical abbreviation Porto polio
Porto polio Elsie lacks
Elsie lacks Glauc o medical term
Glauc o medical term Polio
Polio Papa lolos
Papa lolos Poliomielit
Poliomielit Certified fp&a
Certified fp&a Afp annual conference 2020
Afp annual conference 2020 Afp valores normales
Afp valores normales Descuento afp
Descuento afp Afp vision 2028
Afp vision 2028 Gains rapide
Gains rapide