Interferences to Safety Needs Due to Sensory Deprivation

- Slides: 16

Interferences to Safety Needs Due to Sensory Deprivation and Aging
Cataracts Ø Definition: opacity of the lens Ø Pathophysiology: Ø Lens looses water Ø Density increases Ø Lens becomes opaque Ø Etiology/Genetic Risk (see table 50 -2) Ø Congenital Ø Age-related most common, > age of 70 Ø Traumatic Ø Toxic agents Ø Other diseases
Ø Prevention Ø Sunglasses Ø Eye protection Ø Clinical Manifestations (see chart 50 -6) Ø No pain or eye redness w/ age related cataracts Ø Blurred vision Ø Double vision Ø Impaired color perception Ø Absent red reflex Ø Cloudy, whitish pupil
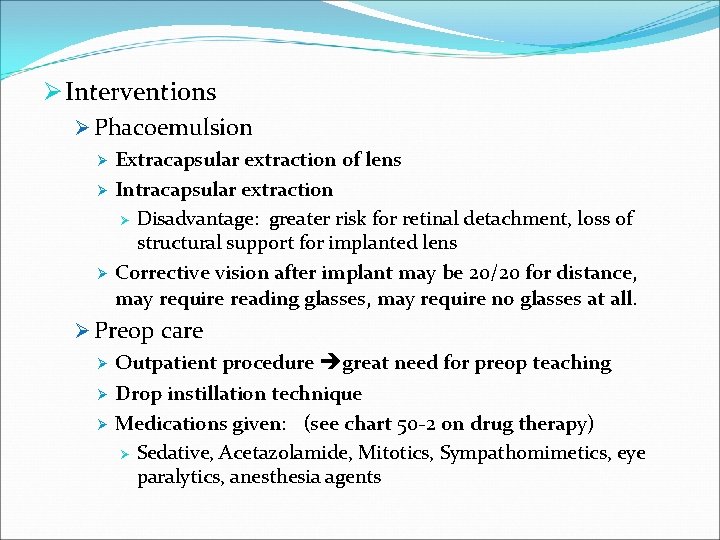
Ø Interventions Ø Phacoemulsion Ø Ø Ø Extracapsular extraction of lens Intracapsular extraction Ø Disadvantage: greater risk for retinal detachment, loss of structural support for implanted lens Corrective vision after implant may be 20/20 for distance, may require reading glasses, may require no glasses at all. Ø Preop care Ø Outpatient procedure great need for preop teaching Ø Drop instillation technique Ø Medications given: (see chart 50 -2 on drug therapy) Ø Sedative, Acetazolamide, Mitotics, Sympathomimetics, eye paralytics, anesthesia agents
Ø Post op care Ø Meds Ø Antibiotics, steroids, mild analgesics (AVOID ASA) Ø Dark glasses Ø S/S of trouble: Ø Pain early after surgery, esp. if assoc. w/ N/V Ø Infection: increasing redness, change in visual acuity, tears, photophobia, yellow/green drainage Ø Bleeding w/ assoc. vision changes report immediately Ø Home care instructions Ø Light housework, cooking Ø See table 50 -3 avoid these activities Ø See Best Practice for Eyedrop Administration chart 50 -5
Glaucoma v. Pathophysiology v Normal IOP = 10 -21 mm Hg v Decreased outflow of aqueous fluid v Overproduction of aqueous humor v Resulting in increased IOP v Increased pressure within eye reduces blood flow to optic nerve and retina ischemia and death, blindness. v Starts at periphery and works toward center of vision classic sign of tunnel vision. v Painless, loss of vision so insidious as to not be noticable until it’s too late. v Age-related v Occurs in about 10% of people older than 80
v. Etiology v Primary open-angle Most common v Usually bilateral, asymptomatic in early stages v Outflow reduction, pressure 22 -32 mm Hg v v Angle-closure v Narrow angle, acute glaucoma v Sudden onset medical emergency v Outflow blockage, pressure 30 mm. Hg or higher v Secondary v Results from ocular diseases which cause narrowing of chamber angle or increased fluid volume within eye v Sudden
v. Interventions v Primarily drug therapy See chart 50 -2 Drug Therapy for Eye Problems v See Evidence Based Practice: adherence to ocular drug tx v v Surgical Management – when drugs don’t work v Laser surgery v trabeculoplasty v Standard surgical therapy v To create new drainage channel v Destroy structures that are overproducing aqueous humor v See Chart 50 -10 Nursing Focus on the Older Adult
Diabetic Retinopathy q. Pathophysiology q Complication of diabetes mellitus poor BS control q Background retinopathy Cells of retinal vessels die with leakage of fluid into eye creating thick yellow-white hard exudates q Microaneurysms form leading to hemorrhages in nerve layer of retina q Visual acuity is reduced q q Proliferative retinopathy q Network of fragile new blood vessels develop, leak blood and protein into surrounding tissue q Leads to reduced visual acuity/blindness
q. Treatment dependent on severity of retinal damage q. Use of laser therapy to seal microaneurysms, decrease bleeding q. Vitrectomy performed if frequent bleeding into vitreous occurs and retinal detachment becomes high risk.
Macular Degeneration Ø Pathophysiology Ø Atrophic = age related, dry Ø Gradual blockage of retinal capillaries leading to ischemia and death of retinal cells blindness Ø Long term dietary intake of antioxidants and lutein and zeaxanthin may decrease risk of disease or slow progression of disease process Ø Exudative = wet Ø Sudden decrease in vision after serous detachment of pigment epithelium in macula Ø Blood collection under macula causes scar formation, visual distortion Ø Treatment goal Ø Maximize remaining vision
Ø Review Trauma section in text pg 1105 -1106 Ø Hyphema Ø Contusion Ø Foreign bodies Ø Lacerations Ø See Best Practice for eye irrigation Ø Be sure to read Key Points at chapters end
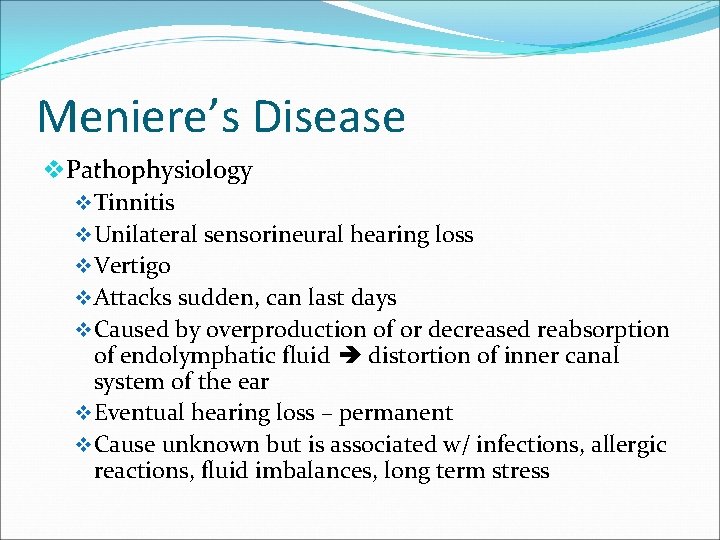
Meniere’s Disease v. Pathophysiology v Tinnitis v Unilateral sensorineural hearing loss v Vertigo v Attacks sudden, can last days v Caused by overproduction of or decreased reabsorption of endolymphatic fluid distortion of inner canal system of the ear v Eventual hearing loss – permanent v Cause unknown but is associated w/ infections, allergic reactions, fluid imbalances, long term stress
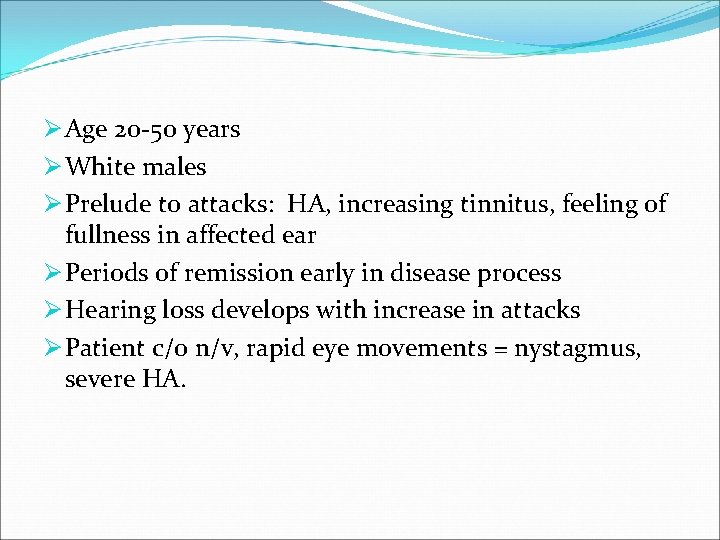
Ø Age 20 -50 years Ø White males Ø Prelude to attacks: HA, increasing tinnitus, feeling of fullness in affected ear Ø Periods of remission early in disease process Ø Hearing loss develops with increase in attacks Ø Patient c/o n/v, rapid eye movements = nystagmus, severe HA.
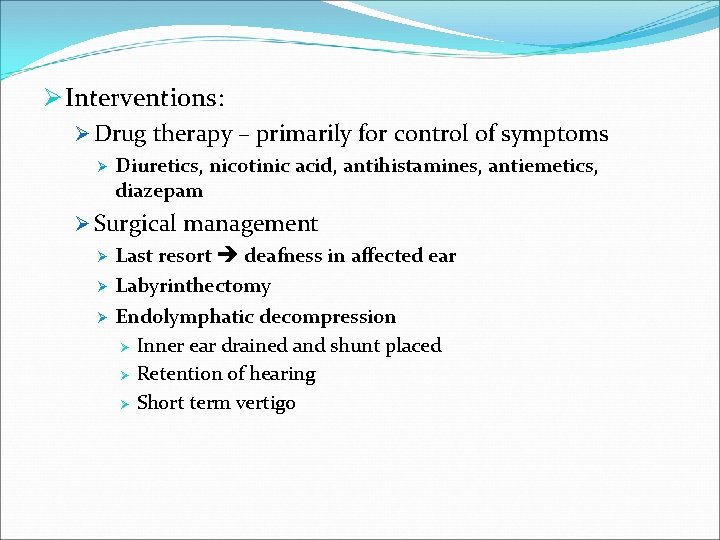
Ø Interventions: Ø Drug therapy – primarily for control of symptoms Ø Diuretics, nicotinic acid, antihistamines, antiemetics, diazepam Ø Surgical management Ø Last resort deafness in affected ear Ø Labyrinthectomy Ø Endolymphatic decompression Ø Inner ear drained and shunt placed Ø Retention of hearing Ø Short term vertigo
�Be sure to review Key Points at chapters end �You are also responsible for any general nursing care that would apply to the disease you have learned about, ie, hearing loss, etc.
 Types of interference in atomic absorption spectroscopy
Types of interference in atomic absorption spectroscopy Interferences
Interferences Primary needs and secondary needs
Primary needs and secondary needs Simple claustral complex
Simple claustral complex Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Primary needs and secondary needs
Primary needs and secondary needs Graves 2000
Graves 2000 Hp deprivation index
Hp deprivation index Maternal deprivation
Maternal deprivation Cultural deprivation theory bourdieu
Cultural deprivation theory bourdieu Vacation deprivation
Vacation deprivation Urban deprivation definition geography
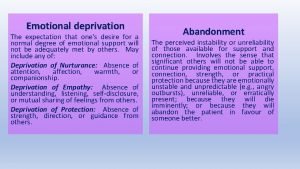
Urban deprivation definition geography Emotional deprevation
Emotional deprevation Malith kumarasinghe
Malith kumarasinghe Examples of cultural deprivation
Examples of cultural deprivation G v an bord uchtála 1980
G v an bord uchtála 1980 What is language deprivation
What is language deprivation